Abstract
Background:
Contrary to the popular belief concerning the aphrodisiac effects of alcohol, there exists scientific evidence which conclude on sexual dysfunction caused by chronic alcohol use. There is a dearth of studies from India.
Aim:
The aim is to estimate the prevalence and correlates of sexual dysfunction in alcohol-dependent patients and to explore the association between sexual dysfunction and various alcohol-related variables.
Materials and Methods:
The study employed a cross-sectional descriptive design and recruited 84 male patients admitted for de-addiction in a tertiary care center. The evaluation was conducted using a specially designed intake proforma and tools such as Severity of Alcohol Dependence Questionnaire, Arizona Sexual Experience Scale, and International Classification of Disease, 10th revision, diagnostic criteria for research.
Results:
Thirty-seven percent of the patients had sexual dysfunction – the most common type being erectile dysfunction (25%), followed by dysfunction in satisfying orgasm (20%) and premature ejaculation (15.5%). Sexual dysfunction was significantly associated with the duration of alcohol dependence, amount of alcohol consumed per day, and severity of alcohol dependence.
Conclusions:
Sexual dysfunction is common in male patients with alcohol dependence. The study highlights the detrimental effects of alcohol on sexual function and this information can be utilized in motivational interviewing of patients with alcohol dependence syndrome.
Keywords: Arizona sexual experiences scale, severity of alcohol dependence questionnaire, sexual dysfunction in alcohol dependence syndrome
INTRODUCTION
Alcohol and sexuality have been paired throughout history, poetry, prose, and brief. Although alcohol may foster the initiation of sexual activity by relieving anxiety and inhibitions,[1] persistent and chronic use of alcohol is known to induce sexual dysfunction.[2] In spite of evidence to the contrary, people often continue to believe that alcohol improves their quality of sexual function.
Proper sexual functioning provides a sense of psychological, physical, and social well-being and is one of the most important elements of quality of life.[3] Dissatisfaction in sexual life is often associated with anger, increased rates of marital violence, less warmth, and unity in relationships, breakups – all of which may in turn worsen the alcohol consumption.
Of the various mechanisms postulated to explain alcohol-induced sexual dysfunction, some of them are inhibition of hypothalamic gonadotropin-releasing hormone and/or pituitary luteinizing hormone,[4,5] thereby altering the hypothalamo–pituitary–adrenal and the hypothalamo–pituitary–gonadal axis, reduction in plasma testosterone levels,[6] increasing the inhibitory activity of gamma-amino butyric acid receptor and decreasing the excitatory activity of glutamate receptor in central nervous system (CNS),[7] psychological factors such as lack of arousability and disinterest in sex in partners – due to aversion, rejection, retaliation for her husband's undesirable drinking behavior, and psychiatric comorbidities such as anxiety and depression as well as those induced by psychotropic medications.
The prevalence of alcohol-induced sexual dysfunction is unclear, probably because of underreporting. Sexual disorders ranging from 8% to 95.2% have been reported in men who have chronic alcohol use.[8,9,10,11,12,13,14,15,16] The common dysfunctions reported were lack of sexual desire,[10,11,12] premature ejaculation,[13,15] and erectile dysfunction.[14,16,17] Some of the predictors of sexual dysfunction noted were advancing age, low educational level, unemployment, early age of onset of alcohol use, greater duration of alcohol dependence, concurrent tobacco use, greater quantity and frequency of drinking, and presence of liver disease.[16,18] Various studies have reported no or negative association between sexual dysfunction and alcohol intake,[18,19,20,21,22] and this has been a matter of debate ever since.
There are various studies that have glanced into sexual dysfunction due to alcohol, but those reported from India are highly insufficient. To the best of our knowledge, studies which tried to find the predictors of sexual dysfunction were scanty.
In a state like Kerala where there is high alcohol consumption, an insight into the matter of sexual dysfunction caused by alcohol can act as a motivational factor to quit alcohol.
