Abstract
Objective
To use the Structural Equation Modeling (SEM) to examined the associations between the home environment (HE), diet and physical activity (PA) factors with Hispanic children’s obesity, cardiovascular fitness (CVF), and insulin resistance (IR) measures.
Design
Cross-sectional analyses of the HE, diet and PA factors with children’s metabolic health.
Setting
Urban Community School, Wisconsin, USA.
Subjects
A total of 187 Hispanic children and their parents participated.
Methods
Children’s reported their diet and PA, and parents reported on the HE through self-administered questionnaires. Outcome variables were measured anthropometrics, CVF assessed using the Progressive Aerobic Cardiovascular Endurance Run (PACER). IR was determined with the homeostasis model assessment of insulin resistance (HOMAIR) in a subgroup of children (n=99) who participated in a one-time blood draw for fasting glucose and insulin concentrations.
Results
Parents exercise (β=0.33), home availability of PA equipment (β=0.20) and sugar-sweetened beverages (SSB) (β=0.19) were all associated with children’s PA and SSB consumption, respectively. Children’s SSB consumption (β=0.15) was associated with BMI z-score, which in turn, was associated with HOMAIR (β=0.61). In contrast, children’s PA (β=0.17) was associated with PACER z-score, which in turn was inversely associated with HOMAIR (β=−0.18). The SEM indices suggested a satisfactory model fit (Chi-square, Χ2 =53.1, comparative fix index=0.92, root-mean-squared error associated=0.04).
Conclusions
The SEM findings confirm the need to focus intervention efforts at the family level where parents are educated on making a healthier HE targeting poor diet and low levels of PA among Hispanic children who are disproportionally affected by obesity-related IR.
Keywords: Structural Equation Modeling, Home Environment, Cardiovascular Fitness, Insulin Resistance, Hispanic Children
INTRODUCTION
Childhood obesity in the United States (US) has increased dramatically in the past three decades, with 30% of US children and adolescents being overweight or obese.(1) Minority children are disproportionally affected with higher obesity rates, including Hispanic children with rates of overweight and obesity at 40% in 2010.(1) Obesity greatly increases the risk for developing type 2 diabetes (T2D), cardiovascular disease, metabolic syndrome, sleep apnea, and asthma.(2) Further, obese children manifest lower cardiovascular fitness (CVF) than their normal weight counterparts, further increasing the risk for T2D given that poor CVF is associated with decreased insulin sensitivity.(3; 4)
Obesity-related risk for T2D is likely attributed to both genetic and lifestyle factors, such as diet and physical activity (PA), (5) since genetic susceptibility alone cannot fully explain the rapid increase in obesity rates in the past three decades. The interaction between genetic susceptibility and environments that promote diets high in energy-dense, nutrient poor foods and beverages with sedentary behaviors can explain, in part, a positive imbalance and excess weight gain.(6; 7) The social-ecological models emphasize that health behaviors such as childhood obesity,(8) are affected by multiple levels of influence, including biologic, demographic, psychological, social, environmental, and policy variables.(9) Successful public health interventions often utilize this theory to address interacting environments at the individual, home, school, community, and society levels.(10) Based on the social-ecological models, past research showed that children’s risks for metabolic disease could be determined by their diet and PA, which are highly influenced by interactions in the home and school environments, which in turn, are influenced by the neighborhood community.(9; 11) Children’s diet and PA are also directly influenced by parental behaviors and home environment (HE) in providing foods and PA opportunities for childhood development. Parents not only create food and PA environments at home, but they also serve as role models influencing children’s diet and PA behaviors.(12; 13) Taken together, efforts to prevent metabolic disease should be based on understanding the dynamic interplay among the individual, parental, social, physical and nutritional layers.(14)
There has been an increasing interest in investigating associations between the HE, children’s diet and PA behaviors; however, most studies have focused on one of these factors, limiting the understanding of how all of these factors mediate an individual’s behavior within a particular environment. Existing analyses have focused on the associations between the HE or parental modeling of diet and children’s diet. (15; 16; 17) Past studies have also investigated parents PA-related behaviors and PA equipment availability at home with children’s PA. (7; 18) There was increasing volume of literature evaluating clustering of diet and PA behaviors at home in relation to children’s lifestyle behaviors or risk for obesity. (19; 20) However, to the best of our knowledge, none of these studies have extended these associations to the risk for metabolic disease. Generally, these studies only provide part of the evidence that a healthy HE and parental modeling of healthy diet and PA-related behaviors influence children’s diet and PA and therefore their risk for metabolic disease. Taken together, these studies point out the research need of evaluating how all of these interactions together may influence children’s metabolic disease.
