Abstract
Obesity and excess weight are significant clinical and public health issues that disproportionately affect African Americans because of physical inactivity and unhealthy eating. We compared the effects of alternate behavioral interventions on obesity-related health behaviors. We conducted a comparative effectiveness education trial in a community-based sample of 530 adult African Americans. Outcomes variables were physical activity (PA) and fruit and vegetable intake. Outcomes were evaluated at baseline and 1-month following interventions about shared risk factors for cancer and cardiovascular disease (CVD) (integrated, INT) or CVD only (disease-specific). Significant increases were found in the proportion of participants who met PA guidelines from baseline (47.4%) to follow-up (52.4%) (P = 0.005). In the stratified analysis that were conducted to examine interaction between education and intervention group assignment, this effect was most apparent among participants who had ≤high school education and were randomized to INT (OR = 2.28, 95% CI = 1.04, 5.00, P = 0.04). Completing the intervention was associated with a 1.78 odds of meeting PA guidelines (95% CI = 1.02, 3.10, P = 0.04). Education about risk factors for chronic disease and evidence-based strategies for health behavior change may be useful for addressing obesity-related behaviors among African Americans.
Introduction
Obesity and excess weight are significant clinical and public health issues that are due in part to physical inactivity and unhealthy eating. Disparities or differences in physical activity (PA) and fruit and vegetable (FV) intake among African Americans are due to environmental resources (e.g. access to grocery stores, parks and recreation centers) and whether individuals have the motivation, confidence, and skills to perform these behaviors [1–4]. These behaviors play a role in the high rates of obesity and being overweight among African Americans [5]. Previous interventions for obesity reduction and prevention have included randomized trials of weight loss programs [6] and interventions designed to improve PA [7–10] and dietary behaviors [11–13] through improved knowledge about recommendations for PA and healthy diets [14, 15]. Motivational interviewing has also been used to enhance FV intake and PA among African American members of churches [16]. But, the results of these interventions have been mixed; African Americans have low rates of meeting guidelines for PA and FV consumption [17].
Community-based participatory research (CBPR) can play an important role in addressing obesity-related behaviors by developing interventions that address community priorities and resources collaboratively with stakeholders. Consistent with this approach, we first conducted a multilevel needs assessment with African American residents in the Philadelphia, PA metropolitan area and found that community members were concerned about chronic health conditions such as cardiovascular disease (CVD) and cancer and wanted greater education about obesity reduction and prevention through lifestyle modification and health behavior change [18]. Next, we used developed an integrated approach for providing education about risk factors for chronic diseases to address the priorities identified by community residents as part of a pilot study [20]. As part of this quasi-experimental study, participants received education about the overlap in risk factors for cancer and CVD and used techniques from motivational interviewing were used to improve self-efficacy for diet and PA. Integrated risk factor education led to significant increases in confidence to make behavioral changes in our pilot quasi-experimental design [20]. To further inform the development of an intervention that addressed community priorities, we also examined barriers and facilitators to PA and FV intake in a community-based sample of African Americans who were recruited from the Philadelphia, PA metropolitan area. As in other reports [1], participants did not meet recommended guidelines for PA and FV intake, but socioeconomic factors were not associated significantly with these behaviors. Collective efficacy, or social cohesion was only associated significantly with fruit intake whereas dietary self-efficacy was associated significantly with both FV intake [19]. None of the socioeconomic, social environment or psychological variables were associated significantly with PA. On the basis of these findings, we focused on further developing the integrated risk education (INT) protocol.
An integrated approach is based on an ecological model of health that emphasizes multiple types of determinants that operate at individual and community levels [21]; in this study, we conceptualized integration in terms of the disease foci because of the priorities and concerns that were identified by community residents in our needs assessment [18]. Moreover, interventions that are integrated in terms of disease foci are consistent with a primary care model of health behavior in which health care providers deliver counseling or advice about multiple health behaviors to patients [22]. An integrated approach may be more effective in terms of increasing dietary behaviors and PA than a disease specific strategy because education that is integrated in terms of disease foci may address literacy challenges and also help individuals to make the connection between the similarities in risk factors for cancer and CVD. As a result, individuals may be more likely to make changes in their health behavior, especially if skills training is provided. However, our previous quasi-experimental design did not allow us to compare the effects of INT to other approaches.
The purpose of this study was to compare the effects of INT versus disease specific education (DSE) on changes in obesity-related behaviors in a comparative effectiveness education randomized trial among African Americans. Both intervention arms were developed using the Health Belief Model and principles of motivational interviewing as theoretical and methodological guides [23, 24]. We chose to address CVD as part of the DSE because of the high rates of risk factors for this condition in the African American community. Further, greater education was identified as a priority among community residents [18]; we wanted to ensure that residents would have access to education about strategies for health promotion and disease prevention, regardless of their randomization to INT or DSE. We focused on changes in diet and PA rather than weight loss because these behaviors are important to obesity and community residents expressed a strong preference for educational interventions that emphasized lifestyle behavior change [18]. We hypothesized that INT, which focused on shared risk factors for cancer and CVD, would lead to greater changes in meeting guidelines for PA and FV intake compared with DSE about CVD only.
