Abstract
Background:
Patients are often concerned about returning to sports after total hip arthroplasty (THA).
Purpose:
To (1) evaluate sports participation and motivation rates in a large cohort of patients who underwent uncemented THA with ceramic-on-ceramic bearings and (2) determine whether patients’ participation was associated with their motivation for each sport, preoperative demographics, or patient-reported outcomes.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
We surveyed 1310 patients (aged <75 years) who underwent uncemented ceramic-on-ceramic THA and collected levels of motivation and participation for 22 different sports as well as patient-reported outcome measure scores. A total of 1042 patients (1206 hips) returned questionnaires; the mean age at index surgery was 60.6 ± 8.8 years.
Results:
At least 51% of patients participated regularly or frequently in at least 1 light sport, 73% in at least 1 moderate sport, and 20% in at least 1 strenuous sport. Sports participation was strongly correlated with motivation (r = 0.97, P < .001) but not with level of discomfort (r = 0.22, P = .292). Participation in strenuous sports was significantly associated with age, body mass index, and sex. There were significant differences among patients who practiced various categories of sports as determined using the Oxford Hip Score (P = .008), but not with regard to the Forgotten Joint Score (P = .054).
Conclusion:
Only 20% of patients practiced strenuous sports regularly or frequently after THA, regardless of pain or discomfort. Participation in sports after THA is strongly correlated with motivation but not with level of discomfort. Longer term studies with a greater focus on complications and survival are necessary to determine whether high-impact sports compromise patient safety or implant longevity.
Keywords: total hip arthroplasty, THA, uncemented, ceramic-on-ceramic, sports participation, strenuous sports, level of activity
Total hip arthroplasty (THA) has been described as the “procedure of the century,”24 and the number of procedures performed annually is increasing worldwide. Patients undergoing THA are becoming younger and more active,23 with rising expectations with regard to their return to daily activities and sports.2,27
A number of studies reported that 21% to 55% of patients participate in athletic activities after THA,2,12,17,18,22,39 with up to 44% of patients resuming high-impact sports despite discouragement from health care professionals.8,26,34 A frequent question of patients is whether they will be able to practice sports after surgery, and surgeons find it difficult to answer this question because of a lack of large survey studies on unselected patients as well as some concerns regarding adverse effects and implant longevity.8,27,31,38
While some surgeons have affirmed that a gradual return to sports does not compromise implant longevity and could instead prevent or delay revision surgery,14 many surgeons do not recommend high-impact sports that may cause fractures18,20 or excessive polyethylene wear.32,33 The concerns of implant wear would be different, however, for other bearing couples such as ceramic-on-ceramic (CoC) or metal-on-metal (MoM). To our knowledge, only Naal et al28 have investigated sports participation after MoM hip resurfacing arthroplasty and reported high levels of activity within 2 postoperative years. Likewise, only Abe et al1 investigated sports participation after CoC THA, but these authors focused solely on jogging, reporting that the activity has no negative influence on short-term implant survival.
CoC bearings have the advantages of generating little or no debris as well as being inert materials, thereby avoiding the osteolytic reactions observed with polyethylene bearings or the release of potentially harmful metal ions into the surrounding tissues. While still popular in Europe and Asia, CoC bearings are less used in North America7 because of squeaking,11,25 concerns of potential implant fractures,29,30 and higher costs.
Although resuming sports activities may depend on patient demographics and surgeon recommendations, recent studies have reported that, beyond the success of arthroplasty procedures, sports participation depends primarily on patient motivation.5,6,37 The purpose of this study was therefore to (1) evaluate sports participation and motivation rates in a large cohort of patients who underwent uncemented THA with CoC bearings and (2) determine whether patients’ participation in sports was associated with their motivation for the sport, preoperative demographics, or patient-reported outcomes.
Methods
Between January 2010 and December 2013, a total of 1381 patients underwent primary THA using uncemented components with a CoC bearing couple. The patients, all younger than 75 years at index surgery, comprised a consecutive series operated by 7 surgeons at 4 centers using the CORAIL Hip System (DePuy Synthes) and the PINNACLE Acetabular Cup (DePuy Synthes). There were no restrictive recommendations on patients regarding postoperative sports activity. Patients were excluded from the study if they were operated on for rheumatoid arthritis (n = 6; 0.4%) or had undergone previous hip or knee arthroplasty (n = 50; 3.6%). Patients with the following postoperative complications were also excluded: dislocations (n = 6; 0.4%), sepsis (n = 6; 0.5%), and other orthopaedic or neurological conditions of the spine or lower limbs that limited patient mobility (n = 3; 0.2%). The study protocol was approved by an institutional review board.
A total of 1310 patients met the criteria for inclusion in this study and were mailed paper questionnaires that comprised 3 sections. The first section collected patient consent, demographics (age, sex, body mass index, operated side, level of activity, date of surgery, and follow-up) as well as a single question judging their current overall satisfaction (very satisfied, satisfied, somewhat satisfied, disappointed, or dissatisfied) with their operated hip(s). The second section surveyed the patients’ motivation for and participation in 22 different sports, studied using the methodology described by Weiss et al.37 For each sport, patients were asked about the frequency of practices after their THA(s) (rare, occasional, regular, or frequent), motivation for the particular sport (little or none, moderate, high, or very high), level of exercise (none, recreational, or competitive), discomfort while practicing (none, moderate, or severe), and/or reason for not practicing (due to my hip, I do not dare, or other reason). The third section collected the following patient-reported outcome measure (PROM) scores:
Forgotten Joint Score4 on a scale from 0 (worst) to 100 (best);
Oxford Hip Score13 on a scale from 60 (worst) to 12 (best); and
Short Form–12 score,15 in which the Physical Component Summary and Mental Component Summary scores each have a mean of 50 ± 10 in the general population and scores greater than 50 reflect better status.
Using the classification of Weiss et al,37 sports were categorized as either light (indoor cycling, outdoor cycling, fishing, swimming, and golf), moderate (gardening, hiking, gym/fitness, hunting, yoga, tai chi chuan, sailing, and dancing), or strenuous (cross-country skiing, downhill skiing, ski touring, rock climbing, judo/karate, tennis/squash, running more than 500 m, team ball games, and trail/mountain running). For each sport, the patients were considered motivated if the question, “Is this activity important in your life?” was answered with “highly” or “very highly.” The patients were considered to participate in sports if the question, “How often do you do this sport?” was answered “regularly” or “frequently.” Patients were considered motivated by a sports category (light, moderate, or strenuous) if their response was “highly” or “very highly” for at least one of the sports in the given category. Patients were considered to be participating in a sports category if their participation was “regular” or “frequent” in at least one of the sports in the given category. We assumed that unanswered questions regarding a sport meant that the patient was not interested in that sport and was therefore considered not motivated and/or nonparticipating.
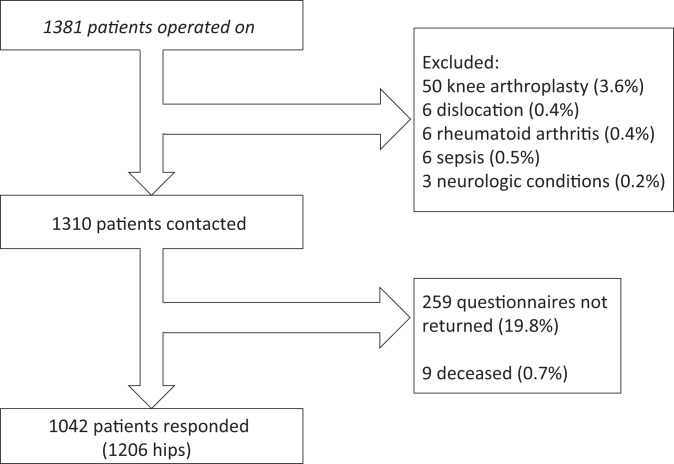
Patients who did not return the questionnaire within 2 months were resent questionnaires by mail. Of the 1310 patients enrolled, 9 (0.7%) had died from causes unrelated to their hip surgery, and 259 (19.8%) did not return the questionnaire after one reminder. Therefore, 1042 patients (1206 hips) responded at a mean follow-up of 44.4 ± 14.0 months (median, 45.0 months; range, 24.0-79.0 months) (Figure 1). The cohort comprised 598 men (699 hips) and 444 women (507 hips), with a mean age of 60.6 ± 8.8 years (median, 62.1 years; range, 18-75 years) at index surgery (Table 1).
