Abstract
Study Objectives
A recent study of patients with moderate–severe obstructive sleep apnea (OSA) in Iceland identified three clinical clusters based on symptoms and comorbidities. We sought to verify this finding in a new cohort in Iceland and examine the generalizability of OSA clusters in an international ethnically diverse cohort.
Methods
Using data on 972 patients with moderate–severe OSA (apnea–hypopnea index [AHI] ≥ 15 events per hour) recruited from the Sleep Apnea Global Interdisciplinary Consortium (SAGIC), we performed a latent class analysis of 18 self-reported symptom variables, hypertension, cardiovascular disease, and diabetes.
Results
The original OSA clusters of disturbed sleep, minimally symptomatic, and excessively sleepy replicated among 215 SAGIC patients from Iceland. These clusters also generalized to 757 patients from five other countries. The three clusters had similar average AHI values in both Iceland and the international samples, suggesting clusters are not driven by OSA severity; differences in age, gender, and body mass index were also generally small. Within the international sample, the three original clusters were expanded to five optimal clusters: three were similar to those in Iceland (labeled disturbed sleep, minimal symptoms, and upper airway symptoms with sleepiness) and two were new, less symptomatic clusters (labeled upper airway symptoms dominant and sleepiness dominant). The five clusters showed differences in demographics and AHI, although all were middle-aged (44.6–54.5 years), obese (30.6–35.9 kg/m2), and had severe OSA (42.0–51.4 events per hour) on average.
Conclusions
Results confirm and extend previously identified clinical clusters in OSA. These clusters provide an opportunity for a more personalized approach to the management of OSA.
Keywords: obstructive sleep apnea, disease subtypes, personalized medicine, excessive sleepiness, insomnia, minimally symptomatic
Statement of Significance
Obstructive sleep apnea is a heterogeneous disorder—two patients with similar disease severity may experience vastly different symptoms and consequences. A prior study in Iceland identified three distinct clinical clusters of patients with obstructive sleep apnea: disturbed sleep, minimally symptomatic, and excessively sleepy. Using a clinical sample of patients with moderate–severe sleep apnea recruited from across the world as part of the Sleep Apnea Global Interdisciplinary Consortium, this study both replicates the original three clusters within a new Icelandic sample and expands on these clusters within a more ethnically diverse population. Establishing the robustness of these clinical phenotypes is crucial for future research examining the impact of disease clusters on treatment response and personalized obstructive sleep apnea management.
Introduction
Obstructive sleep apnea (OSA) is a common sleep disorder characterized by repetitive complete or partial closure of the upper airway during sleep. An estimated 13% of middle-aged men and 6% of middle-aged women suffer from moderate–severe disease, defined as at least 15 apneas or hypopneas per hour of sleep [1]. OSA is associated with a wide range of negative health consequences, including hypertension and cardiovascular disease [2–10], diabetes [11, 12], neurodegenerative disorders [13], cancer [14], and mortality [15, 16]. Frequently reported symptoms in OSA include features of upper airway narrowing (e.g. loud snoring, witnessed apneas, and nocturnal gasping), excessive sleepiness, sleep disturbances, and general fatigue. It is widely recognized that there is considerable variability in etiology, symptoms, and consequences of OSA among patients, which leads to under-recognition of patients with atypical symptom profiles. Thus, recent studies have sought to better characterize clinical subtypes of patients with OSA based on demographics, disease severity, symptoms, and comorbidities. More accurate characterization and diagnosis of OSA is crucial to personalizing and improving clinical management.
The first major attempt to identify clinical presentation subtypes was performed in a population of patients with moderate–severe OSA from the Icelandic Sleep Apnea Cohort (ISAC) [17]. Three distinct clusters were identified as follows: a disturbed sleep group characterized by insomnia and restless sleep, a minimally symptomatic group, and an excessively sleepy group. Subsequent studies in Greece [18], Italy [19], France [20, 21], and Europe [22] have suggested additional or different OSA clusters. These studies cannot be easily compared because of differences in sample characteristics (e.g. inclusion of controls) and variables used to define clusters (e.g. inclusion of apnea hypopnea index [AHI]). However, several studies recognize the existence of clusters of patients with relatively low symptom burden, as well as clusters with predominant sleep disturbance symptoms or daytime sleepiness, as observed in the original ISAC study [17]. To further understand individual differences in OSA clinical presentation, in this article, we focus on clinical symptoms among patients with moderate–severe disease.
Recent studies suggest that OSA etiology varies between racial and ethnic groups [23–27]. For example, Asian patients are less obese and have more prevalent craniofacial risk factors when compared with Caucasians of similar disease severity [26]. Similarly, OSA has been found to be more severe in young African-Americans compared with Caucasians [23]. These differences in disease risk factors and etiology may lead to distinct symptom profiles and disease consequences among ethnicities, raising the question of the robustness and generalizability of OSA clusters previously identified within a single ethnic group [28]. Moreover, it is important to know whether the findings in Iceland are inherent characteristics of OSA or whether they are unique to Iceland, perhaps due to cultural norms or referral patterns. This knowledge would advance our understanding of OSA and help clinicians better recognize the most important disease characteristics in specific patient populations.
Towards this end, in the current study, we first sought to confirm the presence of the three OSA clinical clusters initially identified in ISAC [17] in (1) a new cohort from Iceland and (2) an ethnically diverse international cohort. Second, we sought to determine the optimal number of clinical clusters that exist within the larger ethnically diverse cohort from outside of Iceland. We hypothesized that the previously identified OSA clusters would be confirmed in Iceland and that similar OSA clusters would be observed within the ethnically diverse international cohort.
Methods
Study participants
An international clinical sample of patients with OSA for the present study was recruited from the Sleep Apnea Global Interdisciplinary Consortium (SAGIC) study cohort (http://www.med.upenn.edu/sleepctr/sagic.html). The primary purpose of SAGIC is to establish a large, multinational cohort with detailed phenotyping to understand common and ethnicity-specific OSA presentations and risk profiles. SAGIC consists of participants recruited from eight sleep centers in six countries, including the United States (University of Pennsylvania and The Ohio State University), Australia (University of Sydney and Sir Charles Gairdner Hospital, Perth), Germany (Charité University Hospital), Brazil (Médicado Instituto do Sono), Taiwan (Chang Gung Memorial Hospital), and Iceland (Landspitali—The National University Hospital of Iceland). Given the goals of the present study, participants from Iceland were analyzed separately from participants recruited outside of Iceland. Similar to the original ISAC study [17], the analysis sample was restricted to participants with moderate–severe OSA [defined as AHI ≥ 15 events per hour] and information available on self-reported symptom frequency (Table 1); participants missing responses on >5 symptom questions were excluded from analyses. Using these criteria, a total of 972 SAGIC participants (215 from Iceland and 757 from the remaining sites) were included in analyses. The study protocol was approved by the Institutional Review Board (IRB) at the University of Pennsylvania and additional IRB approval was required and obtained at each site. Informed consent was obtained from all participants.
Table 1.
Demographic characteristics of the SAGIC samples
| Variable | All SAGIC | International | Iceland | P* |
|---|---|---|---|---|
| N | 972 | 757 | 215 | – |
| Demographic variables | ||||
| Age, years | 51.9 ± 12.9 | 50.9 ± 13.4 | 55.3 ± 10.4 | <0.0001 |
| Male, % | 70.3 | 72.8 | 61.4 | 0.001 |
| BMI, kg/m2 | 33.8 ± 8.1 | 33.8 ± 8.5 | 34.0 ± 6.5 | 0.730 |
| AHI, events/hr | 42.9 ± 26.8 | 46.6 ± 28.4 | 29.8 ± 13.6 | <0.0001 |
| ODI, events/hr | 40.2 ± 27.0 | 44.0 ± 28.8 | 27.5 ± 13.4 | <0.0001 |
| Ethnicity, % | <0.0001 | |||
| Caucasian | 58.8 | 47.5 | 98.6 | |
| African/African American | 5.9 | 7.6 | 0.0 | |
| Asian | 21.1 | 27.1 | 0.0 | |
| Central/South American | 6.6 | 8.5 | 0.0 | |
| Other | 7.6 | 9.4 | 1.4 | |
| Site, % | <0.0001 | |||
| Iceland | 22.1 | 0.0 | 100.0 | |
| Berlin | 7.3 | 9.4 | 0.0 | |
| Brazil | 10.9 | 14.0 | 0.0 | |
| Ohio State | 14.5 | 18.6 | 0.0 | |
| U Penn | 10.4 | 13.3 | 0.0 | |
| Sydney | 9.0 | 11.5 | 0.0 | |
| Perth | 6.1 | 7.8 | 0.0 | |
| Taiwan | 19.8 | 25.4 | 0.0 | |
| Clustering variables | ||||
| Epworth Sleepiness Scale (ESS) | 10.2 ± 5.5 | 10.0 ± 5.6 | 10.7 ± 4.9 | 0.067 |
| Symptom, % | ||||
| I feel rested upon waking | 18.9 | 20.4 | 13.5 | 0.022 |
| I feel sleepy during the day | 57.1 | 55.3 | 63.3 | 0.038 |
| Physically tired during the day | 80.6 | 79.3 | 85.1 | 0.059 |
| Fall asleep while watching TV | 62.4 | 59.1 | 74.0 | <0.0001 |
| Fall asleep involuntarily | 26.1 | 29.3 | 15.0 | <0.0001 |
| Take naps | 77.4 | 77.9 | 75.4 | 0.423 |
| Frequently doze while driving | 8.2 | 9.5 | 3.7 | 0.007 |
| Difficulty falling asleep | 34.7 | 33.0 | 40.9 | 0.031 |
| Difficulty maintaining sleep | 54.1 | 48.3 | 74.2 | <0.0001 |
| Waking too early | 40.2 | 39.2 | 43.5 | 0.265 |
| Restless in my sleep | 52.2 | 47.1 | 70.2 | <0.0001 |
| Wake up with a headache | 31.9 | 31.0 | 34.9 | 0.280 |
| Perspire heavily at night | 35.6 | 33.8 | 41.9 | 0.030 |
| Wake up suddenly, can’t breathe | 42.2 | 42.1 | 42.5 | 0.919 |
| Been told I stop breathing | 53.5 | 51.3 | 60.9 | 0.013 |
| Snoring that disturbs partner | 79.3 | 79.3 | 79.1 | 0.932 |
| Restless Legs Syndrome | 13.2 | 11.3 | 20.0 | 0.001 |
| Hypertension, % | 47.2 | 45.5 | 52.8 | 0.060 |
| Diabetes, % | 17.0 | 17.4 | 15.8 | 0.598 |
| Cardiovascular disease, % | 16.0 | 16.7 | 13.5 | 0.253 |
*p-Value from t test and chi-squared or Fisher’s exact test comparing continuous and categorical variables, respectively, between SAGIC non-Icelandic (international) and Iceland samples.