This study set out to examine the effects of specific environmental and social factors on diet, PA, and risk for metabolic disease of Hispanic children living in an inner-city community. In social-ecological models, behavior is viewed as being affected by, and affecting multiple levels of influence. This feature enables us to examine specific influences of the social and food environments. In this regards, the Structural Equation Modeling (SEM) is a powerful statistical tool that fits the social-ecological models for multivariate analysis. The SEM incorporates simultaneous structural equations where variables may influence one-another reciprocally, either directly or through other variables as mediators.(21) Our overall hypothesis is that the HE influences the diet of an individual, while the individual diet contributes to the types of food that are available at home, therefore, implying that there is a bi-directional relationship between behavior and environment.(14) There are very few studies that have utilized the SEM approach and simultaneously evaluated the HE in relation to children’s diet or PA and consequent risk for obesity. Most important, most of these studies were primarily conducted among non-Hispanic White children, which limits the generalizability of the results.(22; 23)
To date, no such trans-disciplinary study approaches have been applied to the problem of childhood obesity, poor fitness, and risk for diabetes, let alone applied to an inner-city Hispanic community. In this study, we developed a series of SEMs to examine the associations between the HE, diet and PA factors with children’s risk for obesity (Body mass index, BMI z-score), low cardiovascular fitness (PACER z-score), and insulin resistance (HOMAIR). We previously showed that sugar-sweetened beverages (SSB) consumption was associated with Hispanic children’s BMI z-score within the home environment [Santiago-Torres et al., in press]. In the present study, we use the SEM to extend this by incorporating the interactions with physical activity to evaluate their associations with children’s BMI z-scores, PACER z-scores and HOMAIR. We hypothesized that a HE that promotes high intakes of energy-dense, nutrient-poor beverages and sedentary behaviors will be associated with children’s diet and PA, which in turn contributes to the risk for obesity-related low cardiovascular fitness (CVF), and insulin resistance (IR).
METHODS
Study population
A total of 187 Hispanic children (aged 10 to 14 years, 47% male) and 173 of their parents (75% mothers) participated in the cross-sectional study. More details on recruitment and study protocols are presented elsewhere.(24) The University of Wisconsin-Madison Institutional Review Board approved the study and all participants provided consent.
Familial Demographics and the Home Environment Assessments
Parents who participated in the study provided data on familial demographics and the HE through self-administered questionnaires that were designed for this study and are described in more details elsewhere.(24) The familial demographics form queried parents age, ethnicity and family income. The HE was assessed using a one-time home environment survey that queried parents on the home food availability, PA areas and equipment availability at home, and parents own diet and PA related behaviors. Single measures of the HE, parents diet and PA-related behaviors were taken from the most widely used and validated HE surveys.(25; 26) In details, parents were asked: ‘During the past week, did you have the following food items available at your home (e.g., SSB, sugars-sweetened beverages; soda and fruit drinks)’; ‘Does your child have any of the following areas and/or equipment available at home’ with response options, yes or no. As for parents own diet and PA-related behaviors, parents were asked: ‘Thinking about last week, how often did you consumed the following foods/beverages (e.g., SSB)?’; and ‘How often did you participate in any of the following PA-related activities’ with response options: never, once per week, 2–4 times per week, 5–6 times per week, once per day or 2 or more per day. Parents (both mothers and fathers) also self-reported on their height and weight, and these values were used to calculate their BMI as kg/m2. All of the questionnaires were available in English and Spanish.
Children’s Dietary Intake and Physical Activity Assessments
Children’s dietary intake was assessed using the Block for Kid’s Food Frequency Questionnaire (FFQ) with Hispanic foods for children, a 77-item questionnaire surveying foods and beverages consumed in the past 7 days.(27) The reliability of this questionnaire has been previously reported.(28; 29) We have previously discussed details on the diets of the Hispanic children who participated in the present study.(24) One of the food items queried by the FFQ was the consumption of SSB, including soda, fruit drinks and sport drinks, and reported intakes were expressed in grams and kilocalories (kcal) per day. In the present analyses, we focused on the consumption of SSB given their known associations with children’s BMI z-score in this cohort [Santiago-Torres et al., in press]. Children’s PA was assessed with a 3-day activity recall, the Graphs for Recalling Activity Time (GReAT) designed for the present study. We have also previously showed the use and reliability of the GReAT assessment tool [unpublished work].The activity recall queries a total of 14 activities for two weekdays and one weekend day, including, napping, study time, active travel (e.g. walking or cycling), non-active travel, watching television (TV), playing video or computer games, computer use, phone use, sports, playing, and meals.
Physical Measurements
All physical measurements were collected at the children’ community school in Wisconsin, USA. Children’s height and weight were measured with standard procedures and expressed as BMI z-scores and BMI percentile categories for age and sex according to the Center for Disease Control growth charts.(30) Cardiovascular fitness (CVF) was assessed using the Progressive Aerobic Cardiovascular Endurance Run (PACER) test, a multistage 20-meter shuttle run where subjects run back and forth along a 20-meter course, and each minute the pace to run the 20 meters distance increases. The pace is determined by beeps from a pre-recorded compact disc. The initial running speed is 8.5 km/hour, and the speed increases by 0.5 km/hour every minute. The test finishes when the subject fails to complete the 20-meter run in the allotted time twice.(31) The PACER result is “scored” as the number of laps successfully completed. Studies have shown that PACER correlates highly with VO2 max in children (r = 0.83, P <0.001).(32) PACER score was used to calculate age and sex-specific PACER z-scores as a continuous variable.(33) Insulin resistance was determine for a subgroups of children (n=99) who participated a single blood test of fasting glucose and insulin concentrations using the derived homeostasis model assessment of IR as follow: HOMAIR = (fasting glucose*fasting insulin)/22.5.(34)
Statistical Analyses
Individual and familial characteristics were summarized in terms of mean ± standard deviation (SD) for continuous variables and as percentages (%) for categorical variables. The distribution of variables was evaluated across all potential confounders, including children’s age and sex, family income, and parents BMIs. Children’s BMI z-scores and PA were not significantly different across sex, however, PACER z-scores were significantly higher among boys compared to girls (data not shown). Given our modest sample size (n=187), we included sex as a covariate in all of the statistical analyses, including the SEM presented here rather than presenting the results across sex. Correlation analyses were performed and guided the inclusion/exclusion of variables in subsequent analyses. In the present analyses we focus on SSB home availability and consumption as reported by the parents and the children as a single measure of dietary factors considered in our model. New variables were created for parental SSB consumption and home SSB availability by combining responses on soda and fruit drinks. Parental SSB consumption and PA-related behaviors were evaluated as categorical variables for reported frequency of intake and participation in PA-related behaviors, respectively, <2 times per week versus ≥2 times per week. The HE variables considered here (home availability of SSB and PA areas/equipment) were also considered as categorical variables (yes/no). Lastly, children’s reported total PA corresponds to the sum of reported time spent on sports, playing time and/or non-motorized travel (walking, riding a bicycle/scooter/skateboard, rollerblading). Total PA was averaged for the 3-day (one weekend day and two weekdays) reported activities in hours per day.
