Abstract
Background:
Patients with major depressive disorder (MDD) usually have high risk of suicidality. Few studies have investigated the effects of stressful life events (SLEs) on the risk of suicide in Chinese patients who have developed MDD. This study aimed to investigate the impact of SLEs on suicidal risk in Chinese patients with MDD.
Methods:
In total, 1029 patients with MDD were included from nine psychiatric hospitals to evaluate the impact of SLEs on suicidal risk. Patients fulfilling the Mini-International Neuropsychiatric Interview (MINI) criteria for MDD were included in the study. Patients were excluded if they had lifetime or current diagnoses of psychotic disorder, bipolar disorder, and alcohol or substance dependence. Depressive symptoms were assessed by the 17-item Hamilton Depression Scale (HAMD-17). The suicidal risk of MDD patients was determined by the suicide risk module of MINI. SLEs were assessed by the Life Events Scale.
Results:
No gender difference was found for suicidal risk in MDD patients. Patients with suicidal risk had younger ages, lower education levels, more drinking behavior, and lower marriage rate, and fewer people had child and more severe depressive symptoms than nonsuicidal risk group. High-level perceived stressfulness (HPS) and number of SLEs that patients were exposed to were significantly greater in patients with suicidal risk than patients without. In multivariate logistic analysis, HPS of SLEs (odds ratio [OR] = 1.54, 95% confidence interval [CI]: 1.16–2.05, P = 0.003) and depressive symptoms (OR = 1.08, 95% CI: 1.05–1.11, P < 0.001) were associated with suicidal risk even after adjustment of gender, age, marriage, drinking behavior, and childless.
Conclusions:
HPS of SLEs is associated with suicide risk in Chinese patients with MDD. Further suicide prevention programs targeting this risk factor are needed.
Trial Registration:
ClinicalTrials.gov: NCT02023567; https://clinicaltrials.gov/ct2/show/NCT02023567?term=NCT02023567&rank=1.
Keywords: Life Stresses, Major Depressive Disorder, Suicide
摘要
背景:
抑郁症患者常有很高的自杀风险,但少有研究去探索中国抑郁症患者应激性生活事件对其自杀风险的影响。
方法学:
研究对象为来自我国9家精神卫生专科机构或综合医院精神科的1029名抑郁症患者,经简明国际神经精神访谈(MINI)检查,符合抑郁症诊断标准。排除标准为终身或现患的精神病性障碍、双相情感障碍、酒精或药物依赖。抑郁疾病严重度用17项汉密尔顿抑郁评定量表(HAMD-17)评估,自杀风险以MINI的自杀风险评估模块来判断。患者所经历的应激性生活事件由生活事件量表(LES)进行评估。
结果:
在抑郁症患者中,并未发现自杀风险存在男女性别差异。与低自杀风险的抑郁症患者相比,有自杀风险的抑郁症患者,其抑郁症状更加严重、起病年龄较小、教育程度更低、有更高比例的饮酒行为、结婚和有子女比例少。在应激性生活事件方面,与无自杀风险组相比,有自杀风险的患者遭遇应激性生活事件的次数更多,感知到的压力更重。在逻辑回归模型中,通过校正性别、年龄、婚姻状况、饮酒行为和有无子女,发现抑郁症患者的自杀风险与对应激性生活事件感知到的高水平压力(OR = 1.54, 95%CI:1.16–2.05, P = 0.003)以及抑郁症状 严重度显著相关(OR = 1.08, 95%CI:1.05–1.11, P < 0.001)。
结论:
在中国抑郁症患者中,自杀风险与患者遭遇应激性生活事件后感知到的高水平压力显著相关。在制定中国抑郁症自杀风险防治策略时,应当考虑到该危险因素,并针对性地进行监测和干预,以降低抑郁症患者的自杀风险。
INTRODUCTION
Suicide remains a significant leading cause of death worldwide.[1] Approximately 800,000 people died by suicide every year, and suicide poses a major public health challenge to worldwide, especially in low- and middle-income countries, due to 78% suicides occurred in those countries, including China.[2] Despite a remarkable reduction in suicide rate of China in the last two decades, accompanying its rapid economic progress,[3] China has 1.3 billion populations, suicide is still a major challenge to public health. Recently, a meta-analysis of the Chinese general population showed that about 50 million people had suicide ideation and 10 million people had suicide attempt in their lifetime.[3]
Major depressive disorder (MDD) is one of the most important risk factors for suicide.[4] Numerous studies have demonstrated that MDD is strongly associated with suicide.[4,5] A meta-analysis of 3275 suicide completers found that 87.3% of cases had a psychiatric disorder before their death,[5] of which 40–70% were diagnosed with depression.[6,7] Patients with depression also commonly presented with suicide risk; a meta-analysis of the Chinese patients with MDD presented that lifetime prevalence of suicide ideation and suicide attempt was 53.1% and 23.7%, respectively, and 1-month prevalence of suicide ideation and suicide attempt was 27.7% and 20.3%, respectively.[8] However, there were relatively scarce studies exploring risk factors of suicide in this diagnostic group.[9] To date, some studies[4,9] have been identified multitude of risk factors of suicide in patients with MDD, including male gender, family history of psychiatric disorder, previous attempted suicide, more severe depression, comorbid anxiety, and alcohol and drug abuse.
