Abstract
Study Objectives
Epidemiological evidence indicates that both short and long sleep at midlife increase mortality risk, but few studies have examined how change in sleep duration between midlife and later life affects this risk. We examined the association between change in sleep duration and mortality risk.
Methods
The Singapore Chinese Health Study is a prospective cohort of 63257 Chinese in Singapore aged 45–74 years at recruitment (1993–1998). Self-reported sleep duration was collected from 39523 participants who completed both baseline (mean age 54.8 years) and follow-up II (mean age 67.9 years; 2006–2010) interviews, which were on average 12.7 years apart. Mortality data were obtained via linkage with national death registry up to December 31, 2015.
Results
Compared with participants who reported sleeping the recommended duration (7 hr) at both interviews, those with persistently short sleep (≤5 hr) had increased risk of all-cause mortality (hazard ratio [HR] 1.27, 95% confidence interval [CI] 1.06–1.53). Similarly, those with persistently long sleep (≥9 hr) had increased risk of all-cause (HR 1.47, 95% CI 1.24–1.73) and cardiovascular (HR 1.40, 95% CI 1.04–1.89) mortality. The proportion of long-sleepers increased with aging (6%–23.7%). Progression to long sleep from short (HR 1.50, 95% CI 1.24–1.81) or recommended (HR 1.43, 95% CI 1.25–1.64) duration was associated with increased all-cause mortality, especially for cardiovascular mortality. Change in sleep duration was not linked to cancer mortality.
Conclusions
Persistent short or long sleep or increasing sleep duration in late adulthood was associated with increased risk of all-cause mortality, especially from cardiovascular causes.
Keywords: sleep duration, sleep change, mortality
Statement of Significance
Although the association between sleep duration and mortality has widely been examined, sleep patterns can change with advancing age and few studies have examined how a change in sleep duration affects mortality risk. Furthermore, the relation between change in sleep duration and cause of death has not been studied. The present study found that compared with those able to maintain the recommended sleep duration of 7 hr, persistent short sleep was associated with increased risk of all-cause mortality, whereas persistent long sleep or an increase in long sleep duration increased the risk of all-cause and cardiovascular mortality. These findings reiterate the benefit of being able to maintain the recommended duration of sleep through to later life.
Introduction
Sleep duration is associated with mortality as well as risk of cardiovascular, cerebrovascular disease, obesity, diabetes mellitus, cancer, and cognitive decline [1–3]. Many studies have reported a U-shape association between habitual sleep duration and mortality [4–8], and recent meta-analyses have concluded that both short and long sleep durations are associated with increased risk of all-cause mortality [9–11] and cardiovascular mortality [10]. However, in most studies, sleep duration was collected at a single time point, and sleep patterns can change with advancing age [12]. A longitudinal study that examined the change of sleep duration assessed at two different time points reported a U-shape association between sleep duration at both time points and total mortality, the association being stronger at the second time point [13]. Although both increased and decreased sleep durations over time were associated with increased risk of all-cause mortality [13], a finer grained account of how much sleep duration changed was not available. Another recent study [14] reported that either progression from short to long sleep or reduction from long to short sleep was associated with higher risk of all-cause mortality. However, this study did not examine cause-specific mortality [14].
Utilizing the longitudinal Singapore Chinese Health Study, we examined the association between changes in sleep duration over about 13 years and risk of all-cause mortality, as well as risk of cardiovascular disease (CVD), ischaemic heart disease (IHD), stroke, and cancer mortality.
Methods
Study population
The Singapore Chinese Health Study consists of 63257 Chinese adults aged 45–74 years recruited between April 1993 and December 1998 [15]. Enrolled participants were citizens or permanent residents of Singapore residing in public housing estates, and they belonged to the two major dialect groups of Chinese in Singapore—the Hokkiens who originated from the southern part of Fujian Province and the Cantonese who came from the central region of Guangdong Province. Follow-up I and follow-up II interviews of surviving participants of the study were conducted from 1999 to 2004 and 2006 to 2010, respectively. Information on sleep duration was collected at both baseline and follow-up II interviews. This study was approved by the Institutional Review Boards at the National University of Singapore and the University of Pittsburgh, and all study participants gave informed consent.
Assessment of sleep duration and covariates
At recruitment, an in-person interview was conducted using a structured questionnaire to elicit information such as the participants’ demographics, sleep duration, height and weight, usual physical activity, alcohol intake, lifetime use of tobacco, and history of physician-diagnosed medical conditions such as hypertension, IHD, stroke, diabetes, and cancer. History of cancer prior to the participation to the study included self-reported cases at baseline interview, as well as cases identified via linkage analysis with the National Cancer Registry of Singapore, to ensure a comprehensive capture of cancer cases that could have occurred before the establishment of the registry in 1968. Height and weight were used to calculate body mass index as weight in kilograms divided by height in meters squared. The usual sleep duration of the participants was assessed by asking the question “On the average, during the last year, how many hours in a day did you sleep?”, with the following response categories: 5 hr or less, 6 hr, 7 hr, 8 hr, 9 hr, and 10 hr or more. Information on sleep duration, tobacco use, physical activity, alcohol intake, and medical history was updated at follow-up II that was administered on average 12.7 (standard deviation [SD] 1.9; range 7.7–17.2) years after the baseline interview.
Ascertainment of mortality
Information on date and cause of death among all cohort participants was obtained through linkage analysis with the Singapore Registry of Births and Deaths after their enrolment into the study up to December 31, 2015. The International Classification of Diseases version 9 codes [16] were recorded in the registry. The primary cause of death was used for the analysis, and the end points in our cause-specific analyses were deaths from CVD (codes 390–459), IHD (codes 410–414), stroke (codes 430–438), and all cancers (codes 140–208).
