Abstract
Background: Reliable information reporting systems ensure that all malaria cases are tested, treated and tracked to avoid further transmission. Botswana aimed to eliminate malaria by 2018, and surveillance is key. This study focused on assessing the uptake of the new malaria case-based surveillance (CBS) system introduced in 2012, which captures information on malaria cases reported in the Integrated Disease Surveillance and Response (IDSR) system.
Methods: This was a retrospective descriptive study based on routine data focusing on Ngami, Chobe and Okavango, three high-risk districts in Botswana. Aggregated data variables were extracted from the IDSR and compared with data from the CBS.
Results: The IDSR reported 456 malaria cases in 2013 and 1346 in 2014, of which respectively only 305 and 884 were reported by the CBS. The CBS reported 34% fewer cases than the IDSR system, indicating substantial differences between the two systems. The key malaria indicators with the greatest variability among the districts included in the study were case identification number and date of diagnosis.
Conclusion: The IDSR and CBS systems are essential for malaria elimination, as shown by the significant gaps in reporting between the two systems. These findings highlight the need for further investigation into these discrepancies. Strengthening the CBS system will help to reach the objective of malaria elimination in Botswana.
Keywords: malaria, operational research, SORT IT, Botswana, surveillance
Abstract
Contexte : Un système fiable de reportage des informations assure que tous les cas de paludisme sont testés, traités et suivis pour éviter toute transmission ultérieure. Le Botswana avait visé à éliminer le paludisme pour 2018, et la surveillance est essentielle. Cette étude s'est concentrée sur l'évaluation de la couverture de la nouvelle surveillance basée sur les cas de paludisme (CBS) introduite en 2012, dans laquelle on saisit les informations relatives aux cas de paludisme rapportés au sein du système intégré de surveillance et de réponse aux maladies (IDSR).
Méthodes: Une étude rétrospective, descriptive, basée sur des données de routine et concentrée sur les trois districts à risque élevé de Ngami, Chobe et Okavango. Les variables de données agrégées ont été extraites de l'IDSR et comparées aux données de la CBS.
Résultats : L'IDSR a rapporté 456 cas de paludisme en 2013 et 1346 en 2014, dont seulement 305 et 884, respectivement, ont été rapportés par la CBS. La CBS a rapporté 34% de cas de moins que l'IDSR, ce qui montre une différence substantielle entre les deux systèmes de déclaration. Les indicateurs clés du paludisme qui ont la plus grande variabilité parmi les districts ont inclus le numéro d'identification des cas et la date du diagnostic.
Conclusion : Les systèmes IDSR et CBS sont essentiels pour l'élimination du paludisme, comme le montrent les disparités significatives de la déclaration entre les deux systèmes. Ces résultats sont en faveur d'investigations ultérieures relatives à ces disparités. Le renforcement du système de CBS aidera à assurer la réalisation de l'objectif d'élimination du paludisme au Botswana.
Abstract
Marco de referencia: Los sistemas fiables de presentación de informes garantizan el examen, el tratamiento y el seguimiento de todos los casos de paludismo con el fin de evitar la transmisión. Botswana busca eliminar el paludismo en el 2018 y la vigilancia representa un aspecto fundamental. En el presente estudio se evaluó la utilización de un nuevo sistema de vigilancia del paludismo basada en los casos (CBS, por Case-Based Surveillance), introducido en el 2012, que capta información sobre los casos de paludismo notificados al sistema Integrado de Vigilancia y Respuesta Sanitaria (IDSR, por Integrated Disease Surveillance and Response).
Métodos: Un estudio retrospectivo descriptivo sobre los datos corrientes, con un interés especial en tres distritos de alto riesgo de transmisión, a saber: Ngami, Chobe y Okavango. Los datos agregados de las variables se extrajeron del IDSR y se compararon con los datos del CBS.
Resultados: En el 2013, el sistema IDSR notificó 456 casos de paludismo y 1346 en 2014, de los cuales solo 305 y 884, respectivamente, se informaban en el CBS. El sistema CBS notificó 34% menos de casos que el sistema IDSR, lo cual puso de manifiesto diferencias considerables en los mecanismos de presentación de informes. Los indicadores fundamentales del paludismo que exhibieron una mayor variabilidad entre los distritos fueron el número de identificación del caso y la fecha del diagnóstico, en ese orden.
