Abstract
The purpose of this study is to explore the associations between polypharmacy and multimorbidity using conventional and novel measures of polypharmacy. In this cross-sectional study, data on fee-for-service (FFS) Medicaid enrollees with at least 1 chronic condition and aged 18–64 years (N = 38,329) were derived from the 2010 Medicaid Analytic eXtract (MAX) files of Maryