Abstract
Objective
This study examines the relationships between hospitals’ annual ARDS case volume with hospitals’ ARDS case fatality rates and individuals’ odds of ARDS hospital mortality.
Design
Retrospective cohort study.
Setting
The US Healthcare Cost and Utilization Project’s Nationwide Inpatient Sample, 2002-2011.
Patients
ARDS discharges defined by the presence of an ARDS ICD-9-CM diagnosis code (518.82 or 518.5) and a mechanical ventilation procedure code (96.70, 96.71 or 96.72) on the discharge diagnosis and procedure lists. If the procedure code 96.71 was on the discharge record (mechanical ventilation < 96 hours duration), the patient also needed to be classified as deceased.
Interventions
None
Measurements and Main Results
We analyzed 2,686 hospitals and 117,204 cases of ARDS. Average annual hospital ARDS in-hospital mortality was 47%. ARDS case volume was categorized as low (1-9), medium (10-49), and high (50-423 cases per year). In a hospital-level Poisson regression adjusting for hospital characteristics, when compared to low volume ARDS hospitals; high and medium volume ARDS hospitals had lower annual ARDS case fatality (RR 0.75 99%CI 0.71-0.79 and RR 0.86 99%CI 0.82-0.90, respectively; p≤0.001 for both). In an individual-level, multivariable model adjusting for hospital and individual characteristics; high and medium ARDS volume hospitals were associated with lower odds of ARDS mortality compared to low volume hospitals ((OR 0.85 (99% CI 0.74-0.99), p=0.006; OR 0.89 (99% CI 0.79-1.00), p= 0.01, respectively).
Conclusions
In this cohort, at both an individual- and hospital-level, higher ARDS hospital case volume is associated with lower ARDS hospital mortality.
Keywords: Respiratory distress syndrome, adult, mortality, high volume hospitals, low volume hospitals, epidemiology
Introduction
Acute respiratory distress syndrome (ARDS) is a severe inflammatory response in the lungs that follows an inciting injury, leading to hypoxic respiratory failure and often multiorgan failure and death. The actual incidence of ARDS in the United States is not completely understood, but two recent population-based studies have estimated the incidence between 40 and 80 cases per 100,000 person-years [1, 2]. The past few decades of translational research have demonstrated improved ARDS survival with specific lung protective mechanical ventilation strategies including low tidal volume ventilation, prone positioning, and use of neuromuscular blockade [1–7]. Given the highly coordinated and complex nature of these ARDS treatment strategies, one may postulate that institutional mastery requires knowledge, time, and ample frequency of patient experiences.
While the volume-outcome relationship has not specifically been studied for ARDS, a recent meta-analysis has demonstrated associations between high annual volumes and improved outcomes amongst all critical care diagnoses [8]. However, among the thirteen studies in this analysis that reported outcomes for respiratory diagnoses in critical care admissions, there was heterogeneity in the types of respiratory diagnoses examined, the categorization of annual hospital volumes, and the direction of volume-outcome relationships [9–21].
We performed a retrospective review of the Healthcare Cost and Utilization Project’s (HCUP) Nationwide Inpatient Sample (NIS) administrative datasets from 2002-2011 and attempted to use a more specific case definition to approximate moderate-severe ARDS cases. The aim of this study is to examine the relationships between annual hospital ARDS case volumes and ARDS mortality. With this underlying conceptual framework, we hypothesized that hospitals with a higher annual volume of ARDS patients would demonstrate improved mortality outcomes.
Methods
Data Source and Population
The NIS dataset contains detailed hospital discharge information and, for the years utilized, represents a stratified probability sample of American Hospital Association hospitals with sampling probabilities targeted to select 20% of the U.S. community hospitals [22]. With a study objective to explore an association in a large US cohort rather than estimate national incidence; and an analytic plan to account for repeated measures in hospitals; the NIS stratified sampling design factors were not utilized in these analyses. The primary analysis includes all hospital discharge records between January 1, 2002 and December 31, 2011. We utilized a prior published ARDS case definition of records with ICD-9-CM code 518.82 or 518.5 among any of the discharge diagnoses plus an accompanying ICD-9-CM procedure code for mechanical ventilation: 96.70, 96.71, or 96.72 (Table 1)[23]. Additionally, if the procedure code 96.71 was on the discharge record (mechanical ventilation < 96 hours duration), the patient also needed to be classified as deceased at discharge. This final stipulation was to create a study sample that most closely approximated moderate-severe ARDS, in which we hypothesize that experience and advanced therapies may have the most differential effect. This rationale is anchored on 2 landmark clinical studies that demonstrated that the 25th percentile of days of mechanical ventilation of survivors of moderate-severe ARDS ranges from 4-9 days [24, 25]. From this cohort we excluded patients < 18 years of age, patients with a missing mortality status, and patients whose reason for admission was “birth.”
Table 1.
ICD-9-CM Diagnosis and Procedure Codes used for Acute Respiratory Distress Case Definition1
| Diagnosis Codes |
|---|
| 518.5 |
Pulmonary insufficiency following trauma and surgery
|
| 518.82 |
Other pulmonary insufficiency, NEC
|
|
|
| Procedure Codes: |
| 96.70 |
| Continuous mechanical ventilation of unspecified duration |
| 96.71 |
| Continuous mechanical ventilation for < 96 h consecutively2 |
| 96.72 |
| Continuous mechanical ventilation for ≥ 96 h consecutively |
ARDS = Acute Respiratory Distress Syndrome; ICD-9-CM = International Classification of Diseases, Ninth Revision, Clinical Modification; NOS = not otherwise specified; NEC = not elsewhere classified
The ICD-9-CM is based upon the World Health Organization’s ninth revision of the International Classification of Diseases. (8)
Variables
The primary hospital-level outcome is a hospital’s annual ARDS case fatality rate (CFR) and the primary individual-level outcome is in-hospital mortality. The primary exposure of interest for both the individual- and hospital-level analyses is a hospital’s annual ARDS case volume. Hospitals that recorded 1-9, 10-49 and 50-423 ARDS cases per year were categorized as “low,” “medium,” and “high” ARDS volume hospitals, respectively.
Statistical Analysis
Initial data management was performed using the SAS 9.4 (SAS Institute, Cary, NC). All graphical and statistical analyses were performed using RStudio 0.99.90. (RStudio Inc., Boston, MA). The exploratory hospital-level analyses utilized a combination of qualitative graphical as well as descriptive statistics to categorize the annual ARDS volumes. Given that hospitals provided repeated years of data, we used random effects Poisson regression models that included hospital of discharge as a random effect for all bivariate associations. For multivariable models we included, as fixed effects, variables that were associated with hospital ARDS CFR at a p-value <0.05 in bivariate Poisson regressions.
Individual-level analyses began with bivariate analyses by primary outcome and primary exposure. For bivariate analyses by individual mortality status, t-tests, chi-squared tests, and logistic regression were used. For bivariate analyses by hospital ARDS volume designation, analysis of variance, chi-square tests, and ordinal logistic regression were deployed. Two individual-level, fixed effects, multivariable models were explored: one a priori model with variables selected based on our prior hypotheses and a selected model with variables drawn from bivariate analyses results. For the selected individual-level model, covariates were selected from bivariate regression analyses as those with odds ratios (OR) ≥ 1.2 or ≤ 0.8 among any of the variable’s response categories for both outcome and exposure. All of these selected variables were then retained in this individual-level model. By our design, both individual-level models included hospital of discharge as a fixed effect.
This study was declared exempt from review by the Emory University institutional review board given that the dataset is publically available, does not contain identifying information, and the data use agreement prohibits attempts of re-identification of persons.
Results
Exploratory Hospital-Level Analysis
The 2002-2011 NIS cohort included 2,686 unique hospitals. The histogram of annual hospital ARDS case volumes demonstrated a rightward skew, with a mean and median of 19 and 8 cases per hospital per year, respectively (interquartile range (IQR) 3-20) (eFigure 1-2). The distribution of annual hospital ARDS CFRs demonstrated disproportionally high frequencies at 0% and 100%, yet otherwise appeared normally distributed around a mean of 47% (standard deviation (SD) 25%) (eFigure 3-4). Amongst low, medium, and high ARDS volume hospitals the mean annual ARDS CFR was 51% (SD 31%), 44% (SD 14%), and 39% (SD 9%), respectively (Figure 1).
Figure 1. Average Annual Hospital ARDS Case Fatality Rate by Average Annual Case Volume, NIS 2002-2011 (N= 2,686 hospitals)a.
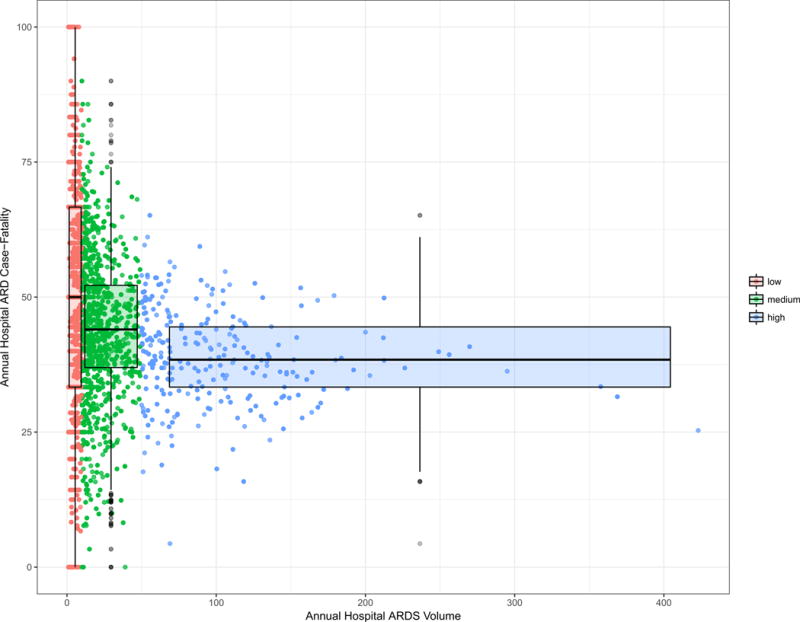
aData plotted are unadjusted average annual hospital case fatality rates by average annual ARDS case volumes among ARDS discharges. Points correspond to each hospital’s average annual mortality by the actual average hospital ARDS case volume while color signifies observations from low, medium, and high volume ARDS hospitals which corresponds to hospitals with 1-9, 10-49, and 50-431 cases annually. The lower and upper bounds of the box represent the 25th and 75th percentile, respectively. The whiskers represent 1.5 × the interquartile range. Box width is proportional to square-root of the number of observations in the group.