The SEM approach was then developed; the model estimation underwent several iterations, to test the hypotheses. The SEM estimated the direct and indirect associations between exogenous variables and endogenous variable (HOMAIR) in four steps. Only specific variables that contributed significantly to the model fitness and substantial meaning were kept for the next steps. First, the bi-directional associations between parents SSB and home SSB availability, as well as associations between PA-related behaviors and home PA areas/equipment availability were evaluated. In this step, only parents’ reporting on exercising at a gym or at home, aerobics, weight training, jogging, or vigorous sports, such as basketball, soccer, tennis, etc. and having basketball, baseball, tennis, or other sports equipment available at home remained significant in the model. Therefore, these two variables represented parents PA-related behaviors and PA equipment at home, respectively, in the final model. Second, the hypothesized associations between children’s SSB consumption and total PA with children’s BMI z-scores and PACER z-scores were examined. Third, the associations between children’s BMI z-scores and PACER z-scores with HOMAIR were determined. Lastly, since the authors’ previous work [Santiago-Torres et al., in press] showed that parents BMIs and family income were strongly associated with children’s BMI z-score, these variables were also included in the final model.
As the sample size is limited, the full information maximum likelihood estimator was used in model estimation such that study subjects with partially missing data could be retained in the sample. Non-normal variables (parents SSB consumption, family income, parents BMIs, and children’s HOMAIR) were transformed by taking their natural log. The model fitness was evaluated by chi-square (Χ2), relative chi-square (Χ2/d.f.), root-mean-square error of approximation (RMSEA), and comparative fit index (CFI) values. Relative chi-square values of greater than 1 and below 2 are considered good model fit. RMSEA values of less than 0.05 indicate a good model fit and values of less than 0.08 imply an acceptable model fit.(35) A good model should also exhibit a CFI value greater than 0.90.(36) The model z-test statistical significance level was set at P ≤ 0.05. Analyses were completed with Mplus (v 6.1, Muthén & Muthén, Los Angeles, CA), and SAS software (v 9.3, SAS Institute Inc., Cary, NC).
RESULTS
Children and Familial Characteristics
Children and familial characteristics are presented in Table 1. A total of 187 Hispanic children, aged 11.9 ± 1.4 years old, 47% male and one of their parents (n=173, mostly mothers) participated in the study. Hispanic families were mostly of Mexican descent (77%), and 23% were of Puerto Rican descent. Forty-seven percent of the children were healthy weight (BMI: ≥5 to 85th percentile), 25% were overweight (BMI: ≥55 to <95th percentile), and 28% were obese (BMI: ≥95 percentile). Calculated age- and sex- BMI z-scores were 0.9 ± 0.9, and PACER z-scores were 0.4 ± 0.9. Fasting blood concentrations of glucose (mg/dl) and insulin (uIU/ml) were 89.3 ± 7.2 and 17.9 ± 10.5, respectively, and were used to calculate HOMAIR (mean, 4.0 ± 2.5). According to parents self-reported anthropometrics and calculated BMI (kg/m2), 90% of the fathers and 67% of the mothers were overweight or obese (BMI ≥25 kg/m2). As for family income, most of the families (66%) reported an annual income of $35,000 or less per year.
Table 1.
Urban Hispanic Children and Familial Characteristics
| Hispanic Children Characteristics, n=187 | Percentage (%) or mean ± SD |
|---|---|
| Gender, % | |
| Male | 47 |
| Female | 53 |
| Age, y | 11.9 ± 1.4 |
| Hispanic Ethnicity, % | |
| Mexican descent | 77 |
| Puerto Rican descent | 23 |
| BMI percentile categoriesb | |
| Healthy weight: ≥ 5 to 85th percentile | 47 |
| Overweight: ≥ 85 to < 95th percentile | 25 |
| Obese: ≥ 95th percentile | 28 |
| BMI z-scorea | 0.9 ± 0.9 |
| PACER z-scorec | 0.4 ± 0.9 |
| HOMAIR, n = 99 | 4.0 ± 2.5 |
| Glucose, mg/dL | 89.3 ± 7.2 |
| Insulin, uIU/mL | 17.9 ± 10.5 |
| Familial Characteristics, n=173 | |
| BMI, kg/m2 | |
| Fathers, n=101 | 29.0 ± 4.9 |
| Mothers, n=143 | 28.0 ± 5.5 |
| Family Income, $/year | |
| 0 to <23,000 | 38 |
| 23 to <35,000 | 28 |
| 35 to <50,000 | 18 |
| ≥50,000 | 16 |
SD, standard deviation; BMI, body mass index; PACER, Progressive Aerobic Cardiovascular Endurance Run; HOMAIR, homeostasis model assessment of insulin resistance.
