Abstract
Purpose
The Italian Network of Longitudinal Metropolitan Studies (IN-LiMeS) is a system of integrated data on health outcomes, demographic and socioeconomic information, and represents a powerful tool to study health inequalities.
Participants
IN-LiMeS is a multicentre and multipurpose pool of metropolitan population cohorts enrolled in nine Italian cities: Turin, Venice, Reggio Emilia, Modena, Bologna, Florence, Leghorn, Prato and Rome. Data come from record linkage of municipal population registries, the 2001 population census, mortality registers and hospital discharge archives. Depending on the source of enrolment, cohorts can be closed or open. The census-based closed cohort design includes subjects resident in any of the nine cities at the 2001 census day; 4 466 655 individuals were enrolled in 2001 in the nine closed cohorts. The open cohort design includes subjects resident in 2001 or subsequently registered by birth or immigration until the latest available follow-up (currently 31 December 2013). The open cohort design is available for Turin, Venice, Reggio Emilia, Modena, Bologna, Prato and Rome. Detailed socioeconomic data are available for subjects enrolled in the census-based cohorts; information on demographic characteristics, education and citizenship is available from population registries.
Findings to date
The first IN-LiMeS application was the study of differentials in mortality between immigrants and Italians. Either using a closed cohort design (nine cities) or an open one (Turin and Reggio Emilia), individuals from high migration pressure countries generally showed a lower mortality risk. However, a certain heterogeneity between the nine cities was noted, especially among men, and an excess mortality risk was reported for some macroareas of origin and specific causes of death.
Future plans
We are currently working on the linkage of the 2011 population census data, the expansion of geographical coverage and the implementation of the open design in all the participating cohorts.
Keywords: inequalities, Italy, mortality, immigrants
Strengths and limitations of this study.
The Italian Network of Longitudinal Metropolitan Studies (IN-LiMeS) is a powerful monitoring system that integrates data on health outcomes, demographic and socioeconomic attributes for nine Italian cities.
The IN-LiMeS provides longitudinal information based on statistical, administrative and health data that have undergone coherence and validity checks and that are already available, minimising the costs.
Detailed socioeconomic information is available only for subjects enrolled in the census-based closed cohorts.
The IN-LiMeS enrolment is based on official administrative sources; therefore, in the studies focusing on immigrants’ health, those regularly present but not formally enrolled in any population register and undocumented immigrants are left out, limiting the generalisability of results.
Introduction
The unequal distribution of the societal determinants is widely recognised to be at the root of health inequalities.1 2 Individual socioeconomic circumstances,3 economic turmoil and policies,4 5 and international migration flow,6 among others dynamics, interplay in shaping differential patterns of mortality and morbidity at the local and global levels.
Describing and monitoring socioeconomic inequalities in health are an essential step towards policy changes aimed at promoting fair outcomes across the population. However, information on individuals’ socioeconomic attributes is seldom available in health and mortality data sources. In order to overcome this limitation, in many European countries monitoring systems at national or subnational levels have been set up. These systems usually combine health information with indicators of socioeconomic status (SES) retrieved from official statistics, administrative sources or surveys.7 8
Evidence accrued throughout the years generally highlighted an inverse relationship between SES and health outcomes.9–11 In terms of mortality, it has been reported that educational disparities increased until around the end of the 20th century all across Europe.12 Since then, relative inequalities widened in most Northern and Eastern European countries, while they remained substantially unchanged in cities and regions of Southern European countries usually included in international comparisons (Madrid, Barcelona and the Basque Country for Spain, and Turin for Italy).13 14
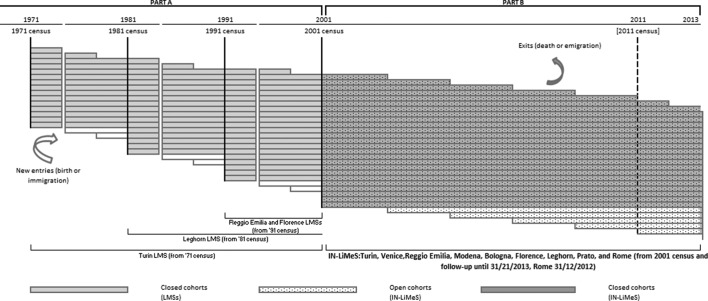
Studies on inequalities are usually either cross-sectional or longitudinal. Cross-sectional studies are based on routine mortality or morbidity statistics, and use official estimates of the population to obtain the denominators. These studies are common in the Baltic Sea and Eastern European countries.15 16 Longitudinal studies collect individual information on SES from official sources or surveys and follow the population up to death or migration. This design is mostly adopted in Northern, Western and Central European countries.17 Whereas in the Nordic countries data are usually available for the whole population,18 in France and the UK relevant information is generally collected in representative samples of the national population through either cross-sectional surveys or longitudinal development of cross-sectional surveys.14 19 This is also the case in Italy, where longitudinal extensions of the National Health Interview Survey have been set up following up the representative sample of the Italian population included in the survey through a record linkage with mortality and hospital discharge archives.20 In addition, census-based longitudinal metropolitan studies (LMS) have been implemented in some Italian cities since the 1980s.21–26 They integrate, for the resident population, individual information coming from the population registers at municipal level with microdata from the census and from the health information system. The first LMS was established in Turin using the 1971 census cohort.25 Lately, other LMSs were set up, namely the Tuscan study (including Leghorn from 1981, Florence from 1991 and Prato from 2001),23 the Emilian LMS (including Reggio Emilia from 1991, Modena and Bologna from 2001),22 and the Rome and the Venice LMSs, which both started with the 2001 census.21 26 Figure 1 part A provides an overview of the LMSs operating before the 2001 census. The LMSs have already worked, independently or in collaboration with the others, to investigate socioeconomic inequalities in health.22 27–31 Currently, other cities across the country are in the process of linking sociodemographic and health data in order to create their own LMS.
Figure 1.
Structure of the Italian Network of Longitudinal Metropolitan Studies (IN-LiMeS) and of the participant longitudinal metropolitan studies (LMSs): population entries and exits and availability of data.
In order to enhance and coordinate these nationwide efforts, the Italian Network of Longitudinal Metropolitan Studies (IN-LiMeS) has been officially created and included in the National Statistical Programme.32
The aim of the IN-LiMeS is to create a harmonised system of cohorts that provides a powerful, coherent and nationally widespread source of integrated data on morbidity and mortality outcomes, demographic and socioeconomic information, and denominators through the exact estimation of person/time at risk.
In this paper we describe the data collection and the data harmonisation process undertaken by the participating cohorts. Furthermore, we present the results of the first application of this network, namely the analysis of differentials in mortality between Italians and immigrants. We also present the features of the open and closed cohorts, the two different study designs that can be applied with the available data.
Cohort description
Setting, coverage and sources
The IN-LiMeS is a multicentre and multipurpose pool of metropolitan population cohorts enrolled in nine Italian cities, namely Turin, Venice, Reggio Emilia, Modena, Bologna, Florence, Leghorn, Prato and Rome. The number of inhabitants in these cities ranges from 140 000 to 2.5 million; they are located in northern and central areas of the peninsula.
