Abstract
Context and Aims:
Impairment in cognition is well-known in patients with major depressive disorder. This study examined the effect of yoga therapy with or without antidepressants and antidepressants alone on certain neuropsychological functions in patients with depression. Correlation between changes in neuropsychological test performance and serum brain-derived neurotrophic factor (BDNF) levels was also explored.
Materials and Methods:
Antidepressant-naïve/antidepressant-free outpatients with depression received antidepressant medication alone (n = 23) or yoga therapy with (n = 26) or without (n = 16) antidepressants. Depression was assessed using the Hamilton Depression Rating Scale. Neuropsychological tests included digit-span forward and backward, Rey Auditory Verbal Learning Test, and Trail Making Tests (TMT-A and B). These tests were administered before and 3 months after the treatment in patients, and once in healthy comparison subjects (n = 19).
Statistical Analysis:
Baseline differences were analyzed using independent sample t-test, Chi-square, and one-way ANOVA. Paired t-test was used to analyze the change from baseline to follow-up. Pearson's correlation was used to explore the association of change between 2 variables.
Results:
Patients had impaired performance on most neuropsychological tests. After 3 months, there was significant improvement – patients’ performance was comparable to that of healthy controls on majority of the tests. Significant inverse correlation was observed between increase in BDNF levels and improvement in TMT “A” duration in Yoga-alone group (r = −0.647; P = 0.009).
Conclusions:
To conclude that, Yoga therapy, alone or in combination with medications, is associated with improved neuropsychological functions and neuroplastic effects in patients with depression.
Keywords: Antidepressants, brain-derived neurotrophic factor, cognition, depression, Rey Auditory Verbal Learning Test, yoga
INTRODUCTION
Depression is a highly prevalent mental disorder characterized by sadness of mood, anhedonia, negative cognitions and retardation of motor behavior, and cognitive process impairment in neurocognition is well-known in patients with major depressive disorder.[1] Patients with depression experience neuropsychological impairment in several domains including verbal learning, memory, attention, motor speed, and executive functions.[2,3,4,5,6] Studies show inconsistent results regarding the influence of antidepressant medications on neurocognitive functioning of patients with depression. While some studies report improved cognitive functioning,[7] other studies report no significant improvement after antidepressant medications.[8,9]
Brain-derived neurotrophic factor (BDNF), a key modulator of neuroplastic changes, has been implicated in the pathophysiology of depression[10] through the stress pathway.[11,12] Decreased serum BDNF levels were observed in medication-free patients with depression in comparison to healthy controls.[13,14] Serum BDNF level has been shown to increase with antidepressant treatment.[15,16,17] In addition, decreased serum BDNF levels were significantly correlated with reduced hippocampal volume in moderately depressed patients.[18] Further, decreased serum BDNF levels were associated with better performance in attention and psychomotor speed tested using Trail Making Test (TMT) in patients with major depression.[19] In this context, abnormal neuroplasticity has been proposed as an important pathophysiological mechanism underlying depression.[20] There is a need to look at complementary and alternative approaches as a treatment option in patients with depression.
Yoga is an effective treatment for depression.[21] It has also been shown to improve cognitive functions. Sahaj Yoga practice (one type of meditation) improved the cognitive domains of verbal working memory, attention span, and visual-motor speed in addition to improvement in executive functions in patients with depression.[22] In a recent study, regular practice of yoga has been shown to enhance serum BDNF levels and reduction in depression scores in patients with depression.[23] Further, the practice of yoga is reported to increase hippocampal volume in elderly participants.[24]
Little is known about the changes in cognitive impairment in depression with practice of generic yoga. We compared the effect of yoga therapy with or without antidepressants, and antidepressants alone, on certain neuropsychological functions in patients with depression. Further, we examined the association between neuropsychological functions, serum BDNF levels, and severity of depression.