Figure 1.
Flowchart indicating numbers of patients (hips) who enrolled, who were excluded, and who responded.
TABLE 1.
Patient Demographicsa
| All (1206 Hips, 1042 Patients) | Unilateral (878 Hips, 878 Patients) | Bilateral (328 Hips, 164 Patients) | |
|---|---|---|---|
| Age at surgery, y | 60.6 ± 8.8 (18.1-75.0) | 60.7 ± 8.6 (18.1-75.0) | 59.6 ± 10.1 (24.6-74.8) |
| Follow-up, mo | 44.4 ± 14.0 (24.0-79.0) | 44.7 ± 14.1 (24.0-79.0) | 42.8 ± 13.6 (24.0-75.0) |
| Body mass index, kg/m2 | 26.6 ± 4.6 (16.6-61.1) | 26.5 ± 4.6 (16.6-61.1) | 27.2 ± 4.7 (17.6-42.2) |
| Male sex, n (%) | 598 (57.4) | 497 (56.6) | 101 (61.6) |
aData are shown as mean ± SD (range) unless otherwise indicated.
Statistical Analysis
Descriptive statistics were used to summarize the data. Normality was tested using the Shapiro-Wilk test. Differences in means between ≥2 groups were respectively tested using the Student t test or analysis of variance. Associations between categorical variables were tested using the chi-square test or Fisher exact test. In case the data were not normally distributed, pairwise comparisons were made using the Mann-Whitney U test and Kruskal-Wallis test. Statistical analyses were performed using R version 3.3.3 (R Foundation). P values <.05 were considered statistically significant.
Results
Of the 1042 patients who responded to the questionnaire, 878 underwent unilateral THA, while 164 underwent bilateral THA. Overall, 92% were satisfied or very satisfied with their operated hip (Table 2), with no significant differences between unilateral and bilateral patients in terms of satisfaction or PROM scores.
TABLE 2.
PROM Scores and Overall Satisfaction at Last Follow-upa
| PROM | All (1206 Hips, 1042 Patients) | Unilateral (878 Hips, 878 Patients) | Bilateral (328 Hips, 164 Patients) |
|---|---|---|---|
| Forgotten Joint Score | 69.2 ± 27.0 (2.1-100.0) | 69.5 ± 27.1 (2.1-100.0) | 68.6 ± 26.5 (2.1-100.0) |
| Oxford Hip Score | 19.8 ± 9.3 (0.0-55.6) | 20.0 ± 9.4 (12.0-54.0) | 19.3 ± 9.0 (12.0-55.6) |
| SF-12 PCS | 50.4 ± 8.4 (11.9-67.3) | 50.4 ± 8.4 (11.9-67.3) | 50.1 ± 8.0 (21.1-64.3) |
| SF-12 MCS | 52.2 ± 10.6 (7.5-79.1) | 52.2 ± 10.6 (7.5-79.1) | 52.4 ± 10.6 (12.2-66.6) |
| Overall satisfaction, n (%) | |||
| Very satisfied | 812 (67.3) | 591 (67.3) | 221 (67.4) |
| Satisfied | 301 (25.0) | 217 (24.7) | 84 (25.6) |
| Somewhat satisfied | 66 (5.5) | 48 (5.5) | 18 (5.5) |
| Disappointed | 8 (0.7) | 8 (0.9) | 0 (0.0) |
| Dissatisfied | 3 (0.2) | 2 (0.2) | 1 (0.3) |
| Did not respond | 16 (1.3) | 12 (1.4) | 4 (1.2) |
aData are shown as mean ± SD (range) unless otherwise indicated. There were no statistically significant differences in any of the PROM scores between unilateral and bilateral patients; likewise, there were no statistically significant differences in level of satisfaction (including nonrespondents) between unilateral and bilateral patients. MCS, Mental Component Summary; PCS, Physical Component Summary; PROM, patient-reported outcome measure; SF-12, Short Form–12.
Regarding patients’ participation in each sports category, 532 (51%) responded that they participated regularly or frequently in at least 1 light sport, 745 (71%) participated in at least 1 moderate sport, and 207 (20%) participated in at least 1 strenuous sport (Table 3). Only 27 (2.6%) patients practiced ≥1 sports at the competitive level, while 93 (9%) patients did not practice any sports. Regarding patients’ motivation in each sports category, 478 (46%) responded that they were highly or very highly motivated by at least 1 light sport, 668 (64%) by at least 1 moderate sport, and 271 (26%) by at least 1 strenuous sport. Only 66 (6%) patients were not motivated by any sport.
TABLE 3.
Regular or Frequent Participation in Different Sports Categoriesa
| All (N = 1042) | Unilateral (n = 878) | Bilateral (n = 164) | |
|---|---|---|---|
| At least 1 light sport | 532 (51.1) | 448 (51.0) | 84 (51.2) |
| At least 1 moderate sport | 745 (72.7) | 622 (72.3) | 123 (75.0) |
| At least 1 strenuous sport | 207 (19.9) | 173 (19.7) | 34 (20.7) |
aData are shown as n (%).
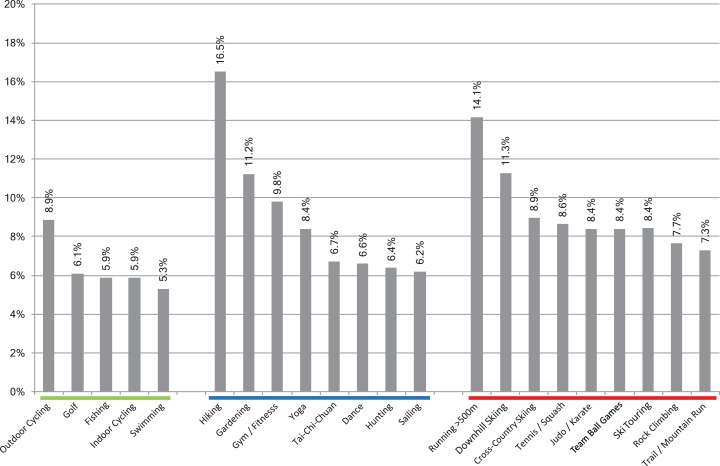
Sports participation was strongly correlated with motivation (r = 0.97, P < .001) (Figure 2). The proportion of patients who were able to practice the sports for which they were motivated was greater for light (88%-100%) and moderate (56%-100%) sports than for strenuous sports (47%-79%). The most popular strenuous sports were downhill skiing and running. Among the 152 patients highly or very highly motivated by downhill skiing, 118 (78%) practiced it regularly/frequently, while among the 58 patients highly or very highly motivated by running, 46 (79%) practiced it regularly/frequently. There were no significant differences in sports participation rates between patients who underwent unilateral versus bilateral THA (Table 3).
Figure 2.
Proportions of patients who were highly or very highly motivated by each sport and patients who participated regularly or frequently in each sport. Green, light sports; blue, moderate sports; red, strenuous sports.