Statistical analysis
Only participants who completed both the baseline and follow-up II interviews were included in the analysis (n = 39523). Daily sleep duration was categorized in both baseline and follow-up II questionnaires as ≤5, 6, 7, 8, and ≥9 hr. The characteristics of the study participants by sleep duration categories at baseline and follow-up II, respectively, were compared using analysis of variance (ANOVA) for continuous variables or chi-square test for categorical variables.
For each participant eligible for the present analysis, the person-year at risk was calculated from date of follow-up II interview to date of death or December 31, 2015. Cox proportional hazards models were used to estimate the hazard ratio (HR) and corresponding 95% confidence intervals (CIs) for mortality associated with different sleep duration categories compared with 7 hr of sleep per day as the reference category. The choice of reference group was based on the recommended sleep duration for healthy older adults by the American Academy of Sleep Medicine and Sleep Research Society [17]. The first Cox regression model was adjusted for age (years), year of recruitment (1993–1995, 1996–1998), gender, dialect group (Hokkien, Cantonese), total weekly duration on moderate or strenuous physical activity (<0.5, 0.5–4, ≥4 hr per week), level of education (no formal education, primary school, secondary school, or higher), smoking status (never, former, current), alcohol intake (none, weekly, daily), and body mass index (<20, 20–<24, 24–<28, ≥28 kg/m2). In the second model, we additionally adjusted for history of medical conditions including hypertension, IHD, stroke, diabetes, and cancer. The proportional hazards assumption of the Cox models was assessed by including a time-dependent covariate for the variable of sleep duration in the model, and we did not observe any violation of the assumption.
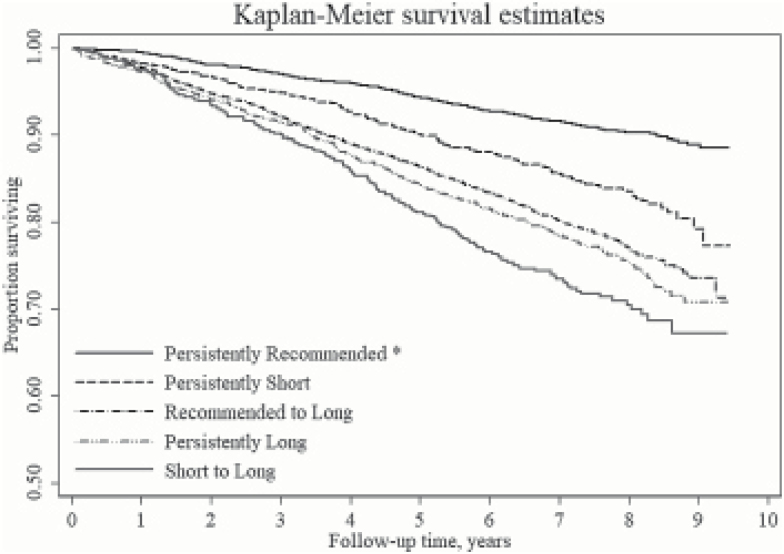
The sleep durations reported at baseline and follow-up II interviews were categorized into “recommended,” “short,” or “long” before we examined the relation between change in category of sleep duration and mortality risk. Recommended sleep duration was defined as 7 hr of sleep, whereas ≤5 and ≥9 hr were labeled short and long sleep durations, respectively. Participants who reported 6 or 8 hr of sleep were excluded from this analysis to allow for a clearer demarcation among short, recommended, and long sleep durations. Kaplan–Meier survival curves were used to examine the association between change in sleep duration between baseline and follow-up II and all-cause mortality. Cox proportional hazards models were then used to evaluate the association between change in sleep duration and risk of all-cause, CVD, IHD, stroke, and cancer mortality.
Kaplan–Meier survival analysis was performed using STATA 13.0 (College Station, Texas). All other statistical analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC) statistical software package, and two-sided p-values of <0.05 were considered statistically significant.
Results
The present analysis included 39523 who completed follow-up II interview. The cutoff date of the present analysis was December 31, 2015. Among the 39523 participants, 5610 deaths occurred from the time of follow-up II interview to the cutoff date and were included in the present analysis with a mean duration of follow-up for all participants being 7.1 (SD 1.7) years. The mean age of death was 78.0 (SD 7.8) years. Of the 5610 deaths, 1690 (30.1%) died from CVD, including 927 (16.5%) from IHD, 446 (8%) from stroke, and 1989 (35.5%) died from cancer.
At baseline interview, 33.9% reported sleeping the recommended duration (7 hr), 9.1% reported short (≤5 hr), and 6% reported long (≥9 hr) sleep duration. At follow-up II, which was after an average of 12.7 (SD 1.9) years from baseline, 23.9% reported recommended sleep duration, 10.8% reported short sleep, and 23.7% reported long sleep, indicating a small increase in proportion of short sleepers and a large increase in proportion of long sleepers at follow-up II compared with baseline. Among those who reported recommended sleep duration at baseline, 47.8% maintained the same duration of sleep, whereas 14.4% became short sleepers and 37.7% became long sleepers. Among those who reported short sleep at baseline, 44.4% remained short sleepers at follow-up II, whereas 29.5% reported recommended sleep duration and 26% became long sleepers. Among those who reported long sleep at baseline, 70.8% remained long sleepers, whereas 21.8% reduced to recommended sleep and 7.4% became short sleepers (Table 1).
Table 1.
