INTRODUCTION
Percutaneous cholecystoscopy is a type of endoscopic gallbladder examination performed after gallbladder drainage by percutaneous transhepatic cholecystostomy (PTC) in patients who are unfit for surgery.[1] The procedure involves percutaneous insertion of endoscopic instruments through the cholecystostomy tract after tract dilation.[2] Recently, peroral cholecystoscopy has also been described after placement of lumen-apposing metal stents (LAMS) during EUS-guided gallbladder drainage (EUS-GBD). The large diameter LAMS acts as a portal for endoscopic access to the gallbladder.[3] This review article aims to provide a summary of various endoscopic methods of examining the gallbladder, with a particular focus on the development of peroral cholecystoscopy and advanced endoscopic gallbladder interventions.
PERCUTANEOUS CHOLECYSTOSTOMY
The gold standard for treating acute cholecystitis is laparoscopic cholecystectomy.[1] However, the procedure may not be suitable for elderly frail patients with multiple comorbidities.[4] As a result, PTC could be performed to provide a means of draining the gallbladder in these patients. With a high technical success rate of 98%, clinical success rate of 90% and adverse event rate of 3.7%, the procedure provides a temporary method for treating acute cholecystitis before patients could be reassessed for suitability of cholecystectomy.[5] In frail patients, the cholecystostomy tube could be a means of permanent drainage of the gallbladder. However, long-term adverse events related to the external drainage catheter such as tract infection and abscess, bile leak, catheter blockade, or dislodgment have been reported in up to 12% of cases. The occurrence of these events frequently mandates repeated unplanned hospital admissions.[6] In addition, high rates of recurrent cholecystitis of up to 33% have been reported after catheter removal in patients who did not undergo cholecystectomy.[3]
As a result, additional management of gallstones including percutaneous cholecystolithotomy (PCCL), extracorporeal shock wave lithotripsy (ESWL), and percutaneous gallbladder stone dissolution with methyl tert-butyl ether (MTBE) were previously described for the treatment of the remaining gallstone following percutaneous gallbladder drainage. PCCL is preferred out of the three as it is suitable in most patients. ESWL is usually applicable in 10%–25% of patients and contact dissolution with MTBE in another 20% of the patients.[7]
PERCUTANEOUS CHOLECYSTOSCOPY AND CHOLECYSTOLITHOTOMY
Previously, peroral endoscopic examination of the gallbladder was impossible as the endoscope is too large to be passed through the cystic duct to access the gallbladder.[2] Hence, percutaneous cholecystoscopy was developed to allow endoscopic examination of the gallbladder pathologies, especially when the correct diagnosis of gallbladder diseases was uncertain by conventional imaging methods. The technique of inserting an endoscope through the fistula tract created after tract dilation from PTC has been practiced since 1981.[8] One study reported on the outcomes of percutaneous cholecystoscopy in 72 patients with gallbladder diseases. Successful diagnosis was made endoscopically in 21 patients with gallbladder carcinoma including 8 patients with early carcinoma.[2] This is in contrast to conventional radiological imaging, which could only detect 70%–82% of the patients with advanced gallbladder carcinoma.[9,10] In addition, successful diagnosis of gallbladder adenoma, cholesterol polyps, and hyperplastic polyps with percutaneous cholecystoscopy was also reported.[2]
Furthermore, percutaneous therapeutic interventions in the gallbladder were also possible. PCCL could be performed under fluoroscopic or endoscopic guidance.[11] The percutaneous fistula tracts created in prior cholecystostomies must be dilated to a diameter large enough to allow for percutaneous insertion of instruments through the tract. Adequate time should be given for maturation of the track before dilation to avoid the risk of intraperitoneal bile leakage and bleeding. PCCL with endoscopic guidance requires dilation to at least 18-Fr to allow for insertion of an ultrathin endoscope. The procedure is usually performed 10–14 days after tract dilation.[12,13] While PCCL under fluoroscopic guidance can be performed in a track that is smaller in diameter and the approach is usually preferred.[12,13,14,15,16,17] In one study, gallstones in 21 patients (63.6%) were removed by endoscopic lithotripsy through percutaneous cholecystoscopy. Lithotripsy was performed with a laser or electrohydraulic shock wave lithotripter 2 weeks after dilation of the fistula tract.[2] Fragmented stones were then removed using a basket catheter. In another study, stone extraction was performed under fluoroscopic guidance after insertion of a small sheath without waiting for tract maturation. This approach reduced the time to perform PCCL to an average of 7.3 days for acute cholecystitis and 9.4 days for gallbladder empyema after PTC.[11] The approach was also associated with reduced pain and bleeding complications. However, the ability to pass larger lithotripsy devices for the fragmentation of larger or harder stones is limited due to a small sheath and the use of basket catheters is required. Despite high technical success rates of percutaneous fluoroscopically guided (94%) and endoscopic-guided PCCL (96%),[18] gallstone recurrences were frequent and reported in 14%–44% of the patients.[13,19,20,21] However, most recurrent gallstones were asymptomatic and only 7.5% of patients eventually required cholecystectomy.[19,20] In other patients, additional surgeries and polypectomies were carried out after gallbladder carcinoma and polypoid lesions were diagnosed.
