Abstract
Objective:
Rapid eye movement sleep behavior disorder (RBD) is characterized by dream enactment and loss of muscle atonia during rapid eye movement sleep. RBD is closely related to α-synucleinopathies including Parkinson's disease, dementia with Lewy bodies, and multiple system atrophy. Many studies have investigated the markers of imaging and neurophysiological, genetic, cognitive, autonomic function of RBD and their predictive value for neurodegenerative diseases. This report reviewed the progress of these studies and discussed their limitations and future research directions.
Data Sources:
Using the combined keywords: “RBD”, “neurodegenerative disease”, “Parkinson disease”, and “magnetic resonance imaging”, the PubMed/MEDLINE literature search was conducted up to January 1, 2018.
Study Selection:
A total of 150 published articles were initially identified citations. Of the 150 articles, 92 articles were selected after further detailed review. This study referred to all the important English literature in full.
Results:
Single-nucleotide polymorphisms in SCARB2 (rs6812193) and MAPT (rs12185268) were significantly associated with RBD. The olfactory loss, autonomic dysfunction, marked electroencephalogram slowing during both wakefulness and rapid eye movement sleep, and cognitive impairments were potential predictive markers for RBD conversion to neurodegenerative diseases. Traditional structural imaging studies reported relatively inconsistent results, whereas reduced functional connectivity between the left putamen and substantia nigra and dopamine transporter uptake demonstrated by functional imaging techniques were relatively consistent findings.
Conclusions:
More longitudinal studies should be conducted to evaluate the predictive value of biomarkers of RBD. Moreover, because the glucose and dopamine metabolisms are not specific for assessing cognitive cognition, the molecular metabolism directly related to cognition should be investigated. There is a need for more treatment trials to determine the effectiveness of interventions of RBD on preventing the conversion to neurodegenerative diseases.
Keywords: Dementia with Lewy Bodies, Multiple System Atrophy, Neurodegenerative Disease, Parkinson's Disease, Rapid Eye Movement Sleep Behavior Disorder
摘要
目标:
快速眼球运动睡眠期行为障碍(RBD)是一种以REM睡眠期间伴随梦境及肢体活动为特征的睡眠疾病。RBD与a-突触核 蛋白病密切相关,包括帕金森病、路易体痴呆和多系统萎缩。许多研究探讨RBD的神经影像和神经生理学、遗传学、认知、自主神经功能相关的生物学标记,及其对神经退行性疾病的预测价值。本综述对这些研究的进展进行回顾,并讨论其局限性和未来研究方向。
数据来源:
使用“RBD”、“神经退行性疾病”、“帕金森病”和“磁共振成像”结合的关键词,PubMed / MEDLINE文献检索到2018 年1月1日。
文献选择:
共有150篇已发表文章被初步确定为引文,其中92篇文章经过进一步详细审查后被选中。本综述全面分析了所有重要的英文全文。
结果:
SCARB2(rs6812193)和MAPT(rs12185268)的单核苷酸多态性与RBD显著相关。 清醒和快速眼动睡眠期间EEG减慢、嗅觉丧失、自主神经功能障碍、认知障碍是RBD转化为神经退行性疾病的潜在预测标记。传统的结构影像学研究结果相对不一致,而功能成像技术显示的左侧壳核和黑质的功能连接、多巴胺转运蛋白摄取的降低是相对一致的结果。
结论:
应进行更多的纵向研究来评估生物标记物对RBD转化为神经退行性疾病的预测价值。 此外,葡萄糖和多巴胺代谢的结果对于评估认知功能并不特异,因此应探讨与认知功能直接相关的代谢分子在RBD发病中的参与作用。另外需要更多的临床试验来确定RBD干预措施对于预防神经退行性疾病的有效性。
INTRODUCTION
Rapid eye movement (REM) sleep behavior disorder (RBD) is characterized by dream enactment and loss of muscle atonia during REM sleep. RBD is generally chronic, progressive, and usually affects 0.5% of the general population aged over 50 years and 7% of people aged over 70 years.[1] Furthermore, males had more aggressive RBD than females.[2,3] Idiopathic RBD (iRBD) refers to RBD in the absence of other neurological diseases, whereas symptomatic RBD is secondary to neurological diseases and medication.[2] It is reported that smoking, head injury, pesticide exposure, and farming were potential risk factors for iRBD.[4] The neural circuits responsible for REM sleep were centered on the pontine and medulla oblongata. In normal REM sleep, the glycinergic or gamma-aminobutyric acid (GABA) ergic premotor neurons in the ventromedial medulla and the spinal cord are activated by the descending glutamatergic fibers from sublaterodorsal nucleus (SLD) neurons. The function of motor neurons is in turn suppressed by premotor neurons, leading to muscle atonia.[5] In RBD, SLD pathology disinhibits the motor commands and results in loss of muscle atonia.[6,7] The iRBD has attracted increasing attention because it is an important precursor of neurodegenerative diseases, especially synucleinopathies including Parkinson's disease (PD), dementia with Lewy bodies (DLB), and multiple system atrophy (MSA). The primary goals of this review were to summarize the screening methods, diagnosis, predictive markers for conversion of RBD to neurodegenerative diseases, and treatment methods of RBD.
DIAGNOSIS OF RAPID EYE MOVEMENT SLEEP BEHAVIOR DISORDER
Screening probable rapid eye movement sleep behavior disorder with questionnaires
The REM Behavior Disorder Screening Questionnaire (RBDSQ) was made in German and English according to the International Classification of Sleep Disorders-II.[8] The RBDSQ is comprised of 10 items with 13 questions (yes/no) which involves the following aspects: frequency, dreaming content, nocturnal movements, injuries to self or bed partner, motor behaviors, nocturnal awakening, sleep disruption, and the presence of a neurological disease. This questionnaire showed a good internal consistency (Cronbach's α = 0.885) in RBD patients and two separate healthy control groups.
The RBDSQ was subsequently translated into Japanese (RBDSQ-J).[9] The RBDSQ-J showed good internal consistency (Cronbach's α = 0.87) and test-retest reliability (Cronbach's α = 0.84). Mean RBDSQ-J scores were significantly different between iRBD patients, obstructive sleep apnea (OSA) patients, and healthy controls, between men and women in all these groups.
The RBDSQ was also translated into Chinese in Hong Kong (RBDQ-HK),[10] which involves more information about the frequency and severity of RBD symptoms. The RBDQ-HK includes 13 questions, with each question answered on two scales: lifetime occurrence (don't know, no, yes) and frequency within recent 1 year (occurred in the last year, once or few times per year, once or few times per month, 1–2 times per week, and 3 + times per week). Questions 1 and 2 ask about dreams and nightmares, questions 3–5 cover the dream content, questions 6 and 7 cover vocalizations during sleep, questions 8–9 cover sleeping motor behavior, questions 10–12 cover injuries during sleep, and question 13 covers sleep disturbance. Internal consistency was excellent for the overall scale (0.90) and good for both factor 1 (0.86) and factor 2 (0.85).