Materials and methods
Design overview
Participants were randomized to INT or DSE following self-referral from community-based recruitment mechanisms [25]. Eligible individuals completed a structured baseline telephone interview after providing verbal informed consent. At the end of the baseline, participants were invited to participate in a lifestyle behavior intervention; those who agreed were randomly assigned to either DSE or INT. Random intervention assignments were completed by a data manager at the University of Pennsylvania who was not involved in collecting study data. Study investigators were blinded to the participant’s randomization; randomization and the dataset were prepared for statistical analysis by the data manager. This study was approved by the Institutional Review Boards (IRB) at the University of Pennsylvania and the Medical University of South Carolina (MUSC). The MUSC IRB approved this study after the PI (CHH) moved to this institution in 2012.
Setting and participants
Participants were adults who self-identified as being African American, were ages 18–75, and resided in the Philadelphia, PA metropolitan area. Participants were recruited through self-referrals from newspaper advertisements and flyers that were distributed in community settings. Residency was determined by self-report using zip code. Individuals who had a personal history of cancer and those who self-reported having a cardiovascular event (e.g. heart attack, stroke or heart disease) were ineligible. We also excluded individuals who had an eating disorder and those enrolled in a commercial weight loss program. Participants were recruited from September 2009 to August 2012.
Randomization and intervention
Because of the high rates of hypertension and diabetes, these conditions were used as blocking factors for the random group assignment process to ensure that participants with hypertension and/or diabetes were balanced across interventions. Specifically, separate random assignment lists were created for participants with hypertension and diabetes, hypertension only, diabetes only and neither diabetes nor hypertension to ensure balance among participants with either condition across INT and DSE. Personal history of hypertension and/or diabetes was determined by self-report during the baseline telephone interview. Socioeconomic factors (e.g. gender, age, marital status, education, employment and income) were also obtained during the baseline by self-report using items from our previous research [18]. We also used the CDC formula to calculate body mass index (BMI) using self-reported height and weight.
Detailed information about the delivery and content of the interventions has been reported previously and is summarized here [26]. Both intervention arms were developed by community partners with input from the entire partnership [18]. INT and DSE consisted of four semi-structured sessions that were delivered in a group format and lasted ∼1�–2 h. Intervention sessions were delivered once per week over a 4-week period by two Master’s levels health educators. Intervention sessions were delivered weekly at a university office to maximize engagement with study participants and enhance completion of sessions because it was centrally located and accessible through multiple modes of public transportation. The INT and DSE protocols included four sessions and brief measures of study outcomes to facilitate dissemination to primary care and community organizations and retention among study participants. The intervention protocols targeted risk factors for cancer and CVD because these conditions were identified as priorities among community residents [8] and there continues to be racial disparities in clinical outcomes and behavioral risk factors for these diseases [1, 27, 28]. INT and DSE sessions focused on: (i) risk factors for disease, (ii) dietary behaviors, (iii) PA and (iv) post-intervention action planning. Specifically, session one focused on shared risk factors of cancer/CVD or CVD only and introduced tools for making dietary changes and increasing PA. Session one included a values clarification exercise from motivational interviewing during which participants were asked to identify values or traits that are important to them and to describe the connection they see between these values and their diet and PA. Participants were then asked to identify health behaviors they want to change, describe barriers and facilitators to making these changes and determine how changing or not changing these behaviors would impact their values. This method has been used in previous interventions that used motivational interviewing to promote diet and PA changes among African Americans [17]. Session two focused on understanding the link between dietary behaviors and cancer/CVD or CVD only, the importance of increasing FV intake and evidence-based strategies (e.g. menu planning, food diaries) for making dietary changes. Session three focused on understanding the link between PA and cancer/CVD or CVD only, the difference between usual and structured activity, barriers to PA and evidence-based strategies for being more physically active. Specifically, participants were given guidance on how to start a walking program and ways to incorporate PA into their lifestyle by exercising in shorter bouts. Session four reviewed the information from previous sessions and also addressed action planning and problem solving for participants to strategize about ways to stay motivated while trying to reach or maintain their goals after the intervention. In addition to the values clarification exercise that was completed during the first group session, the confidence and motivation rating techniques from motivational interviewing were incorporated into each group session. Our decision to incorporate these specific techniques was made to increase the dissemination potential of the INT and DSE protocols to community-based organizations. Health educators received video and in-person training in these motivational interviewing techniques. We monitored intervention fidelity (e.g. performance of motivational interviewing techniques) using several techniques that included randomly audio taping sessions to ensure that the intervention contents were being delivered according to the protocols. Intervention sessions were also observed by research staff while they were being conducted and compliance was monitored using a protocol checklist. Participants were given $35/session to reimburse them for travel and other expenses associated with attending intervention sessions.
