Abstract
Background
Evidence from a limited number of short-term trials indicates the difficulty in achieving population-level improvements in physical activity (PA) through community-wide interventions (CWIs). We sought to evaluate the effectiveness of a 5-year CWI for promoting PA in middle-aged and older adults using a cluster randomized design.
Methods
We randomized 12 communities in Unnan, Japan, to either intervention (9) or control (3). Additionally, intervention communities were randomly allocated to three subgroups by different PA types promoted. Randomly sampled residents aged 40–79 years responded to the baseline survey (n = 4414; 74%) and were followed at 1, 3 and 5 years (78–83% response rate). The intervention was a 5-year CWI using social marketing to promote PA. The primary outcome was a change in recommended levels of PA.
Results
Compared with control communities, adults achieving recommended levels of PA increased in intervention communities [adjusted change difference = 4.6 percentage points (95% confidence interval: 0.4, 8.8)]. The intervention was effective for promoting all types of recommended PAs, i.e. aerobic (walking, 6.4%), flexibility (6.1%) and muscle-strengthening activities (5.7%). However, a bundled approach, which attempted to promote all forms of PAs above simultaneously, was not effective (1.3–3.4%, P ≥ 0.138). Linear dose–response relationships between the CWI awareness and changes in PA were observed (P ≤ 0.02). Pain intensity decreased in shoulder (intervention and control) and lower back (intervention only) but there was little change difference in all musculoskeletal pain outcomes between the groups.
Conclusions
The 5-year CWI using the focused social marketing strategy increased the population-level of PA.
Keywords: exercise, network intervention, resistance training, low-back pain, dissemination, RE-AIM
Key Messages
In this first such cluster randomized trial of a long, 5-year, community-wide intervention on population-level physical activity (PA), adults achieving recommended levels of physical activities increased in the intervention communities, compared with the control (4.6 percentage points of change difference).
The intervention was effective for promoting all types of recommended physical activities, i.e. aerobic, flexibility and muscle-strengthening activities. However, a bundled approach, which attempted to promote all forms of recommended physical activities above simultaneously, was not effective.
A community-wide intervention can be an effective approach to increase population-level PA when it incorporates focused promotion strategies sustained for several years. Since the World Health Organization and other health agencies recommend multiple types of PA as a key lifestyle factor for preventing non-communicable diseases, these findings give critical insights into effective methods to disseminate those recommendations and achieve population-level improvement.
Introduction
Despite the well-known health benefits of physical activity (PA),1–3 physical inactivity remains highly prevalent globally.4 Effective population strategies to promote PA are imperative to reduce the global burden of non-communicable diseases stemming from physical inactivity.5
Considering diverse influences on PA at the individual, environmental, societal and policy levels,6 multilevel and intersectoral approaches are needed to achieve population-wide changes in PA.6,7 Community-wide interventions (CWIs) represent one approach for promoting PA. Typically, CWIs involve (i) interventions delivered across multiple community sectors; (ii) highly visible, broad-based, multi-component strategies; and (iii) may address other non-communicable disease risk factors.8,9 However, evidence on their effectiveness in achieving population-level improvements is limited. A Cochrane review published in 2015 identified 33 studies on this topic and only four high-quality studies (cluster randomized trials with a low risk of bias) among them.10 Overall, the review did not find evidence of beneficial changes in PA resulting from CWIs.10
What remains unclear is whether the absence of benefit stems from the nature of the CWI itself (e.g. the dose, duration, components or complexity of the interventions) or just a lack of sufficient high-quality studies able to detect the anticipated small to moderate effect size. Of note, the most frequent (modal) duration of the intervention in the reviewed studies was 1 year (median 3 years).10 In contrast to individual-level interventions, it may take considerably longer to influence population levels of PA via large-scale interventions. To date, no randomized controlled trial (RCT) has examined a CWI lasting for 4 years or more.
RCTs of social interventions are increasingly popular in public health and other disciplines such as education and economics; however, these broad-reach trials typically face methodological challenges due to their complex nature and real-world research environments that are difficult to control.11 Accumulation of empirical evidence and advancement in epidemiologic methods in this field may benefit a broad range of scientific knowledge.
The COMMUNICATE (COMMUNIty-wide CAmpaign To promote Exercise) study was originally developed as a 1-year cluster RCT to evaluate the effectiveness of a multi-strategic CWI for promoting PA in middle-aged and older adults.12 Then the intervention was continued for a further 4 years when no significant effect on population-level change in PA was seen after the first and third years.12,13 We therefore evaluated the effectiveness of a 5-year CWI for promoting PA in middle-aged and older adults using a cluster RCT design. Our aim was to promote PA through a CWI delivered at the community level. To minimize contamination, the unit of randomization was the community. The hypothesis was that a 5-year CWI delivered at the community level would promote engagement in recommended levels of aerobic, flexibility and/or muscle-strengthening activities in middle-aged and older adults evaluated at the individual level.
Methods
This study reports on findings after 5 years of intervention in the COMMUNICATE study. This is a cluster randomized controlled, superiority trial, stratified by population density, with unbalanced randomization (three intervention communities and one control community). The study location was Unnan City (population 45 364, area 553.7 km2), Shimane Prefecture, Japan. Full details of the original trial protocol can be found elsewhere12 and the original 1-year trial showed short-term effects on the campaign awareness and knowledge of the residents as the first published RCT study to examine the effectiveness of CWI in adults.12 This extended 5-year study was approved by the research ethics committee of the Physical Education and Medicine Research Center UNNAN (H25–2–5–1) and was prospectively registered at UMIN-CTR (UMIN000012464).
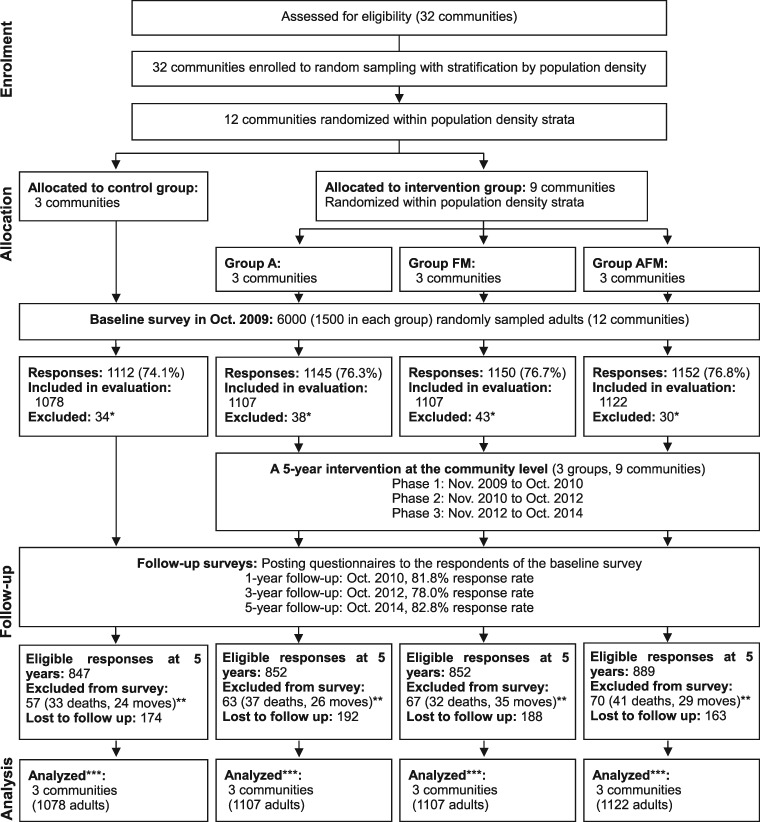
Figure 1 is the flow diagram of the trial. There are 32 communities within Unnan, with a median population and area of 1292 and 10.8 km2, respectively. The eligibility criterion for clusters was all communities in Unnan. Twelve communities (clusters) were randomly sampled, with stratification by blocking within population density category strata, and random allocation to three intervention clusters per control cluster (i.e. nine interventions; three controls). Additionally, each cluster in the intervention group was randomly allocated to aerobic activity promotion (Group A), flexibility and muscle-strengthening activities promotion (Group FM) or aerobic, flexibility and muscle-strengthening activities promotion (Group AFM, ‘all-in-one’ or bundled approach), each consisting of three clusters. This factorial design was for the purpose of subgroup analyses. We chose these three types of activities because, in addition to aerobic activity, muscle-strengthening activity is recommended for adults in general,2,3 whereas flexibility activity is especially recommended for older adults and people with musculoskeletal disorders.14–18 However, most previous CWI studies focused on only aerobic activity (e.g. walking).9,19–27 As arthritis is a potential barrier to PA, mainly aerobic activity,28 identifying effective population strategies to promote flexibility and musculoskeletal activities and prevent musculoskeletal disorders is important.
Figure 1.
Flowchart of the study. Group A, aerobic activity; Group FM, flexibility and muscle-strengthening activities; Group AFM, aerobic, flexibility and muscle-strengthening activities. *Respondents who could not walk unaided. **Accumulated numbers of deaths and moves since baseline survey. ***Analysed with missing data imputation.
Random selection and allocation of the clusters were performed by two clerical staff members of Unnan City Hall, who were not involved in the remainder of the study. A staff member created a matched list of numbers (used later as selected community ID × assignment group ID) by using computer-generated random numbers. Another prepared ID lists of (i) communities and (ii) assignment group were not given to the staff member to conceal the actual allocation of each community. Then the other staff member used the created list of numbers and the ID lists to assign communities (clusters).
Intervention
The 5-year CWI (November 2009 to October 2014) was conducted as an Unnan City Hall public health project targeting all middle-aged and older (40–79 years) community-dwelling residents. In Group A, mainly walking was promoted. In Group FM, stretching exercises and muscle-strengthening activities focused on key muscle groups for treating low-back and knee pain.16,29,30 In Group AFM, all the exercises (walking, stretching and muscle-strengthening activities) were promoted as a bundle.
The intervention adopted social marketing techniques.31 Social marketing techniques apply marketing principles to create, communicate and deliver value that influences target audience behaviours that benefit society as well as the target audience.31 The detailed strategy can be found elsewhere.12 Briefly, the CWI adopted the following processes: (i) situational analysis, (ii) market segmentation and targeting, (iii) setting objectives and (iv) marketing strategy development (supplementary eText). Cooperative partnerships were developed with local organizations.
Throughout the intervention period, the CWI consisted of three components: (i) information delivery (e.g. flyers, posters, local audio broadcasts), (ii) education (e.g. outreach health education programme and encouragement by professionals to individuals as well as to the public during community events) and (iii) support delivery (e.g. promoting encouragement by community leaders, network intervention).32 Details of each component, implementation evaluation and methods to minimize contamination between communities and control the dose of the intervention are described in the Supplementary eText, available as Supplementary Data at IJE online. Sample materials for the intervention are available elsewhere.12,13 In addition to the implementation evaluation, the RE-AIM framework (i.e. Reach, Effectiveness, Adoption, Implementation, and Maintenance)33 was used to assess the public health impact and the external validity of the intervention. Our intervention met the definition of a CWI.34 In the control communities, public health services were delivered by Unnan municipality as usual.
Population-based evaluation
The effectiveness of our intervention was evaluated by population-based surveys designed as a representative cohort. As a baseline, self-administered questionnaires were mailed to a random sample of participants in October 2009. A computer-based resident registry system was used for random sampling. The sampling frame (eligible respondents) was all men and women aged 40–79 years living in the 12 communities. Those excluded from the survey were individuals in assisted living facilities and those who required long-term care. Those who could not complete the questionnaires themselves due to disability and those unable to walk unaided were also excluded from the analyses; 1-, 3- and 5-year follow-up questionnaires were mailed to the baseline respondents in October 2010, 2012 and 2014. Those who had died or moved were excluded from the follow-up surveys but were included in the primary analysis.
All respondents gave written informed consent to participate in these surveys at baseline. Both participants and data collectors were randomly sampled residents. Residents and the CWI collaborators (e.g. community self-administered organization staff) were blinded to (not informed about) the study design and hypothesis (i.e. the existence of the control group and cluster allocation).35 The implementing staff of the CWI (intervention providers), data analysts and the Mayor, Vice-Mayor, supervisory employees and public health nurses of Unnan City Hall were not blinded to the cluster allocation.
Measures
Primary outcome
Our primary outcome was the change in engagement in regular PA (overall PA) evaluated at the individual level from baseline to 5-year follow-up. If respondents met any one of the following conditions, they were defined as ‘engaging in regular PA’: (i) ≥150 minutes/week of walking, (ii) daily flexibility activity or (iii) ≥2 days/week of muscle-strengthening activity. The thresholds were based on the current PA recommendations.1,3,14 A daily threshold for flexibility activity was chosen because flexibility activity had been recommended, preferably, on all days that aerobic or muscle-strengthening activity is performed.14
Respondents were asked about the number of days per week and the mean number of minutes walked per day, for recreation and transport separately, to give the weekly total minutes of walking time. Frequency of flexibility activity was assessed categorically (daily, not daily but occasionally, not at all). The weekly number of days performed was asked for muscle-strengthening activity. The PA questionnaire is available elsewhere.13 Both the test–retest reliability over 10 days and criterion-related validity with an accelerometer of the walking questionnaire were acceptable (Spearman’s r = 0.79 and 0.38, respectively).12,36 The test–retest reliability of the flexibility and muscle-strengthening activities were also acceptable (weighted kappa = 0.72 for flexibility and Spearman’s r = 0.75 for muscle-strengthening activity).12
Secondary outcomes
Musculoskeletal pain was evaluated to represent possible benefits (or harm) related to the CWI.12,37 The pain locations were shoulder, low back and knee. Chronic musculoskeletal pain was defined as current pain lasting longer than 3 months within the past 12 months.38 A visual analogue scale (VAS) from 0 mm (no pain) to 100 mm (most intense pain) was used to assess the average pain intensity experienced during the last few days.39 The test–retest reliability had moderate and acceptable values of Cohen’s kappa for chronic pain (0.68 for shoulder; 0.49 for low back; 0.72 for knee) and Spearman’s r for VAS scores (0.80 for shoulder; 0.70 for low back; 0.78 for knee).12
All outcomes remained the same as the pre-specified ones in the original 1-year trial. As covariates, body mass index (BMI) calculated from self-reported weight and height in kg/m2, self-rated health, years of education, employment status, engagement in farming and chronic disease history were examined by the baseline questionnaire. Information on sex and age were also gathered from the resident registry system. For exploratory purposes, we also evaluated awareness of the CWI at 1-, 3- and 5-year follow-ups (Supplementary eText, available as Supplementary Data at IJE online).12
Statistical analysis
As for the original 1-year investigation, the planned sample size of nine clusters comprising 4500 participants in the intervention arm and three clusters comprising 1500 participants in the control arm was calculated on the assumption of a 50% response rate (i.e. total 3000 analysed participants) to detect an 8% difference in change in regular PA between the intervention and control groups, taking into account the design effect due to clustering.12,40 Based on available data, the estimated rate of regular PA at baseline was 58% with an estimated intra-cluster correlation coefficient of 0.00174. The chi-squared test was used with unbalanced randomization (3:1), a two-sided 5% significance level and a power of 90%.
Primary and secondary analyses
Multilevel analyses, taking into account the multiple measurements (four time points: baseline, 1-, 3- and 5-year follow-ups), were performed. The change difference between nine intervention and three control clusters was calculated for the primary outcome of regular PA (overall PA) from baseline to 5-year follow-up using a generalized linear mixed model (GLMM) with sex, age, BMI, self-rated health, years of education, employment, farming, chronic low-back and knee pain, chronic disease history, community (cluster) where respondents lived, time effect, group allocation (intervention or control), and the interaction between time and group as fixed effects, and individuals as a random effect. Community (cluster) was included as a fixed effect to partial out all the observed and unobserved time-invariant community-level confounding factors.41
As pre-specified secondary analyses, each intervention subgroup (Groups A, FM and AFM) was compared with the control communities for changes in each of the different activities (e.g. walking) using GLMM. Changes in chronic musculoskeletal pain prevalence and VAS pain scores for shoulder, low back and knee were also analysed by GLMM with further adjustment for baseline PA. In addition, pre-specified subgroup analyses were conducted after stratification by sex, age group (40–59 and 60–79 years) and the marketing segment (primary communication target segment, i.e. inactive women aged 60–79 years who had low-back or knee pain at baseline and the remaining population; see Supplementary eText, available as Supplementary Data at IJE online).
As post hoc exploratory analyses, we analysed the associations of cumulative awareness score with prevalence and uptake of regular PA at 5-year follow-up to test the hypothesized logic model12 (Supplementary eText and eFigure 2, available as Supplementary Data at IJE online).
Analyses were performed on an intention-to-treat basis and included all baseline respondents who could walk unaided. Missing information, ranging from 0% for sex and age to 34% for walking time, was imputed to minimize bias due to missing information and repeated nine times, under the assumption of missing at random.42 Each imputation was based on regression models including variables used in the analyses. The 10 imputed datasets were analysed independently and combined for inference. To check whether there was any differential attrition on overall PA, the previous survey values for those respondents with missing PA values were identified.43 Sensitivity analyses were performed by using (i) data after excluding adults who deceased during the follow-up and (ii) complete cases only with respondents who had no missing values. Analyses were carried out using SAS version 9.4 (SAS Institute Inc., Cary, NC).
Results
For the implementation evaluation, the doses of the implemented information, education and support delivery in the intervention communities and public health services in the control communities are described along with the RE-AIM flowchart in the Supplementary File (eTable 1 and eFigure 5, available as Supplementary Data at IJE online). All three dimensions of the CWI were clearly implemented, and mostly delivered as intended, in all intervention communities. The RE-AIM flowchart shows high degrees of adoption, implementation, reach and organizational-level maintenance.
