Abstract
Purpose
The purpose of this study was to estimate the clinical utilization of radiation therapy (RT) in Korea between 2011 and 2015.
Materials and Methods
We analyzed the claims data from the Health Insurance Review and Assessment Service to estimate the clinical utilization of RT. The source population consisted of all patients who had any of the International Classification of Diseases 10th revision cancer diagnoses (C00-C97) and those with diagnostic codes D00-D48, who were also associated with at least one of the procedure codes related to RT.
Results
The total number of patients who received RT in 2011, 2012, 2013, 2014, and 2015 were 54,810, 59,435, 61,839, 64,062, and 66,183, respectively. Among them, the total numbers of male and female patients were 24,946/29,864 in 2011, 27,211/32,224 in 2012, 28,111/33,728 in 2013, 29,312/34,750 in 2014, and 30,266/35,917 in 2015. The utilization rate of RT in cancer patients has also increased steadily over the same period from 25% to 30%. The five cancers that were most frequently treated with RT between 2011 and 2012 were breast, lung, colorectal, liver, and uterine cervical cancers. However, the fifth most common cancer treated with RT that replaced uterine cervical cancer in 2013 was prostate cancer. More than half of cancer patients (64%) were treated with RT in the capital area (Seoul, Gyeonggi, and Incheon).
Conclusion
The total number of patients who underwent RT increased steadily from 2011 to 2015 in Korea. The utilization rate of RT in cancer patients is also increasing.
Keywords: Neoplasms, Radiotherapy, Statistics, Korea
Introduction
Because of the decreases in the incidence of thyroid cancer, the annual cancer incidence has decreased in Korea after 2011 following a steady increase [1]. However, cancer is still a major public health problem in Korea. Radiation therapy (RT) is an effective and widespread method for treating cancer in conjunction with surgery and chemotherapy. RT is required in at least 45%-55% of newly diagnosed cancer cases [2]. A steady rise in the number of patients with cancer has increased the demand for RT in Korea. As we have reported previously [3,4], the number of patients with cancer needing RT has steadily increased over the 5 years between 2009 and 2013.
In the present study, we analyzed the claims data from the Health Insurance Review and Assessment Service (HIRA) to estimate the clinical utilization of RT in the 2011-2015 period.
Materials and Methods
We analyzed open claims data from the HIRA. The analysis methods using claims data from the HIRA are described in detail in a previous study [4]. The customized source population criteria for this study are shown in Table 1. In our previous study [3], type of healthcare facility included tertiary and secondary hospitals. However, in this study, primary and sanatorium hospitals were also included. In addition, information about patriots and veterans affairs’ insurance expenditure by the government, which were not included in the previous study, were also included in this study. The source population consisted of all patients who had any of the International Classification of Diseases 10th revision cancer diagnoses (C00-C97) and those with diagnostic codes D00-D48 (including carcinoma in situ or benign neoplasms), who were also associated with at least one of the procedure codes related to RT treatment [3]. The detailed methods of categorization for diagnostic codes are described in a previous study [3].
Table 1.
Customized source population
| List | Criteria |
|---|---|
| Treatment period | 1 Jan 2011-31 Dec 2015 |
| Type of healthcare facility | Tertiary, secondary, primary, sanatorium |
| Diagnostic code | C00-C97, D00-D48 |
| Type of insurance | Health insurance, medical aid, patriots and veterans affairs’ insurance expenditure by government |
| Hospital region | National |
| Sex | Male, female |
| Age | All ages |
We analyzed the claims data from the HIRA in order to identify the total number of patients who underwent RT, and the number of patients who received RT by primary cancer diagnosis, sex, and age group between 2011 and 2015 in Korea. In addition, through the classification of the procedure codes related to RT [3], we estimated the total number of patients who received specific RT modalities, including brachytherapy, intensity-modulated radiation therapy (IMRT), stereotactic radiation therapy (SRT), and proton therapy. Considering the annual cancer incidence [1], the percentage of patients who underwent RT was calculated. We also analyzed the geographic differences for the number of patients who received RT. The number of patients was based on the location of the healthcare facilities.