Main Exposure Variables within the Home Environment
Table 2 illustrates the main exposure variables that were considered for the SEM to test our main hypotheses. These included parents reported intake of SSBs and PA-related behaviors; home availability of SSBs and PA areas/equipment; and children’s SSB consumption and total PA. More than a third (≥38%) of the parent reported drinking SSB (e.g., soda or fruit drinks) at least twice a week. More than half of parents (52%) reported exercising at least twice per week, while 66% reported slow walking at least twice a week. Only 6% reported doing relaxing exercising, while 39% reported engaging in PA with their child at least twice per week. More than half of the parents reported having SSB available at home, including soda (56%) and fruit drinks (54%). PA areas and equipment availability at home is also presented in Table 2. About a third of families reported having an inside playroom (41%) and exercising room (32%) available at home, while 82% reported access to an outside nearby play area or yard. Most families reported having PA equipment at home (>69%), while only a fraction reported having winter sports (32%). Lastly, children’s reported daily intake of SSB was 74.3 ± 67.5 per 1,000 kcal and engaging in PA for about 1.5 ± 1.8 hours per day.
Table 2.
Main Exposure Variables within the Home Environment
| Parents SSB consumption and Physical Activity (PA) Behaviors | % or mean ± SD |
|---|---|
| SSB consumption, ≥ 2 times per week | |
| Soda | 42 |
| Fruit drinks | 38 |
| PA behaviors, ≥ 2 times per week | |
| Exercising | 54 |
| Heavy work | 37 |
| Moderate housework | 75 |
| Light cleaning | 79 |
| Slow walking | 66 |
| Relaxing exercising (e.g. Yoga or Pilates) | 6 |
| PA with your child | 39 |
| The Home Environment | |
| Food Availability, past 7 days | |
| Soda | 56 |
| Fruit drinks | 54 |
| PA Areas and Equipment Availability | |
| Inside playroom/area | 41 |
| Exercise room | 32 |
| Outside nearby play area/yard | 82 |
| Bicycle, rollerblades/skates, skate board/scooter, jump rode | 87 |
| Basketball, baseball, tennis, or other sports equipment | 69 |
| Winter sports equipment (e.g. ice skates, sled, skis, etc.) | 32 |
| Children’s Reported Diet and PA | |
| SSB consumption, kilocalories per 1,000 kcal | 72.3 ± 67.5 |
| Total PA, hours per day | 1.5 ± 10.5 |
SD, standard deviation; PA, physical activity; SSB, sugar-sweetened beverages
The Structural Equation Model
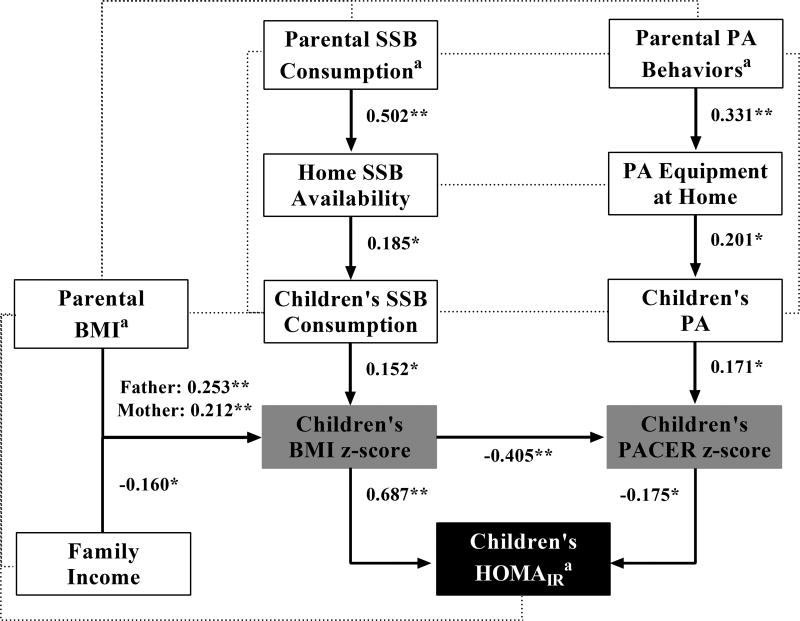
The SEM final model is illustrated in Figure 1. The associations between the HE, diet and PA factors with children’s IR (HOMAIR) were not direct, but instead were indirect through children’s body weight (BMI z-score) and CVF (PACER z-score) measures. Parents SSB consumption was positively associated with the home SSB availability (β = 0.502; P <0.01). Home SSB availability was in turn positively associated with children’s SSB consumption (β = 0.185; P <0.05). As for parents PA-related behaviors, exercising at least twice per week was positively associated with PA equipment at home (β = 0.331; P <0.01). PA equipment at home, in turn, was positively associated with children’s PA (β = 0.171; P <0.05). Children’s SSB consumption and PA were positively associated with children’s BMI z-score (β = 0.152; P <0.05) and PACER z-score (β = 0.171; P <0.05), respectively. Lastly, BMI z-score, PACER z-score and HOMAIR were all interrelated such that BMI z-score was inversely associated with PACER z-score (β = −0.405; P <0.01), and positively associated with HOMAIR (β = 0.608; P <0.01), whereas PACER z- score was inversely associated with HOMAIR (β = −0.175; P <0.05).
