Abstract
Background and objective
The co-occurrence of chronic pain and post-traumatic stress symptoms (PTSS) and post-traumatic stress disorder (PTSD) has gained increasing research attention. Studies on associations among pain and PTSS or PTSD in youth have largely been conducted in the context of acute injury or trauma. Less is known about the risk for co-occurrence with paediatric chronic pain. In this review, we (1) propose a conceptual framework to outline factors salient during childhood that may be associated with symptom severity, co-occurrence and mutual maintenance, (2) present relevant literature on PTSS in youth with acute and chronic pain and identify research gaps and (3) provide recommendations to guide paediatric research examining shared symptomatology.
Databases and data treatment
Electronic databases (PubMed and Google Scholar) were used to identify relevant articles using the search terms ‘child, adolescent, paediatric, chronic pain, acute pain, post-traumatic stress symptoms and post-traumatic stress disorder’. Studies were retrieved and reviewed based on relevance to the topic.
Results
Our findings revealed that existing biobehavioural and ecological models of paediatric chronic pain lack attention to traumatic events or the potential development of PTSS. Paediatric studies are also limited by lack of a conceptual framework for understanding the prevalence, risk and trajectories of PTSS in youth with chronic pain.
Conclusions
Our new developmentally informed framework highlights individual symptoms and shared contextual factors that are important when examining potential associations among paediatric chronic pain and PTSS. Future studies should consider bidirectional and mutually maintaining associations, which will be aided by prospective, longitudinal designs.
1. Background and the importance of PTSS in the context of paediatric chronic pain
The term post-traumatic stress symptom (PTSS) describes symptom-level responses (e.g. re-experiencing, hyperarousal and avoidance) that can occur after a major life stressor or traumatic event. Symptoms can emerge immediately after the event or be delayed several months or years. Distinct from diagnostic criteria for post-traumatic stress disorder (PTSD) or acute stress disorder (ASD), children do not need to be exposed to ‘actual or threatened death, serious injury or sexual violence’ (American Psychiatric 2013) to have post-traumatic stress symptomatology. Major stressors such as hospitalizations, separation from loved ones and peer bullying can be classified as traumas that have the potential to precipitate PTSS.
The experience of trauma is common during childhood. Results of one large epidemiologic study found that approximately 30% of youth experienced one or more traumatic events by age 16, with 13% of those youth endorsing symptoms of post-traumatic stress (Copeland et al., 2007). Researchers have examined factors that predict the development of PTSS in youth and have identified previous trauma history, presence of an anxiety disorder and family factors (e.g. parent PTSS and family adversity) (Copeland et al., 2007; De Young et al., 2014) as conferring risk. A strong literature exists for understanding event-related trauma reactions in children (e.g. natural disaster and motor vehicle accidents). Several risk factors have been identified for heightened trauma reactions, including pre-trauma child characteristics (e.g. age and psychological functioning), contextual factors during the trauma (e.g. perceived threat and level of exposure) and post-trauma variables (e.g. parental responses, support and stressors) (La Greca et al., 1998). Although many of these factors have also been shown to be associated with pain and disability in youth, existing biobehavioural and ecological models of paediatric chronic pain do not incorporate the experience of traumatic events or potential for development of PTSS or PTSD in these youth.
Within the context of other serious or life-threatening medical conditions such as cancer, PTSS and PTSD have been well studied. The lifetime prevalence of PTSD ranges 20–35% in child cancer survivors and 27–54% in their parents (Bruce, 2006). Within this population, several predictors of PTSS severity have been identified, including female sex (of both child and parent) (Kazak et al., 1997; Fuemmeler et al., 2001), prior stressful events, family functioning and social support (see review, Bruce, 2006). The rates of PTSS in other samples of hospitalized or injured children vary widely (10–44%) depending on diagnosis and timing of assessment (Landolt et al., 2003; De Young et al., 2014). This and other research on PTSS in youth indicates that symptoms may not be the result of a single lifethreatening traumatic event but rather emerge after experiencing several major stressors or traumas in the context of other psychosocial difficulties.
The co-occurrence of chronic pain and post-traumatic stress symptoms (PTSS) and post-traumatic stress disorder (PTSD) has gained increasing attention in the adult research literature. Studies in adult samples highlight high comorbidity and suggest that the presence of pain can shape the PTSD experience (Page et al., 2009). This research also shows altered pain processing in adults with PTSD (Geuze et al., 2007) and that the presence of even subsyndromal PTSD symptoms is associated with greater pain complaints (Asmundson et al., 2004). Several theoretical models describe shared vulnerabilities and/or mutually maintaining factors (e.g. anxiety sensitivity, attentional bias and intrusive memories) that contribute to the development and maintenance of comorbid symptoms of pain and PTSD (Sharp and Harvey, 2001; Asmundson et al., 2002; Asmundson, 2014). Additionally, Liedl and Knaevelsrud (2008) put forth the perpetual avoidance model (PAM), which describes PTSD symptoms as contributing to the development of chronic pain through hyperarousal, muscle tension and avoidance. Research shows support for bidirectional influences between perpetual avoidance and pain, with PTSD symptom clusters of re-experiencing and arousal immediately after a trauma predicting pain at 3 months, and pain at 3 months predicting PTSD symptom clusters at 12 months (Liedl et al., 2010).
While these models have been tested in adults who have experienced trauma, they have not yet been applied to paediatric populations. The influences of the developmental and interpersonal contexts in which these problems occur and are maintained are relevant to incorporate into a paediatric-specific model of PTSS and pain. Moreover, extant research in paediatrics has identified the importance of pain-specific cognitive biases (e.g. catastrophizing) in children’s pain experiences and may also serve a contributing role to the co-occurrence or mutual maintenance of PTSS and pain symptoms.
The small body of literature that has examined the co-occurrence of pain and PTSS or PTSD in youth has predominantly examined children’s exposure to physical and sexual abuse (Zafar et al., 2012; Sonneveld et al., 2013) or an inciting trauma (e.g. sports injury and accident) that temporally precedes the onset of pain and PTSS or PTSD symptoms. PTSS has also been studied in the context of paediatric traumatic brain injury (TBI). These studies showed that early symptoms of PTSD and depression predicted functional impairment 12 and 24 months after trauma (Zatzick et al., 2008) and that PTSD symptoms predicted pain 3 and 6 months after the TBI (Brown et al., 2014). Based on their findings, Brown et al. (2014) presented a post-traumatic maintenance model which proposes that in youth with TBI, distress following trauma influences pain, but pain itself does not predict the level of post-traumatic distress.
Research conducted globally suggests that childhood adversities and trauma are linked to the development of chronic pain in adulthood (Jones et al., 2009; Stickley et al., 2015), emphasizing the need for clinical and research attention during earlier developmental periods. Most of this work has been retrospective and failed to examine whether pain makes individuals vulnerable to developing PTSS following trauma. Irrespective of the source or timing of trauma, associated symptomatology may increase vulnerability to and maintenance of chronic pain. Overall work in this area suggests that associations between PTSS and chronic pain in youth are likely bidirectional and mutually maintaining.
In this topical review, we aim to (1) propose a conceptual framework to outline contextual factors salient during childhood and adolescence that may be associated with symptom severity, co-occurrence and mutual maintenance of pain and PTSS in youth, (2) present relevant literature on PTSS symptoms in youth with acute and chronic pain and identify research gaps and (3) provide recommendations to guide paediatric research examining potential shared symptomatology among PTSS and chronic pain. Throughout the review, we highlight dynamic factors that may change across children’s development. Because the presence of PTSS alone has been shown to negatively impact child outcomes (Kazak et al., 2006), and in many youth with chronic pain a single life-threatening event may not have occurred, we focus on the impact of PTSS rather than a clinical PTSD diagnosis. That said, relevant PTSD literature is included as applicable.
To conduct this review, electronic databases (PubMed and Google Scholar) were searched to identify relevant articles. Search terms used were ‘child, adolescent, paediatric, chronic pain, acute pain, post-traumatic stress symptoms and post-traumatic stress disorder’. Studies were retrieved and reviewed based on relevance to the topic. It is important to note that this article is a topical review and the goal is to bring attention to a research area, highlight gaps and spark future research. A systematic literature review was not conducted.
2. A new paediatric model conceptualizing associations among PTSS and chronic pain
In Fig. 1, we present a new developmentally informed framework to highlight individual symptoms and shared contextual factors in the potential associations among chronic pain and PTSS in youth. With intention, the outer circles show the influences of the interpersonal (parent, family and peer influences) and neurobiological (shared activation patterns and impact of trauma on the brain) contexts on comorbidity. The pie diagram placed in the centre of Fig. 1 outlines symptoms and factors that are probable contributors to comorbidity in youth. These factors are likely to influence each other and to influence symptom and diagnostic trajectories for children and adolescents. Our framework posits that associations among PTSS and chronic pain in youth are likely bidirectional and mutually maintaining. Moreover, symptoms and behaviours presented within the inner circle can reciprocally influence contextual factors (e.g. parent–child relationships and cortical connectivity). The factors in the pie diagram may represent direct, moderating, or mediating effects on children’s outcomes over time. This new framework is needed because existing biobehavioural and ecological models of paediatric chronic pain do not incorporate either the experience of traumatic events or the development of PTSS. Furthermore, paediatric studies are limited by the lack of a conceptual framework for understanding the prevalence, risk and trajectories of PTSS in youth with chronic pain.
