Abstract
Objective
There is little empirical evidence supporting the long-term use of opioid therapy for chronic pain, suggesting the need to reevaluate the role of opioids in chronic pain management. Few studies have considered opioid use and opioid cessation from the perspective of the patient.
Methods
This prospective structured interview study included 150 new patients seeking treatment for chronic pain at an outpatient tertiary care pain clinic.
Results
Of the 150 patients, 56% (N = 84) reported current opioid use. Opioids users reported higher pain severity (t(137) = -3.75, P < 0.001), worse physical functioning (t(136) = -3.82, P < 0.001), and more symptoms of depression (t(136) = -1.98, P = 0.050) than nonusers. Among opioid users, 45.6% reported high pain (>7), 60.8% reported low functioning (>7), and 71.4% reported less than a 30% reduction in pain severity since starting opioids, suggesting that many patients are unlikely to be receiving adequate benefit. Overall, 66.3% of current opioid users reported moderate to high opioid-related difficulties on the prescribed opioids difficulties scale, and patients with depression were more likely to report greater difficulties. There was no association between helpfulness of opioids over the past month and opioid-related difficulties (r(75) = -0.07, P = 0.559), current pain severity (r(72)=0.05, P = 0.705), or current pain interference (r(72) = 0.20, P = 0.095).
Conclusions
Despite clinical indicators that question the benefit, patients may continue to report that their opioids are helpful. Such discrepancies in patients’ perceptions will likely pose significant barriers for implementing opioid cessation guidelines in clinical practice.
Keywords: Opioids, Opioid Cessation, Chronic Pain, Helpfulness
Introduction
With the rise in opioid overdoses and deaths, addressing the “opioid epidemic” in the United States has become a significant public health issue [1–3]. The use of opioids to treat chronic pain has increased significantly in the last 20 years, with over 130 million hydrocodone prescriptions filled annually [4]. However, there is little empirical evidence supporting the long-term use of opioid therapy for chronic pain [5–8], suggesting the need to reevaluate the role of opioids in chronic pain management. The recent opioid guidelines from the US Centers for Disease Control (CDC) state that if the benefits of opioids do not outweigh the harms and there is not sufficient evidence of sustained improvement in pain and functioning, physicians should work to taper patients to lower doses or encourage complete opioid cessation [9,10]. It follows that patients who were started on opioids for therapeutic use (i.e., pain relief) but who continue to use opioids when benefit is not apparent are also casualties of the opioid epidemic, and solutions to this complex aspect of prescription opioid use are needed.
In a clinic setting, the issues and concerns associated with maintaining a patient on chronic opioid therapy are distinct from concerns about starting a patient on a new opioid prescription. Few studies have considered opioid use and opioid cessation from the perspective of the patient already prescribed opioids for pain management. One pivotal study found that most patients report that opioids are very helpful yet they also identify significant problems with opioids, which suggests that there are discrepancies in how patients evaluate the risks and benefits of opioid medication [11]. As guidelines for reducing chronic opioid use are developed, a lack of understanding of how patients will respond to a physician’s recommendation to reduce opioid use may make implementing guidelines challenging. Studies that assess the unique personal experiences of patients who have been prescribed opioid therapy for chronic pain are needed in order to understand how best to reduce long-term opioid therapy in the context of chronic pain management.
The broad aim of this study was to solicit information from current opioid users seeking treatment at a tertiary pain clinic regarding their opioid use. This paper has four primary objectives: 1) to assess patterns of opioid use among current opioid users and to compare current opioid users and nonopioid users on key clinical features including pain, functioning, mood, and opioid use history (we hypothesized that opioids users would have a worse clinical phenotype compared with nonopioid users); 2) to use the prescribed opioids difficulties scale to evaluate patients’ beliefs about the difficulties associated with opioids and assess how strongly these difficulties are associated with perceptions of helpfulness, motivation to continue opioids, and effect (we hypothesized that difficulties would be negatively associated with helpfulness and motivation and positively associated with depression); 3) to evaluate the perceptions of helpfulness associated with opioids and to explore the extent to which helpfulness is associated with pain severity and functioning (we hypothesized that helpfulness would be negatively associated with pain and functioning); and 4) to explore how motivational factors may influence willingness to engage in opioid cessation (we hypothesized that desire to continue taking opioids would be positively associated with helpfulness and negatively associated with confidence in managing pain without opioids). Given the recent CDC recommendations, an exploratory aim identified subgroups of opioid users based on clinically meaningful characteristics including improvement in pain since starting opioids, current pain severity, and current functioning.
Methods
Study Setting and Participants
This study included 150 new patients seeking treatment for chronic pain at the Back and Pain Center (Department of Anesthesiology, University of Michigan, Ann Arbor, MI, USA). The Back and Pain Center is an outpatient tertiary care pain clinic where patients are evaluated for a range of chronic pain conditions. Between Novebmer 19, 2014, and March 23, 2015, a research assistant screened the clinic schedule daily. Inclusion criteria for this study were all patients between the ages of 18 and 70 who were scheduled for a new patient visit. Exclusion criteria included age, non-English speaking, and cognitive impairment. There were 277 potentially eligible new patients; however, 41 were excluded during chart review because of age. Additionally, a total of 63 patients were not approached during the enrollment period due to several factors including not having a research assistant available to meet with the patient or clinic flow. Of the 173 patients approached, 19 declined participation and four were excluded due to being non-English speaking (N = 3) and cognitive impairment (N = 1). This resulted in a total of 150 eligible patients who consented to participate in this study. Participation involved a structured interview about current and past opioid use and a brief questionnaire. Patients were not compensated financially for their participation. Institutional review board (Ann Arbor, MI, USA) approval was obtained.
