Abstract
Evidence-based treatments (e.g. quitlines) are greatly underutilized by smokers limiting their public health impact. A three-session phone intervention for nonsmoking family members and friends (i.e. support persons) was successful for increasing smoker quitline enrollment. To enhance the intervention’s potential translatability, in this study, we delivered treatment for the non-smoker within ongoing quitline services and compared the efficacy of the three-call intervention to a streamlined version (one call). A total of 704 adult non-smokers (85% female, 95% White) wanting to help a smoker quit and recruited statewide in Minnesota participated in this randomized controlled trial with parallel groups. Non-smokers received mailed written materials and were randomly assigned to a control condition (no additional treatment, n = 235), or to a one- (n = 233) or three-call (n = 236) intervention delivered by quitline coaches. The main outcome was smoker quitline enrollment through 7-month follow-up. Smoker quitline enrollment was similar for those linked to non-smokers in the one- and three-call interventions (14.6% [34/233] and 14.8% [35/236]), and higher than for smokers linked to control participants (6.4% [15/235]), P = 0.006. Just one quitline coaching call delivered to non-smokers increased treatment enrollment among smokers. The reach of quitlines could be enhanced by targeting the social support network of smokers.
Introduction
In 2014, the prevalence of smoking in the United States was 16.8% [1]. About half of smokers attempt to quit each year [2], but most do not utilize evidence-based interventions that could double or triple their success at quitting [3–5]. For example, the use of quitlines improves smoking cessation [6, 7] but these are used by only 1% of smokers in the population [8]. Therefore, promoting use of evidence-based cessation treatments is an important public health priority [5, 8].
A promising approach for increasing the reach of interventions is to target non-smokers within the social support network of smokers [9, 10]. From observational studies, supportive interpersonal relationships [6] and social networks [11] are correlated with quitting success. However, strategies that use buddy systems or involve family members or friends (i.e. support persons) with smokers seeking cessation treatment have not been uniformly effective [12, 13]. Thus, a key challenge for the field is where and how to leverage social support in the cessation process [12, 14].
Most research has focused on cessation—harnessing support from family members and friends to help smokers who are already in treatment programs and have high levels of quitting readiness [12, 13, 15]. Most smokers, however, are not ready to quit [16], and thus supportive strategies that reach non-treatment seeking smokers may have greater reach and utility. For example, recent studies suggest that targeting community peers and family support networks is effective for increasing quitting among non-treatment seeking smokers [17, 18]. Also, the CDC Tips from Former Smokers national campaign was associated with increases in the proportion of non-smokers who talked to smokers about quitting and recommended treatment [19]. In a prior randomized efficacy trial [20], we evaluated if non-smokers could be effective in prompting a smoker to utilize a quitline. Non-smokers (n = 534) received written materials only (control condition) or written materials plus three counseling calls delivered by research staff. Counselors used behavioral change techniques with a motivational interviewing style to teach participants supportive skills for prompting their smoker’s use of a quitline. Quitline enrollment was significantly greater for smokers linked to participants who received the intervention (16.1%) than for control participants (8.6%); adjusted OR = 2.09, P = 0.008.
To enhance the potential translatability of the intervention, in this study, we conducted a randomized clinical trial within the ongoing services of a quitline, transitioning the non-smoker intervention delivery from research staff to existing quitline coaches. With the ultimate goal of reducing costs and enhancing dissemination, we examined if a streamlined version (one call) was as effective as the three-call intervention; both were compared to a control condition. We hypothesized a dose response relationship between number of phone sessions (0, 1, 3) provided to non-smoking support persons and smoker quitline enrollment. This work is novel because it is the first to evaluate a quitline intervention for non-smokers to engage smokers in cessation treatment. In contrast, prior studies evaluated strategies using health care professionals to engage unmotivated smokers in treatment [21, 22].
Materials and methods
This RCT was conducted in Minnesota, and approved by the Mayo Clinic and National Jewish Health Institutional Review Boards, and registered with clinicaltrials.gov (NCT01331226). All participants provided written informed consent. Data were collected from 2011 to 2014 and analyzed from 2015 to 2016.
Participants
Sample size calculation
A prior efficacy trial [20] found the rate of smoker quitline enrollment was 8% for the control group versus 16% for the three-call support person intervention. From prior quitline studies targeting smokers [23], we assumed quitline enrollment rates for one coaching call to be intermediate between the control (i.e. 0 calls) and the three-call conditions. Assuming a linear trend in a logistic regression model for the primary outcome of quitline enrollment, an alpha of 0.05, and the above assumptions, the study was designed with 90% power to enroll 340 support persons per group for a total sample of 1020 participants.
Screening, eligibility and enrollment
Non-smokers who were concerned about a smoker and interested in learning how to be helpful were recruited statewide in Minnesota over 25 months (September 2011–2013). The first 93 participants were enrolled utilizing flyers sent to various public health organizations, health fairs, community events, press releases and advertisements in small regional newspapers and radios. The next 611 participants were enrolled through targeted mailings done from a list of potential smoking households in Minnesota, purchased from a direct marketing company. Due to study timeline and budget constraints, we stopped recruitment with 704 subjects enrolled. Recruitment advertisements included a study toll-free number and an e-mail address. Screening was completed by research staff by telephone or e-mail; those eligible were mailed a consent form and baseline questionnaire. No incentives were offered for enrollment in the study.
