Abstract
Background
The 2014/2015 Ebola outbreak was the most sustained in history. In Guinea, we compared trends in family planning, antenatal care, and institutional deliveries over the period before, during and after the outbreak.
Methods
We carried out an ecological study involving all the health facilities during pre-Ebola (1 March 2013 to 28 February 2014), intra-Ebola (1 March 2014 to 28 February 2015) and post-Ebola (1 March to 31 July 2016) periods in Macenta district.
Results
Utilization of family planning declined from a monthly average of 531 visits during the pre-Ebola period to 242 visits in the peak month of the Ebola outbreak (51% decline) but recovered in the post-Ebola period. From a monthly average of 2053 visits pre-Ebola, antenatal care visits declined by 41% during Ebola and then recovered to only 63% of the pre-Ebola level (recovery gap of 37%, p<0.001). From a monthly average of 1223 deliveries pre-Ebola, institutional deliveries also declined during Ebola and then recovered to only 66% of the pre-Ebola level (p<0.001).
Conclusions
All services assessed were affected by Ebola. Family planning recovered post-Ebola; however, shortfalls were observed in recovery of antenatal care and institutional deliveries. We call for stronger political will, international support and generous funding to change the current state of affairs.
Keywords: Ebola, Guinea, Health service utilization, Health systems, Operational research, Sustainable Development Goals
Introduction
The 2014/2015 Ebola outbreak was the most sustained and severe Ebola outbreak in history, mainly affecting the West African countries (i.e., Guinea, Sierra Leone and Liberia).1 Spreading to 10 countries worldwide with 28 646 cases and 11 323 deaths, WHO declared it a global public health emergency. Guinea reported a total of 3811 cases and 2543 deaths.1,2
Even prior to the Ebola outbreak, Guinea faced weakness in the health system and a severe shortage of qualified health workers.3 With a population of over 11 million inhabitants,4 the country had only one physician and one nurse per 10 000 population, a 25-fold lower ratio than in the USA.3,5 This low ratio of health care providers to population deteriorated further due to the high rate of Ebola infections and deaths among healthcare workers (192 Ebola infections with 86 deaths).1
Multiple studies have revealed the detrimental effect of the outbreak on public health and health systems in West Africa.6–10 There have been reports of declines in antenatal care (ANC) and family planning visits, institutional deliveries, malaria consultations and surgical interventions.7–10 Deterioration in the quality of HIV/AIDS care11 and a four-fold increase in avoidable all-cause mortality have also been reported.12
The effect of the Ebola outbreak was particularly detrimental to reproductive health services, which are fully dependent on functional and accessible health facilities. Since these services often require direct contact with patients and handling their blood or other body fluids, health staff may have detracted from these activities due to fear of contracting Ebola.7,13,14 This is all the more plausible since health worker protection measures were inadequate under the Ebola outbreak.15 Community quarantine measures, distrust and fear of contracting Ebola at health facilities and repurposing all existing resources to Ebola control efforts might have also negatively affected access and utilization of reproductive health services.12,16
Upholding reproductive health activities is critical in an Ebola outbreak. For example, since Ebola infection in pregnancy is associated with high maternal mortality and a nearly 100% incidence of fetal death,17 pregnancy prevention through access to family planning is of paramount importance. Similarly, a situation such as an Ebola outbreak should raise a high need for maternal preventive and emergency care including antenatal and emergency obstetric services such as caesarean sections.18 Failure to do so may affect maternal and newborn outcomes.
The pre-Ebola national health statistics showed that Guinea was experiencing gains in reproductive health, though most of the indicators were still challenging.4 Assessing the possible effect of the Ebola outbreak on reproductive health services in Guinea is therefore key to guiding post-Ebola interventions for reproductive health improvement. A rapid manner of assessing such an effect is to evaluate whether utilization of these services differed before, during and after the outbreak. A PubMed search revealed no study that has assessed the effect of the Ebola outbreak on the three pillars of reproductive health services, i.e., family planning, antenatal care and institutional deliveries.