Structured Interview Procedure
While patients were waiting to be seen by the physician in the exam room, they were approached by a research assistant and asked if they would be interested in participating in a brief study. The research assistant administered a brief structured interview about opioid use developed by the investigative team. The interview consisted of yes/no items, numeric rating scales, and free text. The research assistants, all highly experienced in interview techniques, were trained on how to administer the questionnaire. For current opioid users, the duration of the interview was approximately 15 minutes. For patients not using opioids, the duration of the interview was approximately five minutes.
Structured Interview Measures
Assessment of Current Opioid Use
Current opioid use was assessed using a comprehensive checklist of opioids that asked participants to indicate whether they currently take opioids (yes = current opioid user, no = nonopioid user). For patients reporting current opioid use, a daily oral morphine equivalency (OME) was calculated using previously described conversions [12]. Patients were asked to report how they take their opioid medication and categorized as either being taken on a fixed schedule, in anticipation of pain, symptomatically in response to pain, or a combination of these categories. The duration of pain relief after taking an opioid was measured with the item “On average how long do you experience pain relief after you take this opioid?” Additional data were collected including duration of use, reason for having that particular opioid prescription, and prescribing physician.
History of Opioid Use
Several items were developed to assess history of opioid use. Data was collected on age of first opioid use and duration of first use. Participants were also asked to describe in their own words their first experience taking opioids (i.e., negative or positive). Additional data was collected on age of first chronic opioid use. Chronic opioid use was defined as using opioids almost every day for three months or longer.
Percentage (%) Pain Reduction Since Starting Opioids and Duration of Pain Relief After Taking Opioids
Participants also answered the following item “On a scale of 0 to 10 with 0 being no pain and 10 being worst pain imaginable, what was your average pain level before you began taking opioids?” This item and the brief pain inventory pain severity score (described below) were used to create a percentage pain reduction score since starting opioids. A 30% reduction or more in pain was considered a clinically meaningful change as this is commonly used as a marker of improvement [13]. Patients also were asked “On average, how long do you experience pain relief for after you take your opioid?”
Assessment of Difficulties of Prescribed Opioids
The prescribed opioids difficulties scale (PODS) was used to measure difficulties attributed to opioids from the patient’s perspective [14]. The PODS is a 15-item validated scale used to assess two domains of difficulties: psychosocial problems associated with opioids and concerns about controlling opioid use. The psychosocial problem subscale consists of eight items that ask the patient to rate the degree to which they relate problems with mood, function, cognition, and side effects to opioids. The concern subscale consists of seven items that address concerns patients have about controlling opioid use. We used the combined scale and grouped patients using the recommended cut-points of 0 to 7 (low), 8 to 15 (intermediate), and 16+ (high) [14].
Self-Reported Perceptions of the Helpfulness of Opioids
Self-reported perceived helpfulness was assessed across multiple domains including 1) degree of pain relief (i.e., “On a scale of 0 to 10 where zero is no relief and 10 is complete relief, what number best describes how much pain relief you get on average after taking this medication?”) and 2) functional improvement (i.e., “Thinking about your ability to do day to day activities, on a scale of 0 to 10 where 0 is no improvement and 10 is complete return to your normal activity level, what number best describes how much your ability to function improves after taking this medication?”). Additionally, one item from the PODS (described in detail below) asks patients to indicate “Over the past month, how helpful have you found opiate pain medications in relieving your pain?” (0 = not at all helpful, 4 = extremely helpful). This item is not included in the total PODS scale score and can be used as a single item to measure helpfulness [14]. The three perceived helpfulness items were analyzed separately.
Motivational Factors
Motivation was assessed using the following four items developed by the researchers: 1) “On a scale of 0 to 10 where 0 is no desire and 10 is full desire, which number best describes your want to continue taking an opioid for your current pain?”; 2) “What % of pain improvement would you need to experience before you would consider stopping use of your opioid medication?”; 3) “On a scale of 0 to 10 where 0 is not at all confident and 10 is very confident, how confident are you in your ability to manage pain without opioids?”; and 4) “On a scale of 0 to 10 where 0 is no desire and 10 is full desire, which number best describes your interest in learning different ways of managing pain other than opioids?”
New Patient Questionnaire Measures
All new patients seen at the Back and Pain Center are mailed a packet of questionnaires prior to their appointment as part of an ongoing clinical care and research initiative [15]. Institutional review board (Ann Arbor, MI, USA) approval was obtained prior to the start of this initiative, and informed consent was waived. For the 150 people included in the current study, the questionnaire data collected as part of their regular new patient visit was entered into the Assessment of Pain Outcomes Longitudinal Electronic Data Capture (APOLO EDC) system. This questionnaire data was merged with the data collected as part of this study. There were seven patients (4.7%) who did not complete an APOLO packet.
