Abstract
Background:
The body mass index (BMI) in the United States (US) is rising and may be contributing to increased anterior cruciate ligament reconstruction (ACLR) rates. It is currently unknown whether the BMI is increasing in patients who undergo ACLR.
Purpose:
To determine whether (1) the BMI changed in pediatric and adult patients who previously underwent ACLR or revision ACLR over a 10-year eligibility period, (2) the BMI changed at a greater rate in pediatric or adult patients, and (3) the percentage of overweight and obese patients in the ACLR population was different than that of the general overweight population.
Study Design:
Case series; Level of evidence, 4.
Methods:
A retrospective investigation of patients who underwent ACLR by 6 surgeons from June 3, 2005, to June 3, 2015, was conducted. Patients were divided into pediatric (<18 years) and adult (≥18 years) categories. BMI at the time of surgery was defined as underweight (<18.5 kg/m2), normal (18.5-24.9 kg/m2), overweight (25.0-29.9 kg/m2), and obese (≥30.0 kg/m2). Patients with an indeterminate BMI were excluded. Comparisons of overweight and obese patients were made with general population trends determined by the Centers for Disease Control and Prevention (CDC) in a single US state. Pearson (R) and Spearman (R s) correlations were used to determine correlations, Student t tests were used for 2-variable comparisons, analyses of variance were used for multivariable comparisons, and analyses of covariance were used for comparing linear relationships.
Results:
There were 1305 patients (733 male, 572 female; 409 pediatric, 896 adult) included. Adults requiring surgical revision demonstrated a strong positive correlation with respect to BMI over time (R s = 0.906, P < .01). No other statistically significant trends in the BMI over time were found. The proportion of overweight pediatric patients undergoing ACLR was significantly greater than that of the general overweight pediatric population (P < .05), and the proportion of obese pediatric and adult patients in the general population was greater than that of the obese patients in the study cohort (P < .05).
Conclusion:
Between 2005 and 2015, the BMI for pediatric and adult patients who underwent ACLR did not demonstrate a significant change over time. However, there was a statistically significant strong positive correlation for increasing BMI in adult patients requiring revision, although the mean BMI in patients who underwent revision was less than that of the general population. In addition, the percentage of overweight pediatric patients undergoing ACLR was significantly greater than that of the general population of overweight patients in a single US state reported by the CDC.
Keywords: ACL, ACLR, BMI, overweight, obese, revision, pediatric, adult, knee, ligaments
Obesity has become a national epidemic, with detrimental implications on morbidity, mortality, and health care expenditure in many aspects of medicine.22 A body mass index (BMI) registering as “overweight” (>25.0 kg/m2) or “obese” (>30.0 kg/m2) can predispose to and increase the morbidity of conditions such as coronary artery disease, osteoarthritis, diabetes mellitus, and hypertension.13,14,22 Studies have demonstrated a positive trend in both the pediatric and adult BMI over the past 25 to 50 years.9,17,18 Recent data have indicated that this trend has started to slow, but trends are not reversing.8
It is also important to understand how BMI affects the musculoskeletal system. A higher BMI subjects the knee to a greater risk of injuries through stress imposed by an increased load and joint space narrowing.16 Obese BMIs have been demonstrated to play a role in “ultra–low velocity” knee injuries that are sustained from activities of daily living, such as falling from standing or falling from a single step.2,10,25 These knee injuries impose a greater risk of neurovascular injuries as the BMI increases as well as a higher postoperative complication rate, including a greater incidence of surgical revision.2,24 Previous studies have indicated a correlation between elevated BMIs and the risk of noncontact anterior cruciate ligament (ACL) injuries.12,21,24 While an overweight or obese BMI cannot be cited as the direct cause for an ACL injury, the greater risk for injuries has major implications for orthopaedics.24 The purpose of this investigation was to determine if (1) the BMI changed in pediatric and adult patients who have undergone ACL reconstruction (ACLR) or revision ACLR over a 10-year eligibility period, (2) the BMI changed at a greater rate in pediatric or adult patients, and (3) the percentage of overweight and obese patients in the ACLR population was different from that of the general overweight population.