We concurrently assessed the comprehensive effect of the Ebola outbreak on facility-based reproductive health services in Macenta, the district with the highest Ebola caseload nationwide, through comparing trends in the following services across the time periods of before, during, and after the Ebola outbreak: family planning visits and methods accessed, antenatal care visits, institutional deliveries including caesarean section, and maternal and newborn outcomes of institutional deliveries.
Methods
Study design and setting
We carried out an ecological study comparing routine service data.
General setting
Guinea lies in West Africa and has a population of approximately 11 million inhabitants. The majority of the population is illiterate (67%) and 55% of inhabitants live under the poverty line.19 The country is bordered by Liberia and Sierra Leone, the two other countries most affected by Ebola during the 2014/2015 outbreak. Guinea has one of the highest maternal mortality ratios in the world estimated at 610 per 100 000 live births (compared to a country like Sweden with two per 100 000).19 The total fertility rate is 4.9 and neonatal mortality is 36 per 1000 live births.4 Utilization of modern family planning methods was 5% whilst ANC attendance for three or more visits was estimated to be 57% in 2012.4 Facility-based deliveries represented 40% of all deliveries. About 2% of all institutional deliveries were by caesarian section.4
Specific setting and study site
Macenta district, located in rural southern Guinea, was the study site. It has 14 sub-districts and the urban town of Macenta. Each of the 14 sub-districts has a health center that refers patients to the Macenta district hospital. There are four urban health centers located within the proximity of the district hospital and a total of 68 health posts. The district has a population of about 278 456 inhabitants. The first Ebola case in Macenta was reported on 14 March 2014 and the last case occurred on 25 February 2015.20 The country was declared Ebola free on 29 December 2015 although a few sporadic cases were identified in a different district in 2016.21 Macenta reported a total of 744 (19.6%) of the 3804 cases reported in Guinea with the peak month being September 2014. The case fatality rate in the district was 66%. There were 13 health care workers infected, with 11 deaths.20 Management of Ebola cases was restricted to a dedicated Ebola treatment center.
Reproductive health services in Macenta district
Reproductive health services are provided in accordance with national guidelines.22 These services include family planning, ANC, referral of complicated pregnancies and institutional deliveries. All hospitals, health centers and some health posts have family planning, antenatal care and conduct deliveries. Emergency obstetric care for complicated deliveries (including caesarean sections) is only offered at the district hospital. There is one district ambulance that transports patients from peripheral health centers to the district hospital. Reproductive health management aligns with WHO guidelines.23 According to these guidelines, women are expected to complete three or more ANC visits during pregnancy and at least 90% of all deliveries are expected to be done in health facilities with a minimum of 5% through caesarean section.23
Study population and period
The study population included all 187 094 women of reproductive age (15–45 year old) presenting to all health facilities in Macenta district either for family planning visits, ANC visits, or deliveries over the study period. The study period included a pre-Ebola (1 March 2013 to 28 February 2014), intra-Ebola (1 March 2014 to 28 February 2015) and post-Ebola (1 March 2016 to 31 July 2016) period. The intra Ebola period was as applicable to Macenta district, while the post Ebola period referred to the countrywide situation.
Data collection, validation and analysis
Data captured included number of family planning visits by type of method, number of ANC visits (first visit and third [or more] visits), number of institutional deliveries (and caesarian sections), maternal outcomes (discharged, death, referred) and newborn outcomes (discharged, death, stillbirth). Data were sourced from district health committee reports and registers. Ebola-related data were sourced from Ebola situation reports of the Ministry of Health, Guinea. Statistics on the number of Ebola cases per month in Macenta district were also collected to identify the peak outbreak periods in the district. Data were entered into a dedicated Microsoft Excel database (Microsoft Corp., Redmond, WA, USA) and analyzed using EpiData (version 2.2.2.182, EpiData Association, Odense, Denmark). Data were cross-validated with health facility registers. Data collection covered May to July 2016.