The IN-LiMeS functions as an integrated monitoring system that gathers demographic, socioeconomic and clinical information at individual level. The minimum core of population data (ie, the standard information required to participate in the network) includes four sources: (1) the municipal population register, (2) the archives of the 2001 population census from the National Institute of Statistics (ISTAT), (3) the archives of mortality registers and (4) the electronic health records, namely hospital discharge archives. The population register databases include exact dates of registration (birth and/or immigration) and cancellation (emigration and/or death) for each individual. Therefore, they keep a dynamic and updated record of all inhabitants’ residential histories, including episodes of emigration, reimmigration and/or death. The estimated level of accuracy of the population registration system is higher than 99% nationally.33 The Italian National Health Service is tax-funded and has universal coverage. All Italian citizens, legal foreign residents and, to a certain extent, undocumented migrants are entitled to receive hospital inpatients care free of charge and the use of private care is negligible.34 Therefore, the hospital discharge archives ensure virtually complete coverage of the inpatient care provision to the resident population.35
The population register, the 2001 census, the mortality and the hospital discharge records are combined, at the individual level, through stepwise deterministic record linkage procedures. The linkage between the population registers and the census is performed using a specific set of keys (codes of the census questionnaire). The linkage rates, calculated as the proportion of subjects who were legal residents according to the official 2001 census figures and those retrieved in the population registers, were 98% for Venice, Bologna and Modena, 97% for Reggio Emilia, 96% for Turin, 92% for Prato, and 84% for Florence, Leghorn and Rome. We generally found no difference in the gender distribution and a small difference in the age distribution: the proportion of subjects in the oldest age groups was slightly higher among those for whom the linkage was unsuccessful than those enrolled in the closed cohort. The linkage with health databases follows different methodologies in each city, depending on the characteristics of local administrative archives. In the case of the mortality register, the linkage rate was around 98% for all cities but Prato (91%); deaths retrieved in the population register but not found in the mortality register are kept and classified as ‘population-register-only’.
Confidentiality is guaranteed through the deletion of personally identifiable information from individual records and the assignment of internal IDs to allow the linkage of multiple data source. The inclusion in the National Statistical Programme complies with the national legislation on the processing of personal data for statistical and scientific research purposes, for both IN-LiMeS and each single LMS.32
Cohort design
The most recent IN-LiMeS cohorts’ enrolment started at the 2001 census day (21 October 2001); at that time, all the cities together counted around five million inhabitants who represented about 9% of the Italian population. The choice of the study design, closed or open (figure 1 part B), mainly depends on three key elements: the research question, the availability of the SES information and the possibility for each LMS to acquire dynamic information on the new entries from the population registers. Most of the SES indicators are available only for subjects who took part in the decennial census; therefore, if the main interest were to study the relationship of SES with health, a census-based cohort would be the natural choice. This study would have a closed design in which all subjects are enrolled at the same point in calendar time, that is, 2001 census date. In these closed cohorts, individuals can exit (ie, death or emigration) but new entries are not allowed. On the other hand, an open cohort design gives the possibility of accounting for the changing dynamics of the population, although only a few indicators of SES may be available. In the open cohort design, enrolment is based on municipal population registers and members can enter (ie, newborn or new residents) and leave (ie, death or emigration) the cohort over time. Eligible individuals are those who have resided in the cities at any time since the 2001 census day until the latest available follow-up update. Turin and Reggio Emilia were the first two cohorts that became open. To date, also Venice, Modena, Bologna, Prato and Rome can adopt this design, while Florence and Leghorn are still working on the acquisition and harmonisation of information on new entries from the population registers. Follow-up data are currently available for all cohorts but Rome until 31 December 2013 (latest follow-up available for Rome, 31 December 2012). Future updates include the addition of the 2011 census data, a periodical update of the follow-up for the new entries and exits (including mortality data), and the opening of the remaining cohorts.
Measurements
IN-LiMeS gathered a rich range of information on sociodemographic characteristics and health outcomes. In table 1 we summarise the variables useful to study health inequalities that are currently available in a harmonised form, with their data sources.
Table 1.
Italian Network of Longitudinal Metropolitan Studies data sources and available variables
| Data sources | ||||
| Population register | 2001 census | Mortality register | Hospital discharge archive | |
| Demographic information | ||||
| Gender | √ | √ | √ | √ |
| Date of birth | √ | √ | √ | √ |
| Place of birth | √ | √ | √ | √ |
| Citizenship | √ | √ | √ | √ |
| Civil status | √ | √ | ||
| Date of immigration in the municipality | √ | |||
| Date of emigration from the municipality | √ | |||
| Socioeconomic characteristics | ||||
| Educational level | √* | √ | √ | |
| Occupational condition | √ | |||
| Occupational class | √ | |||
| Housing characteristics (ownership, dwelling structure and dimensions, sanitary equipment, heating system)† | √ | |||
| Household overcrowding† | √ | |||
| Health outcomes | ||||
| Date of death | √ | √ | ||
| Cause of death | √ | |||
| Date of hospital admission | √ | |||
| Date of hospital discharge | √ | |||
| Main diagnosis of hospital admission | √ | |||
| Type of admission (inpatient or day-hospital) | √ | |||
| Comorbidities | √ | |||
*Educational level from population registers is currently available in the cohorts of Turin, Venice, Reggio Emilia, Modena and Bologna.
†Information available only for non-institutionalised individuals.
Demographic information comes mainly from municipal population registers and includes birth or subsequent registration and death or emigration dates, place of birth, in addition to residence address, household composition, educational level and key variables necessary for record linkage with census. Holding birth or registration dates, and death or emigration dates allows the estimation of the exact person-time at risk for each individual in the cohort.
Citizenship is used to define the migration status according to a geographical classification that groups together people from high migratory pressure countries (HMPC: Central-Eastern Europe, North Africa, Sub-Saharan Africa, Asia except for Israel and Japan, and Central and South America)36 and those from complementary highly developed countries (HDC).
As shown in table 1, socioeconomic attributes currently available for the resident population who took part in the decennial 2001 census encompass information on education, occupation, marital status and household conditions; they pertain to and measure different dimensions of the socioeconomic stratification.37 They can be derived at individual, household and small area levels. An example of the former is the occupational class, which can be based on a neo-Weberian classification and results from the combination of information on occupational position and type of work activity.38 An example of the latter is the Italian Deprivation Index that has been extensively used in epidemiological research to measure social and material deprivation at municipal or census block level.39 A subset of SES indicators is potentially retrievable also from the population registers; an analysis of the consistency of these variables between the census, which we generally consider a gold standard, and the population registers is underway.
Details on mortality and health outcomes come from the mortality register and the electronic health records, respectively. Mortality registers collect the cause of death, coded according to the 9th or the 10th revision of the International Classification of Diseases (ICD), depending on the year of death and when the transition between the two revisions occurred in the mortality register of each city.40 Hospital discharge archives include up to five diagnoses and procedures coded according to the 9th revision of the ICD-Clinical Modification, dates of admission, discharge, wards of inpatient stay and dates of each transfer between wards or hospitals. Hospital discharges enable the calculation of hospitalisation rates, length of stay for each admission episode and comorbidity scores through an analysis of the hospitalisation history of each individual.41
Baseline characteristics
For descriptive purposes, the demographic and socioeconomic characteristics of the 4 466 655 individuals enrolled at the 2001 census day in the nine closed cohorts are reported in table 2.
Table 2.