Conclusión: Los sistemas IDSR y CBS son primordiales en la eliminación del paludismo, pero presentan deficiencias notables de notificación. Estas observaciones incitan a practicar nuevas investigaciones sobre las discrepancias encontradas. El fortalecimiento del sistema CBS ayudara a garantizar el cumplimiento del objetivo de eliminación del paludismo en Botswana.
The goal of malaria elimination relies heavily on surveillance systems that can rapidly and efficiently detect, treat and respond to each individual case. Successful surveillance determines whether malaria elimination is feasible, and is a key component for success.1 Malaria remains a major public health concern, with approximately 214 million malaria cases and 438 000 deaths reported in 2014.2 Africa has the greatest malaria burden globally, accounting for more than 90% of deaths worldwide.2 Since 2000, with combined efforts, Botswana has made substantial reductions in malaria:3 numbers of cases have plunged by approximately 98%, from 70 000 cases reported in 2000 to only 1480 in 2014, placing the country on the verge of malaria elimination.4
Due to the country's success in malaria reduction, Botswana was marked for elimination by 2015, which was later extended to 2018 following a programme review in 2013.3 Malaria elimination is defined as the halt of local transmission in a defined area.5 The elimination target called for reorientation of the programme, which included the scale-up of vector control, case management, advocacy, community mobilisation, strengthening of programme management and, most importantly, reorienting of surveillance.6 The collection and reporting of data on malaria cases and deaths are critical elements for elimination in a successful surveillance system. High quality, reliable information reporting systems are a requirement for malaria elimination to ensure that all cases are tested, treated and tracked to avoid further transmission.7
In Botswana, the National Malaria Programme (NMP) currently relies on two independent surveillance systems for tracking malaria: the Integrated Disease Surveillance and Response (IDSR) system and the case-based surveillance (CBS) system. Botswana adopted the IDSR system according to the World Health Organization (WHO) Regional Committee for Africa 1998 recommendation, with the goal of tracking all epidemic-prone diseases and important public health conditions.8 The IDSR has been the mainstay for passive malaria surveillance, with weekly reporting on basic indicators, and it is the primary source of information for locating malaria cases and prompting action nationwide.
As part of the requirements for surveillance in malaria elimination countries, the CBS system was introduced in 2012 in all districts to report on the malaria elimination indicators. CBS captures data on every positive malaria case, which leads to an immediate investigation at household level and detection of other possible associated cases. While IDSR and CBS are uniquely different reporting systems for malaria deployed in parallel, they complement one another: IDSR contains information on the total number of malaria cases diagnosed (confirmed and unconfirmed) and deaths, and serves as an early warning system, while CBS reports details on confirmed malaria cases only, looking specifically at demographic characteristics, epidemiological and entomological data and other information helpful for the detection of possible cases that might have arisen from the index case.
Although the two systems should have equivalent numbers for the total number of confirmed cases and deaths, they frequently produce different results, with the CBS system reporting fewer cases than the IDSR, which is taken as the gold standard. No studies have previously compared these two systems for malaria elimination programmes in Africa. It is therefore imperative to evaluate the CBS system against the IDSR in Botswana, to identify gaps that need to be addressed. Without further improvement and strengthening of the reporting systems, malaria elimination will likely be unachievable, as late reporting and investigation will lead to missing cases, resulting in onward transmission.
The aim of the present study was to evaluate the uptake of the new malaria CBS system in comparison to the IDSR system for the completeness and quality of malaria data reported between 2013 and 2014 in Botswana. Specific objectives were 1) to compare the number of malaria cases reported through the IDSR and CBS systems for nationwide data (2013–2014), 2) to assess the completeness and quality of data reported via the CBS system in the three districts with the heaviest malaria burden (2013–2014), and 3) to determine the characteristics of cases with missing data reported via the CBS system in these three districts (2013–2014).