MATERIALS AND METHODS
Subjects
Data for this study were obtained from participants, who took part in a three-group, single-blind comparative trial; the detailed methodology of the trial is presented elsewhere.[23] Briefly, patients with depression with a score of 11 or more on Hamilton Depression Rating Scale (HDRS) and score of 2 or less on the suicide item of HDRS[25] were recruited from the outpatient department of psychiatry in an academic psychiatric center. They were aged between 18 and 55 years. Diagnosis of major depressive disorder was made according to the DSM-IV criteria. The diagnosis was confirmed by a psychiatrist using the Mini International Neuropsychiatric Interview.[26] Patients were either antidepressant-naïve or not on antidepressants for at least 1 month. Patients with mental retardation, substance abuse disorders (except nicotine and caffeine), organic disorders such as dementia, epilepsy, or cerebrovascular accidents, psychosis and bipolar disorder were excluded from the study. None of them had received yoga as treatment before. The patients had no indications for electroconvulsive therapy (e.g., catatonia, severe, treatment-resistant depression). Written informed consent to take part in the study was obtained from all study participants. The study was approved by the Institutional Ethics Committee.
One hundred and thirty-seven patients with depression were recruited in the main study.[23] Of these, 65 patients’ neuropsychological assessment data were available for baseline as well as 12 weeks follow-up. There were three naturalistic groups of patients: Medication-alone (n = 23), yoga therapy-alone (n = 16), and medications + yoga therapy (n = 26). The duration of the follow-up was 12 weeks. Out of the 32 age and education-matched healthy subjects, neuropsychological performance data was available for 19. None of the healthy controls had any psychiatric/medical disorder or alcohol/drug use disorders.
Yoga therapy procedure
A yoga module developed and validated for depression was used in this study.[27] The participants of both the yoga groups attended Yoga sessions daily for 2 weeks at Yoga therapy center of NIMHANS, where a yoga professional taught them the yoga practices. Each session of training/practice lasted for about 1 h. They were then asked to come to perform yoga practices in the yoga therapy center twice a week for the next 2 weeks. The participants were instructed to continue the yoga practices at home thereafter, except for one booster session at every month held at the yoga therapy center. Home practices were monitored by a family member for the next 2 months. They were also instructed to maintain a log of each day's yoga at home filled by the family members. The yoga professional was formally trained with a graduate medical degree (5 years) in yoga and naturopathy with 2 years’ postgraduate degree in yoga. Efforts were made to maintain 100% attendance. The patients receiving yoga were encouraged to report any untoward event that they had experienced during the course of the study.
Antidepressant medication
During the 3 months of study, the patients on antidepressant medications received a consultation with their respective psychiatrists. Antidepressant type and dose were not controlled. However, the medications, their dosage, and changes, if any, were noted. The treatment remained unchanged in nearly all patients. Antidepressants administered were escitalopram (10–15 mg/day; n = 63), fluoxetine (20–40 mg/day; n = 30), duloxetine (60 mg/day; n = 1), sertraline (50– 100 mg/day; n = 3); amitriptyline (25– 100 mg/day; n = 13), mirtazapine (7.5–15 mg/day; n = 4). In addition, some patients were given benzodiazepines (lorazepam up to 3 mg/day or alprazolam 1.5 mg/day). The researcher had a telephonic conversation with all the participants to inquire regarding their medication/yoga practice compliance at home.
Assessments
A trained rater blind to the group status of the patients (resident in psychiatry) assessed the severity of depression using HDRS. Neuropsychological functions were assessed by another researcher (Naveen GH). Patients and healthy controls had minimum 5 years of schooling and could read English letters and numerals. The following neuropsychological tests were administered before starting the treatment and at the end of 3 months: (1) Rey auditory verbal learning test,[28,29] (2) digit span test,[30] and (3) TMT.[31,32,33]
Statistical analysis
In this paper, we present an analysis of data from patients in whom neuropsychological test data are available at baselines as well as at 3-month follow-up (n = 65). Baseline differences between patients and controls with respect to sociodemographic data, serum BDNF levels, and neuropsychological test scores were analyzed using independent sample t-test and Chi-square test. Baseline comparisons across three groups of patients with respect to sociodemographic details, illness characteristics, serum BDNF levels, and neuropsychological changes were assessed using Chi-square test and one-way ANOVA. Paired t-test was used to analyze the change, from baseline to follow-up, in HDRS, BDNF, as well as in neuropsychological test scores. Pearson's correlation was used to explore the association of change in serum BDNF levels with change in neuropsychological test scores.