A small proportion of patients responded that they did not practice specific sports because of their operated hip: 5% to 9% for light sports, 6% to 17% for moderate sports, and 7% to 14% for strenuous sports (Figure 3). A smaller proportion of patients reported severe discomfort from their operated hip while practicing sports, particularly running and team ball games: 1% to 5% for light sports, 5% to 8% for moderate sports, and 8% to 18% for strenuous sports (Figure 4). Sports participation was not correlated with level of discomfort (r = 0.22, P = .292). There were significant differences among patients who practiced various categories of sports in terms of the Oxford Hip Score (P = .008) but not in terms of the Forgotten Joint Score (P = .054) (Figure 5).
Figure 3.
Proportion of patients who did not practice sports because of their operated hip. Green, light sports; blue, moderate sports; red, strenuous sports.
Figure 4.
Proportion of patients who reported discomfort during different sports activities. Light gray, no discomfort; medium gray, moderate discomfort; dark gray, severe discomfort. Green, light sports; blue, moderate sports; red, strenuous sports.
Figure 5.
Boxplots of the Oxford Hip Score and Forgotten Joint Score for (1) patients who did not practiced any sport regularly or frequently, (2) patients who practiced regularly or frequently at least 1 light sport but no moderate or strenuous sports, (3) patients who practiced regularly or frequently at least 1 moderate sport but no strenuous sports, and (4) patients who practiced regularly or frequently at least 1 strenuous sport. Only significant pairwise differences are indicated.
Discussion
The literature is divided on whether physical activity increases after THA because of less pain and better mobility28,36 or if it decreases because of aging and fear of damaging the “artificial joint.”10,20,31,39 Several studies have reported high levels of sports participation in patients after THA,2,17,18,39 with some patients resuming high-impact sports such as running, football, or martial arts despite discouragement from health care professionals.26,34 However, most of these studies focused on selected populations of athletes and therefore do not represent the wider population of patients undergoing THA. Patients frequently ask their surgeons while discussing the possibility of THA whether they will be able to practice sports afterward, and surgeons are often reluctant to respond because of the lack of studies reporting actual sports participation rates in large nonselected THA cohorts and demonstrating patient safety and implant longevity.27,31,38
The purpose of this study was to (1) evaluate sports participation and motivation rates in a large cohort of patients who underwent uncemented THA with CoC bearings and (2) determine whether patients’ participation was associated with their motivation for each sport, preoperative demographics, or patient-reported outcomes. The principal findings of this study were that a high proportion of motivated patients practiced strenuous sports regularly or frequently after THA but that a small proportion of patients were unwilling to practice strenuous sports because of their operated hip (7%-14%). The study also revealed that some patients reported pain or discomfort while practicing certain sports, but this did not affect their frequency of participation.
While some surgeons have affirmed that a gradual return to sports does not compromise implant longevity and could in fact prevent or delay revision surgery,14 many surgeons still discourage patients from high-impact sports that expose the bearing surfaces to higher loads,33 which could thereby cause excessive wear32 or fractures.18,20 Our survey was not designed to investigate whether strenuous sports after THA are dangerous for the implant but only to describe sports participation in a nonselected population.
