Abstract
Objective
Pain is an extremely common complaint in primary care, and patient outcomes are often suboptimal. This project evaluated the impact of Project ECHO Pain videoconference case-based learning sessions on knowledge and quality of pain care in two Federally Qualified Health Centers.
Design
Quasi-experimental, pre-post intervention, with comparison group.
Setting
Two large, multisite federally qualified health centers in Connecticut and Arizona.
Subjects
Intervention (N = 10) and comparison (N = 10) primary care providers.
Methods
Primary care providers attended 48 weekly Project ECHO Pain sessions between January and December 2013, led by a multidisciplinary pain specialty team. Surveys and focus groups assessed providers’ pain-related knowledge and self-efficacy. Electronic health record data were analyzed to evaluate opioid prescribing and specialty referrals.
Results
Compared with control, primary care providers in the intervention had a significantly greater increase in pain-related knowledge and self-efficacy. Providers who attended ECHO were more likely to use formal assessment tools and opioid agreements and refer to behavioral health and physical therapy compared with control providers. Opioid prescribing decreased significantly more among providers in the intervention compared with those in the control group.
Conclusions
Pain is an extremely common and challenging problem, particularly among vulnerable patients such as those cared for at the more than 1,200 Federally Qualified Health Centers in the United States. In this study, attendance at weekly Project ECHO Pain sessions not only improved knowledge and self-efficacy, but also altered prescribing and referral patterns, suggesting that knowledge acquired during ECHO sessions translated into practice changes.
Keywords: Pain, Opioids, Project ECHO, Primary Care, Federally Qualified Health Center
Background
There are over 126 million American adults with pain, 25.3 million of whom report daily chronic pain [1]. Chronic low back pain is the leading cause of job-related disability in America [2]. In the United States, an estimated $560 to $635 billion in medical treatment and lost productivity costs are attributable to chronic pain each year [3]. Chronic pain has a significant adverse impact on quality of life [4]. Patients with chronic pain experience difficulty moving (89%), depression (77%), inability to concentrate (70%), strained relationships (52%), and loss of appetite (46%) [5]. Over half of patients with chronic pain feel they have little or no control over their pain symptoms [5].
Opioid prescribing has increased more than fourfold between 1999 and 2014 despite the growing evidence for significant, dose-dependent risk of serious harm and limited evidence of long-term benefits [6–8]. Over 18,000 Americans died from opioid analgesic overdose in 2014 [9]. New and more stringent guidelines for use of opioids to treat pain have recently been released, including the Centers for Disease Control and Prevention (CDC) Guideline for Prescribing Opioids for Chronic Pain [10].
Over half of patients with chronic pain receive their care in a primary care setting [11]. However, evidence suggests that primary care providers (PCPs) are not well-equipped to manage them effectively. Most PCPs express low confidence in their ability to manage pain effectively [12–15] and receive little or no education in chronic pain prevention, evaluation, and management during medical training [16–18]. A recent survey of internal medicine residents found that only 26% expressed confidence in managing chronic noncancer pain [19]. In addition, there is wide variation in primary care providers’ adherence to guidelines for the documentation and management of pain [10,20,21].
Pain complaints are more common in medically underserved patients [22,23], for whom access to specialty care is a significant challenge. Federally Qualified Health Centers (FQHCs) provide access to quality primary care, but they often struggle to find specialists willing to see patients with publicly funded insurance or without insurance coverage.
Project Extension for Community Health Outcomes (ECHO) is an evidence-based tele-mentoring intervention that connects PCPs with expert teams of specialist providers via regularly scheduled videoconference [24]. PCPs attend regular sessions on a specific topic or condition. By presenting actual cases from their practice and listening to brief didactics, participants gain the skills needed to prevent, evaluate, and manage a specific complex condition such as chronic pain. The goal of Project ECHO is to create local content experts within the primary care clinic, helping to bridge the gap between specialty and primary care and improving access and health outcomes for underserved patients.
