Abstract
Objective
To examine factors associated with parents’ uptake of human papillomavirus (HPV) vaccines for their children.
Design
Systematic review and meta-analysis.
Data sources
Cochrane Library, AIDSLINE, CINAHL, EMBASE, PsycINFO, Social Sciences Abstracts, Ovid MEDLINE, Scholars Portal, Social Sciences Citation Index and Dissertation Abstracts International from inception through November 2017.
Methods
We included studies that sampled parents and assessed uptake of HPV vaccines for their children (≤18 years) and/or sociodemographics, knowledge, attitudes or other factors associated with uptake. Study risk of bias was assessed using the Effective Public Health Practice Project tool. We pooled data using random-effects meta-analysis and conducted moderation analyses to examine variance in uptake by sex of child and parent.
Results
Seventy-nine studies on 840 838 parents across 15 countries were included. The pooled proportion of parents’ uptake of HPV vaccines for their children was 41.5% (range: 0.7%–92.8%), twofold higher for girls (46.5%) than for boys (20.3%). In the meta-analysis of 62 studies, physician recommendation (r=0.46 (95% CI 0.34 to 0.56)) had the greatest influence on parents’ uptake, followed by HPV vaccine safety concerns (r=−0.31 (95% CI −0.41 to −0.16)), routine child preventive check-up, past 12 months (r=0.22 (95% CI 0.11 to 0.33)) and parents’ belief in vaccines (r=0.19 (95% CI 0.08 to 0.29)). Health insurance-covered HPV vaccination (r=0.16 (95% CI 0.04 to 0.29)) and lower out-of-pocket cost (r=−0.15 (95% CI −0.22 to −0.07)) had significant effects on uptake. We found significant moderator effects for sex of child.
Conclusions
Findings indicate suboptimal levels of HPV vaccine uptake, twofold lower among boys, that may be improved by increasing physician recommendations, addressing parental safety concerns and promoting parents’ positive beliefs about vaccines, in addition to expanding insurance coverage and reducing out-of-pocket costs. Limitations of this meta-analysis include the lack of intervention studies and high risk of bias in most studies reviewed. Further studies should disaggregate HPV vaccine uptake by sex of child and parent.
Keywords: public health, social medicine, preventive medicine, hpv vaccination, systematic review
Strengths and limitations of this study.
This is the first systematic review and meta-analysis to focus on parents’ uptake of human papillomavirus (HPV) vaccines for their children, more than 10 years after initial licensure of an HPV vaccine.
Our findings provide pooled estimates of HPV vaccine uptake across 79 studies (n=840 838) conducted in 15 countries, indicating modest (41.5%) overall uptake with twofold higher uptake for girls than for boys.
The majority of studies had a high or moderate risk of bias; however, moderation analysis by risk of bias revealed no significant differences in HPV vaccine uptake.
Some meta-analyses of correlates of parents’ uptake of HPV vaccines for their children were based on relatively few studies, but we used random-effects models to compensate for clinical and methodological diversity among studies, and the majority of correlates were based on six or more primary studies.
The risk of publication bias cannot be excluded as 79 studies met the inclusion criteria, but 62 provided sufficient data for meta-analysis; however, there was no significant difference in uptake between studies included and excluded.
Introduction
Human papillomavirus (HPV) is the most prevalent sexually transmitted infection in the world. HPV infection accounts for the majority of cervical and vaginal cancers among women, and of oropharyngeal and anal cancers among men and women.1 HPV infection also accounts for nearly half of vulvar cancer among women and penile cancer among men.1 The bivalent (2vHPV) and quadrivalent HPV vaccine (4vHPV) were licensed in the USA in 2006 for girls and 4vHPV was licensed in 2009 for boys. The nine-valent HPV vaccine (9vHPV) was licensed for girls and boys in 2014. 4vHPV or 9vHPV is recommended for girls and boys age 11 years or older, and women and men through age 26 who have not previously been vaccinated, to prevent HPV infection.2
Increasing evidence supports the safety and effectiveness of HPV vaccination in reducing vaccine-type HPV infections at the population level. A meta-analysis across nine high-income countries that recommend HPV vaccination of girls indicated that in those countries with female HPV vaccination coverage of 50% or greater, vaccine-type infections decreased by 68%, with evidence suggesting cross-protection and herd effects.3 However, in countries with female HPV vaccine coverage lower than 50%, vaccine-type infections decreased by 50%, with no evidence of cross-protection or herd effects.3 According to the WHO, the HPV vaccine was on the national schedule or reimbursed in 74 countries by 2016,4 5 although coverage among girls and young women varied greatly by region—from 1.1%–1.2% in Africa and Asia, to 31.1% in Europe, to 35.6% in North America for series completion.6 While it is estimated that 9vHPV,7 along with newer HPV vaccination schedules requiring two doses,8 9 will improve health outcomes and cost-effectiveness of HPV vaccination for both men and women, accelerating uptake remains crucial to realising the public health benefits of HPV vaccination.
As the prevalence of HPV infection is highest among young people, HPV vaccination is recommended for preadolescent boys and girls, ideally prior to sexual debut.10 Accordingly, parents play a pivotal role in uptake of HPV vaccines.11 The target age group presents particular challenges for HPV vaccine uptake, including more scrutiny of HPV vaccines than traditional infant vaccines.8 Thus in addition to structural and health system issues (eg, cost, insurance coverage, delivery strategies) that contribute to low coverage of HPV vaccines globally,5 the broader context of vaccine hesitancy suggests that parents’ knowledge, attitudes and beliefs about HPV and vaccines may have a substantial influence on uptake.8 Nevertheless, limited evidence documents factors associated with parents’ uptake of HPV vaccines for their children, particularly outside North America.
Earlier research both predating and following initial introduction of HPV vaccines identified factors associated with parents’ HPV vaccine acceptability and intentions to have their children vaccinated.12 13 The decade elapsed since the first HPV vaccine was licensed, and the documented real-world challenges in the introduction and uptake of HPV vaccines globally indicate the importance of synthesising evidence on factors associated with HPV vaccine uptake.5 We build on previous descriptive reviews of HPV vaccine uptake by conducting a meta-analysis to estimate parents’ uptake of HPV vaccines for their children and factors that influence parents’ uptake. In light of emerging public health recommendations for routine HPV vaccination of boys as well as girls,2 and the substantially lower coverage in boys,14 we included boys in all analyses and assessed sex differences in uptake by child and parent.
Objectives
The purpose of this meta-analysis was to synthesise results from quantitative correlational investigations of parents’ uptake of HPV vaccines for their children. Specifically, we aimed to (1) quantify the levels of parents’ HPV vaccine uptake for their children; (2) examine factors correlated with parents’ uptake of HPV vaccines for their children; and (3) identify possible moderating influences of sex of child and parent on uptake.
Methods
We conducted a systematic search of the scientific literature and performed random-effects meta-analysis to examine factors associated with parents’ uptake of HPV vaccines for their children. We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)15 and Meta-Analysis of Observational Studies in Epidemiology (MOOSE) guidelines.16
Selection criteria
We specified eligibility criteria for the search and meta-analyses using the population, intervention (or exposure), comparison, outcome and study design (PICOS) framework. We defined the following key question to be explored: What are the factors associated with parents’ uptake of ≥1 dose of HPV vaccines for their children? We specified the population of interest as parents or guardians of children aged ≤18 years. The intervention or exposure was ≥1 dose of HPV vaccine uptake for children, with the comparator as no doses of HPV vaccine uptake.
The primary outcome of analysis was parents’ uptake of ≥1 dose of HPV vaccine for their children. The secondary outcomes were factors associated with parents’ HPV vaccine uptake for their children, including parents’ sociodemographic characteristics, HPV risk history (eg, genital warts), HPV vaccine and HPV-related disease knowledge and awareness (eg, HPV vaccine awareness), vaccine attitudes and beliefs (eg, safety concerns, perceived benefits), child preventive healthcare utilisation (eg, routine check-up), healthcare provider factors (eg, healthcare provider recommendation), and structural factors (eg, health insurance coverage of HPV vaccination).
We included randomised controlled trials (RCTs), cluster RCTs, non-RCTs, longitudinal studies, cohort studies and cross-sectional studies that explored parents’ uptake of HPV vaccines for their children. There were no language, geographical or time restrictions. Studies were excluded that did not report original data (eg, reviews, editorials) or examine parents’ uptake of HPV vaccines for their children (eg, acceptability or intention to vaccinate).
Search strategy
We conducted a comprehensive search across multiple electronic databases from inception to locate studies meeting the inclusion criteria: Cochrane Library, Cochrane Central Register of Controlled Trials, AIDSLINE, CINAHL, EMBASE, PsycINFO, Social Sciences Abstracts, Ovid MEDLINE, Scholars Portal, Social Sciences Citation Index, Dissertation Abstracts International, Applied Social Sciences Index and Abstracts, CSA Sociological Abstracts, ProQuest Research Library, CSA Social Services Abstracts, and AgeLine. The last search date was November 2017. Search terms were developed in consultation with a research librarian and chosen to draw on the broadest pool of potential studies. A sample of the search string and keywords used is listed in online supplementary file 1. We also searched for additional relevant studies by reviewing references from the included articles (ie, ‘snowballing’).
bmjopen-2017-019206supp001.pdf (100.9KB, pdf)
Data extraction
Two authors (ND and AL-D, or AL-D and PB) independently screened all titles and abstracts for inclusion. When the first reviewer determined the study might meet the inclusion criteria based on the study objectives, the full text was obtained. Two reviewers (ND and AL-D, or AL-D and PB) then independently assessed each study for inclusion based on study type and outcome measures, documenting reasons for exclusion. A consensus approach with input from the senior investigator (PAN) was used to resolve disagreements.
We developed a data extraction form using Microsoft Excel. Two of the five reviewers (ND, AL-D, PB, ST and FA) independently extracted the following data: study information (ie, year of publication, author and journal); descriptive data (ie, sample size, country and participant demographics); study aims, design and methods; outcomes/key findings; and study funding sources and reported conflicts of interest (COIs). Reviewers explored data regarding any variables examined as possible correlates of parents’ HPV vaccine uptake for their children. All members of the research team then developed a list of themes related to HPV vaccine uptake based on a review of the included studies.
Risk of bias
Reviewers independently assessed the risk of bias in individual studies using the Effective Public Health Practice Project (EPHPP) ‘Quality Assessment Tool for Quantitative Studies’.17 The EPHPP tool has been applied in numerous systematic reviews and has demonstrated inter-rater reliability for both individual domains and overall score.17 We modified the EPHPP for use with cross-sectional studies and examined selection bias (representativeness of sample, participation rate), data collection method (validity, reliability) and study design.18 Reviewers followed the EPHPP rubric to assess whether each component had low, moderate or high risk of bias, with any disagreements resolved by consensus with the senior investigator (PAN).17 For the purpose of moderation analysis, studies with low and moderate risk of bias were grouped together and compared with studies with high risk of bias. No studies were excluded on the basis of risk of bias.