RESULTS
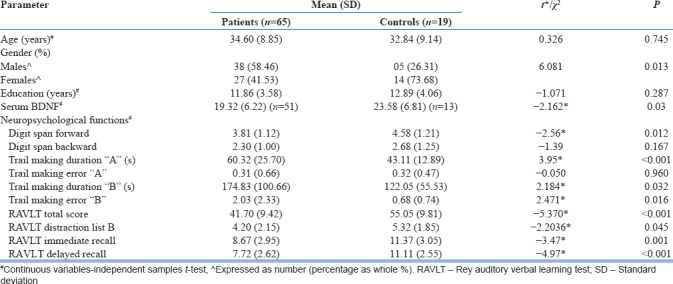
Table 1 presents baseline comparison of sociodemographic details and neuropsychological assessment between patients and controls. There were no significant differences between patients and controls with respect to sociodemographic details, except that females were significantly over-represented in the control group. Patients’ scores on neuropsychological tests were significantly poorer than that of healthy controls on most neuropsychological tests except digit span backward and trail making error “A.” Serum BDNF levels were significantly lower in patients.
Table 1.
Sociodemographic details, serum brain-derived neurotrophic factor levels, and performance of patients and controls on cognitive function tests
As shown in Table 2, patients in the three treatment groups were not significantly different with respect to baseline sociodemographic details and illness characteristics. However, there was a significant difference across 3 group with respect to education (P = 0.03); patients in the yoga alone group had higher education levels than those in the other two.
Table 2.
Comparison of the three treatment groups across demographic, illness, serum brain-derived neurotrophic factor characteristics
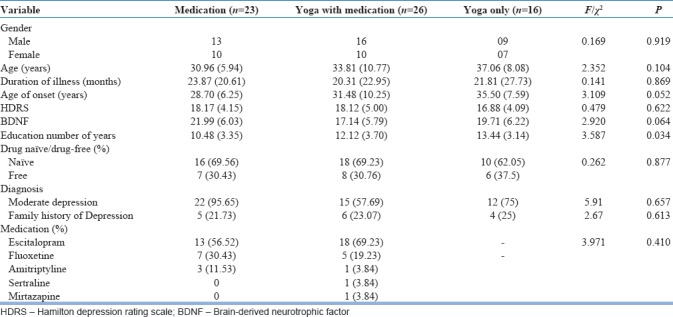
Baseline comparison between three treatment groups were not significantly different with respect to neurocognitive test characteristics, except on digit span backward (P = 0.03), where the medication-alone group performed poorly.
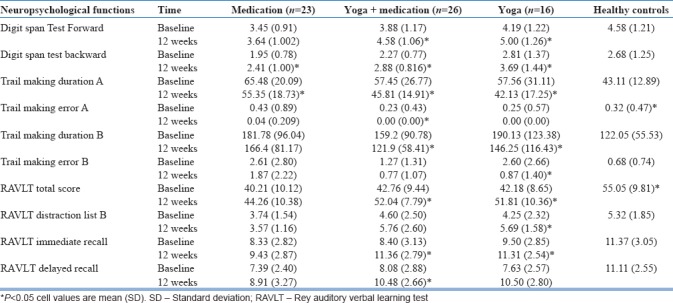
As shown in Table 3, there was a significant improvement in performance on most neuropsychological tests at follow-up. However, significant changes were observed more in the yoga-alone and yoga with antidepressant medication group in comparison with medication group alone. Further, the performance of controls and patients at follow-up on neuropsychological tests did not show any significant differences between patients and controls with respect to performance in most of the neuropsychological tests. Patients scored similarly to healthy controls on most of the neuropsychological tests except trail making error “A” (P = 0.01), and Rey Auditory Verbal Learning Test total score (P = 0.02).
Table 3.