Project ECHO was first developed to address rural health access issues for hepatitis C in New Mexico, but has now been replicated across the United States in both urban and rural locations for a wide range of conditions. Research on Project ECHO’s hepatitis C clinic has demonstrated that primary care providers can achieve equal or superior treatment outcomes as compared with specialists treating the same condition [25]. Less is known about the impact of Project ECHO for other conditions. We conducted a one-year trial in two community health centers to further explore the effect of Project ECHO Pain on a range of provider and patient outcomes.
Methods
Study Design
This study used a quasi-scientific design (pre-post intervention with comparison group) and was reviewed and approved by the Institutional Review Board at Community Health Center, Inc. (CHCI).
Setting
CHCI is a large, statewide FQHC with primary care sites in 13 locations across Connecticut, providing care to 140,000 medically underserved patients. More than 60% are racial/ethnic minorities, and more than 90% are below the 200% Federal Poverty Level. El Rio Community Health Center (El Rio) is an FQHC located in Tucson, Arizona, serving more than 92,000 patients across 16 clinic sites. Among these patients, 63.4% are racial/ethnic minorities (59% Hispanic, 7% American Indian, 4% Black/African American), 51.7% fall below the 200% Federal Poverty Level, and more than 10% are homeless.
Study Participants
Providers
Primary care medical providers (including internists, family doctors, and family nurse practitioners) from 12 sites at CHCI and four sites at El Rio were eligible to take part in the study.
ECHO Faculty
ECHO sessions were led by a team of pain specialists from the Integrative Pain Center of Arizona (IPCA) in Tucson, Arizona. Faculty included specialists in Anesthesiology/Pain Medicine, Behavioral Health, Occupational Medicine, Addiction Medicine, Chinese Medicine/Acupuncture, and Primary Care. ECHO sessions were coordinated and managed by dedicated staff from CHCI’s Weitzman Institute (WI), a research and innovation center located in Middletown, Connecticut.
Patients
A validated algorithm that included data elements from the electronic health record (EHR) including diagnosis codes, pain scores, and medication prescribing information [26] was used to identify a cohort of patients with chronic pain cared for by each provider in the study during the one-year period prior to the intervention and during the one-year period following the intervention.
Recruitment
Participants were recruited using a convenience sampling approach. Primary care medical providers were informed about the study during in-person and videoconference presentation at existing staff meetings and grand rounds presentations at the participating organizations. One interested provider from each participating site was chosen to participate in the intervention. At sites where more than one primary care medical provider was interested, the participant was chosen based on 1) ability to attend Project ECHO Pain sessions, 2) chronic pain patient panel size, 3) ability to find an appropriate matched control provider, and 4) input from the on-site medical or behavioral health director. All primary care providers not chosen to participate in the intervention were asked to serve in a control group. In total, 12 primary care medical providers (PCPs) were recruited for the intervention group, and 11 PCPs were recruited for the control group.
Intervention
“Usual care” for patients with pain at both participating organizations left decisions about treatment and referrals to the discretion of the treating PCP. While each organization had a standard policy about pain care with recommendations for use of opioid agreements and urine toxicology screening, there were no strict guidelines or restrictions on medication selection or dosing. All PCPs in the intervention group joined weekly two-hour Project ECHO Pain videoconference sessions between January and December of 2013. Sessions were scheduled during the clinical workday, and providers were allocated dedicated time to participate fully for the entirety of each session. Participants joined the sessions from a teleconferencing device, a personal computer, a tablet, or a smartphone. Participating clinicians were asked each week to submit cases for presentation at upcoming sessions. PCPs chose cases from their patient panel and entered the consult question along with relevant aspects of the history on a standardized case presentation form. The forms were de-identified, reviewed by the ECHO coordinator, and forwarded to the faculty team. The faculty reviewed submitted cases in advance of the ECHO session to be prepared to lead a discussion on each case. During each session, PCPs briefly presented their cases, along with their behavioral health colleague, when appropriate. Three to four patient cases were scheduled for discussion each week. In addition to case presentations, a 20- to 30-minute didactic presentation was given each session by one of the ECHO faculty. The didactic curriculum and case presentation discussions emphasized a multidisciplinary, team-based model based on current guidelines and a core set of best practices for pain care delivery in primary care [27]. All participants were given access to a secure project website, case submission and presentation forms, and a project database and data collection system. Participants who were unable to attend a live Project ECHO Pain session could view recordings of each case and didactic presentation on the secure project website.