The present study was undertaken with the aim of assessing the prevalence of sexual dysfunction in male inpatients with alcohol dependence syndrome and to explore the relationship between amount of alcohol consumed as well as severity of alcohol dependence and sexual dysfunction. We also aimed to find the correlates of sexual dysfunction in patients with alcohol dependence syndrome. The exclusion of female population was necessitated by the fact that the prevalence of alcohol dependence syndrome among female subjects in Kerala was found to be negligible (<1%) as per a district-based survey report.[23]
MATERIALS AND METHODS
This cross-sectional study was conducted in the Department of Psychiatry, MOSC Medical College, Kolenchery, over 18 months (from January 2015 to June 2016). A total of 84 consecutive male patients admitted for de-addiction with a diagnosis of alcohol dependence syndrome according to The International Classification of Diseases 10th revision diagnostic criteria for research (ICD-10 DCR) were included in the study. All consecutive patients who fulfilled the inclusion and exclusion criteria were assigned to the study group. All patients were subjected to routine clinical examination and biochemical investigations including blood glucose and liver enzymes. Appropriate interventions and referrals were provided for those with altered clinical findings and impaired biochemical parameters.
Inclusion criteria
Male patients between 20 and 50 years of age.
Married or having a regular sexual partner.
Exclusion criteria
Clinically elicited history of primary sexual dysfunction (i.e., history of sexual dysfunction with onset before initiation of alcohol use).
Comorbid systemic illnesses – hypertension, diabetes mellitus, signs and symptoms or investigation findings suggestive of hepatic cirrhosis, other systemic illnesses in terminal stages, clinical diagnosis of endocrine disorders, history of genitourinary surgery, neurological disorders, and spinal cord lesions.
Comorbid psychiatric disorders – dementia, delirium and other organic disorders, mental retardation, psychotic disorders such as schizophrenia, delusional disorder and others, mood disorders, and anxiety disorders (those with transient or subthreshold symptoms were included).
Substance use other than alcohol and tobacco.
Those on medications which may affect sexual function (antidepressants, antipsychotics, disulfiram, antihypertensives, steroids, etc.).
Tools for assessment
-
Proforma for sociodemographic and clinical course variables – to collect details regarding various study variables.
- Sociodemographic variables – Age, education, occupation, religion, monthly income, domicile, duration of marriage, and age at marriage
- Alcohol-related variables – Age at first drink, age of onset of dependence, duration of alcohol dependence, drinking pattern, type of alcohol, quantity consumed per day, family history of alcohol dependence and severity of alcohol dependence questionnaire (SADQ) score
- Tobacco-related variables – History of tobacco use, duration of tobacco use/dependence.
- Sexual dysfunction-related variables – history of sexual dysfunction, subtypes of sexual dysfunction, and Arizona Sexual Experiences Scale (ASEX) score.
SADQ to assess the severity of alcohol dependence:[24] A score of ≥31 indicates severe alcohol dependence, 16 to 30 – moderate dependence, and <16 indicates mild physical dependence.
ASEX to assess sexual dysfunction:[25] A user-friendly rating scale that quantifies sex drive, arousal, vaginal lubrication/penile erection, ability to reach orgasm, and satisfaction from orgasm. The score ranges from 5 to 30. Sexual dysfunction is defined as: Total score ≥19, or a score of ≥5 on any item, or ≥4 on three items.
ICD-10-DCR[26,27] for diagnosing alcohol dependence syndrome (F10.2) and sexual dysfunction, not caused by organic disorder or disease (F52).
Procedure
After obtaining approval from the Institutional Review Board and Ethical Committee, the patients admitted for inpatient de-addiction with a diagnosis of ICD-10-DCR alcohol dependence syndrome (withdrawal state –uncomplicated) were screened. After applying the inclusion and exclusion criteria, the patients were selected. Participants were given information sheet and informed consent was obtained from them. Data were collected and recorded using the proforma specially designed for the study. Information was collected regarding sociodemographic, alcohol-related, tobacco-related, and sexual dysfunction-related variables. To avoid bias, the ratings were sought after 2 weeks of inpatient stay, after the withdrawal period was completely over and ensuring that the patients were properly detoxified with benzodiazepines. The severity of alcohol dependence was assessed using SADQ questionnaire. ICD-10-DCR F52 criteria were used to diagnose sexual dysfunction, and the subtypes and severity were quantified using ASEX. The relationship between sexual dysfunction and the different study variables was examined using relevant statistical tools.
