Abstract
Cardiopulmonary complications associated with epilepsy are generally associated with generalized tonic–clonic seizures, as a consequence of systemic adrenergic discharge and release of inflammatory mediators. We present a case of a 34-year-old woman with a history of Focal epilepsy since adolescence, who presented self-limited pulmonary edema following a focal to bilateral tonic–clonic seizure with subsequent resolution of the symptoms. We also made a brief review of neurogenic pulmonary edema, its proposed pathophysiology, treatment and its relation with sudden unexpected death in epilepsy (SUDEP).
Keywords: Neurogenic pulmonary edema, Focal to bilateral tonic–clonic seizure, Temporal lobe epilepsy
Highlights
-
•
Neurogenic pulmonary edema can be fatal and its early identification allows the initiation of medical surveillance and management.
-
•
Seizures are a rare cause of pulmonary edema and may be recurrent.
-
•
NPE is associated with recurrent seizures and longer epileptic seizure.
-
•
Treatment of NPE centers on resolution of CNS injury and ventilation support.
1. Introduction
Neurogenic pulmonary edema is a rare but potentially life-threatening complication of epileptic seizures, being one of the possible etiological explanations for sudden unexpected death in epilepsy (SUDEP). There is no clarity in literature of acute pharmacological treatment or interventions to prevent recurrence other than the control of ictal frequency. Here we report a case of young women with history of epilepsy, antecedent of postictal respiratory failure and a new episode of self-limited pulmonary edema.
2. Case report
A 34 years old woman was admitted at the emergency department of the San Ignacio Hospital in Bogotá - Colombia, after an episode of deja vu, palpitations and epigastric void, followed by cephalic and ocular left deviation, followed by generalized tonic posture of 1 min of duration, with a posterior confusion period of 40 min. It was established that the woman had a history of epilepsy since 16 years old treated with carbamazepine 400 mg daily with a normal neurological development and cognition. The last episode was 3 years ago associated with respiratory failure requiring orotracheal intubation and intensive care unit motoring.
On physical examination, the patient was alert, with a heart rate of 110 beats per minute, respiratory rate of 26 breaths per minute, blood pressure 120/80 mm Hg, arterial oxygen saturation of 90%, with a normal cardiopulmonary and neurological examination. A diagnosis of focal epilepsy with probable right temporal origin of unknown etiology was suspected, with normal electroencephalography and brain magnetic resonance.
The blood chemistry showed mild leukocytosis attributed to the postictal state and normal arterial gases. The electrocardiogram showed sinus tachycardia and finding related to right ventricular overload, chest X-ray within normal limits and thorax angiogram (Fig. 1) ruled out pulmonary thromboembolism. The bilateral infiltrates were compatible with pulmonary edema.
Fig. 1.
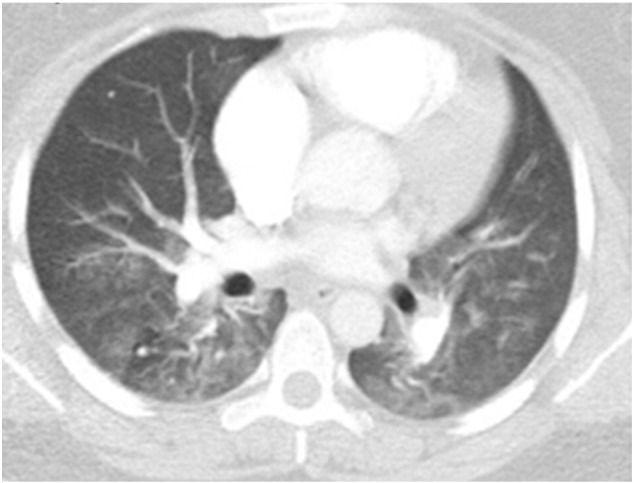
CT angiogram demonstrating bilateral pulmonary edema.
Once the diagnosis of pulmonary edema was established, clinical monitoring and low flow oxygen was implemented. The patient showed a favorable clinical course, with no dyspnea or oxygen requirements after 48 h of treatment and was discharged. In the outpatient clinic, she was asymptomatic with a transthoracic echocardiogram within normal ranges. Diagnosis of neurogenic pulmonary edema was considered as the cause of dyspnea after ruling out other cardiac or pulmonary causes.
3. Discussion
Neurogenic pulmonary edema (NPE) is defined as alveolar occupation produced very shortly after an injury to the central nervous system (CNS) [1]. The complexity of presentation complicated the understanding of its pathophysiology. However, hemodynamic, CNS and systemic inflammatory changes have been identified [1]. Several possible NPE triggers have been described, including aneurysmal subarachnoid hemorrhage, cranial trauma, spinal cord injury, stroke, epilepsy and postoperative intracranial injury.