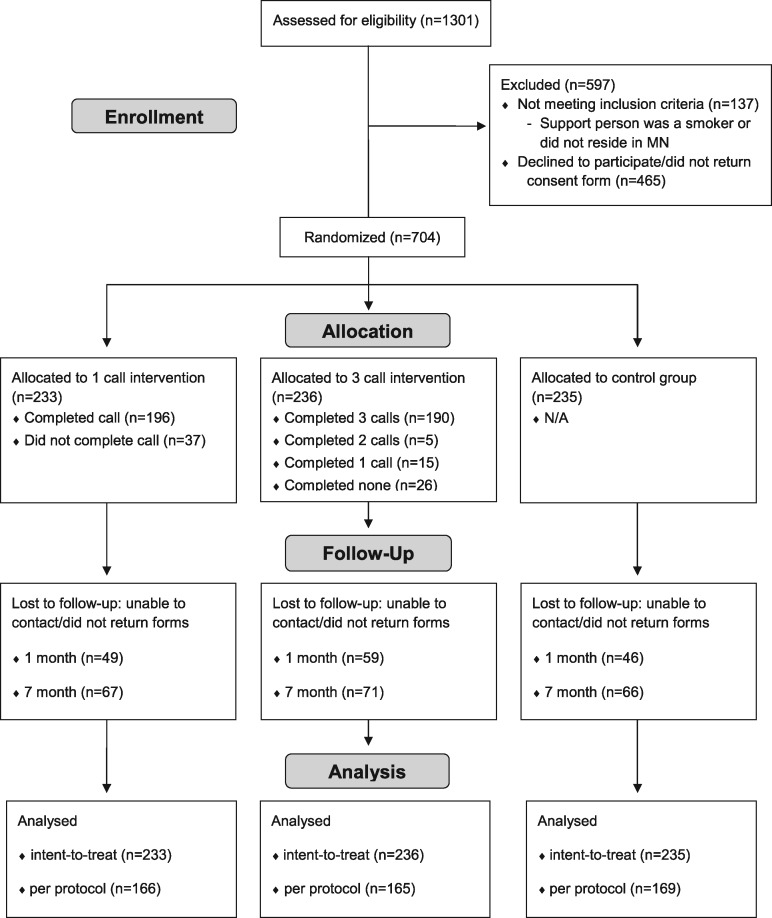
Eligibility criteria were: at least 18 years of age; Minnesota resident; non-smoker (never smoked or no smoking for ≥ 6 months); interested in supporting someone at least 18 years of age who was a Minnesota resident and smoked on average at least one cigarette per day over the previous 7 days, with whom they had any form of contact on at least 3 days/week; access to a working telephone; and provided written informed consent. Individuals were excluded if another participant from the same household had enrolled. A total of 1301 individuals were screened of which 1169 (90%) were eligible; of these 704 (60%) enrolled (Fig. 1 ).
Fig. 1.
Participant flow.
Procedure
In this RCT with parallel groups, participants were stratified according to their gender and if they lived in the same residence as their smoker, and randomly assigned to the one-call intervention group, three-call intervention group or control condition (allocation ratio: 1:1:1). The study stratified participants on gender because some research indicated differences between men and women on provision of and response to social support in smoking cessation [12]. Prior to the trial, the study statistician generated the random allocation sequence based on the stratification variables. Participants completed baseline assessments prior to being informed of their allocation to treatment condition. Participants were mailed a cover letter notifying them of their study group assignment. Enclosed in this mailing were written materials and a colorful silicone wristband with the study logo.
Follow-up data were collected from October 2011 to July 2014. Research staff blinded to treatment condition mailed a questionnaire (i.e. Support Provided Measure [SPM]) at 1 and 7 months to all randomized participants and provided reminders by e-mail or telephone, if needed. Participants received a pen for completing the 1-month follow-up and a key chain for completing the 7-month follow-up. Participants completing each follow-up were entered into a drawing for 1 of 11 Ipod touches that was conducted after all study assessments were completed. A participant’s name was entered after each follow-up was completed, with maximum of two entries.
Support person interventions delivered to the non-smokers
Participants in all three groups received written materials consisting of: (i) the NCI Clearing the Air brochure that they could share with their smoker, and (ii) a tri-fold brochure containing tips on supportive behaviors and statements, information on nicotine dependence including nicotine withdrawal, and a description of services provided by the Helpline. This brochure included a study-specific quitline toll-free number and a reference code linked to the participant’s study ID number that their smoker could use for up to 7 months. This was done to capture the primary endpoint; specifically, to link smokers enrolling in the quitline with the study participants. To ensure consistency in services provided, all smokers who used the study number were eligible to receive quitline services and were not triaged based on insurance status or health plan (the typical procedure for individuals calling). The materials informed participants that their smoker could receive free nicotine replacement therapy and counseling as part of the quitline services. The one- and three-call coaching intervention groups additionally received the Contemplation Ladder as a visual aid for education on readiness to quit.
Control group
Participants assigned to the control group (n = 235) received no additional treatment.
Three-call coaching intervention group
This condition (n = 236) consisted of three proactive telephone sessions delivered by a quitline coach once per week for 3 weeks. The projected duration of each call was 10–20 min. The quitline coaches scheduled and conducted all coaching calls, with appointments available between 7 a.m. and 7 p.m. CST Monday–Friday. Efforts were made to schedule the participant with the same coach for all three sessions. If the participant was unreachable by telephone, a letter was mailed to attempt final contact. The coaches documented call completion and call duration.
The manualized intervention [20] was adapted for implementation within a quitline context (Supplementary Material S1). Coaches used behavior change strategies delivered with a motivational interviewing style [24]. Behavior change techniques used in the intervention manual were independently coded by two authors based on a taxonomy recommended for addiction research [25]; inter-rater agreement 92% (Table I). The conceptual basis for the intervention was Cohen’s theory of social support [10] which postulates that supportive actions promote positive health practices of others by encouraging more effective coping. The types of supportive actions (verbal and non-verbal) taught to participants were correlated with successful smoking cessation [15]. These behaviors were instrumental (e.g. providing material aid), informational (e.g. sharing relevant quitline information), and emotional (e.g. expressing empathy, caring, reassurance) [10]. Supportive behaviors were more likely to predict health outcomes when matched to the demands of the situation (e.g. the smoker’s readiness to quit) [26]. Another important theoretical dimension is the positive–negative nature of supportive behaviors [15]. Increasing positive behaviors (e.g. encouragement) while avoiding negative behaviors (e.g. nagging) is consistently associated with change in smoking behaviors. Further, based on the substance abuse treatment literature [27], another theoretical dimension is the support person’s self-behaviors—those that maintain well-being and morale (e.g. acceptance that the smoker may not seek help). The intervention goal was for support persons to encourage their smoker to call the quitline. Although not assessed, support persons were also taught to recognize any step made by the smoker toward quitting as progress such as expressing interest in what the quitline offers.
Table I.
Behavior change techniques utilized by counselors in support person coaching interventiona
|
|
Behavior change techniques included in one-session coaching intervention manual, based on the taxonomy recommended by Michie et al. [27]. Using this taxonomy, coding was done independently by two authors with inter-rater agreement of 92%.
The session topics were: Session 1: rationale for treatment, role of support person, information about the Helpline (e.g. efficacy, what happens when smokers call), education on readiness to quit; Session 2: supportive behaviors (verbal and non-verbal) based on the smoker’s readiness to quit; and Session 3: supportive behaviors and how to reinforce (shape) progress made by the smoker.
Eighty-one percent (190/236) completed all three sessions (Fig. 1). Call duration in minutes was: (i) 22.0 � 6.3, range 9–52; (ii) 18.0 � 6.7, range 6–58; and (iii) 17.0 � 7.1, range 5–41.
One-call coaching intervention group
This condition (n = 233) consisted of one 15–25-min proactive telephone coaching session initiated by a quitline coach. It was essentially a scaled down version of the same content of the three-call protocol with less time devoted to each topic (Supplementary Material S2). Eighty-four percent (196/233) completed the session (Fig. 1) with a mean � SD duration of 26.0 � 7.8 min (range 12–59).
Coaches
Ten existing QUITPLAN Helpline coaches delivered both interventions. Each had a minimum of a 4-year college degree in a behavioral health or social science-related field. Coaches received 82 h of tobacco-related training as part of their hiring process.
Coaches were provided with ten hours of training on written coaching manuals developed for each intervention and documentation procedures. Training was done using didactics, role plays and simulated treatment sessions. Training emphasized the importance of following the treatment manual, the conceptual framework underlying the intervention, and covered specific strategies for applying the theory to the coaching protocols. Coaches attended quarterly refresher training sessions.
To assess treatment fidelity [28], all sessions were audiotaped and rated using a checklist to compare the number of intended intervention components from the manual that were delivered. Overall, coach adherence was 99% to the one-call intervention and 95% to the three-call intervention manual; thus, the interventions were delivered with fidelity and according to the protocol.
QUITPLAN helpline
At the time of the study, the vendor for the Minnesota QUITPLAN Helpline was National Jewish Health, based in Denver, Colorado. A study-specific toll-free number was set up by the quitline. When a smoker called, the quitline customer service representatives (CSRs) recorded the date and time, their support person’s name, and the study reference code (this was linked to the support person’s study ID number). The CSR explained the services provided by the quitline, and, if interested, enrolled him/her in the program. Once enrolled, the CSR immediately transferred the smoker to a Helpline coach to conduct or set up the first call. For quality assurance, CSRs were trained on-site; test calls were conducted by study staff, along with quarterly refresher trainings conducted by National Jewish Health.
Smokers enrolling into the QUITPLAN Helpline received the same services provided to all Minnesota residents. This consisted of free written materials, up to five telephone coaching sessions (15–20 min each), and the option to receive unlimited text messaging and e-mail support over a 6-month period. Smokers could also receive free nicotine replacement therapy (patches, lozenges or gum) by mail, along with information on other cessation medications that could be prescribed by the smoker’s physician, if appropriate. For smokers not ready to quit, coaches provided interventions to help resolve ambivalence about quitting smoking.
Measures
Non-smoker demographics
A questionnaire documented participant demographics (e.g. age, gender, race/ethnicity) and tobacco use characteristics at baseline.
Smoker information (baseline proxy data)
On the baseline questionnaire, participants completed questions regarding their smoker’s gender, age and race; and were asked to characterize their smoker’s level of readiness to quit using the Contemplation Ladder [29]. The Ladder, adapted for use with proxies [30, 31] (Supplementary Material S3), operates as an 11-point Likert scale from the smoker having no thoughts of quitting to being engaged in action to change one’s smoking behavior. One study [30] found that Contemplation Ladder scores of support people and smokers were moderately correlated (r = .45, P = 0.001), indicating that support people’s reports of smokers’ readiness to quit are reasonably accurate.
Primary outcome: smoker quitline enrollment
The primary endpoint was the proportion of participants’ smokers enrolling in the quitline during the interval from randomization through 7-month follow-up—which is consistent with clinical trials evaluating quitlines [32]. Quitline enrollment was documented by the CSRs. Only calls to the study-specific number were captured. Thus, if a smoker called the general quitline number, the enrollment rates would be underestimated. Once the smoker enrolled, no other data were collected from the quitline for purposes of this study. As a secondary endpoint the proportion of smokers enrolling by 1-month follow-up was also examined.
Secondary outcome: SPM completed by non-smokers
Participants completed the 22-item SPM [33] at baseline and both follow-ups (Supplementary Material S3). The SPM was developed based on our theoretical framework to include instrumental (e.g. ‘engage in smoke-free activity with your smoker’), emotional (e.g. ‘acknowledge that quitting is hard’), and informational (e.g. ‘provide your smoker with information about quitting or medications that can help’) support behaviors and items that apply, irrespective of the smoker’s readiness to quit. Also included are self-behaviors such as modeling how to cope with stress and showing understanding for the changes associated with smoking. Respondents indicated if each behavior occurred (i.e. ‘Yes’ or ‘No’) over the past 2-week period. The SPM demonstrated high internal consistency (alpha = 0.73) in a prior study [20]. For the current baseline sample, Cronbach’s alpha = 0.74. Factor analysis indicated the scale was best characterized by two factors [33]. The first factor (Smoker subscale) comprises 17 items emphasizing behaviors primarily done to help the smoker, e.g. ‘Asked your smoker if they were willing to discuss their smoking’. The second factor (Self subscale) comprises five items emphasizing behaviors the support person could do for him or herself, e.g. ‘Modeled how to cope with stress by relaxing, taking a break, taking a walk or calling a friend’. These factors indicated different functions of support were associated with different behaviors, and thus we examined treatment differences on changes in addition to the total SPM score.