Suicidality arises from a complex interaction of components in which multiple adversities represent one of the most significant risk factors in the decision to take one's own life.[4,10,11] Suicide is associated with psychiatric, social, political, economic, cultural, and moral factors,[11,12] stressful life events (SLEs) have drawn much attention over the past four decades,[11] and accumulating evidence suggests that SLEs are closely associated with suicide.[10,11,12,13] Previous studies have demonstrated that people with suicidal risk often struggled with SLEs, such as interpersonal stressors,[11] conflicts with spouse or other family members,[14] and physical illnesses.[10,15] And, a study has shown that individuals who have suicide attempt were likely to have experienced a higher number of SLEs than those who have not.[16]
However, life stressors have also been identified as a risk factor for mental illness,[13] such as depression,[17,18] which is known to be an important intermediary of suicidality. It has been revealed that the relationship between SLEs and suicide is mediated by depression or depressive symptoms.[19,20] However, a review pointed out that the effects of SLEs on individual varied by individual's subjective or cognitive appraisals. Unfortunately, many studies have not taken it into account when they evaluated the effects of SLEs on suicide.
The role of SLEs that contribute to the suicidal risk of MDD remains unclear. Thus, the aim of this study was to determine whether SLEs increased the risk of suicide in Chinese patients with MDD, and whether the possible association is independent of depressive symptoms.
METHODS
Ethical approval
All procedures in this study were in accordance with the ethical standards of the Declaration of Helsinki. This study was approved by the Ethics Committee of Peking University Sixth Hospital (Approval No. 2013-29-1) and local ethics committee; all individuals provided written informed consent before taking part in this study (ClinicalTrials.gov identifier: NCT02023567).
Subjects
The rationale and design of this study have been described in detail elsewhere.[21] Briefly, patients with MDD were recruited from nine sites in China from December 2013 to December 2016. The enrolled patients, 18–55 years old, were diagnosed by validated Chinese version of the Mini-International Neuropsychiatric Interview (MINI, Version 5.0).[22] Patients were included if the following criteria were met: diagnosis of MDD based on MINI according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition-Text Revision, first-episode or relapse, and inpatients or outpatients. All patients were assessed by the Hamilton Depression Rating Scale 17-item (HAMD-17)[23] to evaluate the severity of depressive symptoms. In this study, item-3 (suicide assessment) score was not included in the total score of HAMD-17 because it was dependent variable. The exclusion criteria were as follows: lifetime or current diagnosis of psychotic disorder, bipolar disorder, alcohol or substance dependence, people suffering from severe physical disease, and women in pregnancy or breastfeeding.
Assessment of suicidality
Suicidality was assessed by the suicidal risk module of MINI with 6 questions, with a total score of MINI suicide module of 33. The risk of suicide was classified as “low” (score 1–5), “moderate” (score 6–9), and “high” (score 10). Following previous studies[24,25] and recommendation by authors of MINI, the risk for suicide was dichotomized as nonsuicidal risk (low or absent suicide risk) or suicidal risk (moderate or high risk).
Measurement of stressful life events
SLEs were assessed by the Life Events Scale (LES),[26] a self-report scale widely used in China that has favorable validity and reliability, in which a total of 48 items are classified into three dimensions: family life (28 items), work and study (13 items), and social interaction and other events (7 items). Life events involve serious illness, housing, relationship, social difficulties, relationship breakdowns, unemployment, and financial crises, etc. All patients described these life events as occurring within a 1-year period before participation.
The perceived stressfulness of each life event was calculated in four parts: the occurrence time of life events (absent = 1, before 1 year = 2, within 1 year = 3, and chronicity = 4), characteristic of life events (positive = 1 and negative = 2), influence on state of mind (absent = 1, mild = 2, moderate = 3, severe = 4, and extreme = 5), and duration of influence (within 3 months = 1, with 6 months = 2, within 1 year = 3, and over 1 year = 4). All life events were calculated to reflect the level of SLEs that patients have experienced with the following equation: total score of LES = the occurrence time of life events × characteristic of life events × influence of mind × duration of influence. The 75th percentile (a score of 32) in the sample was used as a cutoff value for grouping into the high-level perceived stressfulness (HPS) or low-level perceived stressfulness (LPS).[26]
LES was used to measure the perceived stressfulness and number of SLEs that patients exposed. A total of 48-item scale adequately captured complex life events experienced by patients, it can reflect both objectively occurring life events and subjectively perceived stressfulness of experienced life events, the latter is affected by individual cognitive appraisals to the same life events.
Statistical analysis
Demographic and clinical data were analyzed using Chi-square and t-test, as appropriate. To reduce type I error, Bonferroni multiple correction method was used to correct the number of SLE variables tested (family, work and study, and social interaction) using a P value of 0.017 (P = 0.05/3) as a marker of significance.