Characteristics of study participants at follow-up II interview by change in sleep duration from baseline (1993–1998) to follow-up II (2006–2010), the Singapore Chinese Health Study
| Change in sleep duration | P* | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Short (≤5 hr) | Recommended (7 hr) | Long (≥9 hr) | |||||||
| Follow-up II | Short | 7 hr | Long | Short | 7 hr | Long | Short | 7 hr | Long | |
| N | 1054 | 701 | 618 | 1104 | 3659 | 2885 | 114 | 334 | 1085 | |
| Age, years | 68.8 ± 7.7 | 69.2 ± 7.3 | 73.4 ± 7.7 | 67.6 ± 7.2 | 66.2 ± 6.7 | 70.7 ± 7.5 | 70.3 ± 9.0 | 66.5 ± 6.7 | 71.0 ± 7.7 | <0.001 |
| Body mass index, kg/m2 | 23.1 ± 3.6 | 23.2 ± 3.6 | 23.1 ± 3.5 | 23.3 ± 3.6 | 23.2 ± 3.3 | 23.3 ± 3.6 | 23.1 ± 4.0 | 23.1 ± 3.7 | 23.1 ± 3.6 | 0.73 |
| Men | 374 (35.5) | 235 (33.5) | 210 (34.0) | 411 (37.2) | 1580 (43.2) | 1190 (41.3) | 46 (40.4) | 125 (37.4) | 443 (40.8) | <0.001 |
| Dialect group | <0.001 | |||||||||
| Cantonese | 512 (48.6) | 379 (54.1) | 327 (52.9) | 465 (42.1) | 1880 (51.4) | 1396 (48.4) | 54 (47.4) | 172 (51.5) | 568 (52.4) | |
| Hokkien | 542 (51.4) | 322 (45.9) | 291 (47.1) | 639 (57.9) | 1779 (48.6) | 1489 (51.6) | 60 (52.6) | 162 (48.5) | 517 (47.7) | |
| Moderate of vigorous physical activity, hr/week | <0.001 | |||||||||
| <0.5 | 91 (8.6) | 57 (8.1) | 110 (17.8) | 73 (6.6) | 249 (6.8) | 365 (12.7) | 17 (14.9) | 31 (9.3) | 168 (15.5) | |
| 0.5–4 | 127 (12.1) | 77 (11.0) | 128 (20.7) | 165 (15.0) | 559 (15.3) | 555 (19.2) | 21 (18.4) | 51 (15.3) | 193 (17.8) | |
| ≥4 | 836 (79.3) | 567 (80.9) | 380 (61.5) | 866 (78.4) | 2851 (77.9) | 1965 (68.1) | 76 (66.7) | 252 (75.5) | 724 (66.7) | |
| Level of education | <0.001 | |||||||||
| No formal education | 286 (27.1) | 225 (32.1) | 251 (40.6) | 285 (25.8) | 670 (18.3) | 902 (31.3) | 38 (33.3) | 70 (21.0) | 335 (30.9) | |
| Primary school | 473 (44.9) | 308 (43.9) | 285 (46.1) | 482 (43.7) | 1580 (43.2) | 1368 (47.4) | 53 (46.5) | 152 (45.5) | 511 (47.1) | |
| Secondary school or higher | 295 (28.0) | 168 (24.0) | 82 (13.3) | 337 (30.5) | 1409 (38.5) | 615 (21.3) | 23 (20.2) | 112 (33.5) | 239 (22.0) | |
| Smoking status | <0.001 | |||||||||
| Never | 772 (73.2) | 504 (71.9) | 422 (68.3) | 800 (72.5) | 2673 (73.1) | 1956 (67.8) | 80 (70.2) | 240 (71.9) | 708 (65.3) | |
| Former | 177 (16.8) | 107 (15.3) | 132 (21.4) | 180 (16.3) | 594 (16.2) | 575 (19.9) | 17 (14.9) | 60 (18.0) | 215 (19.8) | |
| Current | 105 (10.0) | 90 (12.8) | 64 (10.4) | 124 (11.2) | 392 (10.7) | 354 (12.3) | 17 (14.9) | 34 (10.2) | 162 (14.9) | |
| Alcohol intake | <0.001 | |||||||||
| None | 967 (91.8) | 642 (91.6) | 579 (93.7) | 1029 (93.2) | 3298 (90.1) | 2682 (93.0) | 104 (91.2) | 300 (89.8) | 981 (90.4) | |
| Weekly | 57 (5.4) | 46 (6.6) | 20 (3.2) | 52 (4.7) | 278 (7.6) | 132 (4.6) | 7 (6.1) | 24 (7.2) | 64 (5.9) | |
| Daily | 30 (2.9) | 13 (1.9) | 19 (3.1) | 23 (2.1) | 83 (2.3) | 71 (2.5) | 3 (2.6) | 10 (3.0) | 40 (3.7) | |
| Comorbidities | ||||||||||
| Hypertension | 568 (53.9) | 378 (53.9) | 404 (65.4) | 608 (55.1) | 1902 (52.0) | 1701 (59.0) | 69 (60.5) | 185 (55.4) | 637 (58.7) | <0.001 |
| Ischaemic heart disease | 98 (9.3) | 45 (6.4) | 62 (10.0) | 78 (7.1) | 187 (5.1) | 251 (8.7) | 12 (10.5) | 25 (7.5) | 76 (7.0) | <0.001 |
| Stroke | 48 (4.6) | 26 (3.7) | 55 (8.9) | 53 (4.8) | 92 (2.5) | 202 (7.0) | 8 (7.0) | 15 (4.5) | 69 (6.4) | <0.001 |
| Diabetes | 238 (22.6) | 144 (20.5) | 169 (27.4) | 231 (20.9) | 632 (17.3) | 697 (24.2) | 29 (25.4) | 75 (22.5) | 298 (27.5) | <0.001 |
| Cancer | 92 (8.7) | 47 (6.7) | 60 (9.7) | 93 (8.4) | 227 (6.2) | 269 (9.3) | 12 (10.5) | 31 (9.3) | 88 (8.1) | <0.001 |
*p-Value by ANOVA (continuous variables) or χ2-test (categorical variables).