Data Sources and Data Collection
Surveys
PCPs’ pain care knowledge was assessed using a validated tool, the KnowPain-50 (KP50) [28]. The KP50 measures knowledge in the following domains: initial pain assessment, defining treatment goals and expectations, development of a treatment plan, implementation of a treatment plan, reassessment and management, and management of environmental issues. The KP50 contains multiple choice questions as well as questions scored on a Likert scale, with an overall maximum possible score of 250. In addition, to assess PCPs’ views and attitudes about pain care, we used a set of 11 questions taken from a survey previously developed by and utilized in the Veterans Health Administration (VHA) [18]. All participants completed the surveys online using SurveyMonkey.
Electronic Records Data
To assess the impact of Project ECHO on providers’ treatment of pain overall, we queried the electronic health record and collected treatment data for all patients with chronic pain who received care from primary care providers in the intervention and the control groups for the one-year period prior to starting ECHO (January through December 2012) and for the one-year period following the intervention (January through December 2014). Data included patient demographics, medications prescribed, and referrals to behavioral health and other pain-related specialists.
Focus Groups
A focus group was conducted with all PCPs participating in Project ECHO Pain in June 2013 to assess their opinions of Project ECHO Pain sessions and the applicability of Pain ECHO content to their practice. During this focus group, the faculty team was also invited to speak about their experiences leading Project ECHO Pain sessions and interacting with participating providers via videoconference. A follow-up focus group was held in December 2013 with Project ECHO participants and the faculty team to assess their opinions of the completed intervention and their suggestions for improving Project ECHO Pain sessions for future cohorts of providers. Each focus group was 30 minutes in duration and was moderated by a member of the research team who was not a member of the Project ECHO Pain faculty. The focus group sessions were recorded and transcribed, and qualitative data were evaluated with thematic content analysis.
Statistical Analysis
Descriptive statistics were used to analyze the data. For comparisons, we used the χ2 test to compare proportions and the Student’s t test to compare means using SPSS. Analyses of changes and differences in changes between conditions were done with paired t tests, multiple-group models of changes in Mplus for KP50 (which yields full sample estimates, i.e., including for the missing post-intervention values), and Stata’s xtmixed with clustering option for patient outcomes. All tests were two-sided and considered significant at a P value of less than 0.05.
Results
A total of 48 Project ECHO Pain sessions were held, during which 107 unique patients with chronic pain and complex medical and behavioral health comorbidities were presented. Participating primary care medical and behavioral health providers attended an average of 82.4% of the sessions offered (mean = 39.6 sessions, min = 13, max = 48) during the year. PCPs attended an average of 78.1% of the sessions offered (mean = 37.5 sessions, min = 13, max = 48), while behavioral health providers attended an average of 86.2% of the sessions offered (mean = 41.4 sessions, min = 14, max = 48). ECHO session attendance remained consistent throughout the study period. All participant attrition in study participation can be attributed to providers leaving their positions at participating health centers.
