Abstract
Background:
The impact of different transportation noise sources and noise environments on arterial stiffness remains unknown.
Objectives:
We evaluated the association between residential outdoor exposure to annual average road, railway, and aircraft noise levels, total noise intermittency (IR), and total number of noise events (NE) and brachial-ankle pulse wave velocity (baPWV) following a cross-sectional design.
Methods:
We measured baPWV (meters/second) in 2,775 participants (49–81 y old) at the second follow-up (2010–2011) of the Swiss Cohort Study on Air Pollution and Lung and Heart Diseases in Adults (SAPALDIA). We assigned annual average road, railway, and aircraft noise levels (), total day- and nighttime and (, none or constant noise; , high fluctuation) at the most exposed façade using 2011 Swiss noise models. We applied multivariable linear mixed regression models to analyze associations.
Results:
Medians [interquartile ranges (IQRs)] were (3.1) m/s; (8.0) dB; (8.1) dB; (99.7% exposed): 54.2 (10.6) dB; (179); (870); (27); and (40.3). We observed a 0.87% (95% CI: 0.31, 1.43%) increase in baPWV per IQR of , which was greater with or with daytime sleepiness. We observed a nonsignificant positive association between and baPWV in urban areas and a negative tendency in rural areas. , but not , was associated with baPWV. Associations were independent of the other noise sources and air pollution.
Conclusions:
Long-term exposure to railway noise, particularly in an intermittent nighttime noise environment, and to nighttime noise events, mainly related to road noise, may affect arterial stiffness, a major determinant of cardiovascular disease. Ascertaining noise exposure characteristics beyond average noise levels may be relevant to better understand noise-related health effects. https://doi.org/10.1289/EHP1136
Introduction
There is substantial epidemiological evidence relating long-term exposure to transportation noise with cardiovascular disease (CVD) (Babisch 2014; Vienneau et al. 2015), which is the leading cause of morbidity and mortality worldwide (Lozano et al. 2012; Murray et al. 2012). It is proposed that noise affects CVD through stress reactions that repeatedly trigger the autonomic nervous and endocrine systems (Babisch 2002), particularly during resting periods and while sleeping. This is supported by field and experimental sleep studies that have observed increases in stress hormones, specifically catecholamines (Babisch 2003; Schmidt et al. 2013), as well as in blood pressure, heart rate and endothelial dysfunction (Basner et al. 2011; Schmidt et al. 2013), and little habituation of the cardiac arousals under repeated nighttime noise exposure (Basner et al. 2011). Noise-induced stress and sleep disturbances could also increase cortisol levels, disrupt the circadian rhythm, and promote oxidative stress and inflammation (Münzel et al. 2016; Recio et al. 2016). Long-term noise exposure could therefore lead to chronic homeostatic changes and contribute to vascular damage, diabetes, obesity, and hypertension, which could contribute to CVD (Babisch 2002). However, although there is increasing evidence for the association of noise with hypertension (van Kempen and Babisch 2012), little is known about the impact of noise on relevant cardiovascular end points such as arterial stiffness, a major risk factor and a strong independent predictor of future CVD and mortality (Zieman et al. 2005).
The potential involvement of arterial stiffness was suggested by an experimental study, which observed acute nighttime aircraft noise effects on endothelial dysfunction (Schmidt et al. 2013). Two recent epidemiological studies also observed associations between residential outdoor exposure to annual average road noise levels, commonly used as a long-term exposure indicator, and isolated high systolic blood pressure (Babisch et al. 2014a; Foraster et al. 2014), which indicates loss of arterial elasticity (Franklin et al. 1997) and translates into increased pulse pressure, an indirect marker of arterial stiffness (Zieman et al. 2005). However, to our knowledge, no epidemiological study has assessed the impact of noise on direct markers of arterial stiffness. Recent technological advancements provide the opportunity to use reliable new arterial stiffness measures in clinical practice and in large samples (Vlachopoulos et al. 2012, 2015). Brachial-ankle pulse wave velocity (baPWV) is a valid, noninvasive, easy to use, and reproducible oscillometric measure of both peripheral and central arterial stiffness (Endes et al. 2015).
Transportation noise sources (from road, railway, and aircraft) are the most prevalent environmental noise exposures in the European population (European Environment Agency 2014) but are rarely studied together (Méline et al. 2015). Most epidemiological studies have focused on long-term exposure to either outdoor road or aircraft noise levels at home, as shown in meta-analyses (Babisch 2014; Vienneau et al. 2015), and fewer have evaluated railway noise (Dratva et al. 2012; Seidler et al. 2016a, 2016b; Sørensen et al. 2011). Although previous epidemiological studies have focused on average noise levels, field studies suggest that nighttime noise events correlate better with awakening reactions and cardiac arousals than average levels (Basner et al. 2011; Brink et al. 2008). Therefore, it is unclear whether average levels alone are a good predictor for cardiovascular effects. Studies are needed that evaluate not only average noise levels but the relevance of their content in noise events. Moreover, little is known about the importance of environments with low and high noise fluctuation (i.e., constant noise vs. isolated events that stand out from a quiet background, respectively), particularly at night. Very recently, a new indicator called intermittency ratio was created, which allows the estimation of this characteristic (Wunderli et al. 2016).
In this study, we aimed to evaluate the association of long-term exposure to transportation noise levels and their temporal structure with baPWV in an adult population-based Swiss cohort by assessing residential outdoor annual average levels of road, railway, and aircraft noise; total (all-source) noise intermittency ratio; and total number of noise events, and accounting for several confounders including coexposure to traffic-related air pollution. We also evaluated how the studied associations with baPWV were modified by different noise exposure situations and participant characteristics.
Methodology
Study Sample
The Swiss Cohort Study on Air Pollution and Lung and Heart Diseases in Adults (SAPALDIA) is a population-based cohort of adults. The baseline study population was examined in 1991 (SAP1) and consisted of a random selection of 9,651 adults 18–60 y old from eight environmentally diverse areas in Switzerland corresponding to different municipalities (Martin et al. 1997). The first follow-up (SAP2) was in 2001–2003 (; 83% response rate) (Ackermann-Liebrich et al. 2005). The second follow-up (SAP3) was in 2010–2011 (; 76% response rate), and it aimed to further investigate CVD and aging. In SAP3, arterial stiffness was measured in a random sample of 3,086 participants who were old in the examination year (64% of the 4,832 participants in this age range), which constitutes the gross sample of the present cross-sectional study.
The study was approved by the ethics boards of the eight SAPALDIA study communities, and all participants signed informed consent.
