Abstract
Background: Swaziland is one of the southern African countries that aim to eliminate malaria by 2020. In 2010, the country introduced an Immediate Disease Notification System (IDNS) for immediate reporting of notifiable diseases, including malaria. Health facilities are to report malaria cases within 24 h through a toll-free telephone number (977), triggering an alert for case investigation at the patient's household within 48 h. We assessed the completeness of reporting in the IDNS, the subsequent case investigation, and whether it was done within the stipulated timelines.
Methods: A cross-sectional study using routine country-wide data.
Results: Of 1991 malaria cases notified between July 2011 and June 2015, 76% were reported in the IDNS, of which 68% were investigated—a shortfall of 24% in reporting and 32% in case investigations. Of the 76% of cases reported through the IDNS, 62% were reported within 24 h and 20% were investigated within 48 h. These shortcomings were most pronounced in hospitals and private facilities. Investigated cases (n = 1346) were classified as follows: 60% imported, 35% local and 5% undetermined.
Conclusion: The utilisation of the IDNS for case reporting to trigger investigation is crucial for active surveillance. There is a need to address the reporting and investigation gaps identified to ensure that malaria cases receive appropriate interventions.
Keywords: immediate reporting, response, malaria surveillance
Abstract
Contexte: Le Swaziland est l'un des pays d'Afrique australe visant à éliminer le paludisme d'ici 2020. En 2010, le pays a introduit un système de déclaration immédiate des maladies notifiables (IDNS), dont le paludisme. Les structures de santé doivent déclarer les cas de paludisme dans les 24 h grâce à un numéro de telephone gratuit (977), qui déclenche une alerte pour l'investigation des cas dans leur domicile dans les 48 h. Nous avons évalué la complétude des déclarations dans l'IDNS, l'investigation qui a suivi et si elle a eu lieu dans les délais impartis.
Méthodes : Une étude transversale basée sur des données de routine nationales.
Résultats : Il y a eu 1991 cas de paludisme entre juillet 2011 et juin 2015, dont 76% ont été déclarés dans l'IDNS et 68% d'entre eux ont fait l'objet d'une investigation—un déficit de 24% dans la déclaration et 32% pour l'investigation des cas. Sur les 76% déclarés à travers l'IDNS, 62% ont été déclarés dans les 24 h et 20% ont eu une investigation dans les 48 h. Ces lacunes ont été plus prononcées dans les hôpitaux et les structures privées. Des 1346 patients qui ont eu une investigation, 60% étaient classifies comme cas importés, 35% comme cas locaux et 5% indéterminés.
Conclusion : L'utilisation de l'IDNS pour la déclaration des cas afin de déclencher l'investigation est cruciale pour la surveillance active. Il est nécessaire d'examiner les lacunes identifiées en termes de déclaration et d'investigation afin de s'assurer que les cas bénéficient des interventions appropriées.
Abstract
Marco de referencia: Swazilandia es uno de los países del sur de África que se proponen eliminar el paludismo hacia el 2020. En el 2010, se introdujo en el país un Sistema de Notificación Inmediata de Enfermedades (IDNS, por Immediate Disease Notification System) con el objeto de notificar de inmediato las enfermedades de declaración obligatoria como el paludismo. Los centros de atención de salud deben notificar los casos de paludismo en las primeras 24 h, por conducto de una llamada telefónica sin costo (977), que desencadena una alarma para la investigación del caso en su domicilio en menos de 48 h. En el presente estudio se evaluó el carácter integral de las notificaciones al IDNS, la posterior investigación de los casos y el cumplimiento del cronograma estipulado.
Métodos: Un estudio transversal a partir de los datos corrientes de ámbito nacional.
Resultados: De julio del 2011 a junio del 2015 se presentaron 1991 casos de paludismo, de los cuales se notificó el 76% al IDNS y se investigó el 68% de ellos, es decir una deficiencia de 24% en la notificación y de 32% en la investigación de casos. Del 76% de casos notificados al IDNS, el 62% se informó en las primeras 24 h y el 20% se investigó en las primeras 48 h. Las deficiencias fueron más marcadas en los hospitales y los establecimientos privados. Los casos investigados (n = 1346) se clasificaron en 60% importados, 35% locales y 5% indeterminados.
Conclusión: La utilización del IDNS en la notificación de los casos con el objeto de desencadenar la investigación es un aspecto fundamental de la vigilancia activa. Es necesario actuar frente a las fallas detectadas en la notificación y la investigación, de manera que todos los casos reciban las intervenciones apropiadas.
