Abstract
Emerging tobacco product use is increasing. We evaluated factors associated with perceived risk of and intention to use waterpipe tobacco by surveying students at a large university in the southeastern U.S. (N = 667). Proportional odds modeling assessed whether demographic characteristics and social acceptability are associated with perceived risk of waterpipe tobacco use; and if these factors and perceived risk are related to intention to use waterpipe tobacco. Participants who perceived waterpipe tobacco to be more socially acceptable had lower odds of perceiving it as risky (95% confidence interval [CI] 0.50–0.68). Compared with never users, former tobacco users and current users had lower odds of perceiving waterpipe tobacco use as risky (95% CI 0.38–0.80 and 0.28–0.63, respectively). Similarly, students with greater perceived social acceptability scores had higher odds of intending to use waterpipe tobacco (95% CI 1.41–2.63), while those who perceived greater risk had lower odds of intending to use it (95% CI 0.34–0.64). Compared with never users, former users had higher odds of intending to use waterpipe tobacco (95% CI 1.42–7.21). Among those who had ever used waterpipe tobacco, 90% reported ‘to socialize’ as the most frequent reason for deciding to do so. Findings underscore the need for future prevention efforts.
Introduction
In the 50 years since the first U.S. Surgeon General’s Report [1] revealed the dangers of smoking, adult smoking prevalence in the U.S. has decreased from 42% in 1965 to 18% in 2012 [2]. However, 42 million Americans continue to smoke and many more are exposed to secondhand smoke [2] despite the known immediate and long-term health consequences of smoking [2]. It is estimated that 12% of undergraduate students are current smokers and 16% have smoked cigarettes in their lifetime [3]. Initiation of smoking during the college years has been well studied, with a quarter of these young adults initiating and becoming regular smokers during the college years [4, 5]. Further, college freshmen are more likely to use multiple tobacco products and they maintain similar use patterns across the year [6], reinforcing the need to further investigate use of alternative tobacco products, including waterpipe tobacco, known most commonly in the U.S. as ‘hookah’ [3, 7–10].
Hookahs are waterpipes that are used to smoke specialty tobacco which comes in a variety of flavors such as mint, licorice, strawberry, cappuccino and chocolate. Although there are many different types of waterpipes, the modern version most frequently used in the U.S. has four main parts: the bowl where the tobacco is heated; the base filled with water or other liquids; the pipe, which connects the bowl to the base; and the hose and mouthpiece through which smoke is drawn [11]. The specialty tobacco is heated, usually with burning embers or charcoal. The smoke passes through the water, and is then drawn through the hose to the mouthpiece. Waterpipes are typically used in social settings, with many lounges located near university campuses.
According to the American Lung Association, ‘Waterpipes (also known as hookahs) are the first new tobacco trend of the 21st century’ [11]. Waterpipe tobacco use is increasingly popular among university students. The percentage who have used waterpipe tobacco at least once in their lifetime ranges from 15 to 41%; past year rates from 12 to 31%; and past month from 7 to 21% [12, 13]. According to the most recent American College Health Association (ACHA) National College Health Assessment, 19% of students had ever used tobacco from a waterpipe, and 3.9% reported any use within the last 30 days [14]. Younger university students tend to be at higher risk of using waterpipe tobacco [15]; current university students are at greater risk for waterpipe tobacco use relative to young adults not attending a university [16]. Given the growing trend of waterpipe tobacco use and varying prevalence among university students, who may be more at-risk than their peers not attending post-secondary school, further research is warranted.
Use of waterpipe tobacco is associated with short- and long-term health risks, including carbon monoxide toxicity, infectious disease transmission, reduced lung function and cancer [17, 18]. One session of waterpipe tobacco exposes individuals to a variety of chemicals (e.g. nicotine, carbon monoxide, arsenic, lead), as well as known carcinogens. Shafagoj and Hadidi [19] found high levels of nicotine and cotinine in waterpipe tobacco smokers after one session, increasing up to 250 and 120%, respectively. Most waterpipe sessions are 40–45 min, so a waterpipe tobacco user may inhale as much smoke during a single session as consuming 100 or more cigarettes. These findings reinforce the risk and toxicity of using waterpipe tobacco [20].
However, perceived risk from waterpipe tobacco is lower than from conventional products. Waterpipe tobacco users and non-users express lower perceived harm from waterpipe smoking compared with smoking cigarettes [10, 12, 21–29]. Heinz et al. [23] reported that both waterpipe smokers and non-smokers believed it yields less nicotine, tar and carcinogens than cigarettes and is less harmful to long-term health. Creamer et al. [25] found that over a quarter of university students believed that hookah did not contain tobacco and over a third believed that hookah did not contain nicotine. Similarly, they found that decreased perceived risk was associated with an increased likelihood of waterpipe tobacco use.
University students tend to regard waterpipe tobacco as more socially acceptable and popular than smoking cigarettes [12, 23, 26–28], and describe it as a pleasant social experience [28] that looks cooler than smoking cigarettes [10]. Given the social aspect of waterpipe tobacco use, there is a need to further understand the relationship of social acceptability to intention to use waterpipe tobacco and risk perception among university students.