Arterial Stiffness
At SAP3, we measured baPWV using a noninvasive VaSera VS-1500N vascular screening system (Fukuda Denshi). As described elsewhere (Endes et al. 2015, 2016), measurements were taken in supine position after of rest in a quiet room with constant temperature. Common blood pressure cuffs were placed on each upper arm and above the ankles. The initial notch of the pulse waves at the heart and at the ankle was detected on average over six cardiac cycles (a cardiac cycle or beat includes systole, diastole, and the intervening pause) by attaching electrocardiogram leads at each wrist and a phonocardiogram on the sternal border in the second intercostal space. The time delay of the pulse wave from the heart to the ankle was determined by a foot-to-foot-method. Vascular length between the heart valve and the ankle artery was estimated by the VSS-10 software (Fukuda Denshi) using the manufacturer’s height-based formula. Brachial-ankle pulse wave velocity reflects arterial stiffness between the brachial and tibial arteries and is calculated by dividing the arterial length by the time delay of the pulse waves (meters/second). We used the average of two consecutive measurements at 3–5-min intervals and of both body sides for analyses. Reproducibility was high in this cohort (Endes et al. 2015). Blood pressure was measured following standard protocols (Pickering et al. 2005), in sitting position and after 10 min of rest, using a validated automatic device (Omron 705IT, Omron Healthcare, Japan). Two measurements were taken, separated by , and their mean was calculated. Mean arterial pressure (MAP) was calculated as follows: .
Noise Exposure Assessment
Based on the source-specific noise models described below, we assigned annual average road, railway, and aircraft noise levels, total number of noise events, and total noise intermittency ratio at the height of the floor of the most exposed façade of the geocoded residential addresses. Addresses were indicated by participants. The indicators were derived as follows.
Noise models provided A-weighted long-term average sound pressure levels determined over all day (Lday; 0700–1900 hours), evening (Leve, 1900–2300 hours), and night (Lnight, 2300–0700 hours) periods of a year (in decibels) as defined in Directive 2002/49/EC (European Parliament and Council of the European Union 2002). We combined these time periods to derive the standard 24-h annual average European Union (EU) indicator Lden (in decibels), with 5-dB and 10-dB penalties for Leve and Lnight, respectively, and with truncation at 35 dB for road and at 30 dB for aircraft and railway noise.
As reported previously (Wunderli et al. 2016), the total annual average number of noise events for all sources was counted for nighttime () and daytime (). Noise events were counted when their maximum noise level exceeded a certain calculated threshold (i.e., 3 dB above the total A-weighted average sound pressure level per hour). Total nighttime () and daytime intermittency ratios () were then calculated as the percentage of the total sound energy due to the isolated events, that is to say, the ratio between the events’ noise level for period T () and the total noise level for the same period T (), both expressed in sound energy (unit: percent) (Equation 1). We used the total of all sources to study whether the overall noise environment was fluctuating or more constant.
| [1] |
Source-specific noise models for Switzerland for 2011 were produced to provide detailed exposure assessment in the framework of the SiRENE project (Short and Long Term Effects of Transportation Noise Exposure) and are described elsewhere (Karipidis et al. 2014). Briefly, the aircraft noise modeling included the emissions of one military and the three major civil airports. Noise levels were calculated with FLULA2 software (version 4; Empa) using a combination of traffic statistics (Federal Office of Civil Aviation), radar data (Zürich), acoustic footprints (Basel, Geneva), and idealized number and time of flight paths for the military airport (Payerne). Railway noise levels were derived using sonRAIL (Thron and Hecht 2010), and noise propagation was calculated with the Swiss railway noise model SEMIBEL (FOEN 1990). The calculations considered the railway tracks’ geometry, location of switch points, noise barriers, train types, driving speed, and traffic statistics. Road noise levels were calculated using the sonROAD emission model (Heutschi 2004) and the StL-86 propagation model (FOEN 1987) with input data from 3-D geometry, including bridges, noise barriers, road slopes, type and width, speed limits, traffic statistics in an hourly resolution per each road type, and location and height of noise barriers (Karapidis et al. 2014).
Air Pollution Exposure Assessment
Outdoor air pollution was assigned to the geocoded participants’ addresses as biannual average nitrogen dioxide concentrations () and average particulate matter of diameter (). was prioritized as a marker of near-road air pollution and was thus considered the main potential confounder of road noise effects. Biannual estimates were available from validated land-use regression (LUR) models generated for SAPALDIA and represented exposure during the recruitment period of 2010–2011. Traffic variables and national dispersion model estimates were important predictors in these LUR models (Eeftens et al. 2016).
Other Explanatory Variables
We collected the following information at SAP 3 using personal interview–administered questionnaires: age (continuous), sex (male/female), educational level achieved (low/middle/high), smoking (no/yes), number of pack-years smoked (continuous), passive smoking (no/yes), alcohol consumption (no/yes), consumption of raw vegetables (days/week), cooked vegetables (days/week), and fish (days/week), bedroom orientation (street/backyard), closing windows at night (no/yes), study area (municipality), self-reported hearing impairment (none/mild/severe), self-reported doctor-diagnosed CVD, cardiovascular medication (none vs. ), and the Epworth daytime sleepiness score from 0 (none) to 24 (maximum) (Johns 1991). Based on a short questionnaire, we defined physical activity as exercising for at a moderate intensity according to physical activity guidelines (WHO 2010). General transportation noise annoyance was assessed using the question, “How much are you disturbed by transportation noise at home when windows are opened?” on an International Commission on the Biological Effects of Noise (ICBEN)-type 11-point scale from 0 (not at all annoyed) to 10 (extremely annoyed) (Fields et al. 2001). We also scored the item, “Are you sensitive to noise?” on a 6-point scale from 1 (strongly disagree) to 6 (strongly agree). This item is part of the 10-item Weinstein noise sensitivity score (Weinstein 1980, 1978). We also accounted for an administrative neighborhood-level socioeconomic index (deprivation index) based on the median household income, household occupancy, educational level, and occupation of the head of household reported in the 2000 census (Panczak et al. 2012). Finally, we used the measured height and weight to calculate body mass index (BMI) in kilograms per meter squared.
Statistical Analyses
We included 2,775 participants (i.e., of the sample with baPWV measurements, ) who had complete data on the outcome, exposures, and covariates of the main model described below.
We performed descriptive analyses of all variables and derived the natural logarithm of baPWV to normalize its distribution. We assessed bivariable relationships between baPWV, noise, and air pollution indicators with Spearman rank correlation. To assess the shape of the association of all independent variables with baPWV, we used penalized smoothing splines, and we transformed variables accordingly for nonlinear associations. As a result, we analyzed BMI as a squared term and categorized NE in quartiles. No transformation was required for food consumption variables (days/week). We only dichotomized these variables in descriptive analyses for better visualization, given their skewed distribution.
Lden was prioritized as the EU marker and for conciseness, given its very high correlation with Lday () and particularly with Lnight () levels, for both railway and road noise levels (see Table S1). Furthermore, nighttime aircraft activity was limited in this sample (see Table S2). Correlations were rather high between and () and between and (), but they varied in levels and in range and in their day- and nighttime correlations with source-specific noise levels (see Tables S1 and S2). Therefore, in main analyses, we prioritized nighttime IR and NE as the most relevant time window for cardiovascular noise effects (Basner et al. 2011).
