Summary
Background
Past researches have shown that schoolteachers’ (STs) interventions maximize the consent for vaccination programs. European data regarding knowledge, attitudes and practices of STs towards vaccination are otherwise lacking.
Objectives
The aim of this study was therefore to evaluate knowledge and attitudes of STs regarding vaccinations in a sample from North Italy.
Material and methods
In this cross sectional study, 154 STs from Lombardy region (Northern Italy) responded to a specific questionnaire assessing their attitude towards vaccination and vaccine related knowledge.
Results
In general, 88.3% of subjects were somehow favourable to vaccinations. The main reason for declining vaccination was the risk of side effects whereas the main reason to be vaccinated was to avoid to be infected by VPDs (67.6%). Main information sources were health professionals (75.3%), and new media (13.1%), and the latter were STs more frequently associated with a negative attitude towards vaccinations (p < 0.001). Eventually, regression analysis identified risk perception as positively associated with propensity towards vaccinations, both for Students- and STs-recommended vaccinations (B = 0.372, 95% CI 0.247 to 0.496 and B = 0.005, 95%CI 0.004 to 0.006, respectively).
Conclusions
Our results are consistent with previous reports suggesting a significant knowledge gap in STs, with the risk perception of infectious diseases as the main predictor for vaccine propensity. Moreover, the better knowledge of official vaccination recommendations and policies among STs identifying Health Professionals as information source enlightens the role of the School Physicians and Occupational Physicians, whose intervention may ultimately increase the vaccination acceptance and vaccination rates.
Keywords: Immunization, Vaccination recommendation, Vaccine preventable disease, School environment, Vaccine hesitancy
Introduction
Vaccinations have been repetitively acknowledged as a major tool for reducing the burden of infectious diseases and decreasing their related morbidity, mortality and healthcare costs [1-6]. In order to endure over time vaccination rates required by immunizations with the purpose to retain their efficiency [7], specific recommendations have to be progressively updated by competent Public Health Authorities [3, 4, 8-13]. In Italy, for example, official recommendations are issued by the Ministry of Health issues through the National Immunization Prevention Plan (in Italian, Piano Nazionale di Prevenzione Vaccinale, PNPV), a guidance document for immunization policies [11], listing vaccines actively offered free of charge to the general population, to high-risk subjects, as well as to certain occupational groups [11, 14, 15].
Sound evidence, built on previous studies from various occupational settings, suggests that the spreading of information across occupational groups may be affected by significant gaps and diffuse misconceptions. For instance, workers may be actually unaware that they are targeted by specific vaccination policies, or may receive incomplete and inappropriate information by employers and healthcare providers such as the Occupational Physicians (OPh) or the General Practitioner (GP) [1, 5, 9-16]. Individuals affected by knowledge gaps are usually affected by higher shares of doubts about safety and benefits of vaccines, frequently questioning the need for them, ultimately delaying (i.e. vaccine hesitancy, VH) or refusing vaccination (i.e. vaccine refusal, VR) [6, 17-19]. VH and VR have become a significant public health issue, as many European countries, including Italy, are experiencing increasing difficulties in reaching and maintaining targeted vaccination rates [17-18]. As under-vaccinated individuals tend to cluster together, certain population groups may exhibit even lower vaccination rates, similar to that usually reported by middle income countries [18], being potentially vulnerable to VPDs outbreaks, and possibly epidemics [6, 19].
Because of their large population, high level of close social interaction, frequent personal contact among students, faculty and staff and their interface with the community, schools are workplaces having the potential to become outbreak centres for VPDs [7, 20-23]. Not coincidentally, school-based health programs have been appreciated among the most successful preventive approaches toward VPDs [24-27], significantly improving vaccination rates both in students and school employees (SEs) [28, 29]. In this regard, some analogies between SEs and healthcare workers (HCWs) may be identified. First at all, both HCWs and SEs work in settings at high risk of contracting VPDs and then transmitting the illness to others [21, 23, 30-32], involving also high-risk groups [33]. Second, they represent a significant occupational group in the adult population: recent estimates suggest that in Italy around 1 million people (i.e. 1.7% of total population and 2.6% of adults 18-67 years-old) are employed either as school teachers (STs) or school assistants (SAs). Third, both HCWs and STs are diffusely acknowledged as well trusted professionals. As the credibility of institution and professionals delivering information about vaccines is often more important than its content [34], they may be of significant relevance in the promotion of vaccine acceptance, also among subjects from difficult background (e.g. lower socioeconomic status).
In other words, appropriately informed STs can actively address individuals exhibiting VH because of inappropriate access to the facts or misinformation, and even vaccine objectors. On the contrary, STs sharing information deficits regarding vaccines and their official recommendations may ultimately hold and diffuse doubts or false beliefs about vaccines [34-37].
Knowledge, attitudes and personal beliefs (KAB) of STs towards immunizations have therefore the potential to significantly affect public health and occupational health [38-40]. Unfortunately, the abovementioned issues have been scarcely described, in particular in the European settings [21, 24-27]. In this questionnaire-based cross-sectional study, therefore, we aimed to assess knowledge of STs regarding vaccines and their official recommendations (i.e. knowledge of PNPV 2012-2014 recommendation) both in the paediatric age and for STs themselves, as well as their attitudes and personal beliefs, and whether knowledge and personal beliefs may be predictive of the personal attitude towards immunizations. In doing so, we sought to identify topics that may be target by specific and cost-effective formative and informative interventions.
Methods
PARTICIPANTS
The sample was collected between June and August 2016, and included STs from the provinces of Monza-Brianza and Brescia (2,130,181 out of 10,008,349 inhabitants of Lombardy Region, Northern Italy, at 2016 census) participating to a series of First Aid certification courses. Courses involved a total of 315 SEs from elementary, middle or high schools (i.e. secondary education, respectively of first and secondary grade) including 147 SAs and 168 STs. After the courses were completed and the First Aid certification achieved, STs from this initial sample having at least 6 months of seniority (n = 163, 97.0%) were invited to complete an anonymous questionnaire. As SAs usually don’t share the trust that public opinion deserves to STs, it is implausible that their KAB have the potential to influence the acceptance of vaccinations, and were therefore excluded from the survey.
INSTRUMENTS
Subjects giving their preliminary consent received by hand an anonymous and fully structured questionnaire inquiring attitudes and knowledge about vaccines and vaccinations. The questionnaire was a modified and adapted version of items previously developed for knowledge inquiry in the occupational settings [16, 41-43].
The questionnaire comprised 17 questions divided into 5 areas of inquiry:
Demographic data: age, sex, professional qualification, education level, household size and characteristics.
Attitudes toward vaccinations: participants’ attitude was initially assessed asking their agreement towards vaccination practice through a 5-point Likert scale (“strongly against vaccinations”, “somehow against vaccinations”, “neutral / no opinion”, “somehow favourable to vaccinations”, “strongly favourable to vaccinations”), then explaining why they would get vaccinated (i.e. “to avoid getting VPDs”, “to avoid transmitting VPDs”, “to avoid complications of VPDs”, “to avoid VPDs in subjects who cannot be vaccinated”) or rather would refuse a vaccine or hesitate towards vaccinations (i.e. “To avoid side effects of vaccinations”, “No trust in vaccines”, “Immunization by natural infections is more efficient”, “Fear of shots”, “Preference on other countermeasures”, “Vaccines are superfluous (i.e. natural immunity ultimately overcomes any infectious disease)”, “Vaccinations are against my personal beliefs (religious / ethical)”, “Vaccines are useless (i.e. vaccines are eventually unable to enhance natural immunity)”). Participants were then asked about their preferential information sources: TV/radio/newspapers, new media (i.e. wikis, blog, social media etc), friends, parents, school, health professionals.