Methods
An institutional review board–approved retrospective case series of patients who underwent ACLR in association with an isolated ACL tear or multiligament tear (MLT) was performed by 6 surgeons from June 3, 2005, to June 3, 2015. Isolated ACL tears and MLTs involving the ACL in conjunction with a posterior cruciate ligament, medial collateral ligament, and lateral collateral ligament injury were included in the study. Current Procedural Terminology code 29888 was used to identify patients. ACLR with bone-tendon-bone autografts, semitendinosus-gracilis allografts, Achilles allografts, and central quadriceps tendon autografts were considered. Patients who underwent either primary ACLR or surgical revision were included.
Patient demographics were obtained from either a physical paper chart or electronic medical record. The date of surgery, height (m), weight (kg), demographic information, mechanism of injury, activity causing the injury, and presence or absence of surgical revision were obtained. The minimum follow-up was 2 years. BMI was calculated as weight in kilograms over the height in meters squared (kg/m2). BMI at the time of surgery was defined as underweight (<18.5 kg/m2), normal (18.5-24.9 kg/m2), overweight (25.0-29.9 kg/m2), and obese (≥30.0 kg/m2) as outlined by the Centers for Disease Control and Prevention (CDC).3
Comparisons were made by age, sex, athletic status, single-ligament tears and MLTs, overweight BMI, and obese BMI. Comparisons were also made of the overweight and obese patients in the study cohort to the overweight and obese general population, determined by CDC trends in a single United States (US) state. Patients were categorized as athletes if an ACL injury occurred during an organized athletic sporting event or practice for an organized event, and they were designated as nonathletes if an ACL injury occurred during a recreational sporting activity or during an activity not related to an organized sporting event. A pediatric patient was defined as anyone <18 years of age at the time of surgery, and an adult was defined as any patient ≥18 years of age. Exclusion criteria included patients with no height, weight, BMI, or date of service available.
Statistical Analysis
A 2-tailed Student t test assuming unequal variance was carried out for comparisons between 2 groups. Trends over time were analyzed by Pearson correlation (R) if the Kolmogorov-Smirnov test indicated a normal distribution and by Spearman correlation (R s) if the Kolmogorov-Smirnov test did not indicate a normal distribution. One-way analysis of variance was used for multiple group comparisons. Analysis of covariance was conducted to assess differences between linear models. A P value of <.05 was considered significant for all tests. If the P value was <.05 for multiple group tests, a post hoc comparison utilizing a Tukey honest significant difference test was conducted to determine the significance of the differences.
Results
There were 1691 ACLR procedures completed. Because of missing weight, height, or BMI data, 386 ACLR procedures were excluded from the study, allowing for a retrospective review of 1305 ACLR procedures. There were 896 (68.6%) adult (mean BMI, 27.2 ± 0.7 kg/m2) and 409 (31.3%) pediatric (mean BMI, 24.3 ± 1.1 kg/m2) patients (Table 1 and Figure 1). Overall, 5 (0.6%) adult and 11 (2.7%) pediatric patients were underweight, 361 (40.3%) adult and 108 (26.4%) pediatric patients were overweight, and 202 (22.6%) adult and 38 (9.3%) pediatric patients were obese. Of the 896 adults, 103 (11.5%) had an MLT, and 133 (14.8%) underwent surgical revision, without a significant difference in the mean BMI (F = 1.52, P = .309). Of the 409 pediatric patients, there were 57 (13.9%) known MLTs and 37 (9.0%) surgical revision procedures, without a significant difference in the mean BMI (F = 0.42, P = .67). For pediatric and adult patients, the choice of ACLR allograft or autograft did not significantly differ in terms of BMI for total ACL injuries, revision ACLR, or patients who did not require surgical revision (P = .49 and P = .62, respectively).
TABLE 1.