We assessed each study as to whether commercial entities were declared as providing support for the work reported in the study. Additionally, we indicated potential COIs on the part of study authors, including associations with commercial entities that could be viewed as having an interest in the general area of vaccines (in the 3 years before manuscript submission), per International Committee of Medical Journal Editors guidelines.19
Data synthesis and analysis
We calculated the pooled proportion of HPV vaccine uptake using the proportion of HPV vaccine uptake reported in each included study. We then conducted meta-analysis to critically evaluate and quantitatively synthesise evidence across studies that examined similar correlates of parents’ HPV vaccine uptake for their children. Combining the results of multiple studies increases statistical power to improve estimates of effects in a larger population. We used the Comprehensive Meta-Analysis Software V.2 (Englewood, New Jersey, 2004) to calculate effect sizes for each variable, with a random-effects model to compensate for clinical and methodological diversity among studies. Random-effects models are more conservative than fixed-effect models. Rather than presuming one true effect size, in random-effects models it is assumed that the heterogeneity of studies will contribute to differences in effects between studies, and that there is a distribution of true effect sizes across similar but not identical studies.20 Random-effects models account for the fact that the studies included were conducted by different investigators in different locations at different times, rather than by the same investigator with the same population at a given time point. To derive a global estimate of the correlation of each variable with HPV vaccine uptake, we combined coefficients across studies, and present a summary effect that estimates that distribution’s mean. We calculated the Q statistic to assess homogeneity of correlations across studies and the I2 index to assess the degree of heterogeneity between studies using Higgins and Thompson’s guidelines,21 which indicate that I2 values of 25% represent low, 50% medium and 75% high heterogeneity.
Given disparities in HPV vaccine uptake for boys and girls, we assessed both sex of child and sex of parent as moderator variables in meta-analysis. Moderation analysis allows for evaluating the impact of a covariate on the outcome variable while holding other covariates constant, and helps to explain heterogeneity in effect sizes in meta-analysis.20 The Comprehensive Meta-Analysis V.2 software enables testing of categorical variables as moderators in order to compare effect sizes between two groups.
All studies that provided sufficient data regarding correlates of parents’ HPV vaccine uptake for their children were included in the meta-analysis. For studies that did not report sufficient information to enable inclusion in meta-analysis, we contacted study investigators to provide missing and unreported data. We did not conduct meta-analysis on dichotomous (intervention vs control group) data as the vast majority of studies did not evaluate interventions to increase HPV vaccine uptake. However, if an intervention was implemented as part of the study design and baseline/preintervention uptake data were provided, this uptake percentage was used in calculating the pooled proportion of parents’ HPV vaccine uptake for their children.
Patient and public involvement
No patients were involved in the development of the research question, development of outcome measures, design or conduct of this study. No patients were asked to advise on interpretation or writing up of results. There are no plans to involve patients in the dissemination of the results of this study.
Results
Study selection
The literature search yielded 1345 studies with 100% agreement among reviewers (ND, AL-D and PB) in selecting 271 relevant studies, 79 of which met the inclusion criteria. Of the relevant studies, 192 full-text articles were excluded based on the following reasons: 96 assessed intention to vaccinate rather than uptake, 69 did not focus on parents’ HPV vaccine uptake for children, 12 were not quantitative studies, 6 were reviews, 5 contained insufficient data and 4 studies were duplicates (figure 1).
Figure 1.
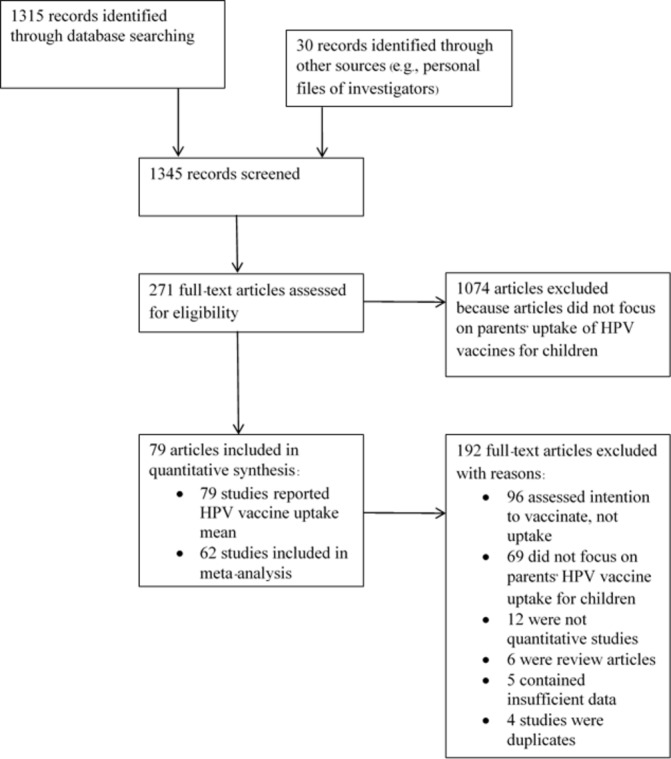
PRISMA flow chart of the searched, identified and included studies of parents’ uptake of human papillomavirus (HPV) vaccination for their children. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Study characteristics
The 79 included studies22–100 were all published in English. The majority (69.6%; n=55) were conducted in the USA,23 27 34 38–41 45 46 48–54 56–62 64 65 67–69 71–77 80–94 97–99 with four conducted in Canada (5.1%),24 28 36 37 four in the Netherlands (5.1%),26 33 35 55 two in Denmark,22 29 two in Norway,30 31 two in Puerto Rico,63 70 and one each in Austria,43 Fiji,44 Hong Kong,96 Italy,47 Kenya,66 South Africa,42 Tanzania,32 Turkey,100 United Arab Emirates95 and Vietnam.25
The majority (57.0%; n=45) of studies assessed parents’ uptake of HPV vaccines for girls only,22–26 29–39 42 44 45 48 52 56–58 61 65–68 71–73 76 77 80 81 83 85 86 88 92–96 30.4% (n=24) for both boys and girls,27 28 40 41 43 46 49–51 53 54 56 59 62 64 75 78 79 82 87 89–91 100 and 12.7% (n=10) for boys only.47 60 63 69 70 74 84 97–99
In terms of the sex of the parents/caregivers surveyed, 55.7% (n=44) of studies included mothers and fathers,23 26 30–32 35–37 40–44 46 47 51–54 57 59 61 63–65 67 69 70 72 74 76 78 81 83–85 88 91 93 94 96–98 30.4% (n=24) only mothers,22 25 29 33 39 45 49 50 55 58 62 66 68 71 73 77 79 80 87 89 90 95 99 100 and 13.9% (n=11) did not specify parent’s/caregiver’s sex.24 27 28 34 38 48 56 60 82 86 92 The majority of studies (92.4%; n=73) used HPV vaccine initiation (≥1 dose) as the primary outcome,22–24 26–43 45–54 56 57 59–82 84 85 87–100 while 7.6% (n=6) specified only three-dose series completion.25 44 55 58 83 86 Individual study aims and recruitment methods are reported in online supplementary file 2.
bmjopen-2017-019206supp002.pdf (438KB, pdf)
Pooled proportion of HPV vaccine uptake
All studies (n=79) quantified parents’ (n=840 838) uptake of HPV vaccines for their children. Table 1 lists the study characteristics and mean uptake of HPV vaccines. Most studies were cross-sectional in design, with seven longitudinal studies,26 33 40 48 52 72 98 one retrospective cohort study,29 one case–control study,32 one quasi-experimental (single-group, pre-post design) study,39 one clustered, non-randomised controlled pragmatic trial62 and one cluster randomised trial.45 Sample sizes ranged from 4345 to 254 48999 (median (M)=617.0), with 88.6% (n=70) ranging from 4345 to 865250 (M=519.5) and 11.4% (n=9) ranging from 15 04934 to 254 48999 (M=65 926).
Table 1.
