A 24-year-old male who had an 8-year-history of episodic attacks of abdominal pain, three recurrences of epigastric pain with diagnosis of acute exacerbation of chronic pancreatitis in the past year, and 1 day on persistent severe abdominal pain radiating to the back with nausea and vomiting was admitted. There was no history of previous biliary surgery or endoscopic treatment. Physical examination revealed a nondistended diffusely tender abdomen. About 1 year ago, computed tomography and magnetic resonance cholangiopancreatography (MRCP) showed pancreas divisum (PD)-induced chronic pancreatitis and dilated pancreatic duct with stones [Figure 1a and b]. The diagnosis is an acute attack of chronic pancreatitis induced by PD. Pain score of the visual analog scale (VAS) was ten, which was not relieved by conservative treatment.
Figure 1.

The radiographic and reconstructed images. (a and b) About 1 year ago, computed tomography and magnetic resonance cholangiopancreatography showed pancreas divisum-induced chronic pancreatitis and dilated pancreatic duct with stones. (c) After admission, urgent magnetic resonance cholangiopancreatography showed the dilated dorsal duct with multiple stones mostly located in the pancreatic head duct and pancreas divisum
The first emergency endoscopic treatment was performed under general sedation with consciousness. The endoscopy showed an obviously swollen minor papilla and a granular major papilla [Figure 2a]. After deep cannulation of the major pancreatic duct [Figure 2b] and pull hook of sphincterotome, there was a few white protein plug and a lot of pancreatic juice flowing out. Then, the pain of the patient relieved obviously but not completely. The precut of the minor pancreatic duct (mPD) was performed by the dual-knife after several failed attempts of deep cannulation. Then, some white stone fragments and pancreatic juice flowed out [Figure 2c] and the pain got relieved completely, with the VAS score of 1.
Figure 2.

The first emergency endoscopic treatment images. (a) The endoscopic image of the duodenal minor and major papilla. (b) The fluoroscopic image after pressurized cholangiopancreatography from major papilla. (c) The endoscopic image of precut of the minor papilla
Unfortunately, the severe epigastric pain, with the VAS score of 10, recurred again in the next day. Urgent MRCP showed the dilated minor duct with multiple stones, atrophy pancreas, chronic pancreatitis, and PD [Figure 1c].
Therefore, the second emergency endotherapy was performed. Endoscopic ultrasonography (EUS) (GF-UCT 260; Olympus, Tokyo, Japan) showed the obviously dilated mPD with a maximum diameter of 25 mm. mPD was obstructed by multiple stones and the largest one measured 12 mm × 6.8 mm [Figure 3a]. EUS-guided puncture of mPD was performed with a 19-gauge (EchoTip; Cook Endoscopy, Limerick, Ireland) needle through the duodenal bulb [Figure 3b]. Subsequently, a zebra guidewire along the needle was introduced into mPD. A 7F soehendra stent retriever (SSR-7; Cook Medical, Winston-Salem, NC) was used to dilate the puncture passage [Figure 3c]. 40 ml cloudy pancreas juice (the bacteria culture of which was negative) was extracted from the direct nasobiliary duct entering mPD along the guidewire [Figure 3f]. We implanted an 8 cm 7F plastic stent (SPSOF-7-8; Cook Endoscopy, Limerick, Ireland) into mPD which passed over the adherent pancreatic stones [Figure 3d]. Finally, the stent located well and the pancreatic juice flowed out fluently [Figure 3e], resulting in complete pain relief. No immediate or late complication was observed in the 3-month follow-up.
Figure 3.
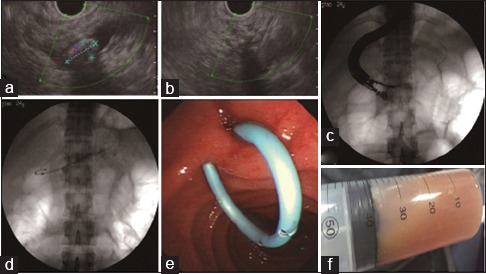
The second emergency endotherapy treatment images. (a) The endoscopic ultrasonography showed the obviously dilated minor pancreatic duct with a maximum diameter of 25 mm, obstructed by multiple stones and the largest one measured 12 mm × 6.8 mm. (b) The endoscopic ultrasonography-guided puncture of minor pancreatic duct was performed with a 19-gauge needle through the duodenal bulb. (c) The puncture passage was dilated by the 7F Soehendra stent retriever. (d) An 8 cm 7F plastic stent was implanted into minor pancreatic duct. (e) The stent located well and the pancreatic juice flowed out fluently. (f) 40 ml cloudy pancreas juice was extracted
PD is the most common congenital anomaly of pancreatic ductal development, occurring in approximately 2.7%–22% of the population.[1] Our case was unique because a large and impacted calculus obstructed the orifice of mPD so that the conventional endoscopic transpapillary drainage, such as sphincterotomy, dilation of stricture, and extraction of stones, could not be achieved. Recently, two novel endoscopic technologies including EUS–guided pancreaticogastrostomy (EPG) and pancreatobulbostomy (EPB) have been reported as alternatives to the conventional endoscopic transpapillary drainage.[2] It is thought that EPB is more preferred than EPG due to the “long” scope position providing with better view, better operation stability, better stent “pushability,”[3] better physiological drainage pathway, and shorter puncture distance. Therefore, we adopted EPB for the first time in PD in which the dilated mPD was inaccessible to transpapillary endoscopic therapy in our case. Moreover, it is proved that EPB is feasible and effective in PD. The follow-up treatments, such as extracorporeal shock wave lithotripsy of mPD calculi with subsequent extraction or place more stents to create a permanent pancreaticobulbar fistula, are scheduled.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understand that his name and initial will not be published and due efforts will be made to conceal his identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Rustagi T, Golioto M. Diagnosis and therapy of pancreas divisum by ERCP: A single center experience. J Dig Dis. 2013;14:93–9. doi: 10.1111/1751-2980.12004. [DOI] [PubMed] [Google Scholar]
- 2.Vignesh S, Jamidar P. EUS-guided pancreatogastrostomy and pancreatobulbostomy in patients with pancreatic-duct obstruction inaccessible to transpapillary endoscopic therapy: Working our way to NOTES. Gastrointest Endosc. 2007;65:242–6. doi: 10.1016/j.gie.2006.09.027. [DOI] [PubMed] [Google Scholar]
- 3.Will U, Fueldner F, Thieme AK, et al. Transgastric pancreatography and EUS-guided drainage of the pancreatic duct. J Hepatobiliary Pancreat Surg. 2007;14:377–82. doi: 10.1007/s00534-006-1139-8. [DOI] [PubMed] [Google Scholar]