We used univariate analysis to preselect variables for inclusion in multivariate logistic analysis; predictors were chosen into final models by considering their clinical relevance or statistical significance of suicide in patients with MDD. Then, multivariate logistic regression was performed to identify the correlates of HPS and suicidal risk in patients with MDD (Model 1). A study has shown that individuals with multiple previous suicide attempts were exposed to higher number of SLEs compared with only one previous suicide attempt.[16] Accordingly, participants who had exposed SLEs were divided into three groups according to the number of SLEs: 1 ≤ SLEs ≤ 2, 3 ≤ SLEs ≤ 5, SLEs > 5, and compared with patients without SLE, to test the relationship between the number of SLEs and suicidal risk (Model 2). Both models were adjusted for gender, age, having no child, marriage, drinking, and depressive symptoms. All the statistical analyses were conducted using SPSS version 22.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
In total, 1100 patients with MDD participated in this study, and 61 patients with incomplete demographic data (work status, marriage, education, smoking, drinking, and has child or not) and clinical characteristics (number of depressive episode and assessment of HAMD-17) were excluded, and 10 patients lacking of information on the suicide risk module of MINI were also excluded. Finally, 1029 patients participated in this study.
Demographic and clinical characteristics
There was no statistically significant difference in gender, work status, BMI, smoking, and numbers of depressive episode between suicidal risk group and nonsuicidal risk group [Table 1]. Patients with suicidal risk were younger and better educated. There were significantly fewer married individuals or individuals with child in the suicidal risk group than nonsuicidal risk group, and patients with suicidal risk had higher rates of drinking behavior. The suicidal risk group presented more severe depressive symptoms comparing with nonsuicidal group, 23.2 and 20.0, respectively.
Table 1.
Demographic and clinical characteristics in patients with MDD
| Characteristics | Nonsuicidal risk group (n = 736) | Suicidal risk group (n = 293) | χ2/t | P |
|---|---|---|---|---|
| Age (years), n (%) | ||||
| 18≤ age ≤25 | 93 (12.6) | 56 (19.1) | 12.677 | 0.005 |
| 25< age ≤35 | 191 (26.0) | 88 (30.0) | ||
| 35< age ≤45 | 193 (26.2) | 72 (24.6) | ||
| 45< age ≤55 | 259 (35.2) | 77 (26.3) | ||
| Gender, n (%) | ||||
| Male | 216 (29.3) | 102 (34.8) | 2.931 | 0.087 |
| Female | 520 (70.7) | 191 (65.2) | ||
| Work status, n (%) | ||||
| No job | 231 (31.4) | 90 (30.7) | 0.044 | 0.978 |
| Part-time job | 15 (2.0) | 6 (2.0) | ||
| Full-time job | 490 (66.6) | 197 (67.2) | ||
| Marriage, n (%) | ||||
| Married | 551 (74.9) | 179 (61.1) | 19.287 | <0.001 |
| Divorced | 40 (5.4) | 25 (8.5) | ||
| Single | 145 (19.7) | 89 (30.4) | ||
| Education, n (%) | ||||
| Illiteracy | 5 (0.7) | 2 (0.7) | 19.858 | 0.001 |
| Primary school | 53 (7.2) | 12 (4.1) | ||
| Junior middle school | 194 (26.4) | 46 (15.7) | ||
| Senior middle school | 147 (20.0) | 76 (25.9) | ||
| Bachelor degree | 292 (39.7) | 133 (45.4) | ||
| Master degree and above | 45 (6.1) | 24 (8.2) | ||
| Smoking, n (%) | ||||
| Never | 588 (79.9) | 232 (79.2) | 1.799 | 0.407 |
| Former | 42 (5.7) | 12 (4.1) | ||
| Smoker | 106 (14.4) | 49 (16.7) | ||
| Drinking, n (%) | ||||
| Never | 546 (74.2) | 188 (64.2) | 12.519 | 0.002 |
| Former | 48 (6.5) | 19 (6.5) | ||
| Drinker | 142 (19.3) | 86 (29.4) | ||
| Childless, n (%) | 189 (25.7) | 114 (38.9) | 17.652 | <0.001 |
| BMI, mean (SD) | 22.9 (3.6) | 22.6 (3.3) | 1.311 | 0.190 |
| Number of depressive episode | 1.7 (2.0) | 1.8 (1.3) | −0.050 | 0.960 |
| HAMD-17* | 20.0 (4.6) | 23.2 (5.6) | −8.676 | <0.001 |
*HAMD-17 without item 3. MDD: Major depressive disorder; HAMD-17: 17-item Hamilton Depression Scale; SD: Standard deviation; BMI: Body mass index.
Suicidal risk assessment
Overall, 28.5% patients had suicidal risk according to the definition that described above; the rate of suicidal risk in male patients was higher than female patients, but the difference did not reach statistical significance [Table 1]. Among patients with MDD, 48.5% patients had suicidal ideation over the last month, 10.7% patients had a lifetime suicide attempt, and 5.4% patients had suicide attempt within the precious month.
Stressful life events assessment
Most of patients (82.2%) reported at least 1 SLE over the last year, 46.7% patients exposed at least 3 SLEs, and only 17.8% patients never experienced SLE within 1-year before participation [Table 2]. Patients with HPS of SLEs had suicidal risk significantly higher than patients with LPS of SLEs: 34.5% vs 23.4% (P < 0.001), and the number of SLEs that patients exposed was significantly higher in suicidal risk group than nonsuicidal risk group. Furthermore, in the subscale of LES, perceived stressfulness of family life (31.0 and 22.3, respectively, P = 0.001) and social interaction (5.5 and 3.0, respectively, P = 0.009) were significantly higher in patients with suicidal risk compared with patients without, and the differences remained significant even after Bonferroni correction [Figure 1]. The suicidal risk group had a higher perceived stressfulness of work and study than the suicidal risk group; however, the difference did not reach the statistical significance (17.0 and 14.4, respectively, P = 0.153).
