INTRODUCTION
In the rapidly expanding field of therapeutic EUS, procedures that were previously considered “novel,” are now becoming part of the repertoire of an interventional endoscopist. With the development of new devices, the field has rapidly expanded allowing for the creation of stable and durable transluminal fistulas for internalized drainage. One established example is EUS-guided drainage of the gallbladder. Among others, it has become one of the many new interventional techniques which have been developed, initially as a strictly palliative measure. However as our experience with this technique has grown, we describe potential long-term outcomes for these patients.
OUTCOMES OF PATIENTS WITH CHOLECYSTITIS
The gold standard in management for cholecystitis is a cholecystectomy (CCY), particularly laparoscopic cholecystectomy which is associated with lower postoperative morbidity and lower length of stay.[1] When patients are considered too high risk to safely undergo a CCY, they are generally managed with percutaneous gallbladder drainage (PTGBD) with a goal to provide a bridge until they clinically improve to undergo cholecystectomy.[2] Unfortunately, many patients are unable to improve from their underlying clinical comorbidities. These patients rely on PTGBD as definitive therapy for cholecystitis.[3] Percutaneous drainage can be associated with complications and morbidity related to the cholecystostomy tube, reported as high as 12% in some series.[4,5] These complications include but are not limited to pneumothorax, bile peritonitis, bleeding, and fistulae after tube removal. In addition, patients complain of morbidity associated with having an external drain.[4] Therefore, endoscopically performed gallbladder drainage procedures are exciting alternatives, which have been revealed as safe, efficacious, and minimally invasive.
ENDOSCOPIC GALLBLADDER DRAINAGE
Methods for endoscopic gallbladder drainage (EGBD) have evolved over the past few decades. Initially, endoscopic transpapillary drainage was performed with stent placement using a transcystic approach.[6] Improvement in EUS led to transmural gallbladder drainage with stent placement directly into the gallbladder from the gastrointestinal (GI) lumen, with similar technical success rates, and fewer adverse events than PTGBD.[7,8] With the development of lumen apposing metal stent (LAMS), EUS-guided gallbladder drainage (EUS-GBD) has emerged as the endoscopically minimally invasive therapeutic option of choice.[9] In addition to not requiring an external drain, transmural drainage offers the additional benefits of puncturing through the GI tract instead of the liver, which is less vascular. The design of the LAMS also gives the ability to be performed in the presence of ascites. Multiple studies have been done looking at safety and efficacy of EUS-GBD. These are associated with decreased length of stay, fewer adverse events, and fewer repeated interventions.[9,10,11]
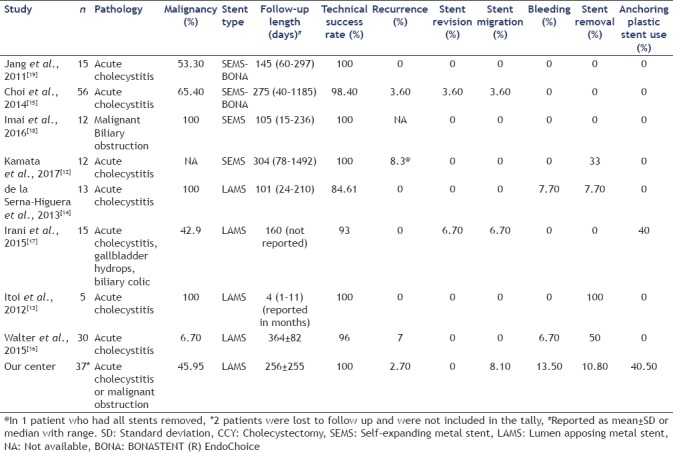
EUS-GBD began as a procedure for patients who would never be considered a surgical candidate: patients with the metastatic malignant disease, or significant age and other comorbidities, and as previously stated, would conventionally receive definitive therapy with a percutaneous drain. However, multiple centers have revealed EUS-GBD as a successful alternative.[12,13,14,15,16,17,18] In our center, we have performed EUS-GBD for similar indications. About half of our patients who underwent EUS-GBD had an underlying malignancy (45.95%) and therefore were not considered operative candidates [Table 1]. The other half of patients had significant age and medical comorbidities (44.05%). Mean age was 74.4 years (±16.51), with 56.8% of males and 43.2% of females. In the majority of patients, the 15 mm diameter LAMS was used (78.4%), compared to the 10 mm diameter LAMS (21.6%). In addition, drainage point was more frequently from the duodenum (62.2%) than the stomach (37.8%). Following the outcomes of these patients, demonstrates the end result of EUS-GBD; either with EUS-GBD used as definite therapy or a patient's medical comorbidities improve so they can undergo the gold standard cholecystectomy.
Table 1.