The literature of NPE is negligible with a prevalence that varies between the studies, in up to 71% of patients with intracranial hemorrhage [1], [2] and no clear percentage in epilepsy. Clinically, NPE should be suspected in any patients suffering a CNS injury followed by acute onset of dyspnea and decreased PaO2 and FiO2 [1]. In the context of epilepsy, NPE is associated with recurrent and longer epileptic seizures. The differential diagnosis includes atelectasis and aspiration pneumonia [3], [4].
Sudden death without an identifiable cause on postmortem examination [5] is a relevant entity in people with epilepsy. Its possible etiologies are central apnea, autonomic dysregulation and NPE. The latter seems to be a frequent autopsy finding given that 52 out of 72 autopsies in patients with SUDEP had marked pulmonary edema [3], [4]. The Mortemus study [5] found that in epilepsy monitoring units, SUDEP follows early postictal severe alteration of respiratory and cardiac function induced by generalized tonic–clonic seizure, leading to immediate death after a short period of partly restored cardiorespiratory function followed by terminal apnea and cardiac arrest.
Two major mechanisms seem to produce NPE. The first one involve intense pulmonary and systemic vasoconstriction as a response to adrenergic release by brain injury [3], [4] leading to an increase in capillary hydrostatic pressure and capillary permeability. Myocardial dysfunction may then ensue resulting in dilated cardiomyopathy, volume overload, increased cardiac work, arrhythmia and, eventually, cardiac arrest [1]. The second mechanism involves inflammatory mediators secondary to endothelial damage which increases capillary permeability leading to edema [1].
Treatment of NPE centers on resolution of CNS injury and ventilation support. Specific treatments have been proposed like endothelin converting enzyme inhibitors or sympathectomy which has been successfully tested in rats [6], [7]; however, the evidence is insufficient for its use as a human treatment [2], and seizure control is essential as the only preventable treatment.
4. Conclusion
NPE is a relevant condition in patients with epilepsy and a possible preventable etiology of SUDEP. Recurrent exposure to CNS injury as in patients with epilepsy increase risk of respiratory dysfunction and fatal outcomes. Further research should focus on finding predictors of respiratory compromise in these patients and possible prophylactic interventions in addition to attempts at seizure control.
Conflicts of interest
None.
References
- 1.Baumann A., Audibert G., McDonnell J., Mertes P.M. Neurogenic pulmonary edema. Acta Anaesthesiol Scand. Apr 2007;51(4):447–455. doi: 10.1111/j.1399-6576.2007.01276.x. [Available from: http://www.ncbi.nlm.nih.gov/pubmed/17378783, [cited 2016 Jun 24]] [DOI] [PubMed] [Google Scholar]
- 2.Dutta G., Demetis S., Dutta G., Demetis S. Neurogenic pulmonary edema associated with underlying lung disease after a breakthrough seizure. Case Rep Med [Internet] 2012;2012:1–3. doi: 10.1155/2012/560942. [Available from: http://www.hindawi.com/journals/crim/2012/560942/, [cited 2016 Jun 24]] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kennedy J.D., Hardin K.A., Parikh P., Li C.-S., Seyal M. Pulmonary edema following generalized tonic clonic seizures is directly associated with seizure duration. Seizure [Internet] Apr 2015;27:19–24. doi: 10.1016/j.seizure.2015.02.023. [Available from: http://www.ncbi.nlm.nih.gov/pubmed/25844030, NIH Public Access, [cited 2016 Jun 24]] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhao H., Lin G., Shi M., Gao J., Wang Y., Wang H. The mechanism of neurogenic pulmonary edema in epilepsy. J Physiol Sci [Internet] Jan 20 2014;64(1):65–72. doi: 10.1007/s12576-013-0291-6. [Available from: http://link.springer.com/10.1007/s12576-013-0291-6, Springer Japan, [cited 2016 Jun 24]] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alison M.P. Sudden unexpected death in the epilepsy monitoring unit. Epilepsy Curr [Internet] 2014;14(2):78–80. doi: 10.5698/1535-7597-14.2.78. http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L373183488%5Cnhttp://dx.doi.org/10.5698/1535-7597-14.2.78%5Cnhttp://sfx.library.uu.nl/utrecht?sid=EMBASE&issn=15357511&id=doi:10.5698/1535-7597-14.2.78&atitle=Sudden+unexpected+death Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Herbst C., Tippler B., Shams H., Simmet T. A role for endothelin in bicuculline-induced neurogenic pulmonary oedema in rats. Br J Pharmacol [Internet] Jul 1995;115(5):753–760. doi: 10.1111/j.1476-5381.1995.tb14997.x. [Available from: http://www.ncbi.nlm.nih.gov/pubmed/8548173, [cited 2016 Jun 25]] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Poulat P., Couture R. Increased pulmonary vascular permeability and oedema induced by intrathecally injected endothelins in rat. Eur J Pharmacol [Internet] Mar 5 1998;344(2–3):251–259. doi: 10.1016/s0014-2999(97)01569-0. [Available from: http://www.ncbi.nlm.nih.gov/pubmed/9600661, [cited 2016 Jun 25]] [DOI] [PubMed] [Google Scholar]