Figure 1. Structural Equation Modelling for the Associations between the Home Environment, Diet and PA factors with Hispanic Children’s BMI z-score, PACER z-score and HOMAIR.
Statistically significant path coefficients are presented as standardized regression coefficients (β); dashed lines represent associations that were included in the exploratory analysis, but were not significant. Model fit: Χ2 = 59.12 (d.f. = 43, P > 0.05), Χ2/d.f. = 1.37 RMSEA = 0.045 (90% C.I. = 0.000, 0.071), and CFI = 0.925.
**P value <0.01; *P value <0.05.
aVariables were log-transformed to improve multivariate normality.
bParental PA behaviors variable corresponds to exercising at a gym or at home, aerobics, weight training, jogging, or vigorous sports, such as basketball, soccer, tennis, etc.
cPA equipment at home corresponds to having basketball, baseball, tennis, or other sports equipment available at home.
dChildren’s PA corresponds to total time (hours per day) spent on sports, playing time and/or non-motorized travel (walking, riding a bicycle/scooter/skateboard, rollerblading).
eParental body mass index (BMI) as kg/m2 included both father and mother BMIs.
BMI, body mass index; CFI, comparative fix index; HOMAIR, homeostasis model assessment of insulin resistance; PA, physical activity; PACER, Progressive Aerobic Cardiovascular Endurance Run; SSB, sugar-sweetened beverages.
Both father’s and mother’s BMIs (kg/m2) were positively associated with children’s BMI z-score (β = 0.253 and β = 0.212; P <0.01, respectively). In contrast, family income was inversely associated with children’s BMI z-score (β = −0.160; P <0.05). Overall, the SEM accounted for 49% of the variance of children’s HOMAIR, 20% of the variance of children’s BMI z-score, and 20% of the variance of children’s PACER z-score. As for children’s diet and PA, the model accounted for 3% of the variance of children’s SSB consumption and 4% of children’s PA. The SEM also accounted for 25% of the variance of the home SSB availability and 10% of the variance of PA equipment available at home. The goodness-of-fit indices were: Χ2 = 59.12 (d.f. = 43, P > 0.05), X2/d.f. = 1.37 RMSEA = 0.045 (90% C.I. = 0.000, 0.071), CFI = 0.925; indicating a satisfactory model fit to data. The complete SEM results are presented in Table 3, where direct and indirect associations to children’s BMI z-scores, PACER z-scores and HOMAIR are reported.
Table 3.
Structural Equation Modelling Results for the Associations between the Home Environment, Diet and PA factors with 187 Hispanic Children’s BMI z-score, PACER z-score and HOMAIR
| From | To | |||||||
|---|---|---|---|---|---|---|---|---|
| Direct association |
Indirect Association |
|||||||
| Home SSB Availability |
PA Equipment at Home |
Children’s SSB Consumption |
Children’s PA |
Children’s BMI z-score |
Children’s PACER z-score |
Children’s HOMAIRa |
Children’s HOMAIRa |
|
| Parental SSB Consumptiona | 0.502** | - | - | - | - | - | - | 0.010 |
| (8.292) | (1.526) | |||||||
| Parents PA Behaviorsa | - | 0.331** | - | - | - | - | - | −0.002 |
| (4.607) | (−1.287) | |||||||
| Home SSB Availability | - | - | 0.185* | - | - | - | - | 0.019 |
| (2.383) | (1.560) | |||||||
| PA Equipment at Home | - | - | - | 0.201** | - | - | - | −0.006 |
| (2.636) | (−1.347) | |||||||
| Mother’sBMIa | - | - | - | - | 0.212* | - | - | 0.144* |
| (2.432) | (2.385) | |||||||
| Father’s BMIa | - | - | - | - | 0.253** | - | - | 0.172** |
| (2.856) | (2.765) | |||||||
| Family Income | - | - | - | - | −0.160* | - | - | −0.109* |
| (−2.057) | (−2.022) | |||||||
| Children’s SSB Consumption | - | - | - | - | 0.152* | - | - | 0.103* |
| (2.175) | (2.136) | |||||||
| Children’s PA | - | - | - | - | - | 0.171* | - | −0.030 |
| (2.379) | (−1.559) | |||||||
| Children’s BMI z-score | - | - | - | - | - | 0.405** | 0.608** | - |
| (−6.185) | (9.149) | |||||||
| Children’s PACER z-score | - | - | - | - | - | - | −0.175* | - |
| (−2.112) | ||||||||
BMI, body mass index; HOMAIR, derived homeostasis model assessment of insulin resistance; PA, physical activity; PACER, progressive aerobic cardiovascular endurance run; SSB, sugar-sweetened beverages.
These variables were log-transformed to improve multivariate normality.
Values in parenthesis correspond to t-statistic.
P < 0.01,
P < 0.05.
DISCUSSSION
To the best of our knowledge, this is the first study using the SEM to simultaneously examine the associations between the HE, diet and PA factors with the risk for metabolic disease among Hispanic children. The contribution of diet and PA to children’s risk for obesity and IR is well established and the strong relationships between body weight, CVF and HOMAIR have been previously reported.(32; 37) What the present study adds is the use of the SEM to simultaneously assess the associations between PA-related behaviors at home with a HE that promotes the intakes of energy-dense, nutrient poor beverages, all of which were associated with Hispanic children’s increased risk for obesity-related low CVF and IR. Our main finding is that although parental PA-related behaviors were positively associated with children’s PA and PACER through the HE, parental SSB consumption and the availability of these beverages at home seemed to contribute the most to Hispanic children’s obesity-related low CVF and IR.