For a more rapid screen of RBD, the Innsbruck RBD Inventory (RBD-I) with only 5 items and RBD Single-Question Screen (RBD1Q) were developed in 2012. Four years later, sleep screaming and yelling were included in a Chinese version of RBD1Q (RBD1Q-C) to obtain a higher sensitivity in 2016.[11]
Definite diagnosis of rapid eye movement sleep behavior disorder
The diagnosis of RBD was as follows: (1) Repeated sleep-related episodes of vocalization and/or motor behaviors. These behaviors are recorded by video polysomnography (vPSG) during REM sleep or based on clinical history. The behaviors showed very high night-to-night stability. The diagnosis of over 80% of RBD cases only required a single vPSG.[12] A second vPSG was necessary in 16% of RBD patients;[3] (2) REM sleep without atonia (RSWA) demonstrated by excessive amounts of elevated submental electromyogram (EMG)-activity or EMG switching. Simultaneous recording of the mentalis, flexor digitorum superficialis, and extensor digitorum brevis muscles provided the highest rates of REM sleep phasic EMG activity in patients with RBD.[13] Recording of EMG activity in the mentalis muscle and phasic EMG activity in the right and left flexor digitorum superficialis muscles in the upper limbs was also recommended;[14] (3) Absence of electroencephalogram (EEG) findings of epileptic activity unless RBD can be differentiated from concurrent epilepsy during REM sleep; and (4) The disturbances are not better explained by another sleep disorder, neurological disorder, mental disorder, and medication or substance abuse.[2]
Biomarkers of neurodegenerative diseases
Genetic biomarkers
Different genetic phenotypes might be helpful for the prediction of conversion of RBD to neurodegenerative diseases and development of targeted treatments of RBD patients. In candidate gene studies, single-nucleotide polymorphisms (SNPs) in SCARB2 (rs6812193) and MAPT (rs12185268) were significantly associated with RBD.[15] RBD patients who carried the USP25 SNP rs2823357 converted to α-synucleinopathies faster than who did not.[15] Patients with PD who carried GBA mutation had an odds ratio (OR) of 6.24 for RBD and an OR of 3.13 for probable RBD.[16] Carriers of the PINK1 SNP rs45478900 among BRD patients have a higher risk for conversion to PD (OR: 2.92) than noncarriers.[17] However, it seemed that the APOE*ε4 allele was not associated with both the risk of RBD occurrence and its conversion to any α-synucleinopathy.[18]
Imaging manifestations of rapid eye movement sleep behavior disorder
Magnetic resonance imaging
A large number of studies have used imaging techniques, including structural and functional magnetic resonance imaging (MRI), diffusion tensor imaging (DTI), and positron emission computed tomography (PET) to explore the abnormalities of brain structure and function related to iRBD and develop the biological markers related to the occurrence and development of RBD and its conversion to neurodegenerative diseases.
Earlier studies reported nonspecific brain changes in iRBD, such as white matter damage,[19] ventricular enlargement,[20] and cortical[19,20] or frontal lobe atrophy.[21] Since these abnormalities are widely present in the elderly, they lack specificity for the presentation of RBD. The voxel-based morphometry analysis did not observe changes in the white matter of iRBD, but rather increased hippocampal and parahippocampal gray matter density.[22] By comparing PD patients with and without iRBD and healthy controls, researchers found right thalamus gray matter volume decrease in PD patients with iRBD.[23] A larger sample study found a broader reduction in gray matter volume in PD patients with iRBD than those without RBD, which was distributed over the pons in the midbrain, hypothalamus, thalamus, putamen, amygdala, and anterior cingulate gyrus.[24]
A DTI study found that iRBD patients had reduced fractional anisotropy (degree of anisotropy of a diffusion process), but increased mean diffusivity (average magnitude of molecular displacement) in the brainstem.[22] Compared with healthy controls, there were extensive reductions in fractional anisotropy and increased mean diffusivity in patients with PD with and without RBD, whereas tract-based spatial statistics did not show any differences between the three groups.[24] However, in general, these traditional structural MRI and DTI studies reported relatively large heterogeneity and cannot find the characteristics of the early stage of diseases, so functional imaging studies are needed.
New functional imaging techniques provide a promising way to investigate the neural mechanism of RBD. Analysis of the substantia nigra-based functional connectivity showed significant differences in connectivity with the left putamen, the right precuneus, and the superior occipital gyrus in RBD patients compared to PD patients and healthy controls; the functional connectivity between the left putamen and substantia nigra in the RBD patients was lower than that of the healthy controls but higher than that of the PD patients, suggesting a continuous pathological change in RBD and PD.[25] Researchers found decreased low-frequency amplitude in the primary motor cortex in PD patients with BRD compared to those without BRD.[26] Another study found that there was an abnormal resting basal ganglia network in patients with PD and iRBD.[27] The specificity of this network in distinguishing iRBD or PD and healthy people was 74% and 78%, respectively. Neural mechanism of RBD is shown in Figure 1.
Figure 1.
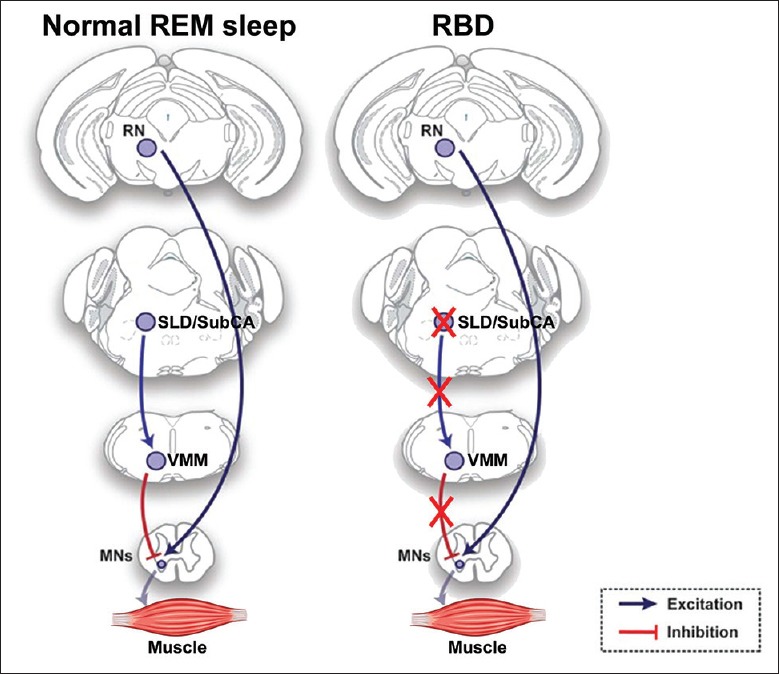
Schematic drawings of the brain circuits responsible for normal REM sleep and RBD presented in the rodent brain. The muscle tone is dually regulated by RN circuit and SLD-VMM circuit. The SLD-VMM circuit inhibits the MNs in normal REM sleep. However, the degeneration of the SLD releases MNs from inhibition in RBD. This resulted in the predominance of excitatory inputs generated by RN during REM sleep. REM: Rapid eye movement; RBD: Rapid eye movement sleep behavior disorder; SLD: Sublaterodorsal nucleus; SubCA: α part of subcoeruleus nucleus; VMM: Ventromedial medulla; MNs: Motor neurons; RN: Red nucleus.