Studies assessing parents’ uptake of HPV vaccines for their children, study characteristics, risk of bias and sponsorship, ordered by mean vaccine uptake (n=79)
| HPV vaccine uptake, x̅* (%) | Number of doses | Source of uptake report | Author(s), year | Sex of parent (female/male) (%) |
Parent’s age, years x̅±SD (range) | Sex of child vaccinated | HPV vaccine uptake by sex of child | Child age, years x̅ (range) | Sample size of parents† | Country | Included in meta-analysis | Risk of bias | Commercial sponsor-ship of study | COI‡ |
| 92.8 | ≥1 | Admin | Slåttelid Schreiber et al, 201522 | F: 100 | NS | F | – | 12 | 65 926† | Denmark | Y | High | N | Y |
| 89.0 | ≥1 | Parent | Perkins et al, 201023 | F: 95 M: 5 |
43.2 (31–62) | F | – | 15.0 (11–18) | 76 | USA | N | Low/Moderate | Y | N |
| 88.2 | 1 | Parent | Krawczyk et al, 201524 | NS | 40.2±6.0 (26–58) | F | – | 9–10 | 774 | Canada | Y | High | N | Y |
| 86.8 | 3 | Parent | Paul et al, 201425 | F: 100 | NS | F | – | 11 | 536 | Vietnam | Y | High | N | N |
| 82.0 | ≥1 | Parent | Alberts et al, 201726 | F: 88 M: 12 |
M=45 | F | – | 13 | 1309 | The Netherlands |
Y | Low | N | Y |
| 82.0 | ≥1 | Parent | Brown et al, 201727 | NS | NS | F, M | F: 71.4 M: 88.6 |
M=12 (10–17) | 200 | USA | N | High | N | N |
| 81.9 | ≥1 | Admin | McClure et al, 201528 | NS | N/S | F, M | F: 84.9 M: 79.0 |
11–12 | 1440† | Canada | Y | High | N | N |
| 80.0 | 1 | Admin | Widgren et al, 201129 | F: 100 | NS | F | – | NS | 33 838† | Denmark | Y | Low/Moderate | NS | NS |
| 78.3 | ≥1 | Admin | Feiring et al, 201530 | F: NS M: NS |
NS | F | – | 12 | 84 319† | Norway | Y | High | N | N |
| 78.2 | 1 | Admin | Hansen et al, 201531 | F: NS M: NS |
NS | F | – | 12–13 | 90 842† | Norway | Y | High | N | Y |
| 74.3§ | ≥1 | Parent | Watson-Jones et al, 201232 | F: 78.0 M: 22.0 |
38.2 | F | – |
M=13 (IQR 13–15) |
404 | Tanzania | Y | Low/Moderate | N | Y |
| 73.0 | ≥1 | Admin | Pot et al, 201733 | F: 100 | 44±4.3 | F | – | 12–18 | 8026 | The Netherlands |
Y | High | NS | N |
| 66.7 | ≥1 | Parent | Hofstetter et al, 201434 | NS | NS | F | – | 15.6 (11–19) | 15 049 | USA | Y | High | Y | Y |
| 66.0 | ≥1 | Parent | Gefenaite et al, 201235 | F: NS M: NS |
44 (35–55) | F | – | 13–16 | 469 | The Netherlands |
Y | High | N | N |
| 65.1 | ≥1 | Parent | Ogilvie et al, 201036 | F: 84.9 M: 14.9 |
Mo: 40–49 | F | – | 11 | 2025 | Canada | Y | Low/Moderate | N | Y |
| 65.0 | ≥1 | Parent | Buchan et al, 201137 | F: 84.6 M: 15.4 |
NS | F | – | 13 | 208 | Canada | N | High | NS | NS |
| 64.0 | ≥1 | Parent | Staras et al, 201438 | NS | NS | F | – | 9–19 | 2422 | USA | Y | High | N | N |
| 61.0 | ≥1 | Parent | Morales-Campos and Parra-Medina, 201739 | F: 100 | 38±7.8 | F | – | 11–17 | 317 | USA | Y | High | N | N |
| 60.0 | ≥1 | Parent | VanWormer et al, 201740 | F: 83 M: 17 |
43.7±6.1 | F, M | F: 62 M: 58 |
11–17 | 221 | USA | Y | High | N | N |
| 59.0¶ | ≥1 | Parent | Rand et al, 201141 | F: 81.0 M: 19.0 |
≤40: 37% >41: 63% |
F, M | NS | 11–17 | 430 | USA | Y | High | N | Y |
| 58.6 | ≥1 | Admin | Botha et al, 201442 | F: NS M: NS |
NS | F | – | 9–12 | 3465 | South Africa | N | High | Y** | N |
| 58.6 | 1 | Parent | Borena et al, 201643 | F: 90 M: 9.6 |
40.8±5.7 | F, M | F: 59.0 M: 51.8 |
9 | 449 | Austria | Y | High | NS | N |
| 58.0 | 3 | Parent | La Vincente et al, 201544 | F: 80.2 M: 13.3 NS: 4.8 |
M=40 (IQR 36–43) |
F | – | 9–12 | 293 | Fiji | N | High | N | Y |
| 56.0 | ≥1 | Parent | Winer et al, 201645 | F: 100 | 41±10 | F | – | 9–12 | 43 | USA | N | Low | N | N |
| 54.8 | 1 | Admin | Fu et al, 201746 | F: 93.5 M: 6.5 |
37.9±7.7 | F, M | NS | 10–12 | 400 | USA | Y | High | N | Y |
| 53.7 | ≥1 | Parent | Bianco et al, 201447 | F: NS M: NS |
42.9 (NS) | M | – | 12–18 | 566 | Italy | N | High | NS | N |
| 50.9 | ≥1 | Parent | Cuff et al, 201648 | NS | NS | F | – | 11–12 | 908 | USA | Y | High | N | N |
| 50.0 | ≥1 | Parent | Donahue et al, 201549 | F: 100 | NS | F, M | F: 60.3 M: 39.7 |
9–13 | 2185 | USA | Y | High | N | Y |
| 49.9 | 1 | Parent | Dorell et al, 201050 | F: 100 | Mo: ≥45 | F, M | NS | 15 (13–17) | 8652 | USA | Y | High | N | N |
| 49.0 | ≥1 | Parent | Moss et al, 201651 | F: 76.8 M: 16.7 |
Mo: ≥45 | F, M | – | 13–17 | 9021 | USA | Y | High | N | Y |
| 48.0 | ≥1 | Parent | Nonzee et al, 201852 | F: 96.3 M: 3.7 |
Mo: 40–49 | F | – | 13–17 | 1779 | USA | Y | High | N | N |
| 47.3 | ≥1 | Parent | Gilkey et al, 201753 | F: 56 M: 44 |
NS | F, M | NS | 11–17 | 1484 | USA | Y | High | Y | Y |
| 47.0 | ≥1 | Parent | Gerend et al, 200954 | F: 95.0 M: 5 |
36.0±9.0 | F, M | NS | <18 | 82 | USA | Y | High | NS | NS |
| 45.0 | 3 | Parent | van Keulen et al, 201355 | F: 100 | 43.4±4.6 | F | – | 13–14 | 952 | The Netherlands |
N | Low/Moderate | N | N |
| 45.0 | ≥1 | Admin | Johnson et al, 201756 | NS | NS | F, M | F: 57.0 M: 33.0 |
13–17 | 18 264† | USA | Y | High | N | N |
| 42.0 | 1 | Parent | Reiter et al, 201157 | F: 94 M: 6 |
Mo: 40+ | F | – | 11–20 | 647 | USA | Y | High | N | Y |
| 41.0 | 3 | Admin | Chao et al, 200958 | F: 100 | 42.1±6.4 | F | – | 9–17 | 18 275 | USA | Y | Low/Moderate | NS | NS |
| 36.3 | ≥1 | Parent | Kepka et al, 201559 | F: 89.6 M: 10.4 |
42.9±7.8 (29–67) | F, M | F: 49.1 M: 23.4 |
11–17 | 67 | USA | Y | High | N | N |
| 34.6 | ≥1 | Parent | Lu et al, 201560 | NS | NS | M | – | 13–17 | 9554 | USA | Y | High | N | N |
| 33.1 | ≥1 | Parent | Reynolds, 201461 | F: 94.7 M: 5.3 |
43.8 (24–65) | F | – | 9–18 | 323 | USA | N | High | NS | N |
| 32.9 | 1 | Admin | Sanderson et al, 201762 | F: 100 | Mo: 30–39 | F, M | NS | 9–18 | 408† | USA | Y | Low | N | N |
| 31.7 | ≥1 | Parent | Colón-López et al, 201563 | F: 91.7 M: 8.3 |
38.6±7.2 | M | – | 9–17 | 60 | Puerto Rico†† | N | High | N | NS |
| 31.7 | ≥1 | Parent | Kepka et al, 201564 | F: 84.4 M: 15.7 |
Mo: 40–49 | F, M | F: 42.6 M: 20.7 |
11–17 | 118 | USA | Y | High | N | N |
| 31.3 | ≥1 | Parent | Reiter et al, 201065 | F: 94 M: 6 |
Mo: 40–49 | F | – | 10–17 | 617 | USA | Y | High | N | N |
| 31.1 | ≥1 | Parent | Vermandere et al, 201466 | F: 100 | M=35 (IQR 32–40) | F | – | 8–18 | 256 | Kenya | Y | High | Y** | N |
| 31.0 | ≥1 | Parent | Cates et al, 201067 | F: 81.5 M: 18.5 |
NS | F | – | 10–17 | 696 | USA | Y | High | N | NS |
| 31.0 | 1 | Parent | Kadis et al, 201168 | F: 100 | Mo: 40–49 | F | – | 11–14 | 496 | USA | N | Low/Moderate | N | Y |
| 30.0 | ≥1 | Parent | Perkins et al, 201369 | F: 80.0 M: 20.0 |
43.5±8.3 | M | – | 11–17 | 120 | USA | Y | High | Y | N |
| 29.3 | ≥1 | Parent | Colón-López et al, 201670 | F: 88.5 M: 11.5 |
37.7±7.2 | M | – | 9–17 | 200 | Puerto Rico†† | Y | High | N | NS |
| 29.0 | ≥1 | Parent | Taylor et al, 201471 | F: 100 | Mo: ≥45 | F | – | 9–17 | 86 | USA | Y | High | N | NS |
| 28.9 | ≥1 | Admin | Fishman et al, 201672 | F: 90.5 M: 9.5 |
41.7±9.2 (23–71) |
F | – | 13–18 | 149 | USA | Y | High | N | N |
| 28.3 | 1 | Parent | Price, 201373 | F: 100 | NS | F | – | 9–18 | 106 | USA | Y | High | N | NS |
| 28.0 | ≥1 | Parent | Rickert et al, 201474 | F: 85.9 M: 14.1 |
41.6 | M | – | 11–15 | 249 | USA | Y | High | Y | Y |
| 27.7 | ≥1 | Parent | Fuchs et al, 201675 | F: 100 | Mo: 30–39 | F, M | NS | 9–17 | 350 | USA | N | High | N | N |
| 27.0‡‡ | ≥1 | Parent | Brewer et al, 201176 | F: 94.3 M: 5.7 |
Mo: <40 | F | – | 10–18 | 567 | USA | Y | High | N | Y |
| 26.0 | ≥1 | Parent | Rosenthal et al, 200877 | F: 100 | 41 (27–77) | F | – | 11–17 | 153 | USA | Y | Low/Moderate | Y | NS |
| 25.8 | ≥1 | Parent | McRee et al, 201778 | F: 67.8 M: 32.2 |
Mo: 40–49 | F, M | NS | 11–17 | 2156 | USA | Y | High | N | Y |
| 25.6 | ≥1 | Parent | Lee et al, 201679 | F: 100 | 44.6±7.6 | F, M | F: 32.6 M: 18.6 |
12–17 | 130 | USA | Y | High | N | N |
| 24.0 | ≥1 | Parent | Hertweck et al, 201380 | F: 100 | 44 | F | – | 13–17 | 68 | USA | Y | Low/Moderate | Y | NS |
| 23.1 | 1 | Parent | Guerry et al, 201181 | F: 89.7 M: 10.3 |
41.7±7.4 (22–71) |
F | – | 11–18 | 503 | USA | Y | Low/Moderate | N | Y |
| 22.5 | 1 | Parent | Wong et al, 201182 | NS | NS | F, M | NS | 9–17 | 2205 | USA | Y | High | N | N |
| 22.0 | 3 | Parent | Clark et al, 201683 | F: 56.7 M: 43.3 |
Mo: 24–44 | F | – | 11–17 | 786 | USA | Y | High | N | N |
| 21.4 | ≥1 | Parent | Taylor et al, 201484 | F: 51.5 M: 48.5 |
42.2±11.5 | M | – | 11–17 | 758 | USA | Y | High | Y | Y |
| 19.4 | ≥1 | Parent | Tiro et al, 201285 | F: 54.6 M: 45.4 |
Mo: 40–49 | F | – | 12–17 | 3615 | USA | Y | Low/Moderate | N | N |
| 19.0 | 3 | Parent | Allen et al, 201086 | NS | NS | F | – | 9–17 | 451 | USA | Y | Low/Moderate | N | N |
| 17.0 | ≥1 | Parent | Berenson et al, 201787 | F: 100 | Mo: 30–39 | F, M | F: 20 M: 11 |
9–17 | 1497 | USA | Y | High | N | N |
| 16.5 | ≥1 | Parent | Thompson et al, 201288 | F: 68.2 M: 30.8 |
40.0±8.3 | F | – | 9–17 | 200 | USA | Y | High | N | Y |
| 15.8 | ≥1 | Parent | Gross et al, 201589 | F: 100 | Mo: 30–39 | F, M | F: 21.8 M: 9.8 |
9–17 | 1372 | USA | N | High | N | N |
| 14.9 | ≥1 | Parent | Berenson et al, 201490 | F: 100 | Mo: 30–39 | F, M | F: 19.5 M: 10.3 |
9–17 | 1256 | USA | Y | High | N | N |
| 13.0 | ≥1 | Parent | Horn et al, 201091 | F: 88.6 M: 11.4 |
Mo: 30–39 | F, M | NS | 9–17 | 325 | USA | N | Low/Moderate | NS | NS |
| 13.0 | ≥1 | Parent | Saak, 201192 | NS | NS | F | – | 12–17 | 649 | USA | Y | High | NS | NS |
| 12.0 | ≥1 | Parent | Reiter et al, 200993 | F: 93.9 M: 6.1 |
Mo: ≥40 | F | – | 10–18 | 886 | USA | Y | Low/Moderate | N | Y |
| 10.3† | ≥1 | Parent | Gottlieb et al, 200994 | F: 89.7 M: 10.3 |
41 (IQR 36–45) | F | – | 11–18 | 886 | USA | Y | High | N | Y |
| 9.8 | 1 | Parent | Ortashi et al, 201495 | F: 100% | 32.4±8.2 | F | – | NS | 640 | United Arab Emirates | N | High | NS | NS |
| 9.8 | ≥1 | Parent | Wang et al, 201796 | F: 74.4 M: 25.6 |
47.7±5.5 | F | – | 12–17 | 988 | Hong Kong | Y | Low | N | N |
| 4.2§§ | ≥1 | Admin | Cates et al, 201497 | F: NS M: NS |
NS | M | – | 9–13 | 176 590† | USA | N | High | N | Y |
| 2.0 | 1 | Parent | Reiter et al, 201398 | F: 52 M: 48 |
Mo: <45 | M | – | 11–17 | 228 | USA | Y | Low/Moderate | Y | Y |
| 1.6 | ≥1 | Admin | Hechter et al, 201399 | F: 100 | NS | M | – | 9–17 | 254 489† | USA | Y | High | N | NS |
| 0.7 | ≥1 | Parent | Kose et al, 2014100 | F: 100 | 32.0±6.5 | F, M | NS | 0–18 | 779 | Turkey | N | High | NS | NS |
*Mean uptake percentage presented for HPV vaccine initiation (≥1 dose), except for six studies that only reported three-dose completion.