Statistical analysis
Data were analyzed using descriptive statistics such as frequency and percentage for categorical variables and mean ± standard deviation for continuous variables. Chi-square test and Pearson's correlation coefficient were used to evaluate the statistical significance of bivariate associations. Multiple linear regression analysis was employed after adjusting for age of subjects. For all the tests, the statistical significance was fixed at 5% level (P < 0.05). Statistical analysis was performed using the Statistical Package for Social Sciences (SPSS for Windows, Version 20, SPSS Inc., Chicago, IL, USA).[27]
The sample size was calculated using the mean and standard deviation values obtained from a similar study conducted at NIMHANS, BENGALURU,[13] fixing the confidence level at 95% and precision at 10%, using the nMaster software. (Version 2.0, Department of Biostatistics, CMC, Vellore).
RESULTS
Sociodemographic variables
The mean age of the patients was 39.14 ± 6.6 years (range: 22–49 years). Out of the 84 patients in our study sample, majority had education up to 12th standard (87%). All of them were employed, of which 45% were skilled laborers. About 54% of the patients got married between 26 and 35 years of age [Table 1].
Table 1.
Sociodemographic profile and psychoactive substance-related variables (n=84)
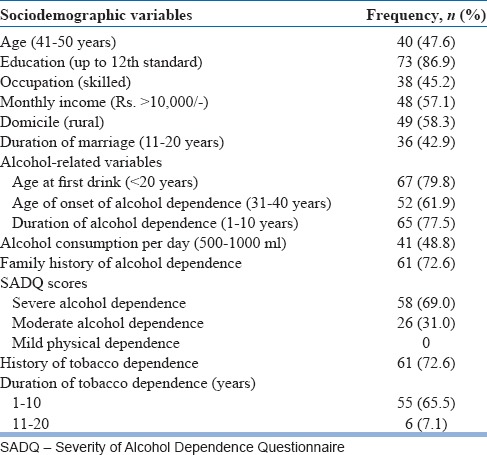
Alcohol-related variables
In our study group, 45% had duration of alcohol consumption between 21 and 30 years. About 80% of the patients had started consuming alcohol during adolescence. Nearly 62% of the patients had begun alcohol consumption in dependence pattern by the age of 31–40 years. The mean quantity of alcohol consumed per day was 636.78 ± 303.04 ml (range: 120–1500 ml). About 73% had family history of alcohol dependence. Sixty-nine percent had severe alcohol dependence as per the SADQ scores [Table 1].
Tobacco-related variables
About 73% of the patients in the study group reported the history of tobacco dependence also, out of which, 90% had duration of dependence of 1–10 years [Table 1].
Sexual dysfunction-related variables
More than one-third (36.9%) of the study group reported having sexual dysfunction. The most common sexual dysfunction reported was erectile dysfunction which was present in a quarter (25%) of patients, followed by dysfunction in satisfying orgasm in 20% of patients. Premature ejaculation was present in 15.5% of the patients [Figure 1].
Figure 1.
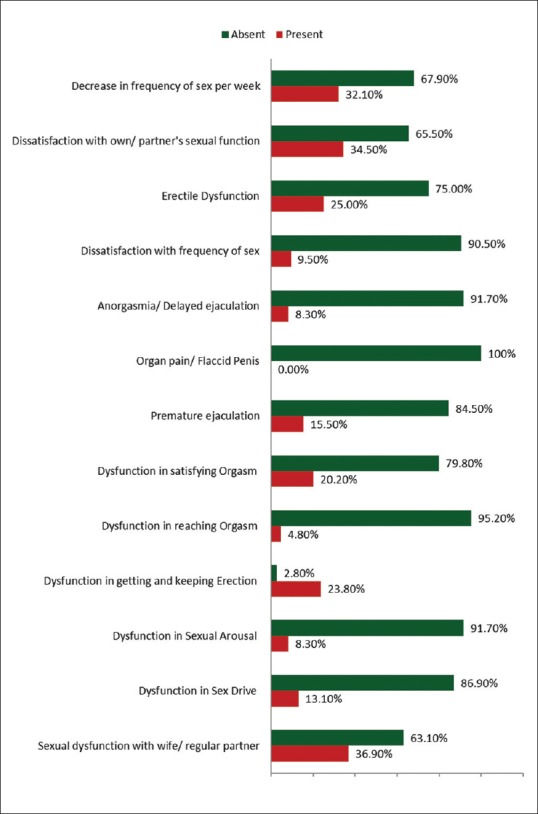
Distribution based on Sexual Dysfunction
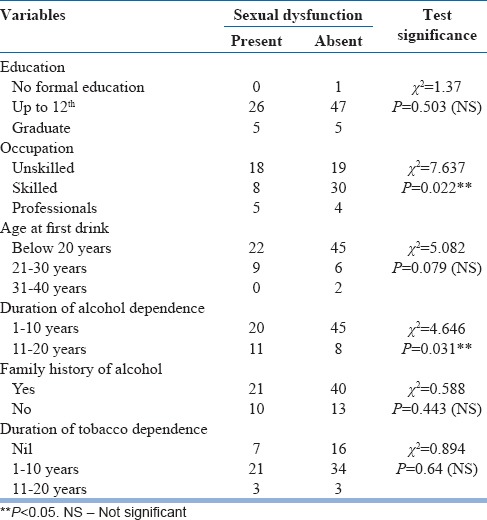
Association of sexual dysfunction with study variables
Significant association was found with only one sociodemographic variable, that is, occupation. More unskilled workers reported sexual dysfunction than skilled workers, whereas 55.6% of the professionals reported significant sexual dysfunction (P = 0.022). Among the alcohol-related variables, sexual dysfunction was significantly associated with duration of alcohol dependence (P = 0.031). None of the tobacco-related variables such as history and duration of tobacco dependence showed any statistically significant association with sexual dysfunction [Table 2].
