Abstract
Objective
This study aims to assess the current antipsychotic prescribing trends for the treatment of schizophrenia and to compare them with available guidelines and research evidence.
Design
An observational retrospective quantitative analysis.
Setting
Data were collected from the prescribing cost analysis for the period between 2007 and 2014, including all drugs from the British National Formulary 4.2.1 and 4.2.2. Prescriptions were included from primary and secondary healthcare settings in England and Wales.
Participants
None.
Main outcome measures
Defined daily doses of antipsychotics were used to compare popularity of individual drugs and classes of antipsychotics.
Results
There is a consistent increase in the proportion of atypical antipsychotics prescribed, compared to typical antipsychotics, between 2007 and 2014, with atypicals accounting for 79.9% of total antipsychotics prescribed in 2014.
Conclusion
The consistent popularity of atypical antipsychotics is not concordant with the current National Institute for Health and Care Excellence guidelines for the treatment of schizophrenia or the most recent research evidence.
Keywords: Psychotic disorders, guidelines, medicines regulation, changing physician behaviour
Introduction
Schizophrenia is a severe, chronic mental disorder with a worldwide global risk of 0.72%.1 Clinical presentation and response to medication are extremely varied, which can mean it is very difficult to decide what treatment to offer.
Treatment of schizophrenia focuses on the use of antipsychotics. Generally, these are categorised into two groups: typical or first-generation antipsychotics and atypical or second-generation antipsychotics. Both act on dopamine receptors, in particular D2, which accounts for their antipsychotic effects.2,3
Typical antipsychotics are less selective in their site of action than atypical antipsychotics. As a result, some may worsen negative symptoms (due to their action in the mesocortical pathway) and can produce unwanted extrapyramidal side effects, such as acute dystonias, tardive dyskinesia and parkinsonian symptoms (due to their action in the nigrostriatal pathway).4
Typical and atypical antipsychotics differ in their pharmaceutical properties, the effect they have on the symptoms and their side-effect profile. Although atypical antipsychotics also block D2 receptors, it is thought that they dissociate more quickly than typicals. Some have additional action at serotonin receptors – there is evidence that this leads to a reduction in the number and severity of extrapyramidal side effects experienced by patients.4 They do, however, cause other adverse reactions, which can be just as severe and debilitating, including metabolic syndrome.5 Clozapine is known to be associated with agranulocytosis; for this reason, clozapine is only considered as a third-line treatment for patients with refractory schizophrenia. Any patient who is prescribed clozapine must be closely monitored with regular blood counts.6
Certain drugs from either class of antipsychotics can be associated with sexual dysfunction and hyperprolactinaemia; however, the effect depends on the individual drug and the dose used.7,8
The first National Institute for Health and Care Excellence guidelines published (2002) focused on the treatment of schizophrenia and advised that, in the case of first presentation schizophrenia, first-line treatment should be an atypical antipsychotic (specifically amisulpride, olanzapine, quetiapine, risperidone and zotepine). They state that when the treatment options cannot be discussed, such as in the case of an acute schizophrenic episode, atypicals should be used due to their lower risk of extrapyramidal side effects.9
However, after publication of these guidelines, the research used in their production was re-assessed and found to be flawed. This initiated further investigation into the efficacy and side-effect profile of typical versus atypical antipsychotics, which yielded findings contrary to the guidance published by the National Institute for Health and Care Excellence.
This research includes the Clinical Antipsychotic Trials of Intervention Effectiveness, a quantitative study by Lieberman and Stroup, which investigated the effectiveness of atypical antipsychotics in comparison to typical antipsychotics, used in the treatment of schizophrenic patients.10 Jones et al. conducted a randomised control trial (known as CUtLASS 1) with the objective of finding out whether the extra cost of atypical antipsychotics is accounted for by improvements in quality of life or reduced costs in other health and social care services.11 While this trial rejected their hypothesis that atypicals are superior to typicals, the question remains whether some individual atypical antipsychotics are more advantageous. Geddes et al.12 produced a meta-analysis investigating the effect of certain antipsychotics on symptom control and their overall acceptability to patients. An important result of this study is the affirmation that using typical antipsychotic drugs at high doses does not improve their efficacy but increases side effects experienced.12 The use of typical antipsychotics at high doses may account for the initial misleading evidence.