Outcomes and follow-up
Our primary outcomes were FV intake and PA. We evaluated the effects of INT versus DSE on changes in the percentage of participants who met guidelines for each of these behaviors. We used items from the Health Information National Trends Survey (HINTS) to evaluate FV intake and PA [29]. Specifically, participants were asked how many cups of FVs they eat each day (1 = none/don’t know to 7 = more than four cups). Participants who reported eating at least 2–3 cups were categorized as meeting guidelines for each variable.
We used items and methods from the HINTS to measure PA. First, participants were read a description of moderate PA and then asked if they had participated in any PA or exercise during the past month (e.g. moderate intensity activities make you breathe somewhat harder than normal. In a typical week, how many days do you do any PA or exercise of at least moderate intensity, such as brisk walking, bicycling at a regular pace, swimming at a regular pace and heavy gardening). Those who reported PA were asked how many days they do any PA/exercise of at least moderate intensity and on these days, how long they typically perform these behaviors. We calculated the total number of minutes for moderate intensity PA per week and categorized participants as having met guidelines (≥150 min per week) or as not having met guidelines (<150 min per week/no PA) for moderate intensity PA [30].
We evaluated study outcomes 1-month following intervention completion. For those who did not complete all four sessions (n = 141), this follow-up was completed 1-month after the last session they completed or was scheduled to be completed. For those who did not complete all intervention sessions, the follow-up was conducted one month after the last intervention date was scheduled to be completed. Study outcomes were evaluated at 1-month because we wanted to first determine if INT and DSE had different effects on making an initial attempt to make changes in obesity-related lifestyle behaviors. Evaluating short-term effects is consistent with established models of intervention evaluation [31]. Participants were not given a financial incentive for completing the follow-up because these resources were used to enhance completion of intervention sessions that required travel to the study site.
Statistical analysis
We based our sample size estimates on the effect sizes that were observed for behavioral changes in similar types of interventions evaluated in other studies [16]. Power calculations were based on two-sample t-tests for effect sizes as determined by differences in outcomes measured at follow-up and baseline in each intervention group, properly adjusting for the within-subject correlations (rho = 0.3) in pre- and post-intervention measures. All power and sample size estimates were constructed at the alpha = 0.05 level for two-sided tests of the null hypotheses using formulations proposed by Donner and Klar [32]. On the basis of previous studies, we anticipated that the INT intervention would have a small effect (Cohen’s D = 0.2) on changes in FV intake and PA compared with DSE and estimated that we would need to enroll and randomize 425 participants per intervention group to detect clinically meaningful differences between groups with 80% power, assuming 30% attrition over the planned 12-month follow-up period.
We analyzed study data by first generating descriptive statistics to characterize the sample in terms of follow-up retention, socioeconomics, BMI and obesity-related behaviors. To evaluate the effects of INT versus DSE on changes in PA and FV intake, we used McNemar tests to compare changes in the percentage of participants who met guidelines for each behavioral outcome overall and stratified by intervention group. We used an intent-to-treat approach for these analyses, including all randomized participants regardless of whether they completed the intervention and follow-up. For participants with no data available at follow-up, we assumed no change from baseline in the intent-to-treat analyses. In a sensitivity analysis, we performed the same analysis with only participants who completed at least the first intervention session and follow-up.
Results
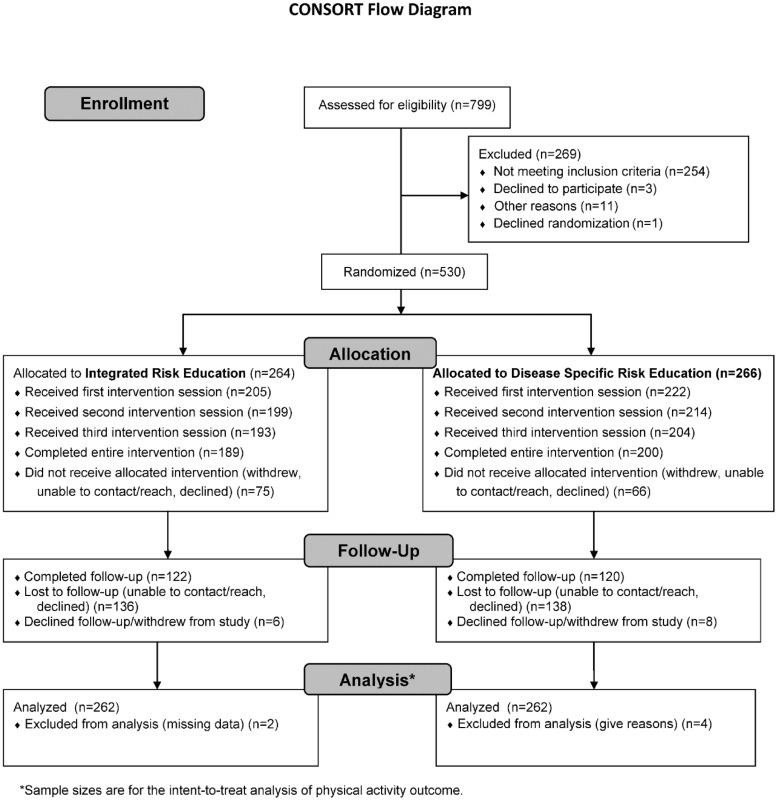
Figure 1 shows the flow of participants through the study. 73% of participants completed all four intervention sessions and 80% completed the first session during which shared risk factors for cancer/CVD or CVD only were addressed and the values clarification exercise was completed. There were no differences in intervention completion based on socioeconomics and intervention groups did not differ significantly in terms of meeting guidelines for PA and FV intake at baseline (Table I). Overall, 46% of participants were retained at follow-up; participants with fewer socioeconomic resources (e.g. lower income, unemployed) and those who were younger in age were less likely to be retained. Among the participants who were lost to follow-up, only ten declined and ten withdrew from the study. The primary reason for being lost to follow-up was because participants could not be reached. There were no differences in follow-up retention based on randomization to INT or DSE (P = 0.80).