When we examined the characteristics of participants by their sleep duration at baseline or follow up II, we observed that participants who reported ≤5 or ≥9 hr of sleep at baseline or follow-up II were older, more likely to be physically inactive (<0.5 hr of moderate or vigorous physical activities weekly), and had a higher prevalence of hypertension, IHD, stroke, and diabetes compared with those who reported 7 hr of sleep (Supplementary Tables 1 and 2). Long sleep duration was also associated with higher prevalence of cancer at follow-up II. In addition, long sleep duration was more likely to be reported by current smokers at both baseline and follow-up II (Supplementary Tables 1 and 2). Comparing all the categories of sleep change, participants who reported recommended sleep duration at both baseline and follow-up II were the youngest, more likely to be men and received higher level of education, less likely to be physically inactive, and had the lowest prevalence of hypertension, IHD, stroke, diabetes, and cancer (Table 1). Short sleepers at baseline who increased to long sleep at follow-up II were the oldest, most likely to be physically inactive, and had the highest prevalence of hypertension and stroke compared with other sleep change categories (Table 1).
The mean duration from baseline interview and time of death for the 5610 participants who died was 17.1 (SD 2.7) years. A U-shape association was observed between baseline sleep duration and all-cause mortality. Further adjustment for history of comorbidities in the statistical models gave similar results, although we observed a slight attenuation of the risk estimates for all-cause, CVD, IHD, and stroke mortality. In the final-adjusted model, there was a statistically significant increased risk of all-cause mortality with ≤5 hr (HR 1.12, 95% CI 1.02–1.23) and ≥9 hr (HR 1.14, 95% CI 1.03–1.27) compared with 7 hr of sleep reported at baseline (Table 2). A similar trend was observed for all the specific causes of death even though most of the associations did not reach statistical significance. A statistically signification result was observed only for the association between ≤5 hr of sleep and cancer mortality (HR 1.22, 95% CI 1.04–1.42) (Table 2). The U-shape association was also observed between sleep duration reported at follow-up II and all-cause mortality, and the risk estimate of all-cause mortality associated with ≥9 hr of sleep at follow-up II was higher than that associated with ≥9 hr of sleep at baseline. Compared with participants who reported 7 hr of sleep at follow-up II, ≤5 hr of sleep at follow-up II was associated with all-cause (HR 1.11, 95% CI 1.01–1.23) and CVD mortality (HR 1.27, 95% CI 1.05–1.52), whereas ≥9 hr of sleep was associated with increased all-cause (HR 1.35, 95% CI 1.25–1.46), CVD (HR 1.50, 95% CI 1.30–1.73), IHD (HR 1.32, 95% CI 1.09–1.59), stroke (HR 1.77, 95% CI 1.33–2.35), and cancer mortality (HR 1.13, 95% CI 1.00–1.29) (Table 3).
Table 2.
Adjusted hazard ratios for sleep duration at baseline (1993–1998) and mortality, the Singapore Chinese Health Study
| Cause of death | Sleep duration at baseline | ||||
|---|---|---|---|---|---|
| ≤5 hr | 6 hr | 7 hr | 8 hr | ≥9 hr | |
| All-cause | |||||
| No. of deaths | 641 | 1285 | 1736 | 1514 | 434 |
| Model 1† | 1.14 (1.04–1.25) | 0.99 (0.92–1.07) | 1.00 (referent) | 1.06 (0.98–1.13) | 1.18 (1.06–1.31) |
| Model 2‡ | 1.12 (1.02–1.23) | 0.99 (0.92–1.06) | 1.00 (referent) | 1.05 (0.98–1.12) | 1.14 (1.03–1.27) |
| Cardiovascular | |||||
| No. of deaths | 191 | 380 | 538 | 449 | 132 |
| Model 1† | 1.11 (0.94–1.31) | 0.95 (0.83–1.08) | 1.00 (referent) | 1.01 (0.89–1.15) | 1.17 (0.96–1.41) |
| Model 2‡ | 1.08 (0.91–1.27) | 0.95 (0.83–1.08) | 1.00 (referent) | 1.00 (0.88–1.14) | 1.11 (0.92–1.34) |
| Ischemic heart disease | |||||
| No. of deaths | 95 | 224 | 289 | 254 | 65 |
| Model 1† | 1.06 (0.84–1.34) | 1.06 (0.89–1.26) | 1.00 (referent) | 1.07 (0.90–1.26) | 1.08 (0.83–1.42) |
| Model 2‡ | 1.03 (0.81–1.30) | 1.05 (0.88–1.24) | 1.00 (referent) | 1.06 (0.89–1.25) | 1.02 (0.77–1.33) |
| Stroke | |||||
| No. of deaths | 56 | 90 | 143 | 119 | 38 |
| Model 1† | 1.14 (0.83–1.56) | 0.83 (0.63–1.08) | 1.00 (referent) | 1.01 (0.79–1.29) | 1.24 (0.86–1.77) |
| Model 2‡ | 1.12 (0.82–1.53) | 0.83 (0.64–1.08) | 1.00 (referent) | 1.00 (0.78–1.27) | 1.19 (0.83–1.70) |
| Cancer | |||||
| No. of deaths | 226 | 465 | 611 | 554 | 133 |
| Model 1† | 1.22 (1.04–1.42) | 1.04 (0.92–1.17) | 1.00 (referent) | 1.10 (0.98–1.24) | 1.07 (0.89–1.29) |
| Model 2‡ | 1.22 (1.04–1.42) | 1.04 (0.92–1.17) | 1.00 (referent) | 1.10 (0.98–1.24) | 1.07 (0.88–1.29) |
†Model 1 adjusted for age (years), year of recruitment (1993–1995 and 1996–1998), gender, dialect group (Hokkien and Cantonese), physical activity (<0.5, 0.5–4, and ≥4 hr/week), level of education (no formal education, primary school, secondary school, or higher), smoking status (never, former, and current), alcohol intake (none, weekly, and daily), and body mass index (<20, 20–<24, 24–<28, and ≥28 kg/m2).