Although only 20% of all patients participated regularly or frequently in at least 1 strenuous sport, this represented 76% of patients motivated to play such sports. Only 5% to 17% of our respondents did not practice sports because of their operated hip. The 2 sports that patients were most discouraged by were running and hiking, both of which exert high impact on the lower limbs. Our questionnaire did not differentiate whether nonparticipation was attributable to pain/discomfort during a given activity or simply to fear of damaging the artificial hip, although patients received no restrictive recommendations from their surgeons regarding sports activities after their surgery. The absence of a correlation between the frequency of participation and level of discomfort at the hip joint while practicing sports supports the second hypothesis that sports participation is not limited by THA in motivated patients. The causes of pain or discomfort while practicing sports after THA have not been investigated so far. Our study was not designed to investigate this particular issue, which is likely multifactorial. The first factor could be lack of practice during the years preceding surgery35,38 or insufficient time for recovery after surgery.19 The second factor could be related to the surgical procedure, including sequelae of tissue aggression, stiffness, or lack of anatomic restoration.3,9 The third factor may be the hardness of the bearing couple, which exacerbates stresses transmitted to the femur,16 even if thigh pain is rarely reported with the stem used.21
The strengths of this study were that it specifically analyzed sports participation in a consecutive nonselected population after THA with a single implant and bearing couple and with a special interest in the subgroup of motivated patients. Its main limitations are that it was a retrospective investigation with limited follow-up on prospectively followed patients and that only 80% of the patients returned their questionnaires. Moreover, while our analyses considered the frequency of sports participation, they did not account for the level of sports practice. However, objective quantification of the sports level could have been possible only for patients practicing sports at the competitive level, which represented a minority (2.6%). Furthermore, our study did not include radiographic analyses or assessments of range of motion and did not investigate general or sports-related complications. Finally, it is important to note that some of our observations may have been related to the mountainous region where the study was performed, in which skiing and hiking are considered social activities, rather than physical exercise per se.
Conclusion
Our results demonstrate that 20% of motivated patients practice strenuous sports regularly or frequently after THA. Sports participation is related to motivation but is not related to pain or discomfort. Longer term studies are required to confirm that high-impact sports do not compromise patient safety and implant longevity.
Acknowledgment
The authors are grateful to Mr Luca Nover, Mr Hugo Bothorel, and Mr Ryan J. Reynolds for their assistance with data processing, statistical analyses, and article finalization.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: M.P.B., J-C.R., J-C.C., T.A-S-S., and L.J. have received educational funding and royalties from DePuy Synthes. J.C. has received educational funding from DePuy Synthes. M-H.F. has received educational funding from DePuy Synthes; receives royalties from DePuy Synthes and SERF; and receives consulting fees from SERF, Zimmer, and Biomet. M.S. receives consulting fees for statistical analyses and article preparation from Artro Group Institute.
Ethical approval for this study was obtained from the Centre Orthopédique Santy, Lyon, France (#2016-21).
References