BMI = body mass index; AHI = apnea–hypopnea index; ODI = oxygen desaturation index.
Sleep studies
In the analysis sample used for clustering (N = 972), a total of 688 (70.8%) patients were diagnosed using laboratory-based polysomnography and 284 (29.2%) with home-based sleep studies. Standard operating procedures were implemented at each site to help ensure uniform data collection. We found a strong inter-rater agreement of respiratory events in scoring both for in-laboratory and home studies among the eight sleep centers [29, 30]. Standards from the American Academy of Sleep Medicine (AASM) manual were used to score sleep stages, arousals, and respiratory events [31]. Apneas were defined as an absence of airflow on the oronasal thermistor or nasal pressure cannula for ≥10 s. Hypopneas were defined as a ≥30% reduction from baseline in airflow for ≥10 s associated with at least a 4% oxygen desaturation. The AHI was calculated as the mean number of apneas and hypopneas per hour of sleep. For home studies, total analysis time was assessed based on patient questionnaires regarding sleep onset and wake times and the sleep technologist’s review of the study; upright time was excluded from analysis. This interval was assumed to be sleep duration. In the Icelandic sample, following standard clinical protocol, OSA diagnosis was made predominantly using in-home studies, as detailed previously [32].
Symptom questionnaire
All SAGIC participants completed a detailed questionnaire on demographics, ethnicity, sleep-related symptoms, comorbidities, and medications. When the SAGIC was started, a common questionnaire was developed based on the Basic Nordic Sleep Questionnaire (BNSQ) [33], the Berlin Questionnaire [34], the Multivariable Apnea Risk Index (MAP) questions on snoring and apneas [35], Epworth Sleepiness Scale (ESS) [36], 12-item Short Form Health Survey [37], and restless legs syndrome (RLS) symptoms [38]. Although the original questionnaires were written in English, the SAGIC questionnaire was translated into the languages of the different participating sites, including Icelandic, German, Portuguese, and Mandarin, using forward and backward translation to assure accuracy [39, 40].
The SAGIC questionnaire includes a number of symptom-related questions, including those related to sleepiness, insomnia, nighttime sleep disturbance, abnormal behaviors during sleep, upper airway symptoms (snoring, witnessed apneas, and waking suddenly unable to breathe), and other symptoms such as headaches and excessive sweating. For a majority of included symptoms, participants answered using the same format as the ISAC, with responses of 0 (never or less than once per month), 1 (less than once a week), 2 (once or twice a week), 3 (three to five times a week), and 4 (every night or almost daily). The SAGIC questionnaire also contained a new “don’t know” alternative (score 5) to the questions on symptoms based on the BNSQ. For the present analysis, available data on 18 relevant OSA symptoms, as well as self-reported diagnoses of medically treated hypertension, diabetes, and cardiovascular disease were included in the cluster analysis (see Supplementary Table S1 and Table 1 for additional details on symptom questions, definitions, and frequency).
Statistical analysis
Additional details on the statistical methods can be found in Supplementary Material. Continuous variables are summarized with means and standard deviations and compared using analysis of variance (ANOVA) or t tests, based on the number of groups compared. Categorical variables are summarized using frequencies and percentages and compared among clusters using chi-squared or Fisher’s exact tests. p-Values of <0.05 were considered statistically significant.
Clustering analysis within each sample was performed using latent class analysis (LCA), a statistical procedure for grouping individuals into a set of mutually exclusive latent classes (i.e. clusters) based on a collection of categorical measurements [41, 42]. As in the previous ISAC study [17], participants reporting symptoms at least once per week were classified as positive for a given symptom; individuals responding “don’t know” were classified as negative for the corresponding symptom. Sensitivity analyses performed in the original ISAC clustering analysis showed that OSA cluster definitions were robust to this threshold [17].
Given our goal of examining the reproducibility (within Iceland) and generalizability (outside of Iceland) of the OSA clusters identified in ISAC [17], we first examined the three-cluster solution in both SAGIC samples. In addition to examining the results of the three-cluster solution, to determine the optimal number of clusters in each sample, we used LCA to obtain solutions for 1 to 10 clusters and compared the resulting Bayesian Information Criterion (BIC) values. Lower BIC values indicate better model fit; thus, the “optimal clustering solution” was defined as the number of clusters that resulted in the lowest BIC. Symptom and demographic characteristics were summarized and compared across the clusters using ANOVA and chi-squared or Fisher’s exact tests. The symptoms and clinical interpretations, as well as the prevalences of the three-cluster solutions, were qualitatively compared with the original definitions described in ISAC [17].
Results
Sample characteristics
A total of 972 SAGIC patients recruited from international sleep clinics with an AHI ≥ 15 events per hour and available symptom questionnaire data were included in clustering analyses (Table 1). Participants were on average middle-aged (51.9 ± 12.9 years), predominantly male (70.3%), moderately obese (33.8 ± 8.1 kg/m2), and had severe OSA based on AHI (42.9 ± 26.8 events per hour). SAGIC is an ethnically diverse population, with 58.8% Caucasian, 21.1% Asian, 5.9% African/African American, 6.6% Central/South American, and 7.6% reporting other or multiple racial/ethnic groups.
Table 1 also compares the Icelandic (N = 215) and non-Icelandic (N = 757) SAGIC samples. Patients recruited from Iceland were generally older, less likely to be male and had less severe OSA than the non-Icelandic patients. There were differences in a number of clinical symptoms in the sample from Iceland compared with the SAGIC sample from outside of Iceland, including higher prevalences of disturbed sleep, RLS, and symptoms related to sleepiness or dozing. There were no significant differences in the prevalence of hypertension (p = 0.060), diabetes (p = 0.598), or cardiovascular disease (p = 0.253) between the two samples.
Validation of the three-symptom clusters in samples from Iceland
We first sought to replicate the ISAC clusters within the subset of the SAGIC sample from Iceland. When examining up to 10 clusters, the optimal result (based on BIC, see Supplementary Table S2) was the three-cluster solution, replicating the original finding in ISAC [17]. Moreover, both the clinical interpretations and prevalence of the three clusters were similar between the SAGIC samples from Iceland and ISAC, providing independent validation of the OSA clinical clusters in Iceland (Table 2).
Table 2.