Table 2.
Stressful life events in both groups
| Characteristics | Nonsuicidal risk group (n = 736) | Suicidal risk group (n = 293) | χ2/Z | P |
|---|---|---|---|---|
| Perceived stressfulness of SLEs, n (%) | ||||
| High-level | 307 (41.7) | 162 (55.3) | 15.577 | <0.001 |
| Low-level | 429 (58.3) | 131 (44.7) | ||
| Number of SLEs, n (%) | ||||
| 0 | 146 (19.8) | 37 (12.6) | 14.282 | 0.003 |
| 1≤ SLEs ≤2 | 267 (36.3) | 98 (33.4) | ||
| 3≤ SLEs ≤5 | 208 (28.3) | 89 (30.4) | ||
| SLEs >5 | 115 (15.6) | 69 (23.5) | ||
| LES subscale, median (P25, P75) | ||||
| Family life subscale | 6.0 (0, 32.0) | 18.0 (0, 46.0) | −4.342 | <0.001 |
| Work and learn subscale | 4.0 (0, 24.0) | 6.0 (0, 24.0) | −0.623 | 0.533 |
| Social interaction subscale | 0 (0, 0) | 0 (0, 0) | −3.071 | 0.002 |
SLEs: Stressful life events; LES: Life Events Scale.
Figure 1.
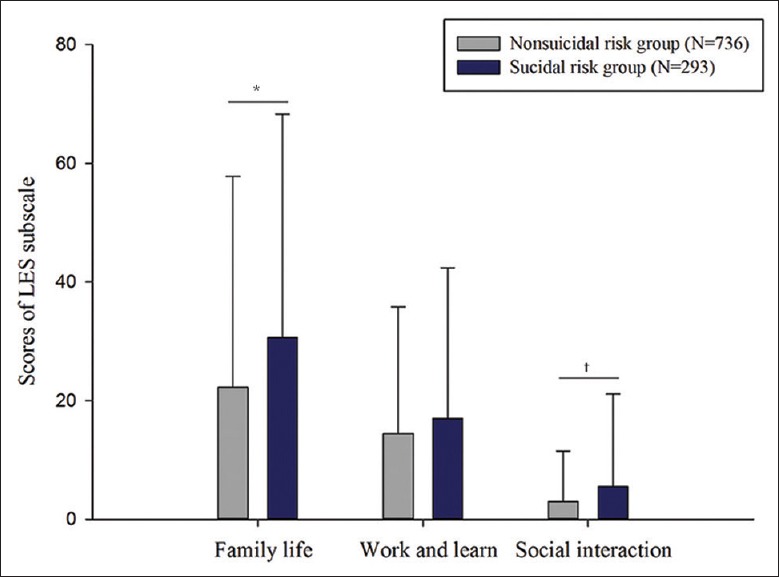
Subscales of SLEs in two groups. *P < 0.001, †P=0.002, nonsuicidal risk group compared with suicidal risk group. SLEs: Stressful life events; LES: Life Events Scale.
Univariate and multivariate logistic analyses
To investigate risk factors of suicide in patients with MDD, univariate analysis was performed. The results [Table 3] shown that patients with younger age was more likely to have suicidal risk than patients with older age, with increasing about 2-fold suicidal risk for patients in 18–25 years old than 45–55 years old. In addition, divorced, single, and childless individuals had increased the suicidal risk. As we expected, drinking behavior increased the risk of suicide, with the risk being 76% greater risk than patients who never drank before. Severity of depressive symptoms assessed by HAMD-17 can predict the risk of suicide; total score of 1 of HAMD-17 may increase suicidal risk by 7%.
Table 3.