Results
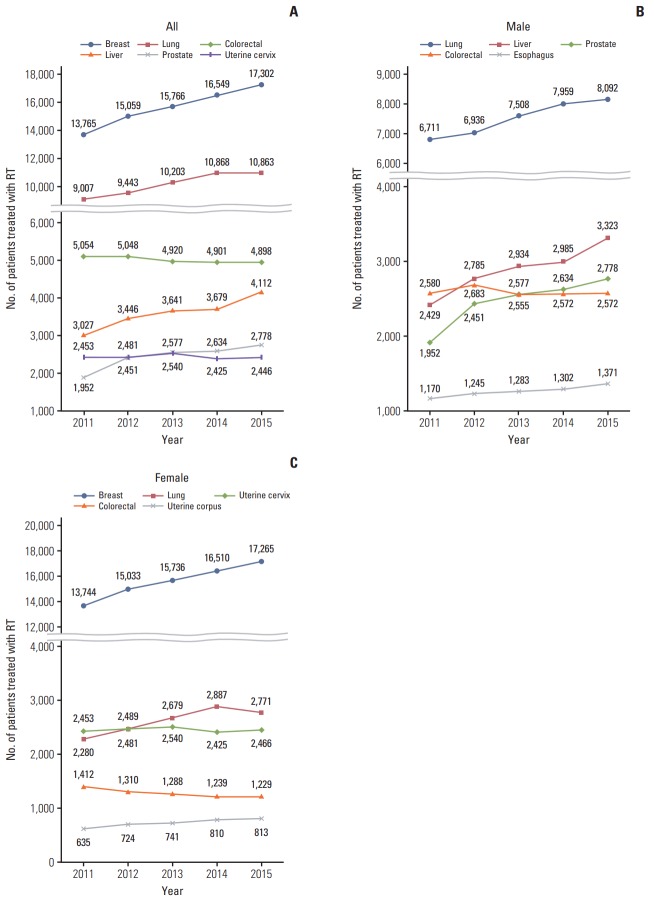
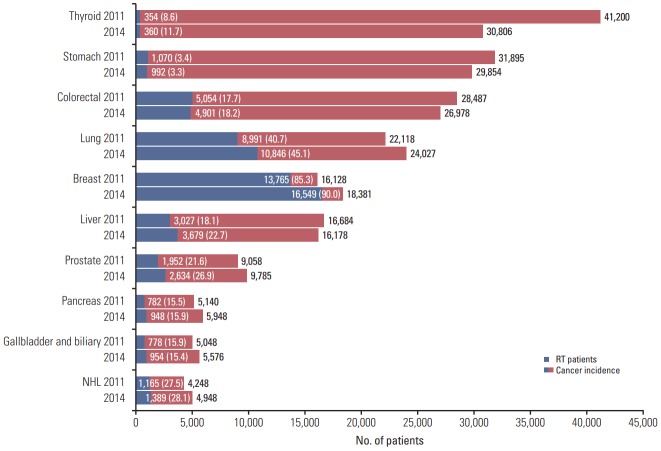
The total number of patients who received RT in 2011, 2012, 2013, 2014, and 2015 were 54,810, 59,435, 61,839, 64,062, and 66,183, respectively (Fig. 1). Among them, the total numbers of male and female patients were 24,946/29,864 in 2011, 27,211/32,224 in 2012, 28,111/33,728 in 2013, 29,312/34,750 in 2014, and 30,266/35,917 in 2015 (Fig. 2). The absolute number of cancer patients who received RT and the cancer incidence from 2011 to 2014 are shown in Fig. 3. The utilization rate of RT in cancer patients has also increased steadily over the same period from 25% to 30%. Because Korea’s cancer incidence in 2015 has not been reported yet, the utilization rate of RT in 2015 could not be calculated.
Fig. 1.
The total number of patients who underwent radiation therapy between 2011 and 2015 in Korea.
Fig. 2.
The total numbers of male and female patients who received radiation therapy between 2011 and 2015 in Korea.
Fig. 3.
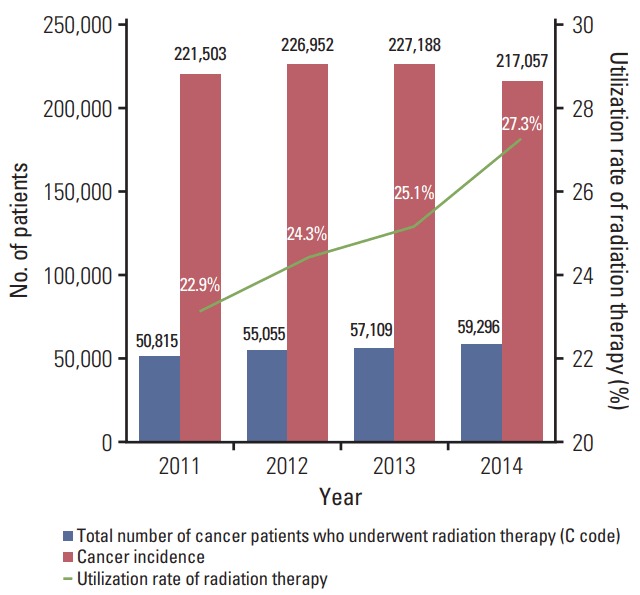
Cancer incidence and the total number of patients who received radiation therapy between 2009 and 2013 in Korea.
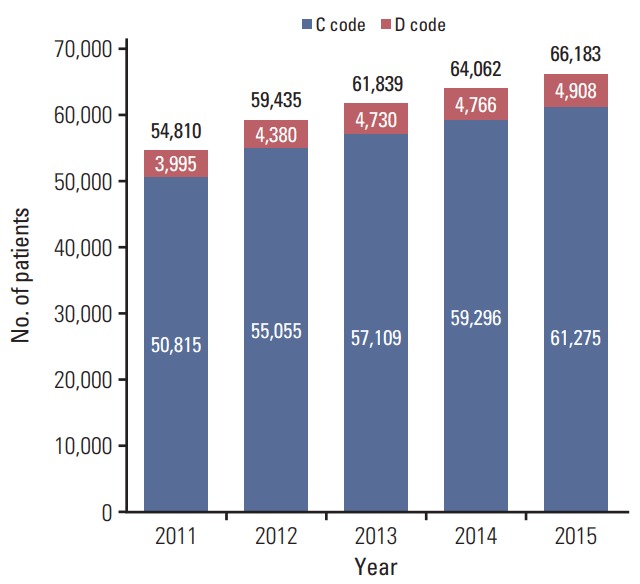
The distribution of patients who received RT by cancer diagnosis between 2011 and 2015 is shown in Table 2. The five cancers that were most frequently treated with RT between 2011 and 2012 were breast, lung, colorectal, liver, and uterine cervical cancers. However, the fifth most common cancer treated with RT that replaced uterine cervical cancer in 2013 was prostate cancer (Fig. 4A). The five most common types of cancer among the male patients were lung, liver, prostate, colorectal, and esophageal cancers, while the incidence of colorectal cancer showed a decreasing trend (Fig. 4B). Among female patients, the five most common types were breast, lung, uterine cervical, colorectal, and uterine corpus cancers, while the incidence of colorectal and uterine cervix cancer showed a decreasing trend (Fig. 4C).
Table 2.
Distribution of cancer patients who underwent radiation therapy based on primary diagnosis between 2011 and 2015 in Korea
| Category | Primary diagnosis (diagnostic code) | Yeara) |
||||
|---|---|---|---|---|---|---|
| 2011 | 2012 | 2013 | 2014 | 2015 | ||
| Breast | (C50) | 13,765 | 15,059 | 15,766 | 16,549 | 17,302 |
| Gastrointestinal | Colorectum (C18-C20) | 5,054 | 5,048 | 4,920 | 4,901 | 4,898 |
| Liver (C22) | 3,027 | 3,446 | 3,641 | 3,679 | 4,112 | |
| Esophagus (C15) | 1,250 | 1,335 | 1,380 | 1,397 | 1,472 | |
| Stomach (C16) | 1,070 | 1,048 | 1,026 | 992 | 1,013 | |
| Pancreas (C25) | 782 | 942 | 906 | 948 | 998 | |
| Gallbladder and biliary (C23-C24) | 778 | 856 | 879 | 954 | 985 | |
| Anus (C21) | 193 | 213 | 211 | 203 | 199 | |
| Small bowel (C17) | 42 | 39 | 43 | 35 | 32 | |
| Other (C26) | 4 | 5 | 3 | 3 | 3 | |
| Subtotal | 12,200 | 12,932 | 13,009 | 13,112 | 13,712 | |
| Thoracic | Lung (C34) | 8,991 | 9,425 | 10,187 | 10,846 | 10,863 |
| Thymus (C37) | 258 | 238 | 249 | 307 | 323 | |
| Mediastinum (C38) | 41 | 44 | 48 | 47 | 54 | |
| Trachea (C33) | 16 | 18 | 16 | 22 | 25 | |
| Other (C39) | 4 | 3 | 2 | 1 | 1 | |
| Subtotal | 9,310 | 9,728 | 10,502 | 11,223 | 11,266 | |
| Head and neck | Larynx (C32) | 773 | 884 | 964 | 912 | 903 |
| Oropharynx (C01, C09-C10) | 509 | 615 | 595 | 621 | 619 | |
| Oral cavity (C02-C06) | 500 | 601 | 588 | 605 | 632 | |
| Nasopharynx (C11) | 414 | 489 | 488 | 488 | 516 | |
| Salivary gland (C07-C08) | 298 | 346 | 347 | 398 | 374 | |
| Hypopharynx (C12-C13) | 354 | 394 | 352 | 437 | 395 | |
| Paranasal sinus (C31) | 149 | 166 | 145 | 179 | 166 | |
| Nasal cavity (C30) | 93 | 129 | 110 | 128 | 142 | |
| Eye and orbit (C69) | 44 | 54 | 51 | 41 | 58 | |
| Lip (C00) | 11 | 8 | 13 | 9 | 18 | |
| Other (C14) | 19 | 20 | 14 | 16 | 17 | |
| Subtotal | 3,164 | 3,706 | 3,667 | 3,834 | 3,840 | |
| Gynecologic | Uterine cervix (C53) | 2,453 | 2,481 | 2,540 | 2,425 | 2,466 |
| Uterine corpus (C54-C55) | 635 | 724 | 741 | 810 | 813 | |
| Ovary and tube (C56) | 217 | 204 | 247 | 248 | 258 | |
| Vagina and vulva (C51-C52) | 111 | 111 | 100 | 90 | 122 | |
| Other (C57-C58) | 15 | 14 | 12 | 9 | 11 | |
| Subtotal | 3,431 | 3,534 | 3,640 | 3,582 | 3,670 | |
| Genitourinary | Prostate (C61) | 1,952 | 2,451 | 2,577 | 2,634 | 2,778 |
| Ureter and bladder (C66-C67) | 498 | 484 | 531 | 608 | 602 | |
| Kidney (C64-C65) | 443 | 422 | 445 | 454 | 525 | |
| Penis and testis (C60, C62-C63) | 65 | 57 | 66 | 57 | 62 | |
| Other (C68) | 11 | 14 | 12 | 18 | 19 | |
| Subtotal | 2,969 | 3,428 | 3,631 | 3,771 | 3,986 | |
| CNS | Brain (C70-C71) | 1,388 | 1,513 | 1,567 | 1,623 | 1,605 |
| Spinal cord (C72) | 60 | 61 | 52 | 48 | 47 | |
| Other (C47) | 45 | 36 | 52 | 32 | 46 | |
| Subtotal | 1,493 | 1,610 | 1,671 | 1,703 | 1,698 | |
| Lymphoma | Non-Hodgkin's lymphoma (C82-C88) | 1,169 | 1,322 | 1,321 | 1,389 | 1,493 |
| Hodgkin's disease (C81) | 98 | 108 | 91 | 93 | 100 | |
| Other (C96) | 22 | 23 | 21 | 30 | 33 | |
| Subtotal | 1,289 | 1,453 | 1,433 | 1,512 | 1,626 | |
| Soft tissue | (C46, C49) | 545 | 581 | 631 | 648 | 715 |
| Mesothelioma | (C45) | 14 | 19 | 18 | 19 | 29 |
| Myeloma and plasmacytoma | (C90) | 316 | 414 | 442 | 450 | 459 |
| Thyroid | (C73) | 354 | 381 | 357 | 360 | 309 |
| Leukemia | (C91-C95) | 359 | 353 | 351 | 411 | 396 |
| Skin | (C44) | 244 | 287 | 264 | 284 | 279 |
| Malignant melanoma | (C43) | 215 | 209 | 225 | 244 | 241 |
| Primary bone and cartilage | (C40-C41) | 213 | 219 | 170 | 206 | 223 |
| Endocrine | (C74-C75) | 56 | 72 | 93 | 101 | 104 |
| Unknown primary | (C48, C76-C80, C97) | 878 | 1,070 | 1,239 | 1,287 | 1,420 |
| Total No. of cancer patients | - | 50,815 | 55,055 | 57,109 | 59,296 | 61,275 |
| Carcinoma in situ of the breast | (D05) | 1,388 | 1,653 | 1,918 | 1,912 | 2,062 |
| Benign neoplasm of meninges | (D32) | 1,022 | 960 | 1,041 | 1,112 | 1,032 |
| Benign neoplasm of CNS | (D33) | 726 | 750 | 744 | 694 | 713 |
| Benign neoplasm of endocrine | (D34-D35) | 229 | 283 | 304 | 319 | 308 |
| Other D code diseases | (D00-D04, D06-D31, D36-D48) | 630 | 734 | 723 | 729 | 793 |
| Total D code patients | - | 3,995 | 4,380 | 4,730 | 4,766 | 4,908 |
| Total | - | 54,810 | 59,435 | 61,839 | 64,062 | 66,183 |
CNS, central nervous system.
Number of patients who received radiation therapy.
Fig. 4.
The fifth most common cancer treated with radiation therapy (RT) between 2011 and 2015 in Korea. (A) All patients. (B) Male patients. (C) Female patients.
Breast cancer and carcinoma in situ of breast patients accounted for nearly 30% of the total patients who underwent RT, and for approximately half of the female patients (Table 2). The diseases with code ‘D’ made up 7% of the total patients treated with RT (Fig. 1).
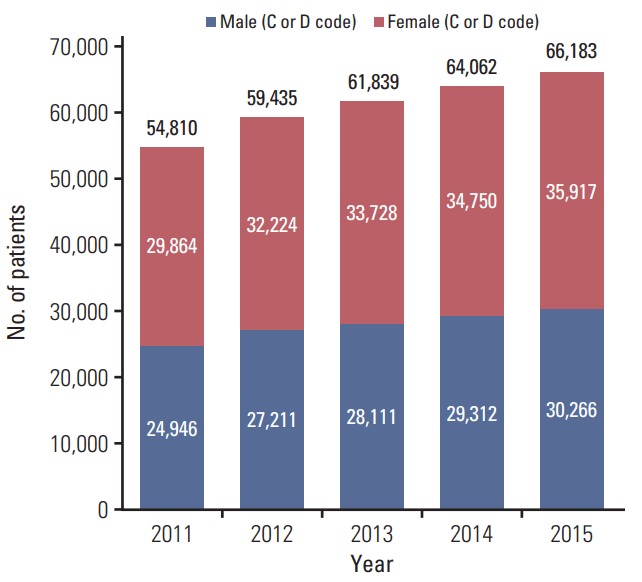
The utilization rates of RT in the 10 most common cancers in Korea [1] are shown in Fig. 5. The utilization rate of RT increased significantly between 2011 and 2014 for breast (from 85% to 90%), lung (from 41% to 45%), liver (from 18% to 25%), and prostate cancer (from 22% to 27%).
Fig. 5.
The utilization rate of radiation therapy (RT) in the 10 most common cancer between 2011 and 2014 in Korea. NHL, non-Hodgkin’s lymphoma.
The distribution of patients who received RT in 2015 based on cancer diagnosis and age group is shown in Table 3. The most common cancer was that of the central nervous system for patients aged 20 years or less, while breast cancer was the most common cancer in patients aged 30-50 years, and lung cancer was the most common cancer in patients aged 60 years or more. Similar trends were observed for previous years.
Table 3.