‡Model 2 further adjusted for history of hypertension, ischaemic heart disease, stroke, diabetes, and cancer.
Table 3.
Adjusted hazard ratios for sleep duration at follow-up II (2006–2010) and mortality, the Singapore Chinese Health Study
| Cause of death | Sleep duration at follow-up II | ||||
|---|---|---|---|---|---|
| ≤5 hr | 6 hr | 7 hr | 8 hr | ≥9 hr | |
| All-cause | |||||
| No. of deaths | 582 | 681 | 994 | 1256 | 2097 |
| Model 1† | 1.14 (1.03–1.26) | 1.04 (0.94–1.15) | 1.00 (referent) | 1.09 (1.00–1.19) | 1.40 (1.30–1.51) |
| Model 2‡ | 1.11 (1.01–1.23) | 1.04 (0.94–1.14) | 1.00 (referent) | 1.08 (0.99–1.17) | 1.35 (1.25–1.46) |
| Cardiovascular | |||||
| No. of deaths | 191 | 191 | 282 | 360 | 666 |
| Model 1† | 1.33 (1.11–1.60) | 1.03 (0.85–1.23) | 1.00 (referent) | 1.11 (0.95–1.29) | 1.57 (1.36–1.81) |
| Model 2‡ | 1.27 (1.05–1.52) | 1.03 (0.86–1.24) | 1.00 (referent) | 1.08 (0.93–1.27) | 1.50 (1.30–1.73) |
| Ischemic heart disease | |||||
| No. of deaths | 103 | 102 | 169 | 210 | 343 |
| Model 1† | 1.22 (0.95–1.56) | 0.91 (0.71–1.16) | 1.00 (referent) | 1.09 (0.89–1.33) | 1.38 (1.14–1.66) |
| Model 2‡ | 1.15 (0.90–1.48) | 0.92 (0.72–1.18) | 1.00 (referent) | 1.06 (0.87–1.30) | 1.32 (1.09–1.59) |
| Stroke | |||||
| No. of deaths | 39 | 51 | 67 | 91 | 198 |
| Model 1† | 1.12 (0.75–1.66) | 1.16 (0.81–1.67) | 1.00 (referent) | 1.16 (0.85–1.60) | 1.92 (1.45–2.55) |
| Model 2‡ | 1.06 (0.71–1.57) | 1.16 (0.80–1.66) | 1.00 (referent) | 1.13 (0.82–1.55) | 1.77 (1.33–2.35) |
| Cancer | |||||
| No. of deaths | 191 | 270 | 415 | 477 | 636 |
| Model 1† | 0.94 (0.79–1.11) | 0.97 (0.83–1.13) | 1.00 (referent) | 1.03 (0.90–1.18) | 1.16 (1.02–1.32) |
| Model 2‡ | 0.93 (0.78–1.10) | 0.97 (0.83–1.12) | 1.00 (referent) | 1.03 (0.90–1.17) | 1.13 (1.00–1.29) |
†Model 1 adjusted for age (years), year of recruitment (1993–1995 and 1996–1998), gender, dialect group (Hokkien and Cantonese), physical activity (<0.5, 0.5–4, and ≥4 hr/week), level of education (no formal education, primary school, secondary school, or higher), smoking status (never, former, and current), alcohol intake (none, weekly, and daily), and body mass index (<20, 20–<24, 24–<28, and ≥28 kg/m2).
‡Model 2 further adjusted for history of hypertension, ischaemic heart disease, stroke, diabetes, and cancer.
Figure 1 shows the Kaplan–Meier survival curves among categories of change in sleep that were significantly different from those who maintained recommended sleep duration at both baseline and follow-up II. This latter category had the highest survival rate, whereas persons who reported increased sleep from short to long duration had the lowest survival. Compared with participants with consistently recommended sleep duration, those who had reported persistently short or long sleep duration at baseline and follow-up II, as well as those who had increased their sleep from recommended to long duration, also had lower survival rates (Figure 1).
Figure 1.
Kaplan–Meir survival curves for all-cause mortality by change in sleep duration from baseline (1993–1998) to follow-up II (2006–2010), the Singapore Chinese Health Study.