Baseline and 12 weeks comparison of neuropsychological functions in patients with depression and comparison of these changes in all patients at follow-up and controls
As reported in the previous publication,[23] there was a significant increase in serum BDNF level from baseline to 3-month follow-up in patients. Mean (standard deviation) serum BDNF level of patients at follow-up (21.36 [6.53] ng/ml) was comparable to that of controls (23.58 [6.81] ng/ml; t = 1.09; P = 0.28). In addition, the correlation coefficients were in the expected direction: the higher the increase in serum BDNF, the better was the test performance. However, they were statistically nonsignificant except in one case: there was a significant negative correlation between increase in BDNF levels and reduction in TMT “A” duration, in the Yoga-alone group [Figure 1; P = 0.009; r = −0.647].
Figure 1.
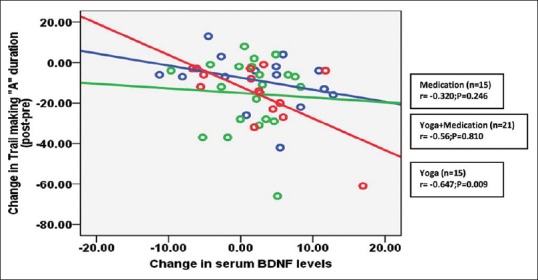
Correlation between change in brain-derived neurotrophic factor levels and Trail Making test “A” duration in patients with depression
DISCUSSION
Patients with depression in this study had impaired performance on most neuropsychological tests when compared to healthy controls. Their performance improved significantly following treatment – improvement was observed across all three treatment groups, antidepressants alone, antidepressants and yoga, and yoga alone. Neuropsychological performance of patients “normalized” after 3 months of treatment. There was a significant increase in the serum BDNF levels in these patients. The increase in serum BDNF correlated with improvement in performance in most neuropsychological tests although it reached statistical significance in only one of the tests of psychomotor speed (Trail-making test A duration) in patients who received yoga alone as treatment.
The finding of impaired neuropsychological test performance is consistent with a number of previous studies that have compared the performance of patients with depression and healthy controls.[2,3,4,5,6] Improvement in the test performance has also been noted in many previous studies.[7,34,35] This is the first study to demonstrate improvement in cognitive functions with yoga therapy alone in depression. This finding is not surprising, given that a number of previous studies have shown that cognitive functions show substantial improvement with yoga in patients with other conditions and healthy controls.[22,36,37,38] A significant increase was noted in serum BDNF level as reported in our previous paper. The direction of correlation between increase in serum BDNF level was in the expected direction – the more the increase in serum BDNF level, the better was the performance in neuropsychological test performance across all tests and groups although it did not reach the level of statistical significance in most cases. Given that the sample sizes were small in each of the subgroups of patients; this perhaps reflected a type-II error.
There was a significant negative correlation between increase in serum BDNF level and duration of time taken to complete the TMT “A” in Yoga-alone group. This reflects the positive effect of yoga on both serum BDNF level and psychomotor speed. The lack of statistical significance in correlations in other groups perhaps reflects possible confounding effects of antidepressants on this correlation. Yoga may have different biological mechanisms that operate with mood-elevation, reduction in cortisol, and BDNF enhancement pathways. A recently published article demonstrated a significant correlation between increase in serum BDNF and reduction in serum cortisol levels in patients with depression.[39] These mechanisms could have mediated the effect of yoga on neuropsychological test performance. Stress reduction mechanisms, by way of quieting the HPA axis, may be particularly relevant to the effect of yoga in reducing depression.
Studying antidepressant-naïve or antidepressant-free patients with depression and the use of neuropsychological tests standardized for local population are the important strengths of this study. The person who assessed the neuropsychological performance of the patients was not blind to the treatment status of the patients. Although this may be perceived as a drawback of the study since the tests provide fairly objective measures of neuropsychological functioning of patients, there was little scope for systematic bias. Some additional limitations of the study need to be mentioned: use of a limited set of neuropsychological tests, a substantial number of dropouts and the possibility of higher education levels in the Yoga group influencing the results. Further, other factors such as lifestyle modification by participants after exposure to yoga such as better nutrition, more attention to physical exercise, and sleep hygiene might have influenced the results in terms of better neuropsychological functions and BDNF levels. The reader may also refer to a recent critical review that summarizes the current evidence for efficacy, plausible mechanisms of action and future research directions in the area of yoga as an intervention in depression.[40] Attending the yoga training may have increased the participants’ awareness and receptiveness to adopt health promotion strategies.