On the other hand, injury of the fistula tract between the liver and abdominal wall was reported in 3 out of 72 patients (4.2%). A catheter could usually be reinserted into the gallbladder for drainage and no further complications such as bleeding or biliary peritonitis developed in these patients.[2]
PERORAL CHOLECYSTOSCOPY AND THERAPEUTIC GALLBLADDER INTERVENTIONS AFTER EUS-GUIDED GALLBLADDER DRAINAGE WITH LUMEN-APPOSING METAL STENTS
Recently, the development in EUS-GBD has allowed the placement of transmural LAMS through a transgastric or transduodenal approach to drain the gallbladder.[3] With comparable clinical success and adverse event rates to PTC (ETM-GBD vs. PTC = 89.8%–96% vs. 89.8%–94.9% and 32.2% vs. 74.6%, P < 0.001), EUS-GBD is gaining popularity over PTC in gallbladder drainage for high-risk patients that are unsuitable for laparoscopic cholecystectomy.[22,23,24] Placement of LAMS could also allow performance of peroral cholecystoscopy and advanced gallbladder interventions through the stent.
Peroral cholecystoscopy could potentially allow diagnostic and therapeutic procedures be performed by conventional endoscopy [Figures 1–3]. In one retrospective study, routine peroral cholecystoscopy was performed 1–3 months after LAMS placement. A large diameter LAMS was placed to allow easy access of the endoscope into the gallbladder.[3] Spontaneous drainage of gallstones was observed in 56% of patients. Three patients had residual gallstones, and these were removed using irrigation, suction, basket (Olympus Medical, Tokyo, Japan), and a Roth net (US Endoscopy, Mentor, Ohio, USA). While in another three patients with larger stones, holmium laser lithotripsy (VersaPulse PowerSuite; UHS, Minneapolis, Minn, USA) was employed. Complete gallstone clearance was achieved in 88% of patients.
Figure 1.
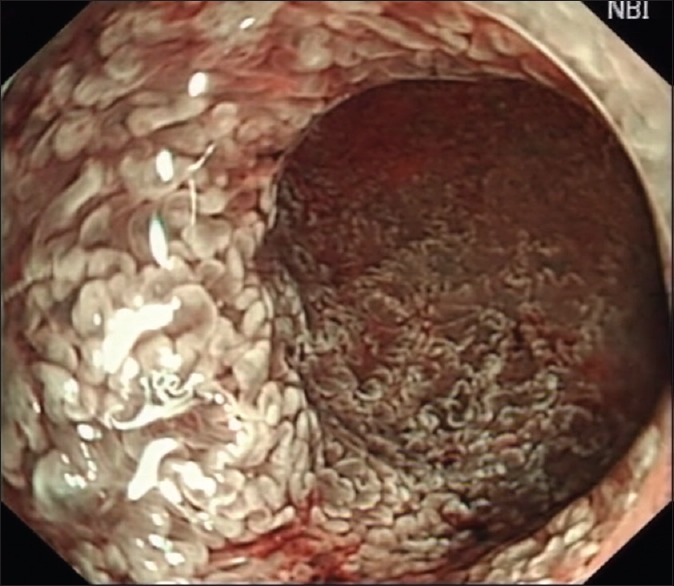
Peroral cholecystoscopic image of papillary mucosa of the gallbladder under narrow band imaging
Figure 3.

Peroral cholecystoscopic image of gallbladder carcinoma
Figure 2.