Pain Severity and Functional Impairment
The brief pain inventory (BPI) is a widely used scale that assesses both the severity of pain and its interference with common activities [16]. The BPI consists of a four-item subscale that is averaged to generate a single composite pain severity score. Participants are asked to rate their worst pain in the last week, least pain in the last week, pain on average, and pain right now on a scale of 0 (no pain) to 10 (pain as bad as you can imagine). These scores are averaged, and a high score indicates greater pain severity. Functional impairment was assessed using the BPI seven-item pain interference subscale. Participants are asked to rate their general activity, mood, walking ability, normal work, relations, sleep, and enjoyment of life on a scale of 0 (does not interfere) to 10 (interferes completely). These scores are averaged, and a high score indicates greater functional impairment.
Symptoms of Depression and Anxiety
Symptoms of depression and anxiety were assessed using two seven-item subscales from the hospital anxiety and depression scale (HADS) [17]. The HADS is a brief and widely-used instrument used to measure psychological distress in both general and medical populations. A score of 0 to 7 is considered within the normal range; a score of 8 to10 is suggestive of the presence of depression/anxiety; and a score of 11 or higher indicates a high probability that depression/anxiety is present.
Statistical Analysis
Descriptive statistics including frequencies, means, and standard deviations were calculated for demographic data, opioid use, perceived helpfulness, and motivation to continue opioids. For those currently taking opioids, pairwise correlations were calculated using Pearson’s r to assess relationships between self-reported helpfulness of opioids, pain severity, and pain interference. Correlations were also calculated to assess relationships between opioid-related difficulties and pain, functioning, helpfulness, and mood. Phenotypic differences between those currently taking opioids and those not taking opioids were assessed with t tests. Finally, differences between patients with less than 30% pain improvement and those with 30% or greater improvement on self-reported helpfulness of opioids in relieving pain over the past month, amount of pain relief after taking an opioid, and functional improvement after taking an opioid were assessed with t tests. Analyses were conducted using Stata version 13.1 [18] .
Results
Characteristics of Opioid Use
Of the 150 new patients, 56% (N = 84) reported current opioid use. Demographic data and patterns of opioid use are presented in Table 1. Of the 84 current opioids users, 10.7% (N = 9) of patients reported using two opioids. The most commonly prescribed opioid was hydrocodone (46.4%). Chronic opioid use, defined as opioid use for 90 days or greater, was reported by 78% of the opioid users, and 90% of patients reported daily use. Back pain (28.6%) was the primary pain complaint reported as the reason for the current opioid prescription. Primary care physicians wrote 60.5% of all prescriptions, followed by surgeons (13.6%) and pain specialists (13.6%). On the BPI, 45.6% of patients reported high pain on the pain severity subscale (>7) and 60.8% reported low functioning on the pain interference subscale (>7). Additionally, 72.4% of patients reported less than a 30% reduction in pain severity since starting opioids. Out of the 84 current opioid users, 27.1% reported no pain relief after taking opioids.
Table 1.
Descriptive characteristics of current opioid users (N = 84) at an outpatient pain clinic
| Demographics | Mean, N | SD, % |
|---|---|---|
| Age, y | 48.75 | 11.80 |
| % male gender | 35 | 41.67 |
| % Caucasian ethnicity | 72 | 90 |
| % college education | 21 | 26.6 |
| Patterns of current opioid use | ||
| % of patients taking 2 opioids | 9 | 10.71 |
| Top 5 opioids reported | ||
| Hydrocodone/norco | 39 | 46.4 |
| Ultram/tramadol | 24 | 28.6 |
| Oxycodone/percocet | 10 | 11.9 |
| Codeine | 5 | 6.0 |
| Morphine | 3 | 3.6 |
| Duration of current use | ||
| <90 d | 18 | 22.00 |
| 90 d–<1 y | 23 | 28.0 |
| 1 y–5 y | 27 | 32.9 |
| 5+ y | 14 | 17.1 |
| Schedule | ||
| Fixed only | 25 | 30.49 |
| Before pain starts only | 5 | 6.10 |
| After pain starts only | 31 | 37.80 |
| Combination of all three | 21 | 25.61 |
| Current daily OME | 25.03 | 37.91 |
| % reporting daily opioid use | 75 | 90 |
| Top 5 pain sites for which opioids are taken | ||
| Back pain only | 24 | 28.6 |
| Lower extremity pain | 11 | 13.1 |
| Upper extremity pain | 10 | 11.9 |
| Widespread pain | 9 | 10.7 |
| Abdominal pain | 7 | 8.3 |
| Prescribing physician | ||
| Primary care | 49 | 60.5 |
| Surgeon | 11 | 13.6 |
| Pain specialist | 11 | 13.6 |
| Neurologist | 3 | 3.7 |
| Other specialist | 7 | 8.6 |
| Clinical indicators of pain and functioning | ||
| % of patients with high pain (>7 on BPI pain severity) | 36 | 45.6 |
| % of patients with low functioning (>7 on BPI pain interference) | 48 | 60.8 |
| % of patients with <30% pain relief since starting opioids | 55 | 72.4 |
| Average duration of pain relief | ||
| No relief | 16 | 27.1 |
| 1 h | 7 | 11.9 |
| >1–<4 h | 12 | 20.3 |
| 4–< 6 h | 14 | 23.7 |
| 6+ h | 10 | 16.9 |
Ns vary due to missing data.