Proportional distribution (%) of the baseline characteristics of subjects enrolled in the closed cohorts at 21 October 2001 in the nine cities of the Italian Network of Longitudinal Metropolitan Studies, by gender
| Turin | Venice | Bologna | Modena | Reggio Emilia | Florence | Leghorn | Prato | Rome | Overall | |||||||||||
| Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female | |
| Total (N) | 393 451 | 437 064 | 124 653 | 139 462 | 166 405 | 193 389 | 81 904 | 89 458 | 65 302 | 71 001 | 138 978 | 159 696 | 63 156 | 68 239 | 76 727 | 81 287 | 997 652 | 1 118 831 | 2 108 228 | 2 358 427 |
| Age group (years) | ||||||||||||||||||||
| 0 | 0.4 | 0.4 | 0.8 | 0.7 | 0.8 | 0.7 | 1.0 | 0.9 | 1.2 | 1.0 | 1.7 | 1.4 | 1.6 | 1.3 | 1.9 | 1.7 | 0.9 | 0.8 | 0.9 | 0.8 |
| 1–14 | 11.2 | 9.5 | 10.5 | 8.7 | 9.6 | 7.9 | 11.9 | 10.4 | 12.9 | 11.5 | 10.3 | 8.6 | 11.6 | 10.1 | 12.5 | 11.3 | 12.9 | 10.8 | 11.9 | 10.1 |
| 15–29 | 16.6 | 14.5 | 15.9 | 13.2 | 15.0 | 12.4 | 16.6 | 14.6 | 17.4 | 15.8 | 16.1 | 13.5 | 17.3 | 15.4 | 19.3 | 17.6 | 18.1 | 16.0 | 17.2 | 15.1 |
| 30–49 | 31.0 | 28.1 | 31.0 | 27.3 | 31.2 | 27.3 | 32.1 | 28.9 | 32.3 | 29.1 | 29.0 | 26.3 | 29.6 | 28.1 | 31.4 | 29.8 | 31.0 | 30.2 | 31.0 | 29.0 |
| 50–64 | 21.2 | 21.5 | 22.1 | 22.1 | 20.8 | 21.0 | 20.1 | 20.1 | 18.8 | 18.4 | 21.7 | 22.0 | 21.7 | 21.5 | 19.5 | 19.6 | 20.2 | 20.9 | 20.6 | 21.0 |
| 65+ | 19.6 | 26.0 | 19.7 | 28.0 | 22.6 | 30.7 | 18.3 | 25.1 | 17.4 | 24.2 | 21.2 | 28.2 | 18.2 | 23.6 | 15.4 | 20.0 | 16.9 | 21.3 | 18.4 | 24.0 |
| Missing value | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Total | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Educational level* (≥30 years old) | ||||||||||||||||||||
| University (ISCED 4–6) | 14.2 | 11.3 | 13.5 | 9.9 | 20.3 | 16.5 | 14.8 | 12.5 | 11.9 | 10.6 | 18.4 | 15.4 | 11.2 | 9.5 | 6.8 | 6.5 | 19.5 | 15.8 | 17.0 | 13.8 |
| Upper secondary school (ISCED 3A–3B) | 24.3 | 18.1 | 23.9 | 17.4 | 24.7 | 19.9 | 25.0 | 20.3 | 24.9 | 20.5 | 25.1 | 20.9 | 25.2 | 20.5 | 20.0 | 16.3 | 30.7 | 25.6 | 27.2 | 22.0 |
| Lower secondary and vocational school (ISCED 2, 3C) | 37.0 | 35.6 | 35.4 | 31.0 | 29.7 | 26.8 | 30.4 | 26.5 | 34.3 | 28.7 | 30.9 | 26.4 | 35.6 | 29.5 | 34.8 | 29.2 | 30.6 | 30.3 | 32.5 | 30.4 |
| Primary school (ISCED 1) | 21.0 | 28.2 | 24.7 | 35.5 | 22.8 | 30.4 | 26.7 | 34.2 | 26.1 | 33.9 | 23.7 | 32.0 | 24.8 | 32.7 | 33.6 | 38.8 | 17.0 | 22.9 | 20.7 | 27.5 |
| No education (ISCED 0) | 3.5 | 6.8 | 2.5 | 6.2 | 2.5 | 6.4 | 3.1 | 6.5 | 2.8 | 6.3 | 1.9 | 5.3 | 3.2 | 7.8 | 4.8 | 9.2 | 2.2 | 5.4 | 2.6 | 6.3 |
| Missing value | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Total (n) |
100 (282 454) |
100 (330 342) |
100 (90 798) |
100 (107 923) |
100 (124 195) |
100 (152 737) |
100 (57 713) |
100 (66 344) |
100 (44 740) |
100 (50 935) |
100 (102 009) |
100 (124 306) |
100 (44 818) |
100 (50 845) |
100 (52 214) |
100 (57 735) |
100 (679 096) |
100 (809 881) |
100 (1 478 038) |
100 (1 754 997) |
| Occupational condition (30–64 years old) | ||||||||||||||||||||
| Employed | 75.2 | 52.9 | 74.3 | 47.1 | 77.3 | 61.6 | 78.4 | 62.7 | 81.1 | 60.7 | 77.5 | 57.9 | 74.4 | 44.3 | 82.1 | 53.7 | 76.5 | 50.9 | 76.5 | 53.0 |
| Unemployed/looking for first occupation | 6.0 | 6.5 | 3.8 | 3.4 | 3.6 | 3.4 | 2.9 | 3.6 | 2.5 | 3.3 | 4.0 | 4.5 | 5.1 | 7.3 | 3.5 | 5.4 | 8.2 | 6.6 | 6.2 | 5.8 |
| Housewife | 0.1 | 25.8 | 0.1 | 38.0 | 0.0 | 15.3 | 0.3 | 16.1 | 0.0 | 20.8 | 0.0 | 21.3 | 0.1 | 38.7 | 0.1 | 29.6 | 0.1 | 32.2 | 0.7 | 28.5 |
| Student | 0.5 | 0.5 | 0.4 | 0.5 | 0.6 | 0.7 | 14.8 | 0.4 | 0.2 | 0.3 | 0.7 | 0.7 | 0.4 | 0.5 | 0.3 | 0.4 | 0.6 | 0.7 | 1.0 | 0.6 |
| Retired | 15.5 | 12.6 | 18.8 | 9.3 | 16.2 | 17.4 | 1.9 | 15.8 | 13.9 | 13.2 | 15.2 | 13.6 | 16.7 | 7.4 | 11.6 | 9.2 | 11.0 | 7.6 | 12.6 | 10.3 |
| Other conditions | 2.7 | 1.7 | 2.0 | 1.3 | 2.3 | 1.6 | 1.7 | 1.4 | 2.3 | 1.7 | 2.6 | 2.0 | 3.3 | 1.8 | 2.4 | 1.7 | 3.6 | 2.0 | 3.0 | 1.8 |
| Missing value | 0.0 | 0.0 | 0.6 | 0.4 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Total (n) |
100 (205 511) |
100 (216 780) |
100 (66 223) |
100 (68 930) |
100 (86 591) |
100 (93 392) |
100 (42 735) |
100 (43 894) |
100 (33 392) |
100 (33 766) |
100 (70 671) |
100 (76 955) |
100 (32 586) |
100 (33 903) |
100 (39 540) |
100 (40 569) |
100 (510 104) |
100 (571 541) |
100 (1 089 453) |
100 (1 179 730) |
| Occupational class (30–64 years old) | ||||||||||||||||||||
| Bourgeoisie | 27.3 | 21.3 | 28.4 | 22.7 | 34.5 | 27.2 | 30.3 | 22.9 | 26.5 | 20.2 | 35.7 | 28.1 | 28.2 | 20.9 | 25.1 | 17.1 | NA | NA | 29.6 | 23.1 |
| Middle class | 17.4 | 36.4 | 18.7 | 36.3 | 17.6 | 36.8 | 17.3 | 36.0 | 15.9 | 36.0 | 16.9 | 36.2 | 17.1 | 37.6 | 11.5 | 28.2 | NA | NA | 17.0 | 35.9 |
| Self-employed with employees | 2.6 | 1.3 | 19.7 | 13.2 | 3.5 | 1.6 | 4.5 | 2.0 | 4.6 | 1.9 | 3.6 | 1.5 | 3.0 | 1.8 | 5.7 | 3.2 | NA | NA | 5.3 | 2.8 |