Review of publications for long-term outcomes of EUS-guided gallbladder drainage
EUS-GUIDED GALLBLADDER DRAINAGE AS DEFINITIVE THERAPY
EUS-GBD can provide permanent drainage. Increasingly published long-term data reveals that as long as the stent remains patent, it can be left in place as there is no significant morbidity to the patient. Multiple studies have revealed that EUS-GBD can provide definitive therapy, whether the stent is left in place, or removed endoscopically[11,12] [Table 1]. The longest clinical follow-up was published by Walter et al. who reported an average LAMS dwell time of 364 days without stent-related complications.[16] The longest time published reported gallbladder drainage stent dwell time is 3 years, though was performed with a SEMS and not a LAMS.[15,19] We have confirmed this with our own clinical experience. In our case series, 10.8% of patients had the LAMS removed. 81.1% of patients maintained the LAMS, and in 8.1% of patients, the LAMS dislodged on its own. Due to their underlying medical disease, on long-term follow-up – an average of 8.5 months, a majority of patients died (74%) with the LAMS in place. Therefore, EUS-GBD can successfully be offered as a method for definitive therapy in cholecystitis. In these cases, where EUS-GBD is planned to be employed as definitive therapy, certain questions still exist. For example, it is unclear whether an additional plastic double pigtail stent is required to act as a buffer between the LAMS and the lumen wall to prevent bleeding as well as to prevent stent occlusion from food. Additional studies will need to evaluate the likelihood of LAMS obstruction, with or without an anchoring plastic stent, resulting in a recurrence of cholecystitis.
EUS-GUIDED GALLBLADDER DRAINAGE AS A BRIDGE TO SURGERY
As previously stated, when patients’ comorbidities improve after EGBD or PTGB, the ideal management for this patient is to undergo surgery. CCY is known to be safe and efficacious after PTGB.[20] Till date, there are a few studies revealing the feasibility of surgical CCY after EUS-GBD. Jang et al. described successful CCY (with no increase rate of open vs. laparoscopic CCY) after EGBD with a plastic nasobiliary drainage catheter.[21] In our clinical experience, patients have also had successful CCY after EUS-GBD with a LAMS. Till date, we have had four patients in our institution who had a successful CCY. Three of the four patients had a cholecystgastrostomy stent and the fourth patient had a cholecystoduodenostomy stent. Only one patient had a postsurgical complication, developing atrial fibrillation with rapid ventricular response. The other three patients had an uncomplicated postoperative course.
EUS-GUIDED GALLBLADDER LONG-TERM OUTCOMES
The main concern with long-term EGBD outcomes remain bleeding, stent migration, and recurrent cholecystitis. The literature reveals low rates of bleeding (reported up to 13% of patients) and stent migration (reported up to 8% of patients) [Table 1]. Some centers use anchoring plastic stents deployed through the LAMS in hopes to prevent stent migration and bleeding. In our experience, we did not find a significant association between deployment of plastic stents and decreased bleeding propensity. Recurrent cholecystitis or gallbladder obstruction remains a rare complication that we have only observed in one patient, although has been reported in the literature of a rate up to 8% [Table 1]. In our case series, 16.2% of patients required a repeat endoscopy, either to remove the stent (4 patients or 10.8%), for management of significant bleeding (1 patient or 5.4%) or management of persistent cholecystitis (1 patient or 2.7%). No patient in our cohort required a repeat admission during the follow-up period for a complication of the LAMS stent or recurrent cholecystitis.
Given the published data demonstrating successful long-term outcomes of EUS-GBD, we propose an algorithm for the management of cholecystitis [Figure 1]. In this algorithm, all patients who are good operative candidates should undergo the gold standard CCY as first-line therapy for cholecystitis. However, patients who are not considered good operative candidates can either undergo EUS-GBD or PTGBD (if an interventional endoscopist is not available). Once a patient's comorbidities improve, a surgeon should reassess the patient's candidacy for a CCY. If a patient is still not a candidate, all PTGBD should be converted to EUS-GBD for long-term gallbladder decompression.
Figure 1.