Demographics of Pediatric and Adult Patientsa
| Pediatric (n = 409) | Adult (n = 896) | All (N = 1305) | ||||
|---|---|---|---|---|---|---|
| n (%) | BMI, kg/m2 | n (%) | BMI, kg/m2 | n (%) | BMI, kg/m2 | |
| Total | 409 (100.0) | 24.3 ± 1.1 | 896 (100.0) | 27.2 ± 0.7 | 1305 (100.0) | 25.7 ± 1.7 |
| BMI, kg/m2 | ||||||
| <18.5 | 11 (2.7) | 17.2 ± 1.2 | 5 (0.6) | 17.3 ± 0.6 | 16 (1.2) | 17.3 ± 1.1 |
| 18.5-24.9 | 252 (61.6) | 22.0 ± 1.6 | 328 (36.6) | 22.6 ± 1.6 | 581 (44.5) | 22.3 ± 1.6 |
| 25.0-29.9 | 108 (26.4) | 27.1 ± 1.3 | 361 (40.3) | 27.1 ± 1.4 | 468 (35.9) | 27.1 ± 1.4 |
| ≥30.0 | 38 (9.3) | 34.6 ± 3.9 | 202 (22.6) | 34.7 ± 4.8 | 240 (18.4) | 34.7 ± 4.6 |
| MLT | 57 (13.9) | 25.3 ± 5.3 | 103 (11.5) | 26.6 ± 4.5 | 160 (12.2) | 26.1 ± 4.8 |
| Sex | ||||||
| Male | 212 (51.8) | 25.2 ± 0.9 | 521 (58.1) | 27.7 ± 0.5 | 733 (56.2) | 26.4 ± 1.5 |
| Female | 197 (48.2) | 23.1 ± 1.0 | 375 (41.8) | 26.5 ± 1.4 | 572 (43.8) | 24.8 ± 2.1 |
| Mode of injury | ||||||
| Contact | 85 (20.8) | 23.8 ± 1.2 | 70 (7.8) | 26.9 ± 1.3 | 155 (11.9) | 25.3 ± 1.9 |
| Noncontact | 191 (46.7) | 24.2 ± 1.7 | 550 (61.4) | 27.2 ± 0.8 | 741 (56.7) | 25.7 ± 2.0 |
| Unknown | 133 (32.5) | 24.0 ± 1.6 | 276 (30.8) | 27.4 ± 0.9 | 409 (31.3) | 25.9 ± 2.1 |
| Athletic status | ||||||
| Athlete | 267 (65.3) | 24.4 ± 1.0 | 133 (14.8) | 25.6 ± 0.6 | 400 (30.6) | 25.1 ± 0.9 |
| Nonathlete | 19 (4.6) | 24.4 ± 3.6 | 525 (58.6) | 27.9 ± 1.2 | 544 (41.7) | 27.3 ± 1.9 |
| Unknown | 123 (30.1) | 23.0 ± 1.8 | 238 (26.6) | 27.0 ± 0.8 | 361 (27.7) | 25.1 ± 2.5 |
| ACL reinjured | 37 (9.0) | 24.2 ± 2.3 | 133 (14.8) | 26.8 ± 1.6 | 170 (12.6) | 25.6 ± 1.5 |
| Male | 14 (3.4) | 26.7 ± 4.6 | 66 (7.4) | 27.0 ± 1.3 | 80 (6.1) | 26.8 ± 0.2 |
| Female | 23 (5.6) | 22.5 ± 2.9 | 67 (7.5) | 26.7 ± 2.8 | 90 (6.9) | 24.8 ± 2.9 |
| ACL nonreinjured | 372 (90.9) | 24.3 ± 0.9 | 769 (85.8) | 27.1 ± 1.2 | 1141 (87.4) | 25.7 ± 1.9 |
| Male | 198 (48.4) | 25.0 ± 0.9 | 458 (51.1) | 27.7 ± 0.5 | 656 (50.3) | 26.3 ± 1.9 |
| Female | 174 (42.5) | 23.2 ± 1.2 | 311 (34.7) | 26.6 ± 1.5 | 485 (37.1) | 24.9 ± 2.4 |
| ACLR allograft | ||||||
| Achilles | 27 (6.6) | 24.8 ± 7.0 | 288 (32.1) | 26.8 ± 5.1 | 315 (24.1) | 27.2 ± 11.5 |
| STG | 4 (0.9) | 23.7 ± 1.8 | 5 (0.6) | 26.8 ± 5.6 | 9 (0.7) | 25.3 ± 3.3 |
| ACLR autograft | ||||||
| BTB | 149 (36.4) | 24.3 ± 4.0 | 318 (35.5) | 26.7 ± 5.5 | 467 (35.8) | 26.4 ± 5.3 |
| STG | 103 (25.2) | 24.6 ± 4.4 | 75 (8.4) | 26.4 ± 3.6 | 178 (13.6) | 25.4 ± 4.2 |
| CQT | 11 (2.7) | 23.0 ± 2.6 | 29 (3.2) | 25.8 ± 3.7 | 40 (3.1) | 25.0 ± 3.6 |
aData are shown as mean ± SD unless otherwise indicated. ACL, anterior cruciate ligament; ACLR, anterior cruciate ligament reconstruction; BMI, body mass index; BTB, bone-tendon-bone; CQT, central quadriceps tendon; MLT, multiligament tear; STG, semitendinosus-gracilis.