Figure 1.
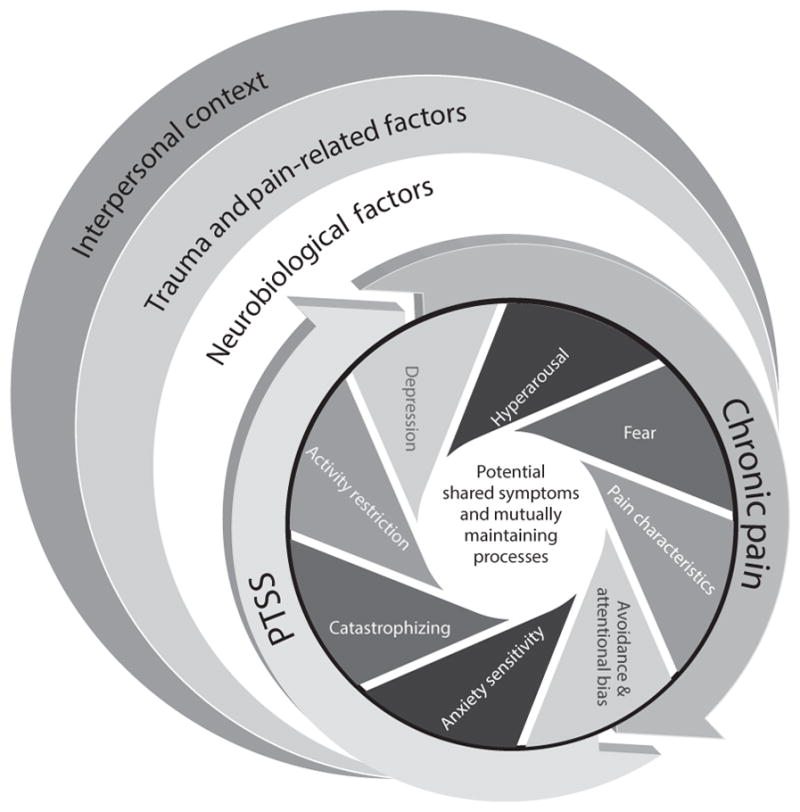
Proposed framework for examining potential associations among chronic pain and PTSS in youth.
2.1 Interpersonal context: the roles of parents, family and peers
2.1.1 Potential parent and family influences on symptom co-occurrence
Parent and family factors have received considerable attention in the child anxiety, PTSS and child pain literatures. Parent and family influences have been identified as important determinants of children’s adaptation at the time a traumatic event occurs and immediately afterwards, both influencing children’s interpretation of the event and subsequent adaptation. For example, high levels of PTSS symptoms in parents of injured children are associated with poorer child recovery (Landolt et al., 2012) and perceptions of child health (Kassam-Adams et al., 2009). Maternal factors (e.g. emotional sensitivity) have also been shown to predict PTSD symptoms in a longitudinal study of young children who experienced a life-threatening trauma (Scheeringa et al., 2015). Witnessing high parental distress increases children’s own PTSS (Fairbrother et al., 2003; Wilson et al., 2010), and specific parent behaviours (e.g. overprotectiveness and coping assistance) are associated with maladaptive child reactions (Bokszczanin, 2008). Conversely, other studies have shown that parent and child PTSS reactions can be independent. In a study of youth with chronic illnesses, there were no associations found between reported symptoms of PTSS in parents and in children (Landolt et al., 2003). That said, in this same study, children’s functional status predicted PTSS levels in parents and children, indicating that specific factors can influence or contribute to shared symptom presentation.
In paediatric chronic pain, parent cognitions, emotions and behaviours towards children’s pain can influence child coping and adaptation and are dynamic over the course of children’s development (Palermo et al., 2014). Moreover, parental distress is associated with child distress and maladaptive behaviours. Parents of youth with chronic pain can directly influence their child’s avoidance behaviour (e.g. removing them from pain-inducing activities), and this may be particularly likely during earlier developmental periods (Asmundson et al., 2012). Poorer family functioning (e.g. higher levels of stress and conflict) in families of youth with chronic pain has also been associated with greater child pain and pain-related disability (Lewandowski et al., 2010). This research highlights the importance of examining functioning of the family unit as well as dyadic relationships in chronic pain populations, particularly as family dysfunction is associated with poor outcomes.
We propose that baseline parent–child relationship quality and ongoing parent–child interactions influence the co-occurrence of PTSS and chronic pain. Dyadic factors such as communal coping or catastrophizing, parent and child threat appraisal and parent–child communication and relationship variables (Robbie Rossman et al., 1997; Muris and Field, 2010; Vervoort et al., 2012; Lynch-Jordan et al., 2013) are important to consider as they are likely to impact the persistence of pain problems, PTSS and related behavioural patterns such as avoidance. Moreover, the relationship between child and parent coping styles is dynamic across children’s development, and dyadic processes occur in the context of the broader family environment. In samples of youth with co-occurring chronic pain and PTSS symptoms, PTSS in both children with chronic pain and their parents will be critical to assess to determine directionality of these relationships.
2.1.2 Peer difficulties as potential risk factors
The reliance on and influence of parents versus peers is expected to change as children age and acquire increasing autonomy. Over childhood, peer interactions play an increasingly important role in the child’s social environment and thus may play an influential role in chronic pain and PTSS co-occurrence. Within both the pain and PTSS literatures, the impact of peer difficulties (e.g. teasing and bullying) has been documented and is becoming an increasingly important focus in chronic pain research. Children with chronic pain are often isolated from peers (Forgeron et al., 2013) and at-risk for bullying, victimization and friendship difficulties (Greco et al., 2007; Forgeron et al., 2010). In adolescent PTSS samples, symptomatology has been associated with peer victimization, with bullying identified as a specific risk factor for PTSD (Mynard et al., 2000; Idsoe et al., 2012). Specific to chronic pain, longitudinal studies are needed to understand whether peer difficulties precede or follow chronic pain onset, and how bullying or teasing may be a risk factor for PTSS development.
While no studies have examined peer difficulties in children with co-occurring chronic pain and PTSS, it is possible that the presence of social problems may be heightened in this population given additional stressors associated with bullying, teasing and relational aggression. It is also possible that achieving typical developmental milestones such as establishing positive peer relationships and individuating from parents is less likely to be achieved in youth with chronic pain. Whether negative or absent peer interactions precede pain onset or develop in response to pain, they may play a key role in shaping a child’s psychological responses to stress and the availability of coping resources. Peers may also influence the development and reframing of pain memories potentially influencing the expression of pain and PTSS.
2.2 Neurobiological context
The neurobiological context is also a critical component of the paediatric framework presented in Fig. 1. Chronic pain and PTSD are both complex experiences that involve multiple neural networks, and neuroimaging research increasingly highlights the importance of shared brain regions and similarities in activation patterns. The majority of neuroimaging research examining pain responses in PTSD or PTSS samples has been in adults. Imaging studies of adults with PTSD have focused on the amygdala, medial prefrontal cortex (mPFC) and the hippocampus, with findings revealing increased connectivity and activation during states of hyperarousal and symptom re-experiencing (Shin et al., 2006; Dunkley et al., 2014; Sadeh et al., 2014). Studies of adults with PTSD also show altered brain activation to laboratory-based heat pain stimuli (Geuze et al., 2007; Strigo et al., 2010). Specifically Geuze’s study showed that compared with controls, adults with PTSD showed: (1) increased left hippocampus activation and decreased activation in both the ventrolateral prefrontal cortex and the right amygdala during a fixed temperature (43 °C) task, and (2) increased activation in the bilateral insula and right putamen and decreased activity in the right precentral gyrus and right amygdala during individually determined temperature task (Geuze et al., 2007). In Strigo’s female-only sample, women with PTSD had greater activation of right middle insula and right dorsolateral prefrontal cortex during an initial heat pain task. However, with repeated exposure to heat pain stimuli, participants had an attenuation of activation within the right anterior insula and reported lower subjective pain intensity. Attenuation was associated with avoidance symptoms of PTSD (Strigo et al., 2010).
Imaging research with paediatric pain populations is in its infancy, although there is emerging work. For example, one research group has examined the changes in grey matter and functional connectivity in youth from pre- to post-treatment in an intensive pain treatment programme (Erpelding et al., 2014; Simons et al., 2014). These studies focused on pain-related fear as a potential mechanism, finding greater amygdala connectivity in youth with higher levels of pain-related fear, and as pain-related fear decreased over treatment, connectivity patterns changed.
