Lesson
Management of retroperitoneal soft tissue sarcomas is complex. Treatment is usually multimodal; involving surgery, chemotherapy and radiotherapy.
Keywords: synovial sarcoma, retroperitoneal, abdominal tumour
Introduction
Sarcomas are malignant tumours that originate from cells of mesenchymal origin. Synovial sarcoma is one of the subtypes of soft tissue sarcomas. The majority of soft tissue sarcomas are present in the extremities; however, many other sites can be affected, including the retroperitoneum, chest wall, head and neck and subcutaneous tissues. Retroperitoneal soft tissue sarcomas account for only 15% of all soft tissue sarcomas.1
It is imperative that other rare causes of an abdominal mass in a young man, such as primary germ cell tumour, lymphoma or metastatic testicular cancer, are excluded. A detailed history, e.g. symptoms related to lymphoma (such as fever, night sweats and weight loss), and a systematic physical examination (including genitalia and local lymph nodes) should be performed. Other benign and malignant tumours, such as schwannomas and paragangliomas, should be considered in the differential diagnosis of a retroperitoneal mass.
Case report
A 17-year-old male presented with one month history of right-sided abdominal swelling and discomfort with no other associated gastrointestinal symptoms. General examination findings were normal. Examination of the abdomen revealed a round mobile palpable mass in right iliac fossa; there was no abdominal distension or clinical evidence of ascites. Bowel sounds were normal. The rest of the systemic physical examination (including a testicular examination) was unremarkable.
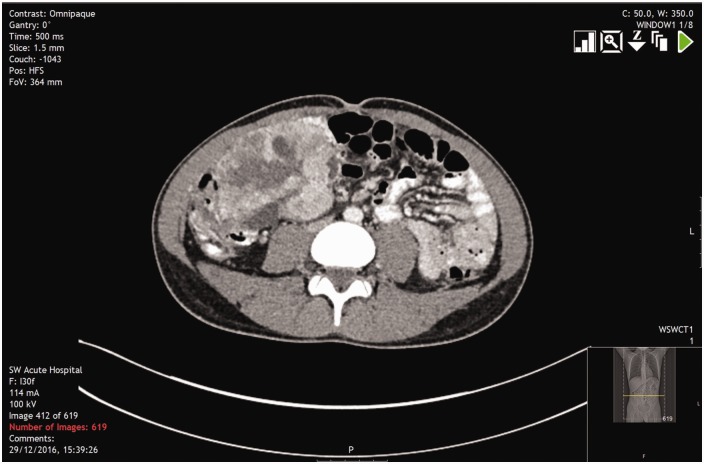
Complete blood count and biochemistry profiles were within normal range. C-reactive protein was slightly elevated (22.5 mg/L). Tumour markers (alpha-fetoprotein and b-HCG) were normal. Contrast-enhanced computed tomography scan of the chest, abdomen and pelvis revealed a well-defined soft tissue mass with mixed enhancement measuring 8 × 10 × 8 cm, lying medial to the ascending colon and extending anteriorly to the anterior abdominal wall and posteriorly to the psoas muscle (Figure 1). There was no evidence of pulmonary metastatic disease. Ultrasound-guided core biopsy from the mass confirmed a grade 2 synovial sarcoma associated with positive immunoreactivity for CD 99, TLE-1 and EMA and negative for CD34.
Figure 1.
Axial CT abdomen and pelvis with contrast demonstrates a well-defined enhanced soft tissue mass (black arrow) in the right retroperitoneal area, which lies medially from the ascending colon and extends anteriorly to the anterior abdominal wall and posteriorly on the psoas muscle.