Clinical Characteristics and Opioid Use History of Patients Reporting Current Opioid Use Compared with Those Not Reporting Opioid Use
Current opioid use was associated with a worse clinical phenotype, including higher pain severity (t(137) = -3.75, P < 0.001), worse physical functioning (t(136) = -3.82, P < 0.001), and more symptoms of depression (t(136) = -1.98, P = 0.050) (see Table 2). Anxiety was not associated with opioid use (t(132) = -1.36, P = 0.177). There were no differences in age of first use or age of first continuous use between current and nonopioid users (t(112) = 1.52, P = 0.131). Current opioid users were more likely to report a positive experience associated with first-time opioid use (P = 0.047). Of the nonopioid users, 92.4% reported opioid use in the past and 21.3% reported a history of continuous opioid use.
Table 2.
Clinical characteristics and opioid use history between current opioid users and nonopioid users
| Opioid use |
|||
|---|---|---|---|
| Yes | No | ||
| N = 84 | N = 66 | P* | |
| Demographics | |||
| Age, y | 48.75 (11.8) | 47.06 (13.4) | 0.41 |
| % male gender | 41.67 | 40.91 | 0.93 |
| % Caucasian ethnicity | 90.0 | 83.6 | 0.260 |
| % college education | 26.6 | 44.3 | 0.029 |
| Pain and mood | |||
| BPI pain severity (range = 0–10) | 6.64 (1.71) | 5.42 (2.1) | <0.001 |
| BPI interference (range = 0–10) | 7.26 (2.08) | 5.71 (2.67) | <0.001 |
| HADS depression | 8.88 (4.37) | 7.31 (4.97) | 0.05 |
| % depression positive | 37.7 | 24.6 | 0.07 |
| HADS anxiety | 8.91 (4.95) | 7.80 (4.37) | 0.177 |
| History of first opioid use | |||
| Age, y | 28.39 (12.04) | 23.16 (14.41) | 0.131 |
| % positive overall experience | 67.2 | 49.2 | 0.047 |
| History of first chronic opioid use | |||
| Age, y | 36.00 (10.46) | 39.00 (10.45) | 0.443 |
BPI = brief pain inventory; HADS = hospital anxiety and depression scale.
Chi-square tests were conducted for categorical variables, and independent samples t tests were conducted for continuous variables. Mean and standard deviation reported for continuous variables.
Assessment of Opioid-Related Difficulties and Associations with Helpfulness, Desire to Continue Taking Opioids, and Mood
Participants were grouped as having low, intermediate, or high levels of opioid-related difficulties based on their total PODS score. The percentages of patients falling into the three groups were 33.8% (low), 31.2% (intermediate), and 35.1% (high). Overall, current opioid users reported a mean total PODS score of 14.60 (11.02), which suggests intermediate opioid-related difficulties. The PODS total score was not associated with helpfulness of opioids in the past month (r(75) = -0.07, P = 0.559) and also not associated with desire to continue taking opioids (r(74) = -0.10, P = 0.390). Patients with symptoms suggestive of depression based on their HADS score had higher PODS total scores (M = 18.96, SD = 12.07) compared with patients without symptoms suggestive of depression (M = 11.42, SD = 9.45; t(69) = -2.94, P = 0.004).
Self-Reported Helpfulness and the Association with Pain Severity and Physical Functioning
Descriptive data on self- reported helpfulness is presented in Table 3. The average pain relief after taking an opioid was 4.98 (SD = 2.41; 0 to 10 scale where zero is no relief and 10 is complete relief), the average improvement in functioning after taking an opioid was 4.41 (SD = 2.88; 0 to 10 scale where 0 is no improvement and 10 is complete return to normal activity level), and the average PODS helpfulness rating for opiate pain medications in relieving pain over the past month was 2.32 (SD = 1.12; 0 = not at all helpful, 4 = extremely helpful). We defined “high helpfulness” as a score of 8 or higher on the pain relief and improvement in functioning helpfulness items and a score of 4 on the PODS helpfulness item. High pain relief was reported by 17.1% of patients, high improvement in functioning was reported by 15.4% of patients, and high helpfulness of opioids in relieving pain in the last month was reported by 17.1% of patients.
Table 3.
Self-reported helpfulness of current opioid
| M | SD | % endorsement of high helpfulness* | |
|---|---|---|---|
| Amount of pain relief (range = 0–10) | 4.98 | 2.41 | 17.1 |
| Improvement in functioning (range = 0–10) | 4.41 | 2.88 | 15.4 |
| Helpfulness in the past month (range = 0–4) | 2.32 | 1.12 | 17.1 |
Ns vary due to missing data. Amount of pain relief: "On a scale of 0 to 10 where zero is no relief and 10 is complete relief, what number best describes how much pain relief you get on average after taking this medication?" Improvement in functioning: "Thinking about your ability to do day-to-day activities, on a scale of 0 to 10 where 0 is no improvement and 10 is complete return to your normal activity level, what number best describes how much your ability to function improves after taking this medication?" Helpfulness in past month: "Over the past month, how helpful have you found opiate pain medication in relieving your pain?"
"Endorsement of high helpfulness" defined as a score of 8 or higher on the pain relief and function items (0–10 scale) and a score of 4 on the helpfulness item (0–4).