Compared with participants who maintained recommended sleep duration at both baseline and follow-up II, persistently short sleep duration was associated with higher risk of all-cause (HR 1.27, 95% CI 1.06–1.53), whereas persistently long sleep duration was associated with higher risk of all-cause (HR 1.47, 95% CI 1.24–1.73), CVD (HR 1.40, 95% CI 1.04–1.89), and stroke mortality (HR 1.84, 95% CI 1.07–3.16) (Table 4). Higher risk of CVD mortality was also observed when sleep was increased from short (HR 1.42, 95% CI 1.01–2.00) or recommended (HR 1.53, 95% CI 1.20–1.95) duration at baseline to long sleep at follow-up II. Cancer mortality was not significantly associated with change in sleep duration. There was no significant increase in risk of mortality when participants who were short or long sleepers at baseline changed to have recommended sleep duration at follow-up II (Table 4). We have further examined the relation between sleep change and mortality with stratification by age group (<70 or ≥70 years at follow-up II), history of medical conditions including hypertension, IHD, stroke, diabetes and cancer (yes to any of the conditions or none of the conditions), and smoking status (never or ever smokers), and similar risk estimates were obtained (Supplementary Table 3). In the stratified analysis, an increase from 7 hr to long sleep duration was associated with statistically significant increased risk of all-cause mortality regardless of age group, history of medical conditions, or smoking status (Supplementary Table 3). Persistently long sleep duration was associated with increased risk of all-cause mortality regardless of age group, history of medical conditions, or smoking status, although the increased mortality risk among ever smokers was of borderline significance (Supplementary Table 3). We have repeated the analysis for sleep duration at baseline using the entire cohort and the results were essentially the same as the results using 39523 participants included in this study. Specifically, compared with 7 hr of sleep, there was a statistically significant increased risk of CVD (HR 1.19, 95% CI 1.10–1.30) and cancer (HR 1.15, 95% CI 1.06–1.25) mortality with ≤5 hr, and increased risk of CVD (HR 1.22, 95% CI 1.12–1.34) and cancer (HR 1.09, 95% CI 0.99–1.20) mortality with ≥9 hr of sleep. This shows that the results from the smaller subcohort in this study were comparable to the entire cohort.
Table 4.
Adjusted hazard ratios for change in sleep duration from baseline (1993–1998) to follow-up II (2006–2010) and mortality, the Singapore Chinese Health Study
| Change in sleep duration from baseline to follow-up II | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | Short (≤5 hr) | Recommended (7 hr) | Long (≥9 hr) | ||||||
| Follow-up II | Short | Recommended | Long | Short | Recommended | Long | Short | Recommended | Long |
| All-cause | |||||||||
| No. of deaths | 170 | 102 | 173 | 145 | 344 | 623 | 23 | 37 | 259 |
| Hazard ratio† | 1.27 | 1.14 | 1.50 | 1.16 | 1.00 | 1.43 | 1.00 | 0.99 | 1.47 |
| 95% CI† | 1.06–1.53 | 0.91–1.43 | 1.24–1.81 | 0.95–1.41 | Referent | 1.25–1.64 | 0.65–1.54 | 0.71–1.40 | 1.24–1.73 |
| Cardiovascular | |||||||||
| No. of deaths | 56 | 29 | 53 | 47 | 107 | 218 | 9 | 12 | 78 |
| Hazard ratio† | 1.33 | 1.05 | 1.42 | 1.19 | 1.00 | 1.53 | 1.20 | 0.99 | 1.40 |
| 95% CI† | 0.96–1.84 | 0.69–1.59 | 1.01–2.00 | 0.84–1.68 | Referent | 1.20–1.95 | 0.60–2.40 | 0.54–1.79 | 1.04–1.89 |
| Ischemic heart disease | |||||||||
| No. of deaths | 27 | 15 | 27 | 27 | 62 | 114 | 4 | 7 | 34 |
| Hazard ratio† | 1.17 | 0.97 | 1.38 | 1.20 | 1.00 | 1.44 | 0.97 | 1.02 | 1.10 |
| 95% CI† | 0.74–1.84 | 0.55–1.71 | 0.86–2.22 | 0.76–1.89 | Referent | 1.04–1.98 | 0.35–2.71 | 0.47–2.24 | 0.72–1.70 |
| Stroke | |||||||||
| No. of deaths | 15 | 10 | 18 | 10 | 28 | 62 | 0 | 3 | 28 |
| Hazard ratio† | 1.27 | 1.33 | 1.64 | 0.93 | 1.00 | 1.54 | — | 0.95 | 1.84 |
| 95% CI† | 0.67–2.40 | 0.64–2.76 | 0.88–3.05 | 0.45–1.92 | Referent | 0.97–2.44 | — | 0.29–3.15 | 1.07–3.16 |
| Cancer | |||||||||
| No. of deaths | 52 | 40 | 52 | 45 | 144 | 180 | 3 | 13 | 73 |
| Hazard ratio† | 1.01 | 1.16 | 1.37 | 0.90 | 1.00 | 1.15 | 0.38 | 0.90 | 1.17 |
| 95% CI† | 0.73–1.40 | 0.81–1.65 | 0.98–1.90 | 0.64–1.26 | Referent | 0.92–1.45 | 0.12–1.19 | 0.51–1.58 | 0.88–1.57 |
†Model 1 adjusted for age (years), year of recruitment (1993–1995 and 1996–1998), gender, dialect group (Hokkien and Cantonese), physical activity (<0.5, 0.5–4, and ≥4 hr/week), level of education (no formal education, primary school, secondary school, or higher), smoking status (never, former, and current), alcohol intake (none, weekly, and daily), body mass index (<20, 20–<24, 24–<28, and ≥28 kg/m2), history of hypertension, ischaemic heart disease, stroke, diabetes, and cancer.
Discussion
The present study found that compared with those with a consistent sleep duration of 7 hr, persistent short sleep was associated with increased risk of all-cause mortality, whereas persistent long sleep or an increase in long sleep duration in late adulthood increased the risk of all-cause and cardiovascular mortality.
The association between sleep duration and mortality has been examined by many studies, and our observation of a U-shape association between sleep duration and all-cause mortality with a nadir at 7 hr at baseline and follow-up II is consistent with current literature [4, 7–9, 11]. Both short and long sleep have been reported by epidemiological studies to be associated with higher risk of cardiovascular outcome and mortality [4, 6, 7, 18]. Insufficient and prolonged sleep duration have been associated with cardiovascular risk factors such as metabolic syndrome, obesity, hypertension, insulin resistance, and type II diabetes [19]. In our cohort, we also observed higher prevalence of comorbidities such as hypertension, IHD, stroke, and diabetes mellitus among short and long sleepers. Short sleep duration may lead to adverse cardiovascular outcomes via mechanisms such as changes in production of leptin and ghrelin, leading to increased energy intake, obesity, and impaired glycemic control, increased secretion of the stress hormone cortisol and altered growth hormone metabolism, and the activation of low-grade inflammation [18]. On the other hand, the underlying mechanism(s) underlying long sleep duration and poorer cardiovascular outcomes is less clear, and possible explanations include the effects of sleep fragmentation, depression, low level of physical activity, and undiagnosed health conditions [18, 20].