An increasing percentage of university students are using waterpipe tobacco. While the negative health risks of conventional cigarette smoking are widely known [9], the same level of perceived risk has not been documented for waterpipe tobacco, particularly among young adults. This aims of this study were to assess whether demographic characteristics, including tobacco use status and social acceptability, are associated with perceived risk of waterpipe tobacco use among university students; and to determine whether these factors (demographics and social acceptability) and perceived risk are related to intention to use waterpipe tobacco among those who had not used this product previously.
Materials and methods
Design and sample
The sample comprised 667 students who participated in a cross-sectional online survey of undergraduate and graduate students attending a large university in the southeastern U.S. While 741 students responded to the survey, 74 were omitted from this analysis due to missing data on tobacco use and/or perceived risk and intention to use waterpipe tobacco. Comparing the respondents retained in the analysis to those with incomplete surveys, the retained and incomplete groups did not differ on sex, race/ethnicity, academic status, type of residence or fraternity/sorority status. The retained sample was relatively consistent with the full group of those invited to participate in terms of academic status: while 19% of those invited were graduate students, 25% of those in the retained sample were graduate students. Similar to many surveys, females comprised a higher percentage of the retained sample (72%), compared with the percentage of females among all those invited to participate (52%).
The university registrar provided e-mail addresses of 5000 randomly-selected students (18 years and older), including 4050 undergraduate and 950 graduate students. This list was chosen from the 26 139 full-time students; part-time and pre-professional students were omitted from the sampling frame. The percentage of undergraduate students (81%) and females (52%) in the sample reflected the demographics in the underlying eligible population. The response rate was 14.8% for the full sample and 13.3% for the sample retained here.
The study was approved by the university’s Institutional Review Board. In April 2013, the randomly-selected students were invited to participate through their official university e-mail. Surveys were administered using Qualtrics [30] which assigned potential participants a unique code to protect confidentiality of participants and was used to send reminder emails to non-responders. Reminders were sent 1 week following the initial mailing and again 1 week later. After 3 weeks, there was no further follow-up and the dataset was finalized. Survey completers were provided a link to enter a drawing to win a $25 gift card.
Measures
Demographic characteristics
Respondents were asked to indicate their sex (‘Female’ and ‘Male’). To assess race/ethnicity, participants were asked ‘How would you usually identify yourself?’ (‘White/non-Hispanic,’ ‘Black/non-Hispanic,’ ‘Hispanic or Latino,’ ‘Asian or Pacific Islander,’ ‘American Indian, Alaskan Native, or Native Hawaiian,’ ‘Middle Eastern,’ ‘Biracial or Multiracial’ and ‘Other’). With relatively few participants in minority racial/ethnic groups, race/ethnicity was dichotomized to ‘White/non-Hispanic’ and ‘Other’ for the analysis.
Participants were asked to indicate their academic status (‘first-year undergraduate’ through ‘fifth-year undergraduate’ or ‘graduate or professional’). First- and second-year undergraduates were combined to form ‘lower-level undergraduate’ and third- through fifth-year undergraduate students formed the ‘upper-level undergraduate’ group. Those who endorsed ‘graduate or professional’ were classified as ‘graduate.’ Students were asked to identify their school-year housing (‘campus residence hall,’ ‘fraternity or sorority house,’ ‘other university housing,’ ‘parent/guardian home’ and ‘other off-campus housing’). The first three options were classified as on-campus housing, while the other two were categorized as off-campus residence. Participants were asked ‘Are you a member of a social fraternity or sorority?’ (yes/no).
Tobacco use groups
Use groups were defined according to reported lifetime tobacco use for conventional cigarettes, waterpipe tobacco, smokeless tobacco, cigars and e-cigarettes. Participants were categorized as: never users, limited users, former users or current users. Never users reported never using cigarettes (i.e. not even a puff) and never using waterpipe tobacco, smokeless tobacco, cigars or e-cigarettes. Limited users smoked at least one but fewer than 100 cigarettes in their lifetime (i.e. never an established cigarette smoker), and never used waterpipe tobacco, smokeless tobacco, cigars or e-cigarettes. Former users had smoked at least 100 cigarettes in their lifetime and/or used waterpipe tobacco, smokeless tobacco, cigars and/or e-cigarettes, but had not used any of these five products within the past 30 days. Current users smoked at least 100 cigarettes and smoked within the past 30 days, and/or used waterpipe tobacco, cigars, smokeless tobacco or e-cigarettes within the past 30 days.
Social acceptability
Social acceptability of waterpipe tobacco (i.e. hookah) was assessed with the item ‘What is the social acceptability of using hookah among your peers?’ Response options included: ‘Very social acceptable,’ ‘Moderately socially acceptable,’ ‘Somewhat socially acceptable’ and ‘Not socially acceptable at all’ [31].