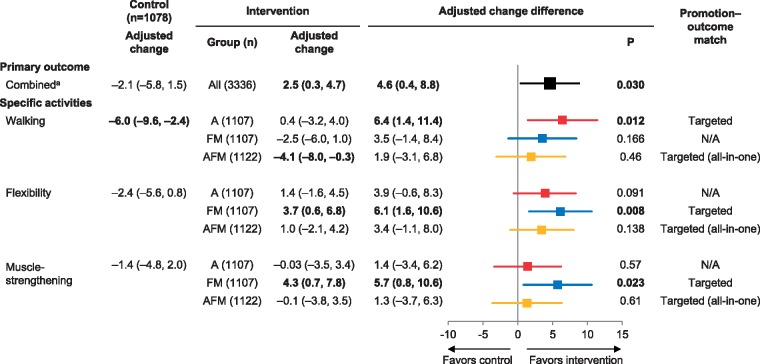
For effectiveness evaluation, data from a total of 4414 respondents (73.6% response rate at baseline) were analysed in the intention-to-treat manner (Figure 1). Follow-up surveys also had high response rates (78.0–82.8%). Baseline characteristics of the eligible respondents are presented in Table 1. Table 2 shows the unadjusted distributions of PA and pain outcomes at baseline and the 5-year follow-up. During the 5-year period, the proportion of adults achieving the recommended levels of PAs decreased from 64.5% (573/889) to 59.2% (432/730) in the control communities, whereas levels were maintained in the intervention communities [63.0% (1745/2769) in 2009 to 63.7% (1446/2270) in 2014]. The adjusted change in PA within group and the adjusted change difference between groups (effect estimate) are presented in Figure 2. For the primary analysis, the adjusted change difference (%) of residents who met the PA recommendations indicated a positive intervention effect in the treatment compared with the control communities {4.6 percentage points [95% confidence interval (CI): 0.4, 8.8], P = 0.030}. For specific PA outcomes, in the control communities, adults who walked ≥150 minutes/week decreased after adjustment of covariables [–6.0 percentage points (95% CI: –9.6, –2.4)], whereas overall and other types of PA showed similarly negative trends. Compared with the control communities, adults walking ≥150 minutes/week increased in Group A [6.4% (1.4, 11.4), P = 0.012] and adults doing flexibility activity daily [6.1% (1.6, 10.6), P = 0.008] and 2 days/week or more of muscle-strengthening activity [5.7% (0.8, 10.6), P = 0.023] increased in Group FM, corresponding to the PA types promoted in the relevant communities (Figure 2). The proportion of active walkers did not change within Group A [0.4% (–3.2, 4.0)]. Thus, the observed change differences in walking were due to the decrease in the control communities aforementioned (i.e. effectively maintained in Group A). In Group AFM (all-in-one approach), there was little change compared with the control (P ≥ 0.138).
Table 1.
Baseline characteristics of participants randomly selected from communities: COMMUNICATE Study
| Control | Intervention |
||||
|---|---|---|---|---|---|
| All | Group A | Group FM | Group AFM | ||
| Cluster | 3 | 9 | 3 | 3 | 3 |
| Residents, n | 5235 | 14 721 | 3700 | 5553 | 5468 |
| Residents aged 40–79 years, n | 2917 | 7493 | 2132 | 2743 | 2618 |
| Population density, mean (SD), /km2 | 131 (137) | 273 (371) | 433 (641) | 145 (46) | 240 (268) |
| Evaluation participants (eligible response rate) | 1078/1500 (71.9%) | 3336/4500 (74.1%) | 1107/1500 (73.8%) | 1107/1500 (73.8%) | 1122/1500 (74.8%) |
| Male | 510/1078 (47.3%) | 1540/3336 (46.2%) | 522/1107 (47.2%) | 517/1107 (46.7%) | 501/1122 (44.7%) |
| Age, mean (SD), years | 61.0 (10.6) | 60.7 (10.5) | 61.2 (10.7) | 60.1 (10.4) | 60.6 (10.5) |
| 40–59 | 471 (43.7%) | 1514 (45.4%) | 477 (43.1%) | 522 (47.2%) | 515 (45.9%) |
| 60–79 | 607 (56.3%) | 1822 (54.6%) | 630 (56.9%) | 585 (52.8%) | 607 (54.1%) |
| Body mass index, mean (SD), kg/m2 | 22.5 (3.2) | 22.6 (3.1) | 22.8 (3.2) | 22.3 (2.9) | 22.6 (3.0) |
| <18.5 | 83 (8.1%) | 226 (7.0%) | 62 (5.9%) | 88 (8.2%) | 76 (6.9%) |
| ≥18.5 to <25 | 744 (72.2%) | 2352 (72.9%) | 770 (72.8%) | 804 (74.8%) | 778 (71.1%) |
| ≥25 | 204 (19.8%) | 650 (20.1%) | 226 (21.4%) | 183 (17.0%) | 241 (22.0%) |
| Self-rated health | |||||
| Excellent/good | 878 (81.9%) | 2722 (82.7%) | 885 (80.8%) | 902 (83.0%) | 935 (84.3%) |
| Fair/poor | 194 (18.1%) | 569 (17.3%) | 210 (19.2%) | 185 (17.0%) | 174 (15.7%) |
| Years of education, mean (SD) | 11.5 (2.3) | 11.5 (2.4) | 11.5 (2.4) | 11.4 (2.3) | 11.5 (2.5) |
| Employed | 695/998 (69.6%) | 2101/3058 (68.7%) | 665/1030 (64.6%) | 711/1015 (70.0%) | 725/1013 (71.6%) |
| Engagement in farming | 552/1054 (52.4%) | 1628/3271 (49.8%) | 466/1091 (42.7%) | 627/1078 (58.2%) | 535/1102 (48.6%) |
| Chronic disease historya | 659/1078 (61.1%) | 2059/3336 (61.7%) | 679/1107 (61.3%) | 673/1107 (60.8%) | 707/1122 (63.0%) |
Group A = aerobic activity; Group FM = flexibility and muscle-strengthening activities; Group AFM = aerobic, flexibility and muscle-strengthening activities. SD, standard deviation. Figures are n (%), n/N (%) or mean (SD) before imputation of missing values unless stated otherwise. Sample sizes (denominators) vary due to missing values.
aHaving the following disease history: hypertension, hyperlipidaemia, diabetes, hyperuricemia, cerebrovascular disease, heart disease, kidney and urologic diseases, liver disease, gastrointestinal disease, endocrine disease, cancer.
Table 2.