Statistical analysis
To assess the adequacy of the randomization, baseline demographics were compared between treatment groups using the chi-square (exact) test for categorical variables and analysis of variance (Kruskal-Wallis) test for continuous variables. The percentage of participants completing each follow-up (retention) was compared across groups using the chi-square test. Logistic regression was utilized to examine baseline characteristics (Table II) associated with retention at month 7, adjusting for treatment group. The chi-square test was used to examine treatment differences on the proportion of participants’ smokers enrolled in the quitline at 1 and 7 months follow-up, using an intent-to-treat analysis; i.e. all randomized participants (n = 704) were included. Logistic regression was used to compare each treatment group to the control condition. A per protocol analysis was also done including smokers whose support person completed the 7-month follow-up assessment. The SPM score at 1-month follow-up was added to these models to assess support provided as a potential mediator of treatment effects on quitline utilization. Logistic regression was used to examine baseline characteristics associated with smoker enrollment in the quitline at 7 months. The first model included the characteristic and treatment group as predictors of quitline enrollment; the second model additionally included the interaction term to assess if the effect of the characteristic was different across treatment groups. The mean change in SPM score (total and subscale scores) at each follow-up was compared between treatment groups using analysis of covariance (ANCOVA) with the baseline score as a covariate. All analyses used two-sided tests with P ≤ 0.050 used to denote statistical significance.
Table II.
Baseline characteristics by study group (n = 704)a
| Coaching interventions | ||||
|---|---|---|---|---|
| One-call group (n = 233) | Three-call group (n = 236) | Control group (n = 235) | ||
| n (%) or mean � SD | n (%) or mean � SD | n (%) or mean � SD | P-valueb | |
| Support person characteristics | ||||
| Age (years) | 47.8 � 16.4 | 46.7 � 15.5 | 47.7 � 15.8 | |
| Range | 18–89 | 20–83 | 18–87 | 0.78 |
| Female gender | 198 (85) | 199 (84) | 200 (85) | 0.97 |
| White | 221 (95) | 225 (95) | 222 (95) | 0.91 |
| Married | 143 (62) | 159 (68) | 149 (63) | 0.38 |
| Lives with smoker | 110 (47) | 115 (49) | 111 (47) | 0.93 |
| Employed | 167 (73) | 171 (75) | 183 (79) | 0.32 |
| Highest level of education | 0.83 | |||
| Elementary school/junior high | 2 (<1) | 0 (0) | 2 (<1) | |
| High school/GED | 14 (6) | 14 (6) | 17 (7) | |
| Some college/trade school | 70 (30) | 71 (30) | 70 (30) | |
| College degree | 110 (48) | 104 (44) | 109 (46) | |
| Postgraduate degree | 35 (15) | 46 (20) | 37 (16) | |
| Tobacco use | 0.28 | |||
| Never | 73 (31) | 77 (33) | 74 (32) | |
| Experimented | 64 (28) | 82 (35) | 80 (34) | |
| Former smoker | 96 (41) | 77 (33) | 81 (35) | |
| Relationship to smoker | 0.97 | |||
| Spouse | 79 (34) | 85 (36) | 80 (34) | 0.93 |
| Child | 45 (19) | 46 (20) | 40 (17) | |
| Friend | 29 (12) | 25 (11) | 30 (13) | |
| Parent | 22 (9) | 21 (9) | 25 (11) | |
| Sibling | 17 (7) | 16 (7) | 19 (8) | |
| Boyfriend/girlfriend | 18 (8) | 18 (8) | 16 (7) | |
| Coworker | 7 (3) | 10 (4) | 7 (3) | |
| Other | 16 (7) | 14 (6) | 18 (8) | |
| Smoker characteristics (proxy data) | ||||
| Female | 96 (41) | 86 (36) | 93 (40) | 0.56 |
| White | 219 (94) | 219 (93) | 218 (93) | 0.84 |
| Age (years) | 43.2 � 14.1 | 41.8 � 14.1 | 44.6 � 14.4 | 0.10 |
| Range | 19–85 | 18–76 | 18–75 | |
| Contemplation Ladder score | 4.6 � 2.3 | 4.7 � 2.4 | 4.6 � 2.4 | 0.59 |
| 0–3 (low) | 67 (29) | 59 (25) | 68 (29) | |
| 4–6 (medium) | 111 (48) | 107 (46) | 103 (44) | |
| 7–10 (high) | 54 (23) | 67 (29) | 63 (27) | |
GED, general educational development.
Because of rounding, not all percentages total 100.
Chi-square (exact test) for categorical variables and analysis of variance (Kruskal-Wallis) for continuous variables.
Results
Non-smoker baseline characteristics and study retention
Baseline characteristics of non-smokers are presented in Table II. The sample was primarily female (85%) and White (95%). Also provided in Table II are demographic information provided about the smokers; i.e. proxy data. The study groups were comparable on all baseline characteristics.
Figure 1 shows the participant flow with respect to non-smoker recruitment, treatment compliance, and study retention. There were no adverse events associated with the interventions. The study groups were comparable for study retention at 1 and 7 months (P = 0.34 and 0.89, respectively). At 7 months, retention rates were 71% for the one call group, 70% for the three call group, and 72% for the control group. Adjusting for treatment group, older age of the participant (odds ratio [OR] = 1.02, 95% CI: 1.01–1.03, P = 0.001) and being married (OR = 1.66, 95% CI: 1.19–2.32, P = 0.003) were associated with study retention at 7-month follow-up. No other baseline characteristics (see Table II) were significantly associated with study retention. Our inability to contact participants contributed to loss to follow-up; reasons for attrition are unknown.