Symptom summary for three-cluster solution in the SAGIC Iceland sample
| Variable | Cluster 1 | Cluster 2 | Cluster 3 | P* |
|---|---|---|---|---|
| Name | Disturbed sleep | Minimally symptomatic | Excessively sleepy | |
| N (%) | 72 (33.5%) | 62 (28.8%) | 81 (37.7%) | – |
| Clustering variables | ||||
| Epworth Sleepiness Scale (ESS) | 8.2 ± 3.3 | 7.7 ± 3.7 | 15.3 ± 3.2 | <0.0001 |
| Symptom, % | ||||
| I feel rested upon waking | 2.8 | 41.9 | 1.2 | <0.0001 |
| I feel sleepy during the day | 63.9 | 21.0 | 95.1 | <0.0001 |
| Physically tired during the day | 100.0 | 53.2 | 96.3 | <0.0001 |
| Fall asleep while watching TV | 56.9 | 62.9 | 97.5 | <0.0001 |
| Fall asleep involuntarily | 2.8 | 0.0 | 37.0 | <0.0001 |
| Take naps | 69.4 | 66.1 | 87.7 | 0.005 |
| Frequently doze while driving | 0.0 | 0.0 | 9.9 | 0.001 |
| Difficulty falling asleep | 70.8 | 19.4 | 30.9 | <0.0001 |
| Difficulty maintaining sleep | 95.8 | 41.7 | 79.0 | <0.0001 |
| Waking too early | 61.1 | 27.9 | 39.5 | 0.0004 |
| Restless in my sleep | 91.7 | 41.9 | 72.8 | <0.0001 |
| Wake up with a headache | 56.9 | 8.1 | 35.8 | <0.0001 |
| Perspire heavily at night | 56.9 | 16.1 | 48.1 | <0.0001 |
| Wake up suddenly and can’t breathe | 26.4 | 24.6 | 70.4 | <0.0001 |
| Been told I stop breathing | 45.8 | 51.6 | 81.5 | <0.0001 |
| Snoring | 0.001 | |||
| No snoring | 5.6 | 11.3 | 6.2 | |
| Snoring that does not disturb partner | 16.7 | 24.2 | 2.5 | |
| Snoring that disturbs partner | 77.8 | 64.5 | 91.4 | |
| Restless legs syndrome | 23.6 | 14.5 | 21.0 | 0.406 |
| Hypertension | 59.7 | 54.8 | 45.0 | 0.179 |
| Diabetes | 11.1 | 21.0 | 16.0 | 0.296 |
| Cardiovascular disease | 8.3 | 12.9 | 18.5 | 0.181 |
| Demographic variables | ||||
| Age, years | 54.6 ± 10.3 | 57.9 ± 9.4 | 53.8 ± 10.9 | 0.057 |
| Male, % | 43.1 | 66.1 | 74.1 | 0.0003 |
| BMI, kg/m2 | 33.5 ± 5.9 | 33.9 ± 5.6 | 34.5 ± 7.5 | 0.609 |
| AHI, events/hr | 27.2 ± 10.8 | 30.2 ± 13.9 | 31.9 ± 15.3 | 0.094 |
| ODI, events/hr | 25.4 ± 11.1 | 27.3 ± 13.8 | 29.6 ± 14.8 | 0.148 |
*p-Value from analysis of variance and chi-squared or Fisher’s exact tests comparing continuous and categorical variables, respectively, across clusters.
BMI = body mass index; AHI = apnea–hypopnea index; ODI = oxygen desaturation index.
Similar OSA symptom clusters within the independent SAGIC sample from Iceland.
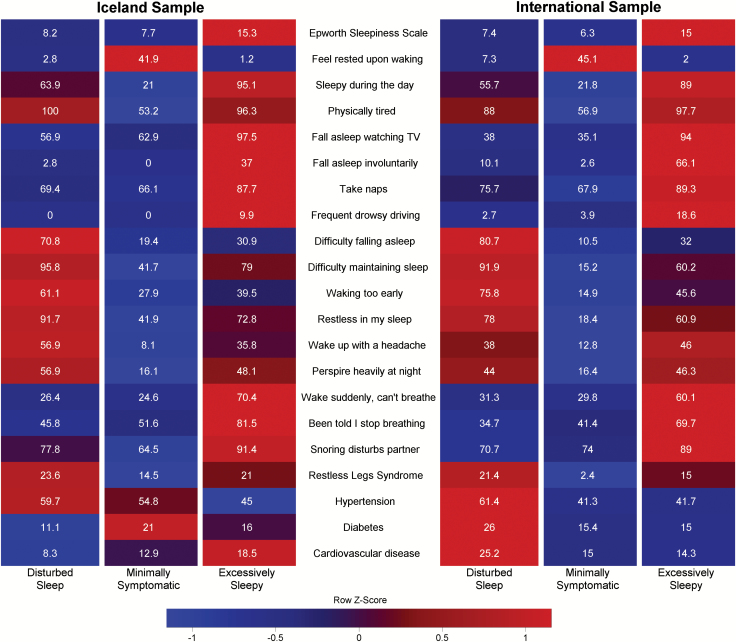
The symptom characteristics of the three-cluster definitions in SAGIC participants from Iceland were similar to those in the original ISAC study (Table 2 and Figure 1), namely, the disturbed sleep, minimally symptomatic, and excessively sleepy.
Figure 1.
Profiles of the three OSA clusters in Icelandic and International SAGIC samples. The relative differences in symptoms among the three OSA clusters (disturbed sleep, minimally symptomatic, and excessively sleepy) are shown in heatmaps within the Icelandic and International samples, separately, where blue indicates a lower relative prevalence/burden and red a higher relative symptom burden. The heatmaps illustrate both the higher prevalence of reported sleepiness and upper airway symptoms in the excessively sleepy and the higher rates of restless sleep and insomnia symptoms in the disturbed sleep. We also see the relative lower reported symptom burden in the minimally symptomatic cluster. Importantly, note the clear similarities in symptom profiles between the Icelandic and International samples of patients. This strongly supports the notion that these OSA subtypes are reproducible both inside and outside of Iceland.
Cluster 1 (N = 72 [33.5%]) is similar to the ISAC disturbed sleep cluster, with the highest rates of difficulty falling asleep (70.8%), difficulty maintaining sleep (95.8%), waking too early (61.1%), and restless sleep (91.7%). This cluster had relatively low rates of reported daytime sleepiness. Rates of upper airway symptoms (snoring, witnessed apneas, and waking suddenly unable to breathe) in this cluster were more similar to those in the minimally symptomatic cluster, described below.
Cluster 2 (N = 62 [28.8%]) is similar to the ISAC minimally symptomatic cluster. This cluster had the lowest symptom burden and the highest prevalence of feeling rested upon waking. In contrast to the results in ISAC, the prevalence of comorbidities was not significantly higher in this cluster within the Iceland SAGIC participants (Table 2).
Finally, Cluster 3 (N = 81 [37.7%]) is similar to the ISAC excessively sleepy cluster. This cluster had an average ESS of 15.3 and high prevalence of feeling sleepy, dozing, and napping. This group also contained all participants who reported dozing while driving (9.9%). The excessively sleepy cluster also had the highest rates of upper airway symptoms.
Comparable symptom cluster prevalence in the two samples from Iceland.
In addition to comparable symptoms, the three clusters had similar prevalence in ISAC and the SAGIC participants from Iceland (p = 0.340 for overall comparison). In both samples, the excessively sleepy cluster was the most prevalent (42.6% in ISAC and 37.7% in SAGIC; p = 0.194), followed by the disturbed sleep cluster (32.7% and 33.5%, p = 0.832), and the minimally symptomatic group the least prevalent (24.7% and 28.8%, p = 0.215).
Demographic characteristics of the three symptom clusters.
There were some differences in demographic factors between the three clusters (Table 2), which could suggest distinct OSA manifestations in certain demographic subgroups. Specifically, there was a significant difference in gender (p = 0.0003) and a borderline association with age (p = 0.057) across the clusters. The disturbed sleep cluster had the highest proportion of females, whereas the minimally symptomatic cluster was 3–4 years older than the other clusters. We observed no significant differences in body mass index (BMI) or OSA severity among clusters. These demographic associations were similar to those noted in the original ISAC study [17], including an older age in the minimally symptomatic and no differences in BMI or OSA severity.
Generalization of the three-symptom clusters in the international sample
Next, we examined the results of a three-cluster solution in the more ethnically diverse SAGIC population from outside of Iceland (Table 3 and Figure 1). Within this multinational sample, the three OSA clusters showed similar clinical symptom definitions as those originally defined in ISAC [17]; however, there was a difference in the prevalence of the clusters. In addition, there are clear similarities in the symptom burdens of the three clusters generated from the SAGIC Iceland sample and this international SAGIC sample (Figure 1).
Table 3.