Distribution of physical activity and pain outcomes at baseline and 5-year follow-up
| Control (n = 1078) | Intervention (n = 3336) | Subgroups |
ICCa | |||
|---|---|---|---|---|---|---|
| Group A (n = 1107) | Group FM (n = 1107) | Group AFM (n = 1122) | ||||
| Overall regular physical activityb, n | ||||||
| At baseline | 573/889 (64.5%) | 1745/2769 (63.0%) | 614/922 (66.6%) | 526/902 (58.3%) | 605/945 (64.0%) | |
| At 5 years | 432/730 (59.2%) | 1446/2270 (63.7%) | 510/766 (66.6%) | 451/731 (61.7%) | 485/773 (62.7%) | 0.0032 |
| Total walking time, min/week | ||||||
| Median (IQR) at baseline | 60 (0–210) | 60 (0–200) | 80 (0–210) | 60 (0–180) | 60 (0–200) | |
| Median (IQR) at 5 years | 40 (0–170) | 60 (0–210) | 80 (0–210) | 43 (0–210) | 60 (0–191) | |
| ≥150, n at baseline | 311/824 (37.7%) | 914/2511 (36.4%) | 319/838 (38.1%) | 282/828 (34.1%) | 313/845 (37.0%) | |
| ≥150, n at 5 years | 198/665 (29.8%) | 736/2091 (35.2%) | 283/701 (40.4%) | 222/675 (32.9%) | 231/715 (32.3%) | 0.0054 |
| Flexibility activity daily, n | ||||||
| At baseline | 253/1036 (24.4%) | 772/3242 (23.8%) | 276/1067 (25.9%) | 214/1081 (19.8%) | 282/1094 (25.8%) | |
| At 5 years | 173/820 (21.1%) | 640/2495 (25.7%) | 217/828 (26.2%) | 190/812 (23.4%) | 233/855 (27.3%) | 0.0039 |
| Muscle-strengthening activity, days/week | ||||||
| Median (IQR) at baseline | 0 (0–3) | 0 (0–3) | 1 (0–3) | 0 (0–3) | 0 (0–3) | |
| Median (IQR) at 5 years | 0 (0–3) | 0 (0–3) | 0 (0–4) | 0 (0–3) | 0 (0–3) | |
| ≥2, n at baseline | 348/916 (38.0%) | 1080/2862 (37.7%) | 390/954 (40.9%) | 310/938 (33.1%) | 380/970 (39.2%) | |
| ≥2, n at 5 years | 278/796 (34.9%) | 910/2444 (37.2%) | 307/805 (38.1%) | 285/796 (35.8%) | 318/843 (37.7%) | 0 |
| Chronic musculoskeletal pain | ||||||
| Shoulder at baseline | 158/1033 (15.3%) | 554/3187 (17.4%) | 176/1062 (16.6%) | 203/1048 (19.4%) | 175/1077 (16.3%) | |
| Shoulder at 5 years | 149/824 (18.1%) | 455/2515 (18.1%) | 144/829 (17.4%) | 156/822 (19.0%) | 155/864 (17.9%) | 0 |
| Low back at baseline | 133/1020 (13.0%) | 441/3152 (14.0%) | 145/1047 (13.9%) | 150/1043 (14.4%) | 146/1062 (13.7%) | |
| Low back at 5 years | 120/816 (14.7%) | 383/2516 (15.2%) | 123/820 (15.0%) | 129/832 (15.5%) | 131/864 (15.2%) | 0 |
| Knee at baseline | 95/1041 (9.1%) | 360/3220 (11.2%) | 115/1069 (10.8%) | 122/1068 (11.4%) | 123/1083 (11.4%) | |
| Knee at 5 years | 80/821 (9.7%) | 304/2488 (12.2%) | 101/816 (12.4%) | 96/821 (11.7%) | 107/851 (12.6%) | 0 |
| Median (IQR) VAS pain score | ||||||
| Shoulder at baseline | 20 (0–48) | 22 (0–48) | 22 (0–49) | 22 (0–48) | 20 (0–48) | |
| Shoulder at 5 years | 12 (0–38) | 12 (0–41) | 11 (0–44) | 14 (0–39) | 12 (0–42) | 0 |
| Low back at baseline | 5 (0–32) | 8 (0–36) | 8 (0–36) | 9 (0–37) | 7 (0–32) | |
| Low back at 5 years | 4 (0–27) | 5 (0–28) | 5 (0–29) | 5 (0–28) | 5 (0–26) | 0 |
| Knee at baseline | 0 (0–7) | 0 (0–13) | 0 (0–15) | 0 (0–11) | 0 (0–12) | |
| Knee at 5 years | 0 (0–7) | 0 (0–14) | 0 (0–13) | 0 (0–13) | 0 (0–15) | 0 |
Group A = aerobic activity; Group FM = flexibility and muscle-strengthening activities; Group AFM = aerobic, flexibility and muscle-strengthening activities; IQR, interquartile range; SD, standard deviation; VAS, visual analogue scale. Figures are n/N (%) or median (IQR) before imputation of missing values unless stated otherwise. Sample sizes (denominators) vary due to missing values.
aIntracluster correlation coefficient (ICC) of each outcome variable at 5-year follow-up was calculated by using samples without imputation as follows: ICC = (BMS – WMS)/(BMS + [K – 1] WMS), where BMS is the between-cluster mean square, WMS is the within-cluster mean square and K is the average number of respondents per cluster. ICC is displayed as zero if the estimated value is smaller than zero.
bEngagement in regular aerobic, flexibility and/or muscle-strengthening activities. If respondents met any one of the following three conditions, the respondents were defined as ‘engaging in regular physical activity’: (i) engaging in 150 min/week or more of walking, (ii) engaging in daily flexibility activity or (iii) engaging two or more days/week in muscle-strengthening activities.
Figure 2.
Effect of community-wide intervention on changes in population-level physical activity. Group A = aerobic activity; Group FM = flexibility and muscle-strengthening activities; Group AFM = aerobic, flexibility and muscle-strengthening activities. Estimates are percentage points with their 95% confidence intervals in parentheses; and they are adjusted for sex, age, body mass index, self-rated health, years of education, employment status, engagement in farming, chronic low-back and knee pain, chronic disease history and community (cluster) where respondents lived. All subgroups were analysed simultaneously. An adjusted change difference greater than zero signifies that the intervention had a positive effect (favourable for physical activity) compared with the control group. Boldface indicates P < 0.05. aEngagement in regular aerobic, flexibility and/or muscle-strengthening activities. If respondents met any one of three following conditions, they were defined as ‘engaging in regular physical activity’: (i) ≥150 mins/week of walking, (ii) daily flexibility activity or (iii) ≥2 days/week of muscle-strengthening activity.