In a simple Poisson regression model including hospital of discharge as a random effect, when compared to low ARDS volume hospitals, high and medium ARDS volume hospitals were significantly associated with lower annual ARDS CFRs (RR 0.76 99%CI 0.76-0.84 and RR 0.85 99%CI 0.85-0.93, respectively; p≤0.001 for both). In a multivariable Poisson model including hospital of discharge as a random effect, and controlling for fixed effects of hospital region, overall bed size, urban/rural location, teaching status, ownership, mean Elixhauser score, and calendar year, hospitals with high and medium ARDS case volumes were associated with lower annual ARDS CFRs (RR 0.75 99%CI 0.71-0.79 and RR 0.86 99%CI 0.82-0.90, respectively; p≤0.001 for both)
Individual-Level Analysis
Of the 79,742,743 discharges from the 2002-2011 NIS, 123,954 met our ARDS case definition and 117,204 remained after exclusions. The selected results of the unadjusted bivariate analyses by mortality status are summarized in Tables 1–2 (eTables 1-5). In a logistic regression controlling for hospital of discharge as a fixed effect, there was a trend towards lower odds of ARDS mortality at high and medium ARDS volume hospitals compared to low ARDS volume hospitals (OR 0.89 (99% CI 0.77-1.03), p=0.03; OR 0.92 (CI 0.82-1.04), p=0.07, respectively).
Table 2.
Demographic and Clinical Characteristics of ARDS Cases by In-Hospital Mortality Status; NIS 2002-2011 (N=117,204)
| Variable | Mortality status | Odds ratio (CI) | p-value | |
|---|---|---|---|---|
| Alive N = 68,848 |
Died in hospital N = 48,356 |
|||
| Demographic | ||||
| Age in years, mean (SD) | 58.42 (18.17) | 66.29 (17.48) | 1.03 (1.02-1.03) | < 0.001 |
| Age group, years, % | ||||
| 18-29 | 9.01 | 4.68 | ref | ref |
| 30-39 | 7.89 | 4.44 | 1.08 (0.99-1.18) | 0.03 |
| 40-49 | 13.10 | 8.21 | 1.21 (1.11-1.31) | < 0.001 |
| 50-59 | 18.10 | 13.54 | 1.44 (1.34-1.55) | < 0.001 |
| 60-69 | 19.84 | 18.03 | 1.75 (1.63-1.88) | < 0.001 |
| 70-79 | 20.20 | 25.51 | 2.43 (2.26-2.61) | < 0.001 |
| ≥80 | 11.87 | 26.50 | 4.15 (3.86-4.47) | < 0.001 |
| Female, % | 41.40 | 44.85 | 1.15 (1.12-1.19) | < 0.001 |
| Race, % | ||||
| White | 58.48 | 59.36 | ref | ref |
| Black | 9.87 | 9.56 | 0.95 (0.90-1.01) | 0.02 |
| Hispanic | 7.54 | 7.18 | 0.94 (0.88-1.00) | 0.01 |
| Asian or Pacific Islander | 1.51 | 1.90 | 1.25 (1.11-1.40) | < 0.001 |
| Native American | 0.55 | 0.45 | 0.81 (0.65-1.01) | < 0.001 |
| Other | 2.77 | 2.75 | 0.98 (0.89-1.08) | 0.57 |
| Expected Primary Payer, % | ||||
| Medicare | 44.48 | 59.79 | ref | ref |
| Medicaid | 12.93 | 8.89 | 0.51 (0.49-0.54) | < 0.001 |
| Private including HMO | 31.36 | 21.93 | 0.52 (0.50-0.54) | < 0.001 |
| Self-pay | 5.31 | 5.45 | 0.76 (0.81-0.82) | < 0.001 |
| No charge | 0.73 | 0.47 | 0.48 (0.39-0.59) | < 0.001 |
| Other | 4.91 | 3.27 | 0.50 (0.46-0.54) | < 0.001 |
| Comorbid Conditionsa | ||||
| Elixhauser Comorbidity Score, mean (SD) | 7.63 (7.20) | 8.98 (7.44) | 1.03 (1.02-1.03) | < 0.001 |
| Severity Measures, % | ||||
| APR-DRG risk of mortalityb | ||||
| Minor likelihood of dying | 2.49 | 0.25 | ref | ref |
| Moderate likelihood of dying | 10.12 | 1.97 | 1.95 (1.50-2.52) | < 0.001 |
| Major likelihood of dying | 33.96 | 18.32 | 5.41 (4.23-6.91) | < 0.001 |
| Extreme likelihood of dying | 52.57 | 78.46 | 14.97 (11.73-19.10) | < 0.001 |
| APR-DRG severity of illness subclassb | ||||
| Minor loss of function | 0.03 | 0.01 | ref | ref |
| Moderate loss of function | 0.82 | 0.49 | 1.93 (0.53-6.98) | 0.19 |
| Major loss of function | 9.86 | 9.35 | 3.06 (0.86-10.92) | 0.02 |
| Extreme loss of function | 88.43 | 89.43 | 3.26 (0.91-11.61) | 0.02 |
| Discharge Quarter | ||||
| January –March | 25.11 | 26.46 | ref | ref |
| April-June | 25.91 | 25.14 | 0.92 (0.88-0.96) | < 0.001 |
| July-September | 25.60 | 25.02 | 0.93 (0.89-0.97) | < 0.001 |
| October-December | 23.33 | 23.29 | 0.95 (0.91-0.99) | < 0.001 |
| Admission-Weekday v. Weekend | ||||
| Monday-Friday | 78.00 | 77.95 | ref | ref |
| Saturday or Sunday | 22.00 | 22.05 | 1.00 (0.97-1.01) | 0.84 |