Table 2.
Association of sexual dysfunction with sociodemographic, alcohol, and tobacco-related variables
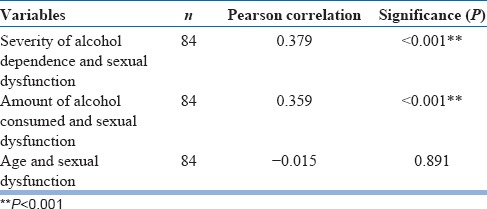
Correlates of sexual dysfunction
A significant positive correlation was obtained between variables like severity of alcohol dependence as well as the amount of alcohol consumed per day and sexual dysfunction [Table 3].
Table 3.
Correlates of sexual dysfunction
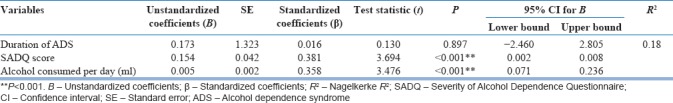
Predictors of sexual dysfunction in subjects with alcohol dependence
On doing linear regression analysis with ASEX total score as the dependent variable and severity of alcohol dependence and amount of alcohol consumed per day as the independent variables, both these variables were identified as significant predictors for sexual dysfunction. Even after adjusting for age of the patients, severity of alcohol dependence and amount of alcohol consumed per day remained as significant predictors [Table 4].
Table 4.
Linear regression analysis of predictors of sexual dysfunction (adjusted to age of the patients)
DISCUSSION
Sex is perhaps the most unique aspect of life on planet earth which makes it heavenly and is a beautiful process of expressing desire, affection, trust and mutual warmth, and experiencing the ultimate bliss of “Tanmayam.” Alcohol increases sexual urge by decreasing the inhibitions; at the same time, it is found to cause impairment in sexual functioning through various mechanisms.
In this study, 84 consecutive patients with alcohol dependence were evaluated in a single sitting using the specially designed proforma and various rating scales, to determine the prevalence and correlates of sexual dysfunction. To get 84 patients as study sample, we had assessed 216 patients, out of which 132 were excluded as per exclusion criteria. Most of them were excluded as they had diabetes or hypertension.
Sociodemographic profile
The mean age of the patients was 39.14 ± 6.6 years. In the study by Arackal and Benegal,[13] the mean age was approximately 37 years, whereas it was 39 years in the study conducted by Saha.[28]
Majority of our study population had education up to 12th standard (87%) reflecting the higher literacy rate of Kerala. All were employed, out of which 45% were skilled laborers – which included drivers, construction workers, painters, plumbers, and electricians – majority getting daily wages, which is an important risk factor for daily drinking. All of the patients reported monogamous relationships with their wives abiding with the traditional concepts of Kerala, even though they were given the confidentiality to report about regular sexual relationships with other partners.