Pre-specified subgroup analyses suggested positive intervention effects on regular PA across all categories of sex, age and the marketing segment, with wider CIs due to smaller samples (adjusted change difference = 3.1–6.3%, P for heterogeneity ≥ 0.43, Supplementary eFigure 3, available as Supplementary Data at IJE online). The exploratory analyses showed adults with a higher cumulative awareness score had higher prevalence (P for trend = 0.0002) and uptake rate (P for trend = 0.02) of regular PA (Supplementary eFigure 4, available as Supplementary Data at IJE online).
For pain outcomes, pain intensity decreased in shoulder (intervention and control) and lower back (intervention only) but there was little change difference (prevalence or intensity) between intervention and control groups (Supplementary eTable 2, available as Supplementary Data at IJE online). Similarly, post hoc subgroup analyses showed little change difference among the primary communication target those who reported pain at baseline (data not shown). Supplementary eTable 3, available as Supplementary Data at IJE online, presents the previous survey’s regular PA prevalence for adults who had missing PA information at each follow-up. In both intervention and control groups, the prevalence was consistently lower than that in the total sample throughout the study period, and no clear differential attrition was observed. Sensitivity analyses with the exclusion of deceased adults and with the complete cases yielded similar results to the main analysis, with wider CIs for the complete cases.
Discussion
This cluster RCT with a long-term (5-year), whole-community intervention showed the CWI effects in improving population-level PA. Our focused promotion strategy was effective in increasing each type of recommended physical activities (for walking, effective in maintaining the level). The intervention effect gradually shifted towards indicating population-level improvement (1.6% change difference at 3-year13 and 4.6% at 5-year follow-ups) for the primary outcome. Our causal interpretation is also supported with (i) improvements in the specific types of PA as targeted by the CWI in the relevant communities (i.e. promotion-outcome match; walking in Group A and flexibility and muscle-strengthening activities in Group FM, respectively) as well as (ii) the linear dose–response relationship between the CWI awareness and the change in PA in line with the hypothesized logic model.12
To our knowledge, this study is the first RCT to examine the effectiveness of a CWI for promoting PA over an intervention period of ≥5 years.10 In addition to the effectiveness of CWIs itself, it is also not known how long a CWI should be conducted to increase PA at the population level. As mentioned above, the most frequent duration of CWIs in the 33 studies in the recent Cochrane review was 1 year (median 3 years), of which high-quality studies failed to achieve population-level PA improvement.10 The current study yielded 4.6% change difference from a 5-year CWI. Another previous systematic review reported a similar finding; the median net increase in the percentage of people who reported being physically active as a result of a community-wide campaign was 4.2% (range, –2.9% to 9.4%) with a median intervention duration of 5 years, although this review was based solely on non-randomized studies and it did not investigate the durations.9 The CWIs should be sustained over several years to expect modest population-level improvements in PA.
An observational study of community-wide programmes targeting risk factors of cardiovascular disease including PA in Franklin County, Maine, USA, suggested these decades-long programmes were associated with reductions in hospitalization and mortality rates over 40 years.44 The previous successful long-term community-wide cardiovascular prevention programmes, including this Franklin project and the North Karelia project in Finland,45 have not provided confirmatory evidence of population-level improvement of PA. Further investigation is needed to clarify how long-term CWI could increase and maintain population-level PA and eventually result in the prevention of non-communicable diseases and premature mortality.
In addition to the question of duration, the content and the dose of intervention need to be considered. The current intervention deployed all six social marketing benchmark criteria,12,46 which is rare in PA interventions in older populations.47 The standardized protocol, training of core team staff members12 and the dose monitoring contributed to the quality control and dose levelling of the CWI between communities. In Group AFM, where all three types of PA were promoted, the amount of information delivered was greater than that for the other groups, thus the burden on the residents might also be greater. If the CWI could succeed in motivating adults to perform all types of PA, then the achieved health benefit would be the greatest.1,14 For the successful dissemination of the current PA recommendations, which include multiple types of PA, a phased strategy (e.g. aerobic activity in the first phase and muscle-strengthening activity later) is worth considering especially when resources are limited. Finally, although the present CWI included multi-dimensional approaches, a more comprehensive approach involving policy and built environmental change strategies might increase the observed intervention effects.9,34
This study has several strengths. First, a cluster RCT can be considered as the optimal design to develop practice-based evidence.48 The original 1-year investigation was rated in the Cochrane review to have the lowest risk of bias among the selected 33 studies.10 Second, the prospective cohort design with repeated measurements enabled individual-level analysis and had more statistical power compared with multiple cross-sectional sampling. A potential disadvantage of this design is the risk of attrition bias. However, the high response rate with the adoption of established methods to increase the response rate12,49 provided less risk for biased results, and no clear differential attrition was observed. Third, confirmation of no harm of the CWI by using a pain questionnaire, which is not often considered in broad-reaching PA interventions, is also a strength of this study. As the logic model hypothesized, if the CWI could improve pain symptoms, this would occur after PA increased,12 and thus more follow-up time would be needed to capture it. Finally, this study examined all aspects of the RE-AIM framework33 to assess the public health impact of the intervention (Supplementary eFigure 5, available as Supplementary Data at IJE online). Collaborations with community organizations and utilization of existing resources realized a high (100%) adoption and implementation rate of the CWI components and long-term maintenance of the self-organized activities. The high implementation adherence of this CWI project, along with the other examples of long-term implementation of CWIs in different countries and settings from urban to rural,9,20 suggests good applicability of the CWI to other locations. Key strategic components shared by such successful cases yielding long-term implementation of quality CWIs should be further investigated to translate this practice-based evidence into policy and dissemination;48 e.g. those keys may be high community engagement, a financially stable headquarters, an interdisciplinary team and/or state-of-the-art social marketing.
However, there are also limitations. First, a self-administered questionnaire might be subject to recall bias. In broad-reaching trials, objective measures (e.g. accelerometers) are often prohibitively expensive, burdensome to participants and logistically difficult, thus resulting in a low response rate50 with potential risk of selection bias. Therefore, self-report measures must be relied on and have been suggested as useful for their comparability of population PA estimates and low respondent burden.51 Additionally, there is no standard method to objectively assess flexibility and muscle-strengthening activities in population-wide studies.52 Using questionnaires with acceptable reliability is a strength of this study and differential measurement error is unlikely to have occurred. Second, potential contamination of the intervention via social networks possibly occurred. Although we assumed older adults mostly interacted within their communities, contamination could have occurred in the later phases, leading to underestimated (not overestimated) effect sizes. Finally, the number of clusters allocated to each study arm was relatively small, although the cluster size was based on the sample size calculation and the majority (28/33) of the previous studies has fewer than 12 clusters.10 To obtain a more stable estimate especially in an earlier phase, future study with more clusters would be ideal. Even if these limitations are considered, our causal interpretation was supported by the results of a series of analyses.