| Admission Typec | ||||
| Emergency | 46.51 | 52.60 | ref | ref |
| Urgent | 14.76 | 15.24 | 0.91 (0.87-0.95) | < 0.001 |
| Elective | 21.82 | 16.23 | 0.66 (0.63-0.69) | < 0.001 |
| Trauma center (beginning in 2003) | 6.12 | 3.79 | 0.55 (0.51-0.59) | < 0.001 |
| Other | 0.02 | 0.01 | 0.37 (0.10-1.37) | 0.05 |
| Length of Stay, Median (IQR) | 23 (16-35) | 10 (4-19) | 0.94 (0.94-0.95) | < 0.001 |
| OR Procedure | 77.16 | 63.61 | 0.52 (0.50-0.54) | < 0.001 |
ARDS = Acute Respiratory Distress Syndrome; APR-DRG = All patient refined diagnosis related grouping; CI = 99% confidence interval; HMO = Health Maintenance Organization; NIS=Nationwide Inpatient Sample; OR = operating room; SD = standard deviation
This represents a weighted Elixhauser Score based on comorbidities on discharge record. Comorbidities within the Healthcare Cost and Utilization Project (HCUP) are determined using the Agency for Healthcare Research and Quality (AHQR) comorbidity software which seeks to identify comorbid medical conditions present prior to admission (https://www.hcup-us.ahrq.gov/tools_software.jsp).
The All Patient Refined Diagnosis Related Grouping (APR-DRG) risk of mortality and severity of illness subclass are assigned using a software developed and maintained by 3M Health Information Systems (www.hcup-us.ahrq.gov). Category of ‘Minor loss of function’ includes cases with no comorbidity or complication.
11.33% of observations missing data on this variable.
In our a priori multivariable, individual-level model adjusting for fixed effects of hospital of discharge, age-group, sex, year, primary payer, hospital teaching status, and individual’s weighted Elixhauser score; high and medium ARDS volume hospitals were associated with lower odds of individual ARDS mortality when compared to low volume hospitals (OR 0.85 (99% CI 0.74-0.99), p=0.006; OR 0.89 (99% CI 0.79-1.00), p= 0.01, respectively) (eFigure 5).
Our multivariable individual-level model constructed from bivariate analyses included the following fixed effects: hospital of discharge, teaching status, race, year, admission type, operating room procedure, primary payer, principle diagnosis category, APR-DRG mortality risk category, hospital urban/rural location, and hospital region. In this model, high and medium ARDS volume hospitals were associated with a lower odds of ARDS mortality compared to low ARDS volume hospitals (OR 0.78 (99% CI 0.65-0.95), p = 0.001; OR 0.83 (99% CI 0.71-0.97), p = 0.002, respectively).
Secondary Analyses
We performed a number of individual-level sensitivity analyses. First, we assessed different case definitions of ARDS. One alternative ARDS case definition utilized the same ICD-9-CM diagnosis and procedure codes as the primary definition but did not have the additional stipulation: “if procedure code 96.71 (continuous mechanical ventilation of < 96 hours) were specified, the candidate case must also have a vital status as deceased”. The resultant cohort was larger, including 210,531 discharges, had a lower mortality at 22%, and we determined low, medium, and high volume hospitals to be hospitals with 1-4, 5-14 and 15-799 cases annually. Using the aforementioned a priori multivariable model covariates, when compared to low volume hospitals, high and medium volume centers were not associated with lower individual odds of hospital mortality (OR 0.88 (99% CI 0.71-1.10) p=0.1 and OR 1.04 (99% CI 0.86-1.25) p=0.6, respectively). A second alternative ARDS case definition used the same two ICD-9-CM diagnosis codes but without procedure codes. This cohort included 482,607 discharges with 16% hospital mortality and we determined low, medium, and high volume hospitals to be hospitals with 1-4, 5-49 and 50-2,243 cases annually. Using the aforementioned a priori multivariable model covariates, when compared to low volume hospitals, high but not medium volume hospitals were associated with lower individual odds of hospital mortality (OR 0.81 (99% CI 0.65-1.01) p=0.01 and OR 0.93 (99% CI 0.75-1.14) p=0.4, respectively).