Trends in the monthly numbers of family planning visits, ANC visits and institutional deliveries were described across the pre, intra and post-Ebola periods. The monthly mean numbers and standard deviations (SD) of these services were compared between the pre and post-Ebola periods to identify any recovery gap (i.e., failure in recovering the pre-Ebola level). Proportions of delivery outcomes were also compared between the pre and the intra-Ebola periods, and between the pre and the post-Ebola periods. Comparions between pre and post-Ebola involved 5 months of the same period of the year to take into consideration the possible influence of seasonal differences. Differences in means and in proportions were estimated using the t test and the χ2 test respectively. The level of significance was set at p≤0.05 with a 95% confidence level.
Results
Trends in numbers of family planning visits by type of family planning method
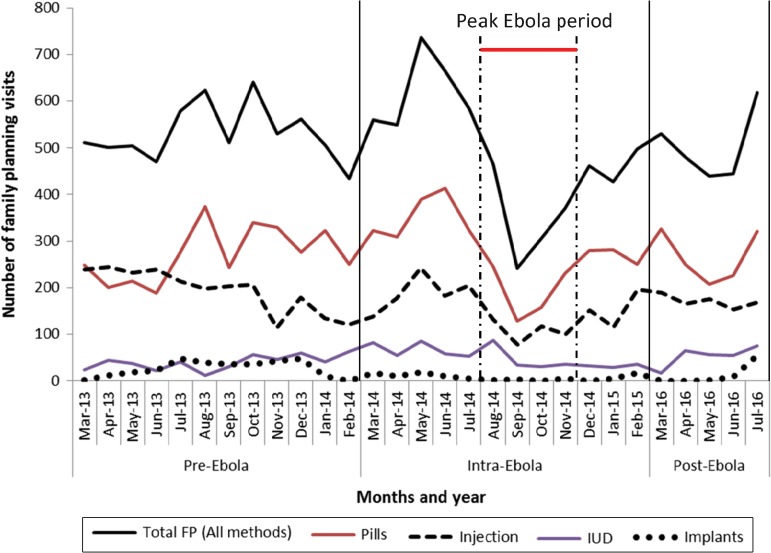
Figure 1 shows the trends in family planning visits during the pre, intra and post-Ebola periods.
Figure 1.
Trend in number of family planning visits by type of family planning method during the pre-Ebola, intra-Ebola and post-Ebola periods, in Macenta district, Guinea (March 2013 to July 2016). FP: Family planning; IUD: Intra uterine device. Data source: Ministry of Health and Sanitation.
From a mean of 531 visits per month in the pre-Ebola period, there was a 47% increase during the first three months of the Ebola outbreak. A decline then ensued to a low of 242 visits in September 2014, the peak month of the Ebola outbreak (a 51% drop from pre-Ebola levels). In the post-Ebola period, the trend recovered back to a monthly mean of 503 visits (SD=66), which is 98% of the pre-Ebola level (513 visits, SD=35, p=0.573). Similar patterns were observed across the different family methods used, except for implant and intrauterine device (IUD), which did not vary.
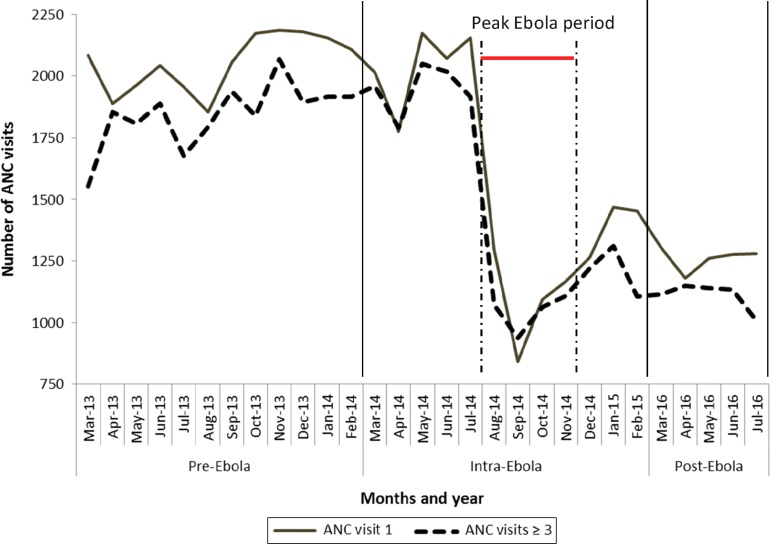
Trends in numbers of antenatal care visits
During the intra-Ebola period, first ANC visits fell steeply from a monthly mean of 2053 pre-Ebola to a low of 842 visits (59% decline) in September 2014 (the peak of the Ebola outbreak, Figure 2). A gradual increase in first ANC visits then followed to a mean of 1260 visits per month in the post-Ebola period - a decrease of 37% compared to pre-Ebola levels. The mean number of first consultations post-Ebola (1260, SD=21) was significantly lower than pre-Ebola (1987, SD=34, p<0.001). The third (or more) ANC visits followed similar trends as the first ANC visits.