Fig. 1.
Flow of study participants.
Table I.
Subject characteristics (n = 530)a
| Variable | Total | INT | DSE | Chi square |
|---|---|---|---|---|
| Age, mean � SD | 48.2, 10.7 | 47.3, 10.8 | 49, 10.5 | 1.82(t) |
| Female gender, n (%) | 303 (57%) | 163 (62%) | 140 (53%) | 4.49* |
| Marrieda, n (%) | 62 (12%) | 27 (10%) | 35 (13%) | 1.07 |
| ≥ Some college educationa, n (%) | 260 (49%) | 129 (49%) | 131 (49%) | 0.01 |
| Employed, n (%) | 177 (34%) | 92 (35%) | 85 (32%) | 0.42 |
| Income > $20 000a, n (%) | 237 (48%) | 114 (47%) | 123 (49%) | 0.18 |
| Insured, n (%) | 414 (78%) | 204 (78%) | 210 (79%) | 0.15 |
| Doctor’s office for medical carea, n (%) | 363 (69%) | 184 (70%) | 179 (67%) | 0.44 |
| Body mass index, mean � SD | 29.9, 6.6 | 30.1, 6.8 | 29.7, 6.4 | −0.79(t) |
| Diabetes, n (%) | 55 (10%) | 26 (10%) | 29 (11%) | 0.16 |
| Hypertension, n (%) | 159 (30%) | 80 (30%) | 79 (30%) | 0.02 |
n does not equal 530 because participants declined to provide data.
P < 0.05; (t) = T-value.
In our intent-to-treat analysis using the total sample, there were significant increases in the proportion of participants who met PA guidelines. At baseline, 47.4% met PA guidelines and 52.4% met these guidelines at follow-up (McNemar = 8.05, P = 0.005). We repeated this analysis stratified by intervention group; only those randomized to INT reported significant increases in meeting PA guidelines (see Table II). There was also a marginal, but non-significant increase in meeting PA guidelines among participants randomized to DSE (see Table II). Since there was post-randomization attrition, we conducted a sensitivity analysis to determine if the changes observed in PA were due to exposure to the intervention. As in our intent-to-treat analyses, there were significant increases in meeting PA guidelines from baseline to follow-up overall (49.1% versus 61.8%, McNemar = 9.72, P = 0.002) and among participants who received INT (43.4% versus 58.5%, McNemar = 7.11, P = 0.001). There were also marginal increases in the PA guidelines among participants who received DSE (54.7% versus 65.1%, McNemar = 3.10, P = 0.08). The absolute changes in PA from baseline to follow-up by intervention group are provided in Table II.
Table II.
Changes in physical activity and fruit and vegetable intake by intervention group
| Variable | Integrated risk education | Disease specific risk education | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Follow-up | Absolute change | McNemar chi square, P-value | Baseline | Follow-up | Absolute change | McNemar chi square, P-value | |
| Physical activity | ||||||||
| Intent-to-treat | 46.2% | 52.3% | 6.1 | 6.4 | 48.7% | 52.5% | 3.8 | 2.27 |
| P = 0.01 | P = 0.13 | |||||||
| Sensitivity | 43.4% | 58.5% | 15.1 | 7.1 | 54.7% | 65.1% | 10.4 | 3.10 |
| P = 0.01 | P = 0.08 | |||||||
| Fruit intake | ||||||||
| Intent-to-treat | 36.2% | 41.2% | 5.0 | 3.78 | 33.2% | 34.8% | 1.6 | 0.38 |
| P = 0.05 | P = 0.54 | |||||||
| Sensitivity | 41% | 51.4% | 10.4 | 3.10 | 38% | 40% | 2.0 | 0.10 |
| P = 0.08 | P = 0.75 | |||||||
| Vegetable intake | ||||||||
| Intent-to-treat | 36.3% | 37.1% | 0.8 | 0.10 | 32.4% | 34.4% | 2.0 | 0.64 |
| P = 0.75 | P = 0.75 | |||||||
| Sensitivity | 37.1% | 43.8% | 6.7 | 1.48 | 38.9% | 42.6% | 3.7 | 0.44 |
| P = 0.22 | P = 0.50 | |||||||
The results of the logistic regression analysis for PA are provided in Table III. This model used an intent-to-treat approach and controlled for baseline PA, factors that were imbalanced between intervention groups, and those associated significantly with follow-up retention. Higher education was positively associated with meeting guidelines (OR = 2.18, 95% CI = 1.29, 3.63, P = 0.004). Participants who had ≥some college education had about twice the odds of meeting PA guidelines compared with those with less education. The OR for intervention group indicated an equal likelihood of there being an increase in meeting PA guidelines in INT and DSE. But, completing all four intervention sessions, regardless of intervention group, had a significant association with meeting PA guidelines (OR = 1.78, 95% CI = 1.02, 3.10, P = 0.04). Since risk education was the primary focus of the intervention, we evaluated the interaction between education and intervention group in an exploratory analysis; this interaction was statistically significant (P = 0.03). To interpret this interaction, we re-ran the model stratified based on education. Among participants who had ≥some college, those who completed all four intervention sessions had about twice the odds of meeting PA guidelines compared with those who did not complete the intervention (OR = 2.43, 95% CI = 1.13, 5.23, P = 0.02). Intervention group did not have a significant effect on the odds of meeting PA guidelines among participants who had ≥some college. But, among participants who had ≤high school education, those randomized to INT had about twice the odds of meeting PA guidelines compared with those randomized to DSE (OR = 2.28, 95% CI = 1.04, 5.00, P = 0.04).