The number of patients who underwent radiation therapy by cancer diagnosis and age group in Korea (2015)
| Category | Primary diagnosis | Age groupa) |
||||||
|---|---|---|---|---|---|---|---|---|
| 20s or under | 30s | 40s | 50s | 60s | 70s or older | Total | ||
| Breast | Breast (C50) | 114 | 1,614 | 5,949 | 5,908 | 2,761 | 956 | 17,302 |
| Gastrointestinal | Colorectum (C18-C20) | 13 | 140 | 563 | 1,330 | 1,376 | 1,476 | 4,898 |
| Liver (C22) | 10 | 89 | 447 | 1,332 | 1,326 | 908 | 4,112 | |
| Esophagus (C15) | 0 | 2 | 50 | 328 | 498 | 594 | 1,472 | |
| Stomach (C16) | 9 | 66 | 151 | 279 | 258 | 250 | 1,013 | |
| Pancreas (C25) | 2 | 16 | 65 | 273 | 340 | 302 | 998 | |
| Gallbladder and biliary (C23-C24) | 0 | 8 | 58 | 237 | 347 | 335 | 985 | |
| Anus (C21) | 3 | 0 | 16 | 52 | 49 | 79 | 199 | |
| Small bowel (C17) | 0 | 3 | 0 | 10 | 12 | 7 | 32 | |
| Other (C26) | 0 | 0 | 0 | 1 | 2 | 0 | 3 | |
| Subtotal | 37 | 324 | 1,350 | 3,842 | 4,208 | 3,951 | 13,712 | |
| Thoracic | Lung (C34) | 14 | 124 | 571 | 2,232 | 3,632 | 4,290 | 10,863 |
| Thymus (C37) | 9 | 26 | 71 | 86 | 79 | 52 | 323 | |
| Mediastinum (C38) | 14 | 4 | 8 | 10 | 11 | 7 | 54 | |
| Trachea (C33) | 1 | 1 | 5 | 4 | 7 | 7 | 25 | |
| Other (C39) | 0 | 0 | 0 | 0 | 1 | 0 | 1 | |
| Subtotal | 38 | 155 | 655 | 2,332 | 3,730 | 4,356 | 11,266 | |
| Head and neck | Larynx (C32) | 0 | 5 | 32 | 204 | 344 | 318 | 903 |
| Oropharynx (C01, C09-C10) | 2 | 7 | 58 | 229 | 211 | 112 | 619 | |
| Oral cavity (C02-C06) | 15 | 36 | 77 | 172 | 166 | 166 | 632 | |
| Nasopharynx (C11) | 21 | 44 | 109 | 162 | 112 | 68 | 516 | |
| Salivary gland (C07-C08) | 21 | 23 | 52 | 100 | 103 | 75 | 374 | |
| Hypopharynx (C12-C13) | 0 | 1 | 11 | 85 | 140 | 158 | 395 | |
| Paranasal sinus (C31) | 3 | 3 | 28 | 42 | 43 | 47 | 166 | |
| Nasal cavity (C30) | 4 | 15 | 20 | 37 | 26 | 40 | 142 | |
| Eye and orbit (C69) | 7 | 3 | 7 | 15 | 11 | 15 | 58 | |
| Lip (C00) | 0 | 0 | 2 | 5 | 3 | 8 | 18 | |
| Other (C14) | 1 | 1 | 0 | 3 | 6 | 6 | 17 | |
| Subtotal | 74 | 138 | 396 | 1,054 | 1,165 | 1,013 | 3,840 | |
| Gynecologic | Uterine cervix (C53) | 24 | 274 | 539 | 702 | 440 | 487 | 2,466 |
| Uterine corpus (C54-C55) | 9 | 24 | 129 | 339 | 213 | 99 | 813 | |
| Ovary and tube (C56) | 1 | 13 | 40 | 98 | 69 | 37 | 258 | |
| Vagina and vulva (C51-C52) | 0 | 2 | 12 | 28 | 21 | 59 | 122 | |
| Other (C57-C58) | 0 | 1 | 1 | 3 | 5 | 1 | 11 | |
| Subtotal | 34 | 314 | 721 | 1,170 | 748 | 683 | 3,670 | |
| Genitourinary | Prostate (C61) | 1 | 0 | 18 | 257 | 918 | 1,584 | 2,778 |
| Ureter and bladder (C66-C67) | 1 | 4 | 31 | 94 | 145 | 327 | 602 | |
| Kidney (C64-C65) | 11 | 14 | 56 | 141 | 156 | 147 | 525 | |
| Penis and testis (C60, C62-C63) | 12 | 14 | 7 | 12 | 7 | 10 | 62 | |
| Other (C68) | 0 | 2 | 2 | 1 | 4 | 10 | 19 | |
| Subtotal | 25 | 34 | 114 | 505 | 1,230 | 2,078 | 3,986 | |
| CNS | Brain (C70-C71) | 250 | 186 | 264 | 391 | 304 | 210 | 1,605 |
| Spinal cord (C72) | 15 | 5 | 7 | 6 | 8 | 6 | 47 | |
| Other (C47) | 9 | 12 | 7 | 7 | 6 | 5 | 46 | |
| Subtotal | 274 | 203 | 278 | 404 | 318 | 221 | 1,698 | |
| Lymphoma | Non-Hodgkin's lymphoma (C82-C88) | 78 | 128 | 220 | 361 | 331 | 375 | 1,493 |
| Hodgkin's disease (C81) | 36 | 19 | 10 | 15 | 5 | 15 | 100 | |
| Other (C96) | 5 | 8 | 8 | 8 | 1 | 3 | 33 | |
| Subtotal | 119 | 155 | 238 | 384 | 337 | 393 | 1,626 | |
| Soft tissue | (C46, C49) | 75 | 73 | 103 | 157 | 135 | 172 | 715 |
| Mesothelioma | (C45) | 0 | 0 | 3 | 8 | 12 | 6 | 29 |
| Myeloma and plasmacytoma | (C90) | 1 | 5 | 43 | 113 | 163 | 134 | 459 |
| Thyroid | (C73) | 3 | 3 | 24 | 75 | 82 | 122 | 309 |
| Leukemia | (C91-C95) | 138 | 54 | 85 | 69 | 34 | 16 | 396 |
| Skin | (C44) | 5 | 11 | 14 | 40 | 53 | 156 | 279 |
| Malignant melanoma | (C43) | 3 | 8 | 31 | 60 | 73 | 66 | 241 |
| Primary bone and cartilage | (C40-C41) | 58 | 23 | 28 | 39 | 34 | 41 | 223 |
| Endocrine | (C74-C75) | 50 | 11 | 4 | 24 | 7 | 8 | 104 |
| Unknown primary | (C48, C76-C80, C97) | 20 | 53 | 168 | 377 | 429 | 373 | 1,420 |
| Total No. of cancer patients | 1,068 | 3,178 | 10,204 | 16,561 | 15,519 | 14,745 | 61,275 | |
| Carcinoma in situ of the breast | (D05) | 18 | 184 | 799 | 661 | 323 | 77 | 2,062 |
| Benign neoplasm of meninges | (D32) | 10 | 36 | 161 | 319 | 266 | 240 | 1,032 |
| Benign neoplasm of CNS | (D33) | 53 | 65 | 136 | 208 | 148 | 103 | 713 |
| Benign neoplasm of endocrine | (D34-D35) | 19 | 41 | 71 | 84 | 60 | 33 | 308 |
| Other D code diseases | (D00-D04, D06-D31, D36-D48) | 88 | 75 | 124 | 189 | 176 | 141 | 793 |
| Total D code patients | 188 | 401 | 1,291 | 1,461 | 973 | 594 | 4,908 | |
| Total | 1,256 | 3,579 | 11,495 | 18,022 | 16,492 | 15,339 | 66,183 | |
CNS, central nervous system.