Figure 2.
Trend in number of antenatal care visits during the pre-Ebola, intra-Ebola and post-Ebola periods, in Macenta district, Guinea (March 2013 to July 2016). ANC: Antenatal care. Data source: Ministry of Health and Sanitation.
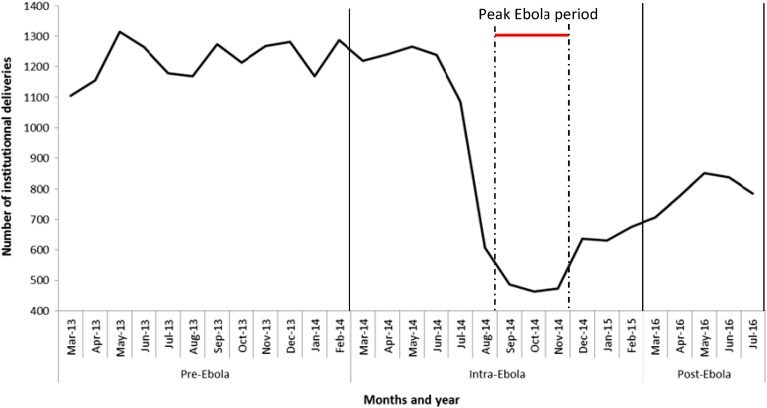
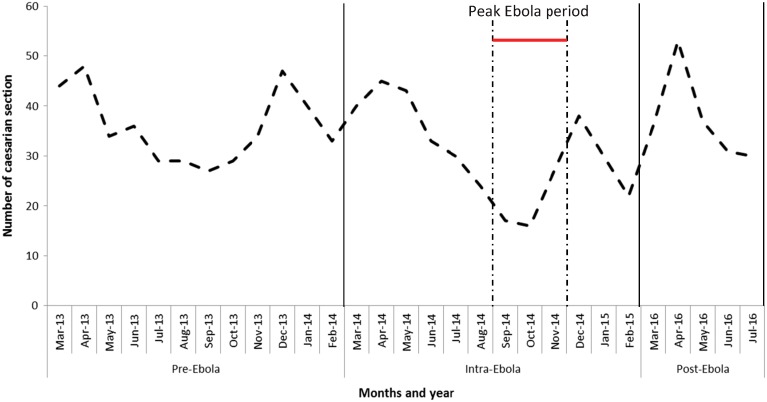
Trend in numbers of institutional deliveries including caesareans
From a monthly average of 1223 deliveries pre-Ebola, there was a 62% decline to 464 deliveries in October 2014 (during peak Ebola period) (Figure 3). This improved to a mean of 792 visits per month in the post-Ebola period. The mean number of institutional deliveries post-Ebola (791, SD=26) was significantly lower than pre-Ebola (1203, SD=38, p<0.001), representing a recovery gap to the pre-Ebola level of 34%. A declining trend in Caesarean sections was also seen during the Ebola outbreak which was most pronounced during the peak of the Ebola outbreak (Figure 4). A full recovery was observed in the post-Ebola monthly mean of caesarean section (37, SD=8) as compared to the pre-Ebola level (38, SD=7, p=0.692).