Symptom summary for three-cluster solution in the international SAGIC sample
| Variable | Cluster 1 | Cluster 2 | Cluster 3 | P* |
|---|---|---|---|---|
| Name | Disturbed sleep | Minimally symptomatic | Excessively sleepy | |
| N (%) | 150 (19.8) | 306 (40.4) | 301 (39.8) | – |
| Clustering variables | ||||
| Epworth Sleepiness Scale | 7.4 ± 3.6 | 6.3 ± 3.8 | 15.0 ± 4.0 | <0.0001 |
| Symptom, % | ||||
| I feel rested upon waking | 7.3 | 45.1 | 2.0 | <0.0001 |
| I feel sleepy during the day | 55.7 | 21.8 | 89.0 | <0.0001 |
| Physically tired during the day | 88.0 | 56.9 | 97.7 | <0.0001 |
| Fall asleep while watching TV | 38.0 | 35.1 | 94.0 | <0.0001 |
| Fall asleep involuntarily | 10.1 | 2.6 | 66.1 | <0.0001 |
| Take naps | 75.7 | 67.9 | 89.3 | <0.0001 |
| Frequently doze while driving | 2.7 | 3.9 | 18.6 | <0.0001 |
| Difficulty falling asleep | 80.7 | 10.5 | 32.0 | <0.0001 |
| Difficulty maintaining sleep | 91.9 | 15.2 | 60.2 | <0.0001 |
| Waking too early | 75.8 | 14.9 | 45.6 | <0.0001 |
| Restless in my sleep | 78.0 | 18.4 | 60.9 | <0.0001 |
| Wake up with a headache | 38.0 | 12.8 | 46.0 | <0.0001 |
| Perspire heavily at night | 44.0 | 16.4 | 46.3 | <0.0001 |
| Wake up suddenly and can’t breathe | 31.3 | 29.8 | 60.1 | <0.0001 |
| Been told I stop breathing | 34.7 | 41.4 | 69.7 | <0.0001 |
| Snoring | <0.0001 | |||
| No snoring | 18.0 | 18.8 | 2.0 | |
| Snoring that does not disturb partner | 11.3 | 7.2 | 9.0 | |
| Snoring that disturbs partner | 70.7 | 74.0 | 89.0 | |
| Restless legs syndrome | 21.4 | 2.4 | 15.0 | <0.0001 |
| Hypertension | 61.4 | 41.3 | 41.7 | <0.0001 |
| Diabetes | 26.0 | 15.4 | 15.0 | 0.008 |
| Cardiovascular disease | 25.2 | 15.0 | 14.3 | 0.009 |
| Demographic variables | ||||
| Age, years | 54.0 ± 12.6 | 51.2 ± 14.2 | 49.1 ± 12.5 | 0.001 |
| Male, % | 63.3 | 80.4 | 69.8 | 0.0002 |
| BMI, kg/m2 | 35.5 ± 8.8 | 32.2 ± 7.9 | 34.5 ± 8.7 | 0.0001 |
| AHI, events/hr | 46.4 ± 29.6 | 44.8 ± 24.9 | 48.4 ± 31.0 | 0.298 |
| ODI, events/hr | 43.2 ± 29.5 | 42.7 ± 26.2 | 45.8 ± 30.8 | 0.393 |
| Ethnicity, % | 0.0009 | |||
| Caucasian | 58.4 | 41.1 | 48.5 | |
| African/African American | 10.1 | 5.9 | 8.0 | |
| Asian | 16.8 | 34.9 | 24.3 | |
| Central/South American | 4.7 | 9.9 | 9.0 | |
| Other | 10.1 | 8.2 | 10.3 | |
*p-Value from analysis of variance or chi-squared tests comparing continuous and categorical variables, respectively, across clusters.
BMI = body mass index; AHI = apnea–hypopnea index; ODI = oxygen desaturation index.
Symptoms of the three clusters from ISAC generalize to international SAGIC population.
We found that the three clusters defined in the ISAC sample, i.e. disturbed sleep, minimally symptomatic, and excessively sleepy, were present in the international population of SAGIC participants from outside of Iceland (Table 3 and Figure 1).
Cluster 1 (N = 150 [19.8%]) is similar to the ISAC disturbed sleep cluster, with the highest rates of difficulty falling asleep (80.7%), difficulty maintaining sleep (91.9%), waking too early (75.8%), and restless sleep (78.0%), and only modest levels of daytime sleepiness. However, in contrast to the ISAC findings [17], this disturbed sleep cluster also had the highest rates of hypertension, diabetes, and cardiovascular disease.
Cluster 2 (N = 306 [40.4%]) had the lowest proportion of sleepiness-related complaints (average ESS of 6.3), the highest proportion of patients reporting feeling rested upon waking, and the lowest prevalence of insomnia-related symptoms. Thus, this cluster is similar to the ISAC minimally symptomatic. As in the SAGIC sample from Iceland, but in contrast to the results in ISAC, this cluster did not have higher rates of comorbidities.
Finally, Cluster 3 (N = 301 [39.8%]) is similar to the ISAC excessively sleepy cluster, with an average ESS of 15.0 and the highest rates of feeling sleepy and dozing. As in ISAC, this cluster also had the highest rates of upper airway symptoms (e.g. snoring, witnessed apneas, and waking suddenly unable to breathe).
Differences in cluster prevalence between ISAC and ethnically diverse SAGIC sample.
Although the three-cluster solution generalizes to the SAGIC sample from outside of Iceland, there were differences in cluster prevalence (p < 0.0001); this may reflect ethnic differences in symptom occurrence or reporting. Compared with ISAC, the SAGIC sample from outside of Iceland had similar prevalence of the excessively sleepy cluster (39.8% vs. 42.6%; p = 0.256), lower prevalence of the disturbed sleep cluster (19.8% vs. 32.7%; p < 0.0001), and higher prevalence of the minimally symptomatic cluster (40.4% vs. 24.7%; p < 0.0001).
Demographic characteristics of the three clusters in SAGIC participants from outside of Iceland.
When examining demographics and OSA severity across the three clusters (Table 3), there were no differences in AHI (p = 0.298) or oxygen desaturation index (ODI; p = 0.393), as in the original ISAC analysis [17]; all clusters had severe OSA on average. Significant differences among the clusters were observed in age, gender, BMI, and ethnicity; these demographics could be valuable when evaluating an individual patient with OSA. Whereas in Iceland the minimally symptomatic group was the oldest on average [17], in this international sample the disturbed sleep cluster was the oldest (54.0 years) and the excessively sleepy the youngest (49.1 years). The minimally symptomatic cluster showed the highest proportion of males (80.4%) and the lowest BMI (32.2 kg/m2), as well as the lowest proportion of Caucasian (41.1%) and highest percentage of Asian (34.9%) participants.
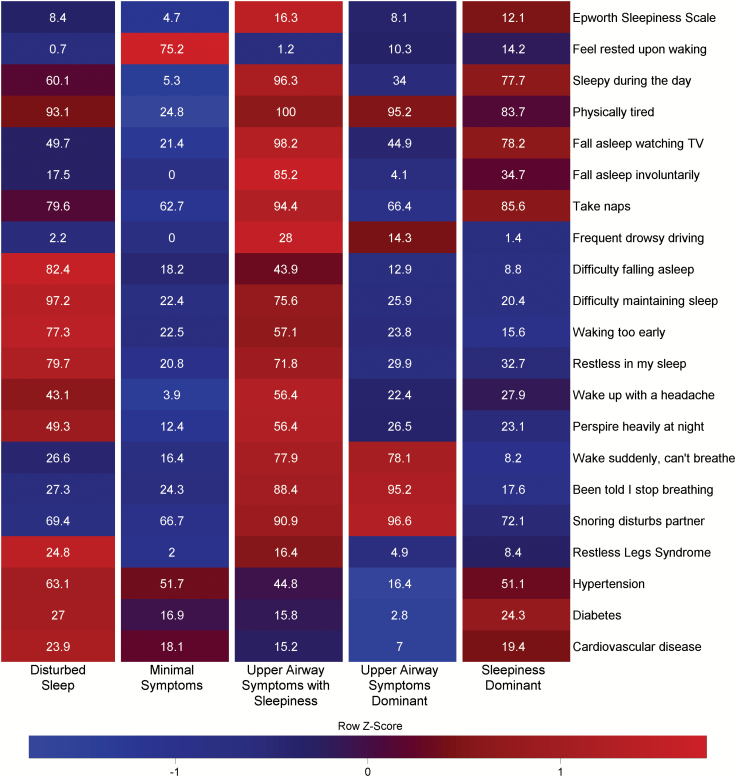
Optimal symptom cluster solution in the international sample
Based on statistical criteria (lowest BIC value), the optimal clustering solution for the international SAGIC sample was five clusters rather than three (Supplementary Table S3). Reasonable clinical interpretations were derived for all five clusters, as discussed below (Table 4 and Figure 2). Moreover, relationships between this optimal five-cluster solution and the three-cluster solution help us to understand clinical significance (Figure 3 and Supplementary Figure S1). Ultimately, the five-cluster solution may provide additional clinical insights into major complaints for a given patient and, relatedly, the primary reasons for sleep center referral.
Table 4.
Symptom summary for optimal clusters in the international SAGIC sample
| Variable | Cluster 1 | Cluster 2 | Cluster 3 | Cluster 4 | Cluster 5 | P* |
|---|---|---|---|---|---|---|
| Name | Disturbed sleep | Minimal symptoms | Upper airway symptoms with sleepiness | Upper airway symptoms dominant | Sleepiness dominant | – |
| N (%) | 144 (19.0) | 154 (20.3) | 164 (21.7) | 147 (19.4) | 148 (19.6) | – |
| Epworth Sleepiness Scale | 8.4 ± 3.9 | 4.7 ± 2.7 | 16.3 ± 3.7 | 8.1 ± 4.5 | 12.1 ± 4.4 | <0.0001 |
| Symptom, % | ||||||
| I feel rested upon waking | 0.7 | 75.2 | 1.2 | 10.3 | 14.2 | <0.0001 |
| I feel sleepy during the day | 60.1 | 5.3 | 96.3 | 34.0 | 77.7 | <0.0001 |
| Physically tired during the day | 93.1 | 24.8 | 100.0 | 95.2 | 83.7 | <0.0001 |
| Fall asleep while watching TV | 49.7 | 21.4 | 98.2 | 44.9 | 78.2 | <0.0001 |
| Fall asleep involuntarily | 17.5 | 0.0 | 85.2 | 4.1 | 35.7 | <0.0001 |
| Take naps | 79.6 | 62.7 | 94.4 | 66.4 | 85.6 | <0.0001 |
| Frequently doze while driving | 2.2 | 0.0 | 28.0 | 14.3 | 1.4 | <0.0001 |
| Difficulty falling asleep | 82.4 | 18.2 | 43.9 | 12.9 | 8.8 | <0.0001 |
| Difficulty maintaining sleep | 97.2 | 22.4 | 75.6 | 25.9 | 20.4 | <0.0001 |
| Waking too early | 77.3 | 22.5 | 57.1 | 23.8 | 15.6 | <0.0001 |
| Restless in my sleep | 79.7 | 20.8 | 71.8 | 29.9 | 32.7 | <0.0001 |
| Wake up with a headache | 43.1 | 3.9 | 56.4 | 22.4 | 27.9 | <0.0001 |
| Perspire heavily at night | 49.3 | 12.4 | 56.4 | 26.5 | 23.1 | <0.0001 |
| Wake up suddenly and can’t breathe | 26.6 | 16.4 | 77.9 | 78.1 | 8.2 | <0.0001 |
| Been told I stop breathing | 27.3 | 24.3 | 88.4 | 95.2 | 17.6 | <0.0001 |
| Snoring | <0.0001 | |||||
| No snoring | 14.6 | 26.1 | 0.6 | 0.0 | 19.1 | |
| Snoring that does not disturb partner | 16.0 | 7.2 | 8.5 | 3.4 | 8.8 | |
| Snoring that disturbs partner | 69.4 | 66.7 | 90.9 | 96.6 | 72.1 | |
| Restless legs syndrome | 24.8 | 2.0 | 16.4 | 4.9 | 8.4 | <0.0001 |
| Hypertension | 63.1 | 51.7 | 44.8 | 16.4 | 51.1 | <0.0001 |
| Diabetes | 27.0 | 16.9 | 15.8 | 2.8 | 24.3 | <0.0001 |
| Cardiovascular disease | 23.9 | 18.1 | 15.2 | 7.0 | 19.4 | 0.003 |
*p-Value from analysis of variance or chi-squared tests comparing continuous or categorical variables, respectively, across clusters.