Knowledge of official recommendations. Immunizations for sixteen VPDs were presented to the participants (i.e. diphtheria, tetanus, poliomyelitis, hepatitis B, pertussis, H influenzae type B, measles, rubella, parotitis, meningococcus C, pneumococcus, influenza, varicella, papillomavirus, hepatitis A, tuberculosis). For instance, PNPV 2012-2014 identified: (a) immunizations for paediatric age subjects, including 4 compulsory vaccinations for all newborns (i.e. diphtheria, tetanus, poliomyelitis and viral hepatitis B) and 9 recommended vaccinations (i.e. pertussis, Haemophilus influenzae type B, pneumococcus, meningococcus C, measles, parotitis, rubella, varicella, human papillomavirus); (b) immunizations for subjects working in the school environment, including 4 specifically recommended vaccination (i.e. measles, parotitis, rubella, varicella). Participants eventually indicated which ones of presented vaccinations were recommended by PNPV 2012-2014 in paediatric-age subjects (i.e. Students-recommended immunization) and/or in STs (i.e. STs-recommended immunization) (possible answers: “yes”, “no”, “don’t know”). As PNPV 2012-2014 recommendations for adults included that at least one of decennial boosters for tetanus and diphtheria incorporates acellular pertussis vaccine, and that subjects at occupational risk would receive vaccination against seasonal influenza (i.e. not only HCWs, but also subjects working in occupational settings at high risk for influenza, or whose sick leave during influenza season would severely impair public services), and both immunizations are recommended in SEs by the PNPV 2017-2019 [11, 15], they were also assessed among those recommended to STs. Knowledge score about official vaccine recommendations (KS-OR) was then calculated as the sum of correctly marked vaccines, separately for students and STs: when the participants correctly answered, +1 was added to a sum score [16].
General knowledge. The original knowledge test developed by Zingg [9] contains true-false statements such as “vaccinations increase the occurrence of allergies” (false) covering some typical misconceptions on vaccination. Both the original test and the revised version applied by Betsch and Wicker interpreted the sum of all incorrect answer as the degree of misconceptions held by the participant [9, 16]. In fact, this test successfully predicted influenza risk perceptions and vaccination intentions in previous studies [9, 16]. Briefly, a total of 13 statements were presented, including the 9 original items from Zingg questionnaire and 4 further items about vaccine misconceptions (i.e. “The addictive used in the vaccines are not dangerous for humans”; “Multiple Sclerosis may be induced by HBV vaccine”; “Neurological disorders are possible side effects of measles vaccine”; “Autism is more frequent in subjects vaccinated against measles”; “Diabetes mellitus may be triggered by vaccination shoots”; “Vaccinations increase the occurrence of auto-immune diseases”; “Vaccinations increase the risk for allergic disorders”; “Vaccine are superfluous, as infectious diseases can be always treated with antibiotics”; “Without massive vaccination programs, smallpox would still exist”; “The efficacy of vaccines has been extensively proven”; “Children would be more resistant to infections if they were not always treated against all diseases”; “Many vaccinations are administered too early. As results, the immune system has no possibility to fully develop by itself”; “The immune system of children may be overwhelmed by a high number of vaccines”; all statements presented as “True” / “False” / “Don’t know”). General knowledge score (KS-G) was then calculated as the sum of correctly marked recommendations, by adding +1 to the sum score when the participants correctly marked presented statements.
Risk perception. We inquired the risk perception of STs about all the 16 VPDs we presented. In particular, we asked the STs about they perceived the severity of the natural infection through a 5-point Likert scale (i.e. 0, “almost zero”; 1, “low”; 2 “moderate”; 3 “high”; 4 “very high”). A risk perception score (RPS) was then calculated separately for all presented vaccination and as a cumulative score, in both cases dichotomized for pediatric-age and STs-recommended immunizations.
Propensity towards vaccinations. STs rated their specific propensity towards the sixteen vaccine-preventable diseases previously presented through a 5-point Likert scale (i.e. 1, “strongly disagree”; 2, “disagree”; 3, “neutral”; 4, “agree”; and 5, “strongly agree”). A cumulative vaccine propensity score (VPS) was calculated for the single attitudes, and separately for pediatric-age and STs-recommended immunizations by awarding a score of +1 for a specific propensity rated as “strongly disagree”, +2 for “disagree”, and so on.
PROCEDURES
Subjects were informed that participation was on a strict voluntary basis, that completion and delivery of the questionnaire implied consent for study participation, and that all gathered data would be confidentially handled and collectively elaborated, having no other purpose than evaluation of vaccine attitudes and knowledge of participants. Because the individual participants cannot be identified through the questionnaire, it is implausible that this study caused them any harm. Moreover, as the consent for the participation was asked only after the course were actually completed and the First Aid certification achieved, it is also improbable that they have felt forced to participation. As the study design assured an adequate protection of study participants, and neither include clinical data about patients nor configure itself as a clinical trial, its preliminary assessment by Ethical Committee of the Provincial Agency of for Health Services (APSS) was not required.
DATA ANALYSIS
Two independent researchers, one of whom read the responses from each questionnaire while the other researcher reviewed the entered data, ensured the accuracy of data entry. The primary investigator examined unclear responses to determine the correct response. Described indices for general knowledge, knowledge about official recommendations, risk perception and propensity score, which assess the extent to which STs may pass on official recommendations, were eventually calculated. In order to more easily compare the scales, all results were normalized as per cent values.
Continuous variables were expressed as mean ± standard deviation and were analyzed through Student’s t test for unpaired data or ANOVA when appropriate. The comparisons among risk perception scores and attitude scores was performed through the Dunnett’s post-hoc test, arbitrarily assuming tetanus as the referent score. Categorical variables were reported as per cent values. Analysis of discrete variables (i.e. age categories, specific attitudes …) was initially performed through bivariate analysis, and their associations with outcome variables were expressed as odds ratios (OR) with their 95% confidence intervals (95%CI). Adjusted OR (adjORs) were calculated through stepwise binary logistic regression analysis only for categorical variables that at bivariate analysis were associated with a general positive attitude towards vaccinations with p values < 0.05. In regression analyses we also assessed the relative influence of attitudes, general knowledge, and knowledge about recommendations on the propensity score. In the analyses, we controlled for age, sex and household characteristics. Significance level was < 0.05. All statistical analyses were performed using IBM SPSS Statistics 24.0 for Macintosh (IBM Corp. Armonk, NY).
Results
DEMOGRAPHIC DATA
Demographic data of the study sample are summarized in Table I. A total of 154 questionnaires were returned (91.7% of the initial sample), including 38 STs from elementary school (24.7%), 40 from Middle school (26.0%), and eventually 76 from High School (49.4%). Mean age of the study population was 48.9 ± 7.8 years, with a mean seniority of 13.3 ± 8.7 years. Female sex was the most extensively represented (87.0%), and only 9 subjects (5.8%) had a migration background, being all other participants of Italian descent. Mean household size (including the participant) was 3.5 ± 1.2 people (min: 1, max: 7). For 41.6% of the participants, household included at least a subject younger than 18 years, whereas in 13.0% it included at least a subject older than 65 years. In total, 66 subjects (42.9%) referred a college degree or higher.
Tab. I.
Demographics of the study population.