Conclusions
This cluster RCT showed the effectiveness of a 5-year CWI using social marketing to improve population-level PA. The focused promotion strategy was effective in promoting each type of recommended PA. The findings from the current randomized study in combination with the evidence from previous shorter trials suggest that population-level change in PA develops gradually over a period of several years and that several years or more may be necessary to observe a modest effect of CWIs. The effect of such modest improvement in population-level behaviour on population-wide morbidity and mortality needs to be further investigated.
Supplementary Data
Supplementary data are available at IJE online.
Funding
This work was supported by the Ministry of Health, Labour and Welfare of Japan (Comprehensive Research on Prevention of Cardiovascular Diseases and Other Lifestyle Related Diseases: H20-Junkankitou-Ippan-001); the Ministry of Education, Culture, Sports, Science and Technology of Japan (Grants-in-Aid for Scientific Research 25282209 and 16H03249); the Japan Society for the Promotion of Science (Postdoctoral Fellowship for Young Scientists) to M.K.; the Sasakawa Sports Foundation (SSF Overseas Research Fellow) to M.K.; and the Meiji Yasuda Life Foundation of Health and Welfare (2015–2016). The funding bodies did not have a role in study design, intervention, data collection and analysis, interpretation of the data, decision to publish or preparation of the manuscript.
Supplementary Material
Acknowledgements
We deeply appreciate the cooperation of the staff members and all other people involved in this study. M.K. conceptualized and designed the study, supervised all aspects of its implementation, performed the data analysis and drafted the manuscript. As the corresponding author, M.K. has full access to all aspects of the research and writing process, and takes final responsibility for the paper. J.K. and T.A. assisted with conception and design of the study, implementation of the intervention and data collection, and drafting the article. M.T. performed the analysis and interpretation of data, and assisted with drafting the article. S.I. and Y.I. assisted with conception and design of the study, and revised the article critically for important intellectual content. A.B., I.M.L., M.M. and I.K. supervised the analysis and interpretation of the data, and helped to draft and revise the manuscript. All authors have reviewed the manuscript and agreed with its contents. Trial Registration: UMIN-CTR, UMIN000012464.
Conflict of interest: The authors have no conflicts of interest to declare.
References
- 1. Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation 2007;116:1081–93. [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization (WHO). Global Recommendations on Physical Activity for Health. Geneva: WHO, 2010. [PubMed] [Google Scholar]
- 3. US Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. 2008. http://www.health.gov/paguidelines/guidelines/default.aspx (6 November 2017, date last accessed). [Google Scholar]
- 4. Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet 2012;380:247–57. [DOI] [PubMed] [Google Scholar]
- 5. Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet 2012;380:219–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bauman AE, Reis RS, Sallis JF, Wells JC, Loos RJ, Martin BW. Correlates of physical activity: why are some people physically active and others not? Lancet 2012;380:258–71. [DOI] [PubMed] [Google Scholar]
- 7. Heath GW, Parra DC, Sarmiento OL, et al. Evidence-based intervention in physical activity: lessons from around the world. Lancet 2012;380:272–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. CDC. Guide to Community Preventive Services: Campaigns and Informational Approaches to Increase Physical Activity: Community-Wide Campaigns. http://www.thecommunityguide.org/pa/campaigns/community.html (6 November 2017, date last accessed). [Google Scholar]
- 9. Kahn EB, Ramsey LT, Brownson RC, et al. The effectiveness of interventions to increase physical activity: a systematic review. Am J Prev Med 2002;22:73–107. [DOI] [PubMed] [Google Scholar]
- 10. Baker PR, Francis DP, Soares J, Weightman AL, Foster C. Community wide interventions for increasing physical activity. Cochrane Database Syst Rev 2015: CD008366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Grant SP, Mayo-Wilson E, Melendez-Torres GJ, Montgomery P. Reporting quality of social and psychological intervention trials: a systematic review of reporting guidelines and trial publications. PLoS One 2013;8:e65442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kamada M, Kitayuguchi J, Inoue S, et al. A community-wide campaign to promote physical activity in middle-aged and elderly people: a cluster randomized controlled trial. Int J Behav Nutr Phys Act 2013;10:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kamada M, Kitayuguchi J, Abe T, et al. Community-wide promotion of physical activity in middle-aged and older Japanese: a 3-year evaluation of a cluster randomized trial. Int J Behav Nutr Phys Act 2015;12:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation 2007;116:1094–105. [DOI] [PubMed] [Google Scholar]
- 15. Hayden JA, van Tulder MW, Tomlinson G. Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Ann Intern Med 2005;142:776–85. [DOI] [PubMed] [Google Scholar]
- 16. American Geriatrics Society Panel on Exercise and Osteoarthritis. Exercise prescription for older adults with osteoarthritis pain: consensus practice recommendations: a supplement to the AGS Clinical Practice Guidelines on the management of chronic pain in older adults. J Am Geriatr Soc 2001;49:808–23. [DOI] [PubMed] [Google Scholar]
- 17. Roddy E, Zhang W, Doherty M. Aerobic walking or strengthening exercise for osteoarthritis of the knee? A systematic review. Ann Rheum Dis 2005;64:544–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage 2008;16:137–62. [DOI] [PubMed] [Google Scholar]
- 19. Beaudoin CE, Fernandez C, Wall JL, Farley TA. Promoting healthy eating and physical activity short-term effects of a mass media campaign. Am J Prev Med 2007;32:217–23. [DOI] [PubMed] [Google Scholar]
- 20. Luepker RV, Murray DM, Jacobs DR Jr., et al. Community education for cardiovascular disease prevention: risk factor changes in the Minnesota Heart Health Program. Am J Public Health 1994;84:1383–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Reger-Nash B, Bauman A, Booth-Butterfield S, et al. Wheeling walks: evaluation of a media-based community intervention. Fam Community Health 2005;28:64–78. [DOI] [PubMed] [Google Scholar]