Figure 2.
Profiles of the five optimal OSA clusters in the International SAGIC sample. The relative symptom burden is shown in a heatmap for each of the five optimal clusters (disturbed sleep, minimal symptoms, upper airway symptoms with sleepiness, upper airway symptoms dominant, and sleepiness dominant), ranging from low burden (blue) to high burden (red). In addition to illustrating the symptomatic differences among the five clusters, note the similarities between the heatmaps for the disturbed sleep, minimal symptoms, and upper airway symptoms with sleepiness and the corresponding heatmaps for the three-cluster solutions in Figure 1.
Figure 3.
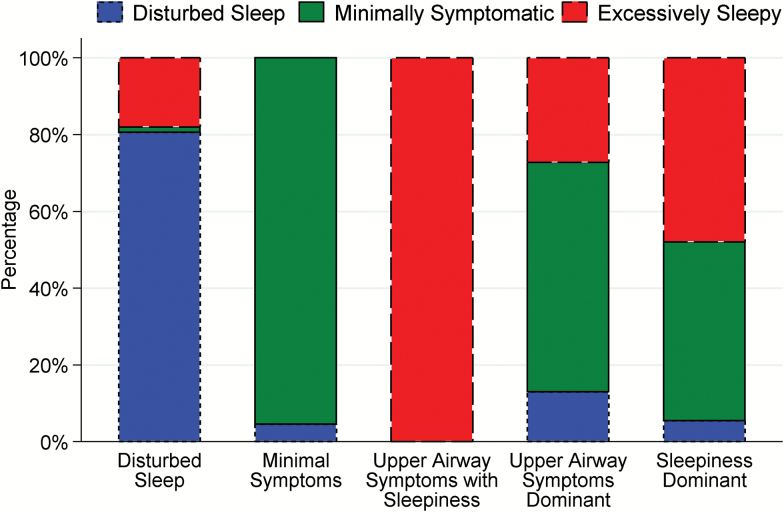
Distribution of the a priori three–OSA clusters within the five optimal OSA clusters found in the International SAGIC sample. The proportions of patients from the a priori three–cluster solution within each of the optimal five clusters are shown. We note that >80% of the disturbed sleep, minimal symptoms, and upper airway symptoms with sleepiness clusters are made up of patients from the similar group in the three-cluster solution, whereas the new upper airway symptoms dominant and sleepiness dominant clusters consist primarily of a mixture of patients from the minimally symptomatic and excessively sleepy clusters.
The five-cluster solution identifies additional subgroups characterized by primary symptom complaints.
In the five-cluster solution, three clusters were similar to the disturbed sleep, minimally symptomatic, and excessively sleepy clusters previously described; greater than eighty percent of individuals in these optimal clusters came from the similar cluster in the three-cluster design (Figure 3). The two new clusters were defined by predominance of upper airway symptoms (Cluster 4) or sleepiness (Cluster 5), with few other symptoms. These two clusters included a mixture of patients from each of the original three clusters, although the majority came from the minimally symptomatic and excessively sleepy clusters (Figure 3 and Supplementary Figure S1).
Specifically, Cluster 1 (N = 144 [19.0%]) is characterized primarily by disturbed sleep symptoms, and 80.6% of this cluster was from the similar disturbed sleep cluster in the three-cluster solution (Figure 3). A large majority of patients in this cluster reported insomnia-related symptoms, including 82.4% difficulty falling asleep, 97.2% difficulty maintaining sleep, 77.3% waking too early, and 79.7% reporting restless sleep. This cluster also had the highest rates of hypertension, diabetes, and cardiovascular disease.
Cluster 2 (N = 154 [20.3%]) consists of patients with OSA with minimal symptoms, and 95.5% of this subgroup fell within the minimally symptomatic cluster in the three-cluster solution (Figure 3). Despite having moderate–severe OSA, most symptoms included in our clustering algorithm were reported by less than 25% of the individuals in this minimal symptoms cluster. These patients had the lowest average ESS (4.7 ± 2.7), 75.2% reported feeling rested upon waking, and 26.1% reported no snoring. Overall, patients in this cluster appear resilient to usual clinical features of OSA, and thus, the impact of disease may not be reflected in measured symptoms.
Cluster 3 (N = 164 [21.7%]) represents the classic presentation of OSA, i.e. upper airway symptoms with sleepiness. All members of this cluster were part of the excessively sleepy cluster in the three-cluster solution (Figure 3), suggesting that it represents a more well-defined subset of the cluster identified in ISAC. Individuals in this cluster had the most severe sleepiness, with an average ESS of 16.3 and 28.0% reporting frequent dozing when driving, as well as the second highest rates of sleep disturbance (e.g. restless sleep and difficulty maintaining sleep). This cluster also reported high rates of upper airway symptoms (e.g. snoring, witnessed apneas, and waking suddenly unable to breathe).
Cluster 4 (N = 147 [19.4%]) includes patients whose symptoms are dominated by indications of upper airway obstruction and thus is characterized as upper airway symptoms dominant OSA. As shown in Figure 3, a majority of this cluster (59.9%) was classified as minimally symptomatic in the three-cluster solution, whereas 27.2% were in the excessively sleepy and 12.9% in the disturbed sleep clusters. This cluster had high rates of snoring, witnessed apneas, and waking suddenly unable to breathe, despite comparatively low rates of sleepiness or insomnia-related symptoms. Also, this cluster has the lowest prevalence of hypertension, diabetes, and cardiovascular disease of all the five clusters. Thus, individuals in this cluster are most likely to have been referred to sleep clinics due to recognized upper airway symptoms of OSA.
Finally, Cluster 5 (N = 148 [19.6%]) includes individuals with excessive sleepiness, but a relative absence of symptoms of upper airway obstruction; thus, this cluster is labeled as sleepiness dominant OSA. This cluster was a mix of patients from the minimally symptomatic (46.6%) and excessively sleepy (48.0%) clusters in the three-cluster solution (Figure 3). Individuals in this cluster met clinical thresholds for subjective sleepiness (mean ESS of 12.1) and had the second highest rates of daytime sleepiness, dozing, and taking naps. Given these symptoms, combined with lower rates of symptoms of upper airway obstruction, this cluster of patients may have been referred to the clinic due to unexplained daytime sleepiness.
Demographic characteristics of the five clusters in SAGIC participants from outside of Iceland.
We observed statistically significant differences in age, gender, BMI, and ethnicity among the five clusters (Table 5). There were also differences in OSA severity, although all clusters had severe disease on average. The upper airway symptoms dominant cluster was the youngest (44.6 years), least obese (30.6 kg/m2), and had the highest proportion of both males (89.1%) and participants of Asian ethnicity (43.8%). In contrast, the disturbed sleep cluster was the oldest (54.5 years), the most obese (35.9 kg/m2), and had the highest proportions of females (43.1%), Caucasians (59.4%), and African/African Americans (12.6%) compared with the other clusters. Overall, the prevalence of the upper airway symptoms dominant (p < 0.0001) and disturbed sleep (p < 0.0001) clusters differed significantly across ethnicities, whereas prevalences of the other three clusters were similar across ethnic groups (Supplementary Table S4). The clusters of upper airway symptoms dominant and upper airway symptoms with sleepiness had the most severe OSA, with AHI and ODI values 5–10 events per hour higher than the other three clusters. Overall, differences in these characteristics may reflect distinct manifestations of OSA based on clinically observed traits such as gender, obesity, and ethnicity.
Table 5.