| Total | Males | Females | |
|---|---|---|---|
| Participants (n, %) | 154 (100%) |
20 (13.0%) |
134 (87.0%) |
| Mean Age (years ± SD) | 48.9 ± 7.8 | 51.8 ± 8.7 | 48.5 ± 7.6 |
| < 40 year-old | 20 (13.0%) |
1 (5.0%) |
19 (95.0%) |
| 40 – 49 year-old | 60 (39.0%) |
8 (13.3%) |
52 (86.7%) |
| 50 – 59 year-old | 62 (40.3%) |
6 (9.7%) |
56 (90.3%) |
| ≥ 60 year-old | 12 (7.8%) |
5 (41.7%) |
7 (58.3%) |
| Seniority (years ± SD) | 13.3 ± 8.7 | 14.1 ± 9.4 | 12.9 ± 7.7 |
| Migration background (n, %) | 9 (5.8%) |
0 (-) |
9 (100%) |
| Household size (mean ± SD) | 3.5 ± 1.2 | 3.8 ± 1.1 | 3.4 ± 1.2 |
| The participant (single) | 14 (9.1%) |
1 (7.1%) |
13 (92.9%) |
| +1 | 18 (11.7%) |
1 (5.6%) |
17 (94.4%) |
| +2 | 29 (18.8%) |
5 (17.2%) |
24 (82.8%) |
| +3 | 71 (46.1%) |
9 (12.7%) |
62 (87.3%) |
| +4 | 16 (10.4%) |
3 (18.7%) |
13 (81.3%) |
| +5 or more | 6 (3.9%) |
1 (16.7%) |
5 (83.3%) |
| Lives with subjects < 18 y.o. | 64 (41.6%) |
9 (14.1%) |
55 (85.9%) |
| Lives with subjects > 65 y.o. | 20 (13.0%) |
5 (25.0%) |
15 (75.0%) |
| Educational level | |||
| High School | 88 (57.1%) |
8 (9.1%) |
80 (90.9%) |
| University or greater | 66 (42.9%) |
12 (18.2%) |
54 (81.8%) |
| Type of school | |||
| Elementary | 38 (24.7%) |
3 (7.9%) |
35 (92.1%) |
| Middle | 40 (26.0%) |
4 (10.0%) |
36 (90.0%) |
| High School | 76 (49.4%) |
13 (17.1%) |
63 (82.9%) |
GENERAL ATTITUDE TOWARD VACCINATIONS
As shown in Table II, a total of 136 out of 154 respondents were “strongly favourable” or “somehow favourable” to vaccinations (88.3%). Negative attitudes peaked in age group 40 – 59 y.o. (n = 10/62 and 6.5% of the total sample), but positive and negative attitudes towards vaccines were actually unrelated with age (48.5 ± 7.7 y.o. vs. 51.8 ± 7.9 y.o., p = 0.088), seniority (12.7 ± 9.1 y vs. 15.1 ± 7.2 y, p = 0.310), household size (3.5 ± 1.2 vs. 3.6 ± 1.2, p = 0.668) and composition (p = 1.000 and p = 0.904 for household including subjects < 18 y.o. and > 65 y.o., respectively), and level of education (p = 1.000). Overall, female STs had more favourable attitude towards vaccinations than males (p = 0.018; OR 4.357, 95%CI 1.414-13.43), but this association was not confirmed by multivariate analysis (adjOR 2.976 95% CI 0.841-10.53).
Tab. II.
Attitudes towards vaccinations by demographic data and information sources. Continuous variables were compared through student’s t test for unpaired data, where categorical ones were assessed through chi-squared test and their associations with outcome variables were expressed as odds ratios (OR) with their 95% confidence intervals (95%CI). Adjusted Odds Ratio (adjOR) were calculated through logistic regression analysis for variables that at bivariate analysis were associated with a general positive attitude towards vaccinations with p values < 0.05.
| Attitudes towards vaccinations | P value | OR | 95%CI | adjOR | 95%CI | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Somehow favorable (n = 136) |
Somehow against (n = 18) |
|||||||||
| Age (mean ± SD(1)) | 48.9 ± 7.8 | 48.5 | 7.7 | 51.8 | 7.9 | 0.088 | - | - | - | - |
| < 40 y.o. (No., %) | 20 (13.0%) | 18 | (90.0%) | 2 | (10.0%) | 1.000 | 1.000 | REF | - | - |
| 40 – 49 y.o. (No., %) | 60 (39.0%) | 56 | (93.3%) | 4 | (6.7%) | 0.790 | 0.737 | 0.077 – 7.007 | - | - |
| 50 – 59 y.o. (No., %) | 62 (40.2%) | 52 | (83.9%) | 10 | (16.1%) | 0.231 | 0.274 | 0.033 – 2.284 | - | - |
| ≥ 60 y.o. (No., %) | 12 (7.8%) | 9 | (75.0%) | 3 | (25.0%) | 0.151 | 0.158 | 0.014 – 1.737 | - | - |
| Seniority (mean ± SD) | 13.3 ± 8.7 | 12.7 | 9.1 | 15.1 | 7.2 | 0.310 | - | - | - | - |
| Household size (mean ± SD) | 3.5 ± 1.2 | 3.5 | 1.2 | 3.6 | 1.2 | 0.668 | - | - | - | - |
| Lives with subjects < 18 y.o. (No., %) | 64 (41.6%) | 57 | (89.1%) | 7 | (10.9%) | 1.000 | 1.134 | 0.414 – 3.104 | - | - |
| Lives with subjects > 65 y.o. (No., %) | 20 (13.0%) | 17 | (85.0%) | 3 | (15.0%) | 0.904 | 0.714 | 0.187 – 2.727 | - | - |
| Female Sex (No., %) | 134 (87.0%) | 122 | (91.0%) | 12 | (9.0%) | 0.018 | 4.357 | 1.414 – 13.43 | 2.976 | 0.841 – 10.53 |
| University education level (No., %) | 66 (42.9%) | 58 | (87.9%) | 8 | (12.1%) | 1.000 | 1.076 | 0.400 – 2.985 | - | - |
| Information source(2) | ||||||||||
| TV / Radio (No., %) | 18 (11.7%) | 16 | (88.9%) | 2 | (11.1%) | 0.757 | 1.067 | 0.224 – 5.077 | - | - |
| New Media(3) (No., %) | 27 (17.5%) | 18 | (66.7%) | 9 | (33.3%) | < 0.001 | 0.153 | 0.053 – 0.435 | 0.143 | 0.047 – 0.437 |
| Friends, relatives (No., %) | 13 (8.4%) | 11 | (84.6%) | 2 | (15.4%) | 1.000 | 0.704 | 0.143 – 3.466 | - | - |
| Professional courses (No., %) | 6 (3.9%) | 5 | (83.3%) | 1 | (16.7%) | 1.000 | 0.649 | 0.071 – 5.889 | - | - |
| Health professionals (No., %) | 116 (75.3%) | 108 | (93.1%) | 8 | (6.9%) | 0.003 | 4.821 | 1.741 – 13.35 | 4.599 | 1.540 – 13.74 |
| Newspapers (No., %) | 18 (11.7%) | 15 | (83.3%) | 3 | (16.7%) | 0.757 | 0.620 | 0.161 – 2.393 | - | - |
(1) SD = Standard Deviation.
(2) As multiple choices were allowed, total sum may exceed 100%.
(3) New Media = wikis, blogs, social media, etc.
Main information sources referred by study population were health professionals (75.3%), new media (17.5%), TV / radio (11.7%), and newspapers (11.7%), whereas 8.4% of participants recalled friends and/or relatives and 3.9% professional courses. STs identifying health professionals as their main referents exhibited a significantly more positive attitude towards vaccines (p = 0.003, OR 4.821 95%CI 1.741-13.35), and even though the majority of participants referring new media as information source were favourable to vaccinations, prevalence of negative attitude was significantly higher than in subjects not relying on such information media (p < 0.001, OR 0.153 95% 0.053-0.435). Eventually, both associations were confirmed at multivariate analysis (adjOR 4.599, 95%CI 1.540-13.74 and adjOR 0.143 95%CI 0.047-0.437, respectively).
Among the reasons for hesitate or even refuse vaccination (Tab. III), all subjects (100%) referred they aimed to avoid side effects, whereas 50% of the respondents claimed lack of trust in vaccines, the belief that the immunization sustained by natural infections is more efficient, and the fear of vaccination shots. A third of the participants then referred preference for other countermeasures, and the belief that vaccines are superfluous as natural immunity ultimately is able to overcome any infectious disease (in both cases 33.3%). Eventually, 27.8% of the respondents claimed for “religious/ethical reasons”, or shared the belief that vaccines are useless, as unable to enhance natural immunity.
Tab. III.
Reasons for hesitate or even refuse vaccination.
| Why do you get vaccinations(1)? | N# (/136) | % |
|---|---|---|
| To avoid getting VPDs | 92 | 67.6% |
| To avoid complications of VPDs | 69 | 50.7% |
| To avoid transmitting VPDs | 59 | 43.4% |
| To avoid VPDs in subjects who cannot be vaccinated | 27 | 19.9% |
| Reasons to decline a vaccine or hesitate towards vaccinations(1) | N# (/18) | % |
|---|---|---|
| To avoid side effects of vaccinations | 18 | 100.0% |
| No trust in vaccines | 9 | 50.0% |
| Immunization by natural infections is more efficient | 9 | 50.0% |
| Fear of shots | 9 | 50.0% |
| Preference on other countermeasures | 6 | 33.3% |
| Vaccines are superfluous (i.e. natural immunity ultimately overcomes any infectious disease) |
6 | 33.3% |
| Vaccinations are against my personal beliefs (religious / ethical) | 5 | 27.8% |
| Vaccines are useless (i.e. vaccines are eventually unable to enhance natural immunity) |
5 | 27.8% |
(1) As multiple choices were allowed, total sum may exceed 100%.