| Self-employed without employees | 16.8 | 12.1 | 0.0 | 0.0 | 19.0 | 11.0 | 16.0 | 10.5 | 21.5 | 12.5 | 19.0 | 10.9 | 18.0 | 15.9 | 22.0 | 15.9 | NA | NA | 17.9 | 11.7 |
| Skilled working class | 18.3 | 7.2 | 15.4 | 8.4 | 13.1 | 7.4 | 17.3 | 8.6 | 17.3 | 9.9 | 12.1 | 7.8 | 16.5 | 6.5 | 17.8 | 14.2 | NA | NA | 16.4 | 9.2 |
| Unskilled working class | 17.6 | 21.7 | 17.8 | 19.4 | 12.3 | 16.0 | 14.6 | 20.0 | 14.2 | 19.5 | 12.7 | 15.5 | 17.2 | 17.3 | 17.9 | 21.4 | NA | NA | 13.8 | 17.3 |
| Missing value | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | NA | NA | 0.0 | 0.0 |
| Total (n) |
100 (154 635) |
100 (114 738) |
100 (49 283) |
100 (32 606) |
100 (66 930) |
100 (57 501) |
100 (34 067) |
100 (27 510) |
100 (27 079) |
100 (20 485) |
100 (54 752) |
100 (44 587) |
100 (24 257) |
100 (15 025) |
100 (32 465) |
100 (21 789) |
NA | NA | 100 (443 468) |
100 (334 241) |
| Civil status (≥ 30 years old) | ||||||||||||||||||||
| Unmarried | 19.0 | 14.0 | 19.3 | 14.6 | 22.3 | 17.7 | 18.2 | 13.3 | 18.7 | 13.2 | 19.2 | 16.0 | 13.4 | 9.9 | 14.5 | 10.4 | 17.1 | 14.6 | 18.1 | 14.5 |
| Married | 70.1 | 58.1 | 70.8 | 57.9 | 66.1 | 52.8 | 71.6 | 59.6 | 71.9 | 60.2 | 70.5 | 56.0 | 76.5 | 62.9 | 77.5 | 66.4 | 73.4 | 59.7 | 71.9 | 58.7 |
| Widowed | 3.9 | 19.4 | 4.4 | 21.5 | 5.0 | 21.7 | 4.3 | 20.0 | 4.0 | 19.9 | 4.6 | 20.8 | 4.4 | 20.3 | 3.6 | 17.7 | 3.7 | 17.3 | 4.0 | 18.9 |
| Separated | 4.3 | 4.6 | 3.4 | 3.2 | 3.8 | 3.7 | 3.4 | 3.6 | 3.2 | 3.4 | 3.3 | 3.5 | 3.8 | 4.0 | 2.8 | 3.0 | 3.7 | 4.8 | 3.7 | 4.3 |
| Divorced | 2.7 | 3.9 | 2.1 | 2.8 | 2.8 | 4.1 | 2.5 | 3.5 | 2.2 | 3.3 | 2.4 | 3.7 | 1.9 | 2.9 | 1.6 | 2.5 | 2.1 | 3.6 | 2.3 | 3.6 |
| Missing value | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Total (n) |
100 (282 454) |
100 (330 342) |
100 (90 798) |
100 (107 923) |
100 (124 195) |
100 (152 737) |
100 (57 713) |
100 (66 344) |
100 (44 740) |
100 (50 935) |
100 (102 009) |
100 (124 306) |
100 (44 818) |
100 (50 845) |
100 (52 214) |
100 (57 735) |
100 (679 096) |
100 (809 881) |
100 (1 478 038) |
100 (1 751 048) |
| Housing characteristics†‡ | ||||||||||||||||||||
| Well-off | 12.4 | 12.2 | NA | NA | 16.1 | 15.6 | 27.1 | 26.3 | 28.1 | 27.3 | 15.3 | 15.2 | 11.5 | 11.5 | 24.3 | 24.5 | NA | NA | 16.6 | 16.2 |
| Large houses | 23.7 | 23.2 | NA | NA | 31.3 | 30.3 | 38.8 | 38.7 | 39.7 | 39.7 | 40.9 | 40.1 | 37.5 | 36.9 | 43.9 | 43.6 | NA | NA | 32.0 | 31.5 |
| Middle-small properties | 36.9 | 37.7 | NA | NA | 31.0 | 31.9 | 15.6 | 16.9 | 15.9 | 17.1 | 26.9 | 27.2 | 28.1 | 28.2 | 20.2 | 20.4 | NA | NA | 29.6 | 30.3 |
| Small houses | 24.5 | 24.7 | NA | NA | 20.0 | 20.6 | 16.7 | 16.4 | 13.6 | 13.3 | 13.6 | 14.1 | 14.1 | 14.3 | 8.0 | 8.1 | NA | NA | 19.0 | 19.3 |
| Uncomfortable | 2.4 | 2.1 | NA | NA | 1.4 | 1.5 | 1.6 | 1.5 | 2.3 | 2.3 | 3.3 | 3.4 | 8.8 | 9.1 | 3.6 | 3.4 | NA | NA | 2.7 | 2.6 |
| Missing value | 0.1 | 0.1 | NA | NA | 0.2 | 0.1 | 0.2 | 0.2 | 0.4 | 0.4 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | NA | NA | 0.1 | 0.1 |
| Total (n) |
100 (392 145) |
100 (435 686) |
NA | NA | 100 (164 515) |
100 (191 196) |
100 (81 405) |
100 (88 574) |
100 (64 839) |
100 (70 301) |
100 (131 485) |
100 (152 245) |
100 (59 125) |
100 (64 478) |
100 (71 535) |
100 (76 258) |
NA | NA | 100 (965 049) |
100 (1 078 739) |
| Household overcrowding† | ||||||||||||||||||||
| Not overcrowded | 68.6 | 72.1 | NA | NA | 81.0 | 83.2 | 86.1 | 88.0 | 87.3 | 89.1 | 85.3 | 86.9 | 80.2 | 81.4 | 87.8 | 88.7 | NA | NA | 67.3 | 80.3 |
| Overcrowded | 31.4 | 27.9 | NA | NA | 18.8 | 16.7 | 13.8 | 11.9 | 12.6 | 10.9 | 14.7 | 13.1 | 19.8 | 18.6 | 12.2 | 11.3 | NA | NA | 32.7 | 19.7 |
| Missing value | 0.0 | 0.0 | NA | NA | 0.2 | 0.1 | 0.1 | 0.1 | 0.1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | NA | NA | 0.0 | 0.0 |
| Total (n) |
100 (392 145) |
100 (435 686) |
NA | NA | 100 (164 515) |
100 (191 196) |
100 (81 405) |
100 (88 574) |
100 (64 839) |
100 (70 301) |
100 (131 485) |
100 (152 245) |
100 (59 125) |
100 (64 478) |
100 (71 535) |
100 (76 258) |
NA | NA | 100 (965 049) |
100 (1 078 739) |
| Citizenship | ||||||||||||||||||||
| Italian | 96.2 | 96.5 | 98.2 | 98.4 | 96.3 | 96.5 | 94.7 | 94.6 | 95.1 | 95.7 | 98.3 | 98.2 | 98.9 | 98.7 | 95.5 | 95.9 | 97.7 | 97.2 | 97.1 | 97.0 |
| Highly developed countries | 0.2 | 0.4 | 1.5 | 1.1 | 0.4 | 0.5 | 0.3 | 0.3 | 0.2 | 0.3 | 0.2 | 0.5 | 0.1 | 0.2 | 0.2 | 0.4 | 0.3 | 0.6 | 0.4 | 0.5 |
| High migratory pressure countries | 3.6 | 3.1 | 0.3 | 0.5 | 3.3 | 3.0 | 5.0 | 5.1 | 4.7 | 4.0 | 1.5 | 1.3 | 1.0 | 1.1 | 4.3 | 3.7 | 2.0 | 2.2 | 2.5 | 2.5 |
| Missing value | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Total | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
*Education is the highest attained level of education. For each educational level the correspondence with the International Standard Classification of Education (ISCED) is provided.