Figure 3.
Trend in number of institutional deliveries (all types) during the pre-Ebola, intra-Ebola and post-Ebola periods, in Macenta district, Guinea (March 2013 to July 2016). Data source: Ministry of Health and Sanitation.
Figure 4.
Trend in number of caesarian sections during the pre-Ebola, intra-Ebola and post-Ebola periods, in Macenta district, Guinea (March 2013 to July 2016). Data source: Ministry of Health and Sanitation.
Maternal and newborn outcomes of institutional deliveries
Table 1 shows maternal and newborn outcomes across the pre-Ebola, intra-Ebola and post-Ebola periods. Maternal deaths were low and remained similar across the three periods (0.1–0.2%, p>0.05). Adverse newborn outcomes (deaths and stillbirths) were also low across the periods (range 1.1–1.7%) but higher in the post-Ebola period as compared to the pre-Ebola period (p<0.01).
Table 1.
Maternal and new born outcomes during the pre-Ebola, intra-Ebola and post-Ebola periods, in Macenta district, Guinea (March 2013 to July 2016)
| Pre-Ebola (1 March 2016 to 31 July 2016) | Intra-Ebola (1 March 2014 to 28 February 2015) | p | Pre-Ebola (1 March to 31 July 2013) | Post-Ebola (1 March to 31 July 2016) | p | |
|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |||
| Maternal outcomes | ||||||
| Total deliveries | 14674 | 10023 | 6015 | 3958 | ||
| Discharged | 14666 (99.9) | 10016 (99.9) | NS | 6011 (99.9) | 3951 (99.8) | NS |
| Maternal deaths | 8 (0.1) | 7 (0.1) | 4 (0.1) | 7 (0.2) | ||
| Newborn outcomes | ||||||
| Total births | 14807 | 10112 | 6057 | 4005 | ||
| Discharged | 14652 (99) | 9986 (98.8) | NS | 5991 (98.9) | 3936 (98.3) | 0.002 |
| Stillbirths | 153 (1) | 121 (1.2) | 65 (1.1) | 62 (1.5) | ||
| Newborn deaths | 2 (0) | 5 (0) | 1 (0) | 7 (0.2) | ||
NS: not significant.
Discussion
This is one of the first studies from one of the worst Ebola affected countries of West Africa assessing trends in utilization of reproductive health services before, during and after Ebola at health district level. It showed that the three pillars, i.e., family planning, antenatal care, and institutional deliveries, were all drastically affected by the Ebola outbreak with declines in service utilization. Considerable recovery gaps persisted in the post Ebola period for antenatal care and institutional deliveries.
The findings about the recovery gaps are important as they herald possible reversal of hard gains made towards achieving the Millennium Development Goals of reducing maternal and child mortality and improving access to family planning services.24 It also puts Guinea at a relative disadvantage in achieving the newly declared Sustainable Development Goal (SDG) target of achieving universal coverage to sexual and reproductive health services by the year 2030.25 In a country where the pre-Ebola maternal and child mortality rates were among the highest worldwide, these findings really indicate the need for further work to recover previous gains and improve toward achieving the SDG.
The study findings have a number of policy and practice implications. First and interestingly, there was a 47% spike in uptake of family planning methods during the first three months of the Ebola outbreak as compared to the mean pre-Ebola number of family planning visits. Further investigation is needed to explain this finding. The subsequent and drastic decline observed thereafter is a likely reflection of health system failure due to reduced access and utilization of health services for various reasons. In the regions of Conakry and Nzérékoré in Guinea, utilization of family planning services fell to 53% in December 2014 (during EVD outbreak) compared to 75% in October 2013 (before the outbreak).10 A more recent study by Delamou et al. in the Forest region of Guinea has confirmed a significant decline of most maternal and child health indicators and urged for targeted interventions to recover the pre-EVD outbreak trend.26 We do not know the exact reasons behind these fluctuations in service utilization, but community fear of visiting health facilities, repurposing of staff to Ebola related activities, possible stock outs of family planning methods or other factors may be to blame. These aspects merit further investigation. Gradual recovery to almost pre-Ebola levels in the period following the outbreak is reassuring. This is likely explained on the one hand by the positive health seeking behavior further to many interventions on community sensitization about heath services utilization, and the other hand by the regular supply of drugs and devices for family planning became more accessible.