On the contrary, the most frequently referred reason to be vaccinated was to avoid be infected by VPDs (67.6%), followed by avoiding complications (50.7%) and transmission of VPDs (43.4%), whereas 19.9% of participants identified the avoiding of VPDs in subjects who cannot be vaccinated.
KNOWLEDGE OF OFFICIAL RECOMMENDATIONS
Mean KS-OR was 51.2 ± 17.8, with an actual range of 0.0 to 93.75 for Students-recommended vaccinations, and 20.7 ± 20.7 (range 0.0 to 75.0) for STs-recommended immunizations. Subjects exhibiting a positive attitude towards vaccinations had a significantly better knowledge of official recommendations for students (52.7 ± 16.9 vs. 39.9 ± 20.2, p = 0.004), whereas KS-OR for vaccinations in STs was not significantly different (21.14 ± 20.7 vs. 15.6 ± 20.9, p = 0.267). Overall, 46 out of 154 participants (29.9% of total sample) were able to identify all the 4 compulsory vaccines for paediatric subjects (Fig. 1).
Fig. 1.
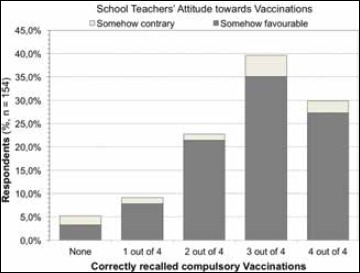
Correctly recalled compulsory vaccinations in pediatric-age subjects (i.e. diphtheria, tetanus, Viral Hepatitis B, poliomyelitis), broken down by attitude towards vaccinations (i.e. somehow contrary vs. somehow favorable).
Knowledge of participants on which vaccinations are recommended in paediatric age subjects by PNPV 2012-2014 is presented in Figure 2. In summary, most of participants (124 out of 154, 80.5%) correctly recalled tetanus, followed by poliomyelitis (n = 122, 79.2%), rubella and diphtheria (in both cases, n = 117, 76.0%), measles (n = 116, 75.3%) and pertussis (n = 115, 74.7%). Conversely, only 25 participants correctly recalled H influenzae type B (16.2%) as a recommended immunization, while 73.4% of the sample (n = 113) was unable to identify whether it was a recommended or not recommended vaccination.
Fig. 2.
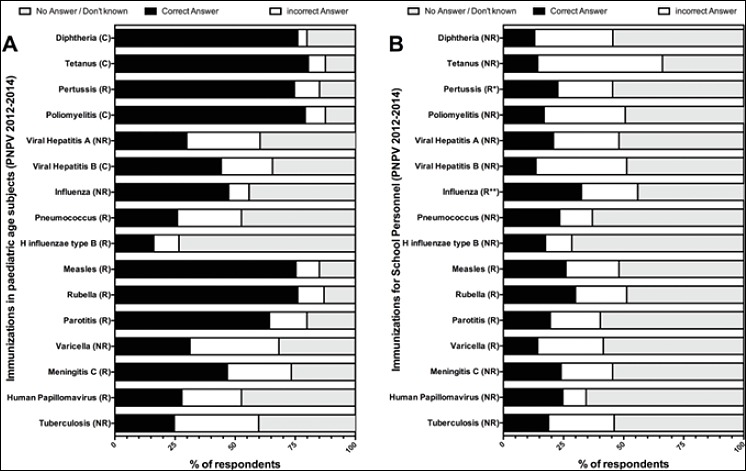
Knowledge of participants on which vaccinations are recommended in paediatric age subjects and for School Personnel (PNPV 2012-2014). (C) = compulsory; (R) = recommended; (NR) = not recommended; * as a part of decennial tetanus-diphtheria booster in subjects > 18 years.** not explicitly recommended, but recalled for occupational settings associated with high risk and where sick leave during influenza season would severely impair public services.
Regarding the knowledge of recommended STs vaccinations, only 8 out of 154 participants correctly recalled all the six immunizations (5.2%), whereas around half of the sample (n = 69, 44.8%) recalled none of them. Focusing on single immunizations, around a third of the sample correctly identified influenza (n = 50, 32.5%) as a recommended immunization, followed by rubella (n = 46, 29.9%), measles (n = 40, 26.0%), pertussis (n = 35, 22.7%), parotitis (n = 30, 19.5%), and varicella (n = 22, 14.3%).
GENERAL KNOWLEDGE
After normalization, the mean KS-G was 50.9 ± 26.8 (actual range 0.0-100.0). Subjects exhibiting a favorable attitude towards vaccinations had a significantly higher score (66.7 ± 21.8 vs. 33.3 ± 19.4, p < 0.001) and exhibited a greater prevalence of false beliefs. For instance, the most reported false belief among the participants was that vaccine additives as dangerous for human health (38/154, 24.7%), with several subjects causatively associating vaccines and autoimmune diseases in general (33/154, 21.4%), the latter including diabetes (13/154 8.4%) and multiple sclerosis (9/154, 5.8%), whereas around one-sixth of the sample associated measles vaccine with neurological diseases (26/154, 16.9%) and autism (25/154, 16.2%) (Fig. 3). Moreover, misconceptions regarding vaccine practices and in particular vaccination schedules were exhibited by around a fifth of the sample, as 28/154 (18.2%) that the immune system may be overwhelmed by the high number of vaccines identified by the vaccine schedules, whereas 16/154 (10.4%) believed that many vaccinations are administered too early.
Fig. 3.
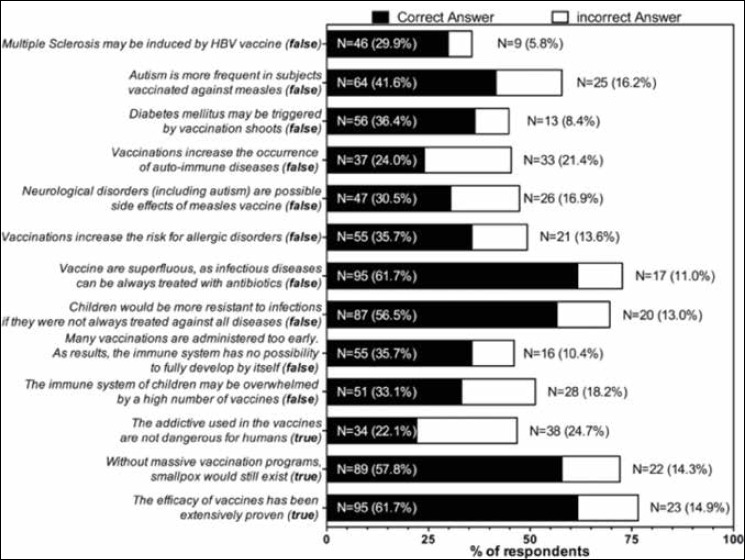
Results of knowledge test among the study respondents (n = 154)
ASSESSMENT OF THE RISK PERCEPTION
Average RPS for natural infections were 61.2 ± 23.2 and 52.2 ± 21.9 for students- and STs-recommended vaccinations, respectively. Most of participants identified tetanus (67.5%), poliomyelitis (66.9%), and meningitis (63.7%) as infections whose severity was either high or very high, whereas only of 29.2% respondents acknowledged varicella as a severe or highly severe VPD (Fig. 4). Similarly, tetanus and poliomyelitis were associated with a greater risk perception score (73.5 ± 29.6 and 73.7 ± 29.5, respectively), followed by meningitis C (70.5 ± 33.6), tuberculosis (68.9 ± 30.1), diphtheria (65.4 ± 30.1), viral hepatitis B (64.6 ± 29.1). In ANOVA, assuming tetanus as the referent one, difference in risk perception score with all the aforementioned infections was not statistically significant (for all cases, p > 0.05). Contrarily, a significantly lower score was associated with HPV (63.8 ± 30.5, p < 0.05), viral hepatitis A (60.6 ± 27.4, p < 0.01), rubella (58.9 ± 29.1, p < 0.001), measles (57.9 ± 28.3, p < 0.0001), pertussis (56.3 ± 25.7, p < 0.0001), parotitis (55.5 ± 28.3, p < 0.0001), H influenzae type B (54.6 ± 29.2, p < 0.0001), pneumococcus (53.7 ± 29.8, p < 0.0001), and eventually influenza having the lowest score (37.2 ± 25.6, p < 0.0001).