We evaluated the percent change in the geometric mean of baPWV per interquartile range (IQR) change in the noise indicators using multivariable linear mixed models. Linear mixed models are an extension of linear regression models that permit the inclusion of a random intercept by study area to account for between-area effects.
First, we studied associations of railway, road, and aircraft Lden levels and and with baPWV separately, in single-exposure models. The main model (model A) was a multiexposure model including all source-specific Lden levels. We further adjusted for (model B) or (model C) to evaluate the impact of the noise level, the fluctuating noise environment, and the noise events independently of each other. In secondary analyses, we further explored models B and C with and instead of and .
All models were adjusted for covariates selected a priori, as suggested in previous literature on baPWV (Endes et al. 2016) and noise-related CVD epidemiology (Vienneau et al. 2015): sex, age, sex×age, education, smoking status, pack-years smoked, second-hand smoke exposure, alcohol consumption, fish and cooked and raw vegetable consumption, BMI, , physical activity, MAP, MAP×sex, and levels. Models were adjusted for MAP to obtain a clean measure of arterial stiffness with baPWV (Endes et al. 2016; Vlachopoulos et al. 2012). Given the substantial left-truncation of the aircraft and railway Lden levels, we also included a source-specific indicator variable with a value of zero for left-truncated observations and a value of 1 otherwise; this allowed us to interpret results for those above the truncation threshold. Covariates were included in consecutive increasing adjustment sets to check their influence on the estimated effect (see Figure S1). Figure S1 also considers adjustment for potential confounders not included in the main model because of missing observations and for two potential mediators of the studied association (noise annoyance and daytime sleepiness).
We studied characteristics of the sample that could modify the association between the source-specific Lden levels and baPWV, specifically: sex, daytime sleepiness score, noise annoyance, noise sensitivity, , study area recategorized as urban versus rural area, bedroom orientation, and closing windows at night. For this purpose, interaction terms between the noise exposure variable and the respective potential modifying factor were tested as part of the main multiexposure model A.
In sensitivity analyses, we studied potential exposure misclassification by residential mobility by excluding movers in the 10 y before the visit. We also evaluated model A after exclusion of participants with hearing impairment or CVD (to avoid uncertainty on perception and outcome due to different degrees of disease and treatment).
To assess potential selection bias, we compared the characteristics of the final sample with those of the underlying SAP3 samples from which it was extracted. Furthermore, we assessed potential participation selection bias due to loss to follow-up from the baseline recruitment (SAP1, ) with inverse probability weighting (IPW), applying the inverse of the probability of participating in the present study to the main model. Probabilities were derived using variables from the baseline recruitment that predicted participation in the present study.
Analyses were performed using Stata v.13.0 (StataCorp LLC) and R v.3.1.3 (R Foundation for Statistical Computing). Statistical significance was considered at an alpha level of 0.05.
Results
The characteristics of the study sample () were similar to those of the underlying SAP3 sample in which baPWV was measured () and to those of the entire SAP3 sample for the same age range (). The final sample differed from the entire SAP3 sample () mainly in being 3 y older and more medicated and in having more CVD but a slightly better lifestyle (see Table S2).
Participants had a median (and average) age of 63 y (; range: 49.4–80.9); 51% were women, and their median baPWV was (; range: 8.8–26.2) (Table 1). The medians (IQRs) of road, railway, and aircraft Lden levels were 54.2 (10.6), 30.0 (8.1), and 32.8 (8.0) dB, respectively; and those of , , , and were 123 (179), 433 (870), 73.1% (27.2), and 63.8% (40.3), respectively. In addition, 99.7%, 44.6% and 57.6% of the study population were exposed to road, railway, and aircraft Lden levels above the truncation value, respectively. Medians (IQRs) for railway and aircraft Lden levels among those exposed were 40.0 (45) and 37.1 (29.4) dB, respectively (Table 1; see also Figure S2).
Table 1.
Main characteristics of the study sample.
| Variables | Total |
|---|---|
| Continuous variables [median (IQR)] | |
| Brachial-ankle pulse wave velocity (m/s) | 13.4 (3.1) |
| Lden, road (dB) | 54.2 (10.6) |
| Lden, railway (dB) | 30.0 (8.1) |
| Lden, aircraft (dB) | 32.8 (8.0) |
| (%) | 73.1 (27.2) |
| (n) | 122.9 (178.9) |
| Nitrogen dioxide () | 17.3 (10.5) |
| Age (years) | 63.2 (12.3) |
| Pack-years smoked | 1.0 (20.5) |
| Body mass index () | 25.9 (5.6) |
| Mean blood pressure (mmHg) | 97.5 (16.0) |
| Noise sensitivity score (n)a | 3.2 (1.6) |
| Daytime sleepiness score (n)b | 14.0 (5.0) |
| Categorical variables [n (%)] | |
| % exposed to Lden,c road | 2,766 (99.7) |
| % exposed to Lden,c railway | 1,237 (44.6) |
| % exposed to Lden,c aircraft | 1,598 (57.6) |
| Sex, women | 1,417 (51.1) |
| Education | |
| Low | 169 (6.1) |
| Middle | 1,817 (65.5) |
| High | 789 (28.4) |
| Smoking | |
| Never | 1,175 (42.3) |
| Former | 1,140 (41.1) |
| Current | 460 (16.6) |
| Secondhand smoke, yes | 330 (11.9) |
| Alcohol consumption, yes | 1,286 (46.3) |
| Moderate physical activity, | 1,648 (59.4) |
| Raw vegetables, | 2,013 (72.5) |
| Cooked vegetables, | 1,586 (57.2) |
| Fish, | 1,889 (68.1) |
| Study area | |
| Basel | 329 (11.9) |
| Wald | 484 (17.4) |
| Davos | 289 (10.4) |
| Lugano | 357 (12.9) |
| Montana | 307 (11.1) |
| Payerne | 350 (12.6) |
| Aarau | 457 (16.5) |
| Geneva | 202 (7.3) |
| Bedroom orientation, backyardb | 1,607 (58.2) |
| Close window at night,b yes | 621 (22.5) |
| Noise annoyance, yes | 1,588 (57.2) |
| CVD medication, yes | 835 (30.1) |
| CVD,b yes | 1,090 (39.3) |
Note: CVD, cardiovascular disease; IQR, interquartile range; IRnight, total nighttime noise intermittency ratio; Lden, annual average noise levels for 24h with and penalties for the evening and night, respectively; NEnight, total nighttime number of noise events.
11.9% missing observations.
missing observations.
Percent exposed above Lden truncation level (road, 35 dB; railway and aircraft, 30 dB). Medians (IQR) for railway and aircraft Lden levels among those exposed were respectively 40.0 (45) dB and 37.1 (29.4) dB.
In bivariate analyses, we observed a small significant correlation between railway noise levels and baPWV (Spearman rank correlation, ) (see Table S1).
The highest correlation between source-specific Lden levels was between railway and aircraft Lden levels. The highest correlation of was with both railway and road Lden levels (), and the lowest was between and road Lden levels (). Road Lden levels had the highest correlation with and ( and , respectively, treated as continuous variables) and with air pollution ( with , and with ). Railway Lden levels had the highest correlation with (), and aircraft Lden levels had the highest correlation with ().
In multivariable analyses (Table 2), railway Lden levels and were significantly associated with baPWV, but road and aircraft Lden levels and were not.
Table 2.
Associations of annual average transportation noise levels (Lden), total nighttime noise intermittency ratio (), and total number of nighttime noise events () with arterial stiffness ().
| Noise indicator | Single-exposure models % (95% CI) | Multiexposure model A % (95% CI) | Multiexposure model B % (95% CI) | Multiexposure model C % (95% CI) |
|---|---|---|---|---|
| Lden, road | 0.19 (, 0.88) | 0.16 (, 0.85) | 0.24 (, 0.95) | (, 0.27) |
| Lden, railway | 0.87 (0.31, 1.43)** | 0.87 (0.31, 1.43)** | 0.92 (0.35, 1.49)** | 1.01 (0.44, 1.58)** |
| Lden, aircraft | (, 0.88) | (, 0.77) | (, 0.79) | (, 0.83) |
| (, 0.57) | — | (, 0.35) | — | |
| , Q1 (0–54.8) | Reference | — | — | Reference |
| , Q2 (55.1–122.9) | 0.71 (, 1.91) | — | — | 0.97 (, 2.17) |
| , Q3 (123.2–233.7) | 0.89 (, 2.11) | — | — | 1.42 (0.14, 2.70)** |
| , Q4 (233.8–1324.3) | 1.77 (0.45, 3.09)** | — | — | 2.64 (1.05, 4.22)** |
Note: Subjects were exposed to road (99.7%), railway (44.6%), and aircraft (57.6%) Lden levels above the truncation value. Single-exposure models include one noise indicator at a time. Multiexposure model A includes all source-specific Lden levels; model ; . All percent changes are per interquartile range (IQR) of the respective noise indicator (road, 10.6 dB; railway, 8.1 dB; aircraft, 8 dB; IR, 27.2%), or quartiles (Qs) for NE. All linear mixed models were adjusted for sex, age, , education, smoking status, pack-years smoked, secondary smoke, alcohol consumption, diet, body mass index (BMI), , physical activity, mean arterial pressure (MAP), , nitrogen dioxide, noise truncation indicators, and a random intercept by study area. *, **.
Specifically, an IQR change in railway Lden levels was associated with an increase of 0.87% (95% CI: 0.31, 1.43) in baPWV in the adjusted single-exposure model (Table 2) or 1.08% (95% CI: 0.39, 1.78) per 10 dB (see Table S3). This association was linear (see Figure S3) and remained after adjustment for all noise sources, or , , , and other additional adjustments. The estimated effect was mainly influenced by age and by MAP, which decreased the association by each (Table 2; see also Figure S1).
The association between and baPWV showed dose dependency and became stronger in magnitude after adjustment for all Lden sources (Table 2), reaching an increment of 2.64% (95% CI: 1.05, 4.22) in baPWV for the highest NE quartile. Compared with the nighttime period, daytime NE was not associated with baPWV, and there was a nonsignificant negative association between daytime IR and baPWV (see Table S4). Adjusting for these variables did not alter the association between railway Lden levels and baPWV.
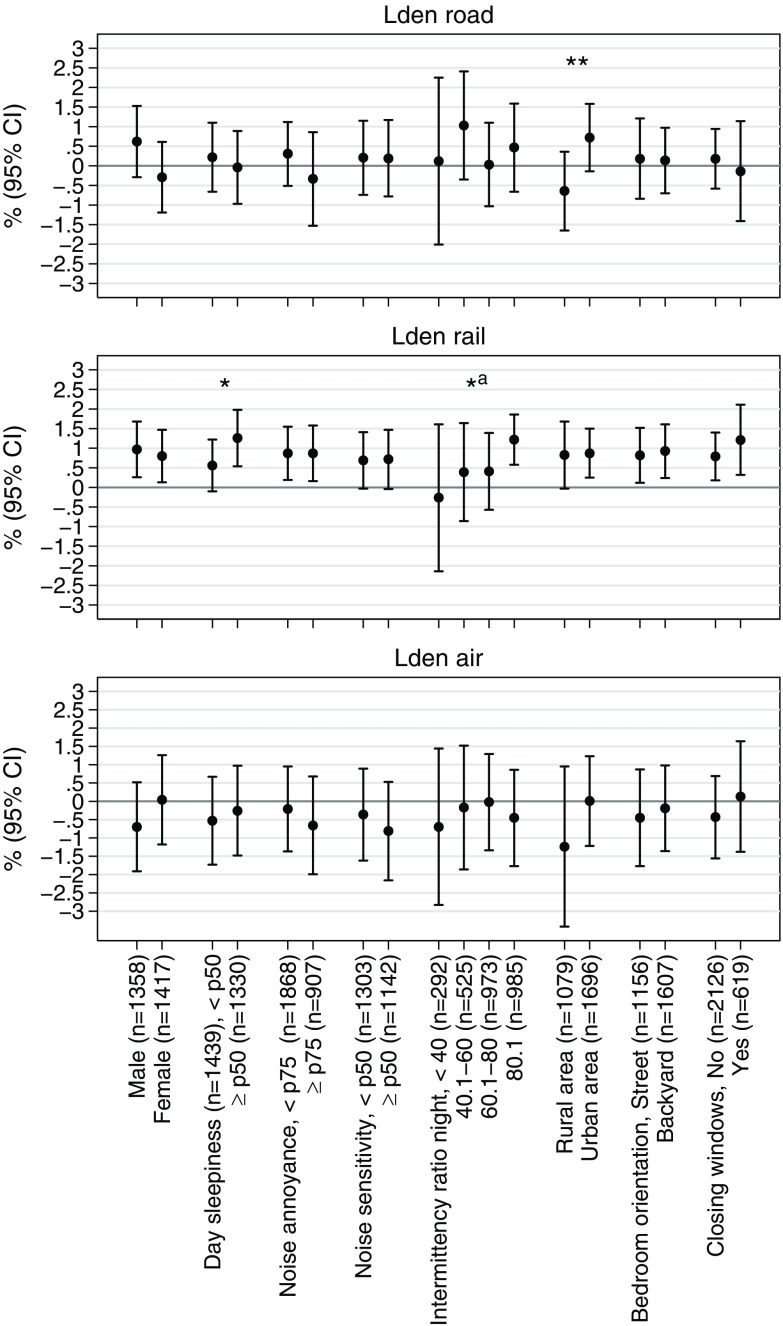
Figure 1 shows the results for the effect modification analyses. A nonsignificant positive association between road Lden levels and baPWV was observed in urban areas [0.72% (95% CI: , 1.58); ], whereas the association was negative but further from significance in rural areas [ (95% CI: , 0.36); ]; the interaction was statistically significant () (Figure 1). The association between railway Lden levels and baPWV was greater at higher levels, reaching a 1.22% increase (95% CI: 0.58, 1.86) in baPWV in the highest IR group (, p-value of interaction for ). The magnitude of the association was also greater for participants who reported daytime sleepiness above the median [1.26% (95% CI: 0.54, 1.98)] than for those who did not [1.00% (95% CI: , 1.22); . We found no evidence of other statistically significant interactions or nonsignificant trends.
Figure 1.
Association between annual average source-specific noise levels (Lden) and arterial stiffness (baPWV) across different subgroups, per interquartile range (IQR) change of the respective noise indicator (road: 10.6 dB, railway: 8.1 dB, aircraft: 8 dB). Multiexposure linear mixed models included an interaction term between Lden and the corresponding subgroup and were adjusted for sex, age, , education, smoking status, pack-years smoked, secondary smoke, alcohol consumption, diet, body mass index (BMI), , physical activity, mean arterial pressure (MAP), , nitrogen dioxide, all source-specific Lden levels and their noise truncation indicators, and a random intercept by study area. **p-value of interaction , *p-value of interaction . ap-value for , p-value of interaction .
In sensitivity analyses, the magnitude of the associations between transportation Lden levels and baPWV were greater after applying IPW to weight for participant selection bias since the beginning of the cohort (see Table S5).
The association between railway Lden levels and baPWV remained similar in magnitude when restricting the sample to nonmovers during the 10 y before examination or to those without hearing impairment or CVD (factors that may interfere with the exposure or the outcome). Associations of road and aircraft Lden levels with baPWV became more positive for nonmovers and more negative for those without CVD or hearing impairment, but all remained highly nonsignificant.
Discussion
To our knowledge, this is the first epidemiological study to evaluate the association between long-term exposure to transportation noise and a direct marker of arterial stiffness, exploring the relative contribution of the different sources and assessing the impact of total noise events and total noise intermittency ratio. We observed a linear association between annual average railway noise levels (expressed with Lden) and baPWV, which might be greater in highly intermittent noise environments at night () as well as in participants reporting daytime sleepiness. A positive but nonsignificant association was observed with road Lden levels in urban areas, whereas this association tended to be negative in rural areas. The total number of nighttime noise events (), mainly representing road noise, was also associated with baPWV independently of average noise levels. The observed associations were also independent of traffic-related air pollution.
Transportation Noise Indicators, Arterial Stiffness, and Comparison with the Literature
No previous epidemiological noise studies have evaluated direct markers of arterial stiffness. Indirectly, our results appear to be in accord with those of a cross-sectional study from the first follow-up of this cohort (SAP2) (Dratva et al. 2012), which yielded an association between annual average levels of railway noise and blood pressure but not with road traffic noise. Our results suggest that long-term exposure to railway noise may affect arterial stiffness irrespective of other noise sources, total noise events, and total noise intermittency ratio. Nevertheless, the impact might be greater for those participants exposed to railway noise who live in an environment with highly intermittent nighttime noise. In ancillary analyses to characterize such situations, we observed that when was , a) the percentage exposed to railway noise (Lden) was higher (50.7%) than average (44.6%), and b) among those exposed to railway noise, railway Lden levels were also higher than average: 42.7 (17.5) versus 39.6 (12.1) dB, respectively, but road and aircraft Lden levels were lower or similar (see Tables S6 and S7). This finding highlights the importance of situations in which railway noise stands out, exhibiting its intermittent nature, thus leading to high noise events with quiet periods in between (which may happen mostly at night). These events should be also frequent enough while still standing out from the background to agree with the observed higher railway Lden levels.
Total was not associated with baPWV, which suggests that not all intermittent noise situations, which are mixtures of different noise-source combinations and background levels, might consistently affect baPWV. For example, a few separated and/or quiet events in a quiet environment could still contribute to high IR but would result in low noise levels, which may not be crucial for baPWV. In contrast, high noise levels with high noise background (more likely during the day), would lead to low IR. Such situations may even lead to negative associations and could explain the observed negative association between and baPWV.
Two previous studies observed associations between annual average road noise levels and isolated high systolic blood pressure (Babisch et al. 2014a; Foraster et al. 2014), an indirect marker of arterial stiffness. Moreover, both studies were conducted in urban areas, namely, Augsburg, Germany (Babisch et al. 2014a), and Girona, Spain (Foraster et al. 2014). A recent study in another urban area (London, UK) also observed a nonsignificant positive association between annual average road noise levels and atherosclerosis, a cardiovascular end point that may contribute to arterial stiffness (Halonen et al. 2017).
The present study did not yield an association between road Lden levels and baPWV in the entire sample, but it did yield an association for , mostly correlated with road Lden noise levels (). This finding suggests that a) the number of nighttime noise events (not daytime noise events) could be a relevant road traffic predictor for high baPWV, and b) average road noise levels might not always be representative of such noise patterns alone. Indeed, the structure of road traffic noise is more complex than those of railway and aircraft noise, whose average noise levels already represent the eventful nature of the source. In line with the abovementioned literature, we observed a nonsignificant positive association between road Lden levels and baPWV in urban areas (), although there was an opposite negative tendency in rural areas (), which could explain the significant interaction. Although chance findings can never be discarded and the results in rural areas are difficult to interpret, the differences could also relate to the type of road noise characteristics captured by Lden in each environment. Interestingly, Lden was more representative of in urban than in rural areas (, data not shown). In fact, participants lived closer to major roads [141.3 (264) m vs. 671 (1,298) m] and were exposed to higher [131 (207) vs. 112 (145)] in urban than in rural areas, respectively (data not shown). In conclusion, situations with more frequent road traffic events that stand out from the background (more likely at night and when living closer to the source) could be more relevant than a few isolated quiet cars with quiet background at night (which could lead to higher IR) or continuous noise with no distinct events (which would provide low IR but high average noise levels).
Although aircraft noise is of intermittent nature as is railway noise, it was not associated with baPWV. Because the night is considered the most susceptible time window for cardiovascular effects (Münzel et al. 2014), such an observation could be related to the lack of aircraft operations after midnight in Switzerland [Lnight, aircraft median (4) dB; see Table S2).
Biological Mechanisms
The association observed with , but not , and the suggestive interactions with and daytime sleepiness appear to be in line with the main proposed biological pathway of cardiovascular noise effects. This pathway suggests that noise triggers a direct stress reaction, which activates the autonomic nervous and endocrine systems, particularly during resting periods and even while sleeping (Babisch 2002). Sleep might be involved in the effects of noise on baPWV because participants with daytime sleepiness seemed to be more susceptible to the estimated effects of railway noise on baPWV. However, the associations were not mediated by daytime sleepiness, which might indicate the implication of other sleep indicators or pathways not tested in this study.