Self-reported helpfulness of opioids in relieving pain over the past month (single PODS item) was positively correlated with the other helpfulness items including amount of pain relief after taking an opioid (r(76) = 0.65, P < 0.001) and functional improvement after taking an opioid (r(72) = 0.38, P < 0.001). However, helpfulness of opioids in the past month was not significantly correlated with current ratings of pain severity (r(72) = 0.05, P = 0.705) or pain interference (r(72) = 0.20, P = 0.095). Similarly, amount of pain relief after taking an opioid was not associated with current pain severity (r(77) = -0.13, P = 0.273) or pain interference (r(77) = -0.002, P = 0.989), and functional improvement after taking an opioid was not significantly correlated with current pain severity (r(73) = -0.22, P = 0.057) or pain interference (r(73) = -0.16, P = 0.174).
Associations Between Motivational Factors and Helpfulness, Pain Severity, and Functioning
Descriptive data on motivational factors is presented in Table 4. On average, patients’ desire to continue taking opioids was 4.13 (SD = 3.97), patients reported needing 71.8% pain improvement before they would consider stopping opioids, and confidence in ability to manage pain without opioids was 3.52 (SD = 3.57). Opioid users reported high interest in learning different ways of managing pain (mean = 8.56, SD = 2.61). Desire to continue taking opioids was positively associated with helpfulness of opioids in managing pain in the past month (r(73) = 0.30, P = 0.009). Additionally, desire to continue taking opioids was not associated with BPI pain severity (r(75) = 0.17, P = 0.152); however, desire to continue taking opioids was positively associated with BPI pain interference (r(75) = 0.24, P = 0.043). Confidence in ability to manage pain without opioids was negatively associated with helpfulness of opioids in managing pain in the past month (r(74) = -0.29, P = 0.013), but not significantly related to pain severity (r(72) = 0.009, P = 0.943) or pain interference (r(72) = -0.15, P = 0.212).
Table 4.
Assessment of motivational factors
| Mean | SD | |
|---|---|---|
| Desire to continue taking opioids | 4.13 | 3.97 |
| % pain improvement needed to consider stopping opioids | 71.82 | 22.57 |
| Confidence in ability to manage pain without opioids | 3.52 | 3.57 |
| Desire to learn different ways of managing pain | 8.56 | 2.61 |
1) "On a scale of 0 to 10 where 0 is no desire and 10 is full desire, which number best describes your want to continue taking an opioid for your current pain?" 2) "What % of pain improvement would you need to experience before you would consider stopping use of your opioid medication?" 3) "On a scale of 0 to 10 where 0 is not at all confident and 10 is very confident, how confident are you in your ability to manage pain without opioids?" 4) "On a scale of 0 to 10 where 0 is no desire and 10 is full desire, which number best describes your interest in learning different ways of managing pain other than opioids?"
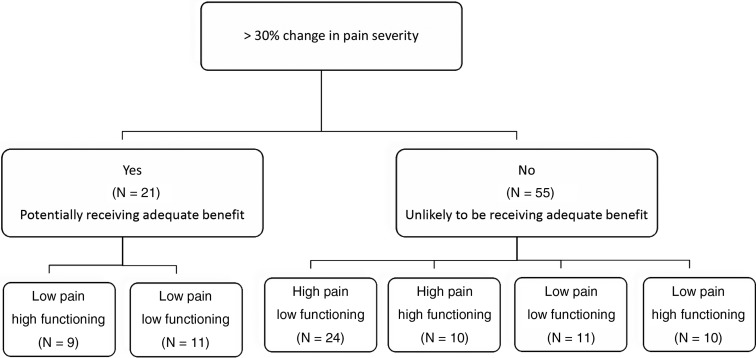
Subgroups of Opioid Users Based on the Improvement in Pain, Pain Severity, and Functioning
In accordance with the recent CDC guidelines, patients were placed into subgroups using three clinical criteria: 1) improvement in pain severity (% improvement), 2) current pain severity (BPI, 0–10 Likert scale), and 3) current pain interference scores (BPI, 0–10 Likert scale) (see Figure 1). A total of eight patients were unable to be grouped due to missing data on one or more grouping components. First, patients were grouped based on percent improvement in pain severity since starting opioids. In this sample, 55 (72.4%) patients reported less than a 30% improvement and 21 (27.6%) patients reported a 30% or greater improvement in pain severity. There was no difference between these groups on self-reported helpfulness of opioids in relieving pain over the past month (t(68) = 0.88, P = 0.384), amount of pain relief after taking an opioid (t(73) = 1.33, P = 0.189), or improvement in functioning after taking an opioid (t(69) = 0.69, P = 0.492).
Figure 1.
Subgroups of opioid users based on % improvement in pain, pain severity, and functioning.