†Variable available only for non-institutionalised individuals.
‡Composite variable that combines housing ownership, home dimension, availability of toilets inside the house and availability of heating system.
NA, not available; in the Venetian data it is not possible to distinguish between self-employed with or without employees.
In all cities, women outnumbered men and their age distribution was visibly shifted towards older ages. The gender-specific age distribution was generally comparable between the cohorts, although inhabitants of Reggio Emilia, Leghorn, Prato and Rome were slightly younger than the average. The distribution of the educational level in people aged more than 30 years differed between cohorts, as it was for the occupational status for those aged 30–64. Housing conditions, in the cohorts for whom this information was available, differed by city; overcrowding was the highest in Turin and the lowest in Reggio Emilia. Immigrants from HMPCs made up approximately 2.5% of the total populations, with the exception of Modena, where about 5% of subjects enrolled came from HMPCs. The population structure by age and gender of immigrants differed between cohorts, but it was consistently different from the native population (data not shown). This observation led to limit the population included in the analyses comparing immigrants with Italians to the age range 1–64 years. Lastly, immigrants from HDCs generally represented less than 0.5%.
Findings to date
The study of immigrant health had a central role in initiating the IN-LiMeS collaborative network, and its first application was the study of differentials in mortality between immigrants and Italians. Indeed, migration is a keenly debated topic in Italy: during the last decade, it has reshaped the demography at national level, and the migration process, from its inception to the arrival in the country of destination, is a relevant social determinant of population’s health.42 In addition, there is scanty evidence on immigrants’ mortality in Italy and, when available, it is based on cross-sectional studies.43
Individual were classified as immigrants if they had a citizenship of any of the HMPCs. Residents with citizenship from HDCs were not included in the analysis as they represent a very small population subgroup and are deemed to be comparable with natives in terms of sociodemographic and health patterns.44 As previously mentioned, only individuals aged 1–64 years during the follow-up time were analysed because subjects over 65 years are strongly under-represented among immigrants in Italy, and infant mortality patterns may differ between Italians and foreigners.
We studied the association between immigrant status and all-cause mortality in the nine IN-LiMeS cities using a closed cohort design with enrolment at 21 October 2001 and follow-up until 31 December 2013. Table 3 reports the number of events, person-years and mortality rate ratios (MRRs) estimated through Poisson regression models (adjusted for 5-year age groups, calendar years and stratified by sex). Individuals contributed with over 32 359 000 person-years. Immigrants’ contribution to person-time at risk was low, ranging from 1.1% in Leghorn to 5.7% in Modena for men, and from 1.4% in Leghorn to 5.6% in Modena for women. Accounting for the different age structure, the all-cause mortality risk was generally lower for immigrants than for Italians (MRR for men: 0.77, 95% CI 0.65 to 0.89; MRR for women: 0.79, 95% CI 0.71 to 0.88), although a certain heterogeneity was noted. Among men, immigrants residing in Venice showed a marked reduction in the risk (MRR 0.35, 95% CI 0.17 to 0.70), while those residing in Modena an indication of excess mortality (MRR 1.17, 95% CI 0.87 to 1.56) (P value from the heterogeneity χ 2 test=0.02). The advantage among immigrant women seems to be mostly minimal with some exceptions (P value from the heterogeneity χ2 test=0.47). The mortality risk was significantly lower among female immigrants living in Florence or Rome (MRR 0.36, 95% CI 0.14 to 0.97; MRR 0.79, 95% CI 0.68 to 0.91, respectively). At the same time, a non-significant excess of risk appeared among immigrant women living in Modena, Leghorn or Prato (MRR 1.04, 95% CI 0.70 to 1.55; MRR 1.08, 95% CI 0.51 to 2.27; MRR 1.11, 95% CI 0.71 to 1.73, respectively).
Table 3.
Number of individual at risk, deaths, person-years, and mortality rate ratios - MRRs - with their 95% confidence interval (95% CI) by gender, immigration status and city, age 1–64 years, follow-up period 2001–2013
| Male | Female | |||
| Italian | Immigrants† | Italian | Immigrants† | |
| Turin | ||||
| Individual at risk | 300 469 | 13 518 | 307 526 | 12 936 |
| Deaths | 7629 | 153 | 4705 | 94 |
| Person-years | 2 874 743.3 | 140 999.3 | 2 956 878.9 | 134 702.3 |
| MRR (95% CI) | 1 | 0.70 (0.60 to 0.83) | 1 | 0.81 (0.66 to 0.99) |
| Venice | ||||
| Individual at risk | 97 883 | 1919 | 98 307 | 1535 |
| Deaths | 2468 | 8 | 1517 | 10 |
| Person-years | 871 259.5 | 15 280.0 | 875 641.9 | 12 695.6 |
| MRR (95% CI) | 1 | 0.35 (0.17 to 0.70) | 1 | 0.83 (0.45 to 1.55) |
| Bologna | ||||
| Individual at risk | 122 681 | 5476 | 127 379 | 5735 |
| Deaths | 2797 | 57 | 1979 | 36 |
| Person-years | 1 104 049.8 | 49 117.0 | 1 152 190.6 | 53 294.1 |
| MRR (95% CI) | 1 | 0.83 (0.64 to 1.08) | 1 | 0.74 (0.53 to 1.03) |
| Modena | ||||
| Individual at risk | 62 615 | 4037 | 62 847 | 3836 |
| Deaths | 1308 | 48 | 838 | 26 |
| Person-years | 585 493.6 | 34 567.7 | 595 517.3 | 34 648.3 |
| MRR (95% CI) | 1 | 1.17 (0.87 to 1.56) | 1 | 1.04 (0.70 to 1.55) |
| Reggio Emilia | ||||
| Individual at risk | 50 767 | 3069 | 50 808 | 2801 |
| Deaths | 1074 | 27 | 642 | 16 |
| Person-years | 494 782.5 | 29 019.4 | 499 821.1 | 27 371.7 |
| MRR (95% CI) | 1 | 0.70 (0.48 to 1.03) | 1 | 0.81 (0.50 to 1.33) |
| Florence | ||||
| Individual at risk | 105 350 | 1987 | 109 650 | 2030 |
| Deaths | 1791 | 12 | 1255 | 4 |
| Person-years | 799 713.1 | 14 239.6 | 830 355.5 | 14 700.9 |
| MRR (95% CI) | 1 | 0.84 (0.47 to 1.48) | 1 | 0.36 (0.14 to 0.97) |
| Leghorn | ||||
| Individual at risk | 50 257 | 589 | 50 452 | 698 |
| Deaths | 1137 | 7 | 694 | 7 |
| Person-years | 509 703.5 | 5857.9 | 512 721.1 | 7392.3 |
| MRR (95% CI) | 1 | 0.76 (0.36 to 1.59) | 1 | 1.08 (0.51 to 2.27) |
| Prato | ||||
| Individual at risk | 60 666 | 3270 | 60 826 | 3002 |
| Deaths | 1266 | 29 | 768 | 20 |
| Person-years | 597 873.3 | 29 359.7 | 602 311.4 | 27 570.9 |
| MRR (95% CI) | 1 | 0.92 (0.64 to 1.34) | 1 | 1.11 (0.71 to 1.73) |
| Rome* | ||||
| Individual at risk | 806 705 | 19 120 | 849 977 | 24 325 |
| Deaths | 16 444 | 232 | 10 833 | 191 |
| Person-years | 7 515 681.0 | 181 382.0 | 7 934 580.0 | 233 861.0 |
| MRR (95% CI) | 1 | 0.83 (0.73 to 0.94) | 1 | 0.79 (0.68 to 0.91) |
| Overall‡ | ||||
| MRR (95% CI) | 1 | 0.77 (0.65 to 0.89) | 1 | 0.79 (0.71 to 0.88) |
| P value | 0.020 | 0.472 | ||
*Follow-up from 21 October 2001 to 31 December 2012.