Reasons for deciding to use waterpipe tobacco
Those who had ever used waterpipe tobacco were asked to complete a checklist of reasons for deciding to use; respondents could check as many as applied. The possible reasons included ‘Thought it would be less expensive,’ ‘Wanted to quit smoking,’ ‘Less harmful to others,’ ‘Less harmful to myself,’ ‘Like the taste of hookah,’ ‘Less addictive than smoking cigarettes,’ ‘Can use it where smoking is not allowed,’ ‘Easily accessible,’ ‘Cultural reasons,’ ‘To hang out with my friends (socialize)’ and ‘received a coupon to use hookah.’ An endorsement indicated a ‘yes’ response for each item.
Perceived risk of waterpipe tobacco
The investigators developed an item assessing perceived risk of tobacco products, reinforcing the known health hazard of waterpipe tobacco use. Participants were asked: ‘In general, do you feel smoking hookah is a ‘Serious health hazard,’ ‘Moderate health hazard,’ ‘Minor health hazard’ or ‘Not a health hazard at all.’
Intention to use waterpipe tobacco
The investigators developed an item assessing intention to use waterpipe tobacco: ‘In the future, do you intend to use hookah?’ Response options were: ‘I do not plan to use it at all,’ ‘I don’t know,’ ‘I plan to use it’ and ‘I very much want to use it.’ While included in the original response set, the ‘I very much want to use it’ choice was not endorsed by any respondent who had not ever tried hookah, so that option was not used in the analysis.
Analysis
Frequency distributions were used to summarize study variables. The Kruskal–Wallis test was used to test for differences among tobacco use groups in perception of risk and intention to use. Due to the ordinal response options for perceived risk and intention, proportional odds modeling (POM) was used to assess factors associated with these outcomes. Both regression models (one for perceived risk and the other for intention to use) included these potential correlates: sex, race, academic status, residence, social fraternity/sorority membership, social acceptability of waterpipe tobacco and tobacco use group. The model with intention to use waterpipe tobacco as the outcome also included perceived risk as a potential correlate. Variance inflation factors (VIFs) were used to assess the presence of multicollinearity; since the VIFs for the selected regressors were all <2.5, there is no evidence to suggest that multicollinearity distorted any of the regression parameters. The Score test was used to check the proportional odds assumption in the POM; the Score test P-values for both models were >0.05, indicating the models did not violate the proportional odds requirement. Analysis was conducted using SAS v. 9.4; as a protection against Type I error, a conservative alpha level of 0.01 was used throughout.
Results
The majority of the sample was female (72%), and most participants were White/non-Hispanic (79%; see Table I). The largest subgroup of participants were lower-level undergraduates (freshman or sophomore; 61%), and one-quarter of those surveyed were graduate students. Most lived in off-campus housing (58%) and did not belong to a social fraternity or sorority (81%). Tobacco use status was based on history of using cigarettes, waterpipe tobacco, smokeless tobacco, cigars and e-cigarettes. The largest tobacco use subgroup was the never users (42%), followed by former users (24%), and current users (20%); 14% of all participants were ‘limited’ tobacco users (had used cigarettes in the past, but did not meet the 100-cigarette threshold for established use; had never used any of the other tobacco products).
Table I.
Frequency distributions of sample characteristics (N = 667)
| Variable | n (%) |
|---|---|
| Sex | |
| Female | 478 (71.8%) |
| Male | 188 (28.2%) |
| Race/ethnicity | |
| White/non-Hispanic | 525 (78.8%) |
| Other | 141 (21.2%) |
| Academic status | |
| Lower-level undergraduate | 406 (61.1%) |
| Upper-level undergraduate | 94 (14.1%) |
| Graduate | 165 (24.8%) |
| Residence | |
| On-campus | 281 (42.3%) |
| Off-campus | 384 (57.7%) |
| Member of social fraternity/sorority | |
| Yes | 128 (19.3%) |
| No | 537 (80.7%) |
| Tobacco use group | |
| Never Users | 281 (42.1%) |
| Limited Usersa | 91 (13.6%) |
| Former Usersb | 160 (24.0%) |
| Current Users | 135 (20.2%) |
Smoked cigarettes but not 100 in lifetime; never used waterpipe tobacco, smokeless tobacco, cigars or e-cigarettes.
Had used cigarettes, waterpipe tobacco, smokeless tobacco, cigars, and/or e-cigarettes, but not in the last 30 days.
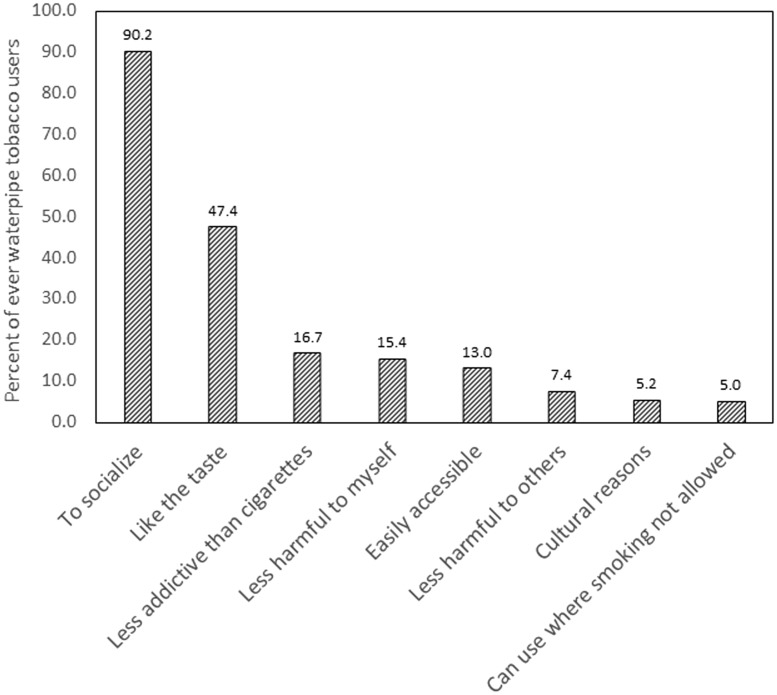
In the full sample of participants, 218 (32.7%) had used waterpipe tobacco. Among these ever-users of waterpipe tobacco, the most frequent reasons for deciding to use this product were ‘to hang out with my friends (socialize),’ indicated by 90% of respondents, and ‘like the taste,’ chosen by 47% (see Fig. 1). Less frequently-endorsed reasons included ‘less addictive than cigarettes’ (17%), ‘less harmful to myself’ (15%) and ‘easily accessible’ (13%). Fewer than one-tenth of waterpipe tobacco users said they decided to use it because it is ‘less harmful to others’ (7%), ‘cultural reasons’ (5%) and ‘can use where smoking is not allowed’ (5%). The remaining options (i.e. ‘received a coupon,’ ‘thought it would be less expensive,’ and ‘wanted to quit smoking’) were chosen by fewer than 5% of waterpipe tobacco users.
Fig. 1.
Most frequent reasons for deciding to use waterpipe tobacco among ever users (n = 218).
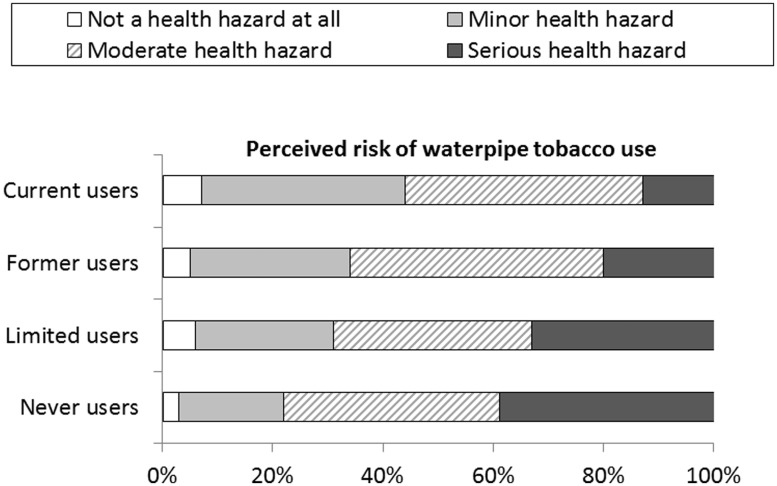
Among all participants, there was a significant association between tobacco use group and perceived risk for waterpipe tobacco (P < 0.001 for the Kruskal–Wallis test; see Fig. 2). In general, those with more recent, established use of tobacco perceived waterpipe tobacco smoking as less serious than never users or limited users. The percentage of never users who rated waterpipe tobacco as a serious health hazard was 39%, compared with 33% of limited users, 20% former users and 13% current tobacco users.
Fig. 2.
Associations between tobacco use group and perceived risk of waterpipe tobacco use.
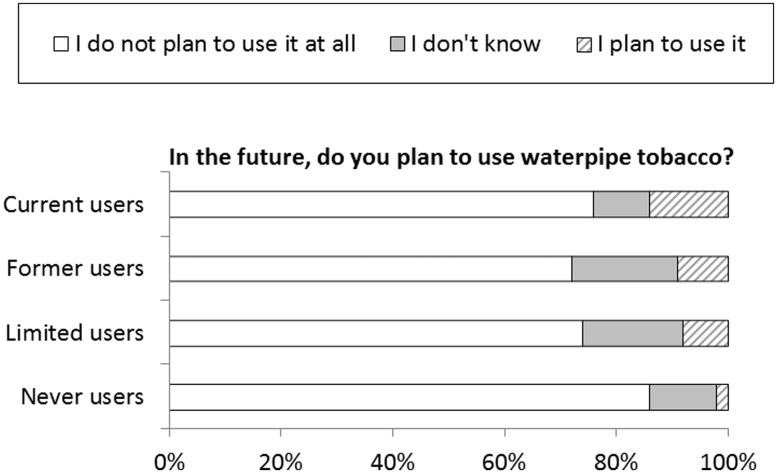
Intention to use waterpipe tobacco was associated with tobacco use group among those who had never used this product previously (P = 0.01 for the Kruskal–Wallis test; see Fig. 3). The largest difference in intention to use was between those who had never used any tobacco product and the other three categories of tobacco use. Among respondents who had never used any form of tobacco, only 2% said they plan to use waterpipe tobacco. Among limited tobacco users (smoked <100 cigarettes in their lifetime), all of whom had never used waterpipe tobacco, cigars, smokeless tobacco or e-cigarettes, 8% said they plan to use waterpipe tobacco. Among former tobacco users who had never used waterpipe tobacco, 9% said they plan to use waterpipe tobacco. Finally, among current tobacco users who had never used waterpipe tobacco, 14% said they plan to do so.