Figure 1.
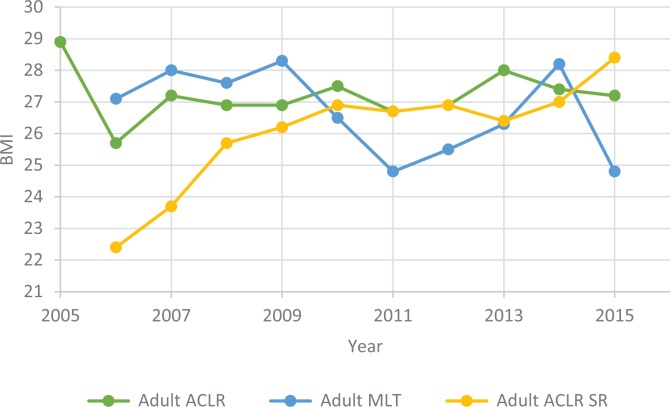
Body mass index (BMI) trends in adult patients with regard to anterior cruciate ligament reconstruction (ACLR), multiligament tear (MLT), and surgical revision (SR).
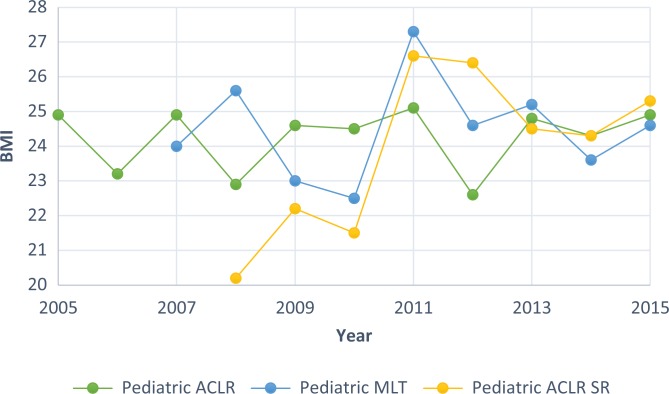
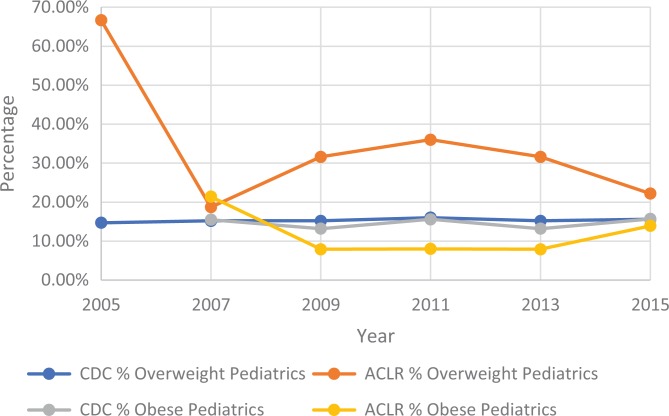
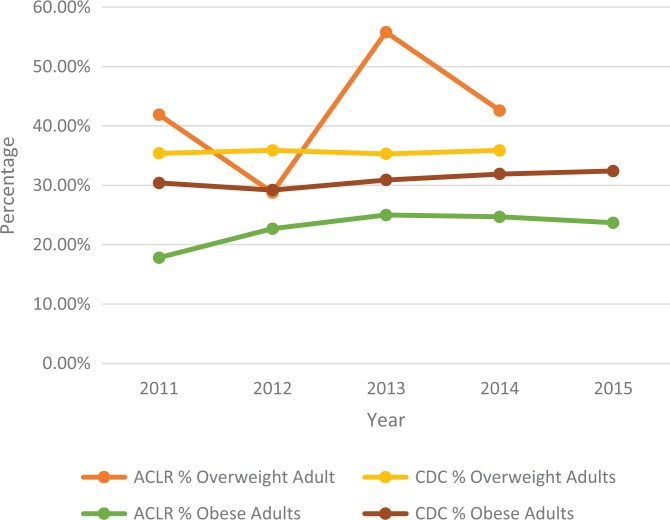
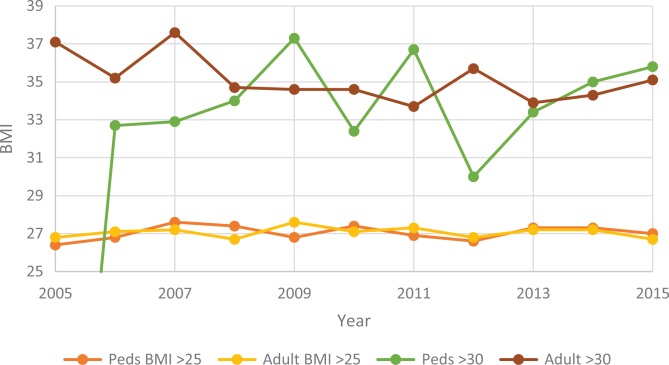
With respect to BMI changes over time, there was a strong positive correlation with adults who underwent revision surgery (R s = 0.906, P < .01) (Figure 1), which was statistically significant. No other significant correlations with respect to BMI and time were found when comparing sex, adult and pediatric patients, overweight patients, or obese patients. There was a significant difference between adult (27.2 ± 0.7 kg/m2) and pediatric BMI (24.3 ± 1.1 kg/m2) (P < .01), adult male (27.7 ± 0.5 kg/m2) and pediatric male BMI (25.2 ± 0.9 kg/m2) (P < .01), and adult female (26.5 ± 1.4 kg/m2) and pediatric female BMI (23.1 ± 1.0 kg/m2) (P < .01) (Table 1 and Figures 1 and 2). The proportion of overweight pediatric patients undergoing ACLR was significantly greater than the percentage of overweight patients in the general population (P < .05) (Figure 3), the proportion of obese adult (Figure 4) and pediatric (Figure 3) patients undergoing ACLR was significantly less than that of the general obese population (P < .05), and no significant difference was found between the percentage of overweight adult patients undergoing ACLR and the percentage overweight in the general adult population (P = .273) (Figure 4).
Figure 2.
Body mass index (BMI) trends in pediatric patients with regard to anterior cruciate ligament reconstruction (ACLR), multiligament tear (MLT), and surgical revision (SR).
Figure 3.
Percentage trends in overweight and obese pediatric individuals undergoing ACLR and those in the general pediatric population in a single American state. ACLR, anterior cruciate ligament reconstruction; CDC, Centers for Disease Control and Prevention.
Figure 4.
Percentage trends in overweight and obese adults undergoing ACLR and those in the general adult population in a single American state. ACLR, anterior cruciate ligament reconstruction; CDC, Centers for Disease Control and Prevention.
There was a significant difference between the percentage of overweight pediatric versus overweight adult ACLR patients (P < .01), overweight adults undergoing ACLR versus CDC-determined overweight adults (P < .01), athlete versus nonathlete ACLR patients (P < .01), obese adults undergoing ACLR versus CDC-determined obese adults (P < .05) (Figures 3 -5), and adult ACLR patient BMI compared with reinjured adult BMI (P < .01) (Table 1 and Figures 1 and 2) over time when controlling for patient age.
Figure 5.
Body mass index (BMI) trends in overweight and obese pediatric and adult patients.