†Sample size refers to the number of parents, unless indicated by †, in cases where the data are drawn from administrative databases and refer to the number of children.
‡COI based on the International Committee of Medical Journal Editors guidelines.19
§Overall mean calculated on uptake across cases and controls.
¶Overall mean calculated on uptake across children’s ages.
**Study vaccine reported as donated by pharmaceutical company.
††An unincorporated territory of the USA, but does not have equal access to all rights and privileges of citizenship. Although officially classified as a high-income country, it has similar health infrastructure deficits and other socioeconomic conditions more typical of some low-income and middle-income countries.
‡‡Longitudinal study, used follow-up mean uptake score.
§§Used preintervention uptake score.
Admin, administrative records; COI, conflict of interest; F, female; HPV, human papillomavirus; M, male; M, median; Mo, mode; N, no; NS, not stated; Parent, parent report; x̅, mean; Y, yes.
The pooled proportion of parents’ uptake of HPV vaccines for their children ranged from 0.7%100 to 92.8%22 across studies, with overall mean uptake of 41.5% (SD=24.2). The pooled proportion of uptake of HPV vaccines for girls (46.5%) was significantly greater than uptake for girls and boys combined (39.8%) and uptake for boys (20.3%; F(2, 76)=4.92, P=0.010). The average uptake of HPV vaccines among six low-income and middle-income countries25 32 42 44 66 100 was 51.6% compared with 40.6% in 73 high-income countries22–24 26–31 33–41 43 45–65 67–99; however, this difference failed to achieve statistical significance (F(1, 77)=1.13, P=0.292). Comparison of uptake of HPV vaccines between studies with sample sizes ranging from 43 to 9554 (x̅=39.8%) and those ranging from 15 049 to 254 489 (x̅=54.2%) revealed a non-significant trend of studies with sample sizes of ≥15 000 reporting higher uptake than studies with sample sizes <15 000 (F(1, 77)=2.89, P=0.095).
Study quality
We assessed risk of bias for all studies: the majority (75.9%; n=60) had a high risk of bias,22 24 25 27 28 30 31 33–35 37–44 46–54 56 57 59–61 63–67 69–76 78 79 82–84 87–90 92 94 95 97 99 100 19.0% (n=15) low/moderate risk of bias23 29 32 36 55 58 68 77 80 81 85 86 91 93 98 and 5.1% (n=4) low risk of bias.26 45 62 96 No significant difference in parents’ uptake of HPV vaccines for their children was identified between studies with low/moderate risk of bias (x̅=41.3%) and studies with high risk of bias (x̅=41.5%; F(1, 77)=0.002, P=0.967).
Funding and COI
Overall, 11 studies (13.9%) declared funding from commercial entities (all pharmaceutical companies),23 34 42 53 66 69 74 77 80 84 98 56 (70.9%) declared funding not including commercial entities,22 24–28 30–32 35 36 38–41 44–46 48–52 55–57 59 60 62–65 67 68 70–73 75 76 78 79 81–83 85–90 93 94 96 97 99 and 12 (15.2%) did not specify funding.29 33 37 43 47 54 58 61 91 92 95 100 Twenty-five studies (31.6%)22 24 26 31 32 34 36 41 44 46 49 51 53 57 68 74 76 78 81 84 88 93 94 97 98 declared or were assessed (ie, if author/coauthor declared a COI in another study included in the review within the stipulated time frame) as having a potential COI, 38 (48.1%) declared no COI,23 25 27 28 30 33 35 38–40 42 43 45 47 48 50 52 55 56 59–62 64–66 69 72 75 79 82 83 85–87 89 90 96 and 16 (20.3%) did not specify COI.29 37 54 58 63 67 70 71 73 77 80 91 92 95 99 100 We found no significant difference in uptake of HPV vaccines between studies that declared any funding from commercial entities (x̅=38.5%) versus studies that did not declare any commercial funding (x̅=42.2%; F(1, 77)=0.19, P=0.668). Similarly, there was no statistically significant difference in HPV vaccine uptake between studies with a potential COI (x̅=44.6%) versus those with no COI (x̅=44.5%; F(1, 77)=0.62, P=0.435).
Correlates of parents’ uptake of HPV vaccines for children
Sixty-two original studies22 24–26 28–36 38–41 43 45 46 48–54 56–59 62 64–67 69–74 76–88 90 92–94 96 98 99 (n=654 100) measured similar correlates of parents’ uptake of HPV vaccines for their children and were included in the meta-analysis (as indicated in table 1). An examination of the pooled proportion of HPV vaccine uptake found no statistically significant difference between studies included in the meta-analysis (n=62; x̅=42.0% uptake) and those not included due to insufficient data (n=17; x̅=39.6% uptake). Based on the available data, we examined correlations between HPV vaccine uptake and 19 factors, organised thematically in eight domains. Table 2 indicates the weighted mean correlational effect sizes (r) measuring associations with HPV vaccine uptake, 95% CI, the Q test of homogeneity and I2 index of between-study variability.
Table 2.
Meta-analysis of correlates of parents’ HPV vaccine uptake for their children (n=62 studies; sample size=654 100)
| Domain | Factor | Studies (n) | Random-effect size (95% CI) | Homogeneity index, Q | Between-study variability, I2 |
| Healthcare provider-related | Physician recommendation | 2140 43 * 46 49–51 54 56 66 70 73 81 83 84 86 90 93 94 97 98 | 0.46 (0.34 to 0.56), P<0.000 | 690.356, P<0.000 | 97.103 |
| Parents’ trust in healthcare provider | 423 46 86 88 | 0.11 (0.01 to 0.21), P=0.026 | 3.975, P=0.264 | 24.528 | |
| Parental HPV vaccine decision-maker | Mother as HPV vaccine decision-maker (vs both parents) | 290 * | 0.34 (0.23 to 0.44), P<0.001 | 0.05, P=0.83 | 0.000 |
| Parents’ vaccine attitudes, beliefs and intentions | Intention to vaccinate child for HPV | 423 26 33 96 | 0.31 (0.17 to 0.43), P<0.000 | 41.288, P<0.000 | 92.734 |
| HPV vaccine safety concerns | 1224 38 40 41 46 48 54 64 74 86 93 98 | −0.23 (−0.35 to 0.11), P<0.000 | 254.017, P<0.000 | 95.670 | |
| Belief in vaccines in general | 1424 32 35 36 38 46 49 54 57 65 69 73 74 86 | 0.19 (0.08 to 0.29), P=0.001 | 337.048, P<0.001 | 96.143 | |
| Perceived HPV vaccine benefits | 1024 38 46 54 73 74 81 86 93 98 | 0.17 (0.10 to 0.24), P<0.000 | 78.43, P<0.000 | 88.525 | |
| Anticipatory regret if child not vaccinated | 224 98 | 0.14 (0.11 to 0.17), P<0.000 | 0.11 (0.74) | 0.000 | |
| Preventive healthcare utilisation for child | Routine childhood preventive check-up, past 12 months | 849 56 57 60 65 71 82 98 | 0.22 (0.11 to 0.33), P<0.001 | 61.472, P<0.000 | 88.613 |
| Health insurance/cost | Health insurance coverage of HPV vaccination | 1052 56 57 63 65 82 88 93 94 98 | 0.16 (0.04 to 0.29), P=0.011 | 49.642, P<0.001 | 81.870 |
| Out-of-pocket cost for HPV vaccination | 359 82 98 | −0.15 (−0.22 to 0.07), P<0.000 | 1.013, P=0.603 | 0.000 | |
| Parents’ HPV risk history | Parent history of HPV | 343 * 87 | 0.16 (0.06 to 0.25), P=0.002 | 0.737, P=0.692 | 0.000 |
| Parent history of receiving a Pap smear | 335 58 99 | 0.06 (0.004 to 0.107), P=0.036 | 65.712, P<0.000 | 95.435 | |
| Parent history of genital warts | 358 88 99 | 0.05 (0.03 to 0.07), P<0.001 | 0.79, P=0.67 | 0.000 | |
| Parent or family history of abnormal Pap smear | 458 87 88 99 | 0.02 (0.01 to 0.04), P=0.012 | 4.191, P=0.242 | 28.425 | |
| Parents’ HPV knowledge and awareness | HPV vaccine knowledge/awareness | 925 39 54 72 73 81 82 86 87 | 0.14 (0.05 to 0.23), P=0.002 | 65.889, P<0.000 | 87.858 |
| Cervical cancer/HPV knowledge | 1424 25 35 38 39 43 * 54 66 69 73 79 87 88 | 0.04 (0.04 to 0.13), P=0.001 | 58.999, P<0.000 | 77.966 | |
| Sociodemographics | Urban/rural | 641 57 60 66 94 98 | 0.10 (0.06 to 0.14), P<0.000 | 2.110, P=0.834 | 0.000 |
| Child age | 1523 41 52 54 56 57 60 65 66 70 71 73 81 86 94 | 0.07 (0.01 to 0.13), P=0.029 | 127.178, P<0.001 | 88.206 |
*Reported outcomes for two different subsamples.
