Abstract
Adult influenza vaccination rates remain suboptimal, particularly among African Americans. Social norms may influence vaccination behavior, but little research has focused on influenza vaccine and almost no research has focused on racially-specific norms. This mixed methods investigation utilizes qualitative interviews and focus groups (n = 118) and national survey results (n = 1643) to assess both descriptive and subjective norms surrounding influenza vaccination. Qualitative results suggest a perceived descriptive norm that ‘about half’ of the population gets vaccinated. Participants describe differing norms by race and vaccine behavior. Quantitative results confirm a perceived descriptive norm that 40–60% of the population gets vaccinated. Both African Americans and Whites accurately identified race-specific vaccination rates relative to the general population. Individuals who report that a majority of people around them want them to be vaccinated were significantly more likely to be vaccinated, suggesting subjective norms are influential for both White and African American adults. While perceived descriptive norms are somewhat accurate (mirroring the actual influenza vaccination rate), emphasizing a suboptimal vaccination rate may not be beneficial. Health promotion efforts, particularly those targeting African Americans, may benefit from focusing on subjective norms and encouraging friends and family members to talk about the benefits of influenza vaccination.
Introduction
Although influenza vaccination is a low-cost preventive measure that can reduce illness, hospitalization and mortality, the majority of American adults do not get vaccinated. Healthy People 2020 sets a target objective of 70% uptake for annual immunization against seasonal immunization for adults [1]. During the 2015–16 flu season, only 41.7% of American adults were immunized for flu [2]. Racial disparities in vaccination rates exacerbate this problem with only 37% of African American adults compared to 45% of Whites [2]. Social norms—which include both perceived and observed rules, and the customs and practices of others—are powerful tools to encourage behavior change, but are understudied when it comes to vaccines in general, and flu vaccine, in particular.
Social psychologists posit that group identity is a major influence on attitudes and behaviors, and that belonging to a group drives individuals to conform to its expected standards [3]. The innate desire by an individual to fit into the group best explains the power of social norms while the reciprocal expectation of individuals within the group reinforces its social norms [3]. Comparisons are made to a referent group, comprised of people whose expectations are valuable to the individual, whether family, friends, neighbors, co-workers or ‘society’ in general, it can be further defined by race, ethnicity, gender, religion, political ideology, sexual orientation, culture or even shared interests. More simply, social norms are the acceptable beliefs by people belonging to a particular group, both explicit and implicit [3].
Scholars have categorized social norms in various ways, making replication imprecise, but two categories have appeared in many studies: descriptive norms (what others do) and subjective norms (what others think one should do) [3]. These two types of norms may be actual or perceived by an individual [4]. For example, if studies show a majority of college students average at least 8 h of sleep, that is an actual descriptive norm; if someone believes the majority of college students average only 4 h of sleep, that is a perceived descriptive norm, whether or not it is accurate.
Norms are used in multiple theoretical frameworks including the Theory of Reasoned Action and its extension, the Theory of Planned Behavior, which posit that intentions are the best predictors of a behavior and that subjective norms are one of three major predictors of behavior, along with attitude towards the behavior and perceived behavior control [5, 6]. The subjective norm is determined by the normative belief multiplied by the motivation to comply with what other people expect [7].
Social Norms Theory posits that widely held misperceptions between perceived and actual norms are strongly connected to risky behaviors [8]. Descriptive norms can explain a person’s perception of the willingness of members of a group to engage in risk behavior. Injunctive norms can explain a person’s perception of the approval of members of a group to engage in risk behavior [9]. The Theory of Social Normative Behavior addresses the failures of norms to highlight the underlying cognitive mechanisms in the relationship between descriptive norms and behavioral intentions [10]. The theory posits that three normative mechanisms–injunctive norms, outcome expectations and group identity–affect descriptive norms [10].
Social norms have been used to develop programs to promote behavior changes. Social norms marketing, a system of marketing designed to alter community perceptions about desirable attitudes and behaviors, has been applied to reduce gender violence and sexual violence [11, 12]. Much norms research has focused on understanding risk behaviors among college students, and social norms marketing has had some success in reducing these behaviors; however, evidence suggests that the long-term effectiveness of these campaigns is quite limited [13–20]. One area of concern is the ‘boomerang effect’ where individuals who may be exhibiting desired behavior, above and beyond the norm, may move back towards the norm after being exposed to a norm [21]. Social norms marketing approaches have been most successful when they have identified appropriate reference groups, ensured that data are credible to target populations and have followed best practices for basic marketing principles [21].
Social norms have also been utilized in promoting vaccination behavior. Several studies of HPV vaccination have found that social norms have a significant influence on vaccine uptake among female college students [22, 23] and on parents deciding to immunize their daughters [24, 25]. Another study found that social norms messaging increased Hepatitis B vaccine intentions among men who have sex with men [26]. Fewer studies have looked at the influence of norms on influenza vaccination, but evidence suggests that young parents are more likely to vaccinate their children against seasonal influenza if they view vaccination to be widespread [27] and a study of healthcare workers in Europe found that strong professional norms towards vaccination were a significant predictor of vaccination [28].
While almost all studies of social norms and vaccination account for race as a demographic variable, we could find no study that specifically asked respondents about descriptive or subjective norms using their own race as the referent group. However, same-race norms have been shown to be an important influence on such diverse health issues as drinking among college students [29], condom use among men who have sex with men [30] and obesity among women [31]. We, therefore, hypothesize that same-race norms may be more important than generalized norms when it comes to vaccination.
In this article, we highlight our findings on social norms, developed as part of a larger mixed methods investigation of racial disparities in influenza vaccination. First, we conducted formative research using semi-structured interviews and focus groups with White and African American adults (n = 118), from which we established several key research questions. Those findings informed a national survey, conducted in March 2015, of African American and White adults (n = 1643). Throughout the study, we examined whether social norms seemed to exist around vaccination, how influential they are and whether social norms could be harnessed to reduce vaccine racial disparities. We posed these research questions, all of which examined racial differences:
Q1: What are the perceived descriptive norms around flu vaccination?
Q2: What are the perceived subjective norms related to flu vaccination?
Q3: What influence do perceived social norms have on flu vaccine behavior?
Materials and methods
Below we describe the methods and findings for both research phases. All study procedures were reviewed and approved by the Institutional Review Board at the University of Maryland (367080).
Qualitative methods
From 2012–14, we gathered and analysed qualitative data following a Grounded Theory approach, interspersing three rounds of data collection with intensive data analysis [32]. Our participants were from rural, suburban and urban areas of Georgia and Maryland. They were recruited through a combination of convenience sampling, community engagement with partners and advertisements (see Quinn et al. 2016, for greater detail) [33]. The overall sample (n = 118) included native-born, English-speaking adults of diverse age, gender and income, who self-identified as White (n = 39) or African American (n = 79). Respondents were purposively selected for variation by vaccine behavior, age, gender, education and income (Table I). We conducted 12 semi-structured exploratory interviews, 9 focus groups (n = 90) divided variously by race and vaccine status and 16 in-depth individual interviews to explore topics that emerged in focus groups (Table II). Interviews averaged about 1 h in length and focus groups averaged about 90 min; trained, same-race moderators led the focus groups.
Table I.
Qualitative sample description by race
| Exploratory interviews | |||
| White (n = 5) | AA (n = 7) | Total (n = 12) | |
| Gender (%) | |||
| Female | 100% | 29% | 58% |
| Male | 0% | 71% | 42% |
| Age range (yrs) | 27–71 | 26–65 | 26–71 |
| Mean age (yrs) | 46.2 | 41.9 | 43.8 |
| Flu vaccine status (%) | |||
| Yes | 83% | 43% | 54% |
| No | 17% | 57% | 46% |
| Education level (%) | |||
| Less than high school | 0% | 14% | 8% |
| High school/GED | 17% | 29% | 23% |
| Some college/associate | 33% | 29% | 31% |
| Bachelor’s degree or higher | 50% | 29% | 38% |
| Focus groups | |||
| White (n = 26) | AA (n = 64) | Total (n = 90) | |
| Gender (%) | |||
| Female | 62% | 34% | 63% |
| Male | 38% | 64% | 36% |
| Other | 0% | 2% | 1% |
| Age (%) | |||
| 18–29 | 15% | 9% | 11% |
| 30–44 | 19% | 25% | 23% |
| 45–59 | 12% | 42% | 33% |
| 60+ | 54% | 23% | 32% |
| Flu vaccine status (%) | |||
| Annually | 44% | 37% | 39% |
| Most years | 15% | 18% | 17% |
| Once or twice | 25% | 22% | 20% |
| Never | 26% | 24% | 24% |
| Education level (%) | |||
| Less than high school | 0% | 3% | 2% |
| High school/GED | 0% | 28% | 19% |
| Some college/associate | 22% | 39% | 34% |
| Bachelor’s degree or higher | 78% | 30% | 44% |
| In-depth interviews | |||
| White (n = 8) | AA(n = 8) | Total (n = 16) | |
| Gender (%) | |||
| Female | 50% | 50% | 50% |
| Male | 50% | 50% | 50% |
| Age range (yrs) | 24–67 | 35–72 | 24–72 |
| Mean age (yrs) | 44.8 | 55 | 49.3 |
| Flu vaccine status (%) | |||
| Annually | 38% | 13% | 25% |
| Most years | 0% | 13% | 6% |
| Once or twice | 13% | 13% | 23% |
| Never | 50% | 63% | 56% |
| Education level (%) | |||
| Less than high school | 0% | 0% | 0% |
| High school/GED | 0% | 0% | 0% |
| Some college/associate | 13% | 13% | 13% |
| Bachelor’s degree or higher | 87% | 87% | 87% |
Table II.
Quantitative sample demographics and flu vaccination behavior and intentions by race
| White (n = 834) | AA (n = 809) | Total (n = 1643) | P from Chi-square test or t-test | |
|---|---|---|---|---|
| Sex (%) | ||||
| Male | 50.5 | 44.7 | 47.7 | 0.011 |
| Female | 49.5 | 55.3 | 62.3 | |
| Age (%) | ||||
| 18–29 | 14.9 | 17.9 | 16.4 | 0.007 |
| 30–44 | 18.6 | 19.3 | 18.9 | |
| 45–59 | 27.0 | 31.1 | 29.0 | |
| 60+ | 39.6 | 31.6 | 35.7 | |
| Mean age (yrs &SD) | 52.7 (17.8) | 49.7 (16.4) | 51.2 (17.2) | <0.001 |
| Education (%) | ||||
| Less than high school | 5.6 | 9.1 | 7.4 | <0.001 |
| High school/GED | 31.4 | 30.9 | 31.2 | |
| Some college/associate | 26.1 | 33.5 | 29.8 | |
| Bachelor’s degree or higher | 36.8 | 26.5 | 31.7 | |
| Income (%) | ||||
| Less than $20 000 | 11.9 | 28.1 | 19.8 | <0.001 |
| $20 000 to $39 999 | 17.0 | 23.6 | 20.3 | |
| $40 000 to $84 999 | 34.2 | 30.9 | 32.6 | |
| 85 000 or more | 36.9 | 17.4 | 27.3 | |
| Vaccine behavior (%) | ||||
| Got flu shot | 53.4 | 44.4 | 49.0 | <0.001 |
| Did not get flu shot | 46.6 | 55.6 | 51.0 |
Note. All numbers and percentages are unweighted. The significant levels are measuring the mean differences between Whites and African Americans.
Questions included attitudes about vaccines and disease, past experience with the healthcare system, trust in institutions such as government agencies and the pharmaceutical industry, cultural and racial identity and past history of discrimination. Our intention was to go beyond questions that are traditionally asked in survey research about vaccination by listening carefully to conversational threads introduced by participants. For social norms, we simply asked their impressions of how many people get vaccinated for flu, who they are and why.
We simultaneously engaged in data collection, analysis and theory development throughout the course of the project [32]. All interviews and focus groups were professionally transcribed and imported into Atlas.ti Qualitative Analysis Software. Using two team members who coded independently, we examined our data through empirically-based, inductive and deductive analysis, including coding, memo writing and theory building [32]. After identifying 121 codes, a second round of broad-brush coding identified larger themes, which were summarized in memos around major concepts, including illustrative quotes from the transcript. Some of the major themes included trust in the flu vaccine, trust in the process and agencies that produce the vaccine, balancing perceived disease risk against perceived risk of vaccine side effects, the influence of social norms, the use of ‘natural’ remedies, the role of history in shaping attitudes and also the role of conspiracy theories related to vaccines [33]. Our research continues to move towards incorporating these themes into an overarching theory of flu vaccine hesitancy and acceptance, but this manuscript will be focused exclusively on our findings related to social norms.
Qualitative results
Our initial probes explored whether clear descriptive social norms existed for flu vaccination. When asked about their perceptions of whether others in the community were getting flu vaccines, many participants reported little awareness of social norms, ‘It’s not something we really talk about, no’ (WFT) [Coding to identify quotes: (W) White, (AA) African American, (F) Female, (M) Male, (T) Vaccine Taker, (NT) Vaccine Non-Taker]. Some people related this to the flu vaccine’s success, because when it works, people do not get sick and its impact is unrecognized, ‘Generally, people don’t tell you when they don’t catch it’ (AAM). Some people noted a lack of advertisements and media coverage: ‘There haven’t been any signs saying ‘There’s an outbreak!’ or ‘Go get the flu vaccine.’ It’s not advertised at all’ (WFT).
Our first objective was to determine whether clear descriptive or subjective norms existed. When asked how many people get the flu vaccine, many respondents answered, ‘50–50’. For some, this reflected a belief that the population is polarized:
And then I would say it’s pretty 50/50, people have pretty strong feelings about it. Either they get it like clockwork every year or they're very against it (WFT).
I think it’s 50/50. I think that some people are all for it. They got to get it every year because they just swear by it. And then others are like, ‘Well, I've never gotten one. So I'm just going to chance it (WFNT).
For others, it’s simply a guess:
I would say it’s probably half and half (AAFNT).
I’m making this up, 50%. I don’t know … Because some people have real fears about getting it and other people don’t have fears, and 50% is half of them fears and half– I mean I know there is stuff out there that would keep people from getting it, and the stuff I don’t believe to be true and other people do believe it’s true (WMT).
I have no idea. I’m guessing half. I don’t know (WMNT).
I would put it at less than 50 is my guess, but I’ve never heard anything, so I’m really just guessing, but I’m just thinking that there have got to be a whole lot of people who–I mean I know there are a lot of people who don’t go to the doctor regularly until its emergency time. I mean we hear about that on the news all the time. So there is a good chance that they are not getting the flu vaccine (WMNT).
Individuals let their own vaccine behavior influence their attitudes about others. For instance, vaccine takers were more likely to see other vaccine takers as more health conscious and considerate:
They take care of themselves first, they take care because a lot of us have grandchildren and a lot of neighbors with children or other people who are older. And I don't know, it’s just a sense of you're doing a right thing by not contributing to more flu going around (WFT).
I think they’re [vaccine takers] just more prevention, I think they’re more conscious. As I see myself, as not wanting to either get it or spread it, so if there is a way that we can do that we’ll take that option (AAFT).
They viewed non-takers negatively, as indifferent, lazy and uncaring:
The two people I don’t think would get the vaccine are mostly because they are not really interested in seeking things out. I think if a doctor showed up at their door with a needle they would probably get a flu shot, but I don’t think that they would be very proactive, and they’re not proactive about anything really, like social life or health stuff (WFT).
In contrast, non-takers tended to view fellow non-takers as having made a rational decision to not vaccinate.
[Non-takers are] Probably people that need to spend that money on other things, people that just aren’t too, I guess people like me that I doubt I’m going to get the flu anyways, so I don’t want to mess with it, people that are more philosophically opposed to pharmaceuticals and that sort of thing, which I doubt is a lot of people, but occasionally I’m sure, people for whom it’s just not an issue for whatever reason (WMNT).
Non-takers viewed vaccine takers as different from themselves, identifying several characteristics that set them apart including greater risk for disease due to sickness or old age, having health insurance and/or easy access to healthcare or needing a flu vaccine as part of a work requirement:
I think older people are more likely to, provided they have access. I think they are strongly encouraged to (WMNT).
Like I said, when you go into CVS or Rite Aid it’s there, especially with the elderly, I think the elderly population probably do (AAFNT).
My guess is they are much more likely to have health insurance and regular visits to their physician for health, a physical, a checkup maybe once a year or close to once a year, that are attentive to that, and people that are older will be more focused on health (WMNT).
Maybe a couple of elderly people, and probably some of my age range or young adults would have gotten it, because a lot of them also work in the medical field or are police officers and stuff like that (AAFNT).
Others are less positive, as some non-takers view vaccine takers as being more easily influenced by ‘experts’:
Probably, I mean people that want to put more faith in experts as kind of a way of achieving truth and enlightenment, people that have gotten the flu really badly before, or people that have a history of other people in their family being really serious about that, people that do have other chronic illnesses that the flu would sort of enhance. Those would be my guesses. (WMNT).
However, both takers and non-takers recognized that mistrust was a significant influence for non-vaccine-takers, particularly among African Americans:
I think there are people who doubt that the vaccine works. I think that there are a number of people who have trust issues. I think some don’t do it because of cost, because everybody thinks it’s not going to be them, ‘I won’t get it. I haven’t gotten it yet.’ That’s what I would go with. (AAFNT).
I hadn’t thought about that, why some do and some don’t. I mean clearly it’s the trust factor again. I think it’s some that are stuck on– oh, you’re going to make me say it again– their awareness of the Tuskegee study (AAMNT).
I do think African Americans have a different attitude about getting healthcare and getting vaccines than others (AAMNT).
Participants were asked to describe the role of friends and family in shaping vaccination norms. Nearly everyone, white and black, takers and non-takers, described family as an important influence on their vaccine decisions. In fact, family was second only to personal physicians as the most trusted source of information related to vaccines.
Mod: Whose information would you trust the most?
A: Besides the doctor’s?
Mod: Yeah.
A: My mom’s.
Mod: Can you tell me why?
A: She’s very wise. She knows a lot of things that I don’t know. And it’s your mom, you know. (WFT).
Mod: So it doesn’t matter where the message, whether it comes from the government or it comes from the news media, it’s no different to you?
S: The most important person is parents, family, and friends. That’s it.
Mod: The people that you know.
S: That’s right. If they’re doing it then I’m more likely to do it (WMNT).
However, a subset of older participants made their decision independent from their family.
And what my friends and family do, that doesn’t influence me. It’s what I’m going to do and I’m kind of at an age now where it’s like I don’t care what you do, this is what I’m doing, this is what is best for me, so I really don’t let that influence me that much (WFNT).
And in terms of what family and friends do, for the most part I tend not to be swayed by, particularly if I have–I will say if I have a strong feeling about something or just not in a category of undecided about something then what friends and family say won’t weigh too heavily (AAFNT).
Most participants described a kind of ‘family culture’ surrounding vaccination that was shaped by their childhood experiences and continued to influence their decisions as adults. There were clear differences between vaccine takers and vaccine non-takers and differences by race. Family practices could encourage vaccination:
So, maybe that's why I'm so used to it. And growing up with my dad being a physician, it was always prioritized that we should get the vaccinations because he always said it was good and we shouldn’t–he has his MPH, too, so it’s like very much–so does my sister–it’s very much like promoted in our family (WFT).
Again I did grow up with understanding the importance of vaccines. So, that influenced, and my folks being, my dad is a doctor, my mom is a nurse, it wasn’t so much discussion of vaccines, but I understood (AAMT).
They could also discourage vaccination:
I grew up with my mother, grandmother, father, great-grandmother, everybody around me, ‘No, I'm not taking that. It ain't gonna give me the flu.’ I mean, that's always what I've heard, so when I became an adult, ‘Well no, not going to give me the flu either.’ So huh-uh, don’t do it (AAFNT)
Mod: So you feel like this was something that was part of the family’s behavior?
F: Oh yeah, we’ve never voluntarily gotten a shot, none of us, none of the family at all for as long as I can remember (AAFNT).
Any kind of flu, we just never got it vaccinated, which is interesting because it’s probably one of those things that passes down. You’re going to ask, like who do you ask? Well, the first person you’re going to ask is probably not your doctor; you’re going to ask your parents, you’re going to ask your grandparents (WMNT).
African Americans were more likely to describe an active debate over vaccination. Both vaccine takers and non-takers could point to friends or family members that held an opposing view on vaccination. The idea of a ‘family divided’ was quite common in both focus groups and interviews.
Mod: And what is your family talking about? What are they saying about getting the vaccine?
M: Very divided, my family.
Mod: Very divided. Tell me about that division.
M: Pretty much half is for and the other half is against. And the younger side is more for. The older side is more against (AAMNT).
In African American families in particular, there was a significant push back against ‘selling out’ or becoming a ‘guinea pig.’ There were also significant debates over the severity and likelihood of side effects:
I can only go by what I’ve seen people that actually have gotten the shot and what happens to them. Other than that I don’t actually know, because I haven’t taken it, but just to see most of them when they get it they get sick, it deters me from taking it. So I haven’t even tried even going about it (AAFNT).
A few [friends] that would begin to question me, ‘Have you researched this? We don’t know what’s coming down the pipe with it (AAFNT).
White participants were less likely to describe discussion among their families, instead describing families quietly supportive of vaccination, or families that were ambivalent but didn’t engage in a debate.
I think I may actually have talked to my mom briefly about it before, like ‘Oh I got the flu shot this week’ and she will say, ‘Oh yeah, I got mine last month.’ And that is the end of the conversation. So I think that she gets it, but we don’t really go into depth (WFT).
The exception was among a small group of non-takers with no family history with flu vaccination.
I mean no one in my family gets vaccinated for the flu. I asked my mom about it. She says she doesn’t see a real benefit in getting vaccinated for the flu. I don’t know if anyone in my family has ever had the flu. I mean I’m sure they’ve had the flu, but I can’t think of actually anyone in my family who has ever been vaccinated, but this year I did go to the doctor’s office to at least talk about it for the first time, just because I had heard it’s probably a good idea (WMNT).
Among our participants, family culture proved to be a strong and lasting influence on social norms surrounding vaccination but racial differences were evident in their discussion.
Quantitative methods
In 2015, we contracted with GfK to conduct a nationally representative online survey with a target sample of 800 U.S. Black and 800 White adults over age 18 selected from GfK’s Knowledge Panel, a probability-based web panel that utilizes an Addressed Based Sampling methodology to capture a representative sample of the U.S. For Whites, 839 completed the survey for a rate of 63.1%. For African Americans, 819 completed the survey for a completion rate of 51.2%. Of the 1657 respondents who completed the survey, 1643 were determined to be valid and included in the final analysis (See Table II for sample description). GfK provided sample weights for both Black and White samples utilizing benchmarks from the 2014 Current Population Survey, such as gender by age, census region, metropolitan status, education level, household income and internet access. The survey consisted of both standard vaccine-related items as well as novel items developed in response to our qualitative findings (see Quinn et al., 2017 for full measures) [34]. The survey was also pre-tested, utilizing 16 cognitive interviews with volunteers who explained their thought-processes as they went through each item so we could ensure the reliability and validity of our novel measures [35].
The constructs of perceived descriptive norms and perceived subjective norms were both measured with single questions. The perceived descriptive norms variable was assessed with two different referent groups. The first used the entire U.S. population as a referent group asking, ‘Thinking about people in the U.S., how many of them do you think get a flu vaccine each year?’ and the second used the respondent’s own racial group as a referent group asking, ‘Thinking about people of your own race, how many of them do you think get a flu vaccine each year?’ The subjective norms question asked, ‘Of the people close to you, what proportion want you to get a flu vaccine?’ All three items were answered on a 5-point scale ranging from ‘few (0–20%)’ to ‘most or nearly all (81–100%).’ The vaccine behavior question asked, ‘Did you get a flu vaccine this season?,’ which was coded either no or yes (0 and 1), respectively. The relations among social norms variables, vaccination and race were assessed using contingency tables and chi-square tests of independence to determine whether the variables appeared to be statistically associated. All analyses were weighted by the post-stratification weights such that the results were nationally representative.
Quantitative results
Research questions 1 and 2 focused on describing perceived descriptive and subjective norms, including racial differences (Table III). Overall, the largest proportion of respondents (43%) answered that between 40% and 60% of Americans get a flu vaccination, and the second largest group (35%) believed that between 20% and 40% of people get flu vaccinations. On the extreme ends, about 6% believed that fewer than 20% of Americans get a flu vaccine, and about 2% believed that most people get vaccinated.
Table III.
Social norms for White and African American (AA) adults
| Descriptive norms(Total population) | Descriptive norms (Own race) | Subjective norms | |||||||
|---|---|---|---|---|---|---|---|---|---|
| White | AA | Total | White | AA | Total | White | AA | Total | |
| Few 0–20% | 5.5% | 5.0% | 5.5% | 5.8% | 15.2% | 7.2% | 35.6% | 39.7% | 36.2% |
| Less than half 21–40% | 36.7% | 23.1% | 34.7% | 25.9% | 36.7% | 27.5% | 13.0% | 15.1% | 13.1% |
| Around half 41–60% | 41.7% | 45.4% | 42.3% | 45.5% | 29.5% | 43.1% | 13.8% | 22.0% | 15.0% |
| More than half 61–80% | 14.9% | 21.8% | 15.9% | 20.3% | 14.8% | 19.5% | 12.1% | 7.8% | 11.4% |
| Most or nearly all 81–100% | 1.1% | 4.6% | 1.7% | 2.5% | 3.8% | 2.7% | 25.6% | 15.5% | 24.1% |
| Total N | 1392 | 238 | 1639 | 1377 | 237 | 1614 | 1385 | 232 | 1617 |
| Chi-Square | P < 0.001 | P < 0.001 | P < 0.001 | ||||||
For the subjective norm, ‘how many of the people close to them would want them to get a flu vaccination’, most respondents fell into the extreme ends: about 36% felt that fewer than 20% of the people close to them would want them to get a flu vaccination, whereas about 26% felt that more than 80% of people close to them would care. In the middle, about 13% felt that slightly less than half of their close loved ones would care, 16% guessed that between 40 and 60% would and about 12% said somewhat more than half would want them to get the flu vaccine.
There were significant racial differences for both descriptive norms and the subjective norm. For the general population norm, African Americans perceived more people getting vaccinated overall than Whites did (P < 0.001); however, both groups over-estimated vaccination rates for the general population. For the race specific descriptive norm, 51.9% of African Americans correctly perceived that fewer African Americans were vaccinated, and Whites correctly perceived that more Whites were vaccinated (P < 0.001). Whites perceived a stronger subjective norm for vaccination than did African Americans (P < 0.001).
In Table IV, we see that regardless of race, adults who got flu vaccine this season perceived higher levels of vaccination evidenced in their descriptive norms than those who did not get the flu vaccine. For those who perceived half of the U.S. population got vaccinated, Whites were more likely to get vaccinated than African Americans. For African Americans, the chi-square test shows that there was no statistically significant association between perceived descriptive norms and vaccine behavior. Perceived descriptive norms using racially-specific referent groups were similar to the results for the perceived descriptive norm for the general population. Whites who got the flu vaccine were associated with perceiving higher racially-specific descriptive norms. For African Americans, the racially-specific descriptive norm and vaccine behavior were not statistically associated.
Table IV.