Fig. 4.
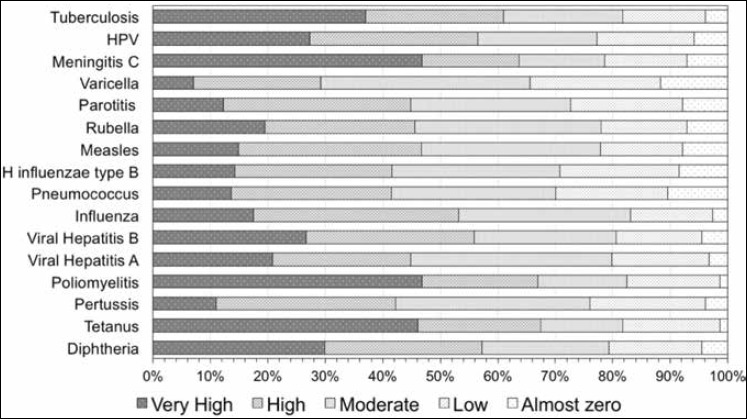
Assessment of the perceived severity of presented natural infections by study participants.
PROPENSITY SCORE
Normalized mean VPS was 81.7 ± 19.4 for Students-recommended vaccines, and 78.9 ± 20.7 for STs-recommended vaccines: when single vaccinations were taken in account, higher VPS was associated with tetanus (84.1 ± 26.9), diphtheria (82.6 ± 26.3), poliomyelitis (82.2 ± 27.6), rubella (80.7 ± 28.5), followed by meningitis C (79.8 ± 27.7), tuberculosis (79.7 ± 26.7), pertussis (79.6 ± 26.8), parotitis (79.4 ± 27.9), measles (79.6 ± 28.6), viral hepatitis B (79.5 ± 28.2), HPV (77.0 ± 27.0), viral hepatitis A (76.0 ± 26.9). For all aforementioned vaccines, VPS was not significantly different from the referent one (i.e. tetanus) in post-hoc Dunnett’s multiple comparison test. Contrarily, pneumococcus (72.4 ± 26.9, p < 0.01), varicella (72.2 ± 27.9, p < 0.01), H influenzae type B (70.7 ± 26.0, p < 0.001) and influenza vaccine had significantly lower acceptance (63.6 ± 28.9, p < 0.0001) (Table IV).
Tab. IV.
Risk Perception Score (RPS) and Vaccine Propensity Score (VPS) for the single vaccinations presented to the study participants. Analysis was performed through ANOVA and Dunnett’s test for multiple comparison by arbitrarily assuming tetanus scores as the referent ones.
| Immunization | RPS (0.0 – 100) | VPS (Range 0.0 – 100) | ||
|---|---|---|---|---|
| Mean ± SD | P value | Mean ± SD | P value | |
| Tetanus | 73.5 ± 29.6 | REFERENCE | 84.1 ± 26.9 | REFERENCE |
| Diphtheria | 65.4 ± 30.1 | > 0.05 | 82.6 ± 26.3 | > 0.05 |
| Pertussis | 54.3 ± 25.7 | < 0.0001 | 79.6 ± 26.8 | > 0.05 |
| Poliomyelitis | 73.7 ± 29.5 | > 0.05 | 82.2 ± 27.6 | > 0.05 |
| Viral Hepatitis A | 60.6 ± 27.4 | < 0.01 | 76.0 ± 26.9 | > 0.05 |
| Viral Hepatitis B | 64.6 ± 29.1 | > 0.05 | 79.5 ± 28.2 | > 0.05 |
| Influenza | 37.2 ± 25.6 | < 0.0001 | 63.6 ± 28.9 | < 0.0001 |
| Pneumococcus | 53.7 ± 29.8 | < 0.0001 | 72.4 ± 26.9 | < 0.01 |
| H influenza type B | 54.6 ± 29.2 | < 0.0001 | 70.7 ± 26.0 | < 0.001 |
| Measles | 57.9 ± 28.3 | < 0.001 | 78.6 ± 28.6 | > 0.05 |
| Rubella | 58.9 ± 29.1 | < 0.001 | 80.7 ± 28.5 | > 0.05 |
| Parotitis | 55.5 ± 28.3 | < 0.0001 | 79.4 ± 27.9 | > 0.05 |
| Varicella | 47.6 ± 27.4 | < 0.0001 | 72.2 ± 27.9 | < 0.01 |
| Meningitis C | 70.5 ± 33.6 | > 0.05 | 79.8 ± 27.7 | > 0.05 |
| Human Papillomavirus | 63.8 ± 30.5 | < 0.05 | 77.0 ± 27.0 | > 0.05 |
| Tuberculosis | 69.0 ± 30.1 | > 0.05 | 79.7 ± 26.7 | > 0.05 |
REGRESSION ANALYSIS
Knowledge about vaccine recommendations was identified as a significant predictor for propensity towards Students-recommended vaccinations (B = 0.196, 95% CI 0.036 to 0.355, p = 0.016), similarly to RPS (B = 0.372, 95%CI 0.247 to 0.496, p < 0.001). In other words, STs having a lower knowledge of official recommendations and lower perception of the risk associated with natural infections had a lower acceptance of vaccines, and conversely a greater risk for vaccine hesitancy, whereas KS-G was unrelated with VPS (B = -0.043, 95%CI -0.147 to 0.060, p = 0.408). Contrarily, VPS towards STs-recommended immunizations was unaffected by the KS-OR (B = 0.001, 95%CI LL -0.001 to 0.002, p = 0.265), and KS-G (B = 0.000, 95%CI -0.001 to 0.001, p = 0.852), and only RPS was predictive for a better VPS (B = 0.005, 95%CI 0.004 to 0.006, p < 0.001).
Discussion
This cross-sectional study aimed to define KAB of STs towards vaccinations, as they represent a significant workforce at occupational risk for contracting and spreading VPDs through their workplaces [22, 31]. Moreover, as usually well trusted professionals, STs may be useful to address both the vaccine hesitant and more specifically individuals with uncertain attitude towards vaccinations (i.e. “fence-sitter”) [34, 44, 45]. More specifically, previous reports actually suggest that STs may actively propagate better awareness and greater knowledge regarding vaccines and vaccination policies in populations groups otherwise affected diffuse lack of specific knowledge and training, whose informative gaps may be easily filled by uncontrolled information sources, with resulting false beliefs and misconceptions – a common feature of VH [1, 24, 34].
Overall, the attitude of the study participants towards vaccinations was largely positive: not only 88.3% of the STs self-declared either “somehow favourable” or “strongly favourable” to vaccinations, but the assessed VPS were similarly high, both for Students- and STs-recommended immunizations (81.7 ± 19.4 and 78.9 ± 20.7, respectively). However, our results were somehow disappointing.
First at all, among the 11.7% of participants self-declaring somehow against vaccination practice, the most frequently reported reason to hesitate and/or refuse vaccinations was identified in the fear of side effects, referred by all subjects self-assessing as against vaccinations, followed by the fear of shots (50.0%), and a series of statements such as the lack of trust in vaccines, or the belief that immunization by natural immunization would be more efficient than that promoted by vaccination.
As some reports from North America previously suggested that school environment may be associated with a significantly high degree of misbelieves about vaccines, such results were not unexpected [21-23], but they still remain somehow worrisome, as available evidence also indicates that knowledge gaps and high prevalence of false beliefs are strongly associated with low vaccination rates, not only in STs but also in the general population interacting with school professionals [7, 21-23].
Also the assessment of the general knowledge was largely ambiguous, and again supported the existence of a significant knowledge gap.
Firstly, although only the statement that “the addictive used in the vaccines are not dangerous for humans” was associated with higher prevalence of incorrect answers (24.7% vs. 22.1%), the share of false beliefs regarding the measles vaccine, including both the causative association with autism and neurological disorders, were noteworthy (16.2% and 16.9%, respectively), and also rates of “don’t know” answers were indeed appreciably high, ranging from 23.4% to 64.3%. Again, this high rate of subjects either unable or unwilling to assess the presented statement may be interpreted as a consequence of incomplete or insufficient knowledge regarding the presented items, whose content was specifically designed in order to describe the prevalence of false beliefs and misunderstanding about vaccinations.