The result was that, in 2009, the National Institute for Health and Care Excellence guidelines were changed so that the advice was simply, ‘for people with newly diagnosed schizophrenia, offer oral antipsychotic medication. Provide information and discuss the benefits and side effect profile of each drug with the service user’. The same advice is given for acute episodes of schizophrenia, and there is no clearly stated preference for atypical over typical antipsychotics.13
Although there has been some research investigating antipsychotic prescribing trends following the 2002 guidelines, there are few studies which look at trends following the changes to the guidelines in 2009. Verdoux et al.14 looked at published studies between 2000 and 2008 which analysed antipsychotic prescribing in the general population. They concluded that overall antipsychotic prescribing has increased. This increase was most commonly related to an increase in atypical antipsychotics. Some of the included studies reported up to an 89% increase in atypical antipsychotic prescribing.
This paper aims to assess more recent prescribing trends in order to find out whether clinical practice has changed in response to evolving research and guidance.
Methods
This analysis was carried out using data collected from the prescribing cost analysis for antipsychotic drugs included in the British National Formulary 4.2.1 and 4.2.2.15 Included were all prescriptions between 2006 and 2014 in England and Wales. These data were presented as the number of defined daily doses, rather than items prescribed.
The World Health Organisation defines a daily dose as, ‘The defined daily dose is the assumed average maintenance dose per day for a drug used for its main indication in adults’.16 The defined daily dose does not always match the prescribed or recommended daily dose. The defined daily dose for individual patients will be different, as it should be based on individual patients and pharmacokinetics.
These data were presented using defined daily doses as it can give an estimate of drug consumption. In this study, an estimate can be used and not exact quantities as it is comparing trends over a period of time involving a large quantity of drugs.
There are limitations to using this format of data because there are alternative uses for some of the antipsychotics including the treatment of agitation in dementia and mood disorders. To mitigate for this confounding factor, British National Formulary 4.2.1 and 4.2.2 were consulted and 26 antipsychotics preparations were eliminated which are unlikely to be used in schizophrenia, either due to the dose prescribed or the preparation used. To ascertain this, the British National Formulary, medicines.com and clinical experience from practitioners was used. The preparations removed were all prescribed at a low frequency, suggesting that they are not used commonly in mainstream practice.
Data from March 2007 to December 2014 were quantitatively analysed, comparing the frequency and distribution of antipsychotic prescribing over time. A comparison was made using Excel software between the prescribing percentages of typical versus atypical antipsychotics by dividing them into two broad groups. In addition, individual drugs were analysed in greater depth. The typical antipsychotics selected were perpehenazine, chlorpromazine, haloperidol, zuclopenthixol, flupenthixol and sulpiride. The atypicals selected were olanzapine, quetiapine, risperidone, amisulpride, zotepine and clozapine. This selection was based on antipsychotics that are most commonly prescribed and those included in the most recent research including the CATIE and CUtLASS trials. They included liquid form, depot preparation and tablets.
Results
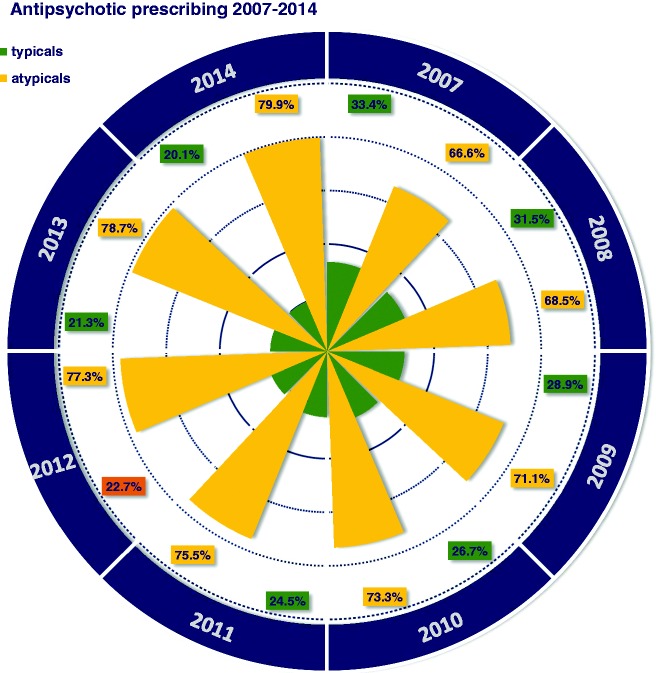
There has been a consistent yearly change in the proportion of typical versus atypical antipsychotics, a year on year increase in atypicals, culminating in an end of study period high of 79.9% of total antipsychotics prescribed (Figure 1).