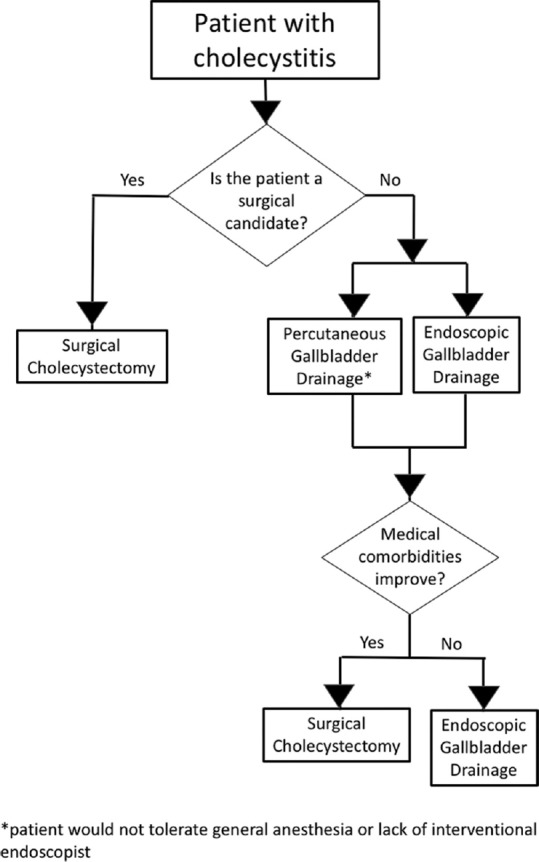
Proposed algorithm for management of cholecystitis. If patients are a surgical candidate, they should undergo a cholecystectomy. If patients are not likely to be surgical candidates, they should consider definitive therapy with EUS-guided gallbladder drainage
EUS-GUIDED GALLBLADDER FUTURE DIRECTIONS
It is becoming more accepted that EGBD should be the standard of care for patients with malignant conditions whom will never become surgical candidates. In these patients, where the maximizing quality of life is paramount, EGBD provides the best method for gallbladder drainage while eliminating the need for an external drain.[18] It remains to be seen whether longer-term studies corroborate similar surgical success rates after EUS-GBD with LAMS. Additional questions to be answered are whether transluminal drainage site (gastric vs. duodenal) can lead to a higher risk of postoperative complications. We assume that if a patient is considered a potential future surgical candidate, transgastric drainage will have fewer operative complications after gallbladder removal, as the retroperitoneal position of the duodenum can make surgical closure more challenging. It is also unclear whether a repeat endoscopy for LAMS removal is necessary before CCY. We hypothesize that prior removal of the LAMS can facilitate a shorter operative time and potentially lower post-operative complications. However, future studies will need to confirm these hypotheses.
CONCLUSIONS
EUS-guided drainage of the gallbladder is an established alternative method for management of cholecystitis. EUS-GBD can be offered as a permanent solution or as a temporizing measure before surgery. We propose an algorithm for management of patients who present with cholecystitis [Figure 1]. Patients with acute cholecystitis who ultimately may become surgical candidates should be offered EGBD as a therapeutic option for gallbladder decompression, and EGBD drainage should not preclude patients from undergoing CCY as part of the standard of care.
REFERENCES
- 1.Livingston EH, Rege RV. A nationwide study of conversion from laparoscopic to open cholecystectomy. Am J Surg. 2004;188:205–11. doi: 10.1016/j.amjsurg.2004.06.013. [DOI] [PubMed] [Google Scholar]
- 2.Gurusamy KS, Belgaumkar AP, Haswell A, et al. Interventions for necrotising pancreatitis. Cochrane Database Syst Rev. 2016;4:CD011383. doi: 10.1002/14651858.CD011383.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chung YH, Choi ER, Kim KM, et al. Can percutaneous cholecystostomy be a definitive management for acute acalculous cholecystitis? J Clin Gastroenterol. 2012;46:216–9. doi: 10.1097/MCG.0b013e3182274375. [DOI] [PubMed] [Google Scholar]
- 4.McGahan JP, Lindfors KK. Percutaneous cholecystostomy: An alternative to surgical cholecystostomy for acute cholecystitis? Radiology. 1989;173:481–5. doi: 10.1148/radiology.173.2.2678261. [DOI] [PubMed] [Google Scholar]
- 5.McKay A, Abulfaraj M, Lipschitz J. Short- and long-term outcomes following percutaneous cholecystostomy for acute cholecystitis in high-risk patients. Surg Endosc. 2012;26:1343–51. doi: 10.1007/s00464-011-2035-0. [DOI] [PubMed] [Google Scholar]
- 6.Itoi T, Coelho-Prabhu N, Baron TH. Endoscopic gallbladder drainage for management of acute cholecystitis. Gastrointest Endosc. 2010;71:1038–45. doi: 10.1016/j.gie.2010.01.026. [DOI] [PubMed] [Google Scholar]
- 7.Kahaleh M, Brijbassie A, Sethi A, et al. Multicenter trial evaluating the use of covered self-expanding metal stents in benign biliary strictures: Time to revisit our therapeutic options? J Clin Gastroenterol. 2013;47:695–9. doi: 10.1097/MCG.0b013e31827fd311. [DOI] [PubMed] [Google Scholar]