In our study, cancer mortality was not associated with change in sleep duration. This is consistent with the results of two recent meta-analyses [21, 22], in which neither short nor long sleep duration was associated with increased risk of cancer. These two meta-analyses [21, 22] also reported long sleep duration to be positively associated with colorectal cancer but inversely associated with hormone-related cancers such as prostate and ovarian cancer. However, we were unable to examine cancer mortality by the different cancer types in our analysis. These findings collectively reflect the lack of consensus in linking sleep duration with cancer risk reflected in epidemiological data [17, 21, 22].
Change in sleep duration has been reported to be associated with higher risk of all-cause mortality [5, 13, 14]. Persistently short and long sleep durations have been reported to be associated with increased risk of all-cause mortality among men in the Finnish Twin Cohort [5], and this is in line with the results of the present study. A recent study conducted in a smaller cohort concluded that there was no association between persistent short or long sleep and risk of mortality [14], although the authors had reported a slight increase in these risk estimates compared with the reference group of consistent 7–8 hr of sleep. One of these studies had examined cause-specific mortality, and the authors reported higher risk of CVD mortality among men to be associated with reduction of sleep duration from 6, 7, or 8 hr, but the association with increased sleep duration was not statistically significant [13]. Conversely, we found that the transition to long sleep at late adulthood was associated with greater risk of CVD mortality, but the association with shortening sleep was not significant.
Although persistently short sleep has been observed to increase the risk of all-cause mortality in other studies and our cohort, we did not observe an increased risk of mortality with reduction of sleep duration in this cohort. Hence, although chronic short sleep is associated with increased mortality risk, our results suggest that shortening of habitual sleep duration among older adults may not be a cause of concern. Our results also suggest that short or long sleepers who changed to recommended sleep duration at later life did not have a significant increased risk of mortality. Conversely, we observed an increased proportion of long sleepers with aging, as well as an increased risk of cardiovascular mortality when sleep duration lengthened to 9 hr or more.
The association between increased sleep duration and CVD mortality needs to be interpreted with caution as increased sleep duration among older adults could be a sign of poorer health outcomes or an epiphenomenon of comorbidity [23, 24]. Our findings generally support the recent sleep duration recommendations for older adults formulated by the American Academy of Sleep Medicine and Sleep Research Society [17] that are based on data mainly from Caucasian populations. The self-reported sleep duration in young adults in East Asia is between 1 and 2 hr less than their counterparts in Europe [25]. As such, our findings contribute to the literature on sleep epidemiology among Asians and provide an impetus for policy makers in this region to incorporate sleep education in plans for lifestyle risk-factor modification.
The strengths of our study include its large sample size, long duration of follow-up, and prospective longitudinal study design with information on sleep duration and other covariates collected at two time points, which allowed us to examine the relation between change in sleep duration and risk of mortality. In addition, we were also able to examine the different causes of death. Although we did not conduct any validation of the question on sleep duration, the duration of sleep assessed using this question has been examined with many other health outcomes in this cohort [23, 26–31]. Among its limitations, self-reported sleep duration likely represents time in bed rather than sleep time. We also did not distinguish between naps and nocturnal sleep. We also lacked information on sleep disorders, sleep quality [32], and social isolation [33], all of which might affect mortality. The sleep duration of the participants could have changed due to retirement, and we lacked data on such information. Nevertheless, since the retirement age in Singapore was between 55 and 60 years during the period of recruitment, as many as 50% of our participants were above 55 years old and could have retired at the time of recruitment. As this study only included participants who completed both baseline and follow-up II interviews, this could potentially introduce a selection bias. However, comparable results were obtained when we examined the association between baseline sleep duration and mortality in the entire cohort and in this smaller subcohort. Even though we adjusted for prevalent comorbidities in our statistical models, there could be misclassifications as these conditions were self-reported, and there could still be residual confounding due to untracked medical conditions. Adjustment for the socioeconomic status of the participants using their highest level of education may also be incomplete.
In summary, keeping to a daily sleep duration of 7 hr is associated with lowest mortality risk and a change from any length of sleep to ≥9 hr in late adulthood should raise concerns about increased risk of mortality. The persistence of both extreme short (≤ 5 hr) and long (≥9 hr) sleep is also not desirable. Factors contributing to such extreme sleep durations or the lengthening of sleep duration remain topics for future experimental studies.
Supplementary Material
Supplementary material is available at SLEEP online.
Funding
This study was supported by the National Institutes of Health, USA (R01 CA144034 and UM1 CA182876). Woon-Puay Koh is supported by the National Medical Research Council, Singapore (NMRC/CSA/0055/2013). Michael Chee is supported by the National Medical Research Council, Singapore (STaR/0013/2013) and by The Far East Organization.
Acknowledgments
The authors thank Siew-Hong Low of the National University of Singapore for supervising the field work of the Singapore Chinese Health Study and Renwei Wang for the maintenance of the cohort study database. We also thank the Ministry of Health in Singapore for assistance with the identification of mortality via database linkages.
Notes
Conflict of interest statement. None declared.
Work Performed: Duke-NUS Medical School, 8 College Road, Singapore 169857, Singapore.