In addition to these sensitivity analyses, we explored 2 other relationships not part of our initial hypothesis. First, we assessed the interaction between patient severity of illness and the volume-outcome relationship using our principle ARDs case definition. We used the covariates from our selected model and included an interaction term between ARDS hospital volume and APR-DRG mortality risk category. There was a statistically significant difference in the model that included the interaction (ANOVA p<0.001, Loess-smoothed curves in Figure 2). Secondly, we explored the interaction of the year of discharge on the volume-outcome association with the interaction model demonstrating a statistically significant difference (ANOVA, p<0.001, eFigure 6).
Figure 2. Adjusted In-Hospital Mortality by Annual Hospital ARDS Case Volume Stratified by Mortality Risk Group, NIS 2002-2011 (N= 117,204)a.
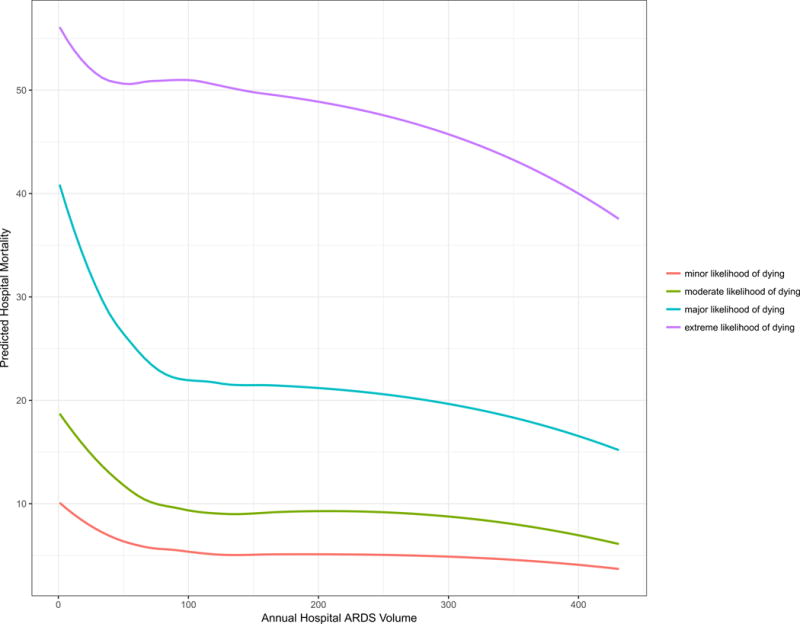
aData plotted are individual predicted hospital mortality by ARDS case volume category among ARDS discharges. Adjustment covariates include hospital, hospital teaching status and individual, sex, year of discharge, expected primary payer, and all payer diagnosis related group risk of mortality category, with an interaction term for risk category, and hospital ARDS volume category. Points correspond to each discharge’s predicted mortality by the actual hospital case volume for that year while color signifies observations from different underlying risk of mortality categories. The curves were created using the Loess method of ggplot2 package.
Discussion
In this analysis of administrative hospital discharge data from a large US cohort, we demonstrate associations of lower ARDS in-hospital mortality with higher annual ARDS case volume. First, at the unit of analysis of a hospital, higher annual hospital ARDS case volumes are associated with 0.75-0.86 relatively lower annual ARDS CFRs, even after adjusting for available hospital-level confounders. This relationship was preserved at the unit of analysis of the individual discharge. After controlling for available confounders, when compared to ARDS patients discharged from low volume hospitals, individuals discharged from high and medium volume hospitals had a range of a 0.78-0.89 lower odds of mortality.
There are several factors to keep in mind when interpreting the results of this data. First, the long timespan and the large sample size increase strengthen the generalizability of the association. Second, our study attempts to address a more specifically defined ARDS case-volume relationship whereas numerous other studies have explored more broad definitions of acute respiratory failure and mechanical ventilation volume [8–10, 12–17, 20]. However, our necessary reliance on an ICD-9 case definition may misclassify true cases of moderate-severe ARDS. Specifically, we recognize that while the disease process of interest is clinically defined moderate-severe ARDS, our case definition is at least 3 steps removed from this entity. First, the Berlin Definition clinical criteria are not specific at identifying histologically defined ARDS [26]. Second, clinicians often miss making the clinical diagnosis of ARDS [24]. Third, we hypothesize further misclassification occurs from the clinical diagnosis to the ICD-9-CM coding on the discharge record. To make this final step even more complicated, while 518.5 and 518.82 are the only ICD-9-CM codes that include ARDS as a synonym, there is no ICD-9-CM that is specifically titled as ARDS. Given these conditions, it is not possible to create a case definition that exactly matches our target population of moderate-severe ARDS. Strengthening the construct validity of the case definition, we did not use codes for “Acute Respiratory Failure, NOS” (518.81), “Chronic Respiratory Failure” (518.83), or “Acute and Chronic Respiratory Failure” (518.84) and did use mechanical ventilation codes that attempted to approach a more severe population [23]. The observation that our hospital mortality of 47% is similar to the mortality of moderate and severe ARDS in clinical studies offers support to our case definition [24, 25]. An additional limitation is that we were unable to account for all relevant hospital-level factors (e.g. number of ICU beds, staffing models, individual provider volume) or individual-level factors (physiologic data for acute illness severity) leaving the potential for residual confounding.