Social norms and vaccine uptake for White and African American (AA) adults
| White | African American | ||||
|---|---|---|---|---|---|
| Did not get flu vaccine this season | Got flu vaccine this season | Did not get flu vaccine this season | Got flu vaccine this season | ||
| Descriptive norms (U.S. population) | Few (0–20%) | 7.0% | 4.1% | 6.3% | 2.1% |
| Less than half (21–40%) | 41.7% | 31.8% | 23.9% | 21.1% | |
| Around half (41–60%) | 38.6% | 44.5% | 46.5% | 43.2% | |
| More than half but not all (61–80%) | 11.5% | 18.3% | 18.3% | 28.4% | |
| Most or nearly all (81–100%) | 1.2% | 1.3% | 4.9% | 5.3% | |
| Chi-square test | P < 0.001 | P = 0.271 | |||
| Descriptive norms (own race) | Few (0–20%) | 7.4% | 4.3% | 17.0% | 12.6% |
| Less than half (21–40%) | 32.9% | 19.4% | 36.2% | 36.8% | |
| Around half (41–60%) | 45.8% | 44.6% | 29.1% | 30.5% | |
| More than half but not all (61–80%) | 12.0% | 28.6% | 14.2% | 15.8% | |
| Most or nearly all (81–100%) | 1.9% | 3.2% | 3.5% | 4.2% | |
| Chi-square test | P < 0.001 | P = 0.920 | |||
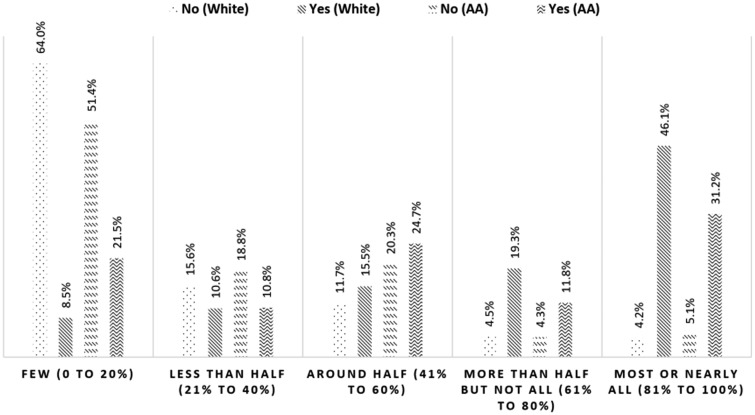
| Subjective norms | Few (0–20%) | 64.0% | 8.5% | 51.4% | 21.5% |
| Less than half (21–40%) | 15.6% | 10.6% | 18.8% | 10.8% | |
| Around half (41–60%) | 11.7% | 15.5% | 20.3% | 24.7% | |
| More than half but not all (61–80%) | 4.5% | 19.3% | 4.3% | 11.8% | |
| Most or nearly all (81–100%) | 4.2% | 46.1% | 5.1% | 31.2% | |
| Chi-square test | P < 0.001 | P < 0.001 | |||
The racial differences between the subjective norms and flu vaccine behavior are shown in Fig. 1. About 49% of our respondents had already received a flu vaccination, and about 51% had not. For both African Americans and Whites, getting a flu vaccine was positively associated with the perception that more family and friends wanted them to be vaccinated. This was statistically significant for both groups.
Fig. 1.
Relation between the subjective norms and vaccine behavior.
Discussion
Our first research question examined the existence of perceived descriptive norms for both racial groups. Our qualitative research on perceived norms around flu vaccination indicate respondents believe about half of the population receives a flu vaccine while the other half does not. Our quantitative findings also support this perception, with the largest proportion of survey respondents indicating that between 40% and 60% of the general population gets vaccinated. While these estimates reflect the actual descriptive norm of about 42%, our research suggests that rather than an informed estimate, it appears this ‘50–50’ response represents little more than a guess for most people. Flu vaccination may be the topic of private conversation with friends, family and co-workers, but is infrequently discussed in wider society, and therefore people do not have any basis for knowledge about the general vaccination rate. Further, most promotion of flu vaccination simply encourages flu vaccination without describing the actual rates of uptake. Often, in interviews, when people reasoned aloud about norms, they based their ideas about frequency of flu vaccine on other factors, such as people’s tendency to avoid medical care. Participants were also not especially confident about their guesses. Because this descriptive norm is not definitive in terms of vaccination behavior, it is not likely to exert social pressure or influence on people in either direction–vaccination or non-vaccination. From the perspective of Social Norms Theory, the misconception between actual norms and perceived norms would typically be seen as an opportunity to correct the misconception and change behavior. Current influenza vaccination rates are not ideal, and yet respondents are actually overestimating vaccine uptake. However, from a public health viewpoint, there is a risk that emphasizing this perceived norm based on mediocre vaccination rates, may normalize non-vaccination and could trigger the ‘boomerang effect’ where some vaccinators may realize they are already exceeding the norm.
We also explored the role of different referent groups in shaping descriptive norms. While our initial item asked about the general population without specifying further, both groups appear to have answered the question in ways that suggest they were mirroring their own group’s actual vaccination rates. In survey results, we see this in the ways both White and African American respondents could accurately differentiate their own racial group’s vaccination rates when compared to the national average. In our qualitative research, many African American respondents introduced racially-specific factors that influenced their vaccination decisions, particularly the history of African Americans’ distrust of medical care.