Alcohol-related variables
Even though 80% of our patients had their first drink before 20 years of age, 62% started drinking in dependence pattern only after 10–20 years. Brandy was the preferred drink in 44% of the patients. This is in line with the finding which says that 94% of the sales for beverages in Kerala is for rum and brandy,[29] which may be attributed to their easier availability and cheaper price. The mean quantity of alcohol consumed per day was 636.78 ± 303.04 ml. Majority (73%) had family history of alcohol consumption, this fact being supported by family and twin studies, which showed moderate-to-high pattern of inheritance for Alcohol dependence syndrome (ADS).[30] About 69% had severe alcohol dependence when SADQ was administered, which may be due to the fact that the study sample was chosen from the group of patients admitted for inpatient de-addiction in a tertiary care center.
Tobacco-related variables
About 73% of the patients in the study group reported a history of tobacco dependence also, out of which 90% had duration of dependence of 1–10 years. Most of the similar studies have also included tobacco use because it was found to be a common comorbidity in alcohol-dependent patients.[13]
Sexual dysfunction-related variables
In our study, sexual dysfunction was present in 37% of the patients, replicating the previous study findings.[8,9,10,11,12,13,14,15,16] The most common sexual dysfunction reported by our study group was erectile dysfunction which was present in 25% of the patients, followed by dysfunction in satisfying orgasm in 20% of patients. In a study of psychosexual dysfunction in patients with alcohol dependence by Aswal et al.,[31] the prevalence of sexual dysfunction was 76%. Impotence was the most common diagnosis in 28%, followed by loss of libido (26%), delayed ejaculation (10%), excessive libido (8%), and premature ejaculation (4%). Sexual dysfunction was present in 72% of the study population as reported by Arackal and Benegal.[13] They had used sexual dysfunction checklist instead of ASEX scale which, in fact, has more validity and reliability. Premature ejaculation was the major dysfunction, followed by low sexual desire and erectile dysfunction.
About one-third of the patients reported a decrease in frequency of sex per week over the past 1 year, some of the reported reasons being falling to sleep early under intoxication, wives feeling aversive towards having sex with the patients who approach them under intoxication, and wives being scared to share bed with the intoxicated patients due to their tendency for sexual aggression.
Relationship between sexual dysfunction and study variables
Among the various sociodemographic variables, we could not find any association with sexual dysfunction except for the variable, occupation. More unskilled workers reported sexual dysfunction than skilled workers; moreover, half of the professionals reported significant sexual dysfunction (P = 0.022). The professionals, probably because of their higher education, awareness, and less stigmatizing attitude toward disclosing about sexual matters, might have reported more freely regarding their sexual dysfunction.
Sexual dysfunction had a significant association with the duration of alcohol dependence. In the study done by Saha,[28] the chance of developing sexual dysfunction appears to increase with increasing years of alcohol consumed. This finding was different from the study of Arackal and Benegal,[13] in which no significant association was found with factors such as duration of alcohol consumption, age at first drink, pattern of drinking, type of alcohol consumed, or with family history of alcohol use. In a pilot study conducted by Mandell and Miller[32] the quantity, frequency, and duration of drinking, from onset of regular drinking to present, were related to sexual dysfunction. As the duration of dependence increases, the cumulative effects of alcohol on CNS, hepatic, endocrine, and gonadal systems will result in the greater severity of sexual dysfunction.
Although tobacco use has been a significant determinant of sexual dysfunction in many studies,[33,34] no significant association was found in our study with any of the tobacco-related variables, namely, history of and duration of tobacco dependence. This might be due to the shorter duration of tobacco dependence in our study. Furthermore, we did not use any standardized scales for assessing tobacco dependence. In a study on the prevalence of sexual dysfunction and potential risk factors that impair sexual function in Turkish females,[35] no significant differences were detected in the smoking history in patients with and without sexual dysfunction.
On examining the correlates of sexual dysfunction in the study group, we found a significant positive correlation with severity of alcohol dependence and the amount of alcohol consumed per day. This finding agrees with earlier studies.[13,14,17] The positive correlation may be explained by the greater neurotoxic effects, actions on gonadal hormones and probable reversible vagal neuropathy which occurs with long-term heavy drinking. No significant correlation was found between age and sexual dysfunction.