Specifically, an experimental sleep study observed acute increases in blood catecholamine levels, endothelial dysfunction, and pulse wave velocity (Schmidt et al. 2013) and suggested a mediation through oxidative stress. However, the authors only assessed nighttime aircraft noise levels. Other sleep studies have observed that awakenings were more related to noise events and to their maximum levels than to average noise levels (Basner et al. 2011; Brink et al. 2008; Elmenhorst et al. 2012), which was also observed for cardiac arousals and heart rate changes, and as in the present study, only for railway and road noise levels (Basner et al. 2011). This finding was explained by the faster noise level rise time of railway and road noise compared with that of aircraft noise events. Basner et al (2011) further observed that cardiac arousals persisted across several nights. This observation suggests that in the long term, such acute repeated reactions could persist and contribute to homeostatic and vascular changes, such as arterial stiffness and hypertension (van Kempen and Babisch 2012), which contribute to CVD (Münzel et al. 2014). By means of stress-related cortisol release and noise-induced sleep disturbance, down-stream mechanisms might also involve oxidative stress, inflammation, impairment of the circadian rhythm and immune system, or a combination of any or all of these mechanisms, promoting insulin resistance and atherosclerosis, which could in turn affect arterial stiffness (Münzel et al. 2016; Recio et al. 2016). Indeed, several pathways could be in place. Our results suggest that part of the studied association might be mediated by blood pressure, given that the magnitude of the association between railway Lden levels and baPWV was 18% smaller after adjustment for MAP. In addition, high blood pressure may also be a consequence of arterial stiffness. Nonetheless, a direct association remained after controlling for MAP, which could respond to pathways independent of blood pressure.
Strengths and Limitations
The main limitation of this study was its cross-sectional design. Nevertheless, our results are supported by initial experimental and epidemiological evidence (Babisch et al. 2014a; Basner et al. 2011). Reverse causality might also be limited because it seems unlikely that participants with high baPWV move to noisier areas (Babisch 2011), and the results remained similar for those without CVD. Regarding selection bias, sensitivity analyses indicated that the results of the present study might be conservative because the magnitude of the studied associations was greater after applying IPW to assess loss to follow-up since the beginning of the cohort and for the entire age range. Another limitation was the small number of participants exposed to nighttime aircraft noise, which may explain the null findings for this exposure, assuming that nighttime is the most relevant period of exposure. Nevertheless, its lack of impact on baPWV might be plausible according to the slower rise time of its events, as explained above (Basner et al. 2011).
The main strength was the novel and detailed individual residential noise exposure assessment for the whole of Switzerland, which was, to our knowledge, not available in previous studies. Moreover, we used new indicators to estimate noise events and intermittency ratio; assessed the three main transportation noise sources, which are acoustically different and could have different effects on health (as observed); and controlled for traffic-related air pollution exposure, a main confounder when studying the effects of road noise on CVD (Tétreault et al. 2013). Exposure misclassification related to residential mobility seemed limited because the results were robust to excluding participants who moved during the last 10 y before the examination. In addition, we observed no exposure modification by closing windows at night or by having the bedroom facing the backyard (Babisch et al. 2014b; Foraster et al. 2014). Exposure misclassification resulting from the use of residential Lden and not Lnight (when participants are mostly at home) levels may also be limited because Lden levels were almost perfectly correlated with Lnight levels for railway and road (0.98–1.00), and we would also expect null associations with Lnight levels for aircraft owing to the little nighttime aircraft noise exposure in this sample. In turn, exposure during the evening at home would be captured by Lden.
This study was also able to use a direct measure of arterial stiffness (baPWV). Although central pulse wave velocity is the gold-standard marker, it is highly dependent on the observer’s skills and thus requires extensive training (Endes et al. 2015), and this information was only available for a small and differently distributed sample in terms of noise exposure, limiting statistical power and comparability. In contrast, baPWV has been proposed as a reproducible, easy-to-apply measure of peripheral and central arterial stiffness, and it is also a predictor of future cardiovascular events and all-cause mortality (Vlachopoulos et al. 2012, 2015). Although baPWV has mainly been validated in Asian populations, its use has recently shown reproducibility in Caucasians in the Swiss population (Endes et al. 2015). We also adjusted for MAP, used to obtain a more representative, clean measure of baPWV. This may lead to overadjustment because blood pressure could be in the pathway or could be a consequence of arterial stiffness. Therefore, our approach was likely conservative and would probably be more representative of the direct association between transportation noise and arterial stiffness. The magnitude of the total estimated effect of railway noise on arterial stiffness may be greater, as observed before adjustment for MAP. Finally, although the magnitude of the estimated effects was small, a systematic review of cohort studies has shown that a small increase in baPWV by was associated with a 13% increase in cardiovascular mortality (Vlachopoulos et al. 2012). Moreover, exposure to transportation noise is prevalent and affects millions of people, and thus is an important contributor to the burden of CVD.
Conclusion
In conclusion, residential outdoor long-term exposure to railway noise (expressed as annual average Lden levels) and to total number of noise events (mainly related to road noise) may be associated with arterial stiffness as measured by baPWV, particularly at night and potentially through sleep impairment. The impact of railway noise might be stronger in highly intermittent nighttime noise environments (i.e., in a noise-fluctuating environment with contribution of high noise events to the total noise level). The number of distinct nighttime noise events may be critical for high baPWV, and it may be a better predictor of the detrimental patterns of road noise than average levels alone. The latter might be less representative in rural than in urban areas, where participants live closer to traffic and exposure to noise events is greater. The association between transportation noise and arterial stiffness adds to the evidence about the long-term impact of noise on the cardiovascular system and the development of CVD. These initial findings should be replicated in future longitudinal studies, considering areas with more exposure contrast in aircraft noise levels and taking additional biomarkers into consideration toward mechanistic understanding.
Supplemental Material
Acknowledgments
This work was supported by the Swiss National Science Foundation, SNF-SAPALDIA (grant numbers 33CS30-148470/1, 33CSCO-134276/1, 33CSCO-108796, 324730_135673, 3247BO-104283, 3247BO-104288, 3247BO-104284, 3247-065896, 3100-059302, 3200-052720, 3200-042532, 4026-028099, PMPDP3_129021/1, PMPDP3_141671/1); SNF-SiRENE (grant number CRSII3_147635); and the Swiss Federal Office for the Environment.
SAPALDIA is also supported by the Federal Office of Public Health; the Federal Office of Roads and Transport; the canton governments of Aargau, Basel-Stadt, Basel-Land, Geneva, Luzern, Ticino, Valais, and Zürich; the Swiss Lung League; the canton Lung Leagues of Basel Stadt/Basel Landschaft, Geneva, Ticino, Valais, Graubünden and Zürich; Stiftung ehemals Bündner Heilstätten; the Swiss National Accident Insurance Fund (SUVA); Freiwillige Akademische Gesellschaft; UBS Wealth Foundation, Talecris Biotherapeutics GmbH; Abbott Diagnostics; European Commission 018996 (GABRIEL); and Wellcome Trust WT 084703MA.