Univariate analyses predicted suicidal risk in patients with MDD
| Characteristics | OR | 95% CI | P |
|---|---|---|---|
| Age (years) | |||
| 45< age ≤55 | 1.00 | – | – |
| 35< age ≤45 | 1.26 | 0.87–1.82 | 0.231 |
| 25< age ≤35 | 1.55 | 1.08–2.22 | 0.017 |
| 18≤ age ≤25 | 2.03 | 1.33–3.07 | 0.001 |
| Gender | |||
| Female | 1.00 | – | – |
| Male | 0.78 | 0.58–1.04 | 0.087 |
| Work status | |||
| No job | 1.00 | – | – |
| Part-time job | 1.03 | 0.38–2.73 | 0.958 |
| Full-time job | 1.03 | 0.77–1.39 | 0.834 |
| Marriage | |||
| Married | 1.00 | – | – |
| Divorced | 1.92 | 1.14–3.26 | 0.015 |
| Single | 1.89 | 1.38–2.58 | <0.001 |
| Education | |||
| Illiteracy | 1.00 | – | – |
| Primary school | 0.57 | 0.10–3.28 | 0.525 |
| Junior middle school | 0.59 | 0.11–3.15 | 0.540 |
| Senior middle school | 1.29 | 0.25–6.82 | 0.762 |
| Bachelor degree | 1.14 | 0.22–5.95 | 0.878 |
| Master degree and above | 1.33 | 0.24–7.39 | 0.742 |
| Smoking | |||
| Never | 1.00 | – | – |
| Former | 0.72 | 0.38–1.40 | 0.337 |
| Smoker | 1.17 | 0.81–1.70 | 0.403 |
| Drinking | |||
| Never | 1.00 | – | – |
| Former | 1.15 | 0.66–2.01 | 0.623 |
| Drinker | 1.76 | 1.28–2.41 | <0.001 |
| Having no child | 1.84 | 1.38–2.46 | <0.001 |
| BMI | 0.97 | 0.94–1.01 | 0.190 |
| Number of depressive episode | 1.00 | 0.93–1.08 | 0.960 |
| HAMD-17* | 1.07 | 1.04–1.10 | <0.001 |
| Perceived stressfulness of SLEs | |||
| Low-level | 1.00 | – | – |
| High-level | 1.73 | 1.32–2.27 | <0.001 |
| Number of SLEs | |||
| 0 | 1.00 | – | – |
| 1≤ SLEs ≤2 | 1.45 | 0.94–2.22 | 0.090 |
| 3≤ SLEs ≤5 | 1.69 | 1.09–2.62 | 0.019 |
| SLEs >5 | 2.37 | 1.48–3.78 | <0.001 |
–: No data. *: Score of item 3 is not included. MDD: Major depressive disorder; HAMD-17: 17-item Hamilton Depression Scale; BMI: Body mass index; SLEs: Stressful life events; OR: Odds ratio; CI: Confidence interval.
To test the association between SLEs and suicidal risk in patients with MDD, whether modulates by depressive symptoms and other risk factors, multivariate logistic analyses were used. A previous study has demonstrated that the association between SLEs and suicidal outcome varied by gender; therefore, gender being as a predictor was also entered into the final model.[19] Accordingly, all significant predictors of suicidal risk of MDD identified by univariate analyses, and gender identified by previous evidence, were evaluated together. Finally, gender, age, having no child, marriage, drinking and depressive symptoms, perceived stressfulness of SLEs, or number of SLEs were included in the final model.
In both multivariate logistic analyses [Table 4], depressive symptoms emerged as the most robust predictors of suicidal risk, but marriage, drinking, and having no child were no longer predictive. In Model 1, after adjusted for gender, age, marriage, drinking, having no children, and depressive symptoms, the results shown that perceived stressfulness of SLEs was still predicating suicidal risk in patients with MDD, with increased the risk by 54% in HPS than LPS. However, in Model 2, the number of SLEs was no longer predictive.
Table 4.
Multivariate analyses predicted suicidal risk in patients with MDD
| Characteristics | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | |
| Age (years) | ||||||
| 45< age ≤55 | 1.00 | – | – | 1.00 | – | – |
| 35< age ≤45 | 1.30 | 0.89–1.92 | 0.177 | 1.24 | 0.84–1.82 | 0.284 |
| 25< age ≤35 | 1.27 | 0.83–1.95 | 0.265 | 1.24 | 0.81–1.90 | 0.324 |
| 18≤ age ≤25 | 1.43 | 0.76–2.68 | 0.265 | 1.40 | 0.75–2.63 | 0.295 |
| Gender | ||||||
| Female | 1.00 | – | – | 1.00 | – | – |
| Male | 0.93 | 0.66–1.31 | 0.668 | 0.94 | 0.67–1.32 | 0.700 |
| Marriage | ||||||
| Married | 1.00 | – | – | 1.00 | – | – |
| Divorced | 1.53 | 0.87–2.68 | 0.139 | 1.57 | 0.90–2.76 | 0.112 |
| Single | 1.28 | 0.68–2.44 | 0.444 | 1.27 | 0.67–2.41 | 0.466 |
| Drinking | ||||||
| Never | 1.00 | – | – | 1.00 | – | – |
| Former | 1.03 | 0.56–1.90 | 0.928 | 1.01 | 0.55–1.84 | 0.954 |
| Drinker | 1.36 | 0.95–2.00 | 0.094 | 1.37 | 0.94–1.97 | 0.088 |
| Having no child | 1.41 | 0.79–2.50 | 0.244 | 1.39 | 0.78–2.47 | 0.260 |
| HAMD-17 | 1.08 | 1.05–1.11 | <0.001 | 1.08 | 1.05–1.11 | <0.001 |
| Perceived stressfulness of SLEs | ||||||
| Low-level | 1.00 | – | – | – | – | – |
| High-level | 1.54 | 1.16–2.05 | 0.003 | – | – | – |
| Number of SLEs | ||||||
| 0 | – | – | – | 1.00 | – | – |
| 1≤ SLEs ≤2 | – | – | – | 1.39 | 0.89–2.15 | 0.150 |
| 3≤ SLEs ≤5 | – | – | – | 1.36 | 0.87–2.17 | 0.171 |
| SLEs >5 | – | – | – | 1.65 | 1.00–2.72 | 0.049 |
–: No data; MDD: Major depressive disorder; HAMD-17: 17-item Hamilton Depression Scale; SLEs: Stressful life events; OR: Odds ratio; CI: Confidence interval.