Future studies could look at into the biochemical mechanisms by which yoga practice increases serum BDNF levels and also association between serum BDNF levels\neuropsychological functions and volumetric changes in the hippocampus, as the reduction of hippocampal volume is seen in patients with depression. This study provides preliminary evidence for the effect of yoga therapy on cognitive performance of patients with depression and a possible correlation with neuroplastic mechanisms. The evidence suggests that yoga may be incorporated in clinical settings as a mind-body intervention to enhance the cognition and BDNF levels in patients with depression. The findings of this study need replication in larger samples with the use of more comprehensive neuropsychological assessments.
Financial support and sponsorship
This study was supported by grants from the Ministry of AYUSH, Government of India.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank Dr. R Nagarathna, Dean of Yoga and life sciences, SVYASA, Bangalore, for her guidance, support, and encouragement.
REFERENCES
- 1.APA. Diagnostic and Statistical Manual-Text Revision (DSM-IV-TRim) Fourth Edition, Text Revision. Washington DC: American Psychiatric Association; 2000. [Google Scholar]
- 2.Austin MP, Mitchell P, Wilhelm K, Parker G, Hickie I, Brodaty H, et al. Cognitive function in depression: A distinct pattern of frontal impairment in melancholia? Psychol Med. 1999;29:73–85. doi: 10.1017/s0033291798007788. [DOI] [PubMed] [Google Scholar]
- 3.Moritz S, Birkner C, Kloss M, Jahn H, Hand I, Haasen C, et al. Executive functioning in obsessive-compulsive disorder, unipolar depression, and schizophrenia. Arch Clin Neuropsychol. 2002;17:477–83. [PubMed] [Google Scholar]
- 4.Porter RJ, Gallagher P, Thompson JM, Young AH. Neurocognitive impairment in drug-free patients with major depressive disorder. Br J Psychiatry. 2003;182:214–20. doi: 10.1192/bjp.182.3.214. [DOI] [PubMed] [Google Scholar]
- 5.Tombaugh TN. Trail making test A and B: Normative data stratified by age and education. Arch Clin Neuropsychol. 2004;19:203–14. doi: 10.1016/S0887-6177(03)00039-8. [DOI] [PubMed] [Google Scholar]
- 6.Wang X, Hou Z, Yuan Y, Hou G, Liu Y, Li H, et al. Association study between plasma GDNF and cognitive function in late-onset depression. J Affect Disord. 2011;132:418–21. doi: 10.1016/j.jad.2011.03.043. [DOI] [PubMed] [Google Scholar]
- 7.Wroolie TE, Williams KE, Keller J, Zappert LN, Shelton SD, Kenna HA, et al. Mood and neuropsychological changes in women with midlife depression treated with escitalopram. J Clin Psychopharmacol. 2006;26:361–6. doi: 10.1097/01.jcp.0000227699.26375.f8. [DOI] [PubMed] [Google Scholar]
- 8.Story TJ, Potter GG, Attix DK, Welsh-Bohmer KA, Steffens DC. Neurocognitive correlates of response to treatment in late-life depression. Am J Geriatr Psychiatry. 2008;16:752–9. doi: 10.1097/JGP.0b013e31817e739a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brown ES, Bobadilla L, Nejtek VA, Perantie D, Dhillon H, Frol A, et al. Open-label nefazodone in patients with a major depressive episode and alcohol dependence. Prog Neuropsychopharmacol Biol Psychiatry. 2003;27:681–5. doi: 10.1016/S0278-5846(03)00079-4. [DOI] [PubMed] [Google Scholar]
- 10.Allen SJ, Dawbarn D. Clinical relevance of the neurotrophins and their receptors. Clin Sci (Lond) 2006;110:175–91. doi: 10.1042/CS20050161. [DOI] [PubMed] [Google Scholar]
- 11.Beyer JL, Krishnan KR. Volumetric brain imaging findings in mood disorders. Bipolar Disord. 2002;4:89–104. doi: 10.1034/j.1399-5618.2002.01157.x. [DOI] [PubMed] [Google Scholar]