Similar amygdala networks have been associated with self-reported trauma symptoms in adolescents (without psychiatric diagnoses), suggesting that the same neurological networks involved in chronic pain may also be influenced by trauma (Nooner et al., 2013). Together these data suggest that imaging studies are needed to explore whether alterations in brain networks due to trauma might predispose a child to developing chronic pain or to experiencing increased pain-related fear. Alternatively, it is also possible that chronic pain might lead to brain alterations that put a child at increased risk for developing PTSS.
2.3 Potentially shared symptomatology and mutually maintaining processes in PTSS and chronic pain
2.3.1 Trauma and pain-related factors
Characteristics of trauma (perceived threat and level of exposure) and the pain experience are intricately associated and together shape an individual’s psychological responses and impairment. Pain is interpreted by the individual as a threat to homeostasis and resultant automatic physiological responses occur (changes in blood pressure and heart rate). Additionally, the experience of pain can invoke fear and helplessness, which are central features of PTSS. The Threat Imminence Model (in animals) describes innate defensive responses to threats (selective attention and escape behaviour) that depend on the proximity to the danger. Hamm et al. (2014) applied this model to panic disorder, suggesting that autonomic arousal (e.g. racing heart and sweaty palms) and fear can trigger panic and defensive/escape behaviours. Following a panic attack, mild bodily sensations can become conditioned such that over time, through alterations in brain circuitry, these sensations trigger threat and lead to increased hypervigilance. As these bodily sensations become more intense, more extreme fear/defensive responses (e.g. panic attack) can be evoked. This model might be applied to pain populations, where following a trauma, internal physiologic signals are triggered by distal threat cues and, in conjunction with activated brain circuitry, contribute to arousal and perception of pain. Moreover, arousal may trigger pain perception even in the absence of threat cues and pain may serve to further fuel fear responses. Research in adults has also shown that innate physiological responses to fear are automatic and that individuals with higher negative affect (including PTSD) have higher magnitude startle responses and greater startle sensitivity (Lang et al., 2000). These data suggest that psychological factors can impact sensitivity to threatening physiological stimuli and that individuals who have experienced trauma may be primed for higher pain reactivity by virtue of having a lower threshold for deployment of automatic defensive responses when pain is experienced.
Importantly, pain can also lead to systematic distortions of memory in the context of chronic pain (Meyer et al., 2015), which might make individuals more susceptible to re-experiencing symptoms that are characteristic of PTSS. Higher pain intensity and inadequate pain management have also been found to be associated with increased PTSD symptoms in youth hospitalized for acute burn-related injuries (e.g. due to unintentional trauma such as house fires and hot water spills) (Saxe et al., 2001, 2005). In their 2008 review examining the impact of unintentional trauma on children, Gold et al. (2008) emphasized early identification of pain and acute stress symptoms as important for preventing the development of PTSD.
2.3.2 Cognitive biases
Cognitive biases include attentional and memory biases, threat appraisal and catastrophizing. Attentional biases towards pain and trauma-related cues are posited to underlie the development and maintenance of both chronic pain and PTSD in adults (Sharp and Harvey, 2001; Asmundson et al., 2002). The role of attentional biases in chronic pain is well studied in adults (e.g. Crombez et al., 2005, 2013; Liossi, 2012) but is just emerging in children. Attentional biases towards pain-related information may facilitate a focus on symptoms and potential threat, thus increasing the risk for PTSS in youth. For example, research conducted in a clinical sample of youth with functional abdominal pain indicates preferential attention towards pain-related information (Beck et al., 2011). However, research with children suggests that attentional bias away from threat may also be maladaptive, which is seen in chronic pain and in PTSS. Indeed, children with higher pain catastrophizing tend to shift attention away from pain, exhibit more avoidance behaviour and have parents who also catastrophize more about their pain (Vervoort et al., 2013). Pain catastrophizing has also been shown to be associated with disability at 6-month follow-up (Vervoort et al., 2009).
Parents’ attentional biases should also be considered as they play a role in shaping children’s responses to contextual threat. Parents who catastrophize about their child’s pain may engage in attentional avoidance and attempt to control their child’s pain to reduce their own distress (Caes et al., 2011; Vervoort et al., 2011, 2014), thus influencing the child’s pain-related cognitions and behaviours. Parents’ attentional biases related to child trauma have not been specifically studied. However, parents can experience clinically significant levels of PTSS related to their child’s trauma experiences (Alderfer et al., 2005; Hall et al., 2006; Martin-Herz et al., 2012), and parental PTSS influences children’s outcomes over time (Scheeringa et al., 2015). Thus, it is likely that parental attentional biases related to trauma cues influence the child’s cognitive responses to traumatic events and this is an important area of future study.
Another area of cognitive bias that is relevant to the co-occurrence of PTSS and pain is memory. Re-experiencing, a core symptom cluster of PTSD, is characterized by intense and threatening memories of the traumatic event, and PTSD is associated with memory disruption, fragmentation and distortion (Coles and Heimberg, 2002; Bedard-Gilligan and Zoellner, 2012). Catastrophic thinking about pain and anxiety has been shown to influence the development of children’s expectancies and memories of pain, with higher catastrophizing and anxiety linked to increasingly distressing pain memories over time (Noel et al., 2012a, 2015). Once developed, these pain memories are related to increases in distress during subsequent pain experiences (Noel et al., 2012b) and have been implicated in the development and maintenance of pain chronicity (Flor, 2012). Once pain becomes chronic, pain can further fuel memory biases (Meyer et al., 2015). Taken together, memory biases might make youth vulnerable to developing PTSS and chronic pain as well as serve to maintain both conditions. Given their malleable nature, they might also be fruitful targets for intervention aimed at reducing co-occurrence and resulting disability.
2.3.3 Avoidance and activity limitations
Avoidance of thoughts, feelings and external reminders (e.g. people and places) connected to trauma are characteristic of PTSS (American Psychiatric 2013). In children exposed to trauma, effortful avoidance has been shown to be associated with impairment (Kassam-Adams et al., 2010). Children’s avoidance of pain is also important to consider in the development and/or maintenance of PTSS. In the context of pain, avoidance may heighten risk for pain chronicity (Sharp and Harvey, 2001; Asmundson et al., 2012). Specifically the Pediatric Fear Avoidance Model posits that a child’s fear of pain leads to a self-perpetuating cycle of avoidance and activity limitations, fuelled by psychological factors such as catastrophizing and depression (Asmundson et al., 2012). Avoidant coping in youth with chronic pain has been associated with activity disengagement, self-isolation, depressive symptoms, disability and low perceived school and social competence (Claar et al., 2008; Walker et al., 2008). In youth with chronic pain, cognitive biases can lead to behavioural avoidance and activity restriction, which in turn contribute to adverse functional and economic impacts on the entire family (Eccleston and Clinch, 2007).
2.3.4 Hyperarousal
Hyperarousal (including sleep disturbance and hypervigilance) is a key feature of PTSS and one of four symptom clusters used in PTSD diagnosis (American Psychiatric 2013). Autonomic arousal leads to increased attention and information processing, which can influence memory encoding and recall for traumatic events (Critchley et al., 2013). In non-pain samples, hyperarousal is found in youth exposed to traumatic events and abuse (Horowitz et al., 1995; Chaffin et al., 1997). Heightened arousal is also particularly relevant to paediatric pain, as hyperarousal to bodily sensations is incompatible with sleep and potentially increases pain sensitivity, lowers pain tolerance and decreases a child’s ability to cope (Lewin and Dahl, 1999; Palermo et al., 2011). In adults with chronic pain, pain can trigger hyperarousal (Page et al., 2009), and both pain and hyperarousal are associated with poorer functioning (Cho et al., 2011). Moreover, hyperarousal increases AS, leading to pain catastrophizing and fear avoidant behaviours (Lopez-Martinez et al., 2014). Research examining hyperarousal and PTSS in paediatric chronic pain samples is needed, as PTSS may further contribute to arousal-related sleep disturbances, pain sensitivity, catastrophizing and avoidance.
2.3.5 Anxiety sensitivity
Anxiety sensitivity (AS) or fear of anxiety-related sensations as signalling physical, psychological and social threat (Reiss and McNally, 1985) is associated with PTSD in youth exposed to trauma (Hensley and Varela, 2008; Leen-Feldner et al., 2008). AS develops early in life and is shaped by vicarious (e.g. modelling illness) and instrumental (e.g. reinforcement of sick behaviours) learning that involves interactions with parents (Watt et al., 2008). Among youth with chronic pain, AS predicts greater pain-related fear and anxiety (Martin et al., 2007) and poorer health (Tsao et al., 2007), social functioning (Tsao et al., 2007) and quality of life (Mahrer et al., 2012). AS also has been shown to predict persistent post-surgical pain 6–12 months following surgery (Page et al., 2013). While research has not examined associations among PTSS and AS in paediatric pain samples, AS is implicated in the development and maintenance of PTSD in adults with chronic pain. AS increases catastrophic cognitions (Sharp and Harvey, 2001; Asmundson et al., 2002), which promotes avoidance (see review, (Ocanez et al., 2010). We propose that AS may serve a similar role in paediatric chronic pain. We conceptualize AS as a dispositional variable that can be shaped by interpersonal influences and view it as a risk factor for developing and maintaining pain and PTSS symptoms.
