To the Editor
Subungual melanoma (SM) represents 0.7–3.5% of melanoma cases, but often carries a worse prognosis than similarly staged cutaneous melanomas.1–3 While longitudinal melanonychia (LM), a brown-black band of the nail plate, is the most common presenting sign of SM (2/3 of cases), it is not specific for SM.4 In fact, in one study, only 6.8% cases of LM showed histological evidence of SM, with the remaining cases benign etiologies including subungual hematoma, nail matrix nevus, trauma, nail apparatus lentigo, and melanocytic activation.3 Therefore, an ABC mnemonic for SM (A: Age, Asian, African, Native American; B: Band, Brown-Black, Breadth ≥ 3mm, Blurred Border; C: Change; D: Digit, Dominant hand; E: Extension of pigment to nail folds; F: Family or personal history melanoma) was developed in 2000 to facilitate early recognition of SM by physicians and the community.2
A nationwide survey-based study was performed to assess nail examinations and management of LM, using secure, anonymous online survey software provided by the Clinical and Translational Science Center at Weill Cornell Medicine. There were 402 respondents: 142 dermatology residents (PGY2-4), 58 junior attendings (<5 years post-residency), and 199 senior attendings, (5 or more years post-residency). Survey questions and responses are shown in Table 1.
Table 1.
Survey questions on nail examinations and management of longitudinal melanonychia, with responses stratified by level of clinical experience
| Survey questions and responses | Level of clinical experience* | P value† | ||
|---|---|---|---|---|
|
| ||||
| Resident (n = 142) | Junior attending physician (n = 58) | Senior attending physician (n = 199) | ||
| Do you ask your patients to remove all their nail polish during visits? | ||||
| Always | 2 (1.4) | 3 (5.2) | 27 (13.6) | <.0001 |
| Sometimes | 17 (12.0) | 18 (31.0) | 59 (29.7) | |
| Only when they complain of a nail problem | 117 (82.4) | 36 (62.1) | 105 (52.8) | |
| Never | 6 (4.2) | 1 (1.7) | 8 (4.0) | |
| How often do you examine the nails? | ||||
| Every visit | 13 (9.5) | 11 (19.0) | 47 (23.6) | <.0001 |
| Only during total body skin examinations | 55 (40.2) | 42 (72.4) | 132 (66.3) | |
| Only when the patient brings it to my attention | 69 (50.3) | 5 (8.6) | 20 (10.1) | |
| How often do you see melanonychia in your practice? | ||||
| At least once a week | 39 (27.5) | 18 (31.0) | 35 (17.6) | <.0001 |
| Approximately once a month | 81 (57.0) | 30 (51.7) | 65 (32.7) | |
| Approximately once every 3 months | 17 (12.0) | 4 (6.9) | 53 (26.6) | |
| Approximately once every 6 months | 5 (3.5) | 6 (10.3) | 46 (23.1) | |
| How confident are you with diagnosing and managing patients with melanonychia? | ||||
| Very confident | 5 (3.5) | 12 (20.7) | 54 (27.1) | <.0001 |
| Fairly confident | 49 (34.5) | 39 (67.2) | 128 (64.3) | |
| Not confident | 88 (62.0) | 7 (12.1) | 17 (8.6) | |
| When your patients present with melanonychia: | ||||
| You bring up the band to them | 99 (69.7) | 41 (70.6) | 135 (67.8) | .0002 |
| They bring up the band to you | 26 (18.3) | 15 (25.9) | 61 (30.7) | |
| Do not discuss it | 17 (12.0) | 2 (3.5) | 3 (1.5) | |
| What is your next step in management when a patient presents with a band concerning for SM? | ||||
| Continue your examination of the nails and skin | 43 (32.3) | 7 (12.7) | 40 (21.6) | .0326 |
| Schedule the patient for a biopsy specimen of the nail(s) | 43 (32.3) | 29 (52.7) | 83 (44.9) | |
| Take pictures of the nail and schedule a follow-up | 20 (15.1) | 9 (16.4) | 34 (18.4) | |
| Refer the patient to a dermatologic nail specialist | 27 (20.3) | 10 (18.2) | 28 (15.1) | |
| Are you aware of the ABC mnemonic described by Levit et al? | ||||
| Yes | 17 (12.0) | 17 (29.3) | 63 (32.0) | <.0001 |
| No | 125 (88.0) | 41 (70.7) | 134 (68.0) | |
| Correct multiple choice representation for mnemonic | ||||
| Correct | 12 (70.6) | 12 (75.0) | 43 (70.5) | 1 |
| Incorrect | 5 (29.4) | 4 (25.0) | 18 (29.5) | |
Unless otherwise noted, data are reported as number (percentage) of respondents.