Discussion
The BMI for adults who required surgical revision demonstrated a statistically significant positive trend over time, but no other significant trends in the pediatric or adult BMI were found. There was not a significant difference in the rate of change over time between the 2 age groups. The percentage of overweight pediatric patients undergoing ACLR was greater than the CDC estimates of overweight in the general pediatric population, the proportion of obese adults in the general population was greater than that of obese adult patients undergoing ACLR, and the proportion of obese pediatric individuals in the general population was greater than that of obese pediatric patients undergoing ACLR. The proportion of overweight adults undergoing ACLR and overweight adults in the general population was not found to be statistically significant.
Trends in the pediatric and adult BMI did not appreciably change with time, which may indicate that BMI trends among patients undergoing ACLR have started to plateau, as studies have suggested for the general population.8 However, there was a strong positive correlation for the BMI of adults who required surgical revision of their ACL. The reason that the mean BMI in the adult surgical revision group was significantly less than the BMI for the total adult ACLR group is unclear. This difference may be secondary to decreased athletic exposure in adults with a greater BMI after the initial injury because of concerns for the risk of reinjuries or a change in body habitus after the initial injury. In addition, the body composition of these patients was not known. While the mean BMI was less than that of the primary injury group, it is possible that these patients had an overall greater body fat composition as compared with muscle mass. The impact that either has on ACL injuries is not known and was not assessed in this study.
The risk of surgical revision may be related to the high proportion of adult patients who did not participate in regular athletic activity (58.6%) compared with the CDC-estimated population (27.0%).4 It has been demonstrated that overweight and obese patients are at a greater risk for ultra–low velocity knee injuries and ACL injuries through noncontact mechanisms.2,10,12,21,24,25 These patients may also be at a greater risk of requiring surgical revision because of ACL reinjuries. Adults who required surgical revision demonstrated a positive trend in the BMI with respect to time but tended to have a lower annual mean BMI than the general population. While this trend is significant, it does not necessarily indicate that BMI is the sole predisposing risk factor in these patients.
Generalized joint laxity as a risk factor for ACL injuries is well described in the literature. Sueyoshi et al23 demonstrated that female adolescents who have already had an ACL injury have a greater risk for joint reinjuries because of increased joint hyperlaxity. Joint laxity was not a variable assessed in this study cohort, but it cannot be ruled out as a superimposed risk factor for the subset of adult and pediatric patients who required surgical revision. That these patients had a lower annual BMI compared with the nonrevision group lends support that there were additional variables predisposing these patients to the risk of reinjuries. Further studies to investigate the relationship of BMI and joint laxity in both pediatric and adult cohorts should be conducted to better assess the relationship and effect on ACL reinjuries.
The lack of a BMI trend over time in any of the pediatric groups studied, despite a growing frequency of ACL injuries in the US,5,15 may be related to the degree of physical activity of the patients. Athletes are generally in better shape and exercise more frequently than the general population, which may account for the lack of an upward trend in the mean BMI over time. In this study, 65.3% of pediatric patients were identified as athletes at the time of their sustained ACL injury. When compared with the general population recorded by the CDC, pediatric patients in this study constituted a greater proportion of athletes and overweight patients but a smaller proportion of obese patients.4 This finding may be related to the overall greater muscle mass that is often seen in patients who compete in sports with a greater risk of ACL injuries, such as football and basketball, as compared with athletes who have lower BMIs, such as runners and cyclists.
It was expected that the mean BMI for patients undergoing ACLR would rise over time because studies have demonstrated that the incidence of pediatric and adult ACLR tears has increased in the US in the past 2 decades, with a predilection of patients aged <20 years and >40 years.5,15 Mall et al15 demonstrated that female patients have increased to the greatest degree, whereas Dodwell et al5 demonstrated that among patients 3 to 20 years of age, pediatric male patients have increased at the greatest rate. The data in the current study suggest that, in both pediatric and adult ACLR patients, there were more male than female patients, whereas female patients had a slightly higher rate of surgical revision. This is interesting because female athletes appear to have many risk factors for an ACL injury, including the normal hormonal changes of menarche, age-related impact on ligament laxity, ovulatory phase of the menstrual cycle, and BMI in relation to noncontact injuries.1,7,11,19,20,24
The data from this study suggest that there are other factors besides BMI that are contributing to the increasing incidence of ACL injuries, such as increasing participation in sporting events that put patients at a greater risk for knee injuries, the age at which patients participate, or even improved clinician detection of ACL injuries. However, the results of this study do not necessarily indicate that BMI plays no role in the mechanism of injury. More studies are needed that assess the impact of BMI on normal physiological fluctuations of hormones, the degree to which the musculoskeletal system is affected in both athletic and sedentary lifestyles, the risk for surgical revision, and the impact of body composition versus body mass on ACL injuries.