2.3.6 Depression
Comorbidity among depressive symptoms and PTSS in youth has largely focused on refugee populations, children who have experienced abuse or youth in foster care. Adult research demonstrates that depression is a common factor underlying both PTSD and chronic pain (e.g. Sharp and Harvey, 2001), with activity restriction and fatigue characteristic of depression hypothesized to maintain both disorders by fuelling disability and impeding exposure to avoided stimuli. Given depressive symptoms are elevated in youth with chronic pain (Blaauw et al., 2014; Coenders et al., 2014), and predict pain persisting into adulthood (Horst et al., 2014), we posit that depression in youth may confer risk for PTSS and pain-related disability. Parental depression has recently been implicated in the development of paediatric chronic pain and severity of PTSS in youth (Coenders et al., 2014), indicating that parental psychological functioning may also play a role in this co-occurrence. Results of a meta-analysis also show that parental depressive symptoms and parental PTSS were associated with child PTSS symptomatology (Morris et al., 2012). More research is needed to understand whether depression is an antecedent, consequence or mechanism underlying both PTSS and chronic pain.
2.3.7 Perceived injustice
In adults, perceived injustice is defined as a person’s feelings of loss, blame and unfairness, including negative appraisals of the severity and irreparability of limitations (Sullivan, 2008). This concept may also be important to examine in the context of paediatric chronic pain and PTSS. Relevant to chronic pain, feelings of perceived injustice (e.g. ‘why me?’; ‘my life is changed forever’) may perpetuate arousal and a focus on pain symptoms, thereby leading to an increase in psychological symptoms or functional limitations. In the adult literature, perceived injustice has been identified as a risk factor for the development or persistence of chronic pain in people with whiplash injuries (Ferrari, 2014), and as a predictor of disability, and PTSS following injury and surgery (Sullivan et al., 2009; Yakobov et al., 2014). Longitudinal associations have also been found with perceived injustice predicting pain intensity, severity of depression and both the presence and intensity of PTSD symptoms 12 months following motor vehicle accidents (Trost et al., 2015). Among children who have experienced trauma (motor vehicle accidents), perceived injustice was associated with increased PTSS symptomatology (Stallard and Smith, 2007). While perceived injustice has not been examined in paediatric chronic pain populations, it may similarly perpetuate arousal and pain focus in youth and may be influenced by parent responses.
3. Consideration of the developmental context
It is important to highlight that in paediatric populations consideration of the developmental context is critical. Notably, cognitive and social abilities undergo dramatic development and change over the course of childhood; therefore, associations among PTSS and chronic pain presented in Fig. 1 will likely depend on age and cognitive functioning. Over the course of development, children gain skills in understanding pain and in their cognitive and affective abilities to modulate pain (Palermo et al., 2014). Young children relate their pain experience almost exclusively to external cues or the situational context, whereas older children and adolescents have a basic understanding of the physiological nature of pain and the contribution of affective states and thoughts to the pain experience (e.g. Harbeck and Peterson, 1992).
As described above, both PTSS and chronic pain are conditions that involve distortions in memory (Koutantji et al., 1999; Moradi et al., 2000). Given memories for pain are strongly influenced by developmental factors (Noel et al., 2015), it is important to consider that children’s memories are susceptible to suggestibility and vulnerable to distortion during early developmental periods (e.g. preschool-aged years). Moreover, with age and cognitive development, children’s ability to use cognitive coping strategies increases. These coping strategies can be adaptive (e.g. distraction and positive self-statements) or maladaptive (e.g. catastrophizing). As children enter adolescence and progress towards adulthood, their ability to intentionally and capably engage in these self-regulatory processes improves and they become less reliant on external sources to cope (Skinner and Zimmer-Gembeck, 2007).
4. Future directions
Review of the literature presented above highlights gaps in knowledge of the prevalence, risk factors, course/trajectory or potential co-occurrence of chronic pain and PTSS in youth. Given that the prevalence of both PTSD and chronic pain increases throughout childhood and adolescence and both diagnoses are more common in females than males (Merikangas et al., 2010; King et al., 2011), these research gaps are striking. Furthermore, given the high co-occurrence of PTSD and chronic pain in adulthood (e.g. Asmundson et al., 2002; McWilliams et al., 2003; Otis et al., 2003) and the fact that chronic pain often first emerges in adolescence (King et al., 2011) and is linked to the development of anxiety disorders (Shelby et al., 2013), research examining this co-occurrence is warranted.
To target this gap in knowledge, descriptive studies are needed including those using standardized assessment of PTSS in paediatric pain samples and those using qualitative research methods. Well-validated measures of PTSS and PTSD (including clinical structured interviews) are available for assessment of children (e.g. www.ptsd.va.gov/). Use of such tools to systematically assess PTSS in youth newly presenting with chronic pain would help to establish prevalence rates, formulate case conceptualization and ultimately inform treatment planning. At this time, we do not know if rates of PTSS in youth with chronic pain differ from those found in healthy samples. Screening for PTSS could lead to better identification of children and families in greatest need of psychological intervention.
Importantly, psychosocial functioning or contextual factors relevant to paediatric chronic pain may not be captured with traditional PTSS measures. Qualitative research and the development of PTSS measures that appropriately capture the potentially diverse trauma experiences of youth with chronic pain are needed. Specifically, it is important to understand the range of traumatic events experienced by these youth and their parents, whether or not traumatic events are related to the pain condition, and how the experience of trauma may differ by aetiology of the pain problem (injury, idiopathic, disease-related, etc.) or type of pain. Strategies to prevent ‘focusing effects’, such as not priming individuals to focus on trauma specifically related to pain, in the measurement of trauma symptoms and use of control groups are important to consider to avoid overestimating rates of occurrence (Phipps et al., 2014).
Informed by the conceptual framework presented in Fig. 1, research in the following areas may help us to better understand associations among pain and PTSS in children.
4.1 Examine PTSS presentation in youth with chronic pain at different points during childhood and adolescence
Research suggests clustering of PTSD symptoms changes during childhood, with greater aggregation in later puberty (Carrion et al., 2002). Given that prevalence for chronic pain also peaks in adolescence (King et al., 2011), it will be important to examine how PTSD and PTSS symptom aggregation may occur in the context of chronic pain across childhood and adolescence. We hypothesize the factors contributing to and influencing co-occurrence of pain and PTSS would be dynamic during different stages of childhood and adolescence, particularly as they relate to peers and parental influences. Studies examining how these potential shared symptoms and mutually maintaining processes shown in Fig. 1 (e.g. depression, avoidance and perceived injustice) present at different stages can be later used to inform treatment strategies.
4.2 Longitudinal research should be conducted to examine trajectories of co-occurrence of pain and PTSS over time
This review highlights the dearth of knowledge available on the trajectories of symptom co-occurrence in children and adolescents. Prospective, longitudinal studies (similar to those on youth with TBI and burn injuries) are needed to assess PTSS trajectories in youth with chronic pain complaints. It is unknown whether PTSS symptoms remain elevated over the course of coping with a chronic pain condition or whether they remit over time as children and families develop stable patterns of coping with symptoms. Research to understand the role of individual and interpersonal factors presented in Fig. 1 in predicting trajectories is needed. Specific models of mechanisms by which PTSS and pain influence each other over time might also be tested in youth, as has been done in adults (Liedl et al., 2010).
4.3 Assessment of PTSS in parents of youth with chronic pain
PTSS has been shown to occur in parents of children with other medical problems (Kazak et al., 2006), and studies examining symptomatology among parents of youth with chronic pain are also needed. This is particularly relevant given the significant role of parent behaviours in shaping children’s chronic pain and functional outcomes. Specifically, these studies could examine correspondence between parent PTSS and child PTSS in child pain samples and how PTSS in parents may be associated with child symptomatology.
4.4 Imaging studies of youth with and without co-occurring symptoms
Additional imaging studies are needed to further understand the neurobiological context and explore whether alterations in brain networks due to trauma might predispose a child to develop chronic pain or to experience increased pain-related fear. Imaging research with youth with chronic pain may help to elicit if persistent pain might lead to brain alterations that put a child at increased risk for developing PTSS. Experimental designs in which youth with PTSS undergo pain tasks in the scanner should also be considered to determine if brain activation patterns to pain stimuli are similar or different as compared to those found in adults. Finally, imaging studies should use longitudinal designs and samples of children across stages of development to help in understanding how age and development impacts brain–behaviour associations.