There were an estimated 214 million new malaria cases worldwide in 2014, with 438 000 deaths, mostly in sub-Saharan Africa.1 In 2007, the Southern Africa Development Community (SADC) identified six countries as having the greatest potential to eliminate malaria by 2015: Botswana, Namibia, South Africa, Swaziland, and the island states of Zanzibar and Madagascar.2 Botswana, Namibia, South Africa and Swaziland, considered the front-line countries, are well positioned to accelerate towards elimination within southern Africa. To successfully eliminate malaria, these four countries need to collaborate closely with their neighbours to the north—Angola, Mozambique, Zambia and Zimbabwe—which face a higher transmission burden. These are considered second-line countries, and will follow suit in malaria elimination to lay the foundation for the gradual expansion of malaria-free areas within the SADC.3 The term ‘malaria elimination’ is defined as the interruption of local mosquito-borne malaria transmission in a defined geographic area, leading to no locally contracted cases. Sustained malaria control interventions are still required to tackle imported cases, which may continue to occur.4
In 2009, the Swaziland National Malaria Control Programme (NMCP) launched an active surveillance programme aiming at investigating all confirmed malaria cases within 7 days. To support this initiative, in August 2010, the Ministry of Health introduced an Immediate Disease Notification System (IDNS) to enhance emergency preparedness and response at national level. The IDNS serves as an early warning system that captures data on all diseases with epidemic potential, including malaria, to enable timely appropriate response, and is managed by the Epidemic Preparedness and Response (EPR) department. All health facilities in the country are obliged to document and report all confirmed malaria cases, tested by rapid diagnostic testing (RDT) or microscopy, immediately or within 24 h to the IDNS through the toll-free 977 telephone number.5 This provides an alert for new malaria cases, which then triggers rapid case investigation for instituting control measures. In addition, malaria surveillance agents routinely visit health facilities in their respective catchment areas to search for unreported confirmed malaria cases in case registers, request health care workers to report the case(s) to the IDNS and attempt case investigation.
In July 2011, the NMCP conducted its mid-term review of the 2008–2015 Strategic Plan and updated its investigation target from within 7 days to within 48 h of confirmation. Malaria surveillance agents were to attempt to conduct an investigation within 48 h of receiving the notification or identifying a case from a health facility register. If they are able to trace the patient and administer the case investigation questionnaire, the case is classified as ‘investigated’. If they are unable to trace the patient for whatever reason, the case is classified as ‘unsuccessfully investigated’. The sequence of events from malaria confirmation at health facility level to case investigation at household level is shown in the Figure.5
FIGURE.
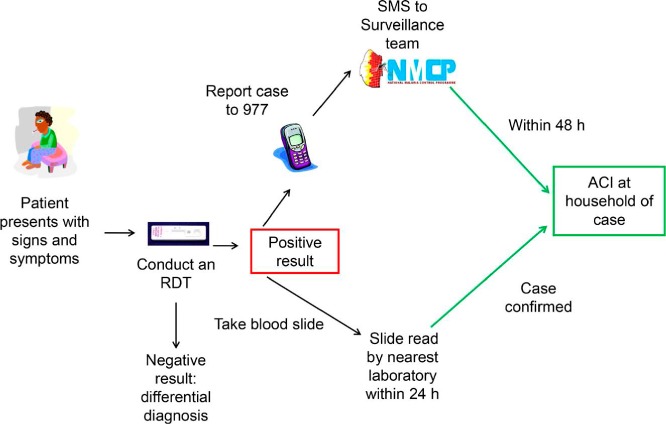
Malaria case diagnosis, reporting and investigation flow diagram. The sequence of events from malaria confirmation at health facility level to case investigation at household level in Swaziland. SMS = short message service; ACI = active case investigation; RDT = rapid diagnostic testing. Source: Swaziland malaria surveillance manual.5
Efficient information transfer between the health facility and the IDNS, leading to case investigation, is vital to ‘shrink the malaria map’ in Swaziland and maintain progress made towards malaria elimination.3 In 2011, the World Health Organization (WHO) Malaria Programme Review (MPR) suggested possible gaps in information transfer from health facilities to the programme through the IDNS system.6 Despite being an identified operational research priority for the front-line countries, to date there has been no formal performance assessment of the timeliness of reporting through the IDNS in Swaziland and the subsequent case investigation at household level. Furthermore, a literature review did not reveal any publications assessing such a system performance in any malaria-elimination country. We thus aimed to assess the reporting of malaria cases through the IDNS in Swaziland, their subsequent investigation and the timeliness of each of these parameters.