- 8.Khan MA, Atiq O, Kubiliun N, et al. Efficacy and safety of endoscopic gallbladder drainage in acute cholecystitis: Is it better than percutaneous gallbladder drainage? Gastrointest Endosc. 2017;85:76–87e3. doi: 10.1016/j.gie.2016.06.032. [DOI] [PubMed] [Google Scholar]
- 9.Irani S, Ngamruengphong S, Teoh A, et al. Similar efficacies of endoscopic ultrasound gallbladder drainage with a lumen-apposing metal stent versus percutaneous transhepatic gallbladder drainage for acute Cholecystitis. Clin Gastroenterol Hepatol. 2017;15:738–45. doi: 10.1016/j.cgh.2016.12.021. [DOI] [PubMed] [Google Scholar]
- 10.Tyberg A, Sharaiha RZ, Kedia P, et al. EUS-guided pancreatic drainage for pancreatic strictures after failed ERCP: A multicenter international collaborative study. Gastrointest Endosc. 2017;85:164–9. doi: 10.1016/j.gie.2016.07.030. [DOI] [PubMed] [Google Scholar]
- 11.Teoh AY, Serna C, Penas I, et al. Endoscopic ultrasound-guided gallbladder drainage reduces adverse events compared with percutaneous cholecystostomy in patients who are unfit for cholecystectomy. Endoscopy. 2017;49:130–8. doi: 10.1055/s-0042-119036. [DOI] [PubMed] [Google Scholar]
- 12.Kamata K, Takenaka M, Kitano M, et al. Endoscopic ultrasound-guided gallbladder drainage for acute cholecystitis: Long-term outcomes after removal of a self-expandable metal stent. World J Gastroenterol. 2017;23:661–7. doi: 10.3748/wjg.v23.i4.661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Itoi T, Binmoeller KF, Shah J, et al. Clinical evaluation of a novel lumen-apposing metal stent for endosonography-guided pancreatic pseudocyst and gallbladder drainage (with videos) Gastrointest Endosc. 2012;75:870–6. doi: 10.1016/j.gie.2011.10.020. [DOI] [PubMed] [Google Scholar]
- 14.de la Serna-Higuera C, Pérez-Miranda M, Gil-Simón P, et al. EUS-guided transenteric gallbladder drainage with a new fistula-forming, lumen-apposing metal stent. Gastrointest Endosc. 2013;77:303–8. doi: 10.1016/j.gie.2012.09.021. [DOI] [PubMed] [Google Scholar]
- 15.Choi JH, Lee SS, Choi JH, et al. Long-term outcomes after endoscopic ultrasonography-guided gallbladder drainage for acute cholecystitis. Endoscopy. 2014;46:656–61. doi: 10.1055/s-0034-1365720. [DOI] [PubMed] [Google Scholar]
- 16.Walter D, Teoh AY, Itoi T, et al. EUS-guided gall bladder drainage with a lumen-apposing metal stent: A prospective long-term evaluation. Gut. 2016;65:6–8. doi: 10.1136/gutjnl-2015-309925. [DOI] [PubMed] [Google Scholar]
- 17.Irani S, Baron TH, Grimm IS, et al. EUS-guided gallbladder drainage with a lumen-apposing metal stent (with video) Gastrointest Endosc. 2015;82:1110–5. doi: 10.1016/j.gie.2015.05.045. [DOI] [PubMed] [Google Scholar]
- 18.Imai H, Kitano M, Omoto S, et al. EUS-guided gallbladder drainage for rescue treatment of malignant distal biliary obstruction after unsuccessful ERCP. Gastrointest Endosc. 2016;84:147–51. doi: 10.1016/j.gie.2015.12.024. [DOI] [PubMed] [Google Scholar]
- 19.Jang JW, Lee SS, Park DH, et al. Feasibility and safety of EUS-guided transgastric/transduodenal gallbladder drainage with single-step placement of a modified covered self-expandable metal stent in patients unsuitable for cholecystectomy. Gastrointest Endosc. 2011;74:176–81. doi: 10.1016/j.gie.2011.03.1120. [DOI] [PubMed] [Google Scholar]
- 20.Patterson EJ, McLoughlin RF, Mathieson JR, et al. An alternative approach to acute cholecystitis. Percutaneous cholecystostomy and interval laparoscopic cholecystectomy. Surg Endosc. 1996;10:1185–8. doi: 10.1007/s004649900275. [DOI] [PubMed] [Google Scholar]
- 21.Jang JW, Lee SS, Song TJ, et al. Endoscopic ultrasound-guided transmural and percutaneous transhepatic gallbladder drainage are comparable for acute cholecystitis. Gastroenterology. 2012;142:805–11. doi: 10.1053/j.gastro.2011.12.051. [DOI] [PubMed] [Google Scholar]