The results presented here suggest that parents not only influence children’s diet and PA through modeling their diet and PA-related behaviors, but also by making certain beverages and PA equipment available at home, which ultimately could have an impact on children’s metabolic health. In other words, parents who consumed SSB more frequently were more likely to have these beverages available at home. Similarly, parents who are more physically active were more likely to have PA areas and equipment available at home, therefore providing more opportunities to their children to be physically active.(7; 20) This is consistent with what others have reported on the parental role modeling of diet and PA potential influence on children’s diet and PA, respectively, including reports on parental encouragement to be physically active impact on adolescents’ PA 5 years later. (13; 25) This is of great importance, given that children’s are forming their lifestyle behaviors at home, and the HE provides a direct effect to children’s metabolic health through dietary options being offered and opportunities for PA at home.
The SEM in addition to demonstrate the associations between the HE and children’s diet and PA, further provided the associations between these environmental variables to children’s metabolic health. A similar study evaluated the associations between the HE with children’s risk for obesity using the SEM approach, and reported that parent’s diet and PA-related behaviors were indirectly associated with children’s diet and PA through the HE.(22) They were also able to present a satisfactory model fit for these associations, but in contrast to our findings, children’s diet was not directly associated with children’s BMI z-score. Our study is also distinguishable from the findings by Hendrie et al(22) in that we were able to examine the associations between the HE with children metabolic disease in addition to obesity risk, including CVF and IR, both known risk factors for T2D.
The present study affirms that body weight and CVF are strong predictors of IR, and both were found to independently influence HOMAIR in Hispanic children. It should be noted that the final SEM underwent several interactions where the directionality of associations were extensively tested. For example, we also investigated the directionality of PACER z-scores to BMI z-scores, but the overall model fitness did not improve (data not shown). Therefore, we concluded that although the PACER-to-BMI association was significant, its magnitude was not high compared to the final model presented here. Further, in the present analyses, children’s PA, while important for CVF, did not appear to influence BMI z-score directly since the PA-to-PACER path resulted in a better model fit. In agreement with our results, some evidence suggests that obesity causes physical inactivity more than PA protects against childhood obesity.(38) Further, there is a biological rationale for PA directly contributing to CVF since PA improves insulin sensitivity by improving insulin signaling and skeletal muscle processing of glucose.(39; 40)
The main strength of our study is the use of the SEM approach to simultaneously investigate the associations between the HE, diet and PA-related behaviors with children’s risk for obesity-related low CVF and IR in one model. Second, the study is one of few conducting within race/ethnicity analyses among minority groups which are necessary to understanding the underlying mechanism by which these groups are disproportionally affected by metabolic disease. Nonetheless, our study is not without limitations. The use of self-reported measures for parents and children’s diet and PA behaviors have not been specifically validated in this group of Hispanic families and therefore, further validation is warranted. Second, parents’ anthropometrics were self-reported since parental physical measurements were not part of the main study design. However, if anything, parental obesity status as presented here could be underestimated since self-reported body weight is known to be underestimated in overweight and obese adults.(41) Third, the study is limited by the use of proxy measures of CVF (PACER) and IR (HOMAIR), however, these measures have been shown to predict metabolic disease in children.(32; 33; 34) Lastly, given the cross-sectional design, results are confined to associations and directionality of the relationships is only suggestive and cannot be presumed in the absence of longitudinal analyses.
The SEM findings demonstrate the associations between PA behaviors at home with a HE that promotes the intakes of energy-dense, nutrient poor beverages in its associations with Hispanic children’s risk for obesity-related low CVF and IR. Further, these findings suggest that targeting the parents own diet and PA-related behaviors could also have a beneficial effect on children’s own diet and PA given their role-modeling capabilities. Therefore, these findings could inform prevention strategies that includes a family component, where parents are educating on the benefits of having a healthier HE in which the availability and accessibility of SSB is reduced together with providing more opportunities for PA.
Acknowledgments
The community-engaged research project, Healthy Activities Partnership Program for Youth (HAPPY), is a partnership among staff from the Community Research Office and Bruce Guadalupe Community School at the United Community Center in Milwaukee, and researchers from the University of Wisconsin-Madison, who are members of the Wisconsin Prevention for Obesity and Diabetes (WiPOD) network. Also contributing to the success of HAPPY is funding from the UW Collaborative Center for Health Equity, an NIH/NIMHD-funded Center of Excellence in Minority Health and Health Disparities (5 P60 MD 003428).
Financial Support
Funding for this project was provided by the UW School of Medicine and Public Health from the Wisconsin Partnership Program (233-PRJ49PH), along with support from the UW Institute for Clinical and Translational Research, an NIH-funded Clinical and Translational Science Award (grant# 9U54TR000021). The sponsors had no involvement in the design, data collection or analysis.
Footnotes
Conflict of Interest
All the authors declare that there are not any conflicts of interest.