HPV, human papillomavirus.
Factors positively associated with parents’ uptake of HPV vaccines for their children were identified in the following domains: (1) healthcare provider—physician recommendation (r=0.46 (95% CI 0.34 to 0.56)) and parents’ trust in healthcare providers (r=0.11 (95% CI 0.01 to 0.21)); (2) parental HPV vaccine decision-maker—mother as HPV vaccine decision-maker (vs both parents) (r=0.34 (95% CI 0.23 to 0.44)); (3) parent’s vaccine beliefs, attitudes and intentions—intention to vaccinate child for HPV (r=0.31 (95% CI 0.17 to 0.43)), belief in vaccines in general (r=0.19 (95% CI 0.08 to 0.29)), perceived HPV vaccine benefits (r=0.17 (95% CI 0.10 to 0.24)) and anticipatory regret if child is not vaccinated (r=0.14 (95% CI 0.11 to 0.17)); (4) preventive healthcare utilisation for child—routine child preventive check-up, past 12 months (r=0.22 (95% CI 0.11 to 0.33)); (5) insurance/cost—health insurance coverage of HPV vaccination (r=0.16 (95% CI 0.04 to 0.29)); (6) parents’ HPV risk history—parent history of HPV (r=0.16 (95% CI 0.06 to 0.25)), mother’s history of having a Pap test (r=0.06 (95% CI 0.004 to 0.107)), parent history of genital warts (r=0.05 (95% CI 0.03 to 0.07)), parent or family member history of abnormal Pap smear (r=0.02 (95% CI 0.01 to 0.04)); (7) parents’ HPV-related knowledge and awareness—HPV vaccine knowledge and awareness (r=0.14 (95% CI 0.05 to 0.23)) and cervical cancer/HPV knowledge (r=0.04 (95% CI 0.04 to 0.13)); and (8) sociodemographic factors—urban versus rural location (r=0.10 (95% CI 0.06 to 0.14)) and child’s age (r=0.07 (95% CI 0.01 to 0.13)). Factors negatively associated with parents’ uptake of HPV vaccines for their children were parents’ vaccine attitudes—HPV vaccine safety concerns (r=−0.31 (95% CI −0.41 to −0.16)); and insurance/cost—out-of-pocket cost (r=−0.15 (95% CI −0.22 to −0.07)).
Between-study variability
The small number of studies examining some of the factors precluded us from conducting subanalyses to assess the impact of risk of bias on the findings for those outcomes; therefore, we examined individual results to identify potential reasons for between-study variability. We found high heterogeneity in the reported correlations between parents’ HPV vaccine uptake for their children and the following factors: physician recommendation, intention to vaccinate child for HPV, HPV vaccine safety concerns, belief in vaccines in general, perceived HPV vaccine benefits, routine child preventive check-up, health insurance coverage of HPV vaccination, mother’s history of receiving a Pap test, HPV vaccine knowledge and awareness, and child age. We found medium heterogeneity in cervical cancer/HPV knowledge, and low heterogeneity in parents’ trust in healthcare provider, mother as HPV vaccine decision-maker (vs both parents), anticipatory regret, out-of-pocket cost for HPV vaccination, parent history of HPV, parent history of genital warts, parent or family history of abnormal Pap smear, and urban versus rural location.
Moderating factors of parents’ uptake of HPV vaccines for children
We conducted moderation analyses to examine whether the variance in HPV vaccine uptake could be explained by three covariates—sex of child, sex of parent and study risk of bias—after adjusting for other factors (eg, physician recommendation, health insurance coverage, HPV vaccine safety concerns and others). We found that the omnibus test for the effect of sex of parent on uptake of HPV vaccines yielded Q=10.41, df=2 (P=0.006); thus, controlling for sex of child and risk of bias, there is some evidence that effect size for parents’ uptake of HPV vaccines for their children may be related to the sex of the parent. More specifically, mothers/female guardians had a coefficient of −0.018, suggesting that uptake may be greater in studies that included mothers/female guardians as opposed to studies that included both mothers/female guardians and fathers/male guardians, controlling for sex of child and risk of bias. However, this model was not statistically significant (P=0.653).
The omnibus test for the effect of sex of child indicated Q=10.37, df=3 (P=0.016); therefore, controlling for sex of parent and risk of bias, there is some evidence that effect size for parents’ uptake of HPV vaccines for their children is related to the sex of the child. More specifically, we found a significant effect for preadolescent and adolescent girls and HPV vaccine uptake. The coefficient for girls of 0.096 (P=0.036) indicates that parents’ uptake of HPV vaccines for their children is greater in studies that included preadolescent and adolescent girls, as opposed to studies that included both preadolescent and adolescent girls and boys, controlling for sex of parent and risk of bias.
We found no significant moderating effect of study risk of bias on HPV vaccine uptake. The proportion of variance in uptake that is explained by all three covariates is 28%. The results of the various sensitivity analyses and examination of a funnel plot of the 62 studies included in the meta-analysis showed no publication bias (Begg and Mazumdar rank correlation, P=0.945).
Discussion
This systematic review and meta-analysis is among the first to assess correlates of parents’ HPV vaccine uptake for their children, rather than proxies such as HPV vaccine acceptability or intention to vaccinate. Results from 79 studies in 15 countries including over 840 000 parents indicate overall suboptimal parental uptake (41.5%) of one or more doses of HPV vaccines for their children. Notably, parents’ HPV vaccine uptake differed significantly by sex of the child: uptake for girls (46.5%) and in mixed samples of girls and boys (39.8%) was higher than uptake for boys (20.3%), indicating substantial sex disparities in uptake.
Parents’ overall modest levels of HPV vaccine uptake for their children more than a decade after the initial licensure of an HPV vaccine indicate the importance of synthesising evidence to support effective programmes to accelerate uptake. The disparities in uptake by sex of child are consistent with the later approval and recommendation of HPV vaccination for boys than girls in the USA, where the majority of studies were conducted, and the lack of coverage of HPV vaccination for boys in many other national insurance programmes.101 However, our findings also suggest a number of enduring factors that may contribute to sex disparities in HPV vaccine uptake. A predominant policy focus in many national public health strategies and funding mechanisms on increasing HPV vaccine coverage among girls and young women in order to achieve herd protection may contribute to a lack of perceived benefits of HPV vaccination for men on the part of parents, healthcare providers and boys/young men themselves101 102—despite the documented effectiveness and substantial health benefits of HPV vaccination for boys.9 36
In line with previous descriptive reviews largely focused on uptake for girls,12 103 physician recommendation had the single greatest effect on parents’ uptake of HPV vaccines for their children, supported by evidence from over 20 studies. As the first meta-analysis of HPV vaccine uptake, to our knowledge, to test for the moderating influence of child’s sex—and based on previous studies that suggest a tendency on the part of healthcare providers to offer HPV vaccine recommendations to those they perceive to be more likely to benefit from and to accept vaccination (ie, girls, patients with health insurance)104—this highlights the importance of physicians making recommendations for boys as well as girls in order to increase parents’ HPV vaccine uptake for their children.103 105 The vital role of physician recommendation of HPV vaccination for boys is further supported by the significant association (with evidence from 10 studies) of parents’ perceived HPV vaccine benefits with their uptake of HPV vaccines for their children, in the context of the enduring perception that HPV is a woman’s concern.102
Results from meta-analyses indicate a substantial negative effect of parents’ concerns about HPV vaccine safety on HPV vaccine uptake for their children, as well as positive effects of belief in vaccines in general and perceived HPV vaccine benefits; each of these factors is supported by findings from 10 or more studies. These parental attitudes and beliefs about vaccines in general, and HPV vaccines in particular, may be strategic targets for both physician engagement with parents and for public health education campaigns in accelerating HPV vaccine uptake. Nevertheless, the broader phenomenon of vaccine hesitancy, evidenced in the USA106 and other countries,8 has resulted in parental resistance to childhood vaccinations, with a subsequent re-emergence of vaccine-preventable diseases in the USA.106 In the context of even greater scrutiny that may be applied to an adolescent vaccine for a sexually transmitted infection,8 the significant effects of parents’ attitudes and beliefs support the importance of careful and respectful healthcare provider engagement with parents and their concerns as a facilitator of HPV vaccine uptake.105 107 The positive impact of parents’ trust in healthcare providers on their uptake of HPV vaccines for their children, as similarly identified in regard to childhood vaccines,108 provides evidence to support the importance of the process of physician engagement in effectively communicating with parents.105 107 109 Findings from this review suggest a substantive focus on addressing parents’ HPV vaccine safety concerns and supporting their positive beliefs in the health benefits of vaccines in general, as well as explaining the particular benefits of HPV vaccines for their children, including boys and girls.
Routine child preventive check-up was identified across eight studies as being positively associated with parents’ HPV vaccine uptake for their children. It may be that the public health focus on routine gynaecological cancer screening in preventive care for women, with no analogously effective screening mechanism available for anal or oropharyngeal cancer among men, may thereby contribute to sex disparities in HPV vaccine uptake. This supports the importance of reducing missed opportunities in encounters with healthcare providers to promote HPV vaccine uptake for boys.103
Beyond healthcare provider-related factors and parents’ attitudes and beliefs about vaccines, the significant impact of health insurance coverage of HPV vaccination and out-of-pocket cost on parents’ uptake of HPV vaccines for their children supports the important role of healthcare policy and funding in promoting HPV vaccine uptake.11 101 We also identified a small but significant effect of urban versus rural location on HPV vaccine uptake. These correlates of uptake underscore the importance of structural interventions, such as the US Vaccines for Children programme which provides vaccines at no cost to low-income children, and school-based HPV vaccine delivery programmes, such as in Australia (including boys and girls), which have helped to reduce disparities in uptake by children’s race/ethnicity, sex and socioeconomic status.110 They also suggest addressing rurality as a sociodemographic factor that may contribute to disparities in HPV vaccine uptake.