Second, drastic declines in antenatal visits and institutional deliveries were observed during the Ebola outbreak which did not recover in the post-Ebola period. Recovery gaps were 37% for antenatal care visits and 34% for institutional deliveries. These gaps are worrying and may be explained by increased recourse to alternative care providers such as traditional birth attendants for ANC and delivery. It may also be a direct result of lower health care worker availability due to health worker deaths. An effective deployment of the 2950 healthcare workers recruited in August 2016 in the Country, as civil servants27 should be key to addressing this issue. The recovery gaps observed through this study have important public health implications in terms of coverage. For example with a pre-Ebola first visit antenatal coverage in Guinea hovering around 85%,19 a post-Ebola recovery gap of 37% would imply coverage declining to 53%. Similarly, with institutional deliveries being 40%4 prior to the Ebola outbreak, a recovery gap of 34% would have brought this level to 24%. Reversing these losses requires active promotion of antenatal care and institutional deliveries coupled with the needed resources to make this an operational reality. Specific qualitative research is also needed to better understand provider, patient and community perspectives in improving health service utilization so as to guide health systems recovery.
Finally, although maternal deaths and adverse newborn outcomes were rare, these figures are likely to be largely underestimated since we did not capture data on community level deaths. According to Evans et al.,28 maternal mortality could have increased by 38% in Guinea during the Ebola outbreak due to the reduction in health staff associated with the outbreak. Pregnant women arriving at health facilities for delivery during Ebola might have been those with relative survival benefit and those who were more ill might have died in the community. As we move towards the era of the SDGs, accurate registration of births and deaths at the community level through improved vital registration systems is primordial.29
This study has some limitations. We did not have population level denominators and were thus unable to estimate coverage indicators for reproductive health services. Available data on maternal and newborn outcomes were also restricted to health facility level and we have no idea of deaths that might have occurred at community level. However, the study strengths are that it included all health facilities in one of the largest districts; the pre, intra and post Ebola periods allowing comparison of trends; and it adheres to STROBE guidelines on reporting.30 The study also responds to an identified national operational research priority and is thus useful to influence policy and practice.
Conclusions
In conclusion, this study has provided sober insight into the current state of affairs of reproductive health services and particularly the lack of recovery of antenatal care utilization and institutional deliveries after the Ebola outbreak in a rural district of Guinea. It also highlights the need for efforts to maintain vital health services during outbreaks. We call for stronger political will, international support and generous funding to change the current state of affairs.
Acknowledgments
Authors’ contributions: BSC, RZ, AD, ED were involved with conception and design of the protocol which was reviewed by AHB, AEA, SS, JO, and JVG. BSC, AD, AHB, FMG and PB were involved with acquisition of data, and BSC, RZ and ED did the data analysis and all authors were involved with interpretation. The first draft manuscript was written by BSC and RZ and critically reviewed by ED and then by all co-authors. All authors have given approval for the final version to be published and are accountable. All authors read and approved the final version. BSC is guarantor of the paper.
Acknowledgements: This research was conducted through the Structured Operational Research and Training Initiative (SORT IT), a global partnership led by the Special Programme for Research and Training in Tropical Diseases at the World Health Organization (WHO/TDR). The training model is based on a course developed jointly by the International Union Against Tuberculosis and Lung Disease (The Union) and Medécins sans Frontières (MSF). The specific SORT IT program which resulted in this publication was implemented by: Medécins Sans Frontières, Brussels Operational Center, Luxembourg and the Centre for Operational Research, The Union, Paris, France. Mentorship and the coordination/facilitation of these SORT IT workshops were provided through the Centre for Operational Research, The Union, Paris, France; the Operational Research Unit (LuxOR), AMPATH, Eldoret, Kenya; Institute of Tropical Medicine, Antwerp, Belgium; University of Gondar ethiopia; School of Public Health, Johns Hopkins University, Baltimore, Maryland, USA; Luke International, Malawi office; The Centre for International Health, University of Bergen, Norway; and the Northern State Medical University, Arkhangelsh, Russia. We also acknowledge the support from the Macenta Health District office for the good collaboration during data collection.