However, no studies examined brain activation abnormalities in the implementation of cognitive tasks in iRBD patients. Therefore, whether brain activation abnormalities related to cognitive processing have been occurred in RBD and, if occurred, whether it can specifically predict the conversion of RBD to neurodegenerative diseases remain to be verified.
Positron emission computed tomography
RBD is associated with abnormalities in multiple neurotransmitter systems. Previous studies have mainly investigated the glucose and dopamine metabolisms in iRBD patients. A study using fluorodeoxyglucose-PET imaging found a brain network associated with PD motor symptoms,[28] which was characterized by increased glucose metabolism in the thalamus, lenticular nucleus, and precentral gyrus, and decreased glucose metabolism in the motor area of prefrontal lobe and parieto-occipital areas. Further, a study has found that RBD patients had increased thalamus, medial frontal gyrus, sensorimotor area, hippocampus, supramarginal gyrus, and posterior cerebellum, but had decreased metabolism in the occipital lobe and temporal gyrus.[29]
The decrease in dopamine transporter (DAT) uptake is an effective imaging marker that indicates the development of iRBD to α-synaptic proteinopathy. A study has found that when healthy people developed subclinical RBD, there was a progressive decrease in striatal DAT.[30] The reduction of DAT in the striatum and putamen was associated with a high risk of α-synaptic proteinopathy.[31] However, the glucose and dopamine metabolisms are not specific for reflecting cognitive function.
Olfactory dysfunction
A number of studies showed that olfactory dysfunction could help to identify patients with iRBD who are at a high risk of conversion to α-synucleinopathy. It was reported that RBD patients with olfactory impairment had 35.7–97.0% conversion rate to α-synucleinopathy, significantly higher than 2.5–16.6% of healthy populations.[32,33,34] Olfactory dysfunction could also predict the conversion of patients with iRBD to mild Parkinsonism and Lewy body disease.[35,36] Nevertheless, the exact causal relation between olfactory dysfunction and iRBD needs to be assessed.
Autonomic dysfunction
Studies using a variety of autonomic function assessments have suggested that the autonomic dysfunction in iRBD was associated with an increased risk of conversion to neurodegenerative diseases.[37,38] It has been reported that RBD patients experienced more severe impairments in gastrointestinal, urinary, and cardiovascular functions, tonic (vagal) and phasic (sympathetic) activities, heart rate response to leg movements, cardiac sympathetic denervation, as well as heart rate variability than that of controls;[39,40,41,42] the degree of autonomic dysfunction was intermediate between PD patients and healthy controls.[41] However, the predictive effectiveness of autonomic function tests for the risk of conversion of RBD to α-synucleinopathy needs to be clarified in future longitudinal studies.
Electroencephalogram
Studies revealed marked EEG slowing in the central and occipital regions during both wakefulness and REM sleep and a loss of resting-state delta-band functional connectivity in patients with iRBD compared with healthy controls.[43,44,45,46,47,48] The EEG pattern shown in RBD patients was similar to that of patients with DLB or PD.[47] The slowing during wakefulness in the posterior cortical regions predicted an increased risk of conversion of RBD to DLB or PD.[48]
Neuropsychological assessments
Progressive decline of cognitive function is an important clinical feature of PD. Compared with motor function, the impairment of cognitive function can affect the ability of daily living and social function. Studies have reported cognitive impairments in RBD patients in several domains,[49,50,51,52,53] including the visuospatial function, attention, executive function, verbal memory, short-term visual memory, and decision-making. The working memory worsened over time in RBD patients during 4-year follow-up.[54] The attention and executive function assessed by the Stroop Color Word Test and Trail Making Test could distinguish the RBD patients who converted to PD from those who converted to DLB.[55] Increased pareidolic responses might be a predictor of conversion of RBD patients to DLB.[56]
RBD can gradually develop similar cognitive symptoms to neurodegenerative diseases as the disease progresses. Data showed that about 50% of patients with iRBD had mild cognitive impairment.[57] Patients with iRBD had impaired linguistic and nonverbal learning and visual space capability.[58,59] Recent studies have shown that event-related memory and prospective memory were impaired in patients with iRBD.[60] A study involving 21 iRBD patients, 26 PD patients, and 26 healthy controls found that the accuracy of visual short-term memory was significantly reduced in patients with iRBD and PD, suggesting that there was a similarity in working memory impairments between them.[55] Even some studies found that iRBD patients were more likely to have impaired word memory and visual space function regardless of whether they had PD,[61] and iRBD without dementia also had a progressive decline in memory and executive functions.[55] The above studies suggested that cognitive impairment, RBD, and PD interacted with each other. Compared with other measures, such as olfactory loss, autonomic dysfunction, and psychiatric symptoms, cognitive impairment was a relatively specific risk factor for the development of neurodegenerative diseases in iRBD patients.
RAPID EYE MOVEMENT SLEEP BEHAVIOR DISORDER AND NEURODEGENERATIVE DISEASES
RBD is closely related to neurodegenerative diseases, especially synucleinopathies including PD, DLB, and MSA. The fact that RBD is a synucleinopathy was evidenced by the presence of prodromal neurodegenerative abnormalities including hyposmia, constipation, and orthostatic hypotension.[2] Braak hypothesis of Lewy pathology progression proposed that a systematic spread of α-synuclein initiated from the olfactory system and brain stem.[62] Meanwhile, RBD can also occur in the context of OSA and narcolepsy. However, whether RBD is correlated with tauopathy is controversial. RBD has been observed in patients with tau-related diseases such as Alzheimer's disease (AD), progressive supranuclear palsy (PSP), and frontotemporal dementia.[6,63] Other studies have reported RBD or RSWA in PSP and AD.[64,65]
Almost 90% of iRBD patients ultimately developed a defined neurodegenerative disease during follow-up period. It was reported that 76 patients with a definite diagnosis of iRBD ended up with PD in 39 patients (51%), DLB in 20 patients (26%), minimal cognitive impairment (MCI) in 9 patients (12%), and MSA in 2 patients (3%).[2] The risk of developing neurodegenerative diseases in iRBD patients was 18% within 5-year follow-up, 41% within 10-year follow-up, and 52% within 12-year follow-up.[1]
Rapid eye movement sleep behavior disorder and Parkinson's disease
The prevalence of RBD in PD ranged from 30% to 41%. An increase in RBD was observed in PD patients during 2-year follow-up, and approximately 65–75% of patients with PD and RBD were male.[66]
Zhou et al.[67] found that PD patients with RBD had more severe olfactory dysfunction than those without RBD. RBD was associated with the severity and frequency of nonmotor symptoms, particularly depressive symptoms, sleep disturbances, and fatigue, in early PD.[68,69] A longer disease duration, lower activity of daily living scores, frequent nighttime awakening, and hallucinations were reported in PD patients with RBDSQ ≥6, compared to those with RBDSQ scores <6.[11] Furthermore, RBD was also related to the subtype of motor symptoms on PD. RBD was more predominant in the rigid-akinetic subtype than in the tremoric subtype.[2] Overall, the presence of RBD in PD predicted a relatively poor prognosis.
Rapid eye movement sleep behavior disorder and minimal cognitive impairment/dementia with Lewy bodies
MCI acts as an intermediate state between normal cognitive function and dementia. RBD predicted a high risk of developing MCI.[57] Attention, episodic verbal memory, executive functions, and nonverbal learning were mostly affected in iRBD patients.[57] EEG slowing was demonstrated to be a potential diagnostic tool for cognitive decline in iRBD patients.[46]
Molano et al.[70] reported that iRBD patients who met MCI criteria subsequently developed autopsy-proven Lewy body disease. It was suggested that RBD patients with MCI predicted a high risk for developing DLB.[51] DLB always has cognitive decline, RBD, and visual hallucinations or fluctuations.[71] DLB patients with RBD exhibited more severe hypometabolism in the frontal regions, precuneus, superior parietal lobule, rolandic operculum, and amygdala, compared to those without RBD.[72]
Rapid eye movement sleep behavior disorder and multiple system atrophy
It was reported that more than half of the MSA patients exhibited symptoms of RBD before the onset of motor deficits.[73] On the other hand, PSG-confirmed RBD was present in 88% of MSA patients.[73] However, the male predominance was not observed in MSA patients with RBD.[74] The severity of RBD depended on the degree of monoaminergic neuron loss in the striatum of MSA patients.[63] Wang et al.[75] reported that the tonic EMG density during RBD in MSA group was higher than that of PD group, suggesting that tonic EMG density served as a potential marker for distinguishing MSA from PD.
MANAGEMENT OF RAPID EYE MOVEMENT SLEEP BEHAVIOR DISORDER
The treatment of RBD mainly includes three aspects as follows:
Strategy to prevent self-injury and injury of bed partner
The strategy should be used to prevent self-injury and injury of bed partner, such as placing mattresses or foam cushions on the floor, removing firearms from the bedroom, advising separate bedrooms to prevent bed partner, a bed alarm to alert the patients during RBD behaviors, and treatment of comorbid OSA.
Withdrawal medications
Drugs that can worsen the frequency and severity of RBD, such as antidepressants, mirtazapine, beta-blockers, or tramadol, should either be discontinued or reduced if medically appropriate. Patients should avoid alcohol abuse and withdrawal, which may worse RBD.
Pharmacotherapy
Since the presence of iRBD strongly predicts an eventual conversion to neurodegenerative diseases, how to prevent this conversion is of great importance in the treatment of iRBD. Two main pharmacological treatments of RBD are clonazepam and melatonin. Clonazepam modulates motor behaviors and dreaming but does not reduce RSWA. Adverse effects include sexual dysfunction, sedation, and imbalance. Although clonazepam is the first-line therapy, it should be carefully monitored over time if patients with RBD have dementia, gait disorders, or OSA[76] because it may exacerbate comorbid OSA and cognitive impairment. Melatonin increases REM sleep atonia levels, thereby diminishing RSWA. Melatonin exhibited a favorable safety, high tolerability, and limited drug–drug interactions.[77] It was reported that melatonin-treated patients had obviously less frequent adverse effects than those treated with clonazepam.[76,77] The adverse effects include the carryover of sedation to the next morning, headache, or daytime sleepiness, which are often dose dependent and can be improved by lowering the dose. The recommended starting dose of melatonin is 3 mg, which can be increased gradually to 6–12 mg, with the average effective dose of 6 mg.
Other RBD treatments which showed efficacy in small-sample clinical trials included pramipexole, donepezil, ramelteon, and cannabinoids.[78,79] Acetylcholinesterase inhibitors may be considered in patients with RBD and a concomitant synucleinopathy.[76] It was reported that plant extracts such as Scutellaria pinnatifida, ginkgolide, bilobalide, and curcumin prevented dopaminergic neurons from α-synuclein toxicity.[80,81,82] Biochemically designed compounds such as KISVRV, GQTYVLPG, and 20C were also demonstrated to disrupt α-synuclein pathogenesis.[83,84] It is presumed that using medications targeting at α-synuclein can retard the conversion of iRBD to neurodegenerative diseases. Further studies on these compounds are required to verify their efficacy and safety for further applications on iRBD patients.
There is no conclusion yet for the treatment of RBD by traditional Chinese medicine. Combined with the characteristics of RBD, the treatment methods to soothe the nerves, prevent wind, and calm the liver can be used. It has been reported that traditional Chinese medicine named “Yi Gan Powder” (including Atractylodes lancea, Poria, Chuanxiong, Angelica, Bupleurum, Radix Glycyrrhizae, and Uncaria) can alleviate RBD.[76] Its mechanism might be related to the influence of GABAergic and serotonergic neurons.
PERSPECTIVES
Previous imaging studies of iRBD were mostly of cross-sectional design and could not evaluate the predictive significance of the indicators for RBD outcomes. In the future, more longitudinal follow-up studies should be conducted to evaluate the predictive significance of biological markers for the conversion of RBD to various types of neurodegenerative diseases. Many well-established predictive biomarkers for neurodegenerative diseases are frequent in the elderly population (such as constipation and depression), which thus are nonspecific. As a highly potential marker to predict the conversion of RBD to neurodegenerative diseases among various markers, the cognitive impairments and its neural mechanisms should be investigated using functional imaging techniques such as resting-state and cognitive task-based fMRI. Moreover, the results of glucose and dopamine metabolisms examined by PET are not specific for assessing cognitive cognition, so the abnormalities of molecular metabolism directly related to cognition such as acetylcholine receptors in RBD patients should be investigated. More treatment trials to determine the effectiveness of interventions of RBD on preventing or slowing down their conversion to neurodegenerative diseases are needed in the future.
Financial support and sponsorship
This study was supported by grants from the National Natural Science Foundation of China (No. 81571294 and No. 81301208) and the National Natural Science Youth Foundation of China (No. 81701779).
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Xin Chen
REFERENCES
- 1.Gagnon JF, Bertrand JA, Génier Marchand D. Cognition in rapid eye movement sleep behavior disorder. Front Neurol. 2012;3:82. doi: 10.3389/fneur.2012.00082. doi: 10.3389/fneur.2012.000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fulda S. Idiopathic REM sleep behavior disorder as a long-term predictor of neurodegenerative disorders. EPMA J. 2011;2:451–8. doi: 10.1007/s13167-011-0096-8. doi: 10.1007/s13167-011-0096-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schenck CH. Expanded insights into idiopathic REM sleep behavior disorder. Sleep. 2016;39:7–9. doi: 10.5665/sleep.5300. doi: 10.5665/sleep.5300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Postuma RB, Montplaisir JY, Pelletier A, Dauvilliers Y, Oertel W, Iranzo A, et al. Environmental risk factors for REM sleep behavior disorder: A multicenter case-control study. Neurology. 2012;79:428–34. doi: 10.1212/WNL.0b013e31825dd383. doi: 10.1212/WNL.0b013e31825dd383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arrigoni E, Chen MC, Fuller PM. The anatomical, cellular and synaptic basis of motor atonia during rapid eye movement sleep. J Physiol. 2016;594:5391–414. doi: 10.1113/JP271324. doi: 10.1113/JP271324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chen MC, Yu H, Huang ZL, Lu J. Rapid eye movement sleep behavior disorder. Curr Opin Neurobiol. 2013;23:793–8. doi: 10.1016/j.conb.2013.02.019. doi: 10.1016/j.conb. 2013.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ramaligam V, Chen MC, Saper CB, Lu J. Perspectives on the rapid eye movement sleep switch in rapid eye movement sleep behavior disorder. Sleep Med. 2013;14:707–13. doi: 10.1016/j.sleep.2013.03.017. doi: 10.1016/j.sleep.2013.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stiasny-Kolster K, Mayer G, Schäfer S, Möller JC, Heinzel-Gutenbrunner M, Oertel WH, et al. The REM sleep behavior disorder screening questionnaire – A new diagnostic instrument. Mov Disord. 2007;22:2386–93. doi: 10.1002/mds.21740. doi: 10.1002/mds.21740. [DOI] [PubMed] [Google Scholar]
- 9.Miyamoto T, Miyamoto M, Iwanami M, Kobayashi M, Nakamura M, Inoue Y, et al. The REM sleep behavior disorder screening questionnaire: Validation study of a Japanese version. Sleep Med. 2009;10:1151–4. doi: 10.1016/j.sleep.2009.05.007. doi: 10.1016/j.sleep.2009.05.007. [DOI] [PubMed] [Google Scholar]
- 10.Li SX, Wing YK, Lam SP, Zhang J, Yu MW, Ho CK, et al. Validation of a new REM sleep behavior disorder questionnaire (RBDQ-HK) Sleep Med. 2010;11:43–8. doi: 10.1016/j.sleep.2009.06.008. doi: 10.1016/j.sleep.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 11.Ma JF, Hou MM, Tang HD, Gao X, Liang L, Zhu LF, et al. REM sleep behavior disorder was associated with Parkinson's disease: A community-based study. BMC Neurol. 2016;16:123. doi: 10.1186/s12883-016-0640-1. [Google Scholar]
- 12.Frauscher B, Iranzo A, Högl B, Casanova-Molla J, Salamero M, Gschliesser V, et al. Quantification of electromyographic activity during REM sleep in multiple muscles in REM sleep behavior disorder. Sleep. 2008;31:724–31. doi: 10.1093/sleep/31.5.724. doi: 10.1093/sleep/31.5.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Frauscher B, Iranzo A, Gaig C, Gschliesser V, Guaita M, Raffelseder V, et al. Normative EMG values during REM sleep for the diagnosis of REM sleep behavior disorder. Sleep. 2012;35:835–47. doi: 10.5665/sleep.1886. doi: 10.5665/sleep.1886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Louter M, Arends JB, Bloem BR, Overeem S. Actigraphy as a diagnostic aid for REM sleep behavior disorder in Parkinson's disease. BMC Neurol. 2014;14:76. doi: 10.1186/1471-2377-14-76. doi: 10.1186/1471-2377-14- [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gan-Or Z, Girard SL, Noreau A, Leblond CS, Gagnon JF, Arnulf I, et al. Parkinson's disease genetic loci in rapid eye movement sleep behavior disorder. J Mol Neurosci. 2015;56:617–22. doi: 10.1007/s12031-015-0569-7. doi: 10.1007/s12031-015-0569-7. [DOI] [PubMed] [Google Scholar]
- 16.Gan-Or Z, Mirelman A, Postuma RB, Arnulf I, Bar-Shira A, Dauvilliers Y, et al. GBA mutations are associated with rapid eye movement sleep behavior disorder. Ann Clin Transl Neurol. 2015;2:941–5. doi: 10.1002/acn3.228. doi: 10.1002/acn3.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Puschmann A, Fiesel FC, Caulfield TR, Hudec R, Ando M, Truban D, et al. Heterozygous PINK1 p.G411S increases risk of Parkinson's disease via a dominant-negative mechanism. Brain. 2017;140:98–117. doi: 10.1093/brain/aww261. doi: 10.1093/brain/aww261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gan-Or Z, Montplaisir JY, Ross JP, Poirier J, Warby SC, Arnulf I, et al. The dementia-associated APOE ε4 allele is not associated with rapid eye movement sleep behavior disorder. Neurobiol Aging. 2017;49:218e13–7. doi: 10.1016/j.neurobiolaging.2016.10.002. doi: 10.1016/j.neurobiolaging.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 19.Mazza S, Soucy JP, Gravel P, Michaud M, Postuma R, Massicotte-Marquez J, et al. Assessing whole brain perfusion changes in patients with REM sleep behavior disorder. Neurology. 2006;67:1618–22. doi: 10.1212/01.wnl.0000242879.39415.49. doi: 10.1212/01.wnl.0000242879.39415.49. [DOI] [PubMed] [Google Scholar]
- 20.Lee JH, Han YH, Cho JW, Lee JS, Lee SJ, Kim DJ, et al. Evaluation of brain iron content in idiopathic REM sleep behavior disorder using quantitative magnetic resonance imaging. Parkinsonism Relat Disord. 2014;20:776–8. doi: 10.1016/j.parkreldis.2014.03.023. doi: 10.1016/j.parkreldis.2014.03.023. [DOI] [PubMed] [Google Scholar]
- 21.Rahayel S, Montplaisir J, Monchi O, Bedetti C, Postuma RB, Brambati S, et al. Patterns of cortical thinning in idiopathic rapid eye movement sleep behavior disorder. Mov Disord. 2015;30:680–7. doi: 10.1002/mds.25820. doi: 10.1002/mds.25820. [DOI] [PubMed] [Google Scholar]
- 22.Scherfler C, Frauscher B, Schocke M, Iranzo A, Gschliesser V, Seppi K, et al. White and gray matter abnormalities in idiopathic rapid eye movement sleep behavior disorder: A diffusion-tensor imaging and voxel-based morphometry study. Ann Neurol. 2011;69:400–7. doi: 10.1002/ana.22245. doi: 10.1002/ana.22245. [DOI] [PubMed] [Google Scholar]
- 23.Salsone M, Cerasa A, Arabia G, Morelli M, Gambardella A, Mumoli L, et al. Reduced thalamic volume in Parkinson disease with REM sleep behavior disorder: Volumetric study. Parkinsonism Relat Disord. 2014;20:1004–8. doi: 10.1016/j.parkreldis.2014.06.012. doi: 10.1016/j.parkreldis.2014.06.012. [DOI] [PubMed] [Google Scholar]
- 24.Lim JS, Shin SA, Lee JY, Nam H, Lee JY, Kim YK, et al. Neural substrates of rapid eye movement sleep behavior disorder in Parkinson's disease. Parkinsonism Relat Disord. 2016;23:31–6. doi: 10.1016/j.parkreldis.2015.11.027. doi: 10.1016/j.parkreldis.2015.11.027. [DOI] [PubMed] [Google Scholar]
- 25.Ellmore TM, Castriotta RJ, Hendley KL, Aalbers BM, Furr-Stimming E, Hood AJ, et al. Altered nigrostriatal and nigrocortical functional connectivity in rapid eye movement sleep behavior disorder. Sleep. 2013;36:1885–92. doi: 10.5665/sleep.3222. doi: 10.5665/sleep.3222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li D, Huang P, Zang Y, Lou Y, Cen Z, Gu Q, et al. Abnormal baseline brain activity in Parkinson's disease with and without REM sleep behavior disorder: A resting-state functional MRI study. J Magn Reson Imaging. 2017;46:697–703. doi: 10.1002/jmri.25571. doi: 10.1002/jmri.25571. [DOI] [PubMed] [Google Scholar]
- 27.Rolinski M, Griffanti L, Piccini P, Roussakis AA, Szewczyk-Krolikowski K, Menke RA, et al. Basal ganglia dysfunction in idiopathic REM sleep behaviour disorder parallels that in early Parkinson's disease. Brain. 2016;139:2224–34. doi: 10.1093/brain/aww124. doi: 10.1093/brain/aww124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tang CC, Poston KL, Dhawan V, Eidelberg D. Abnormalities in metabolic network activity precede the onset of motor symptoms in Parkinson's disease. J Neurosci. 2010;30:1049–56. doi: 10.1523/JNEUROSCI.4188-09.2010. doi: 10.1523/JNEUROSCI.4188-09.2010.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wu P, Yu H, Peng S, Dauvilliers Y, Wang J, Ge J, et al. Consistent abnormalities in metabolic network activity in idiopathic rapid eye movement sleep behaviour disorder. Brain. 2014;137(Pt 12):3122–8. doi: 10.1093/brain/awu290. doi: 10.1093/brain/awu290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Arnaldi D, De Carli F, Picco A, Ferrara M, Accardo J, Bossert I, et al. Nigro-caudate dopaminergic deafferentation: A marker of REM sleep behavior disorder? Neurobiol Aging. 2015;36:3300–5. doi: 10.1016/j.neurobiolaging.2015.08.025. doi: 10.1016/j.neurobiolaging.2015.08.025. [DOI] [PubMed] [Google Scholar]
- 31.Iranzo A, Valldeoriola F, Lomeña F, Molinuevo JL, Serradell M, Salamero M, et al. Serial dopamine transporter imaging of nigrostriatal function in patients with idiopathic rapid-eye-movement sleep behaviour disorder: A prospective study. Lancet Neurol. 2011;10:797–805. doi: 10.1016/S1474-4422(11)70152-1. doi: 10.1016/S1474-4422(11)70152-1. [DOI] [PubMed] [Google Scholar]
- 32.Rossi M, Perez-Lloret S, Millar Vernetti P, Drucaroff L, Costanzo E, Ballesteros D, et al. Olfactory dysfunction evaluation is not affected by comorbid depression in Parkinson's disease. Mov Disord. 2015;30:1275–9. doi: 10.1002/mds.26276. doi: 10.1002/mds.26276. [DOI] [PubMed] [Google Scholar]
- 33.Postuma RB, Lang AE, Massicotte-Marquez J, Montplaisir J. Potential early markers of Parkinson disease in idiopathic REM sleep behavior disorder. Neurology. 2006;66:845–51. doi: 10.1212/01.wnl.0000203648.80727.5b. doi: 10.1212/01.wnl.0000203648.80727.5b. [DOI] [PubMed] [Google Scholar]
- 34.Postuma RB, Gagnon JF, Vendette M, Montplaisir JY. Markers of neurodegeneration in idiopathic rapid eye movement sleep behaviour disorder and Parkinson's disease. Brain. 2009;132(Pt 12):3298–307. doi: 10.1093/brain/awp244. doi: 10.1093/brain/awp244. [DOI] [PubMed] [Google Scholar]
- 35.Mahlknecht P, Kiechl S, Stockner H, Willeit J, Gasperi A, Poewe W, et al. Predictors for mild Parkinsonian signs: A prospective population-based study. Parkinsonism Relat Disord. 2015;21:321–4. doi: 10.1016/j.parkreldis.2014.12.021. doi: 10.1016/j.parkreldis.2014.12.021. [DOI] [PubMed] [Google Scholar]
- 36.Mahlknecht P, Iranzo A, Högl B, Frauscher B, Müller C, Santamaría J, et al. Olfactory dysfunction predicts early transition to a Lewy body disease in idiopathic RBD. Neurology. 2015;84:654–8. doi: 10.1212/WNL.0000000000001265. doi: 10.1212/WNL.0000000000001265. [DOI] [PubMed] [Google Scholar]
- 37.Ferini-Strambi L, Oertel W, Dauvilliers Y, Postuma RB, Marelli S, Iranzo A, et al. Autonomic symptoms in idiopathic REM behavior disorder: A multicentre case-control study. J Neurol. 2014;261:1112–8. doi: 10.1007/s00415-014-7317-8. doi: 10.1007/s00415-014-7317-8. [DOI] [PubMed] [Google Scholar]
- 38.Ferini-Strambi L, Oldani A, Zucconi M, Smirne S. Cardiac autonomic activity during wakefulness and sleep in REM sleep behavior disorder. Sleep. 1996;19:367–9. doi: 10.1093/sleep/19.5.367. [DOI] [PubMed] [Google Scholar]
- 39.Sorensen GL, Mehlsen J, Jennum P. Reduced sympathetic activity in idiopathic rapid-eye-movement sleep behavior disorder and Parkinson's disease. Auton Neurosci. 2013;179:138–41. doi: 10.1016/j.autneu.2013.08.067. doi: 10.1016/j.autneu.2013.08.067. [DOI] [PubMed] [Google Scholar]
- 40.Postuma RB, Lanfranchi PA, Blais H, Gagnon JF, Montplaisir JY. Cardiac autonomic dysfunction in idiopathic REM sleep behavior disorder. Mov Disord. 2010;25:2304–10. doi: 10.1002/mds.23347. doi: 10.1002/mds.23347. [DOI] [PubMed] [Google Scholar]
- 41.Sorensen GL, Kempfner J, Zoetmulder M, Sorensen HB, Jennum P. Attenuated heart rate response in REM sleep behavior disorder and Parkinson's disease. Mov Disord. 2012;27:888–94. doi: 10.1002/mds.25012. doi: 10.1002/mds. 25012. [DOI] [PubMed] [Google Scholar]
- 42.Frauscher B, Nomura T, Duerr S, Ehrmann L, Gschliesser V, Wenning GK, et al. Investigation of autonomic function in idiopathic REM sleep behavior disorder. J Neurol. 2012;259:1056–61. doi: 10.1007/s00415-011-6298-0. doi: 10.1007/s00415-011-6298-0. [DOI] [PubMed] [Google Scholar]
- 43.Bang YR, Jeon HJ, Youn S, Yoon IY. Alterations of awake EEG in idiopathic REM sleep behavior disorder without cognitive impairment. Neurosci Lett. 2017;637:64–9. doi: 10.1016/j.neulet.2016.11.052. doi: 10.1016/j.neulet. 2016.11.052. [DOI] [PubMed] [Google Scholar]
- 44.Fantini ML, Gagnon JF, Petit D, Rompré S, Décary A, Carrier J, et al. Slowing of electroencephalogram in rapid eye movement sleep behavior disorder. Ann Neurol. 2003;53:774–80. doi: 10.1002/ana.10547. doi: 10.1002/ana.10547. [DOI] [PubMed] [Google Scholar]
- 45.Sasai T, Matsuura M, Inoue Y. Electroencephalographic findings related with mild cognitive impairment in idiopathic rapid eye movement sleep behavior disorder. Sleep. 2013;36:1893–9. doi: 10.5665/sleep.3224. doi: 10.5665/sleep.3224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sunwoo JS, Lee S, Kim JH, Lim JA, Kim TJ, Byun JI, et al. Altered functional connectivity in idiopathic rapid eye movement sleep behavior disorder: A Resting-state EEG study. Sleep. 2017;40:zsx071. doi: 10.1093/sleep/zsx058. doi: 10.1093/sleep/zsx058. [DOI] [PubMed] [Google Scholar]
- 47.Iranzo A, Isetta V, Molinuevo JL, Serradell M, Navajas D, Farre R, et al. Electroencephalographic slowing heralds mild cognitive impairment in idiopathic REM sleep behavior disorder. Sleep Med. 2010;11:534–9. doi: 10.1016/j.sleep.2010.03.006. doi: 10.1016/j.sleep.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 48.Rodrigues Brazète J, Montplaisir J, Petit D, Postuma RB, Bertrand JA, Génier Marchand D, et al. Electroencephalogram slowing in rapid eye movement sleep behavior disorder is associated with mild cognitive impairment. Sleep Med. 2013;14:1059–63. doi: 10.1016/j.sleep.2013.06.013. doi: 10.1016/j.sleep.2013.06.013. [DOI] [PubMed] [Google Scholar]
- 49.Massicotte-Marquez J, Décary A, Gagnon JF, Vendette M, Mathieu A, Postuma RB, et al. Executive dysfunction and memory impairment in idiopathic REM sleep behavior disorder. Neurology. 2008;70:1250–7. doi: 10.1212/01.wnl.0000286943.79593.a6. doi: 10.1212/01.wnl.0000286943.79593.a6. [DOI] [PubMed] [Google Scholar]
- 50.Terzaghi M, Sinforiani E, Zucchella C, Zambrelli E, Pasotti C, Rustioni V, et al. Cognitive performance in REM sleep behaviour disorder: A possible early marker of neurodegenerative disease? Sleep Med. 2008;9:343–51. doi: 10.1016/j.sleep.2007.06.013. doi: 10.1016/j.sleep.2007.06.013. [DOI] [PubMed] [Google Scholar]
- 51.Terzaghi M, Zucchella C, Rustioni V, Sinforiani E, Manni R. Cognitive performances and mild cognitive impairment in idiopathic rapid eye movement sleep behavior disorder: Results of a longitudinal follow-up study. Sleep. 2013;36:1527–32. doi: 10.5665/sleep.3050. doi: 10.5665/sleep.3050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fantini ML, Farini E, Ortelli P, Zucconi M, Manconi M, Cappa S, et al. Longitudinal study of cognitive function in idiopathic REM sleep behavior disorder. Sleep. 2011;34:619–25. [PMC free article] [PubMed] [Google Scholar]
- 53.Barber TR, Lawton M, Rolinski M, Evetts S, Baig F, Ruffmann C, et al. Prodromal parkinsonism and neurodegenerative risk stratification in REM sleep behavior disorder. Sleep. 2017;40:zsx071. doi: 10.1093/sleep/zsx071. doi: 10.1093/sleep/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Youn S, Kim T, Yoon IY, Jeong J, Kim HY, Han JW, et al. Progression of cognitive impairments in idiopathic REM sleep behaviour disorder. J Neurol Neurosurg Psychiatry. 2016;87:890–6. doi: 10.1136/jnnp-2015-311437. doi: 10.1136/jnnp-2015-311437. [DOI] [PubMed] [Google Scholar]
- 55.Génier Marchand D, Montplaisir J, Postuma RB, Rahayel S, Gagnon JF. Detecting the cognitive prodrome of dementia with Lewy bodies: A prospective study of REM sleep behavior disorder. Sleep. 2017;40:zsw014. doi: 10.1093/sleep/zsw014. doi: 10.1093/sleep/ [DOI] [PubMed] [Google Scholar]
- 56.Sasai-Sakuma T, Nishio Y, Yokoi K, Mori E, Inoue Y. Pareidolias in REM sleep behavior disorder: A possible predictive marker of Lewy body diseases? Sleep. 2017;40:zsw045. doi: 10.1093/sleep/zsw045. doi: 10.1093/sleep/ [DOI] [PubMed] [Google Scholar]
- 57.Gagnon JF, Vendette M, Postuma RB, Desjardins C, Massicotte-Marquez J, Panisset M, et al. Mild cognitive impairment in rapid eye movement sleep behavior disorder and Parkinson's disease. Ann Neurol. 2009;66:39–47. doi: 10.1002/ana.21680. doi: 10.1002/ana.21680. [DOI] [PubMed] [Google Scholar]
- 58.Ferini-Strambi L, Di Gioia MR, Castronovo V, Oldani A, Zucconi M, Cappa SF, et al. Neuropsychological assessment in idiopathic REM sleep behavior disorder (RBD): Does the idiopathic form of RBD really exist? Neurology. 2004;62:41–5. doi: 10.1212/01.wnl.0000101726.69701.fa. doi: 10.1212/01.WNL.0000101726.69701.FA. [DOI] [PubMed] [Google Scholar]
- 59.Li X, Zhou Z, Jia S, Hou C, Zheng W, Rong P, et al. Cognitive study on Chinese patients with idiopathic REM sleep behavior disorder. J Neurol Sci. 2016;366:82–6. doi: 10.1016/j.jns.2016.04.047. doi: 10.1016/j.jns. 2016.04.047. [DOI] [PubMed] [Google Scholar]
- 60.Bezdicek O, Nikolai T, Nepožitek J, Peřinová P, Kemlink D, Dušek P, et al. Prospective memory impairment in idiopathic REM sleep behavior disorder. Clin Neuropsychol. 2017 doi: 10.1080/13854046.2017.1394493. [Epub ahead of print]. doi: 10.1080/13854046.2017.1394493. [DOI] [PubMed] [Google Scholar]
- 61.Zhang JR, Chen J, Yang ZJ, Zhang HJ, Fu YT, Shen Y, et al. Rapid eye movement sleep behavior disorder symptoms correlate with domains of cognitive impairment in Parkinson's disease. Chin Med J. 2016;129:379–85. doi: 10.4103/0366-6999.176077. doi: 10.4103/0366-6999.176077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.McCann H, Cartwright H, Halliday GM. Neuropathology of α-synuclein propagation and Braak hypothesis. Mov Disord. 2016;31:152–60. doi: 10.1002/mds.26421. doi: 10.1002/mds.26421. [DOI] [PubMed] [Google Scholar]
- 63.Abbott SM, Videnovic A. Sleep disorders in atypical Parkinsonism. Mov Disord Clin Pract. 2014;1:89–96. doi: 10.1002/mdc3.12025. doi: 10.1002/mdc3.12025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Arnulf I, Merino-Andreu M, Bloch F, Konofal E, Vidailhet M, Cochen V, et al. REM sleep behavior disorder and REM sleep without atonia in patients with progressive supranuclear palsy. Sleep. 2005;28:349–54. [PubMed] [Google Scholar]