Number of patients who received radiation therapy.
The distribution of patients who received RT with specific modalities is shown in Table 4. The use of advanced RT modalities like IMRT, SRT, and proton therapy are steadily increasing every year.
Table 4.
Distribution of patients who received radiation therapy according to specific radiation therapy modalities between 2011 and 2015 in Korea
| Radiation therapy modality | Yeara) |
||||
|---|---|---|---|---|---|
| 2011 | 2012 | 2013 | 2014 | 2015 | |
| Brachytherapy | 1,421 (2.6) | 1,421 (2.4) | 1,404 (2.3) | 1,255 (2.0) | 1,247 (1.9) |
| Intensity-modulated radiation therapy | 6,250 (11.4) | 6,372 (10.7) | 6,698 (10.8) | 7,022 (11.0) | 8,397 (12.7) |
| Stereotactic radiation therapy | 3,122 (5.7) | 6,670 (11.2) | 6,772 (11.0) | 7,648 (11.9) | 12,228 (18.5) |
| Proton radiation therapy | 25 (0.0) | 50 (0.1) | 33 (0.1) | 34 (0.1) | 158 (0.2) |
Values are presented as number (%).
Percentage of the number of specific radiation therapy modalities over the total number of radiotherapy in each year.
Table 5 shows the distribution of patients who received RT from 2011 to 2015 in Korea for each prefecture. The population of each prefecture in 2015 is shown as a representative value [5]. The number of patients has steadily increased every year in all prefectures. More than half of cancer patients (64%) were treated with RT in the capital area (Seoul, Gyeonggi, and Incheon).
Table 5.
Demographic data of patients who received radiation therapy between 2011 and 2015 in Korea for each prefecture
| Prefecture | Population (2015) [5], ×103 (%) | Year |
||||
|---|---|---|---|---|---|---|
| 2011 | 2012 | 2013 | 2014 | 2015 | ||
| Seoul | 9,860 (19.5) | 24,713 (45.1) | 26,996 (45.4) | 27,458 (44.4) | 28,303 (44.2) | 29,085 (43.9) |
| Gyeonggi, Incheon | 15,284 (30.2) | 10,651 (19.4) | 11,543 (19.4) | 12,228 (19.8) | 12,859 (20.1) | 13,680 (20.7) |
| Gangwon | 1,506 (3.0) | 1,308 (2.4) | 1,422 (2.4) | 1,365 (2.2) | 1,406 (2.2) | 1,501 (2.3) |
| Chungbuk | 1,561 (3.1) | 654 (1.2) | 684 (1.2) | 683 (1.1) | 696 (1.1) | 742 (1.1) |
| Chungnam, Daejeon | 3,822 (7.5) | 2,548 (4.6) | 2,822 (4.7) | 3,029 (4.9) | 3,047 (4.7) | 3,166 (4.8) |
| Jeonbuk | 1,798 (3.5) | 1,299 (2.4) | 1,334 (2.2) | 1,366 (2.2) | 1,466 (2.3) | 1,393 (2.1) |
| Jeonnam, Gwangju | 3,274 (6.5) | 2,812 (5.1) | 3,024 (5.1) | 3,119 (5.0) | 3,195 (5.0) | 3,359 (5.1) |
| Gyeongbuk, Daegu | 5,097 (10.1) | 4,062 (7.4) | 4,388 (7.4) | 4,702 (7.6) | 4,922 (7.7) | 4,926 (7.4) |
| Gyeongnam, Busan, Ulsan | 7,827 (15.5) | 6,393 (11.7) | 6,774 (11.4) | 7,429 (12.0) | 7,652 (11.9) | 7,802 (11.8) |
| Jeju | 587 (1.1) | 420 (0.7) | 448 (0.8) | 460 (0.8) | 516 (0.8) | 529 (0.8) |
| Total | 50,616 (100) | 54,810 (100) | 59,435 (100) | 61,839 (100) | 64,062 (100) | 66,183 (100) |
Values are presented as number (%).