For all health facilities in the country, and for the period from July 2011 to June 2015, our specific objectives were to evaluate 1) the number of confirmed malaria cases reported to the IDNS and the type of health facility where they were reported, 2) the number of confirmed malaria cases reported to the IDNS that were investigated, and 3) the proportion of confirmed malaria cases reported to the IDNS within 24 h that were subsequently investigated within 48 h of confirmation, in accordance with surveillance guidelines.
METHODS
Study design
This was a cross-sectional study using routine country-wide malaria programme data.
General setting
Swaziland is a landlocked country bordered by Mozambique to the east, a malaria-endemic country, and South Africa. The country's population is estimated at 1040000.7 Swaziland has a total of 287 health facilities: 43% in Manzini region, 29% in Hhohho, 16% in Lubombo and 12% in Shiselweni. According to the 2013 National Service Availability Mapping (SAM), 235 (82%) public and private health facilities offer malaria diagnosis based on RDT and/or treatment. A total of 14 (5%) have the capacity for microscopy.8 Certain areas in the Hhohho and Lubombo regions are considered to be malaria outbreak-prone (receptive areas) as they have sufficient vector populations and favourable environmental conditions for mosquito breeding and further malaria transmission. Most local cases emanate from these areas, which are home to 30% of the Swazi population.8 Local cases are defined as infections assumed to be acquired within the boundaries of the country, with the affected patient reporting not to have travelled to a malaria-endemic area within 2 months preceding the onset of symptoms.
Specific setting: Swaziland Malaria Control Programme
The Swaziland NMCP is comprised of four thematic areas: 1) case management, 2) vector control, 3) health promotion and 4) surveillance, epidemic preparedness and response. These departments work collectively toward implementation of the activities laid out in the 2015–2020 National Malaria Elimination Strategic Plan.9 Immediate reporting and case investigation fall under the surveillance, epidemic preparedness and response thematic area.
Passive and active surveillance system in Swaziland: the Immediate Disease Notification System and the Malaria Surveillance Database System
As malaria is a notifiable disease in Swaziland, all malaria cases confirmed at health facility level must be reported immediately through the IDNS system (Figure).5 Health care workers complete a standardised IDNS form collecting the required patient details, which include contact information to enable active case investigation and travel history for case classification. Once the health care worker has completed the IDNS form, he/she must immediately (within 24 h) report the case to the IDNS by dialling the toll-free number (977) using a landline or cell phone. Once the case has been entered into the IDNS, a short message service (SMS) is sent to a malaria surveillance agent in the relevant catchment area, and the agent then attempts to conduct active case investigation at household level within 48 h. The trained malaria surveillance agent visits the patient's household to gather information on sociodemographic characteristics, treatment progress, travel history, and access/utilisation of vector control and personal protection measures.5
This investigation gathers information to 1) classify the case (local or imported), and 2) identify factors that may be associated with transmission risk and which can be acted upon. The entire process from malaria confirmation to case investigation should be completed within 48 h. Timing is vital to ensure that every confirmed malaria case is investigated and intervention measures are promptly instituted to prevent ongoing transmission.10
Malaria-related information, which includes active case investigation data, is captured and stored in the Malaria Surveillance Database System (MSDS). This is a comprehensive database designed for malaria elimination activities that captures data on all malaria interventions and includes information on confirmed malaria cases at health facility level that may or may not have been reported to the IDNS. Discrepancies in the numbers of malaria cases recorded in the MSDS and the IDNS arise when cases from the health facility level are not reported to the IDNS. Information collected from case investigations by surveillance agents is recorded into a tablet computer that directly feeds information into the web-based MSDS system. Ideally, the data in the IDNS should match those contained in the MSDS, which is housed and managed by the NMCP.
Study sites
The study sites were all health facilities in the country that diagnose and treat malaria cases in Swaziland. Clinics treat out-patient cases and refer severe cases to in-patient facilities; health centres treat out-patient cases and have limited in-patient facilities; hospitals offer both in- and out-patient services.
Study population
All confirmed cases of malaria presenting to health facilities across the country from July 2011 to June 2015 were included. The study was conducted between June 2015 and January 2016.