Fig. 3.
Associations between tobacco use group and intention to use waterpipe tobacco among those who had never used it previously.
Factors associated with perceived risk
The POM for perceived risk of waterpipe tobacco is shown in Table II. The overall model, including sex, race/ethnicity, academic status, residence, fraternity/sorority status, social acceptability of waterpipe tobacco, and tobacco use group, was significant (χ2 = 101.1, P < 0.001). The factors significantly associated with perceived risk of waterpipe tobacco included social acceptability and tobacco use group. For each 1-point increase in social acceptability score, the odds of perceiving waterpipe tobacco as more risky decreased by 41% (odds ratio [OR] = 0.59; 95% confidence interval [CI] 0.50–0.68). With never users as the reference group, former users had 45% lower odds of perceiving waterpipe tobacco as more risky (OR = 0.55; 95% CI 0.38–0.80) and current users had 58% lower odds of doing so (OR = 0.42; 95% CI 0.28–0.63). There was no difference in perceived risk of using waterpipe tobacco between never users and limited users. Sex, race/ethnicity, academic status, residence, fraternity/sorority were not associated with perceived risk of waterpipe tobacco use.
Table II.
Proportional odds logistic model to assess factors associated with greater perceived risk of waterpipe tobacco use (n = 654)
| Variable | Estimated odds ratio (OR) | 95% Confidence interval for OR | P |
|---|---|---|---|
| Sex | |||
| Female | 1.31 | 0.94–1.81 | 0.11 |
| Male | 1.00 | ||
| Race/ethnicity | |||
| White/non-Hispanic | 1.16 | 0.81–1.66 | 0.42 |
| Other | 1.00 | ||
| Academic status | |||
| Lower undergraduate | 0.69 | 0.46–1.03 | 0.068 |
| Upper undergraduate | 1.03 | 0.38–1.03 | 0.065 |
| Graduate | 1.00 | ||
| Residence | |||
| On-campus | 1.03 | 0.73–1.46 | 0.85 |
| Off-campus | 1.00 | ||
| Member of social fraternity/sorority | |||
| Yes | 0.78 | 0.53–1.14 | 0.20 |
| No | 1.00 | ||
| Social acceptability of waterpipe tobacco | 0.59 | 0.50–0.68 | <0.001 |
| Tobacco use group | |||
| Never users | 1.00 | ||
| Limited usersa | 0.72 | 0.45–1.13 | 0.15 |
| Former usersb | 0.55 | 0.38–0.80 | 0.002 |
| Current users | 0.42 | 0.28–0.63 | <0.001 |
Smoked cigarettes but not 100 in lifetime; never used waterpipe tobacco, smokeless, cigars, or e-cigarettes
Had used cigarettes, waterpipe tobacco, smokeless, cigars, and/or e-cigarettes, but not in the last 30 days
Factors associated with intention to use waterpipe tobacco
The POM to assess factors associated with intention to use waterpipe tobacco among those who had never used it previously was significant overall (χ2 = 79.7, P < 0.001). The significant correlates included social acceptability of waterpipe tobacco use, perceived risk of waterpipe tobacco, and tobacco use group (see Table III). For each 1-point increase in social acceptability score, the odds of intention to use waterpipe tobacco rose by 93% (95% CI 1.41–2.63). For each 1-point increase in perceived risk of waterpipe tobacco, the odds of intention to use waterpipe tobacco decreased by 53% (95% CI 0.34–0.64). With never users as the reference group, former users had 221% greater odds of intending to use waterpipe tobacco. The comparisons of never users to limited users and never users to current users were not significant. Sex, race/ethnicity, academic status, residence and fraternity/sorority status were not related to intention to use waterpipe tobacco.
Table III.