Figure 1.
Radar graph showing the general trend in atypical vs. typical antipsychotic prescribing between 2007 and 2014.
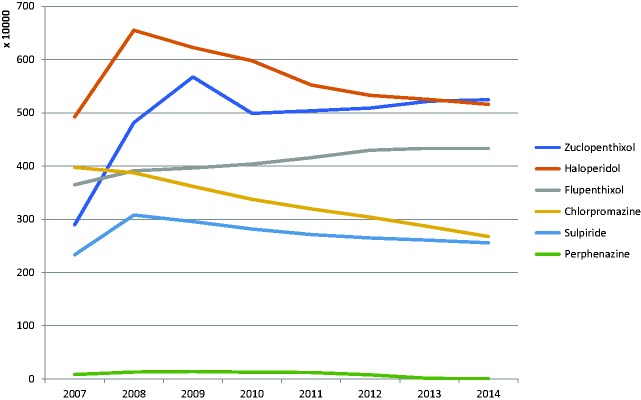
Despite an early increase in some of the individual typical antipsychotics, there is a general downwards trend. The largest decrease can be seen with chloropromazine; however, there is a general increase in zuclopenthixol and flupenthixol. At the end of the study period, zuclopenthixol is the most popular typical, with 5,244,935 defined daily doses being prescribed in 2014 (Figure 2).
Figure 2.
Line graph showing the changes in typical antipsychotic prescribing between 2007 and 2014.
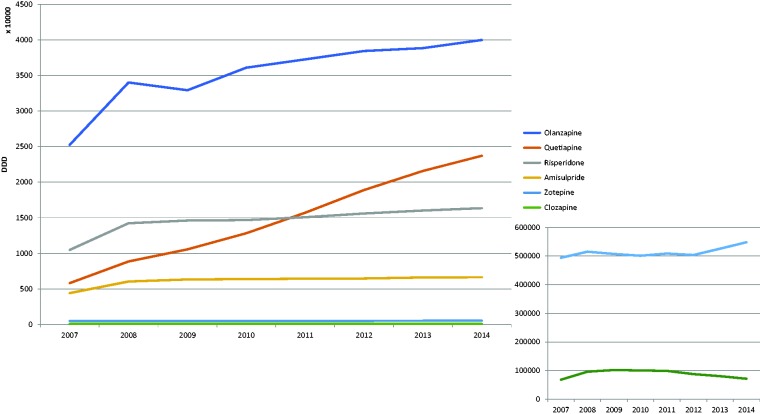
Figure 3 shows the changes in atypical antipsychotic prescribing. These charts correspond with the trend seen in Figure 1 in that all of the atypical antipsychotics increase during the study period. The largest increase is seen with quetiapine; the defined daily doses of quetiapine increased by 17,900,716 between 2007 and 2014. With regard to clozapine, there is a small increase in the defined daily doses prescribed over the study period of 3454.
Figure 3.
Line graph showing the changes in atypical antipsychotic prescribing between 2007 and 2014, with the changes in clozapine and zotepine highlighted.
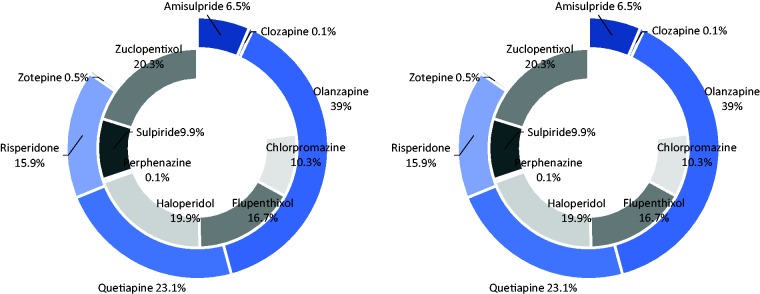
When comparing the most commonly prescribed typical and atypical antipsychotics in 2007 and 2014 (Table 1), it is clear that the drugs most popular at the start of the study period have become more frequently prescribed as compared to other antipsychotics, which are represented by the blank portion of the graph. Despite the strong evidence for the high efficacy of clozapine, this drug only makes up 0.1% of the atypical antipsychotics both in 2007 and 2014. The greatest increases in the proportion of typical and atypical prescriptions are seen in zuclopentixol and quetiapine, respectively; however there are no dramatic reductions in any of the individual antipsychotics which suggest they these increases are replacing other, less frequently prescribed antipsychotics (Figure 4).
Table 1.