Data variables, sources of data and validation
Data variables related to the study objectives were sourced from the MSDS and IDNS databases. Standardised IDNS data collection forms and active case investigation forms were used to gather data. The number of confirmed cases in the MSDS was used as the denominator for assessing the number and proportion reported in the IDNS. The times to reporting in the IDNS and to case investigation were sourced from the MSDS.
Statistical analysis
Data were entered into EpiData software for analysis (v. 3.1 for entry and v. 2.2.2.183 for analysis, EpiData Association, Odense, Denmark). Descriptive analysis was used to compare the groups.
Ethics
Ethical approval of the study protocol was received from the Swaziland Ethics Committee of the Ministry of Health (Mbabane, Swaziland) and the Ethics Advisory Group of the International Union Against Tuberculosis and Lung Disease (Paris, France). As the data used for the study were routine and anonymised, informed patient consent was not necessary.
RESULTS
Reporting of confirmed malaria cases in the IDNS and case investigation
Table 1 shows the confirmed malaria cases that were reported in the IDNS and subsequently investigated. Of 1991 confirmed malaria cases, 76% were reported in the IDNS and 68% were investigated. This represents a shortfall of 24% in IDNS reporting and 32% in case investigations. This shortcoming was observed in all geographic regions of Swaziland, but was more pronounced in hospitals and private health facilities.
TABLE 1.
Cascade analysis of total confirmed malaria cases reported in the MSDS, reported in the IDNS and subsequently investigated in Swaziland, 2011–2015
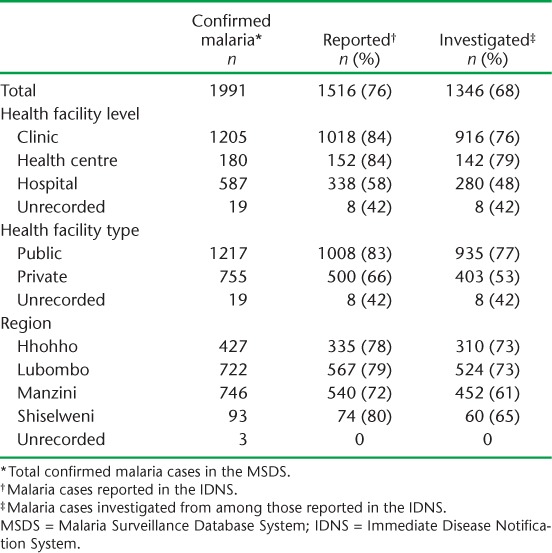
Classification of the 1346 investigated cases showed that 60% of the cases were imported, 35% were local and 5% were undetermined.
Proportions reported in the IDNS within 24 h and investigated within 48 h of malaria confirmation
Of the 1991 confirmed malaria cases, only 66% were reported to the IDNS within 24 h and only 20% of investigations were conducted within 48 h, the stipulated time thresholds for reporting and case investigation, respectively (Table 2).
TABLE 2.
The proportion of confirmed malaria cases reported within 24 h * to the IDNS and investigated within 48 h * in Swaziland, 2011–2015
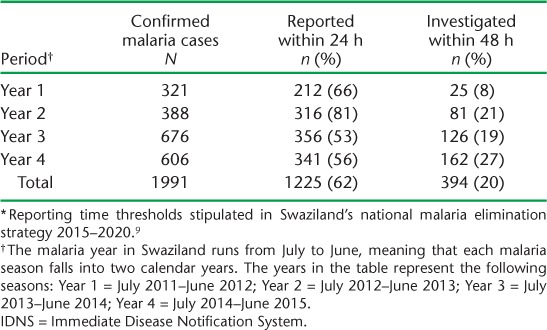
Twenty-five per cent of the cases reported within 24 h were investigated within 72 h, while the overall mean time for an investigation to be completed was 6 days.
Of the 1516 malaria cases reported to the IDNS and included in the analysis, 182 cases had missing or erroneous dates and could not be assessed for timeliness of reporting to the IDNS. These were considered as not having met the time threshold.
DISCUSSION
This is the first study from southern Africa to assess an immediate disease notification (early warning) information system for malaria elimination. Although the system is functioning, considerable shortfalls were noted in both the reporting and the investigation of malaria cases.
This study is important, as failure to immediately report and investigate incident malaria cases may result in onward transmission, and open the door to possible epidemics in areas with transmission potential. In a country nearing malaria elimination, such an eventuality could reverse the progress made toward malaria elimination. Systems need to be implemented and strengthened to allow optimal operation.