References
- 1. Luyster FS, et al. ; Boards of Directors of the American Academy of Sleep Medicine and the Sleep Research Society. Sleep: a health imperative. Sleep. 2012; 35(6): 727–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Institute of Medicine Committee on Sleep Medicine and Research. The National Academies collection: reports funded by National Institutes of Health. In: Colten HR, Altevogt BM, eds. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem. Washington (DC): National Academies Press (US) National Academy of Sciences, 2006. [PubMed] [Google Scholar]
- 3. Miyata S, et al. Insufficient sleep impairs driving performance and cognitive function. Neurosci Lett. 2010; 469(2): 229–233. [DOI] [PubMed] [Google Scholar]
- 4. Cai H, et al. Sleep duration and mortality: a prospective study of 113 138 middle-aged and elderly Chinese men and women. Sleep. 2015; 38(4): 529–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hublin C, et al. Sleep and mortality: a population-based 22-year follow-up study. Sleep. 2007; 30(10): 1245–1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Xiao Q, et al. Sleep duration and total and cause-specific mortality in a large US cohort: interrelationships with physical activity, sedentary behavior, and body mass index. Am J Epidemiol. 2014; 180(10): 997–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ikehara S, et al. ; JACC Study Group Association of sleep duration with mortality from cardiovascular disease and other causes for Japanese men and women: the JACC study. Sleep. 2009; 32(3): 295–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kripke DF, et al. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002; 59(2): 131–136. [DOI] [PubMed] [Google Scholar]
- 9. Liu TZ, et al. Sleep duration and risk of all-cause mortality: a flexible, non-linear, meta-regression of 40 prospective cohort studies. Sleep Med Rev. 2017; 32: 28–36. [DOI] [PubMed] [Google Scholar]
- 10. da Silva AA, et al. Sleep duration and mortality in the elderly: a systematic review with meta-analysis. BMJ Open. 2016; 6(2): e008119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shen X, et al. Nighttime sleep duration, 24-hour sleep duration and risk of all-cause mortality among adults: a meta-analysis of prospective cohort studies. Sci Rep. 2016; 6: 21480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ohayon MM, et al. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004; 27(7): 1255–1273. [DOI] [PubMed] [Google Scholar]
- 13. Ferrie JE, et al. A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep. 2007; 30(12): 1659–1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Aurora RN, et al. Habitual sleep duration and all-cause mortality in a general community sample. Sleep. 2016; 39(11): 1903–1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hankin JH, et al. Singapore Chinese Health Study: development, validation, and calibration of the quantitative food frequency questionnaire. Nutr Cancer. 2001; 39(2): 187–195. [DOI] [PubMed] [Google Scholar]
- 16. Centers for Disease Control and Prevention. International Classification of Diseases, Ninth Revision (ICD-9). Maryland: National Center for Health Statistics, Centers for Disease Control and Prevention. [Google Scholar]
- 17. Watson NF, et al. Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015; 38(6): 843–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cappuccio FP, et al. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. Eur Heart J. 2011; 32(12): 1484–1492. [DOI] [PubMed] [Google Scholar]
- 19. Koren D, et al. Role of sleep quality in the metabolic syndrome. Diabetes Metab Syndr Obes. 2016; 9: 281–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ju SY, et al. Sleep duration and metabolic syndrome in adult populations: a meta-analysis of observational studies. Nutr Diabetes. 2013; 3: e65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zhao H, et al. Sleep duration and cancer risk: a systematic review and meta-analysis of prospective studies. Asian Pac J Cancer Prev. 2013; 14(12): 7509–7515. [DOI] [PubMed] [Google Scholar]
- 22. Lu Y, et al. Association between sleep duration and cancer risk: a meta-analysis of prospective cohort studies. PLoS One. 2013; 8(9): e74723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Smagula SF, et al. Chronic disease and lifestyle factors associated with change in sleep duration among older adults in the Singapore Chinese Health Study. J Sleep Res. 2016; 25(1): 57–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Stranges S, et al. Correlates of short and long sleep duration: a cross-cultural comparison between the United Kingdom and the United States: the Whitehall II Study and the Western New York Health Study. Am J Epidemiol. 2008; 168(12): 1353–1364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gradisar M, et al. Recent worldwide sleep patterns and problems during adolescence: a review and meta-analysis of age, region, and sleep. Sleep Med. 2011; 12(2): 110–118. [DOI] [PubMed] [Google Scholar]
- 26. Odegaard AO, et al. Combined lifestyle factors and cardiovascular disease mortality in Chinese men and women: the Singapore Chinese health study. Circulation. 2011; 124(25): 2847–2854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Shankar A, et al. Sleep duration and coronary heart disease mortality among Chinese adults in Singapore: a population-based cohort study. Am J Epidemiol. 2008; 168(12): 1367–1373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wu AH, et al. Sleep duration, spot urinary 6-sulfatoxymelatonin levels and risk of breast cancer among Chinese women in Singapore. Int J Cancer. 2013; 132(4): 891–896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Pan A, et al. Sleep duration and risk of stroke mortality among Chinese adults: Singapore Chinese Health Study. Stroke. 2014; 45(6): 1620–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Odegaard AO, et al. Combined lifestyle factors and risk of incident colorectal cancer in a Chinese population. Cancer Prev Res (Phila). 2013; 6(4): 360–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wu AH, et al. Sleep duration, melatonin and breast cancer among Chinese women in Singapore. Carcinogenesis. 2008; 29(6): 1244–1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rod NH, et al. The joint effect of sleep duration and disturbed sleep on cause-specific mortality: results from the Whitehall II cohort study. PLoS One. 2014; 9(4): e91965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kuiper JS, et al. Social relationships and risk of dementia: a systematic review and meta-analysis of longitudinal cohort studies. Ageing Res Rev. 2015; 22: 39–57. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.