Demographic characteristics of optimal clusters in the international SAGIC sample
| Variable | Cluster 1 | Cluster 2 | Cluster 3 | Cluster 4 | Cluster 5 | P* |
|---|---|---|---|---|---|---|
| Name | Disturbed sleep | Minimal symptoms | Upper airway symptoms with sleepiness | Upper airway symptoms dominant | Sleepiness dominant | – |
| N (%) | 144 (19.0) | 154 (20.3) | 164 (21.7) | 147 (19.4) | 148 (19.6) | – |
| Age, years | 54.5 ± 12.7 | 54.2 ± 13.9 | 49.5 ± 12.0 | 44.6 ± 12.1 | 51.9 ± 13.6 | <0.0001 |
| Male, % | 56.9 | 78.6 | 70.7 | 89.1 | 68.2 | <0.0001 |
| BMI, kg/m2 | 35.9 ± 8.3 | 33.3 ± 8.9 | 35.1 ± 8.9 | 30.6 ± 6.3 | 34.0 ± 8.7 | <0.0001 |
| AHI, events/hr | 44.7 ± 30.8 | 43.5 ± 24.6 | 51.4 ± 31.4 | 50.6 ± 26.0 | 42.0 ± 27.4 | 0.007 |
| ODI, events/hr | 40.6 ± 30.9 | 40.1 ± 25.7 | 48.1 ± 30.3 | 50.5 ± 27.3 | 40.1 ± 27.9 | 0.001 |
| Ethnicity, % | <0.0001 | |||||
| Caucasian | 59.4 | 48.4 | 51.8 | 35.6 | 41.9 | |
| African/African American | 12.6 | 5.2 | 7.9 | 2.7 | 9.5 | |
| Asian | 13.3 | 25.5 | 22.6 | 43.8 | 30.4 | |
| Central/South American | 5.6 | 8.5 | 7.9 | 11.0 | 9.5 | |
| Other | 9.1 | 12.4 | 9.8 | 6.9 | 8.8 |
*p-Value from analysis of variance (continuous) and chi-squared test (categorical) comparing values across clusters.
BMI = body mass index; AHI = apnea–hypopnea index; ODI = oxygen desaturation index.
Discussion
This study represents an essential next step in understanding OSA clinical presentation clusters, building on those originally described in the ISAC [17]. Using an international sample of apneics recruited from sleep clinics in the SAGIC, we demonstrate the reproducibility of the disturbed sleep, minimally symptomatic, and excessively sleepy OSA clusters within an independent sample from Iceland and in a more ethnically diverse sample from outside of Iceland. Although the three clinical subtypes were generalizable, our results suggested more specific OSA clinical clusters within the international SAGIC sample, furthering our understanding of OSA heterogeneity. Specifically, the optimal solution resulted in five OSA clusters, three of which were similar to the disturbed sleep, minimally symptomatic, and excessively sleepy clusters defined in ISAC—labeled here as disturbed sleep, minimal symptoms, and upper airway symptoms with sleepiness—and two new subtypes associated with a paucity of other symptoms—labeled as upper airway symptoms dominant and sleepiness dominant. Overall, this study provides a novel approach to better characterize patients with OSA presenting at sleep clinics worldwide. This information can help inform personalized medicine approaches to OSA treatment by allowing clinicians to focus interventions on the most relevant OSA symptoms and consequences within an individual patient.
The observation that the clinical clusters defined in ISAC [17] both replicate with respect to symptom characteristics and prevalence in an independent Icelandic sample and generalize to other ethnicities provides strong evidence that these are true disease clusters among patients with OSA. Although five OSA clusters proved to be the optimal number from a statistical perspective in the SAGIC samples from outside of Iceland, we noted clear similarities with the three-cluster solution from ISAC. Both solutions identified individuals with disturbed sleep, a lack of traditional symptoms, and the classical OSA presentation of excessive sleepiness and upper airway symptoms; a large proportion of patients remained similarly defined in both the three- and five-cluster solutions. Thus, utilizing three or five clusters may provide similar benefits in clinical practice. The added clinical benefit of the five OSA clusters appears to be improved accuracy with respect to primary symptom complaints; the new clusters of upper airway symptoms dominant and sleepiness dominant included patients with a narrower symptom spectrum. The ability to more quickly identify these main symptoms could improve efficiency in both diagnosis and treatment decisions.
Comparisons to phenotypes suggested by prior OSA clustering studies
Following the initial clustering in ISAC [17], other publications have examined OSA clusters [18–21]. For example, a study in Greek patients (N = 1472) utilized a combination of the Charlson Comorbidity Index and OSA severity to identify six clusters ranging from healthy participants with sleep-related disturbances and moderate somnolence to severe OSA with severe comorbidities, sleepiness, and obesity [18]. Another study of 198 patients with OSA from southern Italy identified three clusters driven by age, obesity, and OSA/hypoxemia severity [19]. Finally, a large study examining symptoms, demographics, disease severity, comorbidities, and environmental risk factors in 18,263 moderate–severe apneics from France [20] yielded six clusters, labeled as follows: (1) young symptomatic, (2) older obese, (3) multidisease old obese, (4) young snorers, (5) drowsy obese, and (6) multidisease obese symptomatic. Although each study falls under the umbrella of OSA phenotyping, there are predictable distinctions related to the differences in underlying populations and the variables used to determine clusters. However, there are also similarities among studies. Of particular note are parallels between results found in the present article and the large clustering study in France [20]. The young snorers show demographic parallels to SAGIC individuals labeled as upper airway symptoms dominant; both clusters were younger, less obese, and had the highest proportion of males. Similarly, the SAGIC cluster of sleepiness dominant parallels the drowsy obese in France, and the minimal symptoms cluster, which was the oldest and moderately obese, is similar to the older obese. Finally, the multidisease old obese and multidisease obese symptomatic defined in France are similar to the SAGIC clusters of disturbed sleep and upper airway symptoms with sleepiness. Although these similarities support reproducible underlying OSA clusters, the absence of information on insomnia-related symptoms in the French study highlights the impact of methodological differences. Given our results and other research [43], this prior study may have missed an important distinguishing characteristic among patients with OSA, namely, comorbid insomnia.
Our choice to focus on clinical symptoms within moderate–severe patients with OSA reflects the goal of moving beyond typical severity and demographic metrics used to characterize OSA and towards an understanding of individual differences in clinical presentation. In contrast, including disease severity as a clustering input variable, as well as mild OSA and control participants in study populations, has resulted in disease clusters that differ primarily by existing OSA severity metrics. Similarly, studies utilizing demographic variables (e.g. age and BMI) to determine clusters have found subtypes defined by differences in these usual metrics, rather than leveraging these measures to help understand the etiology of independently defined clusters. Ultimately, the limited difference in OSA severity between our clusters underscores an important clinical reality—two patients with the same physiological disease severity may present with distinct clinical symptoms.
Implications of differences in cluster prevalence based on demographic factors
Another important aspect of the current analysis is the ethnic diversity available in SAGIC. For the three OSA clusters originally described in ISAC, nearly half of Asian and Central/South American patients displayed the minimally symptomatic subtype; these patients were less likely to display the disturbed sleep cluster. Conversely, the distributions of the three clusters among Caucasians and African/African Americans were generally similar. For the optimal five OSA clusters, nearly one-third of Asian patients fell into the upper airway symptoms dominant group. This cluster was least prevalent in African/African-American individuals, who were most likely to fall into the disturbed sleep cluster. Caucasian participants showed a relatively equal distribution across the five clusters, whereas Central/South Americans were least likely to display the disturbed sleep cluster, but showed similar prevalence across the other four clusters. These differences in cluster prevalence across ethnicities may reflect cultural or regional differences in symptom reporting [44, 45] or referral strategies and access to care, as well as previously identified differences in OSA etiology across ethnic groups [23–27].
Differences in age, gender, or obesity may provide similar insight into distinct disease etiologies or consequences, helping us to predict the most likely clinical presentations of OSA within a given patient. For example, we noted a consistent ordering of clusters with respect to mean age and prevalence of comorbidities. The upper airway symptoms dominant cluster showed the youngest age and least prevalence of comorbidities, followed by the upper airway symptoms with sleepiness cluster, the sleepiness dominant or minimal symptoms clusters, and the disturbed sleep cluster showing the oldest age and highest prevalence of comorbidities. Although only speculative, one explanation for this ordering is that the symptom profile changes with duration of undiagnosed disease (reflected imprecisely by age in our cohort), and the longer you have the disease, the more likely you are to develop an OSA-related comorbidity. Ultimately, recognizing clinical factors affecting the prevalence of specific clusters is important for both diagnosis and personalized disease management within a given individual or ethnic population.
Next steps for clusters in OSA: insights from other diseases
There is increasing awareness of the importance of characterizing distinct disease clusters within heterogeneous, complex disorders such as OSA. Findings from phenotyping studies in asthma [46] and COPD [47, 48], for example, offer helpful insights for the future of OSA clusters. In COPD [47, 48], clustering analysis has led to characterization of disease severity based not only on airflow limitation (forced expiratory volume in 1 second [FEV1]), but also on symptoms and risk of future exacerbations; this approach is being further extended to include treatable biological and clinical factors for optimizing personalized medicine approaches [47, 48]. A primary impetus for this change was the recognition that, while important, FEV1 is only weakly associated with symptoms and risk of future events [47, 48]. Similar observations have been made for the OSA clusters described here, which do not differ dramatically by the primary measure of disease severity—the AHI. This underscores the need to move beyond a single measure of OSA severity to characterize heterogeneity.