METHODS
Study design
This was a retrospective, descriptive study using previously collected routine health facility and district data.
Setting
Botswana is a landlocked country of about 582 000 km2 that shares borders with Namibia, South Africa, Zimbabwe and Zambia. In 2011, the country had a population of approximately 2 million. The population is generally young, with a mean age of 26.2 years, and is urbanising, with 62% currently living in urban areas; 18% live in malaria high-risk areas.9 Malaria transmission usually occurs between October and May, with the majority of cases reported in January each year, and a peak in February.
The study was conducted using nationwide available data and focused on the three districts with the highest malaria burden, Okavango, Ngami and Chobe, located in northern Botswana.
Case-based surveillance
The NMP is responsible for the overall coordination of malaria surveillance, monitoring and evaluation; advocacy and information, education and communication (IEC); case management; and vector control.8 CBS has an immediate notification system that plays the role of triggering an immediate response, tracking all positive malaria cases from diagnosis to investigation at household level. CBS has disaggregated detailed individual malaria case reporting, and is used in all districts in Botswana to provide detailed information on all local and imported malaria cases and deaths.6 The primary diagnostic tool for malaria is rapid diagnostic testing (RDT), which is performed in all of the facilities (hospitals, clinics and health posts), and not in the laboratories. RDT is available in consultation rooms at all levels. When an RDT result is positive, the protocol should be recorded in the IDSR and the patient should be notified immediately through the CBS system. The reporting tools for both CBS and IDSR are also available at all health facilities.
Health officers at health facilities and in the communities collect data through both passive and active surveillance through the IDSR and CBS systems. In consultation rooms, there is a tally sheet that feeds both the IDSR reporting tool and the CBS reporting tools. Once a patient is clinically diagnosed or confirmed through RDT as having malaria, the case is recorded in a tally sheet, which is then used to compile the weekly IDSR report. The case is then reported immediately via the CBS forms. Active surveillance is conducted by a team of health workers, including facility nurses, who travel with the CBS data collection tools, through which they immediately notify cases while they are working in the field. The same clinicians in the health facilities then collate the collected data. Subjects identified by the CBS system are entered in the IDSR, as they are tallied in both systems. The data source is the facility-based tally sheets, which capture both unconfirmed and confirmed malaria cases. As the figures reflect confirmed malaria cases, the figures from the IDSR and CBS should tally. The IDSR reports confirmed and unconfirmed cases separately, and the definition of confirmed cases is the same in the IDSR and CBS.
In the analysis, only data on confirmed cases were extracted from the IDSR so as to be able to make a proper comparison of information collected in the two systems. It is expected that the same number of cases would be obtained from both systems. ‘Correct data’ refers to data required by the CBS system, and ‘missing data’ refers to empty fields where data were not filled in. All confirmed cases logged in both systems and included in the present study underwent parasitological testing.
Once an individual is confirmed as being positive for malaria through RDT or microscopy at a health facility, a case is immediately reported to the district health management team (DHMT) and the NMP. The same case is then recorded in the out-patient department (OPD) register (MH1048). The case is expected to be investigated at household level within 48 h, with contact screening performed to prevent secondary transmission.
Integrated Disease Surveillance and Response
The IDSR serves as an early warning system for all epidemic-prone diseases in the Ministry of Health (MoH). Data on aggregated unconfirmed and confirmed malaria cases and deaths from all 29 districts are entered into the IDSR on a weekly basis. At facility level, all patients, i.e., unconfirmed cases, confirmed cases and deaths, are tallied in the OPD register. Thus, once a case is confirmed as a true (RDT or microscopically diagnosed) or clinically diagnosed malaria case, this is recorded. A weekly summary of the OPD register at each health facility is completed using the IDSR tool, then the DHMT summarises the health facility reports and sends them on to the IDSR unit in the MoH. Because the CBS system is directly linked to the IDSR reporting system, both systems should report equivalent numbers of malaria cases.
Data validation
All patients diagnosed with malaria from 1 January 2013 to 31 December 2014 were included in the study. Data variables were extracted from the IDSR, which is accessible at district level. CBS data variables for each patient included basic sociodemographic information, date of diagnosis, date of reporting, date of case investigation and case classification, including indigenous, imported and unclassified cases. The variables from each surveillance system were then compared to measure the level of agreement.