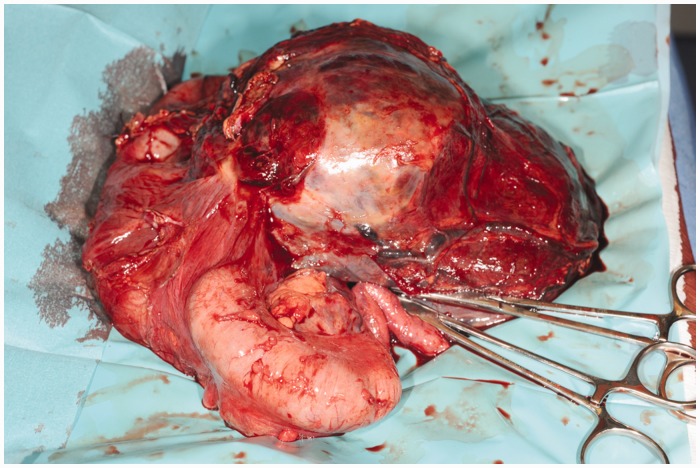
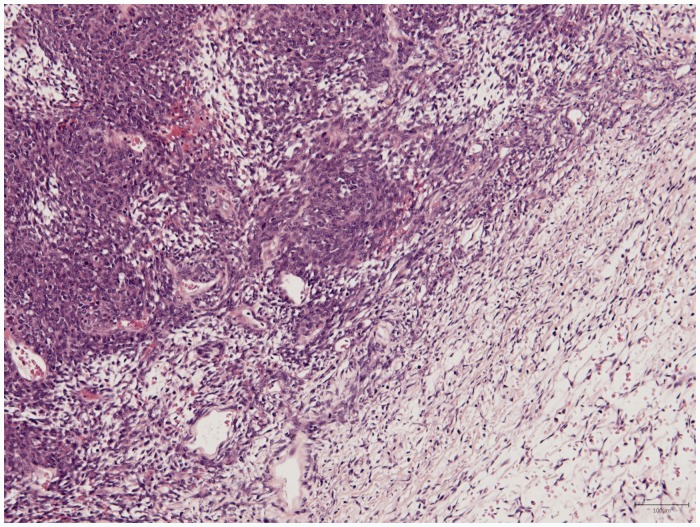
The patient underwent a laparotomy and resection of the mass. A ureteric stent (JJ stent) was inserted prior to commencing the laparotomy in order to allow identification of the right ureter. The right colon was mobilised laterally. The tumour were removed en-bloc (Figure 2) and submitted for final histopathology examination. A primary ileocolic anastomosis (side-to-side) was performed using the gastrointestinal anastomosis and transverse anastomosis stapling devices (Barcelona technique). The Postoperative course was uneventful and the patient was discharged at seven days. The stent was removed on postoperative day 28. The histology of the tumour (R0 complete resection) revealed a monomorphic spindle cell sarcoma with a predominant fascicular architecture and appearances consistent with a synovial sarcoma (Federation Nationale des Centres de Lutte Contre le Cancer grade 3) (Figure 3). The patient has been commenced on Doxifos (a combination of doxorubicin and ifosfamide) adjuvant chemotherapy.
Figure 2.
A specimen from the patient showing retroperitoneal sarcoma.
Figure 3.
Histology shows bland monomorphic tumour spindle cells with alternating hypercellular and myxoid zones. There are some areas of necrosis and haemorrhage of the tumour (haematoxylin and eosin staining, original magnification ×100).
Discussion
Soft tissue sarcomas are most often seen in the extremities (59%), trunk (19%), retroperitoneum (15%) and head and neck (9%).2 Synovial sarcoma is the fourth most common sub type of soft tissue sarcoma,3 often occurring in the vicinity of a large joint. Primary intra-abdominal synovial sarcoma is rare and most cases are retroperitoneal. Synovial sarcoma of the anterior abdominal wall has been reported.3,4 Synovial sarcoma occurs most commonly in the young, representing about 5–10% of all soft tissue sarcomas.2,5,6
Histologically, synovial sarcoma exhibits a biphasic pattern with a distinct epithelial component (glands) and a distinct spindle-cell component. The monophasic synovial sarcomas consist of spindle cell only. Immunohistochemically, synovial sarcoma exhibits positive staining for epithelial membrane antigen (EMA), cytokeratins (AE1/AE3, 7 and 19) and carcinoembryonic antigen in the epithelial component and for E-cadherin, vimentin, CD99 and CD56 in the spindle cell component.7 A combination with a negative CD34 is important to complete the diagnosis.7 The final histology and immunohistology of the tumour were consistent with synovial sarcoma.
Like other soft tissue sarcomas, there is no universal grading system for reporting histopathology results.8 At present, the Federation Nationale des Centres de Lutte Contre le Cancer grading system and the American Joint Committee on Cancer tumour, node and metastasis staging system are generally used as prognostic tools for soft tissue sarcomas. Further surgical and oncological (whether chemotherapy or radiotherapy) approaches depend on the size, location, histologic sub-type and grading and staging of the sarcoma and require a comprehensive multidisciplinary evaluation (involving pathologists, radiologists, surgeons, radiation therapists, medical oncologists and paediatric oncologists if applicable).
CT or, less commonly, magnetic resonance imaging of the abdomen and pelvis usually provides satisfactory primary tumour imaging. A chest CT should also be considered to rule out metastatic disease to the lungs. CT is better in delineating the anatomical relationship of the tumour to other abdominal organs and is less associated with motion-related artefacts compared to magnetic resonance imaging.9 It can also detect metastases to the liver or peritoneum.
Surgery
Surgery for retroperitoneal sarcoma can be complex and may not always be possible. Small low-grade soft tissue tumours usually only require tumour mass resection. High-grade tumours are treated with surgery and often with radiation and chemotherapy in either adjuvant or neoadjuvant settings. Surgical resections can be classified as intralesional (entering the tumour but removing all visible tissue), marginal (through the surrounding pseudocapsule, often leaving microscopic tumour), wide (including a cuff of normal tissue in the resection) and radical (resection of the entire compartment). A wide resection with negative margins (R0) is recommended for all soft tissue sarcomas. However, due to the large size of most retroperitoneal sarcoma, this goal is difficult to achieve. Thus, in practice, resections may be grossly complete but have microscopically positive margins (an R1 resection) or be macroscopically incomplete (an R2 resection).1 Resection with 2 cm margins is the objective standard of care, and incomplete resection can result in high rates of local recurrence.
Chemotherapy
The role of chemotherapy for the treatment of soft tissue sarcomas remains controversial. The sensitivity and response to chemotherapy vary among histologic sub-types. Adjuvant chemotherapy is not used in chemo-resistant tumour, for example, liposarcoma is insensitive to chemotherapy; therefore, it is not used to treat retroperitoneal sarcoma of this sub-type. Adjuvant chemotherapy is usually given in patients with high risk of local tumour recurrence, high-grade tumour or distant metastases. Synovial sarcomas typically metastasise to the lung and less commonly to the bones and lymph nodes.7
Conventional chemotherapy drugs, such as ifosfamide, vincristine, cyclophosphamide and doxorubicin, are cytotoxic. The latter is associated with cardiomyopathy; therefore, it is important that a baseline echocardiogram should be organised prior to starting the medication. The benefit of chemotherapy in synovial sarcoma to overall survival remains unclear, although a recent study has shown that survival of patients with advanced, poorly differentiated disease marginally improves with doxorubicin and ifosfamide treatment.10 Some data suggest that neoadjuvant treatment may facilitate a margin-negative operation that might not otherwise have been possible.
Radiotherapy
Adjuvant radiotherapy may be used to help in local control in patients with high-grade, superficial lesions. Radiation can be beneficial in decreasing local recurrence rate and metastases11 but may not be feasible if there is a risk of radiation injury to an adjacent organ. The benefit of radiotherapy in synovial sarcoma is less clear than for chemotherapy.10
Conclusion
Primary retroperitoneal synovial sarcoma is rare. Although surgery remains the mainstay of treatment of soft tissue sarcoma, adjunctive radiation treatment and chemotherapy, either alone or in combination, may reduce local recurrence and control metastases. Treatment regimens should be planned based on both histologic and molecular subtypes, in addition to other disease- and patient-related factors.
Acknowledgements
This article was previously accepted and presented as a poster presentation at the Royal Society of Medicine President’s day on 29 September 2017 at Cardiff City Hall, UK.
Declarations
Competing Interests
None declared.
Funding
None declared.
Ethics approval
Written informed consent for publication was obtained from the patient.
Guarantor
PDC.
Contributorship
CSW summarised the case and wrote the manuscript. AH and RK provided advise. OPH provided histology images. PDC proofreaded and provided overall supervision in the writing of this article.
Provenance
Not commissioned; peer-reviewed by Imtiaz Wani and Gareth Morris-Stiff.
References
- 1.Raut CP, Pisters PW. Retroperitoneal sarcomas: combined-modality treatment approaches. J Surg Oncol 2006; 94: 81–87. [DOI] [PubMed] [Google Scholar]
- 2.Enzinger FM, Weiss SW. Soft tissue tumor, St Louis: Mosby, 1995. [Google Scholar]
- 3.Kritsaneepaiboon S, Sangkhathat S, Mitarnun W. Primary synovial sarcoma of the abdominal wall: a case report and literature review. J Radiol Case Rep 2015; 9: 47–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saif AH. Primary synovial sarcoma of the abdominal wall: a case report and review of the literature. J Family Community Med 2008; 15: 123–125. [PMC free article] [PubMed] [Google Scholar]
- 5.Milchgrub S, Ghandur-Mnaymneh L, Dorfman HD, Albores-Saavedra J. Synovial sarcoma with extensive osteoid and bone formation. Am J Surg Pathol 1993; 17: 357–363. [DOI] [PubMed] [Google Scholar]
- 6.Miettinen M, Virtanen I. Synovial sarcoma – a misnomer. Am J Pathol 1984; 117: 18–25. [PMC free article] [PubMed] [Google Scholar]
- 7.Vera J, Garcia MD, Marigil M, Abascal M, Lopez JI, Ligorred L. Biphasic synovial sarcoma of the abdominal wall. Virchows Arch 2006; 449: 367–372. [DOI] [PubMed] [Google Scholar]
- 8.Coindre JM. Grading of soft tissue sarcomas: review and update. Arch Pathol Lab Med 2006; 130: 1448–1453. [DOI] [PubMed] [Google Scholar]
- 9.Sanders TG, Parsons TW., 3rd Radiographic imaging of musculoskeletal neoplasia. Cancer Control 2001; 8: 221–231. [DOI] [PubMed] [Google Scholar]
- 10.Thway K, Fisher C. Synovial sarcoma: defining features and diagnostic evolution. Ann Diagn Pathol 2014; 18: 369–380. [DOI] [PubMed] [Google Scholar]
- 11.O'Sullivan B, Ward I, Catton C. Recent advances in radiotherapy for soft-tissue sarcoma. Curr Oncol Rep 2003; 5: 274–281. [DOI] [PubMed] [Google Scholar]