In attempt to explore some of the above limitations, we performed sensitivity analyses using two different, broader ICD-9-CM ARDS case definitions. These case definitions predictably produced larger cohorts with considerably lower average mortality rates with an attenuation of the volume-outcome relationship. For both of these analyses, there is attenuation of the associations at a variable level of significance, perhaps due to the capturing of many non-ARDS cases or lower severity cases.
These findings are novel, yet consistent with an existing body of literature that generally demonstrates improved outcomes among higher volume centers for many critical care diagnostic categories [8, 27]. Over the last several decades, numerous studies have strengthened the hypothesis that patients treated at high volume centers have improved clinical outcomes, particularly amongst surgical and cardiac patients [28, 29]. However, in specific regards to respiratory diagnoses among the critically ill, a recent meta-analysis has demonstrated significant heterogeneity [8, 27]. Our study differs from these included studies in that it attempts to more specifically identify moderate-severe ARDS cases. In additions to exploring the volume-outcome relationship, the study also explores underlying patient mortality risk, and calendar year of discharge on this volume-outcome association. In regards to underlying patient mortality risk, we make two graphical observations: 1) the volume-outcome relationship has a consistent direction throughout all risk categories, yet 2) the slope of volume-outcome relationship varies by risk group and is steepest among those with a “major risk of death” and attenuated in those with either an “extreme risk of death” and a “minor risk of death.” This effect modification supports the clinical intuition that patients with intermediate risk of dying may accrue the greatest benefits from care at an experienced high-volume center. Finally, in regards to the effect of time over the 2002-2011 study period, we see that the initial slope of the volume-outcome relationship remains stable yet for each subsequent time-frame there is a downward shift of the curve. This suggests that over the study period, there was a general downward trend in average ARDS mortality from 2002-2011.
Within the context of our study’s strengths and limitations, the data suggests that both at a hospital- and individual-level, medium and high volume ARDS centers are associated with better ARDS outcomes, even after adjustments for available confounders. Moreover, this association is sensitive to the underlying mortality risk of the ARDS population. The implications of our findings are clinically significant, particularly at a health systems-level, in considering the regionalization of ARDS care. Regionalization involves the processes and infrastructure of routing and transferring ARDS patients from low volume hospitals to higher volume hospitals. While our results generally lend support to regionalization for ARDS care during the study time period, it does not specifically address the question of whether routing or transfers of ARDS to higher volume centers can save lives. The re-routing and transferring of critically ill patients carries significant, potential risks and delays that may mitigate the generally higher performance of higher volume hospitals. Continued investigation of the impactful processes of high performing hospitals and the risks and benefits of regionalization for ARDS is still needed to help clarify whether improving performance in lower volume hospitals or regionalization of care are more beneficial from individual and societal perspectives.
Supplementary Material
Table 3.
Hospital Characteristics of ARDS Cases by In-Hospital Mortality Status, NIS 2002-2011 (N = 117,204)
| Variable | Mortality status | Odds ratio (CI) | p-value | |
|---|---|---|---|---|
| Alive N = 68,848 |
Died in hospital N = 43,922 |
|||
| Bed sizea | ||||
| Small | 9.17 | 8.28 | ref | ref |
| Medium | 18.96 | 19.99 | 1.17 (1.10-1.24) | < 0.001 |
| Large | 70.91 | 70.98 | 1.11 (1.05-1.11) | < 0.001 |
| Ownership | ||||
| Government, nonfederal | 16.51 | 15.71 | ref | ref |
| Private, non-profit | 68.87 | 71.54 | 1.09 (1.05–1.14) | < 0.001 |
| Private, invest-own | 12.68 | 11.29 | 0.94 (0.88-0.99) | < 0.001 |
| Location | ||||
| Rural | 4.00 | 5.56 | ref | ref |
| Urban | 95.04 | 93.70 | 0.71 (0.66-0.76) | < 0.001 |
| Teaching Status | ||||
| Non-teaching | 36.91 | 40.58 | ref | ref |
| Teaching | 62.13 | 58.67 | 0.83 (1.83-0.89) | < 0.001 |
| Region | ||||
| Northeast | 18.33 | 21.70 | ref | ref |
| Midwest | 21.99 | 19.44 | 0.75 (0.71-0.78) | < 0.001 |
| South | 39.05 | 37.85 | 0.82 (0.79-0.85) | < 0.001 |
| West | 20.63 | 21.01 | 0.86 (0.82-0.90) | < 0.001 |
| Total Volume, cases per year of discharge | ||||
| Low (42-10,000 discharges) | 15.00 | 15.99 | ref | ref |
| Medium (10,000-18,000 discharges) | 19.55 | 21.71 | 1.04 (0.99-1.10) | 0.04 |
| High (18,000-121,688 discharges) | 65.45 | 62.30 | 0.89 (0.86-0.93) | < 0.001 |
| ARDS Volume, cases per year of discharge | ||||
| Low (1-9 cases) | 8.96 | 12.32 | ref | ref |
| Medium (10-49 cases) | 35.71 | 39.56 | 0.81 (0.76-0.85) | < 0.001 |
| High (50-431 cases) | 55.33 | 48.11 | 0.63 (0.60-0.67) | < 0.001 |
ARDS = Acute Respiratory Distress Syndrome; CI = 99% confidence interval; SD = standard deviation
Designation of a hospital’s bed size as small, medium, or large is dependent upon geographic region and teaching status per American Hospital Association records. More information on the designations can be found on the Healthcare Cost and Utilization Project’s website (https://www.hcupus.ahrq.gov/db/vars/hosp_bedsize/nisnote.jsp) [29]
Acknowledgments
Funding Sources: Dr. Kempker receives support from the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR000454 and KL2 TR000455.