PCP Pain Knowledge
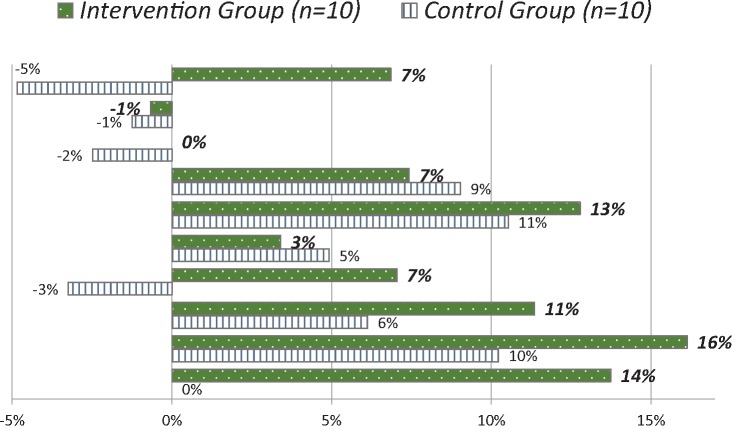
Pre-intervention assessment of knowledge using the KP50 knowledge survey revealed a nearly statistically higher mean baseline score among intervention group providers than control providers (P = 0.060). Results from pre- and postintervention administration of the KP50 knowledge survey to PCPs who participated in Project ECHO Pain sessions are shown in Figure 1. Findings demonstrate a statistically significant increase in pain care knowledge in intervention providers (N = 10), from baseline (mean = 160.20) to postintervention (mean = 172.84; P < 0.001). The intervention group increased by 12.64 points (7.9%) on the KP50 pre- vs post-, compared with a 4.60-point increase (2.9%, P = 0.119) in the control group. (The total possible KP50 score is 250 points.)
Figure 1.
Percent change in KP50 scores: Control and intervention primary care providers (PCPs). This figure shows the percent change in knowledge scores pre- and post-intervention for providers in the intervention and the control. Percent change was calculated using the formula ((X2-X1)/X1) *100, where X1 is the baseline score and X2 is the follow-up score. Note: Individual PCP changes in KP-50 displayed; PCPs ordered in both groups from largest decrease to largest increase.
PCP Attitudes and Beliefs Regarding Pain
There were no significant differences at baseline between intervention and control group providers in response to a range of questions about the attitudes, beliefs, and approach to managing patients with opioids. However, following the intervention, PCPs in the intervention group were more likely to affirm that they used opioid agreements (5.43 vs 5.13, with scale 6 = strongly agree to 1 = strongly disagree; P = 0.050). They expressed less concern about their patients becoming addicted to opioids (average response of 2.87 [post] vs 3.52 [pre] on a six-point Likert scale of agreement with the statement “Patients I treat become addicted to opioids,” with a scale of 6 = strongly agree to 1 = strongly disagree; P = 0.006).
Impact on Pain Treatment
Table 1 shows practice data for all patients with chronic pain cared for by providers in the study in the year prior to and in the year following the intervention. Patients with pain were more likely to be female. Using a difference between changes approach, we found that PCPs in the intervention group had a statistically significantly greater reduction in the percentage of patients with chronic pain treated with an opioid medication compared with providers in the control group (from 56.2% to 50.5% compared with 50.1% to 50.3%; P = 0.002). In addition, the average number of opioid prescriptions written per patient with pain increased significantly less for providers in the intervention compared with their colleagues in the control group (from 4.89 to 5.00 compared with 3.05 to 3.97; P = 0.001) Furthermore, in the year following ECHO, providers in the intervention had a greater increase in referrals to behavioral health than their colleagues in the control group. Referrals to surgical subspecialties (orthopedic and neurosurgery) decreased in the intervention group and increased in the control group, while referrals to physical therapy increased in the intervention group and decreased in the control group. These differences in referrals were all statistically significant. No statistically significant change was observed in referrals to other specialties, such as addiction medicine, chiropractic, and acupuncture.
Table 1.
Patient demographics and providers’ baseline and follow-up descriptives by condition
| Control |
Intervention |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline: 2012 |
Follow up: 2014 |
Baseline: 2012 |
Follow up: 2014 |
|||||||||
| No. | % | No. | % | No. | % | No. | % | |||||
| Patient level | Total patients | 2,020 | 1,695 | 1,586 | 1,485 | |||||||
| Patients/provider, M/SD | 202/93 | 170/86 | 159/97 | 149/73 | ||||||||
| Female | 1,261 | 62.5% | 1041 | 62.0% | 960 | 60.5% | 910 | 62.8% | ||||
| Race | White | 831 | 41.5% | 695 | 42.0% | 671 | 42.6% | 797 | 56.0% | |||
| Hispanic | 849 | 42.4% | 745 | 45.0% | 438 | 27.8% | 388 | 27.2% | ||||
| Black | 182 | 9.1% | 160 | 9.7% | 169 | 10.7% | 174 | 12.1% | ||||
| Native American | 111 | 5.5% | 30 | 1.8% | 265 | 16.8% | 30 | 2.1% | ||||
| Other | 31 | 1.5% | 25 | 1.5% | 33 | 2.1% | 35 | 2.5% | ||||
| Age, M (SE) | 49.5 | (1.41) | 51.6 | (1.42) | 47.9 | (1.42) | 50.7 | (1.42) | ||||
| Provider level | pΔ | pΔ | pd(Δ) | |||||||||
| Visits/y, M (SE) | 7.21 | (0.55) | 7.02 | (0.55) | 0.266 | 8.46 | (0.56) | 8.38 | (0.56) | 0.726 | 0.718 | |
| Opioids | Any opioid Rx, M (SE) | 50.1% | (6.1%) | 50.3% | (6.2%) | 0.907 | 56.2% | (6.2%) | 50.5% | (6.2%) | 0.002 | 0.017 |
| Number of Rx, M (SE) | 3.05 | (0.80) | 3.97 | (0.81) | <0.001 | 4.89 | (0.81) | 5.00 | (0.81) | 0.701 | 0.021 | |
| Mental health | Pts w/BH visit on site | 24.1% | (4.2%) | 25.5% | (4.3%) | 0.348 | 26.6% | (4.3%) | 30.7% | (4.3%) | 0.017 | <0.001 |
| Pain referrals | Physical therapy | 35.3% | (6.0%) | 25.3% | (6.0%) | <0.001 | 20.0% | (6.0%) | 22.2% | (6.0%) | 0.104 | <0.001 |
| Pain management | 6.8% | (2.1%) | 12.1% | (2.2%) | <0.001 | 9.4% | (2.2%) | 9.5% | (2.2%) | 0.930 | <0.001 | |
| Physical med and rehab | 5.7% | (1.5%) | 3.1% | (1.5%) | <0.001 | 7.8% | (1.5%) | 2.0% | (1.5%) | <0.001 | 0.004 | |
| Surgery (neuro or ortho) | 23.5% | (3.8%) | 25.3% | (3.8%) | 0.975 | 26.0% | (3.8%) | 22.1% | (3.8%) | 0.013 | 0.007 | |
| Rheumatology | 3.3% | (0.7%) | 3.3% | (0.7%) | 0.563 | 3.7% | (0.7%) | 3.5% | (0.7%) | 0.794 | 0.868 | |
M (SE) = means and standard errors (from xtmixed models); pΔ are P values for 2012–>2014 changes Δ; pd(Δ) are P values for differences (d) in changes (Δ) by condition (intervention vs control).
Faculty and Provider Focus Groups
Overall, providers suggested that they had acquired knowledge that they were able to apply in their practice. One provider reported that he had “been able to apply what [he] had learned about pain care to all of [his] patients.” Another felt that ECHO made providers “more aware of the psychosocial aspects of pain and the need for a comprehensive approach” and had encouraged them to “re-focus patients” to “engage them in a different way of thinking about pain.” Another provider expressed that the sessions featured “cases just like [participants would] see in [their] practice.” One provider indicated that she “makes a list of things [she has learned about], to follow up on each week,” while another reported that he takes “20 minutes at each staff meeting to discuss what [he has] learned at ECHO, so [his] colleagues can learn from it.”
Providers state that ECHO has given them “a great knowledge base” and has “empowered [them] to know what is in a patient’s best interest.” ECHO has encouraged “structural improvement” in providers’ practice and improvements in provider confidence levels to make treatment changes. A behavioral health provider reports that “ECHO has helped me structure my interventions more” and has “encouraged collaboration between medical and behavioral health providers to treat pain.”
Discussion
Changing clinician behavior is extremely challenging, especially when it relates to the care of a difficult and challenging condition such as chronic pain. This study’s hypothesis was that a more robust, case-based learning intervention conducted by video conference would lead to an increase in knowledge and self-efficacy about guideline-concordant pain care that would translate into actual changes in practice. Results of the study demonstrate a range of changes across the spectrum, including increased adherence to protocols for things such as use of opioid agreements, as well as increased referrals to behavioral health and physical therapy and reduction in prescribing of opioids. Providers in the study, despite working in resource-limited safety net clinics, made significant changes in their overall practice, suggesting that the knowledge gained was being applied not just to cases that were presented and discussed, but across their entire panel of patients. The magnitude of changes observed was modest, even after a year-long intensive immersion in the topic of pain care. However, the findings reflect changes that occurred not just in patients presented at Project ECHO, but across the entire panel of patients with chronic pain cared for by providers in the study. In addition, they occurred in a relatively small, diverse group of providers from two very different locations in markedly resource-limited settings.
New strategies for continuing medical education (CME) are needed to help medical providers manage the rapid increase in available medical knowledge and keep abreast of changes in treatment approaches. More traditional strategies such as lectures and print media are not sufficient [29]. The Institute of Medicine has called for new CME formats and strategies that include increased use of collaborative learning among health professionals and increased utilization of emerging technologies [30]. The Agency for Healthcare Research and Quality (AHRQ) has recommended that CME strategies include the use of “live multimedia” events and interactive techniques that provide clinicians with multiple exposures to important information [29]. Project ECHO is a new approach to CME that meets each of these criteria. Project ECHO uses a repetitive, case-based approach via a live multimedia platform.
Many providers practicing today were trained in an era when opioids were felt to be extremely effective for all types of chronic pain and to pose a low risk for addiction or for side effects. More recent evidence has revealed that opioids pose a significant risk for addiction and that their increased use has resulted in alarming increases in opioid overdose and death [7,8], with little evidence to support their efficacy in treating chronic pain [6]. Clinicians need reliable strategies to “unlearn” much of what they were taught during medical training and to learn new strategies for the safe and effective diagnosis and treatment of patients with pain and opioid addiction. This learning needs to not only address the knowledge deficit, but also to support the application of that knowledge into practice, particularly in primary care, where most patients with pain first seek treatment. The decision to initiate opioid therapy can have far-reaching consequences that must be understood clearly.
One of the most important aspects of Project ECHO is its ability to engage large numbers of providers in varied settings and across large distances. This is a particularly appealing approach for providers in rural and other medically underserved locations where financial limitations are particularly acute and access to specialists is limited. This inexpensive, easy-to-apply videoconference technology was used to create a collaborative learning intervention for this study by joining specialists and primary care providers located on opposite sides of the country.
This study had several strengths. As a pragmatic trial conducted at two FQHC organizations spanning multiple different clinic sites and environments, its results are likely to be highly generalizable. Providers in the study were full-time clinicians in primary care managing diverse panels of patients. Using a novel algorithm, the analysis was able to evaluate changes in practice for all or most patients with chronic pain, not just those presented during ECHO sessions. As a result, the findings demonstrate practice pattern changes that occurred beyond the ECHO referrals.
Several weaknesses limit the conclusions that can be drawn from this study. One of the significant changes noted was the lower number of opioid prescriptions written by providers in the intervention group. This change is promising in light of the rapid increase in prescribing of opioids over the past decade, but the absence of data on the dosage of opioids prescribed limits the conclusions that can be drawn. Furthermore, the changes in knowledge following the intervention were relatively small to account for the change in behaviors of the intervention group compared with the control group. However, the baseline mean provider pain knowledge score of 160.20 in this study was higher than the mean score of 135–138 in groups of community physicians and equal to the scores from academic physicians from a previous study [28]. In fact, the post-intervention mean score of 172.84 was close to the mean score of 177 obtained by pain experts in the same study.
An additional weakness was the potential for bias due to the nonrandom assignment of providers to the intervention group. However, the use of a control group partly mitigates this limitation. Although changes were noted in important process measures, the study did not explore the impact of these changes on actual patient outcomes such as pain, functional status, or quality of life. Further research is needed to assess whether the knowledge gained and applied by participants in interventions leads to lasting improvements in adherence to guidelines and ultimately improves patient outcomes. Lastly, this intervention required a significant commitment from the participating agencies to support consistent attendance of their providers at an average of 82.4% (39.6) of the 48 two-hour sessions offered during the program. This level of time commitment may not be feasible for providers in other practice settings. Studies are underway to test the impact of Project ECHO Pain with a more limited time commitment. Although the cost of hosting and delivering each ECHO session was supported by grant funding, participating primary care practices faced lost revenue due to the need to block out time during the work day for clinicians to participate. Over time, these costs can be significant, leading to the potential for provider attrition and presenting a barrier to further spread. Further research is needed to determine whether these costs are fully or partially offset by any cost savings from reductions in hospitalizations, return visits for unresolved pain or substance abuse issues, emergency room visits, specialty consultations, testing, or imaging.
In summary, this study demonstrated that Project ECHO, a new approach to CME using videoconferencing and case-based learning to train primary care providers in the proper care of patients with chronic pain, resulted in improvement in several pain care process measures, suggesting that knowledge gained in the sessions was being applied in daily practice, resulting in greater use of multimodal approaches, with less reliance on opioids. Project ECHO may provide an important tool to help address the growing prescription opioid crisis in this country and beyond.
Acknowledgments
The authors wish to thank Patricia Healey, MPH, at the Integrative Pain Center of Arizona and Khushbu Khatri, BS, and Ági Erickson, MS, for their contributions to the development and coordination of Project ECHO Pain sessions that occurred during the study period.
References
- 1. Nahin RL. Estimates of pain prevalence and severity in adults: United States, 2012. J Pain 2015;168:769–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. National Institute of Neurological Disorders and Stroke. Back PainFact Sheet. Bethesda, MD: NIH Publication No. 15-5161. National Institutes of Health, Office of Communications and Public Liaison; 2014. [Google Scholar]
- 3. US Department of Health and Human Services. National Pain Strategy: A Comprehensive Population Health-Level Strategy for Pain. Bethesda, MD: National Institutes of Health; 2016. Available at https://iprcc.nih.gov/docs/HHSNational_Pain_Strategy.pdf. (accessed July 25, 2017) [Google Scholar]
- 4. Butchart A, Kerr EA, Heisler M, Piette JD, Krein SL.. Experience and management of chronic pain among patients with other complex chronic conditions. Clin J Pain 2009;254:293.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Michaelson D. Voices of Chronic Pain: A National Study. Baltimore, MD: American Pain Foundation; 2006.
- 6. Martell B, O'Connor P, Kerns R, et al. Systematic review: Opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction. Ann Intern Med 2007;1262:116–27. [DOI] [PubMed] [Google Scholar]
- 7. Chou R, Deyo R, Devine B, et al. The Effectiveness and Risks of Long-Term Opioid Treatment of Chronic Pain. Evidence Reports/Technology Assessments No. 218. Report No. 14-E005-EF. Rockville, MD: Agency for Healthcare Research and Quality; 2014. [DOI] [PubMed] [Google Scholar]
- 8. Von Korff M, Kolodny A, Deyo R, Chou R.. Long-term opioid therapy reconsidered. Ann Intern Med 2011;1555:325–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Center for Health Statistics (US) National Vital Statistics System Mortality File. Number and age-adjusted rates of drug-poisoning deaths involving opioid analgesics and heroin: United States, 1999–2014. 2015. Available at: https://www.cdc.gov/nchs/data/health_policy/AADR_drug_poisoning_involving_OA_Heroin_US_2000-2014.pdf; (accessed July 25, 2017)