Relatedly, asthma [46] was initially defined as a single umbrella phenotype encompassing a wide degree of heterogeneous patient symptoms, severity, onset age, and inflammatory characteristics (including the role of T helper [TH2] immune elements). Recognizing this, studies have suggested different asthma phenotypes, including TH2-associated (e.g. early-onset allergic, late-onset persistent eosinophilic, and exercise-induced asthma) and non-TH2-associated (e.g., obesity-related and neutrophilic asthma) [46]. Importantly, these asthma phenotypes have implications for personalized treatments. For example, TH2-targeted therapies such as corticosteroids are likely to be most effective in TH2-associated asthma, whereas weight loss may be more effective in non-TH2, obesity-related asthma. Developing personalized treatment strategies is crucial for applying precision medicine techniques to OSA clinical care.
Implications of clusters on determining OSA treatment response
Understanding the implication of clinical clusters on treatment approaches, particularly for individuals or symptoms that do not respond to positive airway pressure (PAP), is an important next step. Recent studies have combined OSA phenotyping with assessment of treatment adherence and efficacy [21, 22], including a companion article, Changing Faces of OSA: Treatment Effects by Cluster Designation in the Icelandic Sleep Apnea Cohort [49].
In particular, this companion article utilizes follow-up data on the ISAC sample to examine differences in symptom responses after 2 years of PAP treatment among the clinical clusters defined at baseline [49]. In addition to a small increase in overall PAP adherence in the excessively sleepy cluster, there was evidence for differential OSA treatment response patterns related to initial OSA cluster. The excessively sleepy cluster showed a wide range of symptom improvements, whereas insomnia symptoms were more resistant to PAP therapy in the disturbed sleep group. Importantly, all three clusters, including the minimally symptomatic group, showed some benefit of treatment. Thus, results highlight the importance of considering initial clinical presentation to more accurately define treatment response within a given patient and not relying solely on typical OSA symptoms when recommending therapy.
Relatedly, Gagnadoux et al. utilized demographic, symptom, and comorbidity information to identify five clusters in a sample of 5983 patients with moderate–severe OSA [21]. Subsequently, they examined the relationship between OSA clusters and “successful CPAP treatment”—a composite endpoint of daily CPAP usage ≥4 hr and either a decrease in ESS of at least four points if baseline ESS≥11 or an increase in 36-item Short Form Health Survey (SF-36) energy/vitality of at least seven points. Based on this endpoint, clusters with the most severe OSA were more likely to respond to treatment. Similarly, a recent study using data from the European Sleep Apnea Database (ESADA) compared demographics, comorbidities, and PAP adherence among four a priori–defined clusters based on the combination of excessive daytime sleepiness (EDS), nocturnal sleep problems (insomnia), both, or neither in patients with AHI ≥ 5 events per hour [22]. In addition to confirming a higher rate of cardiovascular disease among patients with OSA with insomnia symptoms, as in our disturbed sleep cluster, results suggest that PAP adherence may be lower among patients exhibiting insomnia-like symptoms and higher among those with EDS [22]; a similar result has also been seen in Iceland [50].
Altogether, these studies support the utility of recognizing underlying OSA clusters in clinical care. Alternative treatment options may be required to achieve the desired efficacy within certain clusters, as well as cluster-specific definitions of successful treatment that more accurately capture an individual patient’s disease characteristics and response to therapy.
Strengths and limitations
Our present study represents an important follow-up to the original cluster analysis performed in ISAC. Replication of the original result and extending the definitions of these clusters to a more ethnically diverse sample are crucial steps towards understanding OSA heterogeneity and, thus, important strengths of this study. Other strengths include the participation of multiple investigators from internationally recognized sleep centers and the application of common questionnaires and phenotyping methodology across a diverse group of patients. The SAGIC sample represents a unique opportunity to understand ethnic similarities and dissimilarities with respect to the complex disease of OSA.
There are also limitations to the present study. The focus on patients with moderate–severe OSA means that the clusters found here may not be generalizable to patients with milder OSA. Similarly, reflecting the established demographic risk factors for OSA, the cohort was generally middle-aged, moderately obese, and predominantly male. Additional studies within populations that are younger (or, alternatively, of advanced age), less obese, or with more females would help further understand the generalizability of these clusters. There were differences in average AHI severity between the participants from Iceland and the sample from outside of Iceland; this likely reflects the impact of predominantly home-based sleep tests in Iceland compared with polysomnography at other sites [51]. Given the design of SAGIC, patients were recruited from clinical sleep centers and thus may not be representative of the general population, where there is likely a high prevalence of undiagnosed OSA. In fact, a recent population study in Iceland [32] observed a high prevalence of moderate–severe OSA, but found that participants identified in the general population generally had minimal symptoms. Thus, the less symptomatic clusters described here may be more prevalent in the general population. Similar to the ISAC study, we defined most symptoms as present if they were reported to occur at least 1–2 times per week. Although alternative definitions (e.g. at least three times per week) would alter the prevalence of characterized symptoms, sensitivity analyses in ISAC suggested subtypes are robust to this definition [17]. Similarly, our analyses utilized LCA, a specific clustering method that leverages categorical responses to determine clusters; other clustering methods could be considered in future analyses. Our study did not include all possible symptoms and comorbidities (e.g., depression, cognitive impairment, and obstructive lung disease) that may occur in patients with OSA. As discussed throughout this article, inclusion of these additional factors may lead to novel clusters. Nevertheless, results here support the existence of OSA clusters that are valid across ethnicities and international borders. New approaches need to be adopted to identify different clusters when they present and to develop personalized strategies to therapy.
Conclusion
This study both replicates and extends previously identified clinical presentation clusters of disturbed sleep, minimally symptomatic, and excessively sleepy OSA patients. Both the symptom characteristics and prevalence of these clusters were replicated in an independent sample of similar Icelandic ancestry as the original interrogation. Moreover, these clusters were shown to exist in a more ethnically diverse international sleep center population, albeit at a different prevalence. In extending the original result to five clusters in this ethnically diverse sample, we identified two more specific OSA clusters with upper airway symptoms dominant and sleepiness dominant, in addition to clusters similar to the three found in ISAC. Although these new clusters could provide some added clinical benefit by recognizing primary symptoms more easily, our results ultimately suggest that, regardless of the number of clusters, insomnia-related complaints, excessive sleepiness, and a lack of these symptoms are important characteristics distinguishing patients with OSA with similar disease severity. Differences in cluster prevalence and associations with ethnicity or demographics among the subtypes suggest that, as has been seen for OSA etiology, symptom reporting and perceived consequences of OSA may differ across ethnic groups. Future studies should explore targeted interventions implied by these clusters, as well as examine the utility of incorporating biological or genetic factors when defining OSA clusters. It will be essential to develop clinical tools that efficiently classify a new OSA patient presenting at the sleep clinic into the appropriate cluster. Ultimately, this understanding should facilitate personalized medicine approaches in OSA patients.
Supplementary Material
Supplementary material is available at SLEEP online.
Funding
Research at the University of Pennsylvania was supported by a Program Project Grant from the National Institutes of Health (P01 HL094307). Dr. Bittencourt has a grant number 401569/2016-0 from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq). The project was also supported by Award Number Grant UL1TR001070 from the National Center For Advancing Translational Sciences; the content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Advancing Translational Sciences or the National Institutes of Health.
Acknowledgments
We thank the participants, study recruiters, technologists, and research team involved in the SAGIC project at each site, including Beth Staley, Sarah Leinwand, Dr. Ingo Fietze, Maria Franczyk, Sigrún Guðmundsdóttir, Lovísa Guðmundsdóttir, Hjördís Sigrún Pálsdóttir, Kristín Anna Ólafsdóttir, and Dr. Erla Björnsdóttir.
Conflict of interest statement. Dr. Arnardottir is a part-time consultant for Nox Medical and has received honorarium from Weinmann. Dr. Cistulli has an appointment to an endowed academic Chair at the University of Sydney that was created from ResMed funding. He has received research support from ResMed, SomnoMed, and Zephyr Sleep Technologies. He has been a consultant/adviser to Zephyr Sleep Technologies, NovoNordisk, and Fisher & Paykel Healthcare. Dr. Pack is The John L. Miclot Professor of Medicine at the University of Pennsylvania; funds for this endowment were provided by the Philips Respironics Foundation. Dr. Penzel reports grant support from Cidelec, Itamar, Resmed, Philips, Heinen and Loewenstein, and Weinmann, as well as speaker support from Itamar, Somnodent, and Weinmann. All other authors report no conflicts of interest related to the present manuscript.