DISCUSSION
The results of this study confirmed that HPS of SLEs increased the risk of suicide in Chinese patients with MDD, even after adjustment of gender, age, marriage, drinking, having no child, and depressive symptoms, but not the number of SLEs. To our best knowledge, this is the first time to investigate the effect of SLEs on suicide risk in a large MDD sample in China.
Our results showed that 28.5% of patients with current MDD had suicidal risk, which is in line with a national survey in China that 32.9% of patients with current MDD had suicidal risk assessed by MINI.[24] However, the lifetime and 1-month prevalence of suicide attempt in this study was 10.7% and 5.4%, respectively, which was notably lower than the results reported in a meta-analysis of Chinese patients with MDD, at 23.7% and 20.3%, respectively.[8] The reason for this discrepancy could be explained by inclusion of different criteria, given that this study had ruled out patients with drug or alcohol dependence, hypomania, and mania, which were all risk factors for suicide attempt.[4]
Admittedly, numerous studies have highlighted that SLEs are associated with self-injury, suicidal ideation, suicide attempt, and completed suicide.[10,11,13] However, most studies have utilized community rather than clinical sample, and the latter may provide a more stringent test of the relationship between SLEs and suicidal risk by taking into account concurrent psychopathology. Truly, SLEs have also been linked with MDD,[17] and the relationship between SLEs and suicidal risk may account for concurrent MDD. Some studies have shown that the effect of stressful event on suicide may be directly or indirectly modulate by MDD.[19,20,27]
Our results demonstrated that HPS of SLEs were associated with suicide risk in Chinese patients with MDD, independent of gender, age, marital status, and depressive symptoms. It is inconsistent with a previous study of Asian patients with MDD that found that negative life events associated with suicidality were partially mediated by depressive symptoms.[19] The failure to find an independent association may be related to two methodological limitations. First, the use of a short 12-item life events instrument may inadequately capture complex life events experienced by patients, rather than detect the association between life events and suicidality.[11] Second, the relationship between SLEs and suicide may be hindered by the time windows of assessment of SLEs and the suicidality, which SLEs were evaluated within 12 months prior to the onset of depressive symptoms rather than suicidality,[11] it posed a significant challenge to determine their relationship, and previous studies shown that recollection of major life events in adult tends to start fading after about a year.[28] Those limitations may attenuate the strength of the relationship between SLEs and suicide.
In addition, in multivariate analyses, we found that the number of SLEs that patients exposed was no longer predictive; however, the perceived stressfulness of SLEs had an independent effect on the risk for suicide in patients with MDD. It suggests that the effects of SLEs on suicidal risk may depend on individual cognitive appraisals of a life event, which is consistent with a review that we discussed previously.[13] Unfortunately, some studies[19,29] have not taken personal cognitive appraisals into account when they investigated the relationship between SLEs and suicidal risk in patients with MDD, resulted in its relationship be diluted.
Our study has several limitations. Given that this study was cross-sectional in design, it is impossible to identify causal relationships between SLEs and suicide risk in Chinese patients with MDD; a prospective study is needed to classify whether HPS of SLEs increases the risk for those patients. Second, SLEs were retrospectively collected; therefore, the findings of this study are subjected to recall bias. Third, this is a single-time-point assessment, recall bias for life events are problematic, because life events may not be adequately captured with long recall period. Multiple time-point assessments in a short time interval may be recommend. Finally, established structured interviews of suicide, such as the Columbia-Suicide Severity Rating Scale,[30] were needed to systematically measure the suicidality of patients with MDD.
These limitations notwithstanding, the strengths of this study are as follows: we conducted a stringent design to reduce the possibility of confounded relationships between SLEs and suicide. For example, patients were excluded if they were concurrent drug or substance dependence[4,9] and severe physical disease,[31] which were associated with suicide; also, as a review pointed out,[11] clinical samples rather than community samples are recommended in consideration of the fact that relationship between SLEs and suicidality may be mediated by mental disorders. Moreover, previous studies have revealed that the impact of SLEs on suicide varied by gender and the level of depressive symptoms;[19,32] thus, a rigorous test was performed to test the relationship between SLEs and suicide in patients with MDD by adjusting for gender, age, marriage, drinking, having no child, and depressive symptoms.
The findings have some practical implications. Many studies of suicide have been conducted in developed countries, and since China has different social, political, economic, and cultural contexts, these findings may not be applicable to the Chinese population.[3] Therefore, the identification of risk factors for suicide in Chinese patients with MDD is essential to develop suicide prevention strategies appropriately and effectively. This study confirmed that HPS of SLEs, rather than the number of SLEs, increased the risk of suicide independent of depressive symptoms in a large sample of MDD. There is good evidence that prediction of and intervention for suicidal risk in MDD may result in improving prevention strategies effectively and reducing suicide rates. A study has shown that individuals experiencing higher incidence of SLEs did not increase suicidal risk if they had moderate–high levels of self-appraisal.[33] This suggests that personal resilience may be a protective factor against suicidality. Stress management techniques may be needed to develop adaptive ways to cope with stressors;[34] also, behavior modification techniques and coping skills focused on the perceived stressfulness of SLEs are also needed, as individual resilience and self-appraisal may be enhanced when coupled with these strategies.
Our results indicate that HPS of SLEs are associated with suicide risk in Chinese patients with MDD. Prospective studies are warranted to determine causal relationships between HPS of SLEs and suicide risk in MDD. Further suicidal prevention strategies aimed at HPS of SLEs for Chinese patients with MDD may offer a more promising method of intervention.
Financial support and sponsorship
This study was supported by grants from the National Key Basic Research Program of China (973 Program) (No. 2013CB531305), the National Key Technology R and D Program (No. 2015BAI13B01), the National Natural Science Foundation of China (No. 81630031), the Beijing Municipal Science and Technology Project (No. Z171100000117016), and the Capital Foundation of Medicine Research and Development (No. 2016-1-4111).
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Yi Cui
REFERENCES
- 1.Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S, et al. Suicide and suicidal behavior. Epidemiol Rev. 2008;30:133–54. doi: 10.1093/epirev/mxn002. doi: 10.1093/epirev/mxn002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Geneva: World Health Organization; 2018. [Last accessed on 2018 Jan 28]. Mental Health: suicide Prevention. Available from: http://www.who.int/mental_health/suicide-prevention/en/ [Google Scholar]
- 3.Cao XL, Zhong BL, Xiang YT, Ungvari GS, Lai KY, Chiu HF, et al. Prevalence of suicidal ideation and suicide attempts in the general population of China: A meta-analysis. Int J Psychiatry Med. 2015;49:296–308. doi: 10.1177/0091217415589306. doi: 10.1177/0091217415589306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Turecki G, Brent DA. Suicide and suicidal behaviour. Lancet. 2016;387:1227–39. doi: 10.1016/S0140-6736(15)00234-2. doi: 10.1016/S0140-6736(15)00234-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arsenault-Lapierre G, Kim C, Turecki G. Psychiatric diagnoses in 3275 suicides: A meta-analysis. BMC Psychiatry. 2004;4:37. doi: 10.1186/1471-244X-4-37. doi: 10.1186/1471-244X-4- [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brådvik L, Mattisson C, Bogren M, Nettelbladt P. Mental disorders in suicide and undetermined death in the Lundby study. The contribution of severe depression and alcohol dependence. Arch Suicide Res. 2010;14:266–75. doi: 10.1080/13811118.2010.494146. doi: 10.1080/13811118.2010.494146. [DOI] [PubMed] [Google Scholar]
- 7.Rihmer Z. Suicide risk in mood disorders. Curr Opin Psychiatry. 2007;20:17–22. doi: 10.1097/YCO.0b013e3280106868. doi: 10.1097/YCO.0b013e3280106868. [DOI] [PubMed] [Google Scholar]
- 8.Dong M, Wang SB, Li Y, Xu DD, Ungvari GS, Ng CH, et al. Prevalence of suicidal behaviors in patients with major depressive disorder in China: A comprehensive meta-analysis. J Affect Disord. 2018;225:32–9. doi: 10.1016/j.jad.2017.07.043. doi: 10.1016/j.jad.2017.07.043. [DOI] [PubMed] [Google Scholar]
- 9.Hawton K, Casañas I Comabella C, Haw C, Saunders K. Risk factors for suicide in individuals with depression: A systematic review. J Affect Disord. 2013;147:17–28. doi: 10.1016/j.jad.2013.01.004. doi: 10.1016/j.jad.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 10.O'Connor RC, Nock MK. The psychology of suicidal behaviour. Lancet Psychiatry. 2014;1:73–85. doi: 10.1016/S2215-0366(14)70222-6. doi: 10.1016/S2215-0366(14)70222-6. [DOI] [PubMed] [Google Scholar]
- 11.Liu RT, Miller I. Life events and suicidal ideation and behavior: A systematic review. Clin Psychol Rev. 2014;34:181–92. doi: 10.1016/j.cpr.2014.01.006. doi: 10.1016/j.cpr.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 12.Aleman A, Denys D. Mental health: A road map for suicide research and prevention. Nature. 2014;509:421–3. doi: 10.1038/509421a. doi: 10.1038/509421a. [DOI] [PubMed] [Google Scholar]
- 13.Liu RT, Cheek SM, Nestor BA. Non-suicidal self-injury and life stress: A systematic meta-analysis and theoretical elaboration. Clin Psychol Rev. 2016;47:1–4. doi: 10.1016/j.cpr.2016.05.005. doi: 10.1016/j.cpr.2016.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang J, Ma Z. Patterns of life events preceding the suicide in rural young Chinese: A case control study. J Affect Disord. 2012;140:161–7. doi: 10.1016/j.jad.2012.01.010. doi: 10.1016/j.jad.2012.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Phillips MR, Yang G, Zhang Y, Wang L, Ji H, Zhou M, et al. Risk factors for suicide in China: A national case-control psychological autopsy study. Lancet. 2002;360:1728–36. doi: 10.1016/S0140-6736(02)11681-3. doi: 10.1016/S0140-6736(02)11681-3. [DOI] [PubMed] [Google Scholar]