- 65.Gagnon JF, Petit D, Fantini ML, Rompré S, Gauthier S, Panisset M, et al. REM sleep behavior disorder and REM sleep without atonia in probable Alzheimer disease. Sleep. 2006;29:1321–5. doi: 10.1093/sleep/29.10.1321. doi: 10.1093/sleep/29.10.1321. [DOI] [PubMed] [Google Scholar]
- 66.Sixel-Döring F, Zimmermann J, Wegener A, Mollenhauer B, Trenkwalder C. The evolution of REM sleep behavior disorder in early Parkinson disease. Sleep. 2016;39:1737–42. doi: 10.5665/sleep.6102. doi: 10.5665/sleep.6102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhou J, Zhang J, Lam SP, Mok V, Chan A, Li SX, et al. Mortality and its risk factors in patients with rapid eye movement sleep behavior disorder. Sleep. 2016;39:1543–50. doi: 10.5665/sleep.6016. doi: 10.5665/sleep.6016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Postuma RB, Iranzo A, Hogl B, Arnulf I, Ferini-Strambi L, Manni R, et al. Risk factors for neurodegeneration in idiopathic rapid eye movement sleep behavior disorder: A multicenter study. Ann Neurol. 2015;77:830–9. doi: 10.1002/ana.24385. doi: 10.1002/ana.24385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Postuma RB, Gagnon JF, Bertrand JA, Génier Marchand D, Montplaisir JY. Parkinson risk in idiopathic REM sleep behavior disorder: Preparing for neuroprotective trials. Neurology. 2015;84:1104–13. doi: 10.1212/WNL.0000000000001364. doi: 10.1212/WNL.0000000000001364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Molano J, Boeve B, Ferman T, Smith G, Parisi J, Dickson D, et al. Mild cognitive impairment associated with limbic and neocortical Lewy body disease: A clinicopathological study. Brain. 2010;133(Pt 2):540–56. doi: 10.1093/brain/awp280. doi: 10.1093/brain/awp280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Postuma RB, Gagnon JF, Vendette M, Fantini ML, Massicotte-Marquez J, Montplaisir J, et al. Quantifying the risk of neurodegenerative disease in idiopathic REM sleep behavior disorder. Neurology. 2009;72:1296–300. doi: 10.1212/01.wnl.0000340980.19702.6e. doi: 10.1212/01.wnl. 0000340980.19702.6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Iaccarino L, Marelli S, Iannaccone S, Magnani G, Ferini-Strambi L, Perani D, et al. Severe brain metabolic decreases associated with REM sleep behavior disorder in dementia with Lewy bodies. J Alzheimers Dis. 2016;52:989–97. doi: 10.3233/JAD-151000. doi: 10.3233/JAD-151000. [DOI] [PubMed] [Google Scholar]
- 73.Palma JA, Fernandez-Cordon C, Coon EA, Low PA, Miglis MG, Jaradeh S, et al. Prevalence of REM sleep behavior disorder in multiple system atrophy: A multicenter study and meta-analysis. Clin Auton Res. 2015;25:69–75. doi: 10.1007/s10286-015-0279-9. doi: 10.1007/s10286-015-0279-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Vetrugno R, Provini F, Cortelli P, Plazzi G, Lotti EM, Pierangeli G, et al. Sleep disorders in multiple system atrophy: A correlative video-polysomnographic study. Sleep Med. 2004;5:21–30. doi: 10.1016/j.sleep.2003.07.002. doi: 10.1016/j.sleep.2003.07.002. [DOI] [PubMed] [Google Scholar]
- 75.Wang Y, Shen Y, Xiong KP, He PC, Mao CJ, Li J, et al. Tonic electromyogram density in multiple system atrophy with predominant Parkinsonism and Parkinson's disease. Chin Med J. 2017;130:684–90. doi: 10.4103/0366-6999.201603. doi: 10.4103/0366-6999.201603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Aurora RN, Zak RS, Maganti RK, Auerbach SH, Casey KR, Chowdhuri S, et al. Best practice guide for the treatment of REM sleep behavior disorder (RBD) J Clin Sleep Med. 2010;6:85–95. [PMC free article] [PubMed] [Google Scholar]
- 77.McCarter SJ, Boswell CL, St. Louis EK, Dueffert LG, Slocumb N, Boeve BF. Treatment outcomes in REM sleep behavior disorder. Sleep Med. 2013;14:237–42. doi: 10.1016/j.sleep.2012.09.018. doi: 10.1016/j.sleep.2012.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Vilas D, Iranzo A, Tolosa E, Aldecoa I, Berenguer J, Vilaseca I, et al. Assessment of α-synuclein in submandibular glands of patients with idiopathic rapid-eye-movement sleep behaviour disorder: A case-control study. Lancet Neurol. 2016;15:708–18. doi: 10.1016/S1474-4422(16)00080-6. doi: 10.1016/S1474-4422(16)00080-6. [DOI] [PubMed] [Google Scholar]
- 79.Doppler K, Jentschke HM, Schulmeyer L, Vadasz D, Janzen A, Luster M, et al. Dermal phospho-alpha-synuclein deposits confirm REM sleep behaviour disorder as prodromal Parkinson's disease. Acta Neuropathol. 2017;133:535–45. doi: 10.1007/s00401-017-1684-z. doi: 10.1007/s00401-017-1684-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sashourpour M, Zahri S, Radjabian T, Ruf V, Pan-Montojo F, Morshedi D, et al. A study on the modulation of alpha-synuclein fibrillation by Scutellaria pinnatifida extracts and its neuroprotective properties. PLoS One. 2017;12:e0184483. doi: 10.1371/journal.pone.0184483. doi: 10.1371/journal.pone. 0184483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hua J, Yin N, Yang B, Zhang J, Ding J, Fan Y, et al. Ginkgolide B and bilobalide ameliorate neural cell apoptosis in α-synuclein aggregates. Biomed Pharmacother. 2017;96:792–7. doi: 10.1016/j.biopha.2017.10.050. doi: 10.1016/j.biopha.2017.10.050. [DOI] [PubMed] [Google Scholar]
- 82.Sharma N, Nehru B. Curcumin affords neuroprotection and inhibits α-synuclein aggregation in lipopolysaccharide-induced Parkinson's disease model. Inflammopharmacology. 2018;26:349–60. doi: 10.1007/s10787-017-0402-8. doi: 10.1007/s10787-017-0402-8. [DOI] [PubMed] [Google Scholar]
- 83.Rezaeian N, Shirvanizadeh N, Mohammadi S, Nikkhah M, Arab SS. The inhibitory effects of biomimetically designed peptides on α-synuclein aggregation. Arch Biochem Biophys. 2017;634:96–106. doi: 10.1016/j.abb.2017.09.015. doi: 10.1016/j.abb.2017.09.015. [DOI] [PubMed] [Google Scholar]
- 84.Zhang QS, Heng Y, Chen Y, Luo P, Wen L, Zhang Z, et al. A novel bibenzyl compound (20C) protects mice from 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine/Probenecid toxicity by regulating the α-synuclein-related inflammatory response. J Pharmacol Exp Ther. 2017;363:284–92. doi: 10.1124/jpet.117.244020. doi: 10.1124/jpet. 117.244020. [DOI] [PubMed] [Google Scholar]