References
- 1. Peppard PE, et al. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013; 177(9): 1006–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Pack AI, et al. Obstructive sleep apnea and cardiovascular disease: a perspective and future directions. Prog Cardiovasc Dis. 2009; 51(5): 434–451. [DOI] [PubMed] [Google Scholar]
- 3. McNicholas WT, et al. ; Management Committee of EU COST ACTION B26 Sleep apnoea as an independent risk factor for cardiovascular disease: current evidence, basic mechanisms and research priorities. Eur Respir J. 2007; 29(1): 156–178. [DOI] [PubMed] [Google Scholar]
- 4. Drager LF, et al. Early signs of atherosclerosis in obstructive sleep apnea. Am J Respir Crit Care Med. 2005; 172(5): 613–618. [DOI] [PubMed] [Google Scholar]
- 5. Savransky V, et al. Chronic intermittent hypoxia induces atherosclerosis. Am J Respir Crit Care Med. 2007; 175(12): 1290–1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Marin JM, et al. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005; 365(9464): 1046–1053. [DOI] [PubMed] [Google Scholar]
- 7. Gottlieb DJ, et al. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: the sleep heart health study. Circulation. 2010; 122(4): 352–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shahar E, et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med. 2001; 163(1): 19–25. [DOI] [PubMed] [Google Scholar]
- 9. Redline S, et al. Obstructive sleep apnea-hypopnea and incident stroke: the sleep heart health study. Am J Respir Crit Care Med. 2010; 182(2): 269–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Marshall NS, et al. Sleep apnea and 20-year follow-up for all-cause mortality, stroke, and cancer incidence and mortality in the Busselton Health Study cohort. J Clin Sleep Med. 2014; 10(4): 355–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Arble DM, et al. Impact of sleep and circadian disruption on energy balance and diabetes: a summary of workshop discussions. Sleep. 2015; 38(12): 1849–1860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pamidi S, et al. Obstructive sleep apnea and type 2 diabetes: is there a link?Front Neurol. 2012; 3: 126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Yaffe K, et al. Sleep-disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women. JAMA. 2011; 306(6): 613–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Campos-Rodriguez F, et al. ; Spanish Sleep Network Association between obstructive sleep apnea and cancer incidence in a large multicenter Spanish cohort. Am J Respir Crit Care Med. 2013; 187(1): 99–105. [DOI] [PubMed] [Google Scholar]
- 15. Peppard PE, et al. Here come the sleep apnea-cancer studies. Sleep. 2013; 36(10): 1409–1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nieto FJ, et al. Sleep-disordered breathing and cancer mortality: results from the Wisconsin Sleep Cohort Study. Am J Respir Crit Care Med. 2012; 186(2): 190–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ye L, et al. The different clinical faces of obstructive sleep apnoea: a cluster analysis. Eur Respir J. 2014; 44(6): 1600–1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Vavougios GD, et al. Phenotypes of comorbidity in OSAS patients: combining categorical principal component analysis with cluster analysis. J Sleep Res. 2016; 25(1): 31–38. [DOI] [PubMed] [Google Scholar]
- 19. Lacedonia D, et al. Characterization of obstructive sleep apnea-hypopnea syndrome (OSA) population by means of cluster analysis. J Sleep Res. 2016; 25(6): 724–730. [DOI] [PubMed] [Google Scholar]
- 20. Bailly S, et al. ; Scientific Council and Investigators of the French National Sleep Apnea Registry (OSFP) Obstructive sleep apnea: a cluster analysis at time of diagnosis. PLoS One. 2016; 11(6): e0157318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gagnadoux F, et al. ; Institut de Recherche en Santé Respiratoire des Pays de la Loire Sleep Cohort Group Relationship between OSA clinical phenotypes and CPAP treatment outcomes. Chest. 2016; 149(1): 288–290. [DOI] [PubMed] [Google Scholar]
- 22. Saaresranta T, et al. ; ESADA Study Group Clinical phenotypes and comorbidity in European sleep apnoea patients. PLoS One. 2016; 11(10): e0163439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Redline S, et al. Racial differences in sleep-disordered breathing in African-Americans and Caucasians. Am J Respir Crit Care Med. 1997; 155(1): 186–192. [DOI] [PubMed] [Google Scholar]
- 24. Ong KC, et al. Comparison of the severity of sleep-disordered breathing in Asian and Caucasian patients seen at a sleep disorders center. Respir Med. 1998; 92(6): 843–848. [DOI] [PubMed] [Google Scholar]
- 25. Li KK, et al. Obstructive sleep apnea syndrome: a comparison between Far-East Asian and white men. Laryngoscope. 2000; 110(10 Pt 1): 1689–1693. [DOI] [PubMed] [Google Scholar]
- 26. Lee RW, et al. Differences in craniofacial structures and obesity in Caucasian and Chinese patients with obstructive sleep apnea. Sleep. 2010; 33(8): 1075–1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. O’Connor GT, et al. ; Sleep Heart Health Study Investigators Variation in symptoms of sleep-disordered breathing with race and ethnicity: the Sleep Heart Health Study. Sleep. 2003; 26(1): 74–79. [PubMed] [Google Scholar]
- 28. Ryan CM, et al. The different clinical faces of obstructive sleep apnea (OSA), OSA in older adults as a distinctly different physiological phenotype, and the impact of OSA on cardiovascular events after coronary artery bypass surgery. Am J Respir Crit Care Med. 2015; 192(9): 1127–1129. [DOI] [PubMed] [Google Scholar]
- 29. Magalang UJ, et al. ; SAGIC Investigators Agreement in the scoring of respiratory events and sleep among international sleep centers. Sleep. 2013; 36(4): 591–596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Magalang UJ, et al. ; SAGIC Investigators Agreement in the scoring of respiratory events among international sleep centers for home sleep testing. J Clin Sleep Med. 2016; 12(1): 71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Iber C, American Academy of Sleep Medicine.. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology, and Technical Specifications. Westchester, IL: American Academy of Sleep Medicine; 2007. [Google Scholar]
- 32. Arnardottir ES, et al. Obstructive sleep apnoea in the general population: highly prevalent but minimal symptoms. Eur Respir J. 2016; 47(1): 194–202. [DOI] [PubMed] [Google Scholar]
- 33. Partinen M, et al. Basic Nordic Sleep Questionnaire (BNSQ): a quantitated measure of subjective sleep complaints. J Sleep Res. 1995; 4(S1): 150–155. [DOI] [PubMed] [Google Scholar]
- 34. Netzer NC, et al. Using the Berlin Questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med. 1999; 131(7): 485–491. [DOI] [PubMed] [Google Scholar]
- 35. Maislin G, et al. A survey screen for prediction of apnea. Sleep. 1995; 18(3): 158–166. [DOI] [PubMed] [Google Scholar]
- 36. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991; 14(6): 540–545. [DOI] [PubMed] [Google Scholar]
- 37. Ware J, Jr, et al. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996; 34(3): 220–233. [DOI] [PubMed] [Google Scholar]
- 38. Allen RP, et al. ; Restless Legs Syndrome Diagnosis and Epidemiology workshop at the National Institutes of Health; International Restless Legs Syndrome Study Group Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health. Sleep Med. 2003; 4(2): 101–119. [DOI] [PubMed] [Google Scholar]
- 39. Koller M, et al. ; EORTC Quality of Life Group Translation procedures for standardised quality of life questionnaires: The European Organisation for Research and Treatment of Cancer (EORTC) approach. Eur J Cancer. 2007; 43(12): 1810–1820. [DOI] [PubMed] [Google Scholar]
- 40. Bullinger M, et al. Translating health status questionnaires and evaluating their quality: the IQOLA Project approach. International Quality of Life Assessment. J Clin Epidemiol. 1998; 51(11): 913–923. [DOI] [PubMed] [Google Scholar]
- 41. Lanza ST, et al. PROC LCA: A SAS procedure for latent class analysis. Struct Equ Modeling. 2007; 14(4): 671–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lanza ST, et al. PROC LCA & PROC LTA users’ guide (Version 1.3.2). University Park: The Methodology Center, Penn State. Retrieved fromhttp://methodology.psu.edu. 2015. Accessed February 5, 2016 [Google Scholar]
- 43. Björnsdóttir E, et al. Symptoms of insomnia among patients with obstructive sleep apnea before and after two years of positive airway pressure treatment. Sleep. 2013; 36(12): 1901–1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Im EO, et al. Symptom clusters among multiethnic groups of cancer patients with pain. Palliat Support Care. 2013; 11(4): 295–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Bauer AM, et al. Prevalence of physical symptoms and their association with race/ethnicity and acculturation in the United States. Gen Hosp Psychiatry. 2012; 34(4): 323–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wenzel SE. Asthma phenotypes: the evolution from clinical to molecular approaches. Nat Med. 2012; 18(5): 716–725. [DOI] [PubMed] [Google Scholar]
- 47. Agusti A. The path to personalised medicine in COPD. Thorax. 2014; 69(9): 857–864. [DOI] [PubMed] [Google Scholar]
- 48. Agusti A, et al. Biomarkers, the control panel and personalized COPD medicine. Respirology. 2016; 21(1): 24–33. [DOI] [PubMed] [Google Scholar]
- 49. Pien GW, et al. Changing faces of OSA: treatment effects by cluster designation in the Icelandic sleep apnea cohort. Sleep. 2017; In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Eysteinsdottir B, et al. Insomnia complaints in lean patients with obstructive sleep apnea negatively affect positive airway pressure treatment adherence. J Sleep Res. 2017; 26(2): 159–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Escourrou P, et al. ; ESADA Study Group The diagnostic method has a strong influence on classification of obstructive sleep apnea. J Sleep Res. 2015; 24(6): 730–738. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.