Defined daily dose of selected antipsychotics rounded to the nearest decimal place.
| Antipsychotics | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 |
|---|---|---|---|---|---|---|---|---|
| Zuclopenthixol | 2,896,307 | 4,814,550 | 5,671,732 | 4,987,741 | 5,036,666 | 5,088,718 | 5,216,819 | 5,244,936 |
| Haloperidol | 4,922,344 | 6,549,801 | 6,225,268 | 5,977,327 | 5,521,783 | 5,327,450 | 5,249,117 | 5,157,594 |
| Flupenthixol | 3,647,639 | 3,908,568 | 3,962,958 | 4,036,929 | 4,156,676 | 4,296,018 | 4,334,184 | 4,328,550 |
| Chlorpromazine | 3,973,965 | 3,872,806 | 3,617,034 | 3,373,057 | 3,194,222 | 3,037,586 | 2,861,237 | 2,675,197 |
| Sulpiride | 2,331,210 | 3,078,441 | 2,956,614 | 2,815,235 | 2,712,167 | 2,647,792 | 2,606,160 | 2,555,799 |
| Perphenazine | 82,624 | 129,319 | 139,835 | 127,286 | 120,206 | 76,866 | 10,976 | 5000 |
| Olanzapine | 25,258,798 | 34,018,851 | 32,932,892 | 36,100,730 | 37,268,466 | 38,447,751 | 38,853,086 | 39,993,225 |
| Quetiapine | 5,816,796 | 8,865,783 | 10,559,849 | 12,829,882 | 15,717,863 | 18,900,611 | 21,582,519 | 23,717,512 |
| Risperidone | 10,479,452 | 14,238,391 | 14,617,122 | 14,681,499 | 15,081,681 | 15,607,863 | 16,020,777 | 16,360,724 |
| Amisulpride | 4,412,009 | 6,048,136 | 6,329,566 | 6,380,441 | 6,430,853 | 6,468,062 | 6,615,597 | 6,651,805 |
| Zotepine | 493,960 | 515,083 | 507,300 | 500,946 | 508,746 | 503,550 | 525,658 | 548,105 |
| Clozapine | 68,126 | 96,117 | 102,037 | 100,516 | 98,953 | 87,816 | 80,551 | 71,581 |
Figure 4.
Donut chart showing the proportion of prescription of six typical and six atypical antipsychotics; 2007 is on the left and 2014 is on the right.
Discussion
These results highlight important aspects relating to guideline implementation and knowledge translation. The increasing trend in atypical antipsychotics can be seen in Figure 1 and continues following the introduction of the 2009 the National Institute for Health and Care Excellence guidelines, despite the change in recommendations.
One limitation of this study is the inability to definitively say which medication was used to treat schizophrenia and what was used in other situations. This means that the trends identified may not be due to changes in antipsychotic prescribing in schizophrenia. While the authors have done their best to ensure the removal of doses that are unlikely to be prescribed for schizophrenia, dose titration or treatment augmentation must be considered. For example, augmentation can be used to reduce side effects as in the case of aripiprazole where mixed therapy helps to control the dysregulation of prolactin levels.
While a strength of this study is the large amount of data collected, there is no accounting for variation between data centres. In a previous study, a large variation was seen between medical centres. The study found that medical centres with fewer patients with severe mental illness had higher rates of polypharmacy. This suggests that clinician experience has a link with adherence to clinical guidelines, particularly in the cases of severe mental illness.17
An important part of the guidelines is the gold standard use of clozapine in treatment-resistant schizophrenia. Between 2008 and 2014, there was only a small increase in the frequency of clozapine prescriptions (Figure 3). This smaller than expected increase could be due to a delay in clozapine use.
This delay has been identified in other research, where clozapine use is preceded by antipsychotic polypharmacy.17 The reduction in clozapine could be an effect of increased patient awareness and clinician apprehension of potentially fatal agranulocytosis and the need for increased rigorous monitoring. Additionally, the last few years have seen the widespread introduction of new atypicals such as depot paliperidone and lurasidone, which provides more options to prescribers who may favour these medicines to clozapine.