Support provided measure
After adjusting for the baseline score, the SPM total score at 1-month follow-up was significantly different across treatment groups (P = 0.006) but not at 7-month follow-up (P = 0.42) (Table III). A similar pattern of results was found for the Smoker subscale score, but for the Self subscale the score was not significantly different across study groups at either time point.
Table III.
Support provided measure scores among support persons at baseline and follow-up by study group (n = 704)a
| Coaching interventions | ||||
|---|---|---|---|---|
| One-call group (n = 233) | Three-call group (n = 236) | Control group (n = 235) | ||
| SPM | mean � SD | mean � SD | mean � SD | P-valueb |
| Total scorec | ||||
| Baseline | 11.4 � 4.1 | 11.0 � 4.1 | 11.2 � 3.8 | 0.61 |
| Range | 4–21 | 4–21 | 4–21 | |
| 1-month follow-up | 15.5 � 3.7d | 16.3 � 3.6e | 15.4 � 3.9 | 0.006 |
| Range | 6–22 | 4–22 | 4–22 | |
| 7-month follow-up | 13.6 � 4.7 | 13.7 � 4.8 | 14.0 � 3.9 | 0.42 |
| Range | 4–22 | 4–22 | 6–22 | |
| Smoker sub-scalef | ||||
| Baseline | 8.5 � 3.4 | 8.1 � 3.3 | 8.3 � 3.2 | 0.56 |
| Range | 2–16 | 3–16 | 1–16 | |
| 1-month follow-up | 11.8 � 3.2 | 12.4 � 3.1 | 11.6 � 3.4 | 0.008 |
| Range | 4–17 | 4–17 | 4–17 | |
| 7-month follow-up | 10.1 � 3.9 | 9.9 � 4.0 | 10.2 � 3.5 | 0.60 |
| Range | 3–17 | 4–17 | 4–17 | |
| Self sub-scaleg | ||||
| Baseline | 2.9 � 1.4 | 2.9 � 1.4 | 2.9 � 1.4 | 0.94 |
| Range | 0–5 | 0–5 | 0–5 | |
| 1-month follow-up | 3.7 � 1.2 | 3.9 � 1.1 | 3.7 � 1.2 | 0.27 |
| Range | 0–5 | 0–5 | 0–5 | |
| 7-month follow-up | 3.5 � 1.4 | 3.8 � 1.2 | 3.8 � 1.2 | 0.09 |
| Range | 0–5 | 0–5 | 0–5 | |
The number of participants with completed SPM forms at baseline were 231 for the one-call intervention, 234 for the three-call intervention and 228 for the control group. The respective numbers at 1 month were 181, 177 and 191; and at 7 months follow-up were 166, 164 and 168.
Analysis of variance at baseline and analysis of covariance at 1- and 7-month follow-up adjusting for the baseline support measure.
The SPM total score is calculated by summing the number of items endorsed in the direction of supportive behaviors and can range from 0 to 22.
Pairwise comparisons were significant for the one- versus three-call group (P = 0.012) but not for the one-call versus control group (P = 0.65).
Pairwise comparisons were significant for the three-call versus control group (P = 0.003).
The Smoker subscale comprises 17 items and emphasizes behaviors done primarily to help the smoker. The score is calculated by summing the number of items endorsed in the direction of supportive behaviors and can range from 0 to 17.
The Self subscale comprises five items and emphasizes behaviors the support person can do for himself or herself. The score is calculated by summing the number of items endorsed in the direction of supportive behaviors and can range from 0 to 5.
Main outcome: smoker quitline enrollment
Using an intent-to-treat analysis, the proportion of smokers enrolling in the quitline at 7 months was significantly different across support person study groups (P = 0.006) (Table IV). The proportion of smokers enrolling was 14.6% in the one-call group, 14.8% in the three-call group, and 6.4% in the control group. When the SPM total score at 1-month follow-up was included in the model, the effect of treatment on quitline utilization (P = 0.040) was not significantly reduced (one-call group versus control: OR = 2.33, 95% CI: 1.18–4.59, P = 0.014; three-call group versus control: OR = 2.04, 95% CI: 1.04–4.01, P = 0.039), indicating that treatment effects were not mediated by support provided. Moreover, SPM subscale scores did not mediate treatment effects.
Table IV.
Smoker quitline utilization by support person study group (n = 704)a
| Support person study group | ||||
|---|---|---|---|---|
| Smoker Quitline Enrollment | One-call intervention group (n = 233) n (%) | Three-call intervention group (n = 236) n (%) | Control group (n = 235) n (%) | P-valuea |
| 1-month follow-up (ITT) | 11 (5) | 8 (3) | 7 (3) | 0.58 |
| 7 months follow-up | ||||
| ITT | 34 (15)b | 35 (15)c | 15 (6) | 0.006 |
| PPd | 26 (16)e | 31 (19)f | 13 (8) | 0.013 |
| Median duration of time to call | ||||
| quitline, daysg | 37 | 60 | 42 | |
| Range | 8–210 | 13–210 | 8–210 | |
Note: ITT, intent to treat; analyses based on the smokers of all randomized support persons (n = 704). PP, Per protocol; analyses based on the smokers of support persons completing the 7-month follow-up.
Chi-square test.
From logistic regression: one call group versus control, OR = 2.51, 95% CI: 1.33-4.74, P = 0.005.
From logistic regression: three call group versus control, OR = 2.55, 95% CI: 1.35–4.82, P = 0.004.
The number in each study group was one call group = 166, three call group = 165, and control group = 169.
From logistic regression: one call group versus control, OR = 2.23, 95% CI: 1.10–4.51, P = 0.026.