We were also interested in understanding the role of subjective norms for both groups. While the subjective norm appeared to be more influential in shaping vaccine behavior among African Americans in the qualitative research, survey results found subjective norms to be a significant influence on both White and African American vaccine behavior. Over 60% of Whites and 50% of African Americans who did not get vaccinated reported that few people close to them wanted them to get the vaccine. Conversely, over 40% of Whites and over 30% of African Americans who took the vaccine reported that most or nearly all wanted them to get the vaccine (Fig. 1). This speaks to the dramatic impact of subjective norms on vaccine behavior.
Similarly, in our qualitative work, many spoke of an importance of a family culture around vaccination. From the perspective of the Theory of Planned Behavior, health communicators may wish to focus on increasing perceived subjective norms within the African American group as a way to increase intention and actual vaccine uptake, thereby decreasing the disparity between the two groups. Several approaches may be effective in doing so: focusing on changing the family culture around vaccination by emphasizing family needs and expectations, particularly in families where members experience chronic diseases that put them at higher risk of complications from influenza, and secondly, seizing opportunities to reach African American families through family reunions, other holiday gatherings and trusted venues, such as barber/beauty shops or faith communities, with messages that encourage conversations with loved ones about the importance of flu vaccinations.
While the Theory of Social Normative Behavior suggests that group identity affects descriptive norms, and we see some consistency between racial group and norms, a central tenet of our research approach has been to recognize that African Americans are not a monolithic group. Therefore, we encourage future research to explore differences within the African American group to determine characteristics in addition to race that may contribute to the influence of descriptive and subjective norms. The influence of subjective norms in any group–including African Americans–may vary with age, education, geography, health status or other characteristics.
Conclusions
Perceived descriptive norms about flu vaccination are weak, but realistic, reflecting the reality that just under half of all adults receive a flu vaccination, with even lower uptake among African Americans. More importantly, we identified a greater association between subjective norms and vaccination behavior, extending across both races. This finding suggests that increasing communication among loved ones about flu vaccine may be an effective tactic to increase flu vaccination.
Acknowledgement
The authors would like to thank Drs. James Butler, Craig Fryer and Susan Passmore for facilitating our focus groups.
Funding
This work was supported by the National Institute of Minority Health and Health Disparities at the National Institutes of Health as a Research Center of Excellence in Race, Ethnicity and Health Disparities Research NIH-NIMHD: P20MD006737 (Quinn and Thomas, PI).
Conflict of interest statement
None declared.
References
- 1. United States Department of Health and Human Services. Healthy People 2020: Immunization and Infectious Disease, 2015. Available at: https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives. Accessed: 8 November 2017.
- 2. Centers for Disease Control and Prevention. Flu Vaccination Coverage, United States, 2015-2016 Influenza Season, 2016. Available at: https://www.cdc.gov/flu/fluvaxview/coverage-1516estimates.htm. Accessed: 8 November 2017.
- 3. Mackie G, Moneti F, Denny E. et al. What are social norms? How are they measured University of California at San Diego-UNICEF Working Paper, San Diego, 2012. Available at: https://www.unicef.org/protection/files/4_09_30_Whole_What_are_Social_Norms.pdf. Accessed: 15 January 2017.
- 4. Elek E, Miller-Day M, Hecht ML.. Influences of personal, injunctive, and descriptive norms on early adolescent substance use. J Drug Issues 2006; 36: 147–72.http://dx.doi.org/10.1177/002204260603600107 [Google Scholar]
- 5. Montano DE, Kasprzyk D, Glanz K. et al. Theory of reasoned action, theory of planned behavior, and the integrated behavioral model. In: Health Behavior: Theory, Research and Practice, 4th edn San Francisco: Jossey-Bass, 2008. [Google Scholar]
- 6. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process 1991; 50: 179–211.http://dx.doi.org/10.1016/0749-5978(91)90020-T [Google Scholar]
- 7. Rivis A, Sheeran P.. Descriptive norms as an additional predictor in the theory of planned behaviour: a meta-analysis. Curr Psychol 2003; 22: 218–33.http://dx.doi.org/10.1007/s12144-003-1018-2 [Google Scholar]
- 8. Scholly K, Katz AR, Gascoigne J. et al. Using social norms theory to explain perceptions and sexual health behaviors of undergraduate college students: an exploratory study. J Am Coll Health 2005; 53: 159–66.http://dx.doi.org/10.3200/JACH.53.4.159-166 [DOI] [PubMed] [Google Scholar]
- 9. Borsari B, Carey KB.. Descriptive and injunctive norms in college drinking: a meta-analytic integration. J Stud Alcohol Drugs 2003; 64: 331.http://dx.doi.org/10.15288/jsa.2003.64.331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rimal RN, Real K.. How behaviors are influenced by perceived norms a test of the theory of normative social behavior. Commun Res 2005; 32: 389–414.http://dx.doi.org/10.1177/0093650205275385 [Google Scholar]
- 11. Paluck EL, Ball L. Social Norms Marketing to Reduce Gender Based Violence IRC Policy Briefcase, 2010. Available at: http://static.squarespace.com/static/5186d08fe4b065e39b45b91e/t/52d1f24ce4b07fea759e4446/1389490764065/Paluck%20Ball%20IRC%20Social%20Norms%20Marketing%20Long.pdf. Accessed: 8 November 2017.