On doing linear regression analysis of predictors of sexual dysfunction in patients with alcohol dependence syndrome, severity of alcohol dependence and amount of alcohol consumed per day emerged as significant predictors, after adjusting for age as a confounding factor. A South Indian study[13] revealed amount of alcohol consumed per day as a significant predictor for the number of sexual complaints likely to occur in the future.
Sexual dysfunction is of high clinical relevance in patients with alcohol dependence syndrome, as it often leads to treatment nonadherence and sexual or marital disharmony, and is a common contributor of relapses. Yet, it is often neglected and unexplored in routine clinical care. This is also reflected by the limited research in this area.
Implications
The results of this study have implications in terms of awareness creation, improvising de-addiction services, training and further research on this special population with alcohol dependence syndrome and their spouses/partners. This may be extended to patients with other psychoactive substance dependence also, thereby bringing out their cumulative effects. Furthermore, it has paved the way for understanding the need for comprehensive, feasible, and psychosocial/sexual services for patients with alcohol dependence having sexual dysfunction. Moreover, this study also enlightens the need to regularly assess sexual function in ADS patients. Planning of similar studies in urban and rural areas of India and also in female gender as well as at the community level can be done. Further work toward planning and implementing newer alcohol policies and regulations can be recommended based on findings from such studies. Sensitization programs at schools and colleges highlighting this aspect, as well as interventional programs and treatment effectiveness studies, comparing the various methods to correct alcohol-induced sexual dysfunction, can be tried.
Limitations
Our sample size was 84; a larger sample size would be required for better generalization of the results. Moreover, the study being conducted among patients admitted for de-addiction in a tertiary care hospital also narrowed the chances for generalization of the findings. We used nonrandomized sampling technique in this study. Cross-sectional nature of our study shows association rather than causality. The personality, psychopathology, and coping strategies employed by the spouse, family dynamics, marital functioning, and other environmental and psychosocial elements which may be additional contributory factors for sexual dysfunction in alcohol dependence syndrome, were not explored in the current study. A comparison with appropriate age- or sex-matched sober individuals as controls would have given more reproducible results. There is a major need for long-term prospective research, if the issues regarding causality have to be adequately addressed. The data on alcohol, tobacco, and sexual function-related parameters were based on self-report, which is vulnerable for bias. Even though the assessments were conducted on patients during early stages of recovery after ensuring that the withdrawal period is fully resolved, it is unclear as to what extent this might have affected the findings.
CONCLUSIONS
Sexual dysfunction appears to be common among male patients with alcohol dependence syndrome – the most common being erectile dysfunction (25%), followed by dysfunction in satisfying orgasm (20%) and premature ejaculation (15%). Our study highlights the detrimental effects of alcohol on sexual functioning, and this knowledge can be utilized while explaining the medical model during motivational interviewing and motivation enhancement therapy sessions of patients with alcohol dependence syndrome.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We express our heartfelt gratitude towards our colleagues and all those subjects and their spouses who participated in this study for their kind co-operation and goodwill. The authors also wish to thank Mrs. Renju Susan Baby, Associate Professor, Department of Mental Health Nursing, AIIMS, Bhubaneswar, for her guidance and assistance in statistical analysis.