4.5 Developing dually targeted interventions for paediatric populations
If future research indicates co-occurrence among PTSD or PTSS and chronic pain in youth, dually targeted interventions may be needed. Combined intervention for PTSD and chronic pain has shown efficacy in several adult populations. For example, in veterans, Plagge et al. (2013) adapted an existing PTSD behavioural activation treatment to include education about pain and a focus on movement and exercise. Another intervention programme included both components of cognitive processing therapy (CPT) for PTSD and cognitive behavioural therapy (CBT) for chronic pain management for veterans (Otis et al., 2009). Interoceptive exposure in combination with trauma-related exposure therapy has also shown preliminary efficacy in treating adults with comorbid PTSD and chronic pain injured in automobile accidents (Wald et al., 2010). In paediatric pain populations, interoceptive exposure [as a component of the pain provocation technique (PPT)] has shown preliminary effectiveness in reducing pain intensity and school avoidance (Hechler et al., 2010). Further definitive trials are needed to understand the potential benefit of interoceptive exposure strategies for co-occurring chronic pain and PTSS.
Overall, our framework suggests that treatments targeting youth with co-occurring PTSS and chronic pain need to take into account developmental status and incorporate a focus on interpersonal and social factors (e.g. parent behaviours). Moreover, given that many of the mutually maintaining factors presented in Fig. 1 are malleable (e.g. activity limitations and attentional biases), these factors might also be important intervention targets.
5. Conclusion
Limited work has been conducted to understand the prevalence, risk and trajectories of PTSS in children and adolescents with chronic pain. Investigators have not yet applied conceptual frameworks to examine how individual and interpersonal factors may confer risk for PTSS and paediatric chronic pain. We strongly encourage research concerning the co-occurrence of chronic pain and PTSS in children and adolescents. We hope that our proposed framework (Fig. 1) and recommendations presented above may provide a springboard for identifying developmentally relevant processes that can be studied in paediatric pain and guide future studies to address these important research gaps.
What does this review add?
This review presents relevant literature on pain and PTSS in youth and proposes a conceptual framework to examine factors salient during childhood that may be associated with symptom severity, comorbidity and mutual maintenance of chronic pain and PTSS in paediatric populations.
We highlight dynamic factors that may change across children’s development and provide recommendations to guide paediatric research examining potential associations among PTSS and chronic pain.
Acknowledgments
Funding sources
This study was supported by the Career Development Awards from the Eunice Kennedy Shriver National Institute on Child Health and Human Development (K23HD071946, ALH; K23 HD064705, AW; K24HD060068, TP). During the time that this research was conducted, Dr. Noel was funded by a Post-PhD Fellowship Award from the Canadian Institutes of Health Research and was a trainee member of Pain in Child Health, a Strategic Training Initiative in Health Research of the Canadian Institutes of Health Research.
We thank Rob Boy for his assistance with the graphic design of the figure that accompanies this article.
Footnotes
Conflicts of interest
The authors have no conflicts of interest to declare.
Author contributions
All authors: Conceptualization and design of review, review of relevant literature, drafting the article and final approval of submitted version.
References
- Alderfer MA, Cnaan A, Annunziato RA, Kazak AE. Patterns of posttraumatic stress symptoms in parents of childhood cancer survivors. J Fam Psychol. 2005;19:430–440. doi: 10.1037/0893-3200.19.3.430. [DOI] [PubMed] [Google Scholar]
- American Psychiatric A. Diagnostic and Statistical Manual of Mental Disorders: DSM-V. Washington DC: American Psychiatric Association; 2013. [Google Scholar]
- Asmundson GJ. The emotional and physical pains of trauma: Contemporary and innovative approaches for treating co-occurring PTSD and chronic pain. Depress Anxiety. 2014;31:717–720. doi: 10.1002/da.22285. [DOI] [PubMed] [Google Scholar]
- Asmundson GJ, Coons MJ, Taylor S, Katz J. PTSD and the experience of pain: Research and clinical implications of shared vulnerability andmutual maintenancemodels. Can J Psychiat. 2002;47:930–937. doi: 10.1177/070674370204701004. [DOI] [PubMed] [Google Scholar]
- Asmundson GJ, Wright KD, Stein MB. Pain and PTSD symptoms in female veterans. Eur J Pain. 2004;8:345–350. doi: 10.1016/j.ejpain.2003.10.008. [DOI] [PubMed] [Google Scholar]
- Asmundson GJ, Noel M, Petter M, Parkerson HA. Pediatric fear-avoidance model of chronic pain: Foundation, application and future directions. Pain Res Manag. 2012;17:397–405. doi: 10.1155/2012/908061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck JE, Lipani TA, Baber KF, Dufton L, Garber J, Smith CA, Walker LS. Attentional bias to pain and social threat in pediatric patients with functional abdominal pain and pain-free youth before and after performance evaluation. Pain. 2011;152:1061–1067. doi: 10.1016/j.pain.2011.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bedard-Gilligan M, Zoellner LA. Dissociation and memory fragmentation in post-traumatic stress disorder: An evaluation of the dissociative encoding hypothesis. Memory. 2012;20:277–299. doi: 10.1080/09658211.2012.655747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blaauw BA, Dyb G, Hagen K, Holmen TL, Linde M, Wentzel- Larsen T, Zwart JA. Anxiety, depression and behavioral problems among adolescents with recurrent headache: The Young- HUNT study. J Headache Pain. 2014;15:38. doi: 10.1186/1129-2377-15-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bokszczanin A. Parental support, family conflict, and overprotectiveness: Predicting PTSD symptom levels of adolescents 28 months after a natural disaster. Anxiety Stress Coping. 2008;21:325–335. doi: 10.1080/10615800801950584. [DOI] [PubMed] [Google Scholar]
- Brown EA, Kenardy JA, Dow BL. PTSD perpetuates pain in children with traumatic brain injury. J Pediatr Psychol. 2014;39:512–520. doi: 10.1093/jpepsy/jsu014. [DOI] [PubMed] [Google Scholar]
- Bruce M. A systematic and conceptual review of posttraumatic stress in childhood cancer survivors and their parents. Clin Psychol Rev. 2006;26:233–256. doi: 10.1016/j.cpr.2005.10.002. [DOI] [PubMed] [Google Scholar]
- Caes L, Vervoort T, Eccleston C, Vandenhende M, Goubert L. Parental catastrophizing about child’s pain and its relationship with activity restriction: The mediating role of parental distress. Pain. 2011;152:212–222. doi: 10.1016/j.pain.2010.10.037. [DOI] [PubMed] [Google Scholar]
- Carrion VG, Weems CF, Ray R, Reiss AL. Toward an empirical definition of pediatric PTSD: The phenomenology of PTSD symptoms in youth. J Am Acad Child Adolesc Psychiatry. 2002;41:166–173. doi: 10.1097/00004583-200202000-00010. [DOI] [PubMed] [Google Scholar]
- Chaffin M, Wherry JN, Dykman R. School age children’s coping with sexual abuse: Abuse stresses and symptoms associated with four coping strategies. Child Abuse Negl. 1997;21:227–240. doi: 10.1016/s0145-2134(96)00148-2. [DOI] [PubMed] [Google Scholar]
- Cho SK, Heiby EM, McCracken LM, Moon DE, Lee JH. Daily functioning in chronic pain: Study of structural relations with posttraumatic stress disorder symptoms, pain intensity, and pain avoidance. Korean J Pain. 2011;24:13–21. doi: 10.3344/kjp.2011.24.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claar RL, Simons LE, Logan DE. Parental response to children’s pain: The moderating impact of children’s emotional distress on symptoms and disability. Pain. 2008;138:172–179. doi: 10.1016/j.pain.2007.12.005. [DOI] [PubMed] [Google Scholar]