The study strengths include the following: all health facilities in the country were included, and thus the study is nationally representative; data on confirmed malaria cases were sourced from the MSDS, which is the most comprehensive database on malaria in the country; and the data spanned a time period of four malaria seasons. The study is also in line with an identified operational research priority for southern Africa, and we adhered to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.11
The study has a number of important policy and practice implications. First, we observed significant shortcomings in IDNS reporting, with more than one third of all confirmed cases not reported on time (within 24 h). This is likely due to underutilisation of the 977 toll-free telephone number by health facilities. Possible reasons for this may include health worker apathy, breakdown of the IDNS and/or the telecommunications networks and overworked health workers failing to call 977. There may also be a misconceived perception that entering data in the routine health facility reporting system, the Health Management Information System (HMIS), will automatically feed into the IDNS. A qualitative assessment needs to be conducted to verify reasons for non-reporting of cases within the stipulated time period.
Second, almost three in 10 malaria cases reported through the IDNS were not investigated. These are often classified as ‘unsuccessful investigations’. Although an attempt is made by the surveillance agent to investigate the case, there could be a number of obstacles, ranging from missing/inaccurate data provided or captured for the reported case, to the case leaving the country after treatment, to the case refusing to be investigated. Possible methods of addressing these challenges include increasing patient and health worker awareness about the public health importance of collecting and providing accurate patient details, including place of residence and contact information.
Third, 80% of the cases reported in the IDNS were not investigated within the stipulated 48 h. Achieving timely case investigation is a public health priority for Swaziland to enable an understanding of the origin of infection to inform the intervention response. An anecdotal review of IDNS case records shows varying levels of data completeness in identifying the exact geographic location of cases and their contact details. Failure to enter such data correctly results in surveillance agents having to make additional enquiries before initiating case investigations. This process often requires more than 48 h, leading to delays or unsuccessful investigations. Another reason for delays in case investigation is the surveillance agents' 5-day work week, whereby cases reported on weekends or public holidays have to wait until the next working day for follow-up. A possible solution would be to intensify mentoring and in-service training by the programme to strengthen the quality of patient data collected and ensuring that a surveillance team is available to respond to cases on all days of the week. The latter point should be an operational priority.
Fourth, the gaps in IDNS reporting and case investigation were most pronounced in hospitals and private health facilities. We attribute this finding to the fact that hospitals often have overworked staff who have multiple clinical responsibilities that take priority over reporting requirements. A lack of clear guidelines on who is responsible for reporting to the IDNS in hospital settings may have accentuated the reporting problems. Some private facilities do not adhere to the malaria diagnosis and treatment guidelines, causing delayed detection of cases by programme officers.12 Refresher in-service training and methods for fostering co-ownership and shared responsibility with health facilities are needed. Closer collaboration between hospital staff who admit malaria cases to the wards and malaria surveillance agents is also important, as this would allow the case investigation to be initiated before a patient is discharged, to allow for the timely roll-out of the required response strategies. To ensure compliance with the national reporting requirements in legislation and guidelines, special attention should be devoted to engaging and motivating private health practitioners.
Fifth, Swaziland is a small country, with much cross-border movement. Patients with malaria may thus be treated in a health facility in the country but then immediately return to their country of residence. This makes case investigation impossible without the introduction of a cross-border reporting and tracking system. One option for obtaining the necessary information would be to train health care workers to ask all patients with malaria if they intend to travel in the near future and, if so, to ask for their travel destination and contact details (telephone and address) to enable case investigation via telephone.
Finally, although Swaziland has set a target of 48 h for case investigation, in other countries, such as China, the target is 72 h. China managed to conduct case investigations for 97% of all malaria cases using this threshold (compared to 20% in our setting) after rolling out their elimination strategy.13 Although reporting and response trends in Swaziland have improved over the years, strengthening programmatic operations and laying the groundwork beforehand is essential to enable the timelines to be met. There is, however, a clear need to conduct more assessments on how to improve the investigation rate to better inform response strategies. Lessons can be learnt from other countries that are successfully implementing investigation programmes.
This study also had some limitations. There were missing data, albeit minimal, on some variables (health facility level, type and region), and about 12% of reported data in the IDNS had missing or erroneous dates. These data errors were seen mostly in the early stages of utilisation of the system, and data entry and quality has since improved.