REFERENCES
- 1.Sadock VA. Normal human sexuality and sexual dysfunctions. In: Sadock BJ, Sadock VA, editors. Kaplan & Sadock's Comprehensive Textbook of Psychiatry. 8th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005. p. 1925. [Google Scholar]
- 2.Graham CA, Bancroft J. The sexual dysfunction. In: Gelder MG, Andreasen CN, Lopez-Ibor JJ, Geddes JR, editors. New Oxford Textbook of Psychiatry. 2nd ed. Oxford, UK: Oxford University Press; 2009. pp. 821–32. [Google Scholar]
- 3.Bancroft J, editor. In: Human Sexuality and Its Problems. 2nd ed. New York: Churchill Livingstone; 1983. Sexual problems; pp. 360–411. [Google Scholar]
- 4.Heinz A, Rommelspacher H, Gräf KJ, Kürten I, Otto M, Baumgartner A, et al. Hypothalamic-pituitary-gonadal axis, prolactin, and cortisol in alcoholics during withdrawal and after three weeks of abstinence: Comparison with healthy control subjects. Psychiatry Res. 1995;56:81–95. doi: 10.1016/0165-1781(94)02580-c. [DOI] [PubMed] [Google Scholar]
- 5.Hiney JK, Dees WL. Ethanol inhibits luteinizing hormone-releasing hormone release from the median eminence of prepubertal female rats in vitro: Investigation of its actions on norepinephrine and prostaglandin-E2. Endocrinology. 1991;128:1404–8. doi: 10.1210/endo-128-3-1404. [DOI] [PubMed] [Google Scholar]
- 6.Gordon GG, Altman K, Southren AL, Rubin E, Lieber CS. Effect of alcohol (ethanol) administration on sex-hormone metabolism in normal men. N Engl J Med. 1976;295:793–7. doi: 10.1056/NEJM197610072951501. [DOI] [PubMed] [Google Scholar]
- 7.Fernandes A, De Sousa A. Alcohol dependence and sexual dysfunction: A clinical review. Paripex Indian J Res. 2014;3:187–90. [Google Scholar]
- 8.Lemere F, Smith JW. Alcohol-induced sexual impotence. Am J Psychiatry. 1973;130:212–3. doi: 10.1176/ajp.130.2.212. [DOI] [PubMed] [Google Scholar]
- 9.Dişsiz M, Oskay ÜY. Evaluation of sexual functions in Turkish alcohol-dependent males. J Sex Med. 2011;8:3181–7. doi: 10.1111/j.1743-6109.2010.02091.x. [DOI] [PubMed] [Google Scholar]
- 10.Vijayasenan ME. Alcohol and sex. N Z Med J. 1981;93:18–20. [PubMed] [Google Scholar]
- 11.Jensen SB. Sexual customs and dysfunction in alcoholics: Part I. Br J Sex Med. 1979;6:29–32. [Google Scholar]
- 12.Whalley LJ. Sexual adjustment of male alcoholics. Acta Psychiatr Scand. 1978;58:281–98. doi: 10.1111/j.1600-0447.1978.tb00236.x. [DOI] [PubMed] [Google Scholar]
- 13.Arackal BS, Benegal V. Prevalence of sexual dysfunction in male subjects with alcohol dependence. Indian J Psychiatry. 2007;49:109–12. doi: 10.4103/0019-5545.33257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dachille G, Lamuraglia M, Leone M, Pagliarulo A, Palasciano G, Salerno MT, et al. Erectile dysfunction and alcohol intake. Urologia. 2008;75:170–6. [PubMed] [Google Scholar]
- 15.Pandey AK, Sapkota N, Tambi A, Shyangwa PM. Clinico-demographic profile, sexual dysfunction and readiness to change in male alcohol dependence syndrome inpatients in a tertiary hospital. Nepal Med Coll J. 2012;14:35–40. [PubMed] [Google Scholar]
- 16.Grover S, Mattoo SK, Pendharkar S, Kandappan V. Sexual dysfunction in patients with alcohol and opioid dependence. Indian J Psychol Med. 2014;36:355–65. doi: 10.4103/0253-7176.140699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee AC, Ho LM, Yip AW, Fan S, Lam TH. The effect of alcohol drinking on erectile dysfunction in Chinese men. Int J Impot Res. 2010;22:272–8. doi: 10.1038/ijir.2010.15. [DOI] [PubMed] [Google Scholar]
- 18.Schiavi RC, Stimmel BB, Mandeli J, White D. Chronic alcoholism and male sexual function. Am J Psychiatry. 1995;152:1045–51. doi: 10.1176/ajp.152.7.1045. [DOI] [PubMed] [Google Scholar]