Discussion
We analyzed the clinical utilization of RT between 2011 and 2015 in Korea using claims data from the HIRA. The total number of patients who underwent RT has increased by 3%-8% per year between 2011 and 2015 (Fig. 1). As shown in Fig. 3, the annual cancer incidence in Korea has slowed after increasing until 2011 [1], and it decreased in 2014 compared with 2013. However, the number of cancer patients who underwent RT increased annually during the same period (Fig. 3). This antithetical pattern seemingly stems from a decrease in the total cancer incidence due to a decrease in the thyroid cancer incidence in recent years in Korea [1]. As shown in Fig. 5, because the role of external beam RT in well-differentiated thyroid cancer remains controversial [6], the decreasing incidence of thyroid cancer does not affect the utilization of RT in cancer patients.
While the numbers of breast, lung, and prostate cancers being treated with RT has increased every year, the numbers of colorectal and uterine cervix cancer treated with RT have not shown any increase (Fig. 4). These trends of RT for these cancers have some correlation with the increasing and decreasing trends in the incidence of these cancers (Fig. 5). Interestingly, liver cancer has shown a significant increase in the number of RT patients (Figs. 4 and 5) although the incidence of liver cancer has been the same or has slightly decreased every year in Korea [1]. The increase of RT for patients with liver cancer seems to have a correlation with the remarkable increase of utilization rate of RT (Fig. 5). This trend may be because recently many studies have reported good clinical outcomes for hepatocellular carcinoma patients receiving high dose radiation in Korea using advanced RT technologies, including IMRT, SRT, and image guided radiotherapy [7-12]. Furthermore, the Korean Practice Guidelines for the Management of Hepatocellular Carcinoma recommend RT for inoperable hepatocellular carcinoma patients [13].
Although the percentage of cancer patients who underwent RT increased from 25% to 30% during these 5 years (Fig. 3), the clinical utilization rate of RT in Korea seems to be lower than of the estimated optimal utilization rate of developed or developing countries (47%-56%) [14-16]. However, recently Mackillop et al. [17] criticized the overestimation of the optimal RT utilization rate in the previous reports and reported that optimal utilization rate is 34% considering the conditions of optimal access to RT. Because the study estimated the optimal utilization rate of RT in Korea under conditions of access to RT of Korea was not reported yet, whether 30% of RT utilization in Korea is appropriate is debatable. Nevertheless, the incidence of breast, lung, and prostate cancers that account for over 50% of RT patients is showing an increasing trend every year [1]. Therefore, the clinical utilization rate of RT among cancer patients in Korea is expected to continue to rise.
There is an overlap in years between the present and a previous study [3]; however, the number of patients who underwent RT are different between the two studies during the same period. Compared to the previous study, annually, an additional 200-300 patients underwent RT between 2011 and 2013. This difference might be because additional healthcare information that was not included in the previous study was integrated in the present study, such as information from primary and sanatorium hospitals and patriots and veterans affairs’ insurance expenditure by the government. Besides, there is lately (after 1 or more years) registered claims data in HIRA.
In terms of RT modalities, the number of cases receiving SRT has steadily increased over the last 5 years and it was notably increased especially in 2015. In 2015, the national health insurance coverage of SRT was expanded from only cranio-spinal tumors and inoperable lung cancer to whole body tumors. Similar to SRT, notable increases in the use of IMRT and proton therapy are expected in 2016 because national health insurance coverage of IMRT and proton therapy has been expanded in the second half of 2015. In addition, a second proton therapy center in Korea started operating in 2016 [18]. However, it should be kept in mind that the claims data from the HIRA only included data of the insured cases and the number of uninsured treatments could not be recorded. Therefore, the actual number of patients who received SRT, IMRT, and proton therapy are expected to be higher than the reported number.
In 2015, the population of Seoul was 19.5% of Korea’s population; however, nearly half of the patients (43.9%) treated with RT were treated in Seoul (Table 5). If we assume that the optimal rate of RT patients is equal to the percentage of population in each prefecture, Seoul had 2.25 fold of RT patients and Chungbuk had 0.35 fold of RT patients. This phenomenon of concentration in Seoul therefore seems very extreme. To explain this severe disproportion between regions, we need to analyze the infrastructure of RT in Korea. However, unfortunately, no such study has been published after 2007 [19]. We are preparing for the report about the status of the infrastructure of radiotherapy in Korea (2015).
The total number of patients who underwent RT increased steadily from 2011 to 2015 in Korea. The utilization rate of RT in cancer patients is also increasing. These trends are expected to continue because the incidences of breast and lung cancers with treatment heavily dependent on RT are also experiencing a rising trend in Korea.
Acknowledgments
This study was supported by a grant of the Korea Institute of Radiological and Medical Sciences (KIRAMS), funded by Ministry of Science, ICT and Future Planning, Republic of Korea (1711045544; 1711042677; 1711045548; 1711045553; 1711045555/50534-2017).
Footnotes
Conflict of interest relevant to this article was not reported.