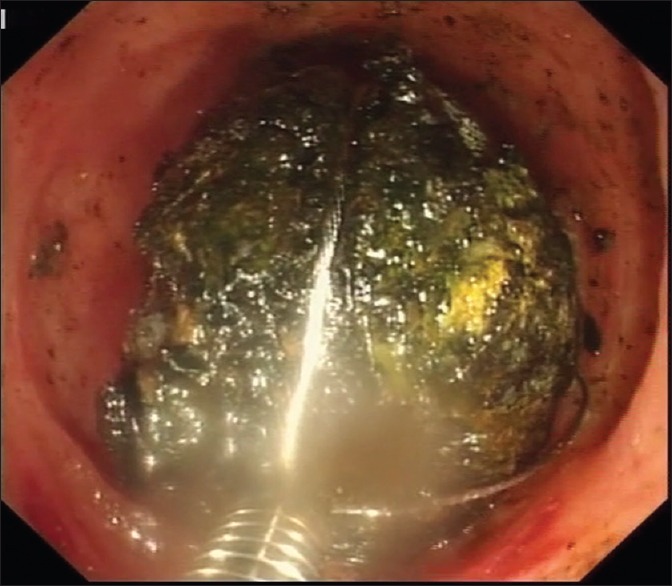
Basket mechanical lithotripsy of a gallstone
Furthermore, a variety of image-enhancing modalities for the evaluation of gallbladder mucosa was also performed. Magnifying narrow band imaging was performed in ten patients and endoscopic images revealed features suggestive of inflammation. These were later confirmed to be compatible with acute on chronic or chronic inflammation on endoscopic biopsy. In one patient, magnifying endoscopy revealed a polypoid growth with irregular mucosal glands and cork-screw microvasculature appearance highly suspicious of malignancy that was not noted on computed tomography performed before EUS-GBD.[25] Confocal laser endomicroscopy demonstrated epithelial structures with thick dark bands or dark clumps.[26] Biopsy was taken and adenocarcinoma of the gallbladder was confirmed. Furthermore, polyps discovered in one patient were also removed by polypectomy with a snare (Olympus Medical, Tokyo, Japan) during the same cholecystoscopy session.
Peroral cholecystoscopy may be advantageous over percutaneous cholecystoscopy in several aspects. Peroral cholecystoscopy avoids the need for additional sessions for fistula tract dilation; the procedure also avoids the need of placing an external tube. Furthermore, regular endoscopic instruments could be used for the procedure, potentially allowing a broader application of diagnostic and therapeutic gallbladder interventions.
CONCLUSION
In conclusion, LAMS in EUS-GBD has opened up exciting possibilities for advanced gallbladder interventions with peroral cholecystoscopy. In the future, studies will need to explore the feasibility and efficacy of the procedure in patients with symptomatic gallbladder pathology in healthy individuals.
REFERENCES
- 1.Teoh AY, Chong CN, Wong J, et al. Routine early laparoscopic cholecystectomy for acute cholecystitis after conclusion of a randomized controlled trial. Br J Surg. 2007;94:1128–32. doi: 10.1002/bjs.5777. [DOI] [PubMed] [Google Scholar]
- 2.Inui K, Nakazawa S, Yoshino J, et al. Percutaneous cholecystoscopy. Endoscopy. 1989;21(Suppl 1):361–4. doi: 10.1055/s-2007-1012991. [DOI] [PubMed] [Google Scholar]
- 3.Chan SM, Teoh AY, Yip HC, et al. Feasibility of per-oral cholecystoscopy and advanced gallbladder interventions after EUS-guided gallbladder stenting (with video) Gastrointest Endosc. 2017;85:1225–32. doi: 10.1016/j.gie.2016.10.014. [DOI] [PubMed] [Google Scholar]
- 4.Yeung B, Teoh AY. Endoscopic management of gallbladder stones: Can we eliminate cholecystectomy? Curr Gastroenterol Rep. 2016;18:42. doi: 10.1007/s11894-016-0518-9. [DOI] [PubMed] [Google Scholar]
- 5.Itoi T, Coelho-Prabhu N, Baron TH. Endoscopic gallbladder drainage for management of acute cholecystitis. Gastrointest Endosc. 2010;71:1038–45. doi: 10.1016/j.gie.2010.01.026. [DOI] [PubMed] [Google Scholar]
- 6.McGahan JP, Lindfors KK. Percutaneous cholecystostomy: An alternative to surgical cholecystostomy for acute cholecystitis? Radiology. 1989;173:481–5. doi: 10.1148/radiology.173.2.2678261. [DOI] [PubMed] [Google Scholar]
- 7.Cheslyn-Curtis S, Russell RC. New trends in gallstone management. Br J Surg. 1991;78:143–9. doi: 10.1002/bjs.1800780206. [DOI] [PubMed] [Google Scholar]
- 8.Inui K, Nakazawa S, Naito Y, et al. Nonsurgical treatment of cholecystolithiasis with percutaneous transhepatic cholecystoscopy. Am J Gastroenterol. 1988;83:1124–7. [PubMed] [Google Scholar]
- 9.Itai Y, Araki T, Yoshikawa K, et al. Computed tomography of gallbladder carcinoma. Radiology. 1980;137:713–8. doi: 10.1148/radiology.137.3.7444054. [DOI] [PubMed] [Google Scholar]
- 10.Yeh HC. Ultrasonography and computed tomography of carcinoma of the gallbladder. Radiology. 1979;133:167–73. doi: 10.1148/133.1.167. [DOI] [PubMed] [Google Scholar]