The dramatic rise in quetiapine prescriptions may be due to its increased use for the treatment of mood disorders, rather than schizophrenia. Its increased use is unlikely to be due to treatment of schizophrenia due to its reduced clinical efficacy compared to other antipsychotic agents.18
Olanzapine is associated with the greatest weight gain and most severe metabolic side effects. Due to this effect, Schizophrenia Patient Outcome Research Team suggests that olanzapine should not be used as first-line treatment unless it gives significant therapeutic benefits.19 Despite such guidance, olanzapine is the most dominant antipsychotic and it continues to show a consistent increase. This may be due to the recent introduction of depot preparations or the introduction of local policies, which have improved metabolic monitoring. This improvement may have led to an increased confidence in the ability to safely prescribe olanzapine and manage the associated side effects. Despite improvements, the increase seen with olanzapine remains a worrying trend as during the last years there has been a rise in the mortality risk associated with schizophrenia. While the increase in mortality can partly be accounted for by suicide metabolic syndrome is associated with a two-fold increase in mortality.1 Future research may be aimed at investigating whether the increased use of olanzapine is affecting the mortality risk associated with schizophrenia.
The above increase in the prescribing of atypical antipsychotics appears to be matched by a decrease in typical antipsychotic prescribing. The biggest reduction can be seen in the prescribing of haloperidol, while zuclopenthixol appears to go against the trend and increases. Haloperidol is associated with high rates of extrapyramidal side effects.19 The reduction in haloperidol use could be accounted for by increased patient awareness of these side effects and their refusal to accept treatment with these risks. Due to the increasing trend towards using atypical antipsychotics there will be a reduced level of experience with typical antipsychotics. Reduced clinical experience with typical antipsychotics will likely mean that clinicians are not as comfortable using these drugs, advocating their use or treating the side effects. This will contribute towards a continued decreasing use of typical antipsychotics. The increasing use of zuclopenthixol is likely due to the fact that it has replaced some discontinued drugs during the study period. The significant increase in the use of this drug in particular may be due to the inclusion of depot injections.
A meta-analysis conducted by Leucht et al.18 compared the efficacy and side-effect profile of typical and atypical antipsychotics with a placebo. Large differences were found in terms of side effects; in concordance with previous research, olanzapine produced greatest weight gain and haloperidol the greatest extrapyramidal side effects. Smaller differences were seen when comparing efficacy, with clozapine being the most effective drug. The authors suggest that if antipsychotics were organised into a hierarchy within different domains, rather than categorised into two groups, clinicians would be able to provide more individualised treatment for each patient.16
Many healthcare professionals who work within the field of mental health use the Maudsley guidelines.13 Within this speciality, there may be a heavier reliance on these guidelines compared to National Institute for Health and Care Excellence guidelines. Previous Maudsley guidelines specifically advocated the use of an atypical antipsychotic in first-episode schizophrenia. However, more recent guidelines agree with the National Institute for Health and Care Excellence guidance and they highlight that different people respond differently to different treatments, and that individual drugs have certain benefits. The previous conflicting information between guidelines may have led to a degree of uncertainty for practitioners.
However, while there may have been previously conflicting guidelines, it is important that practitioners stay up-to-date and rely on other forms of evidence including randomised control trial data and reviews. Certain patients may benefit more from typical antipsychotics; therefore, it is important that their use is not ruled out by clinicians who are not aware of the current evidence. The prescribing data seen in this study suggest that this evidence is not being translated into current practice.
It has been recognised that there are four types of evidence that contribute to care. These are: research, clinical experience, patient experience and local information.20 One study found that GP practices that ranked highly in terms of prescribing quality were those in which doctors made both macro and micro decisions.21
Macro decisions are governed by policy and allow decisions to be research based and consistent. Micro decisions, however, are based on individual patient characteristics. It is suggested that micro decisions, and therefore individual patient prescribing, must be guided by macro decisions to ensure evidence-based prescribing.21 Local practices and policies are therefore important in guiding prescribing decisions including input from specialist pharmacists or practice formularies.
The results of this study confirm the hypothesis that there has been no change in the frequency of prescriptions of typical or atypical antipsychotic drugs following changes to National Institute for Health and Care Excellence guidelines. Furthermore, it offers insight into why clinical practice does not seem to reflect the available research evidence in terms of treating schizophrenia.
To assess the importance of clinical experience in prescribing behaviour, a follow-up thematic analysis study could establish additional factors influencing clinicians’ prescribing.
Declarations
Competing Interests
None declared.
Funding
None declared.
Ethics approval
Ethical approval was not required as the study used anonymised data collected from an open source.
Guarantor
AN.
Contributorship
RR conducted the data collection. RR, CL and AN contributed equally to the writing of the manuscript. AK provided clinical perspective.
Provenance
Not commissioned; peer-reviewed by Dieneke Hubbeling.