References
- 1.National Cancer Center . Goyang: National Cancer Center; 2017. Cancer statistics in Korea: incidence, mortality, survival, and prevalence [Internet] [cited 2017 Jan 17]. Available from: http://ncc.re.kr/cancerStatsView.ncc?bbsnum=397&searchKey=total&searchValue=&pageNum=1. [Google Scholar]
- 2.Slotman BJ, Cottier B, Bentzen SM, Heeren G, Lievens Y, van den Bogaert W. Overview of national guidelines for infrastructure and staffing of radiotherapy. ESTRO-QUARTS: work package 1. Radiother Oncol. 2005;75:349–54. doi: 10.1016/j.radonc.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 3.Kang JK, Kim MS, Jang WI, Seo YS, Kim HJ, Cho CK, et al. The clinical utilization of radiation therapy in Korea between 2009 and 2013. Radiat Oncol J. 2016;34:88–95. doi: 10.3857/roj.2016.01753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kang JK, Kim MS, Jang WI, Kim HJ, Cho CK, Yoo HJ, et al. The clinical status of radiation therapy in Korea in 2009 and 2013. Cancer Res Treat. 2016;48:892–8. doi: 10.4143/crt.2015.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Daejeon: Statistics Korea; 2017. National Index System, Population in 2015 [Internet] [cited 2017 Jan 17]. Available from: http://www.index.go.kr/potal/main/EachDtlPageDetail.do?idx_cd=1007. [Google Scholar]
- 6.Lee N, Tuttle M. The role of external beam radiotherapy in the treatment of papillary thyroid cancer. Endocr Relat Cancer. 2006;13:971–7. doi: 10.1677/ERC-06-0039. [DOI] [PubMed] [Google Scholar]
- 7.Park SH, Kim JC, Kang MK. Technical advances in external radiotherapy for hepatocellular carcinoma. World J Gastroenterol. 2016;22:7311–21. doi: 10.3748/wjg.v22.i32.7311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kang JK, Kim MS, Cho CK, Yang KM, Yoo HJ, Kim JH, et al. Stereotactic body radiation therapy for inoperable hepatocellular carcinoma as a local salvage treatment after incomplete transarterial chemoembolization. Cancer. 2012;118:5424–31. doi: 10.1002/cncr.27533. [DOI] [PubMed] [Google Scholar]
- 9.Paik EK, Kim MS, Jang WI, Seo YS, Cho CK, Yoo HJ, et al. Benefits of stereotactic ablative radiotherapy combined with incomplete transcatheter arterial chemoembolization in hepatocellular carcinoma. Radiat Oncol. 2016;11:22. doi: 10.1186/s13014-016-0597-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rim CH, Seong J. Application of radiotherapy for hepatocellular carcinoma in current clinical practice guidelines. Radiat Oncol J. 2016;34:160–7. doi: 10.3857/roj.2016.01970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bae BK, Kim JC. The response of thrombosis in the portal vein or hepatic vein in hepatocellular carcinoma to radiation therapy. Radiat Oncol J. 2016;34:168–76. doi: 10.3857/roj.2016.01669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seol SW, Yu JI, Park HC, Lim DH, Oh D, Noh JM, et al. Treatment outcome of hepatic re-irradiation in patients with hepatocellular carcinoma. Radiat Oncol J. 2015;33:276–83. doi: 10.3857/roj.2015.33.4.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Korean Liver Cancer Study Group (KLCSG) National Cancer Center Korea (NCC) 2014 KLCSG-NCC Korea practice guideline for the management of hepatocellular carcinoma. Gut Liver. 2015;9:267–317. doi: 10.5009/gnl14460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barton MB, Jacob S, Shafiq J, Wong K, Thompson SR, Hanna TP, et al. Estimating the demand for radiotherapy from the evidence: a review of changes from 2003 to 2012. Radiother Oncol. 2014;112:140–4. doi: 10.1016/j.radonc.2014.03.024. [DOI] [PubMed] [Google Scholar]
- 15.Borras JM, Lievens Y, Dunscombe P, Coffey M, Malicki J, Corral J, et al. The optimal utilization proportion of external beam radiotherapy in European countries: An ESTRO-HERO analysis. Radiother Oncol. 2015;116:38–44. doi: 10.1016/j.radonc.2015.04.018. [DOI] [PubMed] [Google Scholar]
- 16.Rosenblatt E, Barton M, Mackillop W, Fidarova E, Cordero L, Yarney J, et al. Optimal radiotherapy utilisation rate in developing countries: An IAEA study. Radiother Oncol. 2015;116:35–7. doi: 10.1016/j.radonc.2015.06.012. [DOI] [PubMed] [Google Scholar]
- 17.Mackillop WJ, Kong W, Brundage M, Hanna TP, Zhang-Salomons J, McLaughlin PY, et al. A comparison of evidence-based estimates and empirical benchmarks of the appropriate rate of use of radiation therapy in ontario. Int J Radiat Oncol Biol Phys. 2015;91:1099–107. doi: 10.1016/j.ijrobp.2014.11.026. [DOI] [PubMed] [Google Scholar]
- 18.Chung K, Han Y, Kim J, Ahn SH, Ju SG, Jung SH, et al. The first private-hospital based proton therapy center in Korea: status of the Proton Therapy Center at Samsung Medical Center. Radiat Oncol J. 2015;33:337–43. doi: 10.3857/roj.2015.33.4.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huh SJ, Korean Society of Therapeutic Radiology and Oncology (KOSTRO) Current status of the infrastructure and characteristics of radiation oncology in Korea. Jpn J Clin Oncol. 2007;37:623–7. doi: 10.1093/jjco/hym073. [DOI] [PubMed] [Google Scholar]