Analysis and statistics
The selected data were imported into an EpiData database and analysed (v. 3.1 for entry and v. 2.2.2.182 for analysis, EpiData Association, Odense, Denmark). Summary descriptive statistics were completed, including the χ2 test for categorical variables and the t-test for continuous data. A two-tailed P ⩽ 0.05 was used for statistical significance.
Ethical considerations
Ethics approval was obtained from the Research Unit of the Botswana Ministry of Health (Gaborone, Botswana) and the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease (Paris, France).
RESULTS
In 2013, 456 malaria cases were reported in the IDSR and 305 in the CBS (Figure). There was a significant increase in the number of cases reported in each system in 2014: 1346 in the IDSR and 884 in the CBS. The proportional difference between the reporting systems was not significantly different (33% for 2013 vs. 34% for 2014, P = 0.8).
FIGURE.
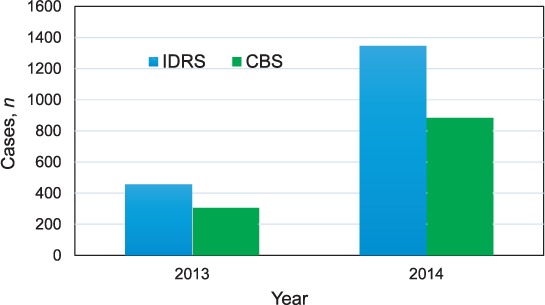
Number of malaria cases reported by the IDSR and CBS systems, Botswana, 2013–2014. IDSR = Integrated Disease Surveillance and Response; CBS = case-based surveillance.
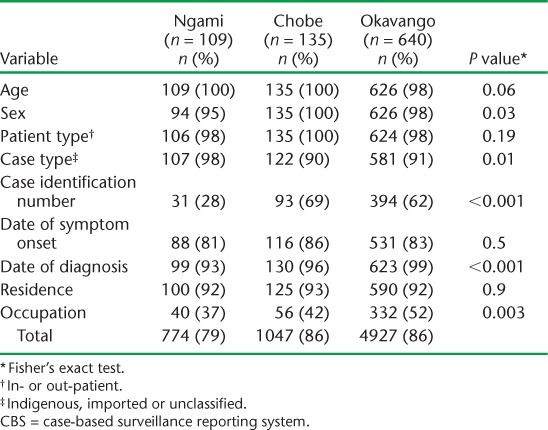
There were substantial differences in correctly reported data in the CBS for the three high-risk malaria districts, Ngami, Chobe and Okavango (Table 1). The greatest number of cases was reported by Okavango district (72%). The key malaria reporting indicators with the greatest variability in the districts of Ngami, Chobe and Okavango in proportion to correctly reported indicators were case identification number (respectively 28%, 69% and 62%, P < 0.001), case type (respectively 98%, 90% and 91%, P = 0.01) and date of diagnosis (respectively 93%, 96% and 99%, P < 0.001). Case identification was a challenge in all three districts, and was lower in Ngami district (28%) than in the other districts (both 60%). The remaining parameters were comparable in the three districts.
TABLE 1.
Proportion of correct data reported in the CBS by Ngami, Chobe and Okavango districts, Botswana, 2013–2014
Further analysis of the CBS data by reported malaria patient type (indigenous, imported from another country or unclassified) also revealed significant differences (Table 2). The case identification numbers had the greatest variability, and were correctly reported among indigenous cases only 61% of the time vs. 44% and 32% for imported and unclassified cases, respectively (P < 0.0001). Similar findings were noted for date of diagnosis, with cases reported correctly 88%, 83% and 84% of the time for indigenous, imported and unclassified cases, respectively (P < 0.0001).
TABLE 2.