P values obtained from χ2 tests for specified proportions with significance set to P < .05.
Very few physicians (32/402, 8%) asked their patients to remove nail polish at every visit. More senior attendings (13.6%) than junior attendings (5.2%) and residents (1.4%) requested that patients remove nail polish at all examinations ( , p<0.0001). In addition, only 18.2% of dermatologists perform nail examinations at each visit, with the majority (58.0%) examining nails only during total body skin examinations. More frequent nail examinations were higher amongst junior and senior attendings as compared to residents ( , p<0.0001).
Many respondents stated that they encounter melanonychia at least once a month (44%), or once a week (23%). Overall, the majority of respondents stated that they were “fairly confident” in assessing melanonychia (54.2%); however, many were “not confident” (28.0%), and less were “very confident” (17.8%). Only 8.6% and 12.1%, junior and senior attendings, respectively reported that they were “not confident”, compared to 62.0% of residents ( , p<0.0001). The most common response when asked about management of questionable melanonychia was “schedule the patient for biopsy of the nail” (41.4%). Significantly more junior (52.8%) and senior (44.9%) attendings would schedule a biopsy compared to residents (32.3%) ( , p<0.0326). Out of the 402 participants, 99 (24.8%) heard of the ABC mnemonic for SM, which comprised more junior (29.3%) and senior attendings (32.0%) than residents (12.0%) ( , p<0.0001).
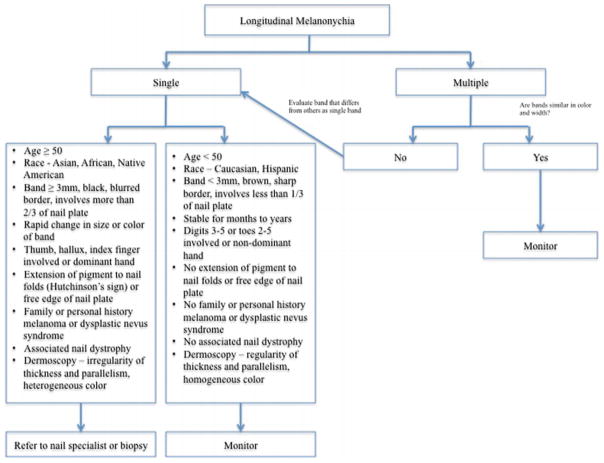
To our knowledge, this is the first study to assess nail examinations, management of LM, and knowledge of the ABC mnemonic for SM amongst dermatologists. Surprisingly, most dermatologists did not ask patients to remove nail polish during all physical examinations or examine the nails at each visit. In addition, many physicians, particularly residents, were “not confident” in managing patients with LM. Most dermatologists were not familiar with the ABC mneumonic for SM and only 41.4% would schedule a nail biopsy; while 17.7% would refer to a nail specialist after examining suspicious LM. Our data reinforce the need for increased efforts in educating dermatologists, particularly residents, about nail examinations, LM, and warning signs for SM. A flowchart depicting an algorithm for evaluation of LM is shown in Figure 1.
Figure 1.
Flowchart depicting algorithm for evaluation of longitudinal melanonychia
Acknowledgments
Funding Sources: Statistical analysis was conducted by Amanda Artis, MS, MPH who is partially supported by the following grant: Clinical and Translational Science Center at Weill Cornell Medical College (UL1-TR000457-06). There is no other source of funding.
Abbreviations
- SM
subungual melanoma
- LM
longitudinal melanonychia
Footnotes
Dr. Lipner, Dr. Scher, Amanda Artis and Pierre Halteh have no conflicts of interest relevant to the content of the submission.
References
- 1.Finley RK, 3rd, Driscoll DL, Blumenson LE, Karakousis CP. Subungual melanoma: an eighteen-year review. Surgery. 1994 Jul;116(1):96–100. [PubMed] [Google Scholar]
- 2.Levit EK, Kagen MH, Scher RK, Grossman M, Altman E. The ABC rule for clinical detection of subungual melanoma. Journal of the American Academy of Dermatology. 2000 Feb;42(2 Pt 1):269–274. doi: 10.1016/S0190-9622(00)90137-3. [DOI] [PubMed] [Google Scholar]
- 3.Jin H, Kim JM, Kim GW, et al. Diagnostic criteria for and clinical review of melanonychia in Korean patients. Journal of the American Academy of Dermatology. 2016 Jun;74(6):1121–1127. doi: 10.1016/j.jaad.2015.12.039. [DOI] [PubMed] [Google Scholar]
- 4.Haneke E, Baran R. Longitudinal melanonychia. Dermatologic surgery. 2001 Jun;27(6):580–584. [PubMed] [Google Scholar]