- Coenders A, Chapman C, Hannaford P, Jaaniste T, Qiu W, Anderson D, Glogauer M, Goodison-Farnsworth E, McCormick M, Champion D. In search of risk factors for chronic pain in adolescents: A case-control study of childhood and parental associations. J Pain Res. 2014;7:175–183. doi: 10.2147/JPR.S48154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coles ME, Heimberg RG. Memory biases in the anxiety disorders: Current status. Clin Psychol Rev. 2002;22:587–627. doi: 10.1016/s0272-7358(01)00113-1. [DOI] [PubMed] [Google Scholar]
- Copeland WE, Keeler G, Angold A, Costello EJ. Traumatic events and posttraumatic stress in childhood. Arch Gen Psychiat. 2007;64:577–584. doi: 10.1001/archpsyc.64.5.577. [DOI] [PubMed] [Google Scholar]
- Critchley HD, Eccles J, Garfinkel SN. Interaction between cognition, emotion, and the autonomic nervous system. Handb Clin Neurol. 2013;117:59–77. doi: 10.1016/B978-0-444-53491-0.00006-7. [DOI] [PubMed] [Google Scholar]
- Crombez G, Van Damme S, Eccleston C. Hypervigilance to pain: An experimental and clinical analysis. Pain. 2005;116:4. doi: 10.1016/j.pain.2005.03.035. [DOI] [PubMed] [Google Scholar]
- Crombez G, Van Ryckeghem DM, Eccleston C, Van Damme S. Attentional bias to pain-related information: A meta-analysis. Pain. 2013;154:497–510. doi: 10.1016/j.pain.2012.11.013. [DOI] [PubMed] [Google Scholar]
- De Young AC, Hendrikz J, Kenardy JA, Cobham VE, Kimble RM. Prospective evaluation of parent distress following pediatric burns and identification of risk factors for young child and parent posttraumatic stress disorder. J Child Adol Psychop. 2014;24:9–17. doi: 10.1089/cap.2013.0066. [DOI] [PubMed] [Google Scholar]
- Dunkley BT, Doesburg SM, Sedge PA, Grodecki RJ, Shek PN, Pang EW, Taylor MJ. Resting-state hippocampal connectivity correlates with symptom severity in post-traumatic stress disorder. Neuroimage Clin. 2014;5:377–384. doi: 10.1016/j.nicl.2014.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eccleston C, Clinch J. Adolescent chronic pain and disability: A review of the current evidence in assessment and treatment. Paediatr Child Health. 2007;12:117–120. doi: 10.1093/pch/12.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erpelding N, Simons L, Lebel A, Serrano P, Pielech M, Prabhu S, Becerra L, Borsook D. Rapid treatment-induced brain changes in pediatric CRPS. Brain Struct Funct. 2014;221:1095–1111. doi: 10.1007/s00429-014-0957-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairbrother G, Stuber J, Galea S, Fleischman AR, Pfefferbaum B. Posttraumatic stress reactions in New York City children after the September 11, 2001, terrorist attacks. Ambul Pediatr. 2003;3:304–311. doi: 10.1367/1539-4409(2003)003<0304:psriny>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Ferrari R. A prospective study of perceived injustice in whiplash victims and its relationship to recovery. Clin Rheumatol. 2014;34:975–979. doi: 10.1007/s10067-014-2693-0. [DOI] [PubMed] [Google Scholar]
- Flor H. New developments in the understanding and management of persistent pain. Curr Opin Psychiatry. 2012;25:109–113. doi: 10.1097/YCO.0b013e3283503510. [DOI] [PubMed] [Google Scholar]
- Forgeron PA, King S, Stinson JN, McGrath PJ, MacDonald AJ, Chambers CT. Social functioning and peer relationships in children and adolescents with chronic pain: A systematic review. Pain Res Manag. 2010;15:27–41. doi: 10.1155/2010/820407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forgeron PA, Evans J, McGrath PJ, Stevens B, Finley GA. Living with difference: Exploring the social self of adolescents with chronic pain. Pain Res Manag. 2013;18:e115–e123. doi: 10.1155/2013/120632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuemmeler BF, Mullins LL, Marx BP. Posttraumatic stress and general distress among parents of children surviving a brain tumor. Children’s Health Care. 2001;30:169–182. [Google Scholar]
- Geuze E, Westenberg HG, Jochims A, de Kloet CS, Bohus M, Vermetten E, Schmahl C. Altered pain processing in veterans with posttraumatic stress disorder. Arch General Psychiat. 2007;64:76–85. doi: 10.1001/archpsyc.64.1.76. [DOI] [PubMed] [Google Scholar]
- Gold JI, Kant AJ, Kim SH. The impact of unintentional pediatric trauma: A review of pain, acute stress, and posttraumatic stress. J Pediatric Nursing. 2008;23:81–91. doi: 10.1016/j.pedn.2007.08.005. [DOI] [PubMed] [Google Scholar]
- Greco LA, Freeman KE, Dufton L. Overt and relational victimization among children with frequent abdominal pain: Links to social skills, academic functioning, and health service use. J Pediatr Psychol. 2007;32:319–329. doi: 10.1093/jpepsy/jsl016. [DOI] [PubMed] [Google Scholar]
- Hall E, Saxe G, Stoddard F, Kaplow J, Koenen K, Chawla N, Lopez C, King L, King D. Posttraumatic stress symptoms in parents of children with acute burns. J Pediatr Psychol. 2006;31:403–412. doi: 10.1093/jpepsy/jsj016. [DOI] [PubMed] [Google Scholar]
- Hamm AO, Richter J, Pane-Farre CA. When the threat comes from inside the body: A neuroscience based learning perspective of the etiology of panic disorder. Restor Neurol Neuros. 2014;32:79–93. doi: 10.3233/RNN-139011. [DOI] [PubMed] [Google Scholar]
- Harbeck C, Peterson L. Elephants dancing in my head: A developmental approach to children’s concepts of specific pains. Child Dev. 1992;63:138–149. [PubMed] [Google Scholar]
- Hechler T, Dobe M, Damschen U, Blankenburg M, Schroeder S, Kosfelder J, Zernikow B. The pain provocation technique for adolescents with chronic pain: Preliminary evidence for its effectiveness. Pain Med. 2010;11:897–910. doi: 10.1111/j.1526-4637.2010.00839.x. [DOI] [PubMed] [Google Scholar]
- Hensley L, Varela RE. PTSD symptoms and somatic complaints following hurricane Katrina: The roles of trait anxiety and anxiety sensitivity. J Clin Child Adolesc. 2008;37:542–552. doi: 10.1080/15374410802148186. [DOI] [PubMed] [Google Scholar]
- Horowitz K, Weine S, Jekel J. PTSD symptoms in urban adolescent girls: Compounded community trauma. J Am Acad Child Adolesc Psychiatry. 1995;34:1353–1361. doi: 10.1097/00004583-199510000-00021. [DOI] [PubMed] [Google Scholar]
- Horst S, Shelby G, Anderson J, Acra S, Polk DB, Saville BR, Garber J, Walker LS. Predicting persistence of functional abdominal pain from childhood into young adulthood. Clin Gastroenterol. 2014;12:2026–2032. doi: 10.1016/j.cgh.2014.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idsoe T, Dyregrov A, Idsoe EC. Bullying and PTSD symptoms. J Abnorm Child Psychol. 2012;40:901–911. doi: 10.1007/s10802-012-9620-0. [DOI] [PubMed] [Google Scholar]
- Jones GT, Power C, Macfarlane GJ. Adverse events in childhood and chronic widespread pain in adult life: Results from the 1958 British Birth Cohort Study. Pain. 2009;143:92–96. doi: 10.1016/j.pain.2009.02.003. [DOI] [PubMed] [Google Scholar]
- Kassam-Adams N, Fleisher CL, Winston FK. Acute stress disorder and posttraumatic stress disorder in parents of injured children. J Trauma Stress. 2009;22:294–302. doi: 10.1002/jts.20424. [DOI] [PubMed] [Google Scholar]
- Kassam-Adams N, Marsac ML, Cirilli C. Posttraumatic stress disorder symptom structure in injured children: Functional impairment and depression symptoms in a confirmatory factor analysis. J Am Acad Child Adolesc Psychiatry. 2010;49:616–625. 625e611–614. doi: 10.1016/j.jaac.2010.02.011. [DOI] [PubMed] [Google Scholar]
- Kazak AE, Barakat LP, Meeske K, Christakis D, Meadows AT, Casey R, Penati B, Stuber ML. Posttraumatic stress, family functioning, and social support in survivors of childhood leukemia and their mothers and fathers. J Consult Clin Psychol. 1997;65:120–129. doi: 10.1037//0022-006x.65.1.120. [DOI] [PubMed] [Google Scholar]
- Kazak AE, Kassam-Adams N, Schneider S, Zelikovsky N, Alderfer MA, Rourke M. An integrative model of pediatric medical traumatic stress. J Pediatr Psychol. 2006;31:343–355. doi: 10.1093/jpepsy/jsj054. [DOI] [PubMed] [Google Scholar]
- King S, Chambers CT, Huguet A, MacNevin RC, McGrath PJ, Parker L, MacDonald AJ. The epidemiology of chronic pain in children and adolescents revisited: A systematic review. Pain. 2011;152:2729–2738. doi: 10.1016/j.pain.2011.07.016. [DOI] [PubMed] [Google Scholar]
- Koutantji M, Pearce SA, Oakley DA, Feinmann C. Children in pain: An investigation of selective memory for pain and psychological adjustment. Pain. 1999;81:237–244. doi: 10.1016/S0304-3959(99)00020-2. [DOI] [PubMed] [Google Scholar]