Proportion of correct data reported in the CBS by patient classification in Ngami, Chobe and Okavango districts, Botswana, 2013–2014
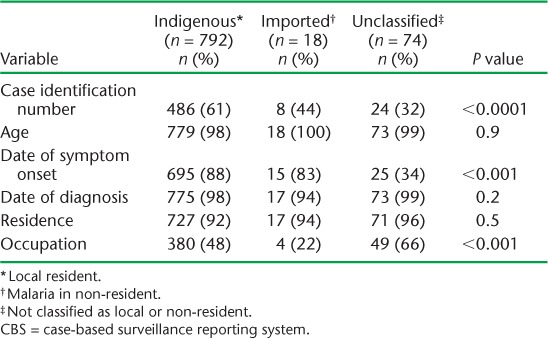
In the indigenous and imported groups, case identification and occupation were frequently not reported. Case identification was less likely to be reported in the unclassified group than the indigenous group (32% vs. 61%). Occupation was less likely to be reported in the imported group (22%) than in the indigenous (48%) and unclassified (66%) groups.
DISCUSSION
This is the first study to assess the performance of the two systems used for tracing malaria cases in Botswana. These findings are key to building on lessons learnt for Botswana and other countries planning for malaria elimination. The results showed significant variability in accuracy between the two systems. According to our analysis, approximately 33% fewer cases were reported in the CBS compared with the IDSR system. This is not surprising, as the CBS was only rolled out in 2012, while the IDSR has been implemented in Botswana since 2001; however, the need for both systems to report similar numbers of cases is fundamental in an elimination programme. Overall, these results highlight a significant gap in reporting accuracy and a crucial need to improve surveillance to meet the malaria elimination goal using a system that is able to detect and characterise all cases.
Further examination of the CBS data revealed that the quality of reporting was not satisfactory. Not all variables are consistently reported, and depended on district and patient type. For example, the case identification number, a critical value utilised for patient identification for further investigation, was reported in only 59% of cases. Thus, almost half of all reported cases in Ngami, Chobe and Okavango districts were missing this essential information. Without the case identification number, tracking and potential epidemiological linkage of cases is not possible, making elimination challenging, as it is difficult to know which cases notified in the CBS are index cases and which are secondary to the index cases. Correcting this pivotal error in the reporting system will require significant support and follow-up at the provider level.
Ngami district had more missing data than Okavango and Chobe districts. This was surprising, as Ngami has fewer cases than the other two districts. We would argue, however, that reporting in Ngami district is thus even more important, and that this district should be prioritised for receiving targeted enhanced support.
The findings from this study may have resulted from the fact that the IDRS and CBS systems are operated under the MoH Department of Public Health by different units, and therefore have different implementation mechanisms. The CBS has not yet been adequately appreciated by health workers, given its recent application countrywide, and health workers may not understand the importance of reporting through both systems, which they may see as duplication. Health workers may not be adequately trained in completing the CBS forms and, finally, the reporting forms may be too cumbersome.
Our findings are consistent with a 2013 study from Botswana, which concluded that to accurately monitor progress towards the goal of elimination, the NMP should strengthen the reporting and capturing of data at household and individual levels.10 However, no similar studies have been conducted in Africa, and other studies have focused primarily on the timeliness of reporting in an elimination programme and not on the completeness or quality of information. The missing parameters are key to identifying detected cases and ensuring that they are epidemiologically linked.
These findings have serious programmatic implications. First, frequent data audits are required to address the discrepancies between the IDSR and CBS data. Second, the NMP needs to conduct intensive training countrywide, with emphasis on correct form completion and exploring options for e-reporting formats, which might lead to improved compliance. These findings are also key to addressing the elimination challenges in Botswana that may be contributing to the persistent low-level transmission noted in the high-burden districts. Although the latter finding has not been systematically assessed, it would be worthwhile evaluating each factor and assessing its importance in sustaining malaria transmission.
The strengths of this study are the use of programme data that are submitted electronically via a standardised method. Furthermore, the study followed the Strengthening the Reporting for Observational Epidemiology (STROBE) guidelines.11 The selection of the three most affected districts for a detailed analysis was significant, as it allows for targeted future interventions that will likely lead to more rapid improvements and greater gains. Limitations of this study include the use of routinely collected programme data, which can have significant challenges.12 Finally, the selection of only three districts may have introduced bias, as these districts are currently receiving the most attention and are thus under frequent review.