Table III.
Multivariate logistic regression analysis of physical activity
| Variable | Level | Odds ratio | 95% confidence interval | P-value |
|---|---|---|---|---|
| Baseline physical activity | Met guidelines | 35.6 | 20.9, 60.7 | 0.0001 |
| Did not meet guidelines | ||||
| Gender | Female | 0.72 | 0.44, 1.25 | 0.26 |
| Male | ||||
| Study group | Integrated risk education | 1.24 | 0.76, 2.02 | 0.39 |
| Disease specific risk education | ||||
| Age | a | 1.06 | 0.82, 1.36 | 0.64 |
| Marital status | Married | 0.94 | 0.44, 2.02 | 0.87 |
| Not married | ||||
| Education level | ≥ Some college | 2.18 | 1.29, 3.67 | 0.004 |
| ≤ High school | ||||
| Employment status | Employed | 0.90 | 0.53, 1.55 | 0.71 |
| Not employed | ||||
| Body mass index | a | 1.10 | 0.86, 1.40 | 0.46 |
| Chronic disease | Yes | 0.68 | 0.31, 1.50 | 0.34 |
| No | ||||
| Intervention completion | Completed | 1.78 | 1.02, 3.10 | 0.04 |
| Not completed |
ORs for continuous variables reflect the OR for a 1-SD unit change in the covariate.
There were also changes in FV intake from baseline to follow-up in the intent-to-treat analysis. At baseline, 34.6% of participants met fruit intake guidelines and 37.8% met this guideline at follow-up McNemar = 3.32, P = 0.07). Similarly, 34.2% and 35.6% of participants met vegetable intake guidelines at baseline and at follow-up, respectively (McNemar = 0.62, P = 0.43). Since the overall changes in meeting guidelines for FV intake were not statistically significant, we did not generate a multivariate logistic regression model for these outcomes.
Discussion
In this study, we compared the effects of alternate strategies for providing education about risk factors for two chronic diseases on changes in obesity-related lifestyle behaviors in a community-based sample of African Americans. African Americans have high rates of obesity and excess body weight and are at increased risk for developing CVD and experiencing morbidity and mortality from cancer [2, 27, 28]. Education is important for activating patients and community members to be more engaged in disease prevention and health promotion and is critical for self-management of chronic conditions. Previous research has shown that greater knowledge about nutrition is associated with increased weight loss among obese and overweight low-income mothers [33]. Further, African American women who received education only reported significant decreases in overall energy intake and percent energy from fat [34] and PA behaviors in women who received education only was similar to those reported in women who received education plus PA training [8]. Other research has shown that individuals with greater knowledge about risk factors for CVD reported lower BMI [35]. Our research has a number of strengths that include using a CBPR approach to develop, implement and evaluate intervention protocols. This approach enabled us to develop education protocols that addressed the priorities and concerns of community residents. Consistent with CBPR principles and national priorities for chronic disease prevention and health promotion [36, 37], we used evidence-based strategies to deliver risk education and motivate health behavior change and designed our protocols and procedures to enhance the likelihood of dissemination and implementation in other settings. For instance, both intervention protocols included four sessions to enhance retention among study participants and brief validated measures were used to evaluate study outcomes by self-report. An additional strength is that the majority of participants completed the interventions. This may be due to providing a financial incentive. Since this approach may not be replicable in practice, future research should determine if intervention completion rates are lower when incentives are not provided.