- 16.Pompili M, Innamorati M, Szanto K, Di Vittorio C, Conwell Y, Lester D, et al. Life events as precipitants of suicide attempts among first-time suicide attempters, repeaters, and non-attempters. Psychiatry Res. 2011;186:300–5. doi: 10.1016/j.psychres.2010.09.003. doi: 10.1016/j.psychres.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 17.Kessler RC. The effects of stressful life events on depression. Annu Rev Psychol. 1997;48:191–214. doi: 10.1146/annurev.psych.48.1.191. doi: 10.1146/annurev.psych.48.1.191. [DOI] [PubMed] [Google Scholar]
- 18.Monroe SM, Harkness KL. Life stress, the “kindling” hypothesis, and the recurrence of depression: Considerations from a life stress perspective. Psychol Rev. 2005;112:417–45. doi: 10.1037/0033-295X.112.2.417. doi: 10.1037/0033-295X.112.2.417. [DOI] [PubMed] [Google Scholar]
- 19.Park S, Hatim Sulaiman A, Srisurapanont M, Chang SM, Liu CY, Bautista D, et al. The association of suicide risk with negative life events and social support according to gender in Asian patients with major depressive disorder. Psychiatry Res. 2015;228:277–82. doi: 10.1016/j.psychres.2015.06.032. doi: 10.1016/j.psychres.2015.06.032. [DOI] [PubMed] [Google Scholar]
- 20.Hardt J, Johnson JG. Suicidality, depression, major and minor negative life events: A mediator model. Psychosoc Med. 2010;7:Doc05. doi: 10.3205/psm000067. doi: 10.3205/psm000067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lv X, Si T, Wang G, Wang H, Liu Q, Hu C, et al. The establishment of the objective diagnostic markers and personalized medical intervention in patients with major depressive disorder: Rationale and protocol. BMC Psychiatry. 2016;16:240. doi: 10.1186/s12888-016-0953-z. doi: 10.1186/s12888-016-0953-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 23.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen L, Liu YH, Zheng QW, Xiang YT, Duan YP, Yang FD, et al. Suicide risk in major affective disorder: Results from a national survey in China. J Affect Disord. 2014;155:174–9. doi: 10.1016/j.jad.2013.10.046. doi: 10.1016/j.jad.2013.10.046. [DOI] [PubMed] [Google Scholar]
- 25.Pompili M, Rihmer Z, Akiskal H, Amore M, Gonda X, Innamorati M, et al. Temperaments mediate suicide risk and psychopathology among patients with bipolar disorders. Compr Psychiatry. 2012;53:280–5. doi: 10.1016/j.comppsych.2011.04.004. doi: 10.1016/j.comppsych.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 26.Yang DS, YL Z. Life Event Scale (LES). Rating scales for mental health (in Chinese) Chin Ment Health J. 1999;12:101–6. [Google Scholar]
- 27.Liu Y, Zhang J. The impact of negative life events on attempted suicide in rural China. J Nerv Ment Dis. 2017;206:187–194. doi: 10.1097/NMD.0000000000000727. doi: 10.1097/NMD.0000000000000727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Paykel ES. The interview for recent life events. Psychol Med. 1997;27:301–10. doi: 10.1017/s0033291796004424. doi: 10.1017/S0033291796004424. [DOI] [PubMed] [Google Scholar]
- 29.Mandelli L, Nearchou FA, Vaiopoulos C, Stefanis CN, Vitoratou S, Serretti A, et al. Neuroticism, social network, stressful life events: Association with mood disorders, depressive symptoms and suicidal ideation in a community sample of women. Psychiatry Res. 2015;226:38–44. doi: 10.1016/j.psychres.2014.11.001. doi: 10.1016/j.psychres.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 30.Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, et al. The columbia-suicide severity rating scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168:1266–77. doi: 10.1176/appi.ajp.2011.10111704. doi: 10.1176/appi.ajp.2011.10111704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brådvik L, Mattisson C, Bogren M, Nettelbladt P. Long-term suicide risk of depression in the Lundby cohort 1947-1997 – Severity and gender. Acta Psychiatr Scand. 2008;117:185–91. doi: 10.1111/j.1600-0447.2007.01136.x. doi: 10.1111/j.1600-0447.2007.01136.x. [DOI] [PubMed] [Google Scholar]
- 32.Leskelä U, Rytsälä H, Komulainen E, Melartin T, Sokero P, Lestelä-Mielonen P, et al. The influence of adversity and perceived social support on the outcome of major depressive disorder in subjects with different levels of depressive symptoms. Psychol Med. 2006;36:779–88. doi: 10.1017/S0033291706007276. doi: 10.1017/S0033291706007276. [DOI] [PubMed] [Google Scholar]
- 33.Johnson J, Gooding PA, Wood AM, Tarrier N. Resilience as positive coping appraisals: Testing the schematic appraisals model of suicide (SAMS) Behav Res Ther. 2010;48:179–86. doi: 10.1016/j.brat.2009.10.007. doi: 10.1016/j.brat.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 34.Weyrauch KF, Roy-Byrne P, Katon W, Wilson L. Stressful life events and impulsiveness in failed suicide. Suicide Life Threat Behav. 2001;31:311–9. doi: 10.1521/suli.31.3.311.24240. doi: 10.1521/suli.31.3.311.24240. [DOI] [PubMed] [Google Scholar]