Methodological considerations
Several methodological issues pose limitations to this review, including the dearth of intervention studies, high risk of bias in the majority of studies reviewed and heterogeneity due to between-study variability. Some variables were meta-analysed across relatively few studies precluding subanalyses of moderator variables, or meta-regression, to assess the impact of risk of bias on the findings. However, we used random-effects models to account for methodological variability, assessed each study for risk of bias, assessed risk of bias as a moderator and calculated accepted statistical indices to assess heterogeneity, in accordance with PRISMA15 and MOOSE guidelines.16 Additionally, 10 of the 19 factors in meta-analyses were supported by findings from at least six or more studies, with six factors supported by findings from 10 or more studies.
An additional limitation is that the vast majority of studies focused on mothers, with very few studies assessing fathers’ HPV vaccine uptake for their children,90 98 and several failing to indicate the sex of the parent surveyed. Future studies should examine fathers’ uptake of HPV vaccines for their children, with parents’ uptake disaggregated by sex, and assess whether fathers’ support for HPV vaccination of their daughters and/or sons differs from that of mothers. Similarly, while nearly all studies reported ages of the children vaccinated, over a quarter did not report parents’ age(s) and many studies failed to include basic descriptive statistics on parents’ age (ie, mean or median, range). As many studies did not identify the type of physician who recommended HPV vaccination, future investigations should specify physician and healthcare provider type to assess differences among providers and specific practice implications. Understandably, some of the missing demographic data may be a result of limitations in national and regional immunisation registries; augmenting the information collected in these databases may provide further evidence to inform tailored interventions to increase parents’ HPV vaccine uptake for their children.
Finally, parents’ uptake of HPV vaccines for their children may be affected by a reduction in the required number of doses to achieve full protection, as well as broad structural and social factors, including high-income versus low-income countries, public funding of HPV vaccination for girls and for boys, school-based versus clinic-based vaccination, HPV prevalence, and cultural differences. As we used HPV vaccine initiation as the primary outcome based on data reported in more than 90% of the studies reviewed, the same factors are likely to be associated with initiation of a two-dose regimen; the latter may help to mitigate to an extent the negative effects of out-of-pocket costs and perhaps parents’ safety concerns on uptake. We compared uptake in high-income versus low-income and middle-income countries; however, the paucity of studies in the latter context, including demonstration projects that may overestimate broader population uptake, may have limited statistical power to detect differences, and we were unable to systematically model other social-structural factors in this meta-analysis. Nevertheless, the significant effects of health insurance coverage and out-of-pocket cost on parents’ uptake of HPV vaccines for their children indicate the impact of national policies and funding mechanisms in the USA—where 9vHPV is now largely a standard of care for insurance companies—and other countries (with only 6% including HPV vaccines for boys in national immunisation programmes vs 37% for girls only).9 It is also crucial to expand investigations in low-income and middle-income countries, with the highest morbidity due to HPV-related cancers and the lowest access to and uptake of HPV vaccines.8
This systematic review and meta-analysis indicates overall suboptimal parental uptake of HPV vaccines for their children across 79 studies conducted in 15 countries, along with significant correlates of uptake at the level of healthcare providers, parental attitudes, beliefs and knowledge, and structural factors such as insurance coverage and out-of-pocket cost. Given the vital role of parents in HPV vaccine uptake for their children, public health strategies should address modifiable factors across multilevel domains that influence parents’ uptake. In particular, a focus on increasing provider, especially family physician,74 recommendation of HPV vaccines to parents of boys as well as girls, including during routine healthcare visits, may reduce sex disparities in HPV vaccine uptake and contribute to accelerating uptake overall.14 Further research including intervention studies and longitudinal designs, with results disaggregated by sex of children and parents, and by HPV vaccine initiation versus series (now two-dose) completion, is needed to advance evidence of factors associated with parents’ uptake of HPV vaccines for their children. Evidence-informed strategies that contribute to accelerating HPV vaccine uptake are critical to realising the full public health potential of HPV vaccines on cancer prevention.
Supplementary Material
Acknowledgments
We would like to thank Jenaya Webb, MA, MI, Public Services Librarian at the Ontario Institute for Studies in Education, University of Toronto, for her assistance with developing and conducting the electronic searches.
Footnotes
CHL, AL-D and PB contributed equally.
Contributors: PAN had full access to all of the data in the study and takes full responsibility for the integrity of the data and the accuracy of the data analysis. PAN conceptualised and designed the study, contributed to data analysis and interpretation, drafted the initial and final manuscript, provided funding support, and supervised study implementation. CHL contributed to study conceptualisation and design, led and supervised statistical analysis, and critically reviewed the manuscript. AL-D led article screening, data extraction and assessment of risk of bias, contributed to data analysis and drafting the manuscript, and provided administrative support. PB contributed to article screening, data extraction, risk of bias assessment, statistical analysis and revision of the manuscript. ST, CR, ND and FA contributed to article screening, data extraction and risk of bias assessment, and reviewed the manuscript.
Funding: This work was supported in part by the Canadian Institutes of Health Research (THA-118570), the Canada Research Chairs Program (Canada Research Chair in Health and Social Justice) and the Canada Foundation for Innovation.
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: There are no additional data available.
References
- 1. Saraiya M, Unger ER, Thompson TD, et al. US assessment of HPV types in cancers: implications for current and 9-valent HPV vaccines. JNCI: Journal of the National Cancer Institute 2015;107:djv086 10.1093/jnci/djv086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Petrosky E, Bocchini JA, Jr, Hariri S, et al. Use of 9-valent human papillomavirus (HPV) vaccine: updated HPV vaccination recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep 2015;64:300–4. [PMC free article] [PubMed] [Google Scholar]
- 3. Drolet M, Bénard Élodie, Boily M-C, et al. Population-level impact and herd effects following human papillomavirus vaccination programmes: a systematic review and meta-analysis. Lancet Infect Dis 2015;15:565–80. 10.1016/S1473-3099(14)71073-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. WHO. Immunization Coverage. Fact Sheet. 2016. http://www.who.int/mediacentre/factsheets/fs378/en/ (accessed 5 Jan 2018).
- 5. Brotherton JML, Zuber PLF, Bloem PJN. Primary prevention of HPV through vaccination: update on the current global status. Curr Obstet Gynecol Rep 2016;5:210–24. 10.1007/s13669-016-0165-z [DOI] [Google Scholar]
- 6. Bruni L, Diaz M, Barrionuevo-Rosas L, et al. Global estimates of human papillomavirus vaccination coverage by region and income level: a pooled analysis. Lancet Glob Health 2016;4:e453–63. 10.1016/S2214-109X(16)30099-7 [DOI] [PubMed] [Google Scholar]
- 7. Chesson HW, Markowitz LE, Hariri S, et al. The impact and cost-effectiveness of nonavalent HPV vaccination in the United States: estimates from a simplified transmission model. Hum Vaccin Immunother 2016;12:1363–72. 10.1080/21645515.2016.1140288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bloem P, Ogbuanu I. Vaccination to prevent human papillomavirus infections: from promise to practice. PLoS Med 2017;14:e1002325 10.1371/journal.pmed.1002325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. WHO. Human papillomavirus vaccines: WHO position paper, May 2017. Wkly Epidemiol Rec 2017;92:241–68. [PubMed] [Google Scholar]
- 10. Zimet GD. Improving adolescent health: focus on HPV vaccine acceptance. J Adolesc Health 2005;37:S17–S23. 10.1016/j.jadohealth.2005.09.010 [DOI] [PubMed] [Google Scholar]
- 11. McRee A-L, Reiter PL, Brewer NT. Vaccinating adolescent girls against human papillomavirus—Who decides? Prev Med 2010;50:213–4. 10.1016/j.ypmed.2010.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hendry M, Lewis R, Clements A, et al. “HPV? Never heard of it!”: A systematic review of girls’ and parents’ information needs, views and preferences about human papillomavirus vaccination. Vaccine 2013;31:5152–67. 10.1016/j.vaccine.2013.08.091 [DOI] [PubMed] [Google Scholar]
- 13. Trim K, Nagji N, Elit L, et al. Parental knowledge, attitudes, and behaviours towards human papillomavirus vaccination for their children: a systematic review from 2001 to 2011. Obstet Gynecol Int 2012;2012:1–12. 10.1155/2012/921236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Daniel-Ulloa J, Gilbert PA, Parker EA. Human papillomavirus vaccination in the United States: Uneven Uptake by gender, race/ethnicity, and sexual orientation. Am J Public Health 2016;106:746–7. 10.2105/AJPH.2015.303039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analysis: the PRISMA statement. PLoS Med 2009;6:e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. JAMA 2000;283:2008–12. [DOI] [PubMed] [Google Scholar]
- 17. National Collaborating Centre for Methods and Tools. Quality assessment tool for quantitative studies. 2012. http://www.nccmt.ca/registry/view/eng/14.html (accessed 5 Jan 2018).
- 18. Deeks JJ, Dinnes J, D’Amico R, et al. Evaluating non-randomised intervention studies. Health Technol Assess 2003;7:1–173. 10.3310/hta7270 [DOI] [PubMed] [Google Scholar]
- 19. International Committee of Medical Journal Editors (ICMJE). Conflicts of Interest. 2018. http://www.icmje.org/conflicts-of-interest/ (accessed 5 Jan 2018).
- 20. Borenstein M, Hedges LV, Higgins JPT, et al. Regression in Meta-analysis. 2015. https://www.meta-analysis.com/downloads/MRManual.pdf (accessed 5 Jan 2018).