†Individuals with citizenship from high migratory pressure countries.
‡MRRs obtained from meta-analysis with random effects and P values from heterogeneity Χ² test.
We also evaluated differences in all-cause and cause-specific mortality between Italians and immigrants adopting an open cohort approach in Turin and Reggio Emilia, which were the two cohorts that first became open. Results of the study are reported in a paper by Pacelli et al.31 In summary, all-cause mortality was lower among immigrants than Italian residents in the two cities (MRR for men: 0.82, 95% CI 0.75 to 0.90; MRR for women: 0.71, 95% CI 0.63 to 0.81). Nonetheless, an excess mortality risk among immigrants was observed for Sub-Saharan African men and women, and for specific death causes, namely infectious diseases, some site-specific cancers and homicide.
Strengths and limitations
The IN-LiMeS is a network of metropolitan longitudinal studies pooled together to create a harmonised monitoring system. The study relies on routine data collected mostly for statistical, administrative and health planning purposes that have undergone coherence and validity checks, minimising the costs and ensuring quality of the information at the national level. The planned expansion of the information sources in order to study other outcomes through the linkage with birth certificates, pathology registers (eg, cancer registries, diabetes registries) and the emergency care information system will enhance the informative capability of the study.
The performance of record linkage between different sources of data can be considered good overall, although we noticed that the linkage rate between the population registers and the census is slightly lower among the oldest age groups. The potential bias introduced by an age-related differential linkage performance is likely to be minimal; moreover, extreme ages are usually excluded from analyses on health inequalities,3 45 unless specific hypotheses want to be tested.46
One of the main weaknesses is that most of the SES information is available from censuses and therefore only for the census closed cohorts, that is, only for the individuals resident at the census date. In the open cohorts, that is, the individuals enrolled independently of their presence at the census date, we only have information that could be retrieved from the population registers, namely educational level, civil status, citizenship, residence and/or household composition, depending on the quality and coverage of that information in the single studies. In addition, details of the socioeconomic attributes from census data date back to 2001; to overcome this limitation, acquisition and linkage with the 2011 population census are underway in most of the cohorts. Furthermore, the closed census-based cohort study is not the ideal design to study neonatal and maternal health outcomes. Indeed, because the recruitment virtually happens on a single day (eg, the census day), only few newborns can be actually enrolled and all the children in their first year of life who are present at the census day represent the survivors of the neonatal mortality. This limitation will be overcome by using an open design, which allows the enrolment of all newborns, to study maternal and infant mortality and morbidity.
To date, the network only includes cities located in the northern and central areas of the country, hindering the comparison of socioeconomic health inequalities at the national level, which have been previously shown to exist.47 Inclusion of other LMSs is a priority of the network and therefore it is in the pipeline.
Specific issues have to be acknowledged in the application of IN-LiMeS for the study of immigrants’ health. The first one is that IN-LiMeS enrolment is based on official administrative sources and only those who are officially resident and registered can be tracked and followed up. Therefore, in the studies focusing on the immigrant population, two categories of immigrants are inherently left out: people regularly present in Italy who are not formally enrolled in any population register (eg, seasonal workers) and undocumented immigrants. These two groups are roughly estimated to be around 400 000 each (0.7% of the Italian population).48 This selection bias needs to be borne in mind and results from the IN-LiMeS cannot be applied to the whole immigrant population.
Moreover, we acknowledge that closed cohorts based on the 2001 enrolment (the current available inclusive data set of the entire network) do not adequately capture the dynamics of the migration flows. Therefore, we are currently working on building open cohorts in all the participant cities in order to account for the massive growth of immigrants in the resident population that occurred in the first decade of the years 2000 and the changes in terms of sex and geographical areas of immigrants’ origin.49 In order to estimate the statistical power of the closed cohorts and its potentially achievable increase by opening the cohorts, we conducted a simulation on a subsample of the IN-LiMeS cohorts (Turin, Venice, Reggio Emilia, Florence, Rome, and pooled) (online supplementary appendix table 1). Results showed that if we were interested in estimating differences between Italian and immigrant men in all-cause mortality (incidence rate 1–4 cases/1000 person-years) with an open cohort design, the pooled cohorts would have an 80% power to detect a difference as small as 5%, with an alpha error of 0.05, while with the closed cohort the minimum detectable difference would be 9%. If we were instead interested in estimating differences in a common cause of death, such as lung cancer (ie, incidence rate 2 cases/10 000 person-years), switching between closed and open design would allow to pass from 26% to 14% in the smallest detectable effect size among the men of the pooled cohorts.
bmjopen-2017-020572supp001.pdf (73.7KB, pdf)
Other specific limitations and biases, which arise when studying immigrants’ health, have been extensively discussed elsewhere.31
In conclusion, despite its limitations, IN-LiMeS represents a powerful integrated system to monitor and document the impact of socioeconomic circumstances on people’s health, including immigrants’ health. Strategic priorities of the network are (1) the inclusion of new metropolitan cohorts in order to expand its geographical coverage, (2) the acquisition of additional information sources in order to enhance the informative capability, and (3) the implementation of an open design in all the participating cohorts in order to keep up with the changing population dynamics and to increase the statistical power of the study.
Collaboration
The IN-LiMeS is a collaborative network of metropolitan studies, and therefore we encourage Italian institutions that are interested in participating in the study to join the network. Each of the governmental institutions that currently take part in the IN-LiMeS holds all the raw data that support the findings of this study. Through their participation to the National Statistical Programme, institutions have been granted a licence for the use of the data. The data cannot be made publicly available to third parties under current rules.