Second, knowledge of official recommendations as defined by PNPV 2012-2014 was unsatisfying, as the majority of participants were in facts either unable or unwilling to assess the status of STs-recommended vaccinations, whose specific knowledge was eventually strikingly low (i.e. 20.7 ± 20.7 with a potential range of 0 to 100). The knowledge gap probably reflects the somehow vague recommendations for occupational settings other than that of healthcare [11, 15], and the frequently inappropriate seeding of official recommendation to the targeted occupational groups [16, 41-44].
In facts, even though some uncertainties could have been expected for immunizations such as influenza and pertussis, whose occupational recommendations for SEs are actually ambiguous, most of participants were unable to characterize vaccinations having a far better defined status, as H influenzae type B, pneumococcus, and HPV. Not coincidentally, the upcoming PNPV 2017-2019, whose approbation is still underway, will identify more detailed occupational recommendations for the school settings [11, 15].
Also the knowledge of official recommendations targeting students as subjects of paediatric age was affected by several uncertainties. Even though around 70% of the sample was able to correctly recall at least three of the four compulsory immunizations, and diphtheria, tetanus and poliomyelitis were accurately reported as compulsory vaccines by more than 75% of the sample, the status of viral hepatitis B vaccine was acknowledged by only 44.2% of the participants. Similar uncertainties were associated with the recalling of significant immunizations such as parotitis, viral hepatitis A, varicella, meningitis C and pneumococcus. Moreover, H influenzae type B was apparently unknown to the large majority of the sample. Such results may again be explained as the consequence of a knowledge gap. Actually, infectious diseasese such tetanus, poliomyelitis, but also meningitis and tuberculosis are usually acknowledged as severe and potentially life-threatening infectious diseases, whereas the status of other VPDs may be more extensively disputed [41, 46-50]. For example, natural infections by measles, parotitis, varicella and pertussis are usually understood as indolent pediatric disorders, as general population usually ignores that such VPDs may be associated with severe complications such as acute respiratory failure, encephalitis or even death [41, 42, 48-52], and that sub-optimal immunization levels are revamping their incidence in EU countries [47, 51]. Not coincidentally, in our survey these vaccinations were associated with a RPS significantly lower than that identified not only for tetanus and diphtheria, but also for tuberculosis and meningitis.
In other words, the inconsistent and not up-to-date awareness of the risk associated with all the presented VPDs may have forced the participants to report “common-sense” rather than “evidence based” recommendations [41-42, 46, 49, 60, 52-55]. In this regard, the ambiguous status of rubella, diffusely acknowledged and publicized as both an indolent disease and a significant infection for childbearing-age women, may explain the relatively high rate of correct answers both for STs- (29.9%) and students-recommended vaccinations (76.0%).
Consistently with such remarks and previous reports, also in our survey the perceived severity of natural infections was identified as the most significant predictors for the acceptance of both Students- and STs-recommended vaccinations [31, 41-42, 49, 52-54]. Hence, the knowledge deficit of STs regarding the actual risk associated with natural infections may also have significantly affected the VPS. In other term, STs may be unaware of their specific risk towards the aforementioned natural infections, as they may consider themselves as either immune (because of previous natural infection or paediatric-age immunization) or unconcerned by somehow “not significant” VPDs. Even though the very low RPS assessed for seasonal influenza may therefore explain by itself the similarly unsatisfactory PS, it is possible that this result may have been also affected by the diffuse misunderstandings and alarming misconceptions about the efficacy of the vaccine [56], a critical issue well described in previous studies investigating knowledge, attitudes and practices of HCWs towards seasonal influenza vaccine [12, 57-63], and possibly shared by other immunizations such as measles vaccine [48-50].
As health professionals (including General Practitioners, OPh, etc.) were the main information source in STs about vaccines and immunizations, our results indirectly suggest that the knowledge gaps of STs may ultimately include not only an informative gap, but also a communicative one, with STs unable to obtain and/or retain up-to-date medical evidence regarding the morbidity and even the epidemiology of VPDs [46, 50, 55]. In this regard, it should be stressed that subjects referring to health professionals in order to be informed showed significantly higher propensity towards vaccinations (adjOR 4.599 95%CI 1.540-13.74), whereas STs referring to uncontrolled information sources such as new media, still retaining a generally positive attitude, were more frequently against vaccinations, and showed higher prevalence of false beliefs and misunderstanding, ultimately confirming the critical role for an appropriate information [1, 24, 34]. In this regard, it should be stressed that several Education systems, including the Italian one, lack of key vaccine stakeholders such as school nurses and school physicians [39, 62, 63]: in such settings, the OPh are therefore called to enhance vaccine acceptance among people who are vaccine hesitant or even refuse vaccinations [43, 64, 65].
LIMITS OF THE STUDY
Our study is affected by several major limitations. Firstly, we assessed a sample of relatively small size, gathered through convenience sampling and a regional basis. As Italy is highly heterogeneous in term of vaccination rates and vaccine acceptance, our sample may therefore not represent neither the whole Italian SEs nor STs populations [11].
Second, our study included a very selected population (i.e. subjects participating to a First Aid course), presumptively encompassing subjects more sensitive to health themes: a significant selection bias cannot therefore be ruled out, ultimately suggesting that our survey overestimated actual vaccine acceptance of the parent occupational group.
Third, we lack data about the vaccination status of the participants. Despite this specific item has been repetitively described as a significant behavioural predictor [44], the self-referred vaccination rates are notoriously inaccurate, in particular for paediatric-age immunizations [7, 23, 32], and therefore we opted for a propensity assessment [41-42]. Unfortunately, this design ultimately hampers the ability of our study to accurately distinguish between vaccine hesitant and “fence sitter” peoples, but this assessment was not included in the endpoints of our study [41-43].
Eventually, our study assessed the risk perception of the participants towards VPDs without dichotomizing the perceived consequences in adults and children/adolescents. This a substantial limit, as health impacts of most VPDs are significantly influenced by age, sex and health status of the recipient, and also their perceptions may be significantly heterogeneous [1-4, 6]. For example, pertussis is frequently acknowledged as a severe disease in children, but general population is usually unaware of its possible consequences in adults and elderly, as well as of their potential role as spreaders of the pathogen among unprotected of partially protected groups. On the contrary, general population frequently ignore the potential severity of H influenzae type B infection in younger age groups, dismisses varicella as an annoying disease of children, undermining its consequences in adults, and similarly ignores that infections such as measles may have severe long term consequences in unvaccinated subjects [3, 14-15, 24-25, 34, 46-52].
Conclusions
In conclusion, our results support the usefulness for STs of educational campaigns and additional training about vaccines and misconceptions about vaccines and vaccine practices in order to fill their knowledge gaps. The primary objective of these interventions should be raising the awareness of STs regarding VPDs, emphasizing that the teachers themselves are at significant risk, and that they may potentially become the source of potentially life-threatening infections for their students and relatives. Moreover, these campaigns should also be aimed to convince STs about safety and efficacy of vaccines, in order that they could proactively share and disseminate up-to-date evidence across the school settings. Cornerstone of these campaigns should be identified in healthcare professionals strictly interconnected with the school environment and well aware of the specific characteristics of the school settings. In health system lacking significant stakeholders such as school nurses and school physicians, the contribution of OPh may be significant.
Acknowledgments
The authors express their gratitude to all participants.
All person who meet authorship criteria are listed as authors, and all authors certify that they have no affiliation with or involvement in any organization or entity with any financial interest, or non-financial interest (such as personal or professional relationship, affiliation, knowledge of beliefs) in the subject matter or material discussed in the manuscript.