The limitations in this study included 386 patients with an unknown BMI, unknown mechanism of injury (contact and noncontact), athletic status, and grafting technique. Approximately 31.3% of the injury mechanism and 27.7% of the athletic status were unknown, which may have affected the BMI trends in athletes and nonathletes. Another limitation was that because this was a retrospective study, the use of an athlete and nonathlete stratification tool such as the Tegner activity scale could not be used, which means that the number of ACL injuries that occurred in athletes and nonathletes may not be accurately depicted.
In this study, patients were categorized as athletes if an ACL injury occurred during an organized athletic sporting event or practice for an organized event; patients were designated as nonathletes if an ACL injury occurred during a recreational activity or during an activity not related to an organized sporting event. Pediatric patients more commonly participate and sustain injuries in organized sporting events, which would classify them as “athletes” at the time of injury. Adults more often sustain ACL injuries in recreational events such as skiing or “pick-up” sporting activities, which would classify them as “nonathletes” during the time of injury, based on the study definition. Because of the small proportion of nonathletes in the pediatric group, and the small athletic subset among adult patients, it was difficult to compare BMI trends in pediatric and adult athletes and nonathletes.
It should also be noted that BMI is a marker for overall body weight rather than body composition.6 As a result, this would mean that patients with both a fat-predominant or muscle-predominant body composition can be considered overweight when using the CDC definition of an “overweight” BMI. This may result in a falsely elevated number of athletes with an overweight or obese BMI, depending on the type of athletic activity. Body composition data were not collected during this study. Loss of follow-up data in which a patient moved to a different area or used a different physician if he or she required surgical revision may have also affected the definitive number of patients and BMI trends in this group.
Conclusion
Between 2005 and 2015, the BMI for pediatric and adult patients who underwent ACLR did not demonstrate a significant change over time. However, there was a statistically significant strong positive correlation for increasing BMI in adult patients requiring revision, although the mean BMI in revision patients was less than that of the general population. In addition, the percentage of overweight pediatric patients undergoing ACLR was significantly greater than that of the general population of overweight patients in a single US state reported by the CDC.
Footnotes
One or more of the authors has declared the following potential conflict of interest: P.C.M. has received research support from Arthrex and DePuy; is a paid speaker for Aastrom Biosciences and Vericel; and has received support for a sports medicine fellowship from Aastrom Biosciences, Arthrex, and MedInc. J.D.H. has received research support from DePuy and Smith & Nephew, has received educational support from Arthrex and MedInc, is a paid consultant for NIA Magellan and Smith & Nephew, is a paid speaker for Ossur and Smith & Nephew, receives publishing royalties from SLACK, and has received support for a sports medicine fellowship from Arthrex and MedInc.
Ethical approval for this study was obtained from the Houston Methodist Research Institute.
References
- 1. Adachi N, Nawata K, Maeta M, Kurozawa Y. Relationship of the menstrual cycle phase to anterior cruciate ligament injuries in teenaged female athletes. Arch Orthop Trauma Surg. 2007;128(5):473–478. [DOI] [PubMed] [Google Scholar]
- 2. Azar F, Brandt J, Miller R, Phillips B. Ultra-low-velocity knee dislocations. Am J Sports Med. 2011;39(10):2170–2174. [DOI] [PubMed] [Google Scholar]
- 3. Centers for Disease Control and Prevention. Defining adult overweight and obesity. Available at: https://www.cdc.gov/obesity/adult/defining.html. Accessed December 28, 2017.
- 4. Centers for Disease Control and Prevention. NPAO data trends and maps: Texas location summary. Available at: https://nccd.cdc.gov/NPAO_DTM/LocationSummary.aspx?state=Texas. Accessed March 22, 2017.