Next, patients were further divided into subgroups based on their current pain severity and pain interference scores. Patients in the less than 30% improvement group were considered “unlikely to be receiving adequate benefit” from opioids and were categorized into the following four subgroups: 1) high pain/low functioning (N = 24): patients who scored above a 7 on pain severity and above a 7 on pain interference subgroup [19]; 2) high pain/moderate-to-high functioning (N = 10): patients who scored above a 7 on pain severity and 7 or below on pain interference; 3) low-to-moderate pain/low functioning (N = 11): patients who scored 7 or less on pain severity and above a 7 on pain interference; and 4) low-to-moderate pain/moderate-to-high functioning (N = 10): patients who scored 7 or less on pain severity and 7 or less on pain interference. The patients reporting a 30% or greater improvement in pain severity since starting opioids were considered “potentially receiving adequate benefit” from opioids and were categorized into the following two subgroups: 1) low-to-moderate pain/moderate-to-high functioning (N = 9): patients who scored 7 or less on both the pain severity and pain interference scale; and 2) low-to-moderate pain/low functioning (N = 11): patients who reported a score of 7 or less on pain severity and 7 or above on pain interference.
Discussion
In order to reduce the number of chronic pain patients maintained on long-term opioids, physicians need clinical guidelines that identify patients not benefiting from opioids. However, even when a physician recommends opioid cessation, patients may be reluctant to discontinue opioids. To our knowledge, this is one of the first studies to 1) explore barriers to opioid cessation from the perspective of the chronic pain patient and 2) use clinically meaningful indicators to identify patients likely not benefiting from opioids. This study suggests that despite clinical indicators that question the benefit, such as high pain and low functioning, patients continue to report that their opioids are helpful. Such discrepancies in patient perceptions will likely pose barriers for implementing guidelines based on objective clinical criteria in clinical practice.
Self-Reported Perceptions of Helpfulness Were not Associated with Expected Clinical Characteristics
A critical and unanswered question is how to best quantify the helpfulness of opioids. When asked, patients may report their opioid medication is helpful at relieving pain and improving functioning. It follows that self-reported helpfulness ratings should be associated with lower pain severity scores, higher physical functioning scores, and improvement in pain since starting opioids. However, counter to our hypothesis we found that helpfulness was unrelated to these important clinical features. There are several hypotheses to consider as to why helpfulness ratings may be inconsistent with the impact of opioids on pain relief and functional status. One possibility is that patients report that opioids are helpful even when there is not sufficient clinical evidence to demonstrate that opioids are in fact helping (e.g., reduced pain, improved functioning) because patients see opioids as their only treatment option or believe nonopioid options are less effective [20]. Another interpretation is that patients may inflate their pain scores because they believe a high pain score is necessary in order to demonstrate the need for opioids. To our knowledge, this hypothesis has not been tested directly. However studies have shown that the odds of being prescribed an opioid in the emergency department increase significantly with increasing levels of pain severity [21]. Finally, factors such as tolerance and dependence may influence how patients appraise helpfulness. If so, patients’ reports of helpfulness may be more related to opioids’ ability to satisfy withdrawal than pain relief [22]. In partial support of the later hypothesis, a prospective study involving medically directed opioid tapering found that patients demonstrated withdrawal hyperalgesia [23]. In summary, the data from the present study question the reliability of patient’s self-report helpfulness ratings and suggest perceptions of helpfulness are likely influenced by factors other than pain relief and improvement in functioning. Physicians should consider each patient’s subjective ratings of helpfulness in the context of other factors including clinical judgment and clear evidence of changes in pain and functioning.
Difficulties Associated with Opioid Use Were Common and Depression Was Associated with Greater Problems and Concerns About Opioid Use
In this sample, 66.3% of patients using opioids reported intermediate-to-high opioid-related difficulties on the PODS. Yet these difficulties were not associated with patients’ appraisal of helpfulness. One possibility is that difficulties (i.e., harms) and benefits (i.e., perceptions of helpfulness) are distinct constructs that patients evaluate independent of the other. That is, a patient may evaluate opioids as causing harm but still feel opioids are helpful and wish to continue use despite the risks. In support of this hypothesis, we did not find an association between opioid-related difficulties and desire to continue taking opioids. We also found that opioid users with symptoms suggestive of comorbid depression reported greater problems and concerns related to opioid use. Interestingly, depressed patients in this study did not demonstrate a stronger desire to discontinue opioids compared with nondepressed patients. Previous studies have shown that depressed patients were more likely to report conflicting attitudes toward opioid use, suggesting a greater desire to cut down opioid use [24]. In summary, interventions that aim to increase perceptions of the risks of opioid use may not simultaneously reduce desire to continue taking opioids, which may be a barrier to increasing motivation for opioid cessation.
Motivational Factors and the Implications for Cessation
Desire to continue taking an opioid was not associated with pain severity or improvement in pain since starting opioids, suggesting a need to better understand what factors influence desire to continue taking opioids. One possibility is that low confidence in ability to manage pain without opioids represents a major barrier to opioid cessation. In support of this hypothesis, patients in this study generally reported low confidence in their ability to manage pain without opioids, and lower confidence was associated with a greater desire to continue taking opioids. It follows that even though many patients may not be receiving meaningful improvements in pain and functioning from opioids, they are motivated to continue taking opioids in part because they lack strategies for managing pain without opioids. Providing patients with nonopioid evidence-based interventions for pain, such as cognitive behavior therapy, is a critical step for increasing self-efficacy for managing pain without opioids. One pivotal study of a comprehensive pain rehabilitation program for chronic pain found that patients who tapered off opioids as part of the program, which included a cognitive behavioral intervention, experienced improvements in treatment outcomes such as pain and functioning [25]. Combining opioid tapering with cognitive behavioral techniques is a promising approach for improving the success of opioid cessation. Importantly, the patients in the current study report a high interest in learning alternative strategies for managing their pain.