CONCLUSION
In comparing the IDSR and CBS malaria reporting systems, both are confirmed to be critical components for malaria elimination. However, significant discrepancies remain that are likely to negatively impact the goal of malaria elimination in Botswana. The CBS system needs strengthening to improve reporting and allow better characterisation of malaria cases for adequate investigation. Progressive improvement should allow Botswana to reach its goal of malaria elimination.
Acknowledgments
This research was conducted through the Structured Operational Research and Training Initiative (SORT IT), a global partnership led by the Special Programme for Research and Training in Tropical Diseases at the World Health Organization (WHO/TDR, Geneva, Switzerland). The SORT IT programmes include a teaching component developed jointly by the International Union Against Tuberculosis and Lung Disease (The Union, Paris, France) and Médecins Sans Frontières (MSF, Geneva, Switzerland). The specific SORT IT programme that resulted in this publication was implemented by the WHO/TDR; the WHO Global Malaria Programme (GMP); WHO/African Region (AFRO); the Operational Research Unit (LuxOR), MSF, Brussels Operational Centre (Luxembourg); the Centre for Operational Research, The Union; University of Nairobi (Nairobi, Kenya); Global AIDS Interfaith Alliance (San Rafael, CA, USA); Academic Model Providing Access to Healthcare (AMPATH, Eldoret, Kenya); and Johns Hopkins University (Baltimore, MD, USA). The programme was funded by the WHO/TDR, WHO GMP and WHO/AFRO. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Conflicts of interest: none declared.
In accordance with WHO's open-access publication policy for all work funded by WHO or authored/co-authored by WHO staff members, the WHO retains the copyright of this publication through a Creative Commons Attribution IGO licence (http://creativecommons.org/licenses/by/3.0/igo/legalcode) that permits unrestricted use, distribution and reproduction in any medium provided the original work is properly cited.
References
- 1. Zhou S S, Zhang S S, Zhang L, . et al. China's 1–3–7 surveillance and response strategy for malaria elimination: is case reporting, investigation and foci response happening according to plan? Infect Dis Poverty 2015; 4: 55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization. . World malaria report, 2015. Geneva; Switzerland: WHO, 2015. [Google Scholar]
- 3. Botswana National Malaria Programme. . Extended malaria strategic plan, 2014–2018. Gaborone, Botswana: Ministry of Health, 2013. [Google Scholar]
- 4. Botswana National Malaria Programme. . National Malaria Programme database. Gaborone, Botswana: Ministry of Health, 2009. [Google Scholar]
- 5. World Health Organization. . Malaria elimination. A field manual for low and moderate endemic countries. Geneva, Switzerland: WHO, 2007. [Google Scholar]
- 6. Botswana National Malaria Programme. . Malaria diagnosis and treatment guidelines. Gaborone, Botswana: Ministry of Health, 2007. [Google Scholar]
- 7. Chihanga S, Haque U, Chanda E, . et al. Malaria elimination in Botswana, 2012–2014: achievements and challenges. Parasit Vectors 2016; 9: 99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ministry of Health. . Technical guidelines for Integrated Disease Surveillance and Response in Botswana. Gaborone, Botswana: Ministry of Health, 2010. [Google Scholar]
- 9. Statistics Botswana. . Housing and Population, Census 11: preliminary results briefs. Gaborone, Botswana: Statistics Botswana, 2011. [Google Scholar]
- 10. Lourenço C, Kandula D, Haidula L, Ward A, Cohen J M.. Strengthening malaria diagnosis and appropriate treatment in Namibia: a test of case management training interventions in Kavango region. Malar J 2014; 13: 508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. von Elm E, Altman D G, Egger M, . et al. The STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370: 1453– 1457. [DOI] [PubMed] [Google Scholar]
- 12. Chihanga S, Moakofhi K, Mosweunyane T, . et al. Malaria control in Botswana, 2008–2012: the path towards elimination. Malar J 2013; 12: 458. [DOI] [PMC free article] [PubMed] [Google Scholar]