References
- [1].Bloom BR, Marcuse E., Mnookin S. Addressing Vaccine hesitancy Science 2014;344:339. [DOI] [PubMed] [Google Scholar]
- [2].Centers for Disease Control and Prevention. Impact of vaccines universally recommended for children--United States, 1990-1998 MMWR 1999;48:243-8. [PubMed] [Google Scholar]
- [3].Bonanni P, Bergamini M. Factors influencing vaccine uptake in Italy Vaccine 2002;20(S1):S8-S12. [DOI] [PubMed] [Google Scholar]
- [4].Bonanni P, Bechini A, Boccalini S, Peruzzi M, Tiscione E, Boncompagni G, Mannelli F, Salmaso S, Filia A, Ciofi degli Atti M. Progress in Italy in control and elimination of measles and congenital rubella Vaccine 2007;25:3105-10. [DOI] [PubMed] [Google Scholar]
- [5].Weigel M, Bruns R, Weitmann K, Hoffmann W. Immunization Rates at the School Entry in 2012 Dtsch Arztebl Int 2014;111:788-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Omer SB, Salmon DA, Orenstein WA, deHart MP, Halsey N. Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases N Engl J Med 2009;360:1981-8. [DOI] [PubMed] [Google Scholar]
- [7].Macintosh J, Luthy KE, Beckstrand RL, Eden LM, Orton J. Vaccination perceptions of school employees in a rural school district Vaccine 2014;32:4766-71. [DOI] [PubMed] [Google Scholar]
- [8].Veronesi L, Virdis R, Bizzoco S, Colucci ME, Affanni P, Paganuzzi F, Riccò M, Capobianco E, Tanzi ML. Vaccination status and prevalence of enteric viruses in internationally adopted children Acta Biomed 2011;82:208-13. [PubMed] [Google Scholar]
- [9].Zingg A, Siegrist M. Measuring people’s knowledge about vaccination: Developing a one-dimensional scale. Vaccine 2012;30:3771-7. [DOI] [PubMed] [Google Scholar]
- [10].Giannattasio A, Mariano M, Romano R, Chiatto F, Liguoro I, Borgia G, Guarino A, Lo Vecchio A. Sustained low influenza vaccination in health care workers after H1N1 pandemic: a cross sectional study in an Italian health care setting for at-risk patients. BMC Infect Dis 2015;15;329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Bonanni P, Ferro A, Guerra R, Iannazzo S, Odone A, Pompa MG, Rizzuto E, Signorelli C. Vaccine coverage in Italy and assessment of the 2012-2014 National Immunization Prevention Plan. Epidemiol Prev 2015;39(4 Suppl. 1):146-58. [PubMed] [Google Scholar]
- [12].Bonaccorsi G, Santomauro F, Porchia B, Niccolai G, Pellegrino E, Bonanni P, Lorini C. Beliefs and opinions of health care workers and students regarding influenza and influenza vaccination in Tuscany, Central Italy. Vaccines (Basel) 2015;3:137-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Alicino C, Iudici R, Barberis I, Paganino C, Cacciani R, Zacconi M, Battistini A, Bellina D, Di Bella AM, Talamini A, Sticchi L, Morando A, Ansaldi F, Durando P. Influenza vaccination among healthcare workers in Italy. Hum Vaccin Immunother 2015;11:95-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Biasio LR, Corsello G, Costantino C, Fara GM, Giammanco G, Signorelli C, Vecchio D, Vitale F. Communication about vaccination: A shared responsibility. Hum Vaccin Immunother 2016;12:2984-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Signorelli C, Odone A, Bonanni P, Russo F. New Italian immunisation plan is built on scientific evidence: Carlo Signorelli and colleagues reply to news article by Michael Day. BMJ 2015;h6775-1. [DOI] [PubMed] [Google Scholar]
- [16].Betsch C, Wicker S. Personal attitudes and misconceptions, not official recommendations guide occupational physicians’ vaccination decisions. Vaccine 2014;32:4478-84. [DOI] [PubMed] [Google Scholar]
- [17].Hull HF, Ambrose CS. Current Experience with School-located influenza vaccination programs in the United States. Hum Vaccin 2011;7:153-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Fefferman NH, Naumova EN. Dangers of vaccine refusal near the herd immunity threshold: a modelling study. Lancet Infect Dis 2015;15:922-6. [DOI] [PubMed] [Google Scholar]
- [19].Dubé E, Gagnon D, MacDonald NESAGE Working Group on Vaccine Hesitancy. Strategies intended to address vaccine hesitancy: Review of published reviews. Vaccine 2015;33:4191-203. [DOI] [PubMed] [Google Scholar]
- [20].Mikolajczyk RT, Akmatov MK, Rastin S, Kretzschmar M. Social contacts of school children and the transmission of respiratory-spread pathogens. Epidemiol Infect 2008;136:813-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Ha C, Rios LM, Pannaraj PS. Knowledge, Attitudes, and Practices of School Personnel Regarding Influenza, Vaccinations, and School Outbreaks. J Schl Health 2013;83:554-61. [DOI] [PubMed] [Google Scholar]
- [22].Luthy KE, Thompson KE, Beckstrand RL, Macintosh JLB, Eden LM. Perception of safety, importance, and effectiveness of vaccinations among urban school employees in Utah. J Am Assoc Nurse Pract 2015;27:313-20. [DOI] [PubMed] [Google Scholar]
- [23].Luthy KE, Houle K, Beckstrand RL, Macintosh J, Lakin RG. Vaccination perceptions and barriers of school employees: a pilot study. J Sch Nurs 2013;29:284-93. [DOI] [PubMed] [Google Scholar]
- [24].Larson HJ, Jarrett C, Eckersberger E, Smith DMD, Paterson P. Understanding vaccine hesitancy around vaccines and vaccinations from a global perspectives: a systematic review of published literature, 2007-2012. Vaccine, 2014;32(19):2150-9. [DOI] [PubMed] [Google Scholar]
- [25].Larson HJ, Cooper LZ, Eskola J, Katz S, Ratzan S. New decade of vaccines 5: addressing the vaccine confidence gap. Lancet 2011;378:526-35. [DOI] [PubMed] [Google Scholar]
- [26].Dempsey AF, Schaffer S, Singer D, Butchart A, Davis M, Freed GL. Alternative vaccination schedule preferences among parents of young children. Pediatrics 2011;128:848-56. [DOI] [PubMed] [Google Scholar]
- [27].Gust DA, Darling N, Kennedy A, Schwartz B. Parents with doubts about vaccines: which vaccines and reasons why. Pediatrics 2008;122:718-25. [DOI] [PubMed] [Google Scholar]
- [28].Ladner J, Besson MH, Rodrigues M, Audureau E, Saba J. Performance of 21 HPV vaccination programs implemented in low and middle-income countries, 2009-2013. BMC Public Health 2014;14:670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Soofi SB, Haq IU, Siddiqui MB, Mirani M, Tahir R, Hussain I, Puri MK, Suhag ZH, Khowaja AR, Lasi AR, Clemens JD, Favorov M, Ochiai RL, Bhutta ZA. School as potential vaccination venue for vaccines outside regular EPI schedule: results from a school census in Pakistan. BMC Res Notes 2012;5:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].De Perio MA, Wiegand DM, Brueck SE. Influenza Vaccination coverage among school employees: assessing knowledge, attitudes, and behaviors. J Sch Health 2014;84:586-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Gargano LM, Painter JE, Sales JM, Morfaw C, Jones LM, Murray D, Wingood GM, DiClemente RJ, Hughes JM. Seasonal and 2009 H1N1 influenza vaccine uptake, predictors of vaccination and self-reported barriers to vaccination among secondary school teachers and staff. Hum Vaccin 2011;7:89-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Luthy KE, Thompson KE, Beckstrand RL, Macintosh JLB, Eden LM. Perception of safety, importance, and effectiveness of vaccinations among urban school employees in Utah J Am Assoc Nurse Pract 2015;27:313-20. [DOI] [PubMed] [Google Scholar]
- [33].De Perio MA, Wiegand DM, Evans SM. Low influenza vaccination rates among child care workers in the United States: assessing knowledge, attitudes, and behaviors J Community Health 2012;37:272-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Yaqub O, Castle-Clarke S, Sevdalis N, Chataway J. Attitudes to vaccination: a critical review Soc Sci Med 2014;112(C):1-11. [DOI] [PubMed] [Google Scholar]