- 21. Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58. 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 22. Slåttelid Schreiber SM, Juul KE, Dehlendorff C, et al. Socioeconomic predictors of human papillomavirus vaccination among girls in the Danish childhood immunization program. J Adolesc Health 2015;56:402–7. 10.1016/j.jadohealth.2014.12.008 [DOI] [PubMed] [Google Scholar]
- 23. Perkins RB, Pierre-Joseph N, Marquez C, et al. Why do low-income minority parents choose human papillomavirus vaccination for their daughters? J Pediatr 2010;157:617–22. 10.1016/j.jpeds.2010.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Krawczyk A, Knäuper B, Gilca V, et al. Parents’ decision-making about the human papillomavirus vaccine for their daughters: I. quantitative results. Hum Vaccin Immunother 2015;11:322–9. 10.1080/21645515.2014.1004030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Paul P, Tanner AE, Gravitt PE, et al. Acceptability of HPV vaccine implementation among parents in India. Health Care Women Int 2014;35:1148–61. 10.1080/07399332.2012.740115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Alberts CJ, van der Loeff MFS, Hazeveld Y, et al. A longitudinal study on determinants of HPV vaccination uptake in parents/guardians from different ethnic backgrounds in Amsterdam, the Netherlands. BMC Public Health 2017;17:220 10.1186/s12889-017-4091-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Brown B, Gabra MI, Pellman H. Reasons for acceptance or refusal of Human Papillomavirus Vaccine in a California pediatric practice. Papillomavirus Res 2017;3:42–5. 10.1016/j.pvr.2017.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. McClure CA, MacSwain M-A, Morrison H, et al. Human papillomavirus vaccine uptake in boys and girls in a school-based vaccine delivery program in Prince Edward Island, Canada. Vaccine 2015;33:1786–90. 10.1016/j.vaccine.2015.02.047 [DOI] [PubMed] [Google Scholar]
- 29. Widgren K, Simonsen J, Valentiner-Branth P, et al. Uptake of the human papillomavirus-vaccination within the free-of-charge childhood vaccination programme in Denmark. Vaccine 2011;29:9663–7. 10.1016/j.vaccine.2011.10.021 [DOI] [PubMed] [Google Scholar]
- 30. Feiring B, Laake I, Molden T, et al. Do parental education and income matter? A nationwide register-based study on HPV vaccine uptake in the school-based immunisation programme in Norway. BMJ Open 2015;5:e006422 10.1136/bmjopen-2014-006422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hansen BT, Campbell S, Burger E, et al. Correlates of HPV vaccine uptake in school-based routine vaccination of preadolescent girls in Norway: A register-based study of 90,000 girls and their parents. Prev Med 2015;77:4–10. 10.1016/j.ypmed.2015.04.024 [DOI] [PubMed] [Google Scholar]
- 32. Watson-Jones D, Tomlin K, Remes P, et al. Reasons for receiving or not receiving HPV vaccination in primary schoolgirls in Tanzania: a case control study. PLoS One 2012;7:e45231 10.1371/journal.pone.0045231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Pot M, van Keulen HM, Ruiter RAC, et al. Motivational and contextual determinants of HPV-vaccination uptake: a longitudinal study among mothers of girls invited for the HPV-vaccination. Prev Med 2017;100:41–9. 10.1016/j.ypmed.2017.04.005 [DOI] [PubMed] [Google Scholar]
- 34. Hofstetter AM, Stockwell MS, Al-Husayni N, et al. HPV vaccination: are we initiating too late? Vaccine 2014;32:1939–45. 10.1016/j.vaccine.2014.01.084 [DOI] [PubMed] [Google Scholar]
- 35. Gefenaite G, Smit M, Nijman HW, et al. Comparatively low attendance during Human Papillomavirus catch-up vaccination among teenage girls in the Netherlands: insights from a behavioral survey among parents. BMC Public Health 2012;12:498 10.1186/1471-2458-12-498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ogilvie G, Anderson M, Marra F, et al. A population-based evaluation of a publicly funded, school-based HPV vaccine program in British Columbia, Canada: parental factors associated with HPV vaccine receipt. PLoS Med 2010;7:e1000270 10.1371/journal.pmed.1000270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Buchan A, Sergi M. Factors influencing parental decisions about HPV immunization for their Grade 8 daughters in the Kingston, Frontenac and Lennox & Addington Area. Can J Public Health 2011;102:476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Staras SAS, Vadaparampil ST, Patel RP, et al. Parent perceptions important for HPV vaccine initiation among low income adolescent girls. Vaccine 2014;32:6163–9. 10.1016/j.vaccine.2014.08.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Morales-Campos DY, Parra-Medina D. Predictors of human papillomavirus vaccine initiation and completion among Latino mothers of 11- to 17-year-old daughters living along the Texas-Mexico border. Fam Community Health 2017;40:139–49. 10.1097/FCH.0000000000000144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. VanWormer JJ, Bendixsen CG, Vickers ER, et al. Association between parent attitudes and receipt of human papillomavirus vaccine in adolescents. BMC Public Health 2017;17:766 10.1186/s12889-017-4787-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Rand CM, Schaffer SJ, Humiston SG, et al. Patient-provider communication and human papillomavirus vaccine acceptance. Clin Pediatr 2011;50:106–13. 10.1177/0009922810379907 [DOI] [PubMed] [Google Scholar]
- 42. Botha MH, Van der Merwe FH, Snyman LC, et al. The Vaccine and Cervical Cancer Screen (VACCS) project: acceptance of human papillomavirus vaccination in a school-based programme in two provinces of South Africa. S Afr Med J 2014;105:40 10.7196/SAMJ.8419 [DOI] [PubMed] [Google Scholar]
- 43. Borena W, Luckner-Hornischer A, Katzgraber F, et al. Factors affecting HPV vaccine acceptance in west Austria: do we need to revise the current immunization scheme? Papillomavirus Res 2016;2:173–7. 10.1016/j.pvr.2016.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. La Vincente SF, Mielnik D, Jenkins K, et al. Implementation of a national school-based Human Papillomavirus (HPV) vaccine campaign in Fiji: knowledge, vaccine acceptability and information needs of parents. BMC Public Health 2015;15:1257 10.1186/s12889-015-2579-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Winer RL, Gonzales AA, Noonan CJ, et al. A cluster-randomized trial to evaluate a mother-daughter dyadic educational intervention for increasing HPV vaccination coverage in American Indian girls. J Community Health 2016;41:274–81. 10.1007/s10900-015-0093-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Fu LY, Zimet GD, Latkin CA, et al. Associations of trust and healthcare provider advice with HPV vaccine acceptance among African American parents. Vaccine 2017;35:802–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Bianco A, Pileggi C, Iozzo F, et al. Vaccination against human papilloma virus infection in male adolescents: knowledge, attitudes, and acceptability among parents in Italy. Hum Vaccin Immunother 2014;10:2536–42. 10.4161/21645515.2014.969614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Cuff RD, Buchanan T, Pelkofski E, et al. Rates of human papillomavirus vaccine uptake amongst girls five years after introduction of statewide mandate in Virginia. Am J Obstet Gynecol 2016;214:752.e1–6. 10.1016/j.ajog.2016.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Donahue KL, Hendrix KS, Sturm LA, et al. Human papillomavirus vaccine initiation among 9–13-year-olds in the United States. Prev Med Rep 2015;2:892–8. 10.1016/j.pmedr.2015.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Dorell C, Yankey D, Kennedy A, et al. Factors that influence parental vaccination decisions for adolescents, 13 to 17 years old: National Immunization Survey-Teen, 2010. Clinical Pediatr 2013;52:162–70. [DOI] [PubMed] [Google Scholar]
- 51. Moss JL, Reiter PL, Rimer BK, et al. Collaborative patient-provider communication and uptake of adolescent vaccines. Soc Sci Med 2016;159:100–7. 10.1016/j.socscimed.2016.04.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Nonzee NJ, Baldwin SB, Cui Y, et al. Disparities in parental human papillomavirus (HPV) vaccine awareness and uptake among adolescents. Vaccine 2018;36:1243–7. 10.1016/j.vaccine.2017.08.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Gilkey MB, Calo WA, Marciniak MW, et al. Parents who refuse or delay HPV vaccine: differences in vaccination behavior, beliefs, and clinical communication preferences. Hum Vaccin Immunother 2017;13:680–6. 10.1080/21645515.2016.1247134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Gerend MA, Weibley E, Bland H. Parental response to human papillomavirus vaccine availability: uptake and intentions. J Adolesc Health 2009;45:528–31. 10.1016/j.jadohealth.2009.02.006 [DOI] [PubMed] [Google Scholar]
- 55. van Keulen HM, Otten W, Ruiter RAC, et al. Determinants of HPV vaccination intentions among Dutch girls and their mothers: a cross-sectional study. BMC Public Health 2013;13:111 10.1186/1471-2458-13-111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Johnson KL, Lin M-Y, Cabral H, et al. Variation in human papillomavirus vaccine uptake and acceptability between female and male adolescents and their caregivers. J Community Health 2017;42:522–32. 10.1007/s10900-016-0284-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Reiter PL, McRee A-L, Gottlieb SL, et al. Correlates of receiving recommended adolescent vaccines among adolescent females in North Carolina. Hum Vaccin 2011;7:67–73. 10.4161/hv.7.1.13500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Chao C, Slezak JM, Coleman KJ, et al. Papanicolaou screening behavior in mothers and human papillomavirus vaccine uptake in adolescent girls. Am J Public Health 2009;99:1137–42. 10.2105/AJPH.2008.147876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Kepka D, Warner EL, Kinney AY, et al. Low human papillomavirus (HPV) vaccine knowledge among Latino parents in Utah. J Immigr Minor Health 2015;17:125–31. 10.1007/s10903-014-0003-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Lu PJ, Yankey D, Jeyarajah J, et al. HPV vaccination coverage of male adolescents in the United States. Pediatr 2015;136:839–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Reynolds D. Religiosity and parental acceptance of human papillomavirus (HPV) vaccine in 9–18 year-old girls. J Christ Nurs 2014;31:172–7. 10.1097/CNJ.0000000000000076 [DOI] [PubMed] [Google Scholar]
- 62. Sanderson M, Canedo JR, Khabele D, et al. Pragmatic trial of an intervention to increase human papillomavirus vaccination in safety-net clinics. BMC Public Health 2017;17:158 10.1186/s12889-017-4094-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Colón-López V, Quiñones V, Del Toro-Mejías LM, et al. HPV awareness and vaccine willingness among Dominican immigrant parents attending a federal qualified health clinic in Puerto Rico. J Immigr Minor Health 2015;17:1086–90. 10.1007/s10903-014-0067-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Kepka D, Ding Q, Bodson J, et al. Latino parents’ awareness and receipt of the HPV vaccine for sons and daughters in a state with low three-dose completion. J Cancer Educ 2015;30:808–12. 10.1007/s13187-014-0781-0 [DOI] [PubMed] [Google Scholar]