Proportional odds logistic model to assess factors associated with greater intention to use waterpipe tobacco (n = 436)
| Variable | Estimated odds ratio (OR) | 95% Confidence interval for OR | P |
|---|---|---|---|
| Sex | |||
| Female | 0.62 | 0.34–1.12 | 0.11 |
| Male | 1.00 | ||
| Race/ethnicity | |||
| White/non-Hispanic | 0.82 | 0.44–1.55 | 0.54 |
| Other | 1.00 | ||
| Academic status | |||
| Lower undergraduate | 1.77 | 0.79–3.95 | 0.17 |
| Upper undergraduate | 1.40 | 0.51–3.81 | 0.52 |
| Graduate | 1.00 | ||
| Residence | |||
| On-campus | 0.99 | 0.54–1.82 | 0.96 |
| Off-campus | 1.00 | ||
| Member of social fraternity/sorority | |||
| Yes | 1.37 | 0.69–2.72 | 0.37 |
| No | 1.00 | ||
| Social acceptability of waterpipe tobacco | 1.93 | 1.41–2.63 | <0.001 |
| Perceived risk of waterpipe tobacco | 0.47 | 0.34–0.64 | <0.001 |
| Tobacco use group | |||
| Never users | 1.00 | ||
| Limited usersa | 1.84 | 0.96–3.53 | 0.067 |
| Former usersb | 3.21 | 1.42–7.21 | 0.005 |
| Current users | 2.02 | 0.77–5.31 | 0.15 |
Smoked cigarettes but not 100 in lifetime; never used waterpipe tobacco, smokeless, cigars, or e-cigarettes.
Had used cigarettes, waterpipe tobacco, smokeless, cigars, and/or e-cigarettes, but not in the last 30 days.
Discussion
University students who viewed waterpipe tobacco as more socially acceptable had lower odds of perceiving it as a health risk. Considering university students have reported higher perceived peer use of waterpipe tobacco as compared to actual use, believing 40–66% of university students are current users [14, 27], there is a need to dispel these perceptions with social norm campaigns [32]. Current and former users had lower odds of perceiving waterpipe tobacco as a health risk. This is consistent with prior research demonstrating that waterpipe tobacco users tend to believe there is less of a health risk, particularly compared to cigarettes [21, 22, 28, 32]. Although this study did not measure intensity of waterpipe tobacco use, Creamer et al. [25] found that increased perceived risk was associated with lower intensity of use among current users. Findings from this study support the need for education on the health risks of waterpipe tobacco use among both tobacco users and non-users, with a special emphasis on current and former tobacco users, in an effort to promote tobacco prevention and curtail tobacco initiation on university campuses.
Among those who had never used waterpipe tobacco, social acceptability, perceived risk, and tobacco use group were associated with intention to use waterpipe tobacco. Greater perception of social acceptability was associated with greater odds of na�ve waterpipe tobacco users intending to use the product. Barnett et al.’s [31] research supports the importance of normative beliefs (i.e. hookah being more socially acceptable) among both users and non-users as a predictor of intention to use waterpipe tobacco in the future. Social acceptability has also been linked to number of friends who use waterpipe tobacco use [26]. Among ever users of waterpipe tobacco in this study, 90% indicated they had decided to use this product for social reasons. Exploring peer-to-peer prevention initiatives may be beneficial given the value placed on social influences among university students.
Similarly, among na�ve waterpipe tobacco users, those who viewed this product as less risky had increased odds of intending to use it. Previous research suggests those who perceive waterpipe tobacco to be less risky report higher intensity of use [25], which may predispose university students to the likelihood of addiction. Interestingly, former tobacco users who had never used waterpipe tobacco reported greater odds of intending to use the product, relative to those who had never used tobacco products. Although previous research supports that current tobacco users are more likely to use waterpipe tobacco [25, 32–34], the notion that former tobacco users may be more inclined to use waterpipe tobacco is novel. Relapse prevention programs need to target the health risks of waterpipe tobacco use to inform former tobacco users of the dangers and consequences of using the product. Given the limited research on intention to use emerging tobacco products, further understanding intention to use waterpipe tobacco and other emerging tobacco products, along with longitudinal assessments of initiation and use during the college years, are needed to maximize the success of current and future tobacco control efforts on university campuses.
In this study, 33% of participants had used waterpipe tobacco, which underscores the prevalence and the need for prevention efforts on university campuses. The increased availability of waterpipe tobacco establishments (i.e. hookah lounges) near universities [12, 31] is concerning, particularly as many of these places cater to university students under the age of 21. Future studies are needed to investigate the links among perception of risk, availability and social influences related to use of waterpipe tobacco. University campuses are an ideal setting to reach waterpipe tobacco users and those who may initiate while on campus [16]. However, it will take comprehensive, evidence-based approaches to decrease current tobacco use and prevent the initiation of waterpipe tobacco use. It is typically believed that the longer one delays the use of tobacco products, the less likely one is to initiate use, but this observation has only been documented for traditional tobacco products [35, 36]. Moreover, tobacco prevention programs and policies on and around university campuses tend to focus on conventional cigarette smoking, but there is a clear need to promote efforts to target emerging tobacco products [15, 32, 37]. Limited research exists regarding waterpipe tobacco prevention programs. Lipkus et al. [38] conducted a quasi-experimental study to test intervention strategies among current waterpipe tobacco users. They reported that intervention participants had greater perceived risk and expressed a stronger desire to quit as compared to the control group following the intervention. There is a need to further understand factors which may motivate university students to initiate waterpipe tobacco in an effort to develop tailored prevention interventions [16, 37]. Evidence-based interventions, including tobacco-free campus policies [16], are essential to decrease the initiation and continued use of all forms of tobacco products among university students and across the lifespan [39].