- 10. Dowell D, Haegerich TM, Chou R.. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA 2016;31515:1624–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Breuer B, Cruciani R, Portenoy RK.. Pain management by primary care physicians, pain physicians, chiropractors, and acupuncturists: A National Survey. South Med J 2010;1038:738–47. [DOI] [PubMed] [Google Scholar]
- 12. Green C, Wheeler J, Marchant B, LaPorte F, Guerrero E.. Analysis of the physician variable in pain management. Pain Med 2001;24:317–27. [DOI] [PubMed] [Google Scholar]
- 13. Jamison RN, Kerry Anne SB, Elizabeth SN, Ross EL.. Beliefs and attitudes about opioid prescribing and chronic pain management: Survey of primary care providers. J Opioid Manag 2014;106:375–82. [DOI] [PubMed] [Google Scholar]
- 14. Ponte C, Johnson-Tribino J.. Attitudes and knowledge about pain: An assessment of West Virginia family physicians. Fam Med 2005;377:477–80. [PubMed] [Google Scholar]
- 15. Upshur CC, Luckmann RS, Savageau JA.. Primary care provider concerns about management of chronic pain in community clinic populations. J Gen Intern Med 2006;216:652–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Matthias MS, Parpart AL, Nyland KA.. The patient-provider relationship in chronic pain care: Provider's perspective. JAMA 2010;11:1688–97. [DOI] [PubMed] [Google Scholar]
- 17. Barry D, Irwin K, Jones E, et al. Opioids, chronic pain, and addiction in primary care. J Pain 2010;1112:1442–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dobscha S, Corson K, Flores J, Tansill E, Gerrity M.. Veterans affairs primary care clinicians' attitudes toward chronic pain and correlates of opioid prescribing rates. Pain Med 2008;95:564–71. [DOI] [PubMed] [Google Scholar]
- 19. Starrels JL, Fox AD, Kunins HV, Cunningham CO.. They don’t know what they don’t know: Internal medicine residents’ knowledge and confidence in urine drug test interpretation for patients with chronic pain. J Gen Intern Med 2012;2711:1521–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Levy B, Paulozzi L, Mack KA, Jones CM.. Trends in opioid analgesic–prescribing rates by specialty, US, 2007–2012. Am J Prev Med 2015;493:409–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Phelan SM, Van Ryn M, Wall M, Burgess D.. Understanding primary care physicians' treatment of chronic low back pain: The role of physician and practice factors. Pain Med 2009;107:1270–9. [DOI] [PubMed] [Google Scholar]
- 22. Anderson KO, Green CR, Payne R.. Racial and ethnic disparities in pain: Causes and consequences of unequal care. J Pain 2009;1012:1187–204. [DOI] [PubMed] [Google Scholar]
- 23. Green CR, Anderson KO, Baker TA, et al. The unequal burden of pain: Confronting racial and ethnic disparities in pain. Pain Med 2003;43:277–94. [DOI] [PubMed] [Google Scholar]
- 24. Arora S, Kalishman S, Dion D, et al. Partnering urban academic medical centers and rural primary care clinicians to provide complex chronic disease care. Health Aff 2011;306:1176–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Arora S, Thornton K, Murata G, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. NEJM 2011;36423:2199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tian TY, Zlateva I, Anderson DR.. Using electronic health records data to identify patients with chronic pain in a primary care setting. J Am Med Inform Assoc 2013;20(e2):275–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Davis B. Best practices in evaluating and treating pain in primary care: Introduction. Pract Pain Manag 2015. Available at: https://www.practicalpainmanagement.com/treatments/9-best-practices-evaluating-treating-pain-primary-care (accessed July 25, 2017). [Google Scholar]
- 28. Harris JM Jr, Fulginiti JV, Gordon PR, et al. KnowPain-50: A tool for assessing physician pain management education. Pain Med 2008;95:542–54. [DOI] [PubMed] [Google Scholar]
- 29. Marinopoulos SS, Dorman T, Ratanawongsa N, et al. Effectiveness of continuing medical education. Evid Rep Technol Assess (Full Rep) 2007;149149:1–69. [PMC free article] [PubMed] [Google Scholar]
- 30. Warden GL, Mazmanian PE, Leach DC.. Redesigning Continuing Education in the Health Professions. Washington, DC: National Academies Press; 2010. [PubMed] [Google Scholar]