Dr. Martin receives support from the National Center for Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR000454.
Copyright form disclosure: Drs. Kempker and Martin received support for article research from the National Institutes of Health (NIH). Dr. Kempker’s institution received funding from National Center for Advancing Translational Sciences (NCATS). Dr. Martin’s institution received funding from NIH/NCATS (U01 TR-000454), Astute Medical, and Bristol-Myers Squibb, and he received funding from Bard, Edwards, Grifols, and Regeneron.
Footnotes
The remaining authors have disclosed that they do not have any potential conflicts of interest.
Contributor Information
John D. Ike, Emory University School of Medicine.
Jordan A. Kempker, Assistant Professor of Medicine, Division of Pulmonary, Allergy, Critical Care and Sleep Medicine, Emory University School of Medicine, 49 Jesse Hill Jr Dr SE, Atlanta, GA 30303.
Michael R. Kramer, Department of Epidemiology, Rollins School of Public Health, Emory University.
Greg S. Martin, Professor of Medicine, Division of Pulmonary, Allergy, Critical Care and Sleep Medicine, Emory University School of Medicine.
References
- 1.Li G, Malinchoc M, Cartin-Ceba R, Venkata CV, Kor DJ, Peters SG, Hubmayr RD, Gajic O. Eight-year trend of acute respiratory distress syndrome: a population-based study in Olmsted County, Minnesota. Am J Respir Crit Care Med. 2011;183(1):59–66. doi: 10.1164/rccm.201003-0436OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rubenfeld GD, Caldwell E, Peabody E, Weaver J, Martin DP, Neff M, Stern EJ, Hudson LD. Incidence and outcomes of acute lung injury. N Engl J Med. 2005;353(16):1685–1693. doi: 10.1056/NEJMoa050333. [DOI] [PubMed] [Google Scholar]
- 3.Amato MB, Barbas CS, Medeiros DM, Magaldi RB, Schettino GP, Lorenzi-Filho G, Kairalla RA, Deheinzelin D, Munoz C, Oliveira R, et al. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med. 1998;338(6):347–354. doi: 10.1056/NEJM199802053380602. [DOI] [PubMed] [Google Scholar]
- 4.Papazian L, Forel JM, Gacouin A, Penot-Ragon C, Perrin G, Loundou A, Jaber S, Arnal JM, Perez D, Seghboyan JM, et al. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med. 2010;363(12):1107–1116. doi: 10.1056/NEJMoa1005372. [DOI] [PubMed] [Google Scholar]
- 5.Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med. 2000;342(18):1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 6.Baumann WR, Jung RC, Koss M, Boylen CT, Navarro L, Sharma OP. Incidence and mortality of adult respiratory distress syndrome: a prospective analysis from a large metropolitan hospital. Crit Care Med. 1986;14(1):1–4. doi: 10.1097/00003246-198601000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Erickson SE, Martin GS, Davis JL, Matthay MA, Eisner MD. Recent trends in acute lung injury mortality: 1996-2005. Crit Care Med. 2009;37(5):1574–1579. doi: 10.1097/CCM.0b013e31819fefdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nguyen YL, Wallace DJ, Yordanov Y, Trinquart L, Blomkvist J, Angus DC, Kahn JM, Ravaud P, Guidet B. The Volume-Outcome Relationship in Critical Care: A Systematic Review and Meta-analysis. Chest. 2015;148(1):79–92. doi: 10.1378/chest.14-2195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cooke CR, Kennedy EH, Wiitala WL, Almenoff PL, Sales AE, Iwashyna TJ. Despite variation in volume, Veterans Affairs hospitals show consistent outcomes among patients with non-postoperative mechanical ventilation. Crit Care Med. 2012;40(9):2569–2575. doi: 10.1097/CCM.0b013e3182591eee. [DOI] [PubMed] [Google Scholar]
- 10.Darmon M, Azoulay E, Fulgencio JP, Garrigues B, Gouzes C, Moine P, Villers D, Teboul V, le Gall JR, Chevret S. Procedure volume is one determinant of centre effect in mechanically ventilated patients. Eur Respir J. 2011;37(2):364–370. doi: 10.1183/09031936.00195209. [DOI] [PubMed] [Google Scholar]
- 11.Dres M, Tran TC, Aegerter P, Rabbat A, Guidet B, Huchon G, Roche N, Group C-R Influence of ICU case-volume on the management and hospital outcomes of acute exacerbations of chronic obstructive pulmonary disease*. Crit Care Med. 2013;41(8):1884–1892. doi: 10.1097/CCM.0b013e31828a2bd8. [DOI] [PubMed] [Google Scholar]
- 12.Durairaj L, Torner JC, Chrischilles EA, Vaughan Sarrazin MS, Yankey J, Rosenthal GE. Hospital volume-outcome relationships among medical admissions to ICUs. Chest. 2005;128(3):1682–1689. doi: 10.1378/chest.128.3.1682. [DOI] [PubMed] [Google Scholar]