Funding: The program was funded by the United Kingdom's Department for International Development (DFID), The Union, MSF and La Fondation Veuve Emile Metz-Tesch (Luxembourg). La Fondation Veuve Emile Metz-Tesch supported open access publications costs. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: None declared.
Ethical approval: Ethical approval was obtained from the Ethics Review Board, Conakry, Guinea. The study fulfilled the exemption criteria set by the Ethics Review Board (ERB) of Médecins Sans Frontières (MSF), Geneva, Switzerland, for a-posteriori analyses of routinely collected data and thus did not require MSF ERB review. It was conducted with permission from the MSF Medical Director, Operational Centre Brussels, Belgium. Approval was also received from the Union Ethics Advisory Group (International Union against Tuberculosis and Lung Disease, Paris, France). As this was an aggregate data review study with anonymized data, the issue of informed patient consent did not apply.
References
- 1. WHO Ebola response roadmap - Situation report: February 2016. Geneva: World Health Organization; 2016. http://apps.who.int/ebola/current-situation/ebola-situation-report-3-february-2016 [accessed 20 February 2016].
- 2. Gostin LO, Lucey D, Phelan A.. The Ebola epidemic: a global health emergency. JAMA 2014;312:1095–6. [DOI] [PubMed] [Google Scholar]
- 3. Ministère de la Santé et de l'Hygiène Publique de Guinée Annuaire des statistiques sanitaires nationales 2012. Conakry: Ministère de la Santé et de l'Hygiène Publique; Septembre 2015. [Google Scholar]
- 4. The DHS Program Guinea DHS, 2012. - Final Report (French). http://dhsprogram.com/publications/publication-fr280-dhs-final-reports.cfm [accessed 17 February 2016].
- 5. World Bank Open data: physicians (per 1000 people). Washington, DC: World Bank; 2016. http://data.worldbank.org/indicator/SH.MED.PHYS.ZS [accessed 20 February 2016].
- 6. Delamou A, Delvaux T, Van Belle S et al. Public health impact of the recent Ebola outbreak in West Africa. BMJ Glob Health 2017. http://dx.doi.org/10.1136/bmjgh-2016-000202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Delamou A, Hammonds RM, Caluwaerts S et al. Ebola in Africa: beyond epidemics, reproductive health in crisis. Lancet 2014;384:2105. [DOI] [PubMed] [Google Scholar]
- 8. Plucinski MM, Guilavogui T, Sidikiba S et al. Effect of the Ebola-virus-disease epidemic on malaria case management in Guinea, 2014: a cross-sectional survey of health facilities. Lancet Infect Dis 2015;15:1017–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bolkan HA, Bash-Taqi DA, Samai M et al. Ebola and indirect effects on health service function in Sierra Leone. PLoS Curr 2014;6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Brolin Ribacke KJ, Saulnier DD, Eriksson A et al. Effects of the West Africa Ebola virus disease on health-care utilization - a systematic review. Front Public Health 2016;4:222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Leuenberger D, Hebelamou J, Strahm S et al. Impact of the Ebola epidemic on general and HIV care in Macenta, Forest Guinea, 2014. AIDS 2015;29:1883–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Elston JW, Moosa AJ, Moses F et al. Impact of the Ebola outbreak on health systems and population health in Sierra Leone. J Public Health 2015;27. [DOI] [PubMed] [Google Scholar]