- [35].Rose SB, Lanumata T, Lawton BA. Promoting uptake of the HPV Vaccine: the knowledge and views of school staff. J Sch Health 2011;81:680-7. [DOI] [PubMed] [Google Scholar]
- [36].Goldstein ST, Cassidy WM, Hodgson W, Mahoney FJ. Factors associated with student participation in a school-based hepatitis B immunization program. J Sch Health 2001;71:184-7. [DOI] [PubMed] [Google Scholar]
- [37].Tung CS, Middleman AB. An evaluation of school-level factors used in a successful school-based hepatitis B immunization initiative. J Adolesc Health 2005;37:61-8. [DOI] [PubMed] [Google Scholar]
- [38].Jourdan D, Pommier J, Quidu F. Practices and representations of health education among primary school teachers. Scand J Public Health 2010;38:86-94. [DOI] [PubMed] [Google Scholar]
- [39].Salmon DA, Moulton LH, Omer SB, Chace LM, Klassen A, Talebian P, Halsey NA. Knowledge, attitudes, and beliefs of school nurses and personnel and associations with nonmedical immunization exemptions. Pediatrics 2004;113:e552-e559. [DOI] [PubMed] [Google Scholar]
- [40].Signorelli C, Riccò M, Odone A. The Italian National Health Service expenditure on workplace prevention and safety (2006-2013): a national-level analysis. Ann Ig. 2016;28:313-8. [DOI] [PubMed] [Google Scholar]
- [41].Riccò M, Cattani S, Casagranda F, Gualerzi G, Signorelli C. Knowledge, attitudes, beliefs and practices of Occupational Physicians towards vaccinations of Health Care Workers: a cross sectional pilot study from North-Eastern. Italy Int J Occup Med Environ Health 2017;30:775-90. [DOI] [PubMed] [Google Scholar]
- [42].Riccò M, Cattani S, Veronesi L, Colucci ME. Knowledge, attitudes, beliefs and practices of construction workers towards tetanus vaccine in Northern Italy. Ind Health 2016;54:554-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Riccò M, Razio B, Panato C, Poletti L, Signorelli C. Knowledge, Attitudes And Practices Of Agricultural Workers Towards Tetanus Vaccine: A Field Report. Ann Ig 2017;29:239-55. [DOI] [PubMed] [Google Scholar]
- [44].Betsch C, Korn L, Holtmann C. Don’t try to convert the antivaccinators, instead target the fence-sitters. Proc Natl Acad Sci U S A 2015;112:E6725-E6726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Leask J. Target the fence-sitters Nature 2011;473(7348):443-5. [DOI] [PubMed] [Google Scholar]
- [46].Pulcini C, Massin S, Launay O, Verger P. Knowledge, attitudes, beliefs and practices of general practitioners towards measles and MMR vaccination in southeastern France in 2012. Clin Microbiol Infect 2014;20:38-43. [DOI] [PubMed] [Google Scholar]
- [47].Carrillo-Santisteve P, Lopalco PL. Measles still spreads in Europe: who is responsible for the failure to vaccinate? Clin Microbiol Infect 2012;18(Suppl. 5):S50-S56. [DOI] [PubMed] [Google Scholar]
- [48].Maltezou HC, Gargalianos P, Nikolaidis P, Katerelos P, Tedoma N, Maltezos E, Lazanas M. Attitudes towards mandatory vaccination and vaccination coverage against vaccine-preventable diseases among health-care workers in tertiary-care hospitals. J Infect 2012;64:319-24. [DOI] [PubMed] [Google Scholar]
- [49].Tafuri S, Gallone MS, Cappelli MG, Martinelli D, Prato R, Germinario C. Addressing the anti-vaccination movement and the role of HCWs. Vaccine 2014;32:4860-5. [DOI] [PubMed] [Google Scholar]
- [50].Barbadoro P, Marigliano A, Di Tondo E, De Paolis M, Martini E, Prospero E, D’Errico MM. Measles among healthcare workers in a teaching hospital in Central Italy. J Occup Health 2012;54:336-9. [DOI] [PubMed] [Google Scholar]
- [51].Lopalco PL, Martin R. Measles still spreads in Europe: who is responsible for the failure to vaccinate? Euro Surveillance 2010;15:pii=19557. [DOI] [PubMed] [Google Scholar]
- [52].Barrière J, Vanjak D, Kriegel I, Otto J, Peyrade F, Estève M, Chamorey E. Acceptance of the 2009 A(H1N1) influenza vaccine among hospital workers in two French cancer centers. Vaccine, 2010;28:7030-4. [DOI] [PubMed] [Google Scholar]
- [53].Harrison N, Brand A, Forstner C, Tobudic S, Burgmann K, Burgmann H. Knowledge, risk perception and attitudes toward vaccination among Austrian health care workers: A cross-sectional study. Hum Vaccin Immunother 2016;12:2459-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Quach S, Pereira JA, Heidebrecht CL, Kwong JC, Guay M, Crowe L, Quan S, Bettinger JA. Public Health Agency of Canada/Canadian Institutes of Health Research Influenza Research Network (PCIRN) Vaccine Coverage Theme Group. Health care worker influenza immunization rates: The missing pieces of the puzzle. Am J Infect Control 2013;41:685-90. [DOI] [PubMed] [Google Scholar]
- [55].Botelho-Nevers E, Gautret P, Biellik R, Brouqui P. Nosocomial transmission of measles An updated review. Vaccine 2012;30:3996-4001. [DOI] [PubMed] [Google Scholar]
- [56].Hollmeyer HG, Hayden F, Poland G, Buchholz U. Influenza vaccination of health care workers in hospitals-A review of studies on attitudes and predictors. Vaccine 2009;27:3935-44. [DOI] [PubMed] [Google Scholar]
- [57].Hofmann F, Ferracin C, Marsh G, Dumas R. Influenza vaccination of healthcare workers: a literature review of attitudes and beliefs. Infection 2006;34:142-7. [DOI] [PubMed] [Google Scholar]
- [58].Spadea A, Unim B, Ursillo P, Saulle R, Giraldi G, Miccoli S, Barbato A, Corda B, D’Amici AM, Boccia A, La Torre G. [Effectiveness of a training course on influenza vaccination in changing medical students and healthcare workers attitudes towards vaccination]. Ig Sanita Pubbl 2013;69:387-402. Italian [PubMed] [Google Scholar]
- [59].Albano L, Matuozzo A, Marinelli P, Di Giuseppe G. Knowledge, attitudes and behaviour of hospital health-care workers regarding influenza A/H1N1: a cross sectional survey BMC Infect Dis 2014;14:208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Cadeddu C, Di Thiene D, Ricciardi W, Boccia A, La Torre G. Knowledge about pandemic flu among Italian health care workers (HCWs) an Italian survey. J Prev Med Hyg, 2011;52:127-30. [PubMed] [Google Scholar]
- [61].Boccia A, Di Thiene D, De Giusti M, La Torre G. Seasonal and pandemic influenza: the role of communication and preventive strategies. J Prev Med Hyg, 2011;52:124-26. [PubMed] [Google Scholar]
- [62].Falato R, Ricciardi S, Franco G. [Influenza risk perception and vaccination attitude in medical and nursing students during the vaccination campaigns of 2007-2008 (seasonal influenza) and 2009/2010 (H1N1 influenza)]. Med Lav 2011;102:208-15. [PubMed] [Google Scholar]
- [63].Bonfiglioli R, Vignoli M, Guglielmi D, Depolo M, Violante FS. Getting vaccinated or not getting vaccinated? Different reasons for getting vaccinated against seasonal or pandemic influenza. BMC Public Health, 2013;13:1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Caskey RN, Macario E, Johnson DC, Hamlish T, Alexander KA. A school-located vaccination adolescent pilot initiative in Chicago: lessons learned J Pediatric Infect Dis Soc. 2013;2:198-204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Grandahl M, Tydén T, Rosenblad A, Oscarsson M, Nevéus T, Stenhammar C. School nurses’ attitudes and experiences regarding the human papillomavirus vaccination programme in Sweden: a population-based survey. BMC Public Health 2014;14:540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Black S, Rappuoli R. A crisis of public confidence in vaccines. Sci Transl Med 2010;2:61mr1. [DOI] [PubMed] [Google Scholar]
- [67].Larson HJ, Jarrett C, Eckersberger E, Smith DMD, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007-2012. Vaccine 2014;32:2150-9. [DOI] [PubMed] [Google Scholar]