- La Greca AM, Silverman WK, Wasserstein SB. Children’s predisaster functioning as a predictor of posttraumatic stress following Hurricane Andrew. J Consult Clin Psychol. 1998;66:883–892. doi: 10.1037//0022-006x.66.6.883. [DOI] [PubMed] [Google Scholar]
- Landolt MA, Vollrath M, Ribi K, Gnehm HE, Sennhauser FH. Incidence and associations of parental and child post-traumatic stress symptoms in pediatric patients. J Child Psychol Psychiatry. 2003;44:1199–1207. doi: 10.1111/1469-7610.00201. [DOI] [PubMed] [Google Scholar]
- Landolt MA, Ystrom E, Sennhauser FH, Gnehm HE, Vollrath ME. The mutual prospective influence of child and parental posttraumatic stress symptoms in pediatric patients. J Child Psychol Psychiatry. 2012;53:767–774. doi: 10.1111/j.1469-7610.2011.02520.x. [DOI] [PubMed] [Google Scholar]
- Lang PJ, Davis M, Ohman A. Fear and anxiety: Animal models and human cognitive psychophysiology. J Affect Disorders. 2000;61:137–159. doi: 10.1016/s0165-0327(00)00343-8. [DOI] [PubMed] [Google Scholar]
- Leen-Feldner EW, Feldner MT, Reardon LE, Babson KA, Dixon L. Anxiety sensitivity and posttraumatic stress among traumatic event-exposed youth. Behav Res Ther. 2008;46:548–556. doi: 10.1016/j.brat.2008.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewandowski AS, Palermo TM, Stinson J, Handley S, Chambers CT. Systematic review of family functioning in families of children and adolescents with chronic pain. J Pain. 2010;11:1027–1038. doi: 10.1016/j.jpain.2010.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewin DS, Dahl RE. Importance of sleep in the management of pediatric pain. J Dev Behav Pediatr. 1999;20:244–252. doi: 10.1097/00004703-199908000-00007. [DOI] [PubMed] [Google Scholar]
- Liedl A, Knaevelsrud C. Chronic pain and PTSD: The Perpetual Avoidance Model and its treatment implications. Torture. 2008;18:69–76. [PubMed] [Google Scholar]
- Liedl A, O’Donnell M, Creamer M, Silove D, McFarlane A, Knaevelsrud C, Bryant RA. Support for the mutual maintenance of pain and post-traumatic stress disorder symptoms. Psychol Med. 2010;40:1215–1223. doi: 10.1017/S0033291709991310. [DOI] [PubMed] [Google Scholar]
- Liossi C. Attentional biases in chronic pain: Do they exist and does it really matter? Pain. 2012;153:9–10. doi: 10.1016/j.pain.2011.10.013. [DOI] [PubMed] [Google Scholar]
- Lopez-Martinez AE, Ramirez-Maestre C, Esteve R. An examination of the structural link between post-traumatic stress symptoms and chronic pain in the framework of fear-avoidance models. Eur J Pain. 2014;18:1129–1138. doi: 10.1002/j.1532-2149.2014.00459.x. [DOI] [PubMed] [Google Scholar]
- Lynch-Jordan AM, Kashikar-Zuck S, Szabova A, Goldschneider KR. The interplay of parent and adolescent catastrophizing and its impact on adolescents’ pain, functioning, and pain behavior. Clin J Pain. 2013;29:681–688. doi: 10.1097/AJP.0b013e3182757720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahrer NE, Montano Z, Gold JI. Relations between anxiety sensitivity, somatization, and health-related quality of life in children with chronic pain. J Pediatr Psychol. 2012;37:808–816. doi: 10.1093/jpepsy/jss054. [DOI] [PubMed] [Google Scholar]
- Martin AL, McGrath PA, Brown SC, Katz J. Anxiety sensitivity, fear of pain and pain-related disability in children and adolescents with chronic pain. Pain Res Manag. 2007;12:267–272. doi: 10.1155/2007/897395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin-Herz SP, Rivara FP, Wang J, Russo J, Zatzick DF. Predictors of parental posttraumatic stress disorder symptoms in the year after adolescent traumatic injury. Academic Pediatrics. 2012;12:198–204. doi: 10.1016/j.acap.2012.02.008. [DOI] [PubMed] [Google Scholar]
- McWilliams LA, Cox BJ, Enns MW. Mood and anxiety disorders associated with chronic pain: An examination in a nationally representative sample. Pain. 2003;106:127–133. doi: 10.1016/s0304-3959(03)00301-4. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer P, Karl A, Flor H. Pain can produce systematic distortions of autobiographical memory. Pain Med. 2015;16:905–910. doi: 10.1111/pme.12716. [DOI] [PubMed] [Google Scholar]
- Moradi AR, Taghavi R, Neshat-Doost HT, Yule W, Dalgleish T. Memory bias for emotional information in children and adolescents with posttraumatic stress disorder: A preliminary study. J Anxiety Disord. 2000;14:521–534. doi: 10.1016/s0887-6185(00)00037-2. [DOI] [PubMed] [Google Scholar]
- Morris A, Gabert-Quillen C, Delahanty D. The association between parent PTSD/depression symptoms and child PTSD symptoms: A meta-analysis. J Pediatr Psychol. 2012;37:1076–1088. doi: 10.1093/jpepsy/jss091. [DOI] [PubMed] [Google Scholar]
- Muris P, Field AP. The role of verbal threat information in the development of childhood fear. “Beware the Jabberwock!”. Clin Child Fam Psychol Rev. 2010;13:129–150. doi: 10.1007/s10567-010-0064-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mynard H, Joseph S, Alexander J. Peer victimization & post traumatic stress. Personality Individ Differ. 2000;29:815–821. [Google Scholar]
- Noel M, Chambers CT, McGrath PJ, Klein RM, Stewart SH. The role of state anxiety in children’s memories for pain. J Pediatr Psychol. 2012a;37:567–579. doi: 10.1093/jpepsy/jss006. [DOI] [PubMed] [Google Scholar]
- Noel M, Chambers CT, Petter M, McGrath PJ, Klein RM, Stewart SH. Pain is not over when the needle ends: A review and preliminary model of acute pain memory development in childhood. Pain management. 2012b;2:487–497. doi: 10.2217/pmt.12.41. [DOI] [PubMed] [Google Scholar]
- Noel M, Palermo TM, Chambers CT, Taddio A, Hermann C. Remembering the pain of childhood: Applying a developmental perspective to the study of pain memories. Pain. 2015;156:31–34. doi: 10.1016/j.pain.0000000000000001. [DOI] [PubMed] [Google Scholar]
- Nooner KB, Mennes M, Brown S, Castellanos FX, Leventhal B, Milham MP, Colcombe SJ. Relationship of trauma symptoms to amygdala-based functional brain changes in adolescents. J Trauma Stress. 2013;26:784–787. doi: 10.1002/jts.21873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ocanez KL, McHugh RK, Otto MW. A meta-analytic review of the association between anxiety sensitivity and pain. Depress Anxiety. 2010;27:760–767. doi: 10.1002/da.20681. [DOI] [PubMed] [Google Scholar]
- Otis JD, Keane TM, Kerns RD. An examination of the relationship between chronic pain and post-traumatic stress disorder. J Rehabil Res Dev. 2003;40:397–405. doi: 10.1682/jrrd.2003.09.0397. [DOI] [PubMed] [Google Scholar]
- Otis JD, Keane TM, Kerns RD, Monson C, Scioli E. The development of an integrated treatment for veterans with comorbid chronic pain and posttraumatic stress disorder. Pain Med. 2009;10:1300–1311. doi: 10.1111/j.1526-4637.2009.00715.x. [DOI] [PubMed] [Google Scholar]
- Page GM, Kleiman V, Asmundson GJ, Katz J. Structure of posttraumatic stress disorder symptoms in pain and pain-free patients scheduled for major surgery. J Pain. 2009;10:984–991. doi: 10.1016/j.jpain.2009.03.011. [DOI] [PubMed] [Google Scholar]
- Page MG, Stinson J, Campbell F, Isaac L, Katz J. Identification of pain-related psychological risk factors for the development and maintenance of pediatric chronic postsurgical pain. J Pain Res. 2013;6:167–180. doi: 10.2147/JPR.S40846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palermo TM, Wilson AC, Lewandowski AS, Toliver-Sokol M, Murray CB. Behavioral and psychosocial factors associated with insomnia in adolescents with chronic pain. Pain. 2011;152:89–94. doi: 10.1016/j.pain.2010.09.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palermo TM, Valrie CR, Karlson CW. Family and parent influences on pediatric chronic pain: A developmental perspective. Am Psychol. 2014;69:142–152. doi: 10.1037/a0035216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phipps S, Klosky JL, Long A, Hudson MM, Huang Q, Zhang H, Noll RB. Posttraumatic stress and psychological growth in children with cancer: Has the traumatic impact of cancer been overestimated? J Clin Oncol. 2014;32:641–646. doi: 10.1200/JCO.2013.49.8212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plagge JM, Lu MW, Lovejoy TI, Karl AI, Dobscha SK. Treatment of comorbid pain and PTSD in returning veterans: A collaborative approach utilizing behavioral activation. Pain Med. 2013;14:1164–1172. doi: 10.1111/pme.12155. [DOI] [PubMed] [Google Scholar]