- 12.Schmidt HD, Duman RS. The role of neurotrophic factors in adult hippocampal neurogenesis, antidepressant treatments and animal models of depressive-like behavior. Behav Pharmacol. 2007;18:391–418. doi: 10.1097/FBP.0b013e3282ee2aa8. [DOI] [PubMed] [Google Scholar]
- 13.Karege F, Bondolfi G, Gervasoni N, Schwald M, Aubry JM, Bertschy G, et al. Low brain-derived neurotrophic factor (BDNF) levels in serum of depressed patients probably results from lowered platelet BDNF release unrelated to platelet reactivity. Biol Psychiatry. 2005;57:1068–72. doi: 10.1016/j.biopsych.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 14.Varambally S, Naveen GH, Rao MG, Thirthalli J, Sharma R, Christopher R, et al. Low serum brain derived neurotrophic factor in non-suicidal out-patients with depression: Relation to depression scores. Indian J Psychiatry. 2013;55:S397–9. doi: 10.4103/0019-5545.116311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aydemir O, Deveci A, Taneli F. The effect of chronic antidepressant treatment on serum brain-derived neurotrophic factor levels in depressed patients: A preliminary study. Prog Neuropsychopharmacol Biol Psychiatry. 2005;29:261–5. doi: 10.1016/j.pnpbp.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 16.Huang TL, Lee CT, Liu YL. Serum brain-derived neurotrophic factor levels in patients with major depression: Effects of antidepressants. J Psychiatr Res. 2008;42:521–5. doi: 10.1016/j.jpsychires.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 17.Matrisciano F, Bonaccorso S, Ricciardi A, Scaccianoce S, Panaccione I, Wang L, et al. Changes in BDNF serum levels in patients with major depression disorder (MDD) after 6 months treatment with sertraline, escitalopram, or venlafaxine. J Psychiatr Res. 2009;43:247–54. doi: 10.1016/j.jpsychires.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eker C, Kitis O, Taneli F, Eker OD, Ozan E, Yucel K, et al. Correlation of serum BDNF levels with hippocampal volumes in first episode, medication-free depressed patients. Eur Arch Psychiatry Clin Neurosci. 2010;260:527–33. doi: 10.1007/s00406-010-0110-5. [DOI] [PubMed] [Google Scholar]
- 19.Oral E, Canpolat S, Yildirim S, Gulec M, Aliyev E, Aydin N, et al. Cognitive functions and serum levels of brain-derived neurotrophic factor in patients with major depressive disorder. Brain Res Bull. 2012;88:454–9. doi: 10.1016/j.brainresbull.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 20.Pittenger C, Duman RS. Stress, depression, and neuroplasticity: A convergence of mechanisms. Neuropsychopharmacology. 2008;33:88–109. doi: 10.1038/sj.npp.1301574. [DOI] [PubMed] [Google Scholar]
- 21.Pilkington K, Kirkwood G, Rampes H, Richardson J. Yoga for depression: The research evidence. J Affect Disord. 2005;89:13–24. doi: 10.1016/j.jad.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 22.Sharma VK, Das S, Mondal S, Goswami U, Gandhi A. Effect of Sahaj Yoga on neuro-cognitive functions in patients suffering from major depression. Indian J Physiol Pharmacol. 2006;50:375–83. [PubMed] [Google Scholar]
- 23.Naveen GH, Thirthalli J, Rao MG, Varambally S, Christopher R, Gangadhar BN, et al. Positive therapeutic and neurotropic effects of yoga in depression: A comparative study. Indian J Psychiatry. 2013;55:S400–4. doi: 10.4103/0019-5545.116313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hariprasad VR, Varambally S, Shivakumar V, Kalmady SV, Venkatasubramanian G, Gangadhar BN, et al. Yoga increases the volume of the hippocampus in elderly subjects. Indian J Psychiatry. 2013;55:S394–6. doi: 10.4103/0019-5545.116309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The mini-international neuropsychiatric interview (M.I.N.I): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 27.Naveen GH, Rao MG, Vishal V, Thirthalli J, Varambally S, Gangadhar BN, et al. Development and feasibility of yoga therapy module for out-patients with depression in India. Indian J Psychiatry. 2013;55:S350–6. doi: 10.4103/0019-5545.116305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rey A, editor. L'examen Clinique En Psychologie. Paris: Presses Universitaires de France; 1964. [Google Scholar]
- 29.Schmidt M. Rey Auditory Verbal Learning Test: A Handbook. Los Angeles, California: Western Psychological Services; 1996. [Google Scholar]
- 30.Lezak MD. Neuropsychological assessment. Third Edition. Newyork: Oxford University Press, Inc; 1995. [Google Scholar]
- 31.Corrigan JD, Hinkeldey NS. Relationships between parts A and B of the trail making test. J Clin Psychol. 1987;43:402–9. doi: 10.1002/1097-4679(198707)43:4<402::aid-jclp2270430411>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 32.Gaudino EA, Geisler MW, Squires NK. Construct validity in the trail making test: What makes part B harder? J Clin Exp Neuropsychol. 1995;17:529–35. doi: 10.1080/01688639508405143. [DOI] [PubMed] [Google Scholar]
- 33.Lezak MD, Howieson DB, Loring DW, editors. Neuropsychological Assessment. 4th ed. New York: Oxford University Press; 2004. [Google Scholar]
- 34.Culang-Reinlieb ME, Sneed JR, Keilp JG, Roose SP. Change in cognitive functioning in depressed older adults following treatment with sertraline or nortriptyline. Int J Geriatr Psychiatry. 2012;27:777–84. doi: 10.1002/gps.2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Herrera-Guzmán I, Gudayol-Ferré E, Lira-Mandujano J, Herrera-Abarca J, Herrera-Guzmán D, Montoya-Pérez K, et al. Cognitive predictors of treatment response to bupropion and cognitive effects of bupropion in patients with major depressive disorder. Psychiatry Res. 2008;160:72–82. doi: 10.1016/j.psychres.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 36.Hariprasad VR, Koparde V, Sivakumar PT, Varambally S, Thirthalli J, Varghese M, et al. Randomized clinical trial of yoga-based intervention in residents from elderly homes: Effects on cognitive function. Indian J Psychiatry. 2013;55:S357–63. doi: 10.4103/0019-5545.116308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Manjunath NK, Telles S. Spatial and verbal memory test scores following yoga and fine arts camps for school children. Indian J Physiol Pharmacol. 2004;48:353–6. [PubMed] [Google Scholar]
- 38.Naga Venkatesha Murthy PJ, Janakiramaiah N, Gangadhar BN, Subbakrishna DK. P300 amplitude and antidepressant response to Sudarshan Kriya Yoga (SKY) J Affect Disord. 1998;50:45–8. doi: 10.1016/s0165-0327(98)00029-9. [DOI] [PubMed] [Google Scholar]
- 39.Naveen GH, Varambally S, Thirthalli J, Rao M, Christopher R, Gangadhar BN, et al. Serum cortisol and BDNF in patients with major depression-effect of yoga. Int Rev Psychiatry. 2016;28:273–8. doi: 10.1080/09540261.2016.1175419. [DOI] [PubMed] [Google Scholar]
- 40.Uebelacker LA, Epstein-Lubow G, Gaudiano BA, Tremont G, Battle CL, Miller IW, et al. Hatha yoga for depression: Critical review of the evidence for efficacy, plausible mechanisms of action, and directions for future research. J Psychiatr Pract. 2010;16:22–33. doi: 10.1097/01.pra.0000367775.88388.96. [DOI] [PubMed] [Google Scholar]