CONCLUSION
This assessment has shown that although health facilities are utilising the IDNS, it is critical that the reporting rates be improved, especially in health facilities in receptive areas, to ensure that all cases are investigated in accordance with national surveillance policy. A surveillance system is only as useful as the response it elicits. All cases can be reported, but if there is delayed or no response, then the system in place does not fully serve its purpose.
Acknowledgments
This research was conducted through the Structured Operational Research and Training Initiative (SORT IT), a global partnership led by the Special Programme for Research and Training in Tropical Diseases at the World Health Organization (WHO/TDR, Geneva, Switzerland). SORT IT programmes include a teaching component developed jointly by the International Union Against Tuberculosis and Lung Disease (The Union, Paris, France) and Médecins Sans Frontières (MSF, Geneva, Switzerland). The specific SORT IT programme that resulted in this publication was implemented by the WHO/TDR, the WHO Global Malaria Programme (GMP), the WHO/African Region (AFRO), the Operational Research Unit (LuxOR), MSF (Brussels Operational Centre, Luxembourg); the Centre for Operational Research (The Union), University of Nairobi (Nairobi, Kenya), Global AIDS Interfaith Alliance (San Rafael, CA, USA), Academic Model Providing Access to Healthcare (AMPATH, Eldoret, Kenya) and Johns Hopkins University (Baltimore, MD, USA). The programme was funded by WHO/TDR, WHO GMP and WHO/AFRO. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Conflicts of interest: none declared.
In accordance with WHO's open-access publication policy for all work funded by WHO or authored/co-authored by WHO staff members, the WHO retains the copyright of this publication through a Creative Commons Attribution IGO licence (http://creativecommons.org/licenses/by/3.0/igo/legalcode) that permits unrestricted use, distribution and reproduction in any medium provided the original work is properly cited.
References
- 1. World Health Organization. . World malaria report, 2015. Geneva, Switzerland: WHO, 2015. http://www.who.int/malaria/publications/world-malaria-report-2015/report/en/ Accessed December 2017. [Google Scholar]
- 2. Southern Africa Development Community. . Malaria strategic framework, 2007–2015. Gaborone, Botswana: SADC, 2007. [Google Scholar]
- 3. Elimination 8. . Elimination 8 strategic plan: 2015–2020. Windhoek, Namibia: Elimination 8 Secretariat, 2015. http://www.shrinkingthemalariamap.org/files/content/resource/attachment/E8%20Strategic%20Plan%20(2015-2020).pdf Accessed December 2017. [Google Scholar]
- 4. Feachem R G A, Phillips A A, Targett G A, . et al. Shrinking the malaria map: a guide to malaria elimination for policy makers. San Francisco, CA, USA: Global Health Group, University of California San Francisco, 2009. http://core.ac.uk/download/pdf/11307280.pdf Accessed December 2017. [Google Scholar]
- 5. Swaziland National Malaria Control Programme. . Surveillance manual. Mbabane, Swaziland: Ministry of Health, 2014. [Google Scholar]
- 6. Swaziland National Malaria Control Programme. . Malaria programme review report. Mbabane, Swaziland: Ministry of Health, 2011. [Google Scholar]
- 7. Swaziland Central Statistics Office. . Statistics highlights. Mbabane, Swaziland: Swaziland Central Statistics Office, 2015. http://www.swazistats.org.sz/ Accessed December 2017. [Google Scholar]
- 8. Swaziland National Malaria Control Programme. . Annual report 2012–2013. Mbabane Swaziland: Ministry of Health, 2013. [Google Scholar]
- 9. Swaziland National Malaria Control Programme. . National malaria strategic plan, 2015–2020. Mbabane, Swaziland: Ministry of Health, 2014. [Google Scholar]
- 10. Swaziland National Malaria Control Programme. . National malaria strategic plan 2008–2015. Mbabane, Swaziland: Ministry of Health, 2008. [Google Scholar]
- 11. von Elm E, Altman D G, Egger M, . et al. The STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007; 370: 1453– 1457. [DOI] [PubMed] [Google Scholar]
- 12. Swaziland National Malaria Control Programme. . Malaria diagnosis and treatment guidelines. Mbabane, Swaziland: Ministry of Health, 2014. [Google Scholar]
- 13. Zhou S S, Zhang S S, . et al. China's 1–3–7 surveillance and response strategy for malaria elimination: is case reporting, investigation and foci response happening according to plan? Infect Dis Poverty 2015; 4: 55. [DOI] [PMC free article] [PubMed] [Google Scholar]