- Reiss S, McNally RJ. Expectancy model of fear. In: Reissand S, Bootzin RR, editors. Theoretical Issues in Behavior Therapy. San Diego: Academic Press; 1985. pp. 107–121. [Google Scholar]
- Robbie Rossman BB, Bingham RD, Emde RN. Symptomatology and adaptive functioning for children exposed to normative stressors, dog attack, and parental violence. J Am Acad Child Adol Psychiat. 1997;36:1089–1097. doi: 10.1097/00004583-199708000-00016. [DOI] [PubMed] [Google Scholar]
- Sadeh N, Spielberg JM, Warren SL, Miller GA, Heller W. Aberrant neural connectivity during emotional processing associated with posttraumatic stress. Clin Psychol Sci. 2014;2:748–755. doi: 10.1177/2167702614530113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saxe G, Stoddard F, Courtney D, Cunningham K, Chawla N, Sheridan R, King D, King L. Relationship between acute morphine and the course of PTSD in children with burns. J Am Acad Child Adol Psychiat. 2001;40:915–921. doi: 10.1097/00004583-200108000-00013. [DOI] [PubMed] [Google Scholar]
- Saxe GN, Stoddard F, Hall E, Chawla N, Lopez C, Sheridan R, King D, King L, Yehuda R. Pathways to PTSD, part I: Children with burns. Am J Psychiatry. 2005;162:1299–1304. doi: 10.1176/appi.ajp.162.7.1299. [DOI] [PubMed] [Google Scholar]
- Scheeringa MS, Myers L, Putnam FW, Zeanah CH. Maternal factors as moderators or mediators of PTSD symptoms in very young children: A two-year prospective study. J Fam Violence. 2015;30:633–642. doi: 10.1007/s10896-015-9695-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharp TJ, Harvey AG. Chronic pain and posttraumatic stress disorder: Mutual maintenance? Clin Psychol Rev. 2001;21:857–877. doi: 10.1016/s0272-7358(00)00071-4. [DOI] [PubMed] [Google Scholar]
- Shelby GD, Shirkey KC, Sherman AL, Beck JE, Haman K, Shears AR, Horst SN, Smith CA, Garber J, Walker LS. Functional abdominal pain in childhood and long-term vulnerability to anxiety disorders. Pediatrics. 2013;132:475–482. doi: 10.1542/peds.2012-2191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin LM, Rauch SL, Pitman RK. Amygdala, medial prefrontal cortex, and hippocampal function in PTSD. Ann NY Acad Sci. 2006;1071:67–79. doi: 10.1196/annals.1364.007. [DOI] [PubMed] [Google Scholar]
- Simons LE, Pielech M, Erpelding N, Linnman C, Moulton E, Sava S, Lebel A, Serrano P, Sethna N, Berde C, Becerra L, Borsook D. The responsive amygdala: Treatment-induced alterations in functional connectivity in pediatric complex regional pain syndrome. Pain. 2014;155:1727–1742. doi: 10.1016/j.pain.2014.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner EA, Zimmer-Gembeck MJ. The development of coping. Annu Rev Psychol. 2007;58:119–144. doi: 10.1146/annurev.psych.58.110405.085705. [DOI] [PubMed] [Google Scholar]
- Sonneveld LP, Brilleslijper-Kater SN, Benninga MA, Hoytema van Konijnenburg EM, Sieswerda-Hoogendoorn T, Teeuw AH. Prevalence of child sexual abuse in pediatric patients with chronic abdominal pain. J Pediatr Gastroenterol Nutr. 2013;56:475–480. doi: 10.1097/MPG.0b013e31828b5145. [DOI] [PubMed] [Google Scholar]
- Stallard P, Smith E. Appraisals and cognitive coping styles associated with chronic post-traumatic symptoms in child road traffic accident survivors. J Child Psychol Psychiatry. 2007;48:194–201. doi: 10.1111/j.1469-7610.2006.01692.x. [DOI] [PubMed] [Google Scholar]
- Stickley A, Koyanagi A, Kawakami N, Group WHOWMHJS. Childhood adversities and adult-onset chronic pain: Results from the World Mental Health Survey, Japan. Eur J Pain. 2015;19:1418–1427. doi: 10.1002/ejp.672. [DOI] [PubMed] [Google Scholar]
- Strigo IA, Simmons AN, Matthews SC, Grimes EM, Allard CB, Reinhardt LE, Paulus MP, Stein MB. Neural correlates of altered pain response in women with posttraumatic stress disorder from intimate partner violence. Biol Psychiatry. 2010;68:442–450. doi: 10.1016/j.biopsych.2010.03.034. [DOI] [PubMed] [Google Scholar]
- Sullivan MJ. Toward a biopsychomotor conceptualization of pain: Implications for research and intervention. Clin J Pain. 2008;24:281–290. doi: 10.1097/AJP.0b013e318164bb15. [DOI] [PubMed] [Google Scholar]
- Sullivan MJ, Thibault P, Simmonds MJ, Milioto M, Cantin AP, Velly AM. Pain, perceived injustice and the persistence of post-traumatic stress symptoms during the course of rehabilitation for whiplash injuries. Pain. 2009;145:325–331. doi: 10.1016/j.pain.2009.06.031. [DOI] [PubMed] [Google Scholar]
- Trost Z, Agtarap S, Scott W, Driver S, Guck A, Roden-Foreman K, Reynolds M, Foreman ML, Warren AM. Perceived injustice after traumatic injury: Associations with pain, psychological distress, and quality of life outcomes 12 months after injury. Rehabil Psychol. 2015;60:213–221. doi: 10.1037/rep0000043. [DOI] [PubMed] [Google Scholar]
- Tsao JC, Meldrum M, Kim SC, Zeltzer LK. Anxiety sensitivity and health-related quality of life in children with chronic pain. J Pain. 2007;8:814–823. doi: 10.1016/j.jpain.2007.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vervoort T, Eccleston C, Goubert L, Buysse A, Crombez G. Children’s catastrophic thinking about their pain predicts pain and disability 6 months later. Eur J Pain. 2009;14:90–96. doi: 10.1016/j.ejpain.2009.03.001. [DOI] [PubMed] [Google Scholar]
- Vervoort T, Caes L, Crombez G, Koster E, Van Damme S, Dewitte M, Goubert L. Parental catastrophizing about children’s pain and selective attention to varying levels of facial expression of pain in children: A dot-probe study. Pain. 2011;152:1751–1757. doi: 10.1016/j.pain.2011.03.015. [DOI] [PubMed] [Google Scholar]
- Vervoort T, Caes L, Trost Z, Notebaert L, Goubert L. Parental attention to their child’s pain is modulated by threat-value of pain. Health Psychol. 2012;31:623–631. doi: 10.1037/a0029292. [DOI] [PubMed] [Google Scholar]
- Vervoort T, Trost Z, Van Ryckeghem DM. Children’s selective attention to pain and avoidance behaviour: The role of child and parental catastrophizing about pain. Pain. 2013;154:1979–1988. doi: 10.1016/j.pain.2013.05.052. [DOI] [PubMed] [Google Scholar]
- Vervoort T, Trost Z, Sutterlin S, Caes L, Moors A. Emotion regulatory function of parent attention to child pain and associated implications for parental pain control behaviour. Pain. 2014;155:1453–1463. doi: 10.1016/j.pain.2014.04.015. [DOI] [PubMed] [Google Scholar]
- Wald J, Taylor S, Chiri LR, Sica C. Posttraumatic stress disorder and chronic pain arising from motor vehicle accidents: Efficacy of interoceptive exposure plus trauma-related exposure therapy. Cog Behav Ther. 2010;39:104–113. doi: 10.1080/16506070903183570. [DOI] [PubMed] [Google Scholar]
- Walker LS, Beck JE, Garber J, Lambert W. Children’s somatization inventory: Psychometric properties of the revised form (CSI-24) J Pediatr Psychol. 2008;34:430–440. doi: 10.1093/jpepsy/jsn093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt MC, O’Connor RM, Stewart SH, Moon EC, Terry L. Specificity of childhood learning experiences related to anxiety sensitivity and illness/injury sensitivity: Implications for health anxiety and pain. J Cog Psychother. 2008;39:128–142. [Google Scholar]
- Wilson AC, Lengua LJ, Meltzoff AN, Smith KA. Parenting and temperament prior to September 11, 2001, and parenting specific to 9/11 as predictors of children’s posttraumatic stress symptoms following 9/11. J Clin Child Adoles Psychol. 2010;39:445–459. doi: 10.1080/15374416.2010.486317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yakobov E, Scott W, Stanish W, Dunbar M, Richardson G, Sullivan M. The role of perceived injustice in the prediction of pain and function after total knee arthroplasty. Pain. 2014;10:2040–2046. doi: 10.1016/j.pain.2014.07.007. [DOI] [PubMed] [Google Scholar]
- Zafar M, Kashikar-Zuck SM, Slater SK, Allen JR, Barnett KA, Lecates SL, Kabbouche MA, Hershey AD, Powers SW. Childhood abuse in pediatric patients with chronic daily headache. Clin Pediatr. 2012;51:590–593. doi: 10.1177/0009922811407181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zatzick DF, Jurkovich GJ, Fan MY, Grossman D, Russo J, Katon W, Rivara FP. Association between posttraumatic stress and depressive symptoms and functional outcomes in adolescents followed up longitudinally after injury hospitalization. Arch Pediatr Adolesc Med. 2008;162:642–648. doi: 10.1001/archpedi.162.7.642. [DOI] [PubMed] [Google Scholar]