References
- Ackermann-Liebrich U, Kuna-Dibbert B, Probst-Hensch NM, Schindler C, Felber Dietrich D, Stutz EZ, et al. 2005. Follow-up of the Swiss Cohort Study on Air Pollution and Lung Diseases in Adults (SAPALDIA 2) 1991-2003: methods and characterization of participants. Soz-Präventivmed 50:245–263, 10.1007/s00038-005-4075-5. [DOI] [PubMed] [Google Scholar]
- Babisch W. 2002. The noise/stress concept, risk assessment and research needs. Noise Health 4(16):1–11, PMID: 12537836. [PubMed] [Google Scholar]
- Babisch W. 2003. Stress hormones in the research on cardiovascular effects of noise. Noise Health 5(18):1–11, PMID: 12631430. [PubMed] [Google Scholar]
- Babisch W. 2011. Cardiovascular effects of noise. Noise Health 13(52):201–204, PMID: 21537102, 10.4103/1463-1741.80148. [DOI] [PubMed] [Google Scholar]
- Babisch W. 2014. Updated exposure-response relationship between road traffic noise and coronary heart diseases: a meta-analysis. Noise Health 16:1–9, PMID: 24583674, 10.4103/1463-1741.127847. [DOI] [PubMed] [Google Scholar]
- Babisch W, Wolf K, Petz M, Heinrich J, Cyrys J, Peters A. 2014a. Associations between traffic noise, particulate air pollution, hypertension, and isolated systolic hypertension in adults: The KORA Study. Environ Health Perspect 122(5):492–498, PMID: 24602804, 10.1289/ehp.1306981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babisch W, Wölke G, Heinrich J, Straff W. 2014b. Road traffic noise and hypertension – Accounting for the location of rooms. Environ Res 133:380–387, PMID: 24952459, 10.1016/j.envres.2014.05.007. [DOI] [PubMed] [Google Scholar]
- Basner M, Müller U, Elmenhorst E-M. 2011. Single and combined effects of air, road, and rail traffic noise on sleep and recuperation. Sleep 34(1):11–23, PMID: 21203365, 10.1093/sleep/34.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brink M, Lercher P, Eisenmann A, Schierz C. 2008. Influence of slope of rise and event order of aircraft noise events on high resolution actimetry parameters. Somnologie - Somnologie 12(2):118–128, 10.1007/s11818-008-0345-9. [DOI] [Google Scholar]
- Dratva J, Phuleria HC, Foraster M, Gaspoz J-M, Keidel D, Künzli N, et al. 2012. Transportation noise and blood pressure in a population-based sample of adults. Environ Health Perspect 120(1):50–55, PMID: 21885382, 10.1289/ehp.1103448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eeftens M, Meier R, Schindler C, Aguilera I, Phuleria H, Ineichen A, et al. 2016. Development of land use regression models for nitrogen dioxide, ultrafine particles, lung deposited surface area, and four other markers of particulate matter pollution in the Swiss SAPALDIA regions. Environ Health 15:53, PMID: 27089921, 10.1186/s12940-016-0137-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elmenhorst E-M, Pennig S, Rolny V, Quehl J, Mueller U, Maaß H, et al. 2012. Examining nocturnal railway noise and aircraft noise in the field: Sleep, psychomotor performance, and annoyance. Sci Total Environ 424:48–56, PMID: 22444069, 10.1016/j.scitotenv.2012.02.024. [DOI] [PubMed] [Google Scholar]
- Endes S, Caviezel S, Dratva J, Schaffner E, Schindler C, Rothe T, et al. 2015. Reproducibility of oscillometrically measured arterial stiffness indices: results of the SAPALDIA 3 cohort study. Scand J Clin Lab Invest 75(2):170–176, PMID: 25594797, 10.3109/00365513.2014.993692. [DOI] [PubMed] [Google Scholar]
- Endes S, Schaffner E, Caviezel S, Dratva J, Autenrieth CS, Wanner M, et al. 2016. Physical activity is associated with lower arterial stiffness in older adults: results of the SAPALDIA 3 Cohort Study. Eur J Epidemiol 31(3):275–285, PMID: 26220521, 10.1007/s10654-015-0076-8. [DOI] [PubMed] [Google Scholar]
- European Environment Agency. 2014. Noise in Europe 2014. Luxembourg:Publications Office. [Google Scholar]
- European Parliament and Council of the European Union. 2002. Directive 2002/49/EC of the European Parliament and of the Council of 25 June 2002 relating to the assessment and management of environmental noise - Declaration by the Commission in the Conciliation Committee on the Directive relating to the assessment and management of environmental noise. Official Journal L 189:12–26. [Google Scholar]
- Fields JM, De Jong RG, Gjestland T, Flindell IH, Job RFS, Kurra S, et al. 2001. Standardized general-purpose noise reaction questions for community noise surveys: research and a recommendation. J Sound Vib 242(4):641–679, 10.1006/jsvi.2000.3384. [DOI] [Google Scholar]
- FOEN. 1987. Computer model for the calculation of street noise, part 1, operating instructions for the computer program StL-86, in the environmental protection series. Swiss Federal Office for the Environment, Bern. [Google Scholar]
- FOEN. 1990. SEMIBEL: Swiss Emission and Immission Model for the calculation of railway noise. Swiss Federal Office for the Environment, Bern. [Google Scholar]
- Foraster M, Künzli N, Aguilera I, Rivera M, Agis D, Vila J, et al. 2014. High blood pressure and long-term exposure to indoor noise and air pollution from road traffic. Environ Health Perspect 122(11):1193–1200, PMID: 25003348, 10.1289/ehp.1307156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franklin SS, Gustin W, Wong ND, Larson MG, Weber MA, Kannel WB, et al. 1997. Hemodynamic patterns of age-related changes in blood pressure. Circulation 96(1):308–315, PMID: 9236450, 10.1161/01.CIR.96.1.308. [DOI] [PubMed] [Google Scholar]
- Halonen JI, Dehbi H-M, Hansell AL, Gulliver J, Fecht D, Blangiardo M, et al. 2017. Associations of night-time road traffic noise with carotid intima-media thickness and blood pressure: the Whitehall II and SABRE study cohorts. Environ Int 98:54–61, PMID: 27712935, 10.1016/j.envint.2016.09.023. [DOI] [PubMed] [Google Scholar]
- Heutschi K. 2004. SonRoad: New Swiss Road Traffic Noise Model. Acta Acust. United Acust 90:548–554. [Google Scholar]
- Johns MW. 1991. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14(6):540–545, PMID: 1798888, 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- Karipidis I, Vienneau D, Habermacher M, Köpfli M, Brink M, Probst-Hensch N, et al. 2014. Reconstruction of historical noise exposure data for environmental epidemiology in Switzerland within the SiRENE project. Noise Mapp 1(1):3–14, 10.2478/noise-2014-0002. [DOI] [Google Scholar]
- Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. 2012. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859):2095–2128, PMID: 23245604, 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin BW, Ackermann-Liebrich U, Leuenberger P, Künzli N, Stutz EZ, Keller R, et al. 1997. SAPALDIA: methods and participation in the cross-sectional part of the Swiss Study on Air Pollution and Lung Diseases in Adults. Soz Praventivmed 42(2):67–84, PMID: 9151378, 10.1007/BF01318136. [DOI] [PubMed] [Google Scholar]
- Méline J, Van Hulst A, Thomas F, Chaix B. 2015. Road, rail, and air transportation noise in residential and workplace neighborhoods and blood pressure (RECORD Study). Noise Health 17(78):308–319, PMID: 26356373, 10.4103/1463-1741.165054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Münzel T, Gori T, Babisch W, Basner M. 2014. Cardiovascular effects of environmental noise exposure. Eur Heart J 35(13):829–836, PMID: 24616334, 10.1093/eurheartj/ehu030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Münzel T, Sørensen M, Gori T, Schmidt FP, Rao X, Brook FR, et al. 2016. Environmental stressors and cardio-metabolic disease: Part II–mechanistic insights. Eur Heart J 38(8):557–564, PMID: 27460891, 10.1093/eurheartj/ehw294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray CJL, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, et al. 2012. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet 380(9859):2197–2223, PMID: 23245608, 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- Panczak R, Galobardes B, Voorpostel M, Spoerri A, Zwahlen M, Egger M, et al. 2012. A Swiss neighbourhood index of socioeconomic position: development and association with mortality. J Epidemiol Community Health 66(12):1129–1136, PMID: 22717282, 10.1136/jech-2011-200699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves J, Hill MN, et al. 2005. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation 111(5):697–716, PMID: 15699287, 10.1161/01.CIR.0000154900.76284.F6. [DOI] [PubMed] [Google Scholar]
- Recio A, Linares C, Banegas JR, Díaz J. 2016. Road traffic noise effects on cardiovascular, respiratory, and metabolic health: An integrative model of biological mechanisms. Environ Res 146:359–370, PMID: 26803214, 10.1016/j.envres.2015.12.036. [DOI] [PubMed] [Google Scholar]
- Schmidt FP, Basner M, Kröger G, Weck S, Schnorbus B, Muttray A, et al. 2013. Effect of nighttime aircraft noise exposure on endothelial function and stress hormone release in healthy adults. Eur Heart J 34(45):3508–3514, PMID: 23821397, 10.1093/eurheartj/eht269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seidler A, Wagner M, Schubert M, Dröge P, Pons-Kühnemann J, Swart E, et al. 2016a. Myocardial infarction risk due to aircraft, road, and rail traffic noise. Dtsch Arztebl Int 113(24):407–414, PMID: 27380755, 10.3238/arztebl.2016.0407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seidler A, Wagner M, Schubert M, Dröge P, Römer K, Pons-Kühnemann J, et al. 2016b. Aircraft, road and railway traffic noise as risk factors for heart failure and hypertensive heart disease—a case-control study based on secondary data. Int. J Hyg. Environ. Health 219:749–758, 10.1016/j.ijheh.2016.09.012. [DOI] [PubMed] [Google Scholar]
- Sørensen M, Hvidberg M, Hoffmann B, Andersen ZJ, Nordsborg RB, Lillelund KG, et al. 2011. Exposure to road traffic and railway noise and associations with blood pressure and self-reported hypertension: a cohort study. Environ Health 10:92, PMID: 22034939, 10.1186/1476-069X-10-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tétreault L-F, Perron S, Smargiassi A. 2013. Cardiovascular health, traffic-related air pollution and noise: are associations mutually confounded? A systematic review. Int J Public Health 58(5):649–666, PMID: 23887610, 10.1007/s00038-013-0489-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thron T, Hecht M. 2010. The sonRAIL emission model for railway noise in Switzerland. Acta Acust. United Acust 96:873–883, 10.3813/AAA.918346. [DOI] [Google Scholar]
- van Kempen E, Babisch W. 2012. The quantitative relationship between road traffic noise and hypertension: a meta-analysis. J Hypertens 30(6):1075–1086, PMID: 22473017, 10.1097/HJH.0b013e328352ac54. [DOI] [PubMed] [Google Scholar]
- Vienneau D, Schindler C, Perez L, Probst-Hensch N, Röösli M. 2015. The relationship between transportation noise exposure and ischemic heart disease: a meta-analysis. Environ Res 138:372–380, PMID: 25769126, 10.1016/j.envres.2015.02.023. [DOI] [PubMed] [Google Scholar]
- Vlachopoulos C, Xaplanteris P, Aboyans V, Brodmann M, Cífková R, Cosentino F, et al. 2015. The role of vascular biomarkers for primary and secondary prevention. A position paper from the European Society of Cardiology Working Group on peripheral circulation. Atherosclerosis 241(2):507–532, PMID: 26117398, 10.1016/j.atherosclerosis.2015.05.007. [DOI] [PubMed] [Google Scholar]
- Vlachopoulos C, Aznaouridis K, Terentes-Printzios D, Ioakeimidis N, Stefanadis C. 2012. Prediction of cardiovascular events and all-cause mortality with brachial-ankle elasticity index: a systematic review and meta-analysis. Hypertension 60(2):556–562, PMID: 22733468, 10.1161/HYPERTENSIONAHA.112.194779. [DOI] [PubMed] [Google Scholar]
- Weinstein ND. 1978. Individual differences in reactions to noise: a longitudinal study in a college dormitory. J Appl Psychol 63(4):458–466, PMID: 701213, 10.1037/0021-9010.63.4.458. [DOI] [PubMed] [Google Scholar]
- Weinstein ND. 1980. Individual differences in critical tendencies and noise annoyance. J Sound Vib 68:241–248, 10.1016/0022-460X(80)90468-X. [DOI] [Google Scholar]
- WHO (World Health Organization). 2010. Global Recommendations on Physical Activity for Health. Geneva, Switzerland:WHO. [PubMed] [Google Scholar]
- Wunderli JM, Pieren R, Habermacher M, Vienneau D, Cajochen C, Probst-Hensch N, et al. 2016. Intermittency ratio: a metric reflecting short-term temporal variations of transportation noise exposure. J Expo Sci Environ Epidemiol 26(6):575–585, PMID: 26350982, 10.1038/jes.2015.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zieman SJ, Melenovsky V, Kass DA. 2005. Mechanisms, pathophysiology, and therapy of arterial stiffness. Arterioscler Thromb Vasc Biol 25(5):932–943, PMID: 15731494, 10.1161/01.ATV.0000160548.78317.29. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.