- 11.Kim YH, Kim YJ, Shin TB. Fluoroscopy-guided percutaneous gallstone removal using a 12-Fr sheath in high-risk surgical patients with acute cholecystitis. Korean J Radiol. 2011;12:210–5. doi: 10.3348/kjr.2011.12.2.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wong SK, Yu SC, Lam YH, et al. Percutaneous cholecystostomy and endoscopic cholecystolithotripsy in the management of acute cholecystitis. Surg Endosc. 1999;13:48–52. doi: 10.1007/s004649900896. [DOI] [PubMed] [Google Scholar]
- 13.Kim HJ, Lee SK, Kim MH, et al. Safety and usefulness of percutaneous transhepatic cholecystoscopy examination in high-risk surgical patients with acute cholecystitis. Gastrointest Endosc. 2000;52:645–9. doi: 10.1067/mge.2000.107286. [DOI] [PubMed] [Google Scholar]
- 14.Picus D, Hicks ME, Darcy MD, et al. Percutaneous cholecystolithotomy: Analysis of results and complications in 58 consecutive patients. Radiology. 1992;183:779–84. doi: 10.1148/radiology.183.3.1533946. [DOI] [PubMed] [Google Scholar]
- 15.Cope C, Burke DR, Meranze SG. Percutaneous extraction of gallstones in 20 patients. Radiology. 1990;176:19–24. doi: 10.1148/radiology.176.1.2353089. [DOI] [PubMed] [Google Scholar]
- 16.Picus D, Marx MV, Hicks ME, et al. Percutaneous cholecystolithotomy: Preliminary experience and technical considerations. Radiology. 1989;173:487–91. doi: 10.1148/radiology.173.2.2798880. [DOI] [PubMed] [Google Scholar]
- 17.Bonnel DH, Liguory CE, Cornud FE, et al. Common bile duct and intrahepatic stones: Results of transhepatic electrohydraulic lithotripsy in 50 patients. Radiology. 1991;180:345–8. doi: 10.1148/radiology.180.2.2068295. [DOI] [PubMed] [Google Scholar]
- 18.Ohashi S. Percutaneous transhepatic cholecystoscopic lithotomy in the management of acute cholecystitis caused by gallbladder stones. Diagn Ther Endosc. 1998;5:19–29. doi: 10.1155/DTE.5.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gibney RG, Chow K, So CB, et al. Gallstone recurrence after cholecystolithotomy. AJR Am J Roentgenol. 1989;153:287–9. doi: 10.2214/ajr.153.2.287. [DOI] [PubMed] [Google Scholar]
- 20.Zou YP, Du JD, Li WM, et al. Gallstone recurrence after successful percutaneous cholecystolithotomy: A 10-year follow-up of 439 cases. Hepatobiliary Pancreat Dis Int. 2007;6:199–203. [PubMed] [Google Scholar]
- 21.Donald JJ, Cheslyn-Curtis S, Gillams AR, et al. Percutaneous cholecystolithotomy: Is gall stone recurrence inevitable? Gut. 1994;35:692–5. doi: 10.1136/gut.35.5.692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Irani S, Ngamruengphong S, Teoh A, et al. Similar efficacies of endoscopic ultrasound gallbladder drainage with a lumen-apposing metal stent versus percutaneous transhepatic gallbladder drainage for acute Cholecystitis. Clin Gastroenterol Hepatol. 2017;15:738–45. doi: 10.1016/j.cgh.2016.12.021. [DOI] [PubMed] [Google Scholar]
- 23.Tyberg A, Saumoy M, Sequeiros EV, et al. EUS-guided versus percutaneous gallbladder drainage: Isn’t it time to convert? J Clin Gastroenterol. 2018;52:79–84. doi: 10.1097/MCG.0000000000000786. [DOI] [PubMed] [Google Scholar]
- 24.Teoh AY, Serna C, Penas I, et al. Endoscopic ultrasound-guided gallbladder drainage reduces adverse events compared with percutaneous cholecystostomy in patients who are unfit for cholecystectomy. Endoscopy. 2017;49:130–8. doi: 10.1055/s-0042-119036. [DOI] [PubMed] [Google Scholar]
- 25.Teoh AY, Chan AW, Chiu PW, et al. In vivo appearances of gallbladder carcinoma under magnifying endoscopy and probe-based confocal laser endomicroscopy after endosonographic gallbladder drainage. Endoscopy. 2014;46(Suppl 1):E13–4. doi: 10.1055/s-0033-1359139. [DOI] [PubMed] [Google Scholar]
- 26.Nakai Y, Isayama H, Shinoura S, et al. Confocal laser endomicroscopy in gastrointestinal and pancreatobiliary diseases. Dig Endosc. 2014;26(Suppl 1):86–94. doi: 10.1111/den.12152. [DOI] [PubMed] [Google Scholar]