- 65. Reiter PL, Cates JR, McRee A-L, et al. Statewide HPV vaccine initiation among adolescent females in North Carolina. Sex Transm Dis 2010;37:549–56. 10.1097/OLQ.0b013e3181d73bf8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Vermandere H, Naanyu V, Mabeya H, et al. Determinants of acceptance and subsequent uptake of the HPV vaccine in a cohort in Eldoret, Kenya. PLoS One 2014;9:e109353 10.1371/journal.pone.0109353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Cates JR, Shafer A, Carpentier FD, et al. How parents hear about human papillomavirus vaccine: implications for uptake. J Adolesc Health 2010;47:305–8. 10.1016/j.jadohealth.2010.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Kadis JA, McRee A-L, Gottlieb SL, et al. Mothers’ support for voluntary provision of HPV vaccine in schools. Vaccine 2011;29:2542–7. 10.1016/j.vaccine.2011.01.067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Perkins RB, Apte G, Marquez C, et al. Factors affecting human papillomavirus vaccine use among White, Black and Latino parents of Sons. Pediatr Infect Dis J 2013;32:e38–e44. 10.1097/INF.0b013e31826f53e3 [DOI] [PubMed] [Google Scholar]
- 70. Colón-López V, Toro-Mejías LMD, Conde-Toro A, et al. Views on HPV and HPV Vaccination: the experience at a federal qualified clinic in Puerto Rico. J Health Care Poor Underserved 2016;27:1411–26. 10.1353/hpu.2016.0126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Taylor VM, Burke NJ, Ko LK, et al. Understanding HPV vaccine uptake among Cambodian American girls. J Community Health 2014;39:857–62. 10.1007/s10900-014-9844-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Fishman J, Taylor L, Frank I. Awareness of HPV and uptake of vaccination in a high-risk population. Pediatrics 2016;138:e20152048 10.1542/peds.2015-2048 [DOI] [PubMed] [Google Scholar]
- 73. Price K. A preliminary study of mothers' social support, spirituality, knowledge, and acceptability of the HPV vaccine for daughters: University of Cincinnati [Thesis], 2013. [Google Scholar]
- 74. Rickert VI, Auslander BA, Cox DS, et al. School-based vaccination of young US males: impact of health beliefs on intent and first dose acceptance. Vaccine 2014;32:1982–7. 10.1016/j.vaccine.2014.01.049 [DOI] [PubMed] [Google Scholar]
- 75. Fuchs EL, Rahman M, Berenson AB. Examining maternal beliefs and human papillomavirus vaccine uptake among male and female children in low-income families. Papillomavirus Res 2016;2:38–40. 10.1016/j.pvr.2016.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Brewer NT, Gottlieb SL, Reiter PL, et al. Longitudinal predictors of human papillomavirus vaccine initiation among adolescent girls in a high-risk geographic area. Sex Transm Dis 2011;38:197–204. 10.1097/OLQ.0b013e3181f12dbf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Rosenthal SL, Rupp R, Zimet GD, et al. Uptake of HPV vaccine: demographics, sexual history and values, parenting style, and vaccine attitudes. J Adolesc Health 2008;43:239–45. 10.1016/j.jadohealth.2008.06.009 [DOI] [PubMed] [Google Scholar]
- 78. McRee A-L, Maslow GR, Reiter PL. Receipt of recommended adolescent vaccines among youth with special health care needs. Clin Pediatr 2017;56:451–60. 10.1177/0009922816661330 [DOI] [PubMed] [Google Scholar]
- 79. Lee H, Kim M, Kiang P, et al. Factors associated with HPV vaccination among Cambodian American teenagers. Public Health Nurs 2016;33:493–501. 10.1111/phn.12294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Hertweck SP, LaJoie AS, Pinto MD, et al. Health care decision making by mothers for their adolescent daughters regarding the quadrivalent HPV vaccine. J Pediatr Adolesc Gynecol 2013;26:96–101. 10.1016/j.jpag.2012.10.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Guerry SL, De Rosa CJ, Markowitz LE, et al. Human papillomavirus vaccine initiation among adolescent girls in high-risk communities. Vaccine 2011;29:2235–41. 10.1016/j.vaccine.2011.01.052 [DOI] [PubMed] [Google Scholar]
- 82. Wong CA, Berkowitz Z, Dorell CG, et al. Human papillomavirus vaccine uptake among 9- to 17-year-old girls: National Health Interview Survey, 2008. Cancer 2011;117:5612–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Clark SJ, Cowan AE, Filipp SL, et al. Parent perception of provider interactions influences HPV vaccination status of adolescent females. Clin Pediatr 2016;55:701–6. 10.1177/0009922815610629 [DOI] [PubMed] [Google Scholar]
- 84. Taylor JL, Zimet GD, Donahue KL, et al. Vaccinating sons against HPV: results from a U.S. National survey of parents. PLoS One 2014;9:e115154 10.1371/journal.pone.0115154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Tiro JA, Tsui J, Bauer HM, et al. Human papillomavirus vaccine use among adolescent girls and young adult women: an analysis of the 2007 California Health Interview Survey. J Womens Health 2012;21:656–65. 10.1089/jwh.2011.3284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Allen JD, Othus MKD, Shelton RC, et al. Parental decision making about the HPV vaccine. Cancer Epidemiol Biomarkers Prev 2010;19:2187–98. 10.1158/1055-9965.EPI-10-0217 [DOI] [PubMed] [Google Scholar]
- 87. Berenson AB, Brown VG, Fuchs EL, et al. Relationship between maternal experiences and adolescent HPV vaccination. Hum Vaccin Immunother 2017;13:2150–4. 10.1080/21645515.2017.1332551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Thompson VLS, Arnold LD, Notaro SR. African American parents' attitudes toward HPV vaccination. Ethn Dis 2012;21:335–41. [PMC free article] [PubMed] [Google Scholar]
- 89. Gross TT, Laz TH, Rahman M, et al. Association between mother-child sexual communication and HPV vaccine uptake. Prev Med 2015;74:63–6. 10.1016/j.ypmed.2015.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Berenson AB, Laz TH, Hirth JM, et al. Effect of the decision-making process in the family on HPV vaccination rates among adolescents 9–17 years of age. Hum Vaccin Immunother 2014;10:1807–11. 10.4161/hv.28779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Horn L, Howard C, Waller J, et al. Opinions of parents about school-entry mandates for the human papillomavirus vaccine. J Low Genit Tract Dis 2010;14:43–8. 10.1097/LGT.0b013e3181b0fad4 [DOI] [PubMed] [Google Scholar]
- 92. Saak B. Factors associated with parental decisions to vaccinate girls against human papillomavirus. California State University, Long Beach [Dissertation] 2011;45:1504531. [Google Scholar]
- 93. Reiter PL, Brewer NT, Gottlieb SL, et al. Parents' health beliefs and HPV vaccination of their adolescent daughters. Soc Sci Med 2009;69:475–80. 10.1016/j.socscimed.2009.05.024 [DOI] [PubMed] [Google Scholar]
- 94. Gottlieb SL, Brewer NT, Sternberg MR, et al. Human papillomavirus vaccine initiation in an area with elevated rates of cervical cancer. J Adolesc Health 2009;45:430–7. 10.1016/j.jadohealth.2009.03.029 [DOI] [PubMed] [Google Scholar]
- 95. Ortashi O, Raheel H, Shalal M. Acceptability of human papilloma virus vaccination among women in the United Arab Emirates. Asian Pac J Cancer Prev 2014;15:2007–11. 10.7314/APJCP.2014.15.5.2007 [DOI] [PubMed] [Google Scholar]
- 96. Wang LD-L, Lam WWT, Fielding R. Determinants of human papillomavirus vaccination uptake among adolescent girls: A theory-based longitudinal study among Hong Kong Chinese parents. Prev Med 2017;102:24–30. 10.1016/j.ypmed.2017.06.021 [DOI] [PubMed] [Google Scholar]
- 97. Cates JR, Diehl SJ, Crandell JL, et al. Intervention effects from a social marketing campaign to promote HPV vaccination in preteen boys. Vaccine 2014;32:4171–8. 10.1016/j.vaccine.2014.05.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Reiter PL, McRee A-L, Pepper JK, et al. Longitudinal predictors of human papillomavirus vaccination among a national sample of adolescent males. Am J Public Health 2013;103:1419–27. 10.2105/AJPH.2012.301189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Hechter RC, Chao C, Sy LS, et al. Quadrivalent human papillomavirus vaccine uptake in adolescent boys and maternal utilization of preventive care and history of sexually transmitted infections. Am J Public Health 2013;103:e63–e68. 10.2105/AJPH.2013.301495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Kose D, Erkorkmaz U, Cinar N, et al. Mothers' knowledge and attitudes about HPV vaccination to prevent cervical cancers. Asian Pac J Cancer Prev 2014;15:7263–6. 10.7314/APJCP.2014.15.17.7263 [DOI] [PubMed] [Google Scholar]
- 101. Newman PA, Lacombe-Duncan A. Human papillomavirus vaccination for men: advancing policy and practice. Future Virol 2014;9:1033–47. 10.2217/fvl.14.91 [DOI] [Google Scholar]
- 102. Newman PA, Logie CH, Doukas N, et al. HPV vaccine acceptability among men: a systematic review and meta-analysis. Sex Transm Infect 2013;89:568–74. 10.1136/sextrans-2012-050980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Holman DM, Benard V, Roland KB, et al. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr 2014;168:76–82. 10.1001/jamapediatrics.2013.2752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Gerend MA, Shepherd MA, Lustria ML, et al. Predictors of provider recommendation for HPV vaccine among young adult men and women: findings from a cross-sectional survey. Sex Transm Infect 2016;92:104–7. 10.1136/sextrans-2015-052088 [DOI] [PubMed] [Google Scholar]
- 105. Gilkey MB, McRee AL. Provider communication about HPV vaccination: a systematic review. Hum Vaccin Immunother 2016;12:1454–68. 10.1080/21645515.2015.1129090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Phadke VK, Bednarczyk RA, Salmon DA, et al. Association between vaccine refusal and vaccine-preventable diseases in the United States: a review of measles and pertussis. JAMA 2016;315:1149–58. 10.1001/jama.2016.1353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Politi MC, Jones KM, Philpott SE. The role of patient engagement in addressing parents' perceptions about immunizations. JAMA 2017;318:237–8. 10.1001/jama.2017.7168 [DOI] [PubMed] [Google Scholar]
- 108. Benin AL, Wisler-Scher DJ, Colson E, et al. Qualitative analysis of mothers' decision-making about vaccines for infants: the importance of trust. Pediatrics 2006;117:1532–41. 10.1542/peds.2005-1728 [DOI] [PubMed] [Google Scholar]
- 109. Lacombe-Duncan A, Newman PA, Baiden P. Human papillomavirus vaccine acceptability and decision-making among adolescent boys and parents: A meta-ethnography of qualitative studies. Vaccine 2018. doi: 10.1016/j.vaccine.2018.02.079 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 110. Walker AT, Smith PJ, Kolasa M; Centers for Disease Control and Prevention (CDC). Reduction of racial/ethnic disparities in vaccination coverage, 1995-2011. MMWR Suppl 2014;63:7–12. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-019206supp001.pdf (100.9KB, pdf)
bmjopen-2017-019206supp002.pdf (438KB, pdf)