- 5. Dodwell ER, Lamont LE, Green DW, Pan TJ, Marx RG, Lyman S. 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med. 2014;42(3):675–680. [DOI] [PubMed] [Google Scholar]
- 6. Etchison W, Bloodgood E, Minton C, et al. Body mass index and percentage of body fat as indicators for obesity in an adolescent athletic population. Sports Health. 2011;3(3):249–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Evans K, Kilcoyne K, Dickens J, et al. Predisposing risk factors for non-contact ACL injuries in military subjects. Knee Surg Sports Traumatol Arthrosc. 2011;20(8):1554–1559. [DOI] [PubMed] [Google Scholar]
- 8. Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2010. JAMA. 2012;307(5):491–497. [DOI] [PubMed] [Google Scholar]
- 9. Flegal KM, Carroll MD, Kuczmarski RJ, Johnson CL. Overweight and obesity in the United States: prevalence and trends, 1960-1994. Int J Obes Relat Metab Disord. 1998;22(1):39–47. [DOI] [PubMed] [Google Scholar]
- 10. Georgiadis A, Guthrie S, Shepard A. Beware of ultra-low-velocity knee dislocation. Orthopedics. 2014;37(10):656–658. [DOI] [PubMed] [Google Scholar]
- 11. Heitz N, Eisenman P, Beck C, Walker J. Hormonal changes throughout the menstrual cycle and increased anterior cruciate ligament laxity in females. J Athl Train. 1999;34(2):144–149. [PMC free article] [PubMed] [Google Scholar]
- 12. Hewett TE, Myer GD, Ford KR. Anterior cruciate ligament injuries in female athletes, part 1: mechanisms and risk factors. Am J Sports Med. 2006;34(2):299–311. [DOI] [PubMed] [Google Scholar]
- 13. Hillier TA, Pedula KL. Characteristics of an adult population with newly diagnosed type 2 diabetes: the relation of obesity and age of onset. Diabetes Care. 2001;24(9):1522–1527. [DOI] [PubMed] [Google Scholar]
- 14. Huang Z, Willett W, Manson J, et al. Body weight, weight change, and risk for hypertension in women. Ann Intern Med. 1998;128(2):81. [DOI] [PubMed] [Google Scholar]
- 15. Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014;42(10):2363–2370. [DOI] [PubMed] [Google Scholar]
- 16. Marin E, Bifulco S, Fast A. Obesity: a risk factor for knee dislocation. Am J Phys Med Rehabil. 1990;69(3):132–134. [PubMed] [Google Scholar]
- 17. Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006;295(13):1549–1555. [DOI] [PubMed] [Google Scholar]
- 18. Ogden CL, Carroll MD, Lawman H, et al. Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA. 2016;315(21):2292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Prodromos C, Han Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury–reduction regimen. Arthroscopy. 2007;23(12):1320–1325.e6. [DOI] [PubMed] [Google Scholar]
- 20. Shultz S, Kirk S, Johnson M, Sander T, Perrin D. Relationship between sex hormones and anterior knee laxity across the menstrual cycle. Med Sci Sports Exerc. 2004;36(7):1165–1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Stracciolini A, Stein C, Zurakowski D, Meehan W, Myer G, Micheli L. Anterior cruciate ligament injuries in pediatric athletes presenting to sports medicine clinic. Sports Health. 2015;7(2):130–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sturm R. The effects of obesity, smoking, and drinking on medical problems and costs. Health Aff (Millwood). 2002;21(2):245–253. [DOI] [PubMed] [Google Scholar]
- 23. Sueyoshi T, Emoto G, Yuasa T. Generalized joint laxity and ligament injuries in high school–aged female volleyball players in Japan. Orthop J Sports Med. 2016;4:232596711666769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Uhorchak J, Scoville C, Williams G, Arciero R, Pierre P, Taylor D. Risk factors associated with noncontact injury of the anterior cruciate ligament. Am J Sports Med. 2003;31(6):831–842. [DOI] [PubMed] [Google Scholar]
- 25. Werner B, Gwathmey F, Higgins S, Hart J, Miller M. Ultra-low velocity knee dislocations: patient characteristics, complications, and outcomes. Am J Sports Med. 2014;42(2):358–363. [DOI] [PubMed] [Google Scholar]