Acknowledgments
The authors thank the National Institute for Health, Migration and Poverty (INMP) for the financial support of the study and for the coordination of the network. They also thank Moreno Demaria for his contribution to the study conception, data management and methods development; Delia Furio and Rossella Miglio (University of Bologna), Silvia Candela and Marco Biocca for their contribution to the background documentation and the study conception; Carlo Alberto Goldoni, Giuliano Carozzi and Paolo Pandolfi for their support in the development of the longitudinal metropolitan studies of Modena and Bologna.
Footnotes
NC and CDG contributed equally.
Contributors: NC, GiuC, TS, AB, PGR, BP, NA, AMB, CC, GiaC, CM and AP contributed to the study design and to IN-LiMeS conception. NC, LCa, AP, TS, CDG, PB and CC retrieved references for the background. BP, NZ, LCa, LG, CC, LCe, SB, GT, CDG and NC worked on data system integration, quality control and analysis. All the authors contributed to the selection of research questions and the interpretation of the results. NC and CDG drafted and edited the manuscript. AP, PGR, TS, NZ, CDG, LCa, AMB, NA, CC, LCe, SB, PB, AB, LG and BP revised major contents. All authors read and approved the final manuscript.
Funding: The study was funded by the National Institute for Health, Migration and Poverty (INMP).
Competing interests: All authors declare support from National Institute for Health, Migration and Poverty (INMP) in the form of a grant that has funded the study.
Patient consent: Detail has been removed from this case description/these case descriptions to ensure anonymity. The editors and reviewers have seen the detailed information available and are satisfied that the information backs up the case the authors are making.
Ethics approval: The record linkage procedures were performed with an anonymised individual key, complying with privacy protection rules. The IN-LiMeS is included in the Italian Statistical Program; privacy and ethical issues have been assessed by the Italian Data Protection Authority.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available. A licence for the use of the data has been granted by the National Statistical Program to the institutions participating in the Italian Network of Longitudinal Metropolitan Studies (IN-LiMeS) but restrictions apply; therefore, the data cannot be made publicly available under current rules.
Collaborators: Luisa Mondo, Paolo Carnà (Epidemiology Unit, ASL TO3, Grugliasco (TO), Italy); Moreno Demaria (Environmental Epidemiologic Unit, Regional Agency for Environmental Protection, Turin, Italy); Laura Bonvicini, Ferdinando Luberto (Epidemiology Unit, Azienda Unità Sanitaria Locale and Arcispedale Santa Maria Nuova, Istituto di Ricovero e Cura a Carattere Scientifico – IRCCS, Reggio Emilia, Italy); Giulia Cesaroni, Marina Davoli (Department of Epidemiology, Lazio Regional Health Service, Rome, Italy); and Lorenzo Simonato (Department of Molecular Medicine, University of Padova, Padova, Italy).
Contributor Information
on behalf of the IN-LiMeS Group:
Luisa Mondo, Paolo Carnà, Moreno Demaria, Laura Bonvicini, Ferdinando Luberto, Giulia Cesaroni, Marina Davoli, and Lorenzo Simonato
Collaborators: on behalf of the IN-LiMeS Group
References
- 1. WHO Commission on Social Determinants of Health. Closing the gap in a generation. Geneva, 2008. http://www.who.int/social_determinants/thecommission/finalreport/en/ (accessed 16 Apr 2018). [DOI] [PubMed] [Google Scholar]
- 2. Marmot M, Allen J, Bell R, et al. . WHO European review of social determinants of health and the health divide. Lancet 2012;380:1011–29. 10.1016/S0140-6736(12)61228-8 [DOI] [PubMed] [Google Scholar]
- 3. Stringhini S, Carmeli C, Jokela M, et al. . Socioeconomic status and the 25×25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1·7 million men and women. Lancet 2017;389:1229–37. 10.1016/S0140-6736(16)32380-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Regidor E, Vallejo F, Granados JAT, et al. . Mortality decrease according to socioeconomic groups during the economic crisis in Spain: a cohort study of 36 million people. Lancet 2016;388:2642–52. 10.1016/S0140-6736(16)30446-9 [DOI] [PubMed] [Google Scholar]
- 5. Nour S, Labonté R, Bancej C. Impact of the 2008 global financial crisis on the health of Canadians: repeated cross-sectional analysis of the Canadian Community Health Survey, 2007-2013. J Epidemiol Community Health 2017;71:336–43. 10.1136/jech-2016-207661 [DOI] [PubMed] [Google Scholar]
- 6. Castañeda H, Holmes SM, Madrigal DS, et al. . Immigration as a social determinant of health. Annu Rev Public Health 2015;36:375–92. 10.1146/annurev-publhealth-032013-182419 [DOI] [PubMed] [Google Scholar]
- 7. Cox F, Marshall A. Using the Census Longitudinal Studies for research on health and health inequalities, 2017. [Google Scholar]
- 8. Braveman PA, Cubbin C, Egerter S, et al. . Socioeconomic status in health research. JAMA 2005;294:2879 10.1001/jama.294.22.2879 [DOI] [PubMed] [Google Scholar]
- 9. Hu Y, van Lenthe FJ, Borsboom GJ, et al. . Trends in socioeconomic inequalities in self-assessed health in 17 European countries between 1990 and 2010. J Epidemiol Community Health 2016;70:644–52. 10.1136/jech-2015-206780 [DOI] [PubMed] [Google Scholar]
- 10. Hoffmann K, De Gelder R, Hu Y, et al. . Trends in educational inequalities in obesity in 15 European countries between 1990 and 2010. Int J Behav Nutr Phys Act 2017;14:63 10.1186/s12966-017-0517-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Agabiti N, Pirani M, Schifano P, et al. . Income level and chronic ambulatory care sensitive conditions in adults: a multicity population-based study in Italy. BMC Public Health 2009;9:457 10.1186/1471-2458-9-457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mackenbach JP, Bos V, Andersen O, et al. . Widening socioeconomic inequalities in mortality in six Western European countries. Int J Epidemiol 2003;32:830–7. 10.1093/ije/dyg209 [DOI] [PubMed] [Google Scholar]
- 13. Mackenbach JP, Kulhánová I, Artnik B, et al. . Changes in mortality inequalities over two decades: register based study of European countries. BMJ 2016;353:i1732 10.1136/bmj.i1732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mackenbach JP, Kulhánová I, Menvielle G, et al. . Trends in inequalities in premature mortality: a study of 3.2 million deaths in 13 European countries. J Epidemiol Community Health 2014;69:1–11. 10.1136/jech-2014-204319 [DOI] [PubMed] [Google Scholar]
- 15. Leinsalu M, Vågerö D, Kunst AE. Estonia 1989-2000: enormous increase in mortality differences by education. Int J Epidemiol 2003;32:1081–7. 10.1093/ije/dyg192 [DOI] [PubMed] [Google Scholar]
- 16. Shkolnikov VM, Andreev EM, Jasilionis D, et al. . The changing relation between education and life expectancy in central and eastern Europe in the 1990s. J Epidemiol Community Health 2006;60:875–81. 10.1136/jech.2005.044719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mackenbach JP, Stirbu I, Roskam AJ, et al. . Socioeconomic inequalities in health in 22 European countries. N Engl J Med 2008;358:2468–81. 10.1056/NEJMsa0707519 [DOI] [PubMed] [Google Scholar]