Evidence Supporting the Benefits of Opioids for the Treatment of Chronic Pain Is Limited
This study replicates other studies that have shown that opioid users appear phenotypically worse compared with nonopioid users [6]. As we previously reported [26], patients already taking opioids report higher pain severity, worse physical functioning, and more symptoms of depression. Additionally, 27.1% of patients in this study reported less than an hour of pain relief after taking an opioid, 36% of patients have a pain score of above 7, and 48% of patients have a pain interference score of above 7. Taken together, these findings contribute to the growing literature that questions the use of opioids for the treatment of chronic pain.
Clinical Implications
The CDC recently proposed guidelines that state, “If the benefits of opioids do not outweigh the harms and there is not sufficient evidence of sustained improvement in pain and functioning, physicians should work to taper patients to lower doses or encourage complete opioid cessation” [9,10]. While the guidelines did not set specific cut-points per se, we categorized opioid users into subgroups using clinically meaningful criteria based on change in pain severity since initiating opioids, current pain severity, and current physical functioning (see Figure 1). In our sample, 71.4% of patients reported less than a 30% reduction in pain severity since starting opioids and were classified as “unlikely to be receiving adequate benefit.” In comparison, 28.6% reported a 30% or greater improvement in pain severity and were classified as “potentially receiving adequate benefit.” Several subgroups emerged that highlight the complexity of using cut-points to define benefit. For example, among patients who reported a 30% or greater improvement in pain severity, nine patients demonstrated benefit across both pain severity and functioning. However, 11 patients reported adequate changes in pain severity but inadequate functional benefits. In the later scenario, benefit is less clear and emphasis should be placed on increasing functional goals in order to justify continued opioid use. Similarly, among patients who reported less than a 30% reduction in pain severity, we were able to clearly identify a subgroup of patients (N = 24) not deriving pain and functional benefits from opioids. In addition, several complex subgroups of patients were identified. Determining if a patient is benefiting from opioids is challenging; however, understanding where a patient falls in different categories may help physicians assess overall efficacy and identify targeted treatment goals, especially when benefit is questioned.
Operationalizing the CDC’s clinical guidelines and putting them into practice is an important first step; however, the current study suggests that many patients still report their opioids are helpful regardless of clinical indicators. This discrepancy between the clinical guidelines and patients’ beliefs will likely be a significant barrier to implementing guidelines into clinical practice. For example, a patient may report minimal improvement in pain and functioning over time, but continue to report opioids are helpful. In this clinical scenario, this patient will likely be resistant to stopping opioids because their beliefs about helpfulness do not reflect where they fall within clinical guidelines. Therefore, in order to increase motivation for opioid cessation when benefit is questioned, physicians will need to address patient-level barriers. This study highlights several potential reasons a patient may be resistant when a physician recommends tapering, including the perception that opioids are helping pain and low confidence in one’s ability to manage pain without opioids.
Strengths and Limitations
One of the strengths of this study was the prospective collection of structured interview data from a tertiary pain clinic to describe patterns of opioid use among new patients. Patients already prescribed opioids at the time of their first visit at a pain clinic pose unique challenges for the physician, and this study identified several important patient-level barriers to opioid cessation. Another strength of this study was the exploratory aim and the use of clinically meaningful cut-points for assessing the benefits of opioids, similar to what was recommended by the CDC. There are several important limitations to note. One limitation is that the item used to create the percent improvement score asked patients to recall their average pain severity prior to starting opioids. This could potentially introduce recall bias. To address concerns about bias, we asked patients the following follow-up item: “How confident are you that your answer accurately captures your pain prior to starting opioids?” (0 = not at all confident, 10 = completely confident), and the mean confidence rating was 9.19 (SD = 1.48). A second limitation is the use of several items developed by the research team to assess helpfulness and motivation. These items were developed based on theoretically important constructs but have not been validated. Another limitation is that these data were cross-sectional, which limits the causal interpretations of these results. A fourth limitation is that these data were collected with predominately Caucasian patients living in the Midwest, presenting to a specialty outpatient pain center. This limits the generalizability of these results to other patient populations and treatment settings.
Conclusions and Future Directions
Guidelines for assessing the risks and benefits of chronic opioid therapy should be implemented in all settings where patients receive opioids. For example, physicians should consistently monitor improvements (or lack of) in pain severity and physical functioning in all patients on long-term opioid therapy. When the risks exceed the benefits, opioid cessation should be initiated. However, little progress will be made toward reducing the number of patients maintained on opioids if physicians do not address the unique cessation needs of chronic pain patients. Therefore, future studies should consider adherence to guidelines for opioid prescribing in the context of chronic pain management, barriers to following guidelines, and challenges of implementing opioid cessation from the physician and patient perspectives. One long-term goal is to develop an opioid cessation intervention to help patients not benefiting from opioids taper off this medication and provide nonopioid interventions for pain management.