References
- 1.McGrath J, Saha S, Chant D, Welham J. Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol Rev 2008; 30: 67–76. [DOI] [PubMed] [Google Scholar]
- 2.Mackin PT, Thomas SHL. Atypical antipsychotic drugs. BMJ 2011; 342. [DOI] [PubMed] [Google Scholar]
- 3.Seeman P. Atypical antipsychotics: mechanism of action. Can J Psychiatry 2002; 47: 27–38. [PubMed] [Google Scholar]
- 4.Miyamoto S, Miyake N, Jarskog LF, Fleischhacker WW, Lieberman JA. Pharmacological treatment of schizophrenia: a critical review of the pharmacology and clinical effects of current and future therapeutic agents. Mol Psychiatry 2012; 17: 1206–1227. [DOI] [PubMed] [Google Scholar]
- 5.Alberti KG, Zimmet P, Shaw J. Group IETFC. The metabolic syndrome – a new worldwide definition. Lancet 2005; 366: 1059–1062. [DOI] [PubMed] [Google Scholar]
- 6.Gaszner P, Makkos Z, Kosza P. Agranulocytosis during clozapine therapy. Prog Neuropsychopharmacol Biol Psychiatry 2002; 26: 603–607. [DOI] [PubMed] [Google Scholar]
- 7.Uçok A, Gaebel W. Side effects of atypical antipsychotics: a brief overview. World Psychiatry 2008; 7: 58–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cutler AJ. Sexual dysfunction and antipsychotic treatment. Psychoneuroendocrinology 2003; 28(Suppl 1): 69–82. [DOI] [PubMed] [Google Scholar]
- 9.NICE. Schizophrenia: core interventions in the treatment and management of schizophrenia in primary and secondary care, London: National Institute for Clinical Excellence, 2002. [Google Scholar]
- 10.Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO, et al. Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med 2005; 353: 1209–1223. [DOI] [PubMed] [Google Scholar]
- 11.Jones PB, Barnes TR, Davies L, Dunn G, Lloyd H, Hayhurst KP, et al. Randomized controlled trial of the effect on Quality of Life of second- vs first-generation antipsychotic drugs in schizophrenia: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS 1). Arch Gen Psychiatry 2006; 63: 1079–1087. [DOI] [PubMed] [Google Scholar]
- 12.Geddes J, Freemantle N, Harrison P, Bebbington P. Atypical antipsychotics in the treatment of schizophrenia: systematic overview and meta-regression analysis. BMJ 2000; 321: 1371–1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Taylor D, Paton C, Kapur S. The Maudsley prescribing guidelines in psychiatry, 12th ed Chichester: Wiley-Blackwell, 2015, pp. 15–188. [Google Scholar]
- 14.Verdoux H, Tournier M, Bégaud B. Antipsychotic prescribing trends: a review of pharmaco-epidemiological studies. Acta Psychiatr Scand 2010; 121: 4–10. [DOI] [PubMed] [Google Scholar]
- 15.Joint Formulary Committee. British national formulary 72, London: BMJ Publishing and the Royal Pharmaceutical Society, 2016. [Google Scholar]
- 16.WHO. Introduction to drug utilisation research. In: WIWGfDS (ed.) Methodology. Oslo: Author, 2003, p.38.
- 17.Gören JL, Meterko M, Williams S, Young GJ, Baker E, Chou CH, et al. Antipsychotic prescribing pathways, polypharmacy, and clozapine use in treatment of schizophrenia. Psychiatr Serv 2013; 64: 527–533. [DOI] [PubMed] [Google Scholar]
- 18.Leucht S, Cipriani A, Spineli L, Mavridis D, Orey D, Richter F, et al. Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet 2013; 382: 951–962. [DOI] [PubMed] [Google Scholar]
- 19.Buchanan RW, Kreyenbuhl J, Kelly DL, Noel JM, Boggs DL, Fischer BA, et al. The 2009 schizophrenia PORT psychopharmacological treatment recommendations and summary statements. Schizophr Bull 2010; 36: 71–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rycroft-Malone J, Seers K, Titchen A, Harvey G, Kitson A, McCormack B. What counts as evidence in evidence-based practice? J Adv Nurs 2004; 47: 81–90. [DOI] [PubMed] [Google Scholar]
- 21.Grant A, Sullivan F, Dowell J. An ethnographic exploration of influences on prescribing in general practice: why is there variation in prescribing practices? Implement Sci 2013; 8: 72–72. [DOI] [PMC free article] [PubMed] [Google Scholar]