- 1. Abe H, Sakai T, Nishii T, Takao M, Nakamura N, Sugano N. Jogging after total hip arthroplasty. Am J Sports Med. 2014;42(1):131–137. [DOI] [PubMed] [Google Scholar]
- 2. Arnold JB, Walters JL, Ferrar KE. Does physical activity increase after total hip or knee arthroplasty for osteoarthritis? A systematic review. J Orthop Sports Phys Ther. 2016;46(6):431–442. [DOI] [PubMed] [Google Scholar]
- 3. Asayama I, Chamnongkich S, Simpson KJ, Kinsey TL, Mahoney OM. Reconstructed hip joint position and abductor muscle strength after total hip arthroplasty. J Arthroplasty. 2005;20(4):414–420. [DOI] [PubMed] [Google Scholar]
- 4. Behrend H, Giesinger K, Giesinger JM, Kuster MS. The “forgotten joint” as the ultimate goal in joint arthroplasty: validation of a new patient-reported outcome measure. J Arthroplasty. 2012;27(3):430–436.e1. [DOI] [PubMed] [Google Scholar]
- 5. Bonnin M, Laurent JR, Parratte S, Zadegan F, Badet R, Bissery A. Can patients really do sport after TKA? Knee Surg Sports Traumatol Arthrosc. 2010;18(7):853–862. [DOI] [PubMed] [Google Scholar]
- 6. Bonnin MP, Laurent JR, Zadegan F, Badet R, Pooler Archbold HA, Servien E. Can patients really participate in sport after high tibial osteotomy? Knee Surg Sports Traumatol Arthrosc. 2013;21(1):64–73. [DOI] [PubMed] [Google Scholar]
- 7. Bozic KJ, Kurtz S, Lau E, et al. The epidemiology of bearing surface usage in total hip arthroplasty in the United States. J Bone Joint Surg Am. 2009;91(7):1614–1620. [DOI] [PubMed] [Google Scholar]
- 8. Bradley BM, Moul SJ, Doyle FJ, Wilson MJ. Return to sporting activity after total hip arthroplasty: a survey of members of the British Hip Society. J Arthroplasty. 2017;32(3):898–902. [DOI] [PubMed] [Google Scholar]
- 9. Chamnongkich S, Asayama I, Kinsey TL, Mahoney OM, Simpson KJ. Difference in hip prosthesis femoral offset affects hip abductor strength and gait characteristics during obstacle crossing. Orthop Clin North Am. 2012;43(5):e48–e58. [DOI] [PubMed] [Google Scholar]
- 10. Chatterji U, Ashworth MJ, Lewis PL, Dobson PJ. Effect of total hip arthroplasty on recreational and sporting activity. ANZ J Surg. 2004;74(6):446–449. [DOI] [PubMed] [Google Scholar]
- 11. Chevillotte C, Pibarot V, Carret JP, Bejui-Hugues J, Guyen O. Hip squeaking: a 10-year follow-up study. J Arthroplasty. 2012;27(6):1008–1013. [DOI] [PubMed] [Google Scholar]
- 12. Del Piccolo N, Carubbi C, Mazzotta A, et al. Return to sports activity with short stems or standard stems in total hip arthroplasty in patients less than 50 years old. Hip Int. 2016;26(suppl 1):48–51. [DOI] [PubMed] [Google Scholar]
- 13. Delaunay C, Epinette JA, Dawson J, Murray D, Jolles BM. Cross-cultural adaptations of the Oxford-12 HIP score to the French speaking population. Orthop Traumatol Surg Res. 2009;95(2):89–99. [DOI] [PubMed] [Google Scholar]
- 14. Dubs L, Gschwend N, Munzinger U. Sport after total hip arthroplasty. Arch Orthop Trauma Surg. 1983;101(3):161–169. [DOI] [PubMed] [Google Scholar]
- 15. Gandek B, Ware JE, Aaronson NK, et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51(11):1171–1178. [DOI] [PubMed] [Google Scholar]
- 16. Girard J, Miletic B, Deny A, Migaud H, Fouilleron N. Can patients return to high-impact physical activities after hip resurfacing? A prospective study. Int Orthop. 2013;37(6):1019–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Healy WL, Iorio R, Lemos MJ. Athletic activity after joint replacement. Am J Sports Med. 2001;29(3):377–388. [DOI] [PubMed] [Google Scholar]
- 18. Healy WL, Sharma S, Schwartz B, Iorio R. Athletic activity after total joint arthroplasty. J Bone Joint Surg Am. 2008;90(10):2245–2252. [DOI] [PubMed] [Google Scholar]
- 19. Horstmann T, Vornholt-Koch S, Brauner T, Grau S, Mundermann A. Impact of total hip arthroplasty on pain, walking ability, and cardiovascular fitness. J Orthop Res. 2012;30(12):2025–2030. [DOI] [PubMed] [Google Scholar]