From logistic regression: three call group versus control, OR = 2.78, 95% CI: 1.40–5.52, P = 0.004.
Of smokers who enrolled in the quitline; calculated from date of support person’s enrollment.
Using a per protocol analysis, the proportion of smokers enrolling in the quitline at 7 months was significantly different across treatment groups (P = 0.013) (Table IV). When the SPM total score at 1 month was included in this model, the effect of treatment on quitline utilization was similar although not statistically significant (P = 0.060) (one call versus control, OR = 2.08, 95%: 0.98–4.38, P = 0.055 versus control; three call versus control OR = 2.33, 95%: 1.13–4.80, P = 0.022 versus control). SPM subscale scores did not mediate treatment effects.
Quitline utilization at 1-month follow-up was not significantly different across study groups (Table IV). Table IV provides median duration for time to call the quitline by treatment condition.
All baseline characteristics of non-smokers (and smokers via proxy data; see Table II) were examined as potential predictors of quitline utilization at 7-month follow-up. No significant associations were detected between quitline utilization and support person: gender, race, marital status, employment, education, tobacco use history, type of relationship to the smoker, residing with the smoker or SPM score; or smoker: gender, age or race. Adjusting for treatment group, older age of the non-smoker (OR = 1.02, 95% CI: 1.01–1.04, P = 0.009) and higher Contemplation Ladder score of the smoker (OR = 1.19, 95% CI: 1.07–1.32, P = 0.001) were associated with increased likelihood of smoker enrollment in the quitline. To illustrate the later finding, the rate of quitline enrollment was 7% (13/194) for smokers with low levels of readiness to quit, 12% (40/321) for those with medium levels, and 16% (30/184) for those with high readiness. However, there was no interaction effect detected between Contemplation Ladder score and treatment group on quitline enrollment (P = 0.71). Thus, the effect of treatment group on quitline enrollment was not dependent on the smokers’ baseline readiness to quit; i.e. no moderation effect.
Discussion
This RCT found that coaching interventions for non-smokers can be successfully conducted within a ‘real world’ quitline setting, and just one call is effective for increasing quitline enrollment among smokers. The information and skills learned within one brief session may be sufficient for non-smokers, without the added contact time and counselor support being necessary (unlike clinical trials enrolling smokers where providing more treatment corresponds to better outcomes) [6]. Previous studies of social support interventions have not been uniformly effective [12, 13] but most were conducted among smokers already engaged in treatment. Because the majority of smokers are not ready to quit in the next month [15, 34, 35], targeting the social support network is a promising avenue to reach smokers on a population level. Encouragingly, we observed the treatment effect on quitline enrollment was consistent across smoker levels of quitting readiness.
One of the strengths of this translational work is that the effectiveness of the three-call intervention on smoker quitline enrollment (15%) was similar to the original efficacy trial in which the coaching was delivered by research staff (16%) [20]. Other strengths are the use of an experimental design [36]; verified quitline utilization by smokers [37]; use of theoretically-based, well-specified manuals to enhance replicability of the intervention method [25]; treatments delivered by real-world quitline coaches with high fidelity; inclusion of quality control procedures; and very good rates of participant treatment completion and follow-up retention.
This study does have limitations. We did not assess the potential downstream effect of this approach on quitting or the level of engagement in the quitline program after the smoker enrolled—such as use of pharmacotherapy. The interventions were designed to motivate smoker calls to the quitline. This outcome, consistent with a phase-based framework recommended for advancing the science of tobacco treatment [38], was achieved. Nonetheless, it is possible that smokers enrolling in a quitline, as prompted by a support person, may be a select group compared to smokers initiating cessation treatment on their own with very different quitting outcomes. Another limitation is that all smoker information at baseline was from proxy reports with unknown reliability. Thus, as the next step, we plan to attempt to engage and incentivize smokers to complete assessments to measure the potential impact of this approach on quitting and to directly assess smoker characteristics such as heaviness of smoking.
Another limitation was that it is unclear how the interventions worked because support provided by the non-smoker as measured by the SPM did not appear to account for the treatment effects on quitline utilization. Thus, alternative constructs of social support could be considered in future research to better understand the mechanisms of the intervention effect such as, social control and autonomy support provided [12, 39]. Potential theory-based mechanisms that could also be explored among the smokers including support received and enhanced coping [12, 39].
Some sample characteristics limited generalizability and potential impact of the intervention, i.e. 85% female, 95% White, and highly educated non-smokers. Finally, the sample size recruited was less than originally targeted. However, the observed treatment differences were statistically significant even with a smaller sample size.
Despite these limitations, the results provide evidence for tobacco cessation quitlines—a treatment available in all 50 states via 1-800-Quit-Now. The North American Quitline Consortium [8] reported that about 5% of ∼500 000 annual quitline callers (25 000) were individuals calling on behalf of a loved one who smokes; these calls are unsolicited. Findings from this study provide real-world guidance for the first time to quitlines on the types of coaching that may aid non-smokers in linking their family members and friends to quitline services. Quitlines could elect to advertise the availability of such coaching targeting non-smokers though a ‘Help a Loved One Quit’ campaign or other promotional activities [19]. These marketing efforts could leverage the enormous potential of online social networks [14, 40–42]. The cost to the Minnesota quitline to implement this one-call intervention (not recruitment) was $60, including the coaching session and 10–12 min of subsequent documentation. A standard quitline call was $38; however, the one-call support person intervention was $60 due to the extended length of the call, and the cost for the three-call intervention was $135 (same rationale). The cost is very reasonable in light of the finding that one call was associated with essentially a doubling of the rate of smoker enrollment in the quitline beyond written materials—currently the ‘standard of care’ provided by most state quitlines [43]. Although on average the one- and three-call interventions were not time intensive it is important to note the wide range of session durations and thus implementing the interventions on a wide scale basis would require greater standardization of intervention delivery among quitline coaches.
An important next step for this line of research is to understand how the interventions apply to underserved populations as cultural and family differences may influence how support is received (acceptability) and effectiveness [44–47]. The emerging use of mobile technologies such as text messaging in low-income populations offers novel opportunities to deliver the support person interventions [48].
Conclusions
This real-world quitline study found that coaching interventions targeting non-smokers can result in significant increases in the rates that a smoker enrolls in a quitline. Just one session yielded results essentially equal to having three calls. These results provide early guidance for quitlines that want to expand their services to offer an efficient (one call) intervention to help non-smokers link their family members and friends to quitline services. Our two studies—one an efficacy trial, the other an effectiveness trial—showed brief coaching delivered to non-smokers significantly increased quitline enrollment among smokers and would seem to constitute a basis for broad adoption of such a program by quitlines.
Supplementary data
Supplementary data are available at HEAL online.
Supplementary Material
Acknowledgements
We appreciate the contributions of Christina Smith, Christine Hughes, and Marcelo Hanza at Mayo Clinic, Rochester, MN to implementation of the study. We are grateful for the contributions of the Minnesota QUITPLAN Helpline coaches and customer service representatives to the conduct of this study. In addition, we appreciate the assistance of Dr Michael Fiore and Dr Bruce Christiansen at the University of Wisconsin, Madison, for their advice on the study design and review of an earlier draft of this article. The research presented in this article is that of the authors and does not reflect the official policy of ClearWay Minnesota. Authors R.B. and J.S. (ClearWay Minnesota) contributed to the study design, study protocol, article development and final approval of the submitted manuscript but had no role in data collection, data entry or the statistical analyses. The study was approved by the Mayo Clinic Institutional Review Board, No. 11-00179600 and the National Jewish Health Institutional Review Board, No. HS-2610. The trial was registered with www.clinicaltrials.gov: NCT01331226. The full trial protocol can be accessed by contacting the corresponding author CAP.
Funding
This work was supported by the ClearWay MinnesotaSM research program (grant number RC 2011-0008).
Conflict of interest statement
None declared.
References
- 1. Jamal A, Homa DM, O’Connor E. et al. Current cigarette smoking among adults - United States, 2005-2014. MMWR Morb Mortal Wkly Rep 2015; 64:1233–40. [DOI] [PubMed] [Google Scholar]
- 2. U.S. Department of Health and Human Services. The Health Consequences of Smoking: 50 Years of Progress. A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2014. Printed with corrections, January 2014. Available at: http://www.surgeongeneral.gov/library/reports/50-years-of-progress/full-report.pdf. Accessed: 1 July 2016.
- 3. Cokkinides VE, Ward E, Jemal A. et al. Under-use of smoking-cessation treatments: results from the National Health Interview Survey, 2000. Am J Prev Med 2005; 28:119–22. [DOI] [PubMed] [Google Scholar]
- 4. Shiffman S, Brockwell SE, Pillitteri JL. et al. Use of smoking-cessation treatments in the United States. Am J Prev Med 2008; 34:102–11. [DOI] [PubMed] [Google Scholar]
- 5. Zhu S, Melcer T, Sun J. et al. Smoking cessation with and without assistance: a population-based analysis. Am J Prev Med 2000; 18:305–11. [DOI] [PubMed] [Google Scholar]
- 6. Fiore MC, Ja�n CR, Baker TB. et al. Treating Tobacco Use and Dependence: 2008 Update. Quick Reference Guide for Clinicians. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service, 2009. [Google Scholar]
- 7. Stead LF, Hartmann-Boyce J, Perera R. et al. Telephone counselling for smoking cessation. Cochrane Database Syst Rev 2013; 8:CD002850.. [DOI] [PubMed] [Google Scholar]
- 8. North American Quitline Consortium (NACQ). 2014. Results from the 2103 NACQ Survey of Quitlines. Available at: http://www.naquitline.org/. Accessed: 1 June 2016.
- 9. Martire LM, Franks MM.. The role of social networks in adult health: introduction to the special issue. Health Psychol 2014; 33:501–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cohen S. Social relationships and health. Am Psychol 2004; 59:676–84. [DOI] [PubMed] [Google Scholar]
- 11. Christakis NA, Fowler JH.. The collective dynamics of smoking in a large social network. N Engl J Med 2008; 358:2249–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Westmaas JL, Bontemps-Jones J, Bauer JE.. Social support in smoking cessation: reconciling theory and evidence. Nicotine Tob Res 2010; 12:695–707. [DOI] [PubMed] [Google Scholar]
- 13. Park EW, Tudiver FG, Campbell T.. Enhancing partner support to improve smoking cessation. Cochrane Database Syst Rev 2012; 7:CD002928. [DOI] [PubMed] [Google Scholar]
- 14. Cobb NK, Graham AL, Byron MJ. et al. Online social networks and smoking cessation: a scientific research agenda. J Med Internet Res 2011; 13:e119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cohen S, Lichtenstein E.. Partner behaviors that support quitting smoking. J Consult Clin Psychol 1990; 58:304–9. [DOI] [PubMed] [Google Scholar]
- 16. Burris JL, Wahlquist AE, Carpenter MJ.. Characteristics of cigarette smokers who want to quit now versus quit later. Addict Behav 2013; 38:2257–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. G�mez-Pardo E, Fern�ndez-Alvira JM, Vilanova M. et al. A comprehensive lifestyle peer group-based intervention on cardiovascular risk factors: the randomized controlled fifty-fifty program. J Am Coll Cardiol 2016; 67:476–85. [DOI] [PubMed] [Google Scholar]
- 18. Tsoh JY, Burke NJ, Gildengorin G. et al. A social network family-focused intervention to promote smoking cessation in Chinese and Vietnamese American male smokers: a feasibility study. Nicotine Tob Res 2015; 17:1029–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. McAfee T, Davis KC, Alexander RL. et al. Effect of the first federally funded US antismoking national media campaign. Lancet 2013; 382:2003–11. [DOI] [PubMed] [Google Scholar]