Several other potential limitations should also be considered. First, we evaluated short-term changes in PA and FV intake using self-report dichotomous variables. Relatedly, we did not include objective measures of PA or FV. This approach may not be sensitive to behavioral change. While this decision was made to increase the dissemination and implementation potential of the interventions, it is important for long-term outcomes to be evaluated using objective measures in future studies. To minimize the possibility of under- and over-estimation of diet and PA, we used measures that are administered in national surveys to monitor these behaviors in population-based samples. An additional limitation is that our follow-up retention rates were modest and we did not reach our planned accrual goal. Our retention rates may have been low because we did not provide a financial incentive for completing follow-ups. We used our financial resources for incentives to enhance completion of intervention sessions because participants were required to travel to the study site. With respect to study enrollment, of the individuals who were self-referred and were screened for eligibility, 32% did not meet the inclusion criteria; not meeting this criterion was the most common factor for individuals being excluded from study participation. The challenges associated with recruiting and retaining African Americans in research because of distrust and lack of knowledge and opportunity to participate are well-documented [38–40]. Importantly, however, very few participants declined to complete the follow-up or withdrew from the study; there were no differences in follow-up retention based on randomization to intervention groups. The majority of our sample was unemployed and had low incomes; these economic issues are likely to have played a role in our retention rates.
Overall, there were significant increases in meeting PA guidelines; this effect was most evident in the sensitivity analyses. There was a 15.1 increase in the proportion of participants who met PA guidelines from baseline to follow-up among those randomized to INT. But, there was also 10.4 increase in PA among those randomized to DSE. This may have been because both interventions provided education about how to increase PA through strategies such as starting a walking a program, incorporating PA into daily routines and exercising in short bouts. Since both intervention groups had large increases in meeting PA guidelines, there were small absolute differences between intervention groups and the effect for intervention was equivalent in the multivariate logistic regression model in our intent-to-treat analysis. This is probably because the DSE protocol provided information that was relevant and meaningful to participants: 30% had hypertension, 10% had diabetes, and the average BMI was at the clinical criteria for obesity. Hypertension, diabetes and obesity are established risk factors for CVD. We may have observed a more pronounced effect for INT if we had used an education protocol that was not relevant to the prevention needs of participants as the comparison intervention. Although the regression analysis did not support our hypotheses, our findings are meaningful and important from a public health and clinical perspective because they show that two types of brief educational interventions can lead to increased levels of PA in a population that has high rates of physical inactivity and obesity [1, 2]. The PA rates we observed at follow-up were higher than those observed in national samples of African Americans [1].
We did not find significant increases in the rates of meeting guidelines for FV intake; there are a number of potential explanations for this. It could be that individuals can only make one behavioral change at a time; for this reason, are likely to start with those that are easiest to make. However, other studies have shown that African American members of religious organizations are able to make changes to their FV intake and PA simultaneously [17]. Our findings may differ from previous research because of the nature of our sample (e.g. general community sample) and the focus of our intervention. Nevertheless, it may have been easier for subjects to implement the PA strategies (e.g. starting a walking program, exercising in 10-min bouts) that were addressed in the interventions because they were low cost and required less cognitive capacity to implement. African Americans have several health literacy challenges [41]; this may impact their ability to read and understand food labels and keep track of and plan meals using structured forms. This explanation is consistent with our finding that participants who had ≥some college were about twice as likely to meet PA guidelines compared with those with fewer years of education and why the interaction between education and intervention group was significant. Further analysis of this interaction revealed that among participants who had ≤high school education, those who were randomized to INT were about twice as likely as those randomized to DSE to meet PA guidelines. A goal of INT was to help participants to see the connection between risk factors for cancer and CVD. Individuals with limited education may be likely to also have health literacy challenges [42]; this may explain why explicit efforts to show the relationship between risk factors for chronic disease had beneficial effects among participants with a high school or less education. Another possible explanation for the lack of significant change in FV intake is because of the high unemployment rates and low incomes of our study population. Financial strain has been associated with cancer risk behaviors among African Americans [43].
Even though the effect for intervention group was not significant in the logistic regression analysis, completing the intervention was associated with a 1.78 odds of meeting PA guidelines. This finding further supports the benefits of both of the interventions we developed, especially when they are completed in their entirety. Nevertheless, additional research is needed to understand the extent to which individuals are able to cognitively process and understand risk factor information and recommendations for lifestyle behavior change that are provided as part of multi-component and multi-session health promotion interventions. Future research should also determine the behavior change strategies that participants use after a lifestyle intervention and examine the effects of health literacy on behavioral outcomes in health promotion interventions. Lastly, dissemination and implementation studies are needed to determine if the interventions we designed specifically for this purpose can be delivered in diverse clinical and public health settings. As part of this, it is important to determine if our interventions can be delivered by community members in clinical and community settings (e.g. diabetes centers and clinics) and to understand the ways in which CBPR can be used to increase the applicability of health promotion interventions. If our interventions can be implemented in other settings with fidelity, then providers would have an additional evidence-based referral resource for patients. This is important because education and counseling for lifestyle and health behavior change among adults who are overweight or obese and have CVD risk factors has a Grade B Recommendation from the US Preventive Task Services Force (USPTSF) [44], but providers have a limited amount of time to address these issues during clinical visits. A Grade B recommendation is a service that is recommended by the USPTSF because there is some certainty that the net benefits to patients is moderate. Similarly, public health providers would have an additional resource for offering an evidence-based approach for health promotion and disease prevention to members of a population that is at risk for obesity and excess weight.
Acknowledgements
This research was supported by National Institute of Minority Health and Health Disparities grant #R24MD001594, National Cancer Institute grant #R01CA132656, grant #R18HS019339 from the Agency for Healthcare Research and Quality, and the Charleston Health Equity and Rural Outreach Innovation Center (grant #CIN 13-410) at the Ralph H. Johnson Veteran’s Administration Medical Center. The funders of this study did not play role in implementing the research, evaluating outcomes or manuscript preparation. We would like to acknowledge Aliya Collier, BA for assistance with data management, Stacey Brown, MSW for conducted risk education sessions, and Brenda Bryant, BA for assistance with project coordination. We are grateful to all of the men and women who participated in this research.
Trial Registration: NCT01299883.
Conflict of interest statement
None declared.
References
- 1. Corral I, Landrine H, Hao Y. et al. Residential segregation, health behavior and overweight/obesity among a national sample of African American adults. J Health Psychol 2012; 17: 371–8. [DOI] [PubMed] [Google Scholar]
- 2. Grigsby-Toussaint DS, Zenk SN, Odoms-Young A. et al. Availability of commonly consumed and culturally specific fruits and vegetables in African-American and Latino neighborhoods. J Am Diet Assoc 2010; 110: 746–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shaikh AR, Vinokur AD, Yaroch AL. et al. Direct and mediated effects of two theoretically based interventions to increase consumption of fruits and vegetables in the Healthy Body Healthy Spirit trial. Health Educ Behav 2011; 38: 492–01. [DOI] [PubMed] [Google Scholar]
- 4. Zenk SN, Odoms-Young AM, Dallas C. et al. “You have to hunt for the fruits, the vegetables”: environmental barriers and adaptive strategies to acquire food in a low-income African American neighborhood. Health Educ Behav 2011; 38: 282–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ogden CL, Carroll MD, Kit BK. et al. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014; 311: 806–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mayer-Davis EJ, D'Antonio AM, Smith SM. et al. Pounds off with empowerment (POWER): a clinical trial of weight management strategies for black and white adults with diabetes who live in medically underserved rural communities. Am J Public Health 2004; 94: 1736–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Yancey AK, McCarthy WJ, Harrison GG. et al. Challenges in improving fitness: results of a community-based, randomized, controlled lifestyle change intervention. J Women Health 2006; 15: 412–29. [DOI] [PubMed] [Google Scholar]
- 8. Agurs-Collins TD, Kumanyika SK, Ten Have TR. et al. A randomized controlled trial of weight reduction and exercise for diabetes management in older African-American subjects. Diabetes Care 1997; 20: 1503–11. [DOI] [PubMed] [Google Scholar]
- 9. Will JC, Farris RP, Sanders CG. et al. Health promotion interventions for disadvantaged women: overview of the WISEWOMAN projects. J Womens Health 2004; 13: 484–502. [DOI] [PubMed] [Google Scholar]
- 10. Kumanyika SK, Charleston JB.. Lose weight and win: a church-based weight loss program for blood pressure control among black women. Patient Educ Couns 1992; 19: 19–32. [DOI] [PubMed] [Google Scholar]
- 11. Buller D, Morrill C, Taren D. et al. Randomized trial testing the effect of peer education at increasing fruit and vegetable intake. J Natl Cancer Inst 1999; 91: 1491–500. [DOI] [PubMed] [Google Scholar]
- 12. Resnicow K, Campbell MK, Carr C. et al. Body and soul. A dietary intervention conducted through African-American churches. Am J Prev Med 2004; 27: 97–105. [DOI] [PubMed] [Google Scholar]
- 13. Resnicow K, Jackson A, Blissett D. et al. Results of the healthy body healthy spirit trial. Health Psychol 2005; 24: 339–48. [DOI] [PubMed] [Google Scholar]
- 14. Stolley MR, Fitzgibbon ML.. Effects of an obesity prevention program on the eating behavior of African American mothers and daughters. Health Educ Behav 1997; 24: 152–64. [DOI] [PubMed] [Google Scholar]
- 15. Baranowski T, Simons-Morton B, Hooks P. et al. A center-based program for exercise change among black-American families. Health Educ Q 1990; 17: 179–96. [DOI] [PubMed] [Google Scholar]
- 16. Centers for Disease Control and Prevention/National Center for Health Statistics. National Health Interview Survey Data on Exercise or Physical Activity Available at: http://www.cdc.gov/nchs/fastats/exercise.htm.