References
- 1. Manchikanti L. Prescription drug abuse: What is being done to address this new drug epidemic? Testimony before the Subcommittee on Criminal Justice, Drug Policy and Human Resources. Pain Physician 2006;94:287–321. [PubMed] [Google Scholar]
- 2. Manchikanti L. National drug control policy and prescription drug abuse: Facts and fallacies. Pain Physician 2007;103:399–424. [PubMed] [Google Scholar]
- 3. Paulozzi LJ, Budnitz DS, Xi YL.. Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiol Drug Safety 2006;159:618–27. [DOI] [PubMed] [Google Scholar]
- 4. Manchikanti L, Benyamin R, Datta S, Vallejo R, Smith H.. Opioids in chronic noncancer pain. Expert Rev Neurother 2010;105:775–89. [DOI] [PubMed] [Google Scholar]
- 5. Chaparro LE, Furlan AD, Deshpande A, et al. Opioids compared to placebo or other treatments for chronic low-back pain. Cochrane Database Syst Rev 2013;8:CD004959.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Eriksen J, Sjogren P, Bruera E, Ekholm O, Rasmussen NK.. Critical issues on opioids in chronic non-cancer pain: An epidemiological study. Pain 2006;125(1–2):172–9. [DOI] [PubMed] [Google Scholar]
- 7. Martell BA, O'Connor PG, Kerns RD, et al. Systematic review: Opioid treatment for chronic back pain: Prevalence, efficacy, and association with addiction. Ann Intern Med 2007;1462:116–27. [DOI] [PubMed] [Google Scholar]
- 8. Noble M, Tregear SJ, Treadwell JR, Schoelles K.. Long-term opioid therapy for chronic noncancer pain: A systematic review and meta-analysis of efficacy and safety. J Pain Symptom Manage 2008;352:214–28. [DOI] [PubMed] [Google Scholar]
- 9. Frieden TR, Houry D.. Reducing the risks of relief–The CDC opioid-prescribing guideline. N Engl J Med 2016;37416:1501–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dowell D, Haegerich TM, Chou R.. CDC guideline for prescribing opioids for chronic pain—United States, 2016. MMWR Recomm Rep 2016;651:1–49. [DOI] [PubMed] [Google Scholar]
- 11. Sullivan MD, Von Korff M, Banta-Green C, Merrill JO, Saunders K.. Problems and concerns of patients receiving chronic opioid therapy for chronic non-cancer pain. Pain 2010;1492:345–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. McMaffery M, Pasero C.. Pain: Clinical Manual, 2 ed St. Louis, MO: Mosby, Inc; 1999. [Google Scholar]
- 13. Farrar JT, Young JP Jr., LaMoreaux L, Werth JL, Poole RM.. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2000;942:149–58. [DOI] [PubMed] [Google Scholar]
- 14. Banta-Green CJ, Von Korff M, Sullivan MD, et al. The prescribed opioids difficulties scale: A patient-centered assessment of problems and concerns. Clin J Pain 2010;266:489–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hassett AL, Wasserman R, Goesling J, et al. Longitudinal assessment of pain outcomes in the clinical setting: Development of the “APOLO” electronic data capture system. Reg Anesth Pain Med 2012;374:398–402. [DOI] [PubMed] [Google Scholar]
- 16. Cleeland CS, Ryan KM.. Pain assessment: Global use of the brief pain inventory. Ann Acad Med Singapore 1994;232:129–38. [PubMed] [Google Scholar]
- 17. Zigmond AS, Snaith RP.. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361–70. [DOI] [PubMed] [Google Scholar]
- 18. StataCorp. Stata Statistical Software: Release 13. College Station, TX; 2013. [Google Scholar]
- 19. Wasserman RA, Brummett CM, Goesling J, Tsodikov A, Hassett AL.. Characteristics of chronic pain patients who take opioids and persistently report high pain intensity. Reg Anesth Pain Med 2014;391:13–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Frank JW, Levy C, Matlock DD, et al. Patients’ perspectives on tapering of chronic opioid therapy: A qualitative study. Pain Med 2016;171:1838–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Iyer GR. Pain documentation and predictors of analgesic prescribing for elderly patients during emergency department visits. J Pain Symptom Manage 2011;412:367–72. [DOI] [PubMed] [Google Scholar]
- 22. Rosenblum A, Marsch LA, Joseph H, Portenoy RK.. Opioids and the treatment of chronic pain: Controversies, current status, and future directions. Exp Clin Psychopharmacol 2008;165:405–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hooten WM, Mantilla CB, Sandroni P, Townsend CO.. Associations between heat pain perception and opioid dose among patients with chronic pain undergoing opioid tapering. Pain Med 2010;11:1587–98. [DOI] [PubMed] [Google Scholar]
- 24. Howe CQ, Sullivan MD, Saunders KW, et al. Depression and ambivalence toward chronic opioid therapy for chronic noncancer pain. Clin J Pain 2012;287:561–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Townsend CO, Kerkvliet JL, Bruce BK, et al. A longitudinal study on the efficacy of a comprehensive pain rehabilitation program with opioid withdrawal: Comparison of treatment outcomes based on opioid use at admission. Pain 2008;1401:177–89. [DOI] [PubMed] [Google Scholar]
- 26. Goesling J, Henry MJ, Moser SE, et al. Symptoms of depression are associated with opioid use regardless of pain severity and physical functioning among treatment-seeking patients with chronic pain. J Pain 2015;169:844–51. [DOI] [PubMed] [Google Scholar]