- 20. Patten CA, Smith CM, Brockman TA. et al. Support-person promotion of a smoking quitline: randomized, controlled trial. Am J Prev Med 2011; 41:17–23. [DOI] [PubMed] [Google Scholar]
- 21. Sewali B, Thomas JL, Guo H. et al. Enrolling smokers from health systems into quitline services: results of two enrollment strategies. J Smok Cessat 2014; 11:179–87. [Google Scholar]
- 22. Thompson TP, Greaves CJ, Ayres R. et al. Lessons learned from recruiting socioeconomically disadvantaged smokers into a pilot randomized controlled trial to explore the role of Exercise Assisted Reduction then Stop (EARS) smoking. Trials 2015; 16:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zhu SH, Stretch V, Balabanis M. et al. Telephone counseling for smoking cessation: effects of single-session and multiple-session interventions. J Consult Clin Psychol 1996; 64:202–11. [DOI] [PubMed] [Google Scholar]
- 24. Miller WR, Rollnick S.. Motivational Interviewing: Helping People Change. New York: Guilford Press, 2013 [Google Scholar]
- 25. Michie S, Richardson M, Johnston M. et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med 2013; 46:81–95. [DOI] [PubMed] [Google Scholar]
- 26. Uchino BN, Cacioppo JT, Kiecolt-Glaser JK.. The relationship between social support and physiological processes: a review with emphasis on underlying mechanisms and implications for health. Psychol Bull 1996; 119:488–531. [DOI] [PubMed] [Google Scholar]
- 27. Smith JE, Meyers RJ.. Motivating Substance Abusers to Enter Treatment: Working with Family Members. New York: Guilford Press, 2007. [Google Scholar]
- 28. Bellg AJ, Borrelli B, Resnick B. et al. Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH Behavior Change Consortium. Health Psychol 2004; 23:443–51. [DOI] [PubMed] [Google Scholar]
- 29. Biener L, Abrams DB.. The Contemplation Ladder: validation of a measure of readiness to consider smoking cessation. Health Psychol 1991; 10:360–5. [DOI] [PubMed] [Google Scholar]
- 30. Patten CA, Petersen LR, Hughes CA. et al. Feasibility of a telephone based intervention for support persons to help smokers quit: a pilot study. Nicotine Tob Res 2009; 11:427–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zhu SH, Nguyen QB, Cummins S. et al. Non-smokers seeking help for smokers: a preliminary study. Tob Control 2006; 15:107–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. North American Quitline Consortium (NAQC). Guide on Quitlines and Research. Available at: http://c.ymcdn.com/sites/www.naquitline.org/resource/resmgr/research/researchguideapril2013.pdf. Published 2011. Accessed: 1 August 2016.
- 33. Thomas JL, Patten CA, Decker PA. et al. Development and preliminary evaluation of a measure of support provided to a smoker among young adults. Addict Behav 2005; 30:1351–69. [DOI] [PubMed] [Google Scholar]
- 34. Campbell S, Bohanna I, Swinbourne A. et al. Stages of change, smoking behaviour and readiness to quit in a large sample of indigenous Australians living in eight remote north Queensland communities. Int J Environ Res Public Health 2013; 10:1562–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Fu M, Fernandez E, Pascual JA. et al. Stages of change, smoking characteristics, and cotinine concentrations in smokers: setting priorities for smoking cessation. Prev Med 2011; 52:139–45. [DOI] [PubMed] [Google Scholar]
- 36. Carroll KM, Rounsaville BJ.. A vision of the next generation of behavioral therapies research in the addictions. Addiction 2007; 102:850–62. discussion 863–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. McClure JB, Peterson D, Derry H. et al. Exploring the “active ingredients” of an online smoking intervention: a randomized factorial trial. Nicotine Tob Res 2014; 16:1129–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Baker TB, Mermelstein R, Collins LM. et al. New methods for tobacco dependence treatment research. Ann Behav Med 2011; 41:192–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Ochsner S, Knoll N, Stadler G. et al. Interacting effects of receiving social control and social support during smoking cessation. Ann Behav Med 2015; 49:141–6. [DOI] [PubMed] [Google Scholar]
- 40. Maher CA, Lewis LK, Ferrar K. et al. Are health behavior change interventions that use online social networks effective? A systematic review. J Med Internet Res 2014; 16:e40.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Post SD, Taylor SC, Sanders AE. et al. If you build (and moderate it), they will come: the Smokefree Women Facebook page. J Nat Cancer Inst Monogr 2013; 47:206–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Smith AD, Smith AA.. Gender perceptions of smoking and cessation via technology, incentives and virtual communities. Int J Electron Healthc 2011; 6:1–33. [DOI] [PubMed] [Google Scholar]
- 43. North American Quitline Consortium (NAQC) . Results from the 2012 NAQC Annual Survey of Quitlines. 2013. . Available at: http://www.naquitline.org/?page=2012Survey. Accessed: 15 July 2016.
- 44. Alberg AJ, Carpenter MJ.. Enhancing the effectiveness of smoking cessation interventions: a cancer prevention imperative. J Natl Cancer Inst 2012; 104:260–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Passey M, Bonevski B.. The importance of tobacco research focusing on marginalized groups. Addiction 2014; 109:1049–51. [DOI] [PubMed] [Google Scholar]
- 46. Ford P, Clifford A, Gussy K. et al. A systematic review of peer-support programs for smoking cessation in disadvantaged groups. Int J Environ Res Public Health 2013; 10:5507–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Marquez B, Elder JP, Arredondo EM. et al. Social network characteristics associated with health promoting behaviors among Latinos. Health Psychol 2014; 33:544–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Smith A. U.S Smart Phone Use in 2015. Pew Research Statistics. Available at: http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/. First published 2015. Accessed: 26 July 2016
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.