- 19.Gümüş B, Yiǧitoǧlu MR, Lekili M, Uyanik BS, Müezzinoǧlu T, Büyüksu C, et al. Effect of long-term alcohol abuse on male sexual function and serum gonadal hormone levels. Int Urol Nephrol. 1998;30:755–9. doi: 10.1007/BF02564864. [DOI] [PubMed] [Google Scholar]
- 20.Cheng JY, Ng EM, Chen RY, Ko JS. Alcohol consumption and erectile dysfunction: Meta-analysis of population-based studies. Int J Impot Res. 2007;19:343–52. doi: 10.1038/sj.ijir.3901556. [DOI] [PubMed] [Google Scholar]
- 21.Okulate G, Olayinka O, Dogunro AS. Erectile dysfunction: Prevalence and relationship to depression, alcohol abuse and panic disorder. Gen Hosp Psychiatry. 2003;25:209–13. doi: 10.1016/s0163-8343(03)00015-x. [DOI] [PubMed] [Google Scholar]
- 22.Asboe D, Catalan J, Mandalia S, Dedes N, Florence E, Schrooten W, et al. Sexual dysfunction in HIV-positive men is multi-factorial: A study of prevalence and associated factors. AIDS Care. 2007;19:955–65. doi: 10.1080/09540120701209847. [DOI] [PubMed] [Google Scholar]
- 23.Vidhukumar K, Nazeer E, Anil P. Prevalence and pattern of alcohol use in Kerala – A district based survey. Int J Recent Trends Sci Technol. 2016;18:363–7. [Google Scholar]
- 24.Stockwell T, Murphy D, Hodgson R. The severity of alcohol dependence questionnaire: Its use, reliability and validity. Br J Addict. 1983;78:145–55. doi: 10.1111/j.1360-0443.1983.tb05502.x. [DOI] [PubMed] [Google Scholar]
- 25.McGahuey CA, Gelenberg AJ, Laukes CA, Moreno FA, Delgado PL, McKnight KM, et al. The Arizona Sexual Experience Scale (ASEX): Reliability and validity. J Sex Marital Ther. 2000;26:25–40. doi: 10.1080/009262300278623. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic Criteria for Research. Geneva: World Health Organization; 1993. pp. 70–1. [Google Scholar]
- 27.World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic Criteria for Research. Geneva: World Health Organization; 1993. pp. 140–5. [Google Scholar]
- 28.Saha A. Prevalence of sexual dysfunction in cases of alcohol dependence syndrome. Int J Adv Med. 2015;2:110–9. [Google Scholar]
- 29.Colley AJ. Deception in the service of the family: Observations on alcoholism treatment in Kerala, India. J Groups Addict Recover. 2016;11:194–204. [Google Scholar]
- 30.Pickens RW, Svikis DS, McGue M, Lykken DT, Heston LL, Clayton PJ, et al. Heterogeneity in the inheritance of alcoholism. A study of male and female twins. Arch Gen Psychiatry. 1991;48:19–28. doi: 10.1001/archpsyc.1991.01810250021002. [DOI] [PubMed] [Google Scholar]
- 31.Mandell W, Miller CM. Male sexual dysfunction as related to alcohol consumption: A pilot study. Alcohol Clin Exp Res. 1983;7:65–9. doi: 10.1111/j.1530-0277.1983.tb05413.x. [DOI] [PubMed] [Google Scholar]
- 32.Aswal S, Verma KK, Mathur A, Singh H, Jain L, Kapur T. Study of psychiatric morbidity and psychosexual dysfunctions in patients of alcohol dependence. Delhi Psychiatry J. 2012;15:379–84. [Google Scholar]
- 33.Lam TH, Abdullah AS, Ho LM, Yip AW, Fan S. Smoking and sexual dysfunction in Chinese males: Findings from men's health survey. Int J Impot Res. 2006;18:364–9. doi: 10.1038/sj.ijir.3901436. [DOI] [PubMed] [Google Scholar]
- 34.Feldman HA, Goldstein I, Hatzichristou DG, Krane RJ, McKinlay JB. Impotence and its medical and psychosocial correlates: Results of the Massachusetts male aging study. J Urol. 1994;151:54–61. doi: 10.1016/s0022-5347(17)34871-1. [DOI] [PubMed] [Google Scholar]
- 35.Cayan S, Akbay E, Bozlu M, Canpolat B, Acar D, Ulusoy E, et al. The prevalence of female sexual dysfunction and potential risk factors that may impair sexual function in Turkish women. Urol Int. 2004;72:52–7. doi: 10.1159/000075273. [DOI] [PubMed] [Google Scholar]