- 22. Reger-Nash B, Bauman A, Cooper L, et al. WV Walks: replication with expanded reach. J Phys Act Health 2008;5:19–27. [DOI] [PubMed] [Google Scholar]
- 23. Renger R, Steinfelt V, Lazarus S. Assessing the effectiveness of a community-based media campaign targeting physical inactivity. Fam Community Health 2002;25:18–30. [DOI] [PubMed] [Google Scholar]
- 24. Tudor-Smith C, Nutbeam D, Moore L, Catford J. Effects of the Heartbeat Wales programme over five years on behavioural risks for cardiovascular disease: quasi-experimental comparison of results from Wales and a matched reference area. BMJ 1998;316:818–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wray RJ, Jupka K, Ludwig-Bell C. A community-wide media campaign to promote walking in a Missouri town. Prev Chronic Dis 2005;2:A04. [PMC free article] [PubMed] [Google Scholar]
- 26. Young DR, Haskell WL, Taylor CB, Fortmann SP. Effect of community health education on physical activity knowledge, attitudes, and behavior. The Stanford Five-City Project. Am J Epidemiol 1996;144:264–74. [DOI] [PubMed] [Google Scholar]
- 27. De Cocker KA, De Bourdeaudhuij IM, Brown WJ, Cardon GM. Effects of ‘10 000 steps Ghent’: a whole-community intervention. Am J Prev Med 2007;33:455–63. [DOI] [PubMed] [Google Scholar]
- 28. CDC. Arthritis as a potential barrier to physical activity among adults with heart disease—United States, 2005 and 2007. MMWR Morb Mortal Wkly Rep 2009;58:165–9. [PubMed] [Google Scholar]
- 29. American Academy of Orthopaedic Surgeons. Treatment of Osteoarthritis of the Knee (Non-Arthroplasty). 2008. http://www.aaos.org/research/guidelines/guidelineoaknee.asp (6 November 2017, date last accessed). [Google Scholar]
- 30. Ettinger WH Jr, Burns R, Messier SP, et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. The Fitness Arthritis and Seniors Trial (FAST). JAMA 1997;277:25–31. [PubMed] [Google Scholar]
- 31. Lee NR, Kotler P. Social Marketing: Influencing Behaviors for Good, 4th edn Thousand Oaks: SAGE Publications, 2011. [Google Scholar]
- 32. Valente TW. Network interventions. Science 2012;337:49–53. [DOI] [PubMed] [Google Scholar]
- 33. Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health 1999;89:1322–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Baker PR, Francis DP, Soares J, Weightman AL, Foster C. Community wide interventions for increasing physical activity. Cochrane Database Syst Rev 2011: CD008366. [DOI] [PubMed] [Google Scholar]
- 35. Boutron I, Guittet L, Estellat C, Moher D, Hrobjartsson A, Ravaud P. Reporting methods of blinding in randomized trials assessing nonpharmacological treatments. PLoS Med 2007;4:e61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kamada M, Kitayuguchi J, Shiwaku K, Inoue S, Okada S, Mutoh Y. Differences in association of walking for recreation and for transport with maximum walking speed in an elderly Japanese community population. J Phys Act Health 2011;8:841–7. [DOI] [PubMed] [Google Scholar]
- 37. Thiese MS, Hegmann KT, Garg A, Porucznik C, Behrens T. The predictive relationship of physical activity on the incidence of low back pain in an occupational cohort. J Occup Environ Med 2011;53:364–71. [DOI] [PubMed] [Google Scholar]
- 38. Wijnhoven HA, de Vet HC, Picavet HS. Explaining sex differences in chronic musculoskeletal pain in a general population. Pain 2006;124:158–66. [DOI] [PubMed] [Google Scholar]
- 39. Dixon JS, Bird HA. Reproducibility along a 10 cm vertical visual analogue scale. Ann Rheum Dis 1981;40:87–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Campbell MK, Elbourne DR, Altman DG. CONSORT statement: extension to cluster randomised trials. BMJ 2004;328:702–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Brumback BA, Dailey AB, Brumback LC, Livingston MD, He Z. Adjusting for confounding by cluster using generalized linear mixed models. Stat Probab Lett 2010;80:1650–4. [Google Scholar]
- 42. Barnard J, Meng XL. Applications of multiple imputation in medical studies: from AIDS to NHANES. Stat Methods Med Res 1999;8:17–36. [DOI] [PubMed] [Google Scholar]
- 43. Perry CL, Kelder SH, Murray DM, Klepp KI. Communitywide smoking prevention: long-term outcomes of the Minnesota Heart Health Program and the Class of 1989 Study. Am J Public Health 1992;82:1210–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Record NB, Onion DK, Prior RE, et al. Community-wide cardiovascular disease prevention programs and health outcomes in a rural county, 1970–2010. JAMA 2015;313:147–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Puska P, Vartiainen E, Tuomilehto J, Salomaa V, Nissinen A. Changes in premature deaths in Finland: successful long-term prevention of cardiovascular diseases. Bull World Health Organ 1998;76:419–25. [PMC free article] [PubMed] [Google Scholar]
- 46. Andreasen AR. Marketing social marketing in the social change marketplace. J Public Policy Mark 2002;21:3–13. [Google Scholar]
- 47. Fujihira H, Kubacki K, Ronto R, Pang B, Rundle-Thiele S. Social marketing physical activity interventions among adults 60 years and older: a systematic review. Soc Mar Q 2015;21:214–29. [Google Scholar]
- 48. Ammerman A, Smith TW, Calancie L. Practice-based evidence in public health: improving reach, relevance, and results. Annu Rev Public Health 2014;35:47–63. [DOI] [PubMed] [Google Scholar]
- 49. Edwards PJ, Roberts I, Clarke MJ, et al. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev 2009: MR000008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Wilson DK, Van Horn ML, Siceloff ER, et al. The results of the ‘Positive Action for Today’s Health’ (PATH) trial for increasing walking and physical activity in underserved African-American communities. Ann Behav Med 2015;49:398–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Reeves MM, Marshall AL, Owen N, Winkler EA, Eakin EG. Measuring physical activity change in broad-reach intervention trials. J Phys Act Health 2010;7:194–202. [PubMed] [Google Scholar]
- 52. Conger SA, Guo J, Fulkerson SM, Pedigo L, Chen H, Bassett DR. Objective assessment of strength training exercises using a wrist-worn accelerometer. Med Sci Sports Exerc 2016;48:1847–55. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.