- 17. Resnicow K, Jackson A, Wang T. et al. A motivational interviewing intervention to increase fruit and vegetable intake through Black churches: results of the Eat for Life trial. Am J Public Health 2001; 91: 1686–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Weathers B, Barg FK, Bowman M. et al. Using a mixed-methods approach to identify health concerns in an African American community. Am J Public Health 2011; 101: 2087–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Halbert CH, Bellamy SL, Briggs V. et al. Collective efficacy and obesity-related health behaviors in a community sample of African Americans. J Community Health 2014; 39: 124–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Halbert CH, Bellamy S, Bowman M. et al. Effects of integrated risk counseling for cancer and cardiovascular disease in African Americans. J Natl Med Assoc 2010; 102: 396–02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kumanyika SK, Morssink CB.. Bridging domains in efforts to reduce disparities in health and health care. Health Educ Behav 2006; 33: 440–58. [DOI] [PubMed] [Google Scholar]
- 22. Pronk NP, Peek CJ, Goldstein MG.. Addressing multiple behavioral risk factors in primary care. A synthesis of current knowledge and stakeholder dialogue sessions. Am J Prev Med 2004; 27: 4–17. [DOI] [PubMed] [Google Scholar]
- 23. Champion VL, Skinner CS.. The health belief model In: Glanz K, Rimer BK, Viswanath K (eds.). Health Behavior and Health Education. Theory, Research, and Practice. San Francisco, CA: John Wiley & Sons, 2008, 45–62. [Google Scholar]
- 24. Markland D, Ryan RM, Tobin VJ. et al. Motivational interviewing and self-determination theory. J Soc Clin Psychol 2005; 24: 811–31. [Google Scholar]
- 25. Halbert CH, Kumanyika S, Bowman M. et al. Participation rates and representativeness of African Americans recruited to a health promotion program. Health Educ Res 2010; 25: 6–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Halbert CH, Bellamy S, Briggs V. et al. Intervention completion rates among African Americans in a randomized effectiveness trial for diet and physical activity changes. Cancer Epidemiol Biomarker Prev 2014; 23: 1306–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Go AS, Mozaffarian D, Roger VL.. on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2014 update: a report from the American Heart Association. Circulation 2014; 129: e28–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. American Cancer Society. Cancer Facts and Figures, 2013. Atlanta, GA: American Cancer Society, 2013.
- 29. National Cancer Institute. Health Information National Trends Survey. Available at: http://hints.cancer.gov.
- 30. Oh A, Shaikh A, Waters E. et al. Health disparities in awareness of physical activity and cancer prevention: findings from the National Cancer Institute's 2007 Health Information National Trends Survey (HINTS). J Health Commun 2010; 15: 60–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Glasgow RE, Vogt TM, Boles SM.. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health 1999; 89: 1322–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Donner A, Klar N.. Design and Analysis of Cluster Randomization Trials in Health Research. London: Arnold, 2000. [Google Scholar]
- 33. Klohe-Lehman DM, Freeland-Graves J, Anderson ER. et al. Nutrition knowledge is associated with greater weight loss in obese and overweight low-income mothers. J Am Diet Assoc 2006; 106: 65–75. quiz 76–9. [DOI] [PubMed] [Google Scholar]
- 34. McCarthy WJ, Yancey AK, Harrison GG. et al. Fighting cancer with fitness: dietary outcomes of a randomized, controlled lifestyle change intervention in healthy African-American women. Prev Med 2007; 44: 246–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Lynch EB, Liu K, Kiefe CI. et al. Cardiovascular disease risk factor knowledge in young adults and 10-year change in risk factors: the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J Epidemiol 2006; 164: 1171–9. [DOI] [PubMed] [Google Scholar]
- 36. Israel BA, Schulz AJ, Parer EA. et al. Critical issues in developing and following community based participatory research principles. In: Community-Based Participatory Research for Health. 1998, 53–76. [Google Scholar]
- 37. American Cancer Society. Cancer Prevention and Early Detection Facts and Figures, 2013. Atlanta, GA: American Cancer Society, 2013. [Google Scholar]
- 38. Ford JG, Howerton MW, Lai GY. et al. Barriers to recruiting underrepresented populations to cancer clinical trials: a systematic review. Cancer 2008; 112: 228–42. [DOI] [PubMed] [Google Scholar]
- 39. Parra-Medina D, D'Antonio A, Smith SM. et al. Successful recruitment and retention strategies for a randomized weight management trial for people with diabetes living in rural, medically underserved counties of South Carolina: the POWER study. J Am Diet Assoc 2004; 104: 70–5. [DOI] [PubMed] [Google Scholar]
- 40. Yancey AK, Ortega AN, Kumanyika SK.. Effective recruitment and retention of minority research participants. Annu Rev Public Health 2006; 27: 1–28. [DOI] [PubMed] [Google Scholar]
- 41. US Department of Education, Institute of Education Sciences, National Center for Education Statistics. National Assessment of Adult Literacy Available at: http://nces.ed.gov/naal/.
- 42. U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. National Action Plan to Improve Health Literacy Washington, DC, 2010.
- 43. Advani PS, Reitzel LR, Nguyen NT. et al. Financial strain and cancer risk behaviors among African Americans. Cancer Epidemiol Biomarker Prev 2014; 23: 967–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lin JS, O'Connor E, Evans CV. et al. Behavioral counseling to promote a healthy lifestyle in persons with cardiovascular risk factors: a systematic review for the U.S. Preventive Services Task Force. Ann Intern Med 2014; 161: 568–78 [DOI] [PubMed] [Google Scholar]