The primary study limitation is the low response rate. However, this response rate is similar to other e-mailed surveys of university students [40]. Consistent with many surveys, the majority of the sample (72%) was female. These concerns are partially mitigated by the observation that those included in this analysis did not differ demographically from those who submitted incomplete surveys; and those who participated were similar to the underlying population in terms of percent graduate students. Other limitations stem from the measures used to assess social acceptability, perception of risk and intention to use. While these single-item assessments were expedient in the online survey format, more detailed measures of these items (unavailable at the time of this study) may have provided a greater understanding of these constructs. Further research will benefit from the use of validated, in-depth assessments in this area. We also did not measure income or marital status in this population, limiting our ability to assess the full range of demographic characteristics that may be associated with perceived risk and intention to use.
Nearly one-third of participants reported ever using hookah, reinforcing the need for further understanding on factors which impact intention to use. Health professionals and university leaders have a responsibility to address the health risks of waterpipe tobacco use by university students. These findings suggest that former tobacco users who have never used waterpipe tobacco may be at higher risk for initiating use of that product. Further, those who view waterpipe tobacco as more socially acceptable and less risky may also be more likely to use the product. There is an urgent need to design and test evidence-based interventions aimed at prevention and reduction of waterpipe tobacco use by university students. The fact that waterpipe tobacco contains the same hazardous ingredients in conventional cigarettes suggests that over time, similar health risks may be empirically confirmed [9, 18, 19]. As of August 2016, waterpipe tobacco is subject to action by the U.S. Food and Drug Administration (FDA) for false or misleading information and claims of modified risk. FDA also has the authority to review product promotions and ensure consumers are informed of the risks of emerging tobacco products. The impact of these FDA regulations needs to be explored. In addition, future research is warranted on factors related to initiation and use of emerging tobacco products by university students as well as identification and testing of effective interventions including policy change. These efforts may help to prevent the creation of a new generation of tobacco users with the inherent personal and public health risks and associated societal costs.
Funding
This study was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through grant number UL1TR000117. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Conflict of interest statement
None declared.
Acknowledgements
We would like to thank the George and Betty Blanda Endowed Professorship awarded to Dr. Melody Noland for providing the incentives for this study.
References
- 1. U. S. Department of Health and Human Services. 1st Surgeon General Report: Smoking and Health. Atlanta, GA: USDHHS, 1964. [Google Scholar]
- 2. U. S. Department of Health and Human Services. The Health Consequences of Smoking-50 Years of Progress: a Report of the Surgeon General. Rockville, MD: USDHHS, 2014. [Google Scholar]
- 3. American College Health Association. American College Health Association - National College Health Assessment II: reference group undergraduates executive summary. Hanover, MD, 2016.
- 4. Rigotti NA, Lee J, Wechsler H.. US college students' use of tobacco products—results of a national survey. JAMA 2000; 284:699–705. [DOI] [PubMed] [Google Scholar]
- 5. Staten RR, Noland M, Rayens MK. et al. Social influences on cigarette initiation among college students. Am J Health Behav 2007; 31:353–62. [DOI] [PubMed] [Google Scholar]
- 6. Cooke ME, Cho S, Kendler KS. et al. Predicting tobacco use across the first year of college. Am J Health Behav 2016; 40:484–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lee Y, Hebert C, Nonnemaker J. et al. Multiple tobacco product use among adults in the US: cigarettes, cigars, electronic cigarettes, hookah, smokeless tobacco, and snus. Prev Med 2014; 62:14–9. [DOI] [PubMed] [Google Scholar]
- 8. Richardson A, Rath J, Villanti AC. et al. The next generation of users: prevalence and longitudinal patterns of tobacco use among US young adults. J Pub Health 2014; 104:1429–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. U. S. Department of Health and Human Services. Preventing tobacco use among youth and young adults: a report of the Surgeon General. Rockville, MD, 2012. [PubMed]
- 10. Sutfin EL, McCoy TP, Reboussin BA. et al. Prevalence and correlates of waterpipe tobacco smoking by college students in North Carolina. Drug Alcohol Depend 2011; 115:131–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. American Lung Association. An emerging deadly trend: waterpipe tobacco use. 2007.
- 12. Primack BA, Sidani J, Agarwal AA. et al. Prevalence of and associations with waterpipe tobacco smoking among U.S. university students. Ann Behav Med 2008; 36:81–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gerkin ER. Waterpipe smoking among college students in the United States: a review of the literature. J Am Coll Health 2012; 60:244–9. [DOI] [PubMed] [Google Scholar]
- 14. American College Health Association. American College Health Association-National College Health Assessment II: reference group executive summary spring 2015. Hanover, MD, 2015.