Authorship
This manuscript represents original work that has not been published previously and is currently not considered by another journal. The authors confirm that the manuscript will not be published elsewhere in the same form, in English or any other language. M. Santiago-Torres and Y. Cui contributed equally to the work. Each author has seen and approved the contents of the submitted manuscript. All authors conceived the study and participated in its design and coordination, contributed to conception and design, acquisition of data analysis or interpretation of data and revised the article critically for important intellectual content.
References
- 1.Ogden CL, Carroll MD, Kit BK, et al. Prevalence of Obesity and Trends in Body Mass Index Among US Children and Adolescents, 1999–2010. Jama-J Am Med Assoc. 2012;307:483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Park MH, Falconer C, Viner RM, et al. The impact of childhood obesity on morbidity and mortality in adulthood: a systematic review. Obes Rev. 2012;13:985–1000. doi: 10.1111/j.1467-789X.2012.01015.x. [DOI] [PubMed] [Google Scholar]
- 3.Pate RR, Wang CY, Dowda M, et al. Cardiorespiratory fitness levels among US youth 12 to 19 years of age - Findings from the 1999–2002 National Health and Nutrition Examination Survey. Arch Pediat Adol Med. 2006;160:1005–1012. doi: 10.1001/archpedi.160.10.1005. [DOI] [PubMed] [Google Scholar]
- 4.Sinha R, Dufour S, Petersen KF, et al. Assessment of Skeletal Muscle Triglyceride Content by 1H Nuclear Magnetic Resonance Spectroscopy in Lean and Obese Adolescents: Relationships to Insulin Sensitivity, Total Body Fat, and Central Adiposity. Diabetes. 2002;51:1022–1027. doi: 10.2337/diabetes.51.4.1022. [DOI] [PubMed] [Google Scholar]
- 5.Wells JCK, Siervo M. Obesity and energy balance: is the tail wagging the dog? Eur J Clin Nutr. 2011;65:1173–1189. doi: 10.1038/ejcn.2011.132. [DOI] [PubMed] [Google Scholar]
- 6.Johnson L, Mander AP, Jones LR, et al. Energy-dense, low-fiber, high-fat dietary pattern is associated with increased fatness in childhood. American Journal of Clinical Nutrition. 2008;87:846–854. doi: 10.1093/ajcn/87.4.846. [DOI] [PubMed] [Google Scholar]
- 7.Sirard JR, Laska MN, Patnode CD, et al. Adolescent physical activity and screen time: associations with the physical home environment. The international journal of behavioral nutrition and physical activity. 2010;7:82. doi: 10.1186/1479-5868-7-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bronfenbrenner U. Ecology of the family as a context for human development: Research perspectives. Developmental Psychology. 1986;22:723–742. [Google Scholar]
- 9.Booth SL, Sallis JF, Ritenbaugh C, et al. Environmental and societal factors affect food choice and physical activity: Rationale, influences, and leverage points. Nutr Rev. 2001;59:S21–S39. doi: 10.1111/j.1753-4887.2001.tb06983.x. [DOI] [PubMed] [Google Scholar]
- 10.Kumanyika SK, Obarzanek E, Stettler N, et al. Population-based prevention of obesity: the need for comprehensive promotion of healthful eating, physical activity, and energy balance: a scientific statement from American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention (formerly the expert panel on population and prevention science) Circulation. 2008;118:428–464. doi: 10.1161/CIRCULATIONAHA.108.189702. [DOI] [PubMed] [Google Scholar]
- 11.Elder JP, Lytle L, Sallis JF, et al. A description of the social-ecological framework used in the trial of activity for adolescent girls (TAAG) Health education research. 2007;22:155–165. doi: 10.1093/her/cyl059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johannsen DL, Johannsen NM, Specker BL. Influence of parents' eating behaviors and child feeding practices on children's weight status. Obesity (Silver Spring) 2006;14:431–439. doi: 10.1038/oby.2006.57. [DOI] [PubMed] [Google Scholar]
- 13.Bauer KW, Nelson MC, Boutelle KN, et al. Parental influences on adolescents' physical activity and sedentary behavior: longitudinal findings from Project EAT-II. The international journal of behavioral nutrition and physical activity. 2008;5:12. doi: 10.1186/1479-5868-5-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Davison KK, Birch LL. Childhood overweight: a contextual model and recommendations for future research. Obes Rev. 2001;2:159–171. doi: 10.1046/j.1467-789x.2001.00036.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van der Horst K, Oenema A, Ferreira I, et al. A systematic review of environmental correlates of obesity-related dietary behaviors in youth. Health education research. 2007;22:203–226. doi: 10.1093/her/cyl069. [DOI] [PubMed] [Google Scholar]
- 16.Campbell KJ, Crawford DA, Ball K. Family food environment and dietary behaviors likely to promote fatness in 5–6 year-old children. Int J Obesity. 2006;30:1272–1280. doi: 10.1038/sj.ijo.0803266. [DOI] [PubMed] [Google Scholar]