- 20. Huch K, Muller KA, Sturmer T, Brenner H, Puhl W, Gunther KP. Sports activities 5 years after total knee or hip arthroplasty: the Ulm Osteoarthritis Study. Ann Rheum Dis. 2005;64(12):1715–1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jacquot L, Bonnin MP, Machenaud A, Chouteau J, Saffarini M, Vidalain JP. Clinical and radiographic outcomes at 25-30 years of a hip stem fully coated with hydroxylapatite. J Arthroplasty. 2018;33(2):482–490. [DOI] [PubMed] [Google Scholar]
- 22. Karampinas PK, Papadelis EG, Vlamis JA, Basiliadis H, Pneumaticos SG. Comparing return to sport activities after short metaphyseal femoral arthroplasty with resurfacing and big femoral head arthroplasties. Eur J Orthop Surg Traumatol. 2017;27(5):617–622. [DOI] [PubMed] [Google Scholar]
- 23. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–785. [DOI] [PubMed] [Google Scholar]
- 24. Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370(9597):1508–1519. [DOI] [PubMed] [Google Scholar]
- 25. Mai K, Verioti C, Ezzet KA, Copp SN, Walker RH, Colwell CW., Jr Incidence of ‘squeaking’ after ceramic-on-ceramic total hip arthroplasty. Clin Orthop Relat Res. 2010;468(2):413–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Massin P, Schmidt L, Engh CA. Evaluation of cementless acetabular component migration: an experimental study. J Arthroplasty. 1989;4(3):245–251. [DOI] [PubMed] [Google Scholar]
- 27. Meira EP, Zeni J., Jr Sports participation following total hip arthroplasty. Int J Sports Phys Ther. 2014;9(6):839–850. [PMC free article] [PubMed] [Google Scholar]
- 28. Naal FD, Maffiuletti NA, Munzinger U, Hersche O. Sports after hip resurfacing arthroplasty. Am J Sports Med. 2007;35(5):705–711. [DOI] [PubMed] [Google Scholar]
- 29. Park KS, Seon JK, Yoon TR. The survival analysis in third-generation ceramic-on-ceramic total hip arthroplasty. J Arthroplasty. 2015;30(11):1976–1980. [DOI] [PubMed] [Google Scholar]
- 30. Porat M, Parvizi J, Sharkey PF, Berend KR, Lombardi AV, Jr, Barrack RL. Causes of failure of ceramic-on-ceramic and metal-on-metal hip arthroplasties. Clin Orthop Relat Res. 2012;470(2):382–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ritter MA, Meding JB. Total hip arthroplasty: can the patient play sports again? Orthopedics. 1987;10(10):1447–1452. [DOI] [PubMed] [Google Scholar]
- 32. Schmalzried TP, Shepherd EF, Dorey FJ, et al. The John Charnley Award: wear is a function of use, not time. Clin Orthop Relat Res. 2000;(381):36–46. [DOI] [PubMed] [Google Scholar]
- 33. Sechriest VF, 2nd, Kyle RF, Marek DJ, Spates JD, Saleh KJ, Kuskowski M. Activity level in young patients with primary total hip arthroplasty: a 5-year minimum follow-up. J Arthroplasty. 2007;22(1):39–47. [DOI] [PubMed] [Google Scholar]
- 34. Seyler TM, Mont MA, Ragland PS, Kachwala MM, Delanois RE. Sports activity after total hip and knee arthroplasty: specific recommendations concerning tennis. Sports Med. 2006;36(7):571–583. [DOI] [PubMed] [Google Scholar]
- 35. Tuominen U, Sintonen H, Hirvonen J, et al. The effect of waiting time on health and quality of life outcomes and costs of medication in hip replacement patients: a randomized clinical trial. Osteoarthritis Cartilage. 2009;17(9):1144–1150. [DOI] [PubMed] [Google Scholar]
- 36. Visuri T, Honkanen R. The influence of total hip replacement on selected activities of daily living and on the use of domestic aid. Scand J Rehabil Med. 1978;10(4):221–225. [PubMed] [Google Scholar]
- 37. Weiss JM, Noble PC, Conditt MA, et al. What functional activities are important to patients with knee replacements? Clin Orthop Relat Res. 2002;(404):172–188. [DOI] [PubMed] [Google Scholar]
- 38. Williams DH, Greidanus NV, Masri BA, Duncan CP, Garbuz DS. Predictors of participation in sports after hip and knee arthroplasty. Clin Orthop Relat Res. 2012;470(2):555–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wylde V, Blom A, Dieppe P, Hewlett S, Learmonth I. Return to sport after joint replacement. J Bone Joint Surg Br. 2008;90(7):920–923. [DOI] [PubMed] [Google Scholar]