- 15. Majeed BA, Sterling KL, Weaver SR. et al. Prevalence and harm perceptions of hookah smoking among U.S. adults, 2014–2015. Addict Behav 2017; 69:78–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lee YO, Bahreinifar S, Ling PM.. Understanding tobacco-related attitudes among college and noncollege young adult hookah and cigarette users. J Am Coll Health 2014; 62:10–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. Smoking and tobacco use: hookahs. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/tobacco_industry/hookahs/index.htm. Accessed: 13 March 2017.
- 18. Fauci L, Steiner IP, Shavit I.. Carbon monoxide poisoning in narghile (water pipe) tobacco smokers. CJEM 2012; 14:57–9. [DOI] [PubMed] [Google Scholar]
- 19. Shafagoj YA, Hadidi KA.. Hubble-bubble (waterpipe) smoking: levels of nicotine and cotinine in plasma, saliva and urine. Int J Clin Pharmacol Ther 2002; 40:249–55. [DOI] [PubMed] [Google Scholar]
- 20. World Health Organization. WHO advisory note: waterpipe tobacco smoking: health effects, research needs and recommended actions by regulators. 2005. [DOI] [PMC free article] [PubMed]
- 21. Eissenberg T, Ward KD, Smith-Simone S. et al. Waterpipe tobacco smoking on a U.S. college campus: prevalence and correlates. J Adolesc Health 2008; 42:526–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nuzzo E, Shensa A, Kim KH. et al. Associations between hookah tobacco smoking knowledge and hookah smoking behavior among US college students. Health Ed Res 2013; 28:92–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Heinz A, Gledgowd G, Crane N. et al. A comprehensive examination of hookah smoking in college students: use patterns and contexts, social norms and attitudes, harm perception, psychological correlates and co-occurring substance use. Add Behav 2013; 38:2751–60. [DOI] [PubMed] [Google Scholar]
- 24. Smith SY, Stillman FA.. Harm perception of nicotine products in college freshmen. Nicotine Tob Res 2007; 9:977–82. [DOI] [PubMed] [Google Scholar]
- 25. Creamer MR, Loukas A, Xiaoyin L. et al. College students’ perceptions and knowledge of hookah use. Drug Alcohol Depend 2016; 168:191–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Berg C, Ling P, Hayes R. et al. Smoking frequency among current college student smokers: distinguishing characteristics and factors related to readiness to quit smoking. Health Educ Res 2012; 27:141–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Noland M, Ickes MJ, Rayens MK. et al. Social influences on use of cigarettes, e-cigarettes, and hookah by college students. J Am Coll Health 2016; 64:319–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Noonan D, Patrick ME.. Factors associated with perceptions of hookah addictiveness and harmfulness among young adults. Subst Abuse 2013; 34:83–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lipkus IM, Schwartz-Bloom R, Prokhorov A. et al. Relationships among factual and perceived knowledge of harms of waterpipe tobacco, perceived risk, and desire to quit among college users. J Health Psychol 2014; 19:1525–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Qualtrics Inc. Qualtrics Software. Vol v.37,892. Provo, UT: Qualtrics Research Suite, 2013.
- 31. Barnett T, Smith T, He Y. et al. Evidence of emerging hookah use among university students: a cross sectional comparison between hookah and cigarette use. Pub Health 2013; 13:302.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Berg CJ, Gillian ES, Schauer L. et al. Perceived harm, addictiveness, and social acceptability of tobacco products and marijuana among young adults: marijuana, hookah, and electronic cigarettes win. Sub Use Misuse 2015; 50:79–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lipkus I, Wolfson M, Sutfin EL.. Assessing and predicting susceptibility to waterpipe tobacco use among college students. Nicotine Tob Res 2015; 17:1120–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Haidera M, Islama F, Ortiza KS. et al. Factors associated with smoking frequency among current waterpipe smokers in the United States: findings from the National College Health Assessment II. Drug Alcohol Depend 2015; 153:359–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Everett SE, Kann L, Warren CW. et al. Smoking initiation and smoking patterns among US college students. J Am Coll Health 1999; 48:55–60. [DOI] [PubMed] [Google Scholar]
- 36. Taioli E, Wynder EL.. Effect of age at which smoking begins on frequency of smoking in adulthood. N Engl J Med 1991; 325:968–9. [DOI] [PubMed] [Google Scholar]
- 37. Martinasek M, Bryant CA.. Antecdents of university students’ hookah smoking intention. Am J Health Behav 2013; 37:599–609. [DOI] [PubMed] [Google Scholar]
- 38. Lipkus IM, Schwartz-Bloom RD, Prokhorov AV. et al. Affecting perceptions of harm and addiction among college waterpipe tobacco smokers. Nicotine Tob Res 2011; 13:599–610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. American College Health Association. Position statement on tobacco on college and university campuses. J Am Coll Health 2009; 58:291–2. [DOI] [PubMed] [Google Scholar]
- 40. Dennison O, Wang Q, Ickes M.. Prevalence of HIV testing and associated risk factors in college students. J Am Coll Health 2014; 62:309–18 [DOI] [PMC free article] [PubMed] [Google Scholar]