- 17.Hendrie G, Sohonpal G, Lange K, et al. Change in the family food environment is associated with positive dietary change in children. The international journal of behavioral nutrition and physical activity. 2013;10:4. doi: 10.1186/1479-5868-10-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patnode CD, Lytle LA, Erickson DJ, et al. The relative influence of demographic, individual, social, and environmental factors on physical activity among boys and girls. The international journal of behavioral nutrition and physical activity. 2010;7:79. doi: 10.1186/1479-5868-7-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rodenburg G, Oenema A, Kremers SPJ, et al. Clustering of diet- and activity-related parenting practices: cross-sectional findings of the INPACT study. Int J Behav Nutr Phy. 2013;10 doi: 10.1186/1479-5868-10-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Crawford D, Cleland V, Timperio A, et al. The longitudinal influence of home and neighbourhood environments on children's body mass index and physical activity over 5 years: the CLAN study. Int J Obesity. 2010;34:1177–1187. doi: 10.1038/ijo.2010.57. [DOI] [PubMed] [Google Scholar]
- 21.Kline RB. Principles and practice of structural equation modeling. Guilford press; 2010. [Google Scholar]
- 22.Hendrie GA, Coveney J, Cox DN. Defining the complexity of childhood obesity and related behaviours within the family environment using structural equation modelling. Public Health Nutr. 2012;15:48–57. doi: 10.1017/S1368980011001832. [DOI] [PubMed] [Google Scholar]
- 23.Heitzler CD, Lytle LA, Erickson DJ, et al. Evaluating a model of youth physical activity. American journal of health behavior. 2010;34:593–606. doi: 10.5993/ajhb.34.5.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Santiago-Torres M, Adams AK, Carrel AL, et al. Home food availability, parental dietary intake, and familial eating habits influence the diet quality of urban Hispanic children. Childhood obesity. 2014;10:408–415. doi: 10.1089/chi.2014.0051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gattshall ML, Shoup JA, Marshall JA, et al. Validation of a survey instrument to assess home environments for physical activity and healthy eating in overweight children. The international journal of behavioral nutrition and physical activity. 2008;5:3. doi: 10.1186/1479-5868-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hanson NI, Neumark-Sztainer D, Eisenberg ME, et al. Associations between parental report of the home food environment and adolescent intakes of fruits, vegetables and dairy foods. Public Health Nutr. 2005;8:77–85. doi: 10.1079/phn2005661. [DOI] [PubMed] [Google Scholar]
- 27.Block G, Hartman AM, Dresser CM, et al. A Data-Based Approach to Diet Questionnaire Design and Testing. Am J Epidemiol. 1986;124:453–469. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- 28.Block G, Thompson FE, Hartman AM, et al. Comparison of 2 Dietary Questionnaires Validated against Multiple Dietary Records Collected during a 1-Year Period. Journal of the American Dietetic Association. 1992;92:686–693. [PubMed] [Google Scholar]
- 29.Cullen KW, Watson K, Zakeri I. Relative reliability and validity of the Block Kids Questionnaire among youth aged 10 to 17 years. Journal of the American Dietetic Association. 2008;108:862–866. doi: 10.1016/j.jada.2008.02.015. [DOI] [PubMed] [Google Scholar]
- 30.Kuczmarski RJ, Ogden CL, Guo SS. 2000 CDC growth charts for the United States: Methods and development. Vital Health Stat: National Center for Health Statistics; 2002. [PubMed] [Google Scholar]
- 31.Plowman S, Meredith M. Fitnessgram/Activitygram Reference Guide. 4. Dallas, TX: The Cooper Institute; 2013. [Google Scholar]
- 32.Allen DB, Nemeth BA, Clark RR, et al. Fitness is a stronger predictor of fasting insulin levels than fatness in overweight male middle-school children. J Pediatr. 2007;150:383–387. doi: 10.1016/j.jpeds.2006.12.051. [DOI] [PubMed] [Google Scholar]
- 33.Carrel AL, Bowser J, White D, et al. Standardized Childhood Fitness Percentiles Derived from School-Based Testing. J Pediatr. 2012;161:120–124. doi: 10.1016/j.jpeds.2012.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gungor N, Saad R, Janosky J, et al. Validation of surrogate estimates of insulin sensitivity and insulin secretion in children and adolescents. J Pediatr. 2004;144:47–55. doi: 10.1016/j.jpeds.2003.09.045. [DOI] [PubMed] [Google Scholar]
- 35.Browne MW, R C, KA B, et al. Alternative ways of assessing model fit. Vol. 154. Sage Focus Editions; 1993. [Google Scholar]
- 36.Bentler PM. Comparative Fit Indexes in Structural Models. Psychol Bull. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 37.Krekoukia M, Nassis GP, Psarra G, et al. Elevated total and central adiposity and low physical activity are associated with insulin resistance in children. Metabolism: clinical and experimental. 2007;56:206–213. doi: 10.1016/j.metabol.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 38.Giammattei J, Blix G, Marshak HH, et al. Television watching and soft drink consumption - Associations with obesity in 11-to 13-year-old schoolchildren. Arch Pediat Adol Med. 2003;157:882–886. doi: 10.1001/archpedi.157.9.882. [DOI] [PubMed] [Google Scholar]
- 39.Anderson SE, Economos CD, Must A. Active play and screen time in US children aged 4 to 11 years in relation to sociodemographic and weight status characteristics: a nationally representative cross-sectional analysis. Bmc Public Health. 2008;8 doi: 10.1186/1471-2458-8-366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Houmard JA, Tanner CJ, Slentz CA, et al. Effect of the volume and intensity of exercise training on insulin sensitivity. Journal of applied physiology. 2004;96:101–106. doi: 10.1152/japplphysiol.00707.2003. [DOI] [PubMed] [Google Scholar]
- 41.Hattori A, Sturm R. The Obesity Epidemic and Changes in Self-Report Biases in BMI. Obesity. 2013;21:856–860. doi: 10.1002/oby.20313. [DOI] [PMC free article] [PubMed] [Google Scholar]