- 12. Fabiano PM, Perkins HW, Berkowitz A. et al. Engaging men as social justice allies in ending violence against women: evidence for a social norms approach. J Am Coll Health 2003; 52: 105–12.http://dx.doi.org/10.1080/07448480309595732 [DOI] [PubMed] [Google Scholar]
- 13. Lewis MA, Neighbors C.. Social norms approaches using descriptive drinking norms education: a review of the research on personalized normative feedback. J Am Coll Health 2006; 54: 213–8.http://dx.doi.org/10.3200/JACH.54.4.213-218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Perkins HW. Social norms and the prevention of alcohol misuse in collegiate contexts. J Stud Alcohol Drugs Suppl 2002; 14: 164–72. [DOI] [PubMed] [Google Scholar]
- 15. Werch CE, Pappas DM, Carlson JM. et al. Results of a social norm intervention to prevent binge drinking among first-year residential college students. J Am Coll Health 2000; 49: 85–92.http://dx.doi.org/10.1080/07448480009596288 [DOI] [PubMed] [Google Scholar]
- 16. Turner J, Perkins HW, Bauerle J.. Declining negative consequences related to alcohol misuse among students exposed to a social norms marketing intervention on a college campus. J Am Coll Health 2008; 57: 85–94.http://dx.doi.org/10.3200/JACH.57.1.85-94 [DOI] [PubMed] [Google Scholar]
- 17. Foxcroft DR, Moreira MT, Almeida Santimano NM. et al. Social norms information for alcohol misuse in university and college students. Cochrane Library 2015; 12: CD006748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hansen WB, Graham JW.. Preventing alcohol, marijuana, and cigarette use among adolescents: peer pressure resistance training versus establishing conservative norms. Prev Med 1991; 20: 414–30.http://dx.doi.org/10.1016/0091-7435(91)90039-7 [DOI] [PubMed] [Google Scholar]
- 19. Carter CA, Kahnweiler WM.. The efficacy of the social norms approach to substance abuse prevention applied to fraternity men. J Am Coll Health 2000; 49: 66–71.http://dx.doi.org/10.1080/07448480009596286 [DOI] [PubMed] [Google Scholar]
- 20. Procter-Scherdtel A, Collins D.. Social norms and smoking bans on campus: interactions in the Canadian university context. Health Educ Res 2013; 28: 101–12.http://dx.doi.org/10.1093/her/cys075 [DOI] [PubMed] [Google Scholar]
- 21. Burchell K, Rettie R, Patel K.. Marketing social norms: social marketing and the ‘social norm approach’. J Consum Behav 2013; 12: 1–9. [Google Scholar]
- 22. Allen JD, Mohllajee AP, Shelton RC. et al. Stage of adoption of the human papillomavirus vaccine among college women. Prev Med 2009; 48: 420–5.http://dx.doi.org/10.1016/j.ypmed.2008.12.005 [DOI] [PubMed] [Google Scholar]
- 23. Hopfer S, Clippard JR.. College women's HPV vaccine decision narratives. Qual Health Res 2010; 21: 262–77. [DOI] [PubMed] [Google Scholar]
- 24. Marlow LAV, Waller J, Wardle J.. Parental attitudes to pre-pubertal HPV vaccination. Vaccine 2007; 25: 1945–52.http://dx.doi.org/10.1016/j.vaccine.2007.01.059 [DOI] [PubMed] [Google Scholar]
- 25. Ogilvie GS, Remple VP, Marra F. et al. Parental intention to have daughters receive the human papillomavirus vaccine. Can Med Assoc J 2007; 177: 1506–12.http://dx.doi.org/10.1503/cmaj.071022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Vet R, de Wit JBF, Das E.. The efficacy of social role models to increase motivation to obtain vaccination against hepatitis B among men who have sex with men. Health Educ Res 2011; 26: 192–200.http://dx.doi.org/10.1093/her/cyq074 [DOI] [PubMed] [Google Scholar]
- 27. Daley MF, Crane LA, Chandramouli V. et al. Misperceptions about influenza vaccination among parents of healthy young children. Clin Pediatr (Phila) 2007; 46: 408–17.http://dx.doi.org/10.1177/0009922806298647 [DOI] [PubMed] [Google Scholar]
- 28. Godin G, V�zina-Im L-A, Naccache H.. Determinants of influenza vaccination among healthcare workers. Infect Control Hosp Epidemiol 2010; 31: 689–93. [DOI] [PubMed] [Google Scholar]
- 29. LaBrie JW, Hummer JF, Neighbors C. et al. Whose opinion matters? The relationship between injunctive norms and alcohol consequences in college students. Addict Behav 2010; 35: 343–9.http://dx.doi.org/10.1016/j.addbeh.2009.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Peterson JL, Rothenberg R, Kraft JM. et al. Perceived condom norms and HIV risks among social and sexual networks of young African American men who have sex with men. Health Educ Res 2009; 24: 119–27. [DOI] [PubMed] [Google Scholar]
- 31. Averett S, Korenman S.. Black-white differences in social and economic consequences of obesity. Int J Obes (Lond) 1999; 23: 166.http://dx.doi.org/10.1038/sj.ijo.0800805 [DOI] [PubMed] [Google Scholar]
- 32. Charmaz K. Constructing Grounded Theory, vol. 1. London: Sage, 2014. [Google Scholar]
- 33. Quinn S, Jamison A, Musa D. et al. Exploring the continuum of vaccine hesitancy between African American and white adults: results of a qualitative study. PLOS Currents Outbreaks 2016; 10.1371/currents.outbreaks.3e4a5ea39d8620494e2a2c874a3c4201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Quinn SC, Jamison A, Freimuth VS. et al. Exploring racial influences on flu vaccine attitudes and behavior: results of a national survey of White and African American adults. Vaccine 2017; 35: 1167–74.http://dx.doi.org/10.1016/j.vaccine.2016.12.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Collins D. Pretesting survey instruments: an overview of cognitive methods. Qual Life Res 2003; 12: 229–38http://dx.doi.org/10.1023/A:1023254226592 [DOI] [PubMed] [Google Scholar]