- 13. Dallatomasina S, Crestani R, Sylvester Squire J et al. Ebola outbreak in rural West Africa: epidemiology, clinical features and outcomes. Trop Med Int Health 2015;20:448–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zachariah R, Ortuno N, Hermans V et al. Ebola, fragile health systems and tuberculosis care: a call for pre-emptive action and operational research. Int J Tuberc Lung Dis 2015;19:1271–5. [DOI] [PubMed] [Google Scholar]
- 15. Delamou A, Beavogui AH, Konde MK et al. Ebola: better protection needed for Guinean health-care workers. Lancet 2015;385:503–4. [DOI] [PubMed] [Google Scholar]
- 16. Thiam S, Delamou A, Camara S et al. Challenges in controlling the Ebola outbreak in two prefectures in Guinea: why did communities continue to resist. Pan Afr Med J 2015;22(Suppl 1):22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Black BO, Caluwaerts S, Achar J.. Ebola viral disease and pregnancy. Obstet Med 2015;8:108–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tayler-Smith K, Zachariah R, Manzi M et al. Achieving the millennium development goal of reducing maternal mortality in rural Africa: an experience from Burundi. Trop Med Int Health 2013;18:166–74. [DOI] [PubMed] [Google Scholar]
- 19. WHO World Health Statistics 2015. Geneva: World Health Organization; 2015. http://apps.who.int/iris/bitstream/10665/170250/1/9789240694439_eng.pdf?ua=1 [accessed 17 February 2016].
- 20. Coordination Nationale Ebola en Guinée et OMS Rapport de la Situation Epidémiologique, Maladie à Virus Ebola en Guinée du 28 Février 2018. Sit. Rep. No 319, 2015. Conakry, Guinea. http://guinea-ebov.github.io/sitreps.html [accessed 17 December 2016].
- 21. WHO Latest updates on the Ebola outbreak. March-June 2016.Geneva: World Health Organization; 2016. http://www.who.int/csr/disease/ebola/top-stories-2016/en/ [accessed 19 February 2016].
- 22. WHO WHO guidelines: maternal, reproductive and women's health. Geneva: World Health Organization; 2016. http://www.who.int/publications/guidelines/reproductive_health/en/ [accessed 11 December 2016].
- 23. WHO Monitoring Emergency Obstetric Care: A Handbook. Geneva: World Health Organization; 2009. http://www.who.int/reproductivehealth/publications/monitoring/9789241547734/en/ [accessed 19 December 2016].
- 24. UN. MDG Africa Steering Group Achieving the Millennium Development Goals in Africa. New York: United Nations; 2008. www.who.int/pmnch/events/2008/mdgsteeringgrouprecommendations.pdf [accessed 11 November 2016].
- 25. UN. Sustainable Development Goals. 17 Goals to transform our world. New York: United Nations; 2015. http://www.un.org/sustainabledevelopment/sustainable-development-goals/ [accessed 11 November 2016].
- 26. Delamou A, Ayadi AM, Sidibe S et al. Effect of Ebola virus disease on maternal and child health services in Guinea: a retrospective observational cohort study. Lancet Glob Health 2017. pii: S2214-109X(17)30078-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Guinee Live. Fonction Publique: 2.950 Candidats admis au compte du ministère de la santé. http://guineelive.com/2016/08/26/fonction-publique-2-950-candidats-admis-au-compte-du-ministere-de-la-sante/ [accessed 11 December 2016].
- 28. Evans DK, Goldstein M, Popova A.. The Next Wave of Deaths from Ebola? The Impact of Health Care Worker Mortality Policy Research working paper; no. WPS 7344. Washington, DC: World Bank Group; 2015, p 17. [Google Scholar]
- 29. Zachariah R, Mwagomba B, Misinde D et al. Vital registration in rural Africa: is there a way forward to report on health targets of the Millennium Development Goals. Trans R Soc Trop Med Hyg 2011;105:301–9. [DOI] [PubMed] [Google Scholar]
- 30. von Elm E, Altman DG, Egger M et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007;370:1453–7. [DOI] [PubMed] [Google Scholar]