- 18. Westerling R, Gullberg A, Rosén M. Socioeconomic differences in ’avoidable' mortality in Sweden 1986-1990. Int J Epidemiol 1996;25:560–7. 10.1093/ije/25.3.560 [DOI] [PubMed] [Google Scholar]
- 19. Cavelaars AE, Kunst AE, Geurts JJ, et al. . Differences in self reported morbidity by educational level: a comparison of 11 western European countries. J Epidemiol Community Health 1998;52:219–27. 10.1136/jech.52.4.219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Marinacci C, Grippo F, Pappagallo M, et al. . Social inequalities in total and cause-specific mortality of a sample of the Italian population, from 1999 to 2007. Eur J Public Health 2013;23:582–7. 10.1093/eurpub/cks184 [DOI] [PubMed] [Google Scholar]
- 21. Cesaroni G, Badaloni C, Romano V, et al. . Socioeconomic position and health status of people who live near busy roads: the Rome Longitudinal Study (RoLS). Environ Health 2010;9:41 10.1186/1476-069X-9-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Candela S, Cavuto S, Luberto F. Condizioni socioeconomiche e mortalià nella popolazione di Reggio Emilia. Azienda USL di Reggio Emilia. 2005. http://www.epicentro.iss.it/territorio/Emilia-Romagna/pdf/CondizioniocioeconomicheMortalit%C3%A0_ReggioEmilia.pdf (accessed 16 Apr 2018). [Google Scholar]
- 23. Biggeri A, Marchi M, Dreassi E, et al. . [The Tuscany longitudinal study: mortality among selected causes in inner city of Florence and Leghorn]. Epidemiol Prev 1999;23:161–74. [PubMed] [Google Scholar]
- 24. Cardano M, Costa G, Demaria M, et al. . [Inequalities in mortality in the Italian longitudinal studies]. Epidemiol Prev 1999;23:141–52. [PubMed] [Google Scholar]
- 25. Costa G, Demaria M. [A longitudinal system of mortality surveillance according to socio-economic characteristics, as shown by population censuses: description and documentation of the system]. Epidemiol Prev 1988;10:37–47. [PubMed] [Google Scholar]
- 26. Simonato L, Canova C, Tessari R. La geografia delle malattie nel comune di Venezia. Padova: CLEUP, 2009. [Google Scholar]
- 27. Merler E, Benvenuti A, Baldi P, et al. . [Socioeconomic inequalities in health in the Tuscany Longitudinal Study (SLTO): persistence and changes over time in overall mortality and selected causes (lung cancer, liver cirrhosis, AIDS and overdose)]. Epidemiol Prev 1999;23:207–14. [PubMed] [Google Scholar]
- 28. Cacciani L, Bargagli AM, Cesaroni G, et al. . Education and mortality in the rome longitudinal study. PLoS One 2015;10:e0137576 10.1371/journal.pone.0137576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Stringhini S, Spadea T, Stroscia M, et al. . Decreasing educational differences in mortality over 40 years: evidence from the Turin Longitudinal Study (Italy). J Epidemiol Community Health 2015;69:1208–16. 10.1136/jech-2015-205673 [DOI] [PubMed] [Google Scholar]
- 30. Petrelli A, Gnavi R, Marinacci C, et al. . Socioeconomic inequalities in coronary heart disease in Italy: a multilevel population-based study. Soc Sci Med 2006;63:446–56. 10.1016/j.socscimed.2006.01.018 [DOI] [PubMed] [Google Scholar]
- 31. Pacelli B, Zengarini N, Broccoli S, et al. . Differences in mortality by immigrant status in Italy. Results of the Italian Network of Longitudinal Metropolitan Studies. Eur J Epidemiol 2016;31:691–701. 10.1007/s10654-016-0177-z [DOI] [PubMed] [Google Scholar]
- 32. Nazionale SS. Piano statistico nazionale. 2017. http://www.sistan.it/index.php?id=513 (accessed 15 Sep 2017).
- 33. Istituto Nazionale di Statistica. La revisione post-censuaria delle anagrafi: 2012-2014. Roma, 2016. [Google Scholar]
- 34. Ferre F, de Belvis AG, Valerio L, et al. . Italy: health system review. Health Syst Transit 2014;16:1–168. [PubMed] [Google Scholar]
- 35. Agabiti N, Davoli M, Fusco D, et al. . [Comparative evaluation of health services outcomes]. Epidemiol Prev 2011;35:1–80. [PubMed] [Google Scholar]
- 36. Buja A, Gini R, Visca M, et al. . Prevalence of chronic diseases by immigrant status and disparities in chronic disease management in immigrants: a population-based cohort study, Valore Project. BMC Public Health 2013;13:504 10.1186/1471-2458-13-504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Galobardes B, Shaw M, Lawlor DA, et al. . Indicators of socioeconomic position (part 1). J Epidemiol Community Health 2006;60:7–12. 10.1136/jech.2004.023531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Schizzerotto A. Classi sociali e società contemporanea. Milano: F. Angeli, 1988. [Google Scholar]
- 39. Caranci N, Biggeri A, Grisotto L, et al. . [The Italian deprivation index at census block level: definition, description and association with general mortality]. Epidemiol Prev 2010;34:167–76. [PubMed] [Google Scholar]
- 40. Brocco S, Vercellino P, Goldoni CA, et al. . [«Bridge Coding» ICD-9, ICD-10 and effects on mortality statistics]. Epidemiol Prev 2010;34:109–19. [PubMed] [Google Scholar]
- 41. Simonato L, Canova C, Corrao G, et al. . [Exploiting electronic health archives for epidemiological purpose. An experience using a standardized approach to estimate diseases in various areas of Italy]. Epidemiol Prev 2008;32:1–96. [PubMed] [Google Scholar]
- 42. Zimmerman C, Kiss L, Hossain M. Migration and health: a framework for 21st century policy-making. PLoS Med 2011;8:e1001034 10.1371/journal.pmed.1001034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Fedeli U, Ferroni E, Pigato M, et al. . Causes of mortality across different immigrant groups in Northeastern Italy. PeerJ 2015;3:e975 10.7717/peerj.975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Malmusi D, Borrell C, Benach J. Migration-related health inequalities: showing the complex interactions between gender, social class and place of origin. Soc Sci Med 2010;71:1610–9. 10.1016/j.socscimed.2010.07.043 [DOI] [PubMed] [Google Scholar]
- 45. de Gelder R, Menvielle G, Costa G, et al. . Long-term trends of inequalities in mortality in 6 European countries. Int J Public Health 2017;62:127–41. 10.1007/s00038-016-0922-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Moe JO, Steingrímsdóttir ÓA, Strand BH, et al. . Trends in educational inequalities in old age mortality in Norway 1961-2009: a prospective register based population study. BMC Public Health 2012;12:911 10.1186/1471-2458-12-911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Federico B, Mackenbach JP, Eikemo TA, et al. . Educational inequalities in mortality in northern, mid and southern Italy and the contribution of smoking. J Epidemiol Community Health 2013;67:603–9. 10.1136/jech-2012-201716 [DOI] [PubMed] [Google Scholar]
- 48. Fondazione I. Ventunesimo Rapporto sulle migrazioni 2015. Milano, 2015. [Google Scholar]
- 49. Caritas E M. XXVI Rapporto Immigrazione 2016 - Nuove generazioni a confonto. Roma, 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-020572supp001.pdf (73.7KB, pdf)