- 13.Fernandez R, Altaba S, Cabre L, Lacueva V, Santos A, Solsona JF, Anon JM, Catalan RM, Gutierrez MJ, Fernandez-Cid R, et al. Relationship between volume and survival in closed intensive care units is weak and apparent only in mechanically ventilated patients. Anesthesiology. 2013;119(4):871–879. doi: 10.1097/ALN.0b013e31829c3029. [DOI] [PubMed] [Google Scholar]
- 14.Gopal S, O’Brien R, Pooni J. The relationship between hospital volume and mortality following mechanical ventilation in the Intensive Care Unit. Minerva Anestesiol. 2011;77(1):26–32. [PubMed] [Google Scholar]
- 15.Kahn JM, Goss CH, Heagerty PJ, Kramer AA, O’Brien CR, Rubenfeld GD. Hospital volume and the outcomes of mechanical ventilation. N Engl J Med. 2006;355(1):41–50. doi: 10.1056/NEJMsa053993. [DOI] [PubMed] [Google Scholar]
- 16.Kahn JM, Ten Have TR, Iwashyna TJ. The relationship between hospital volume and mortality in mechanical ventilation: an instrumental variable analysis. Health Serv Res. 2009;44(3):862–879. doi: 10.1111/j.1475-6773.2009.00959.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lecuyer L, Chevret S, Guidet B, Aegerter P, Martel P, Schlemmer B, Azoulay E. Case volume and mortality in haematological patients with acute respiratory failure. Eur Respir J. 2008;32(3):748–754. doi: 10.1183/09031936.00142907. [DOI] [PubMed] [Google Scholar]
- 18.Lin HC, Xirasagar S, Chen CH, Hwang YT. Physician’s case volume of intensive care unit pneumonia admissions and in-hospital mortality. Am J Respir Crit Care Med. 2008;177(9):989–994. doi: 10.1164/rccm.200706-813OC. [DOI] [PubMed] [Google Scholar]
- 19.Moran JL, Bristow P, Solomon PJ, George C, Hart GK, Australian, New Zealand Intensive Care Society Database Management C Mortality and length-of-stay outcomes, 1993-2003, in the binational Australian and New Zealand intensive care adult patient database. Crit Care Med. 2008;36(1):46–61. doi: 10.1097/01.CCM.0000295313.08084.58. [DOI] [PubMed] [Google Scholar]
- 20.Needham DM, Bronskill SE, Rothwell DM, Sibbald WJ, Pronovost PJ, Laupacis A, Stukel TA. Hospital volume and mortality for mechanical ventilation of medical and surgical patients: a population-based analysis using administrative data. Crit Care Med. 2006;34(9):2349–2354. doi: 10.1097/01.CCM.0000233858.85802.5C. [DOI] [PubMed] [Google Scholar]
- 21.Shahin J, Harrison DA, Rowan KM. Is the volume of mechanically ventilated admissions to UK critical care units associated with improved outcomes? Intensive care medicine. 2014;40(3):353–360. doi: 10.1007/s00134-013-3205-4. [DOI] [PubMed] [Google Scholar]
- 22.HCUP NI Database Documentations. [ www.hcup-us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp.]
- 23.Reynolds HN, McCunn M, Borg U, Habashi N, Cottingham C, Bar-Lavi Y. Acute respiratory distress syndrome: estimated incidence and mortality rate in a 5 million-person population base. Crit Care. 1998;2(1):29–34. doi: 10.1186/cc121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, Gattinoni L, van Haren F, Larsson A, McAuley DF, et al. Epidemiology, Patterns of Care, and Mortality for Patients With Acute Respiratory Distress Syndrome in Intensive Care Units in 50 Countries. Jama. 2016;315(8):788–800. doi: 10.1001/jama.2016.0291. [DOI] [PubMed] [Google Scholar]
- 25.Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L, Slutsky AS. Acute respiratory distress syndrome: the Berlin Definition. Jama. 2012;307(23):2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 26.Thille AW, Esteban A, Fernandez-Segoviano P, Rodriguez JM, Aramburu JA, Penuelas O, Cortes-Puch I, Cardinal-Fernandez P, Lorente JA, Frutos-Vivar F. Comparison of the Berlin definition for acute respiratory distress syndrome with autopsy. Am J Respir Crit Care Med. 2013;187(7):761–767. doi: 10.1164/rccm.201211-1981OC. [DOI] [PubMed] [Google Scholar]
- 27.Kanhere MH, Kanhere HA, Cameron A, Maddern GJ. Does patient volume affect clinical outcomes in adult intensive care units? Intensive care medicine. 2012;38(5):741–751. doi: 10.1007/s00134-012-2519-y. [DOI] [PubMed] [Google Scholar]
- 28.Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med. 2002;137(6):511–520. doi: 10.7326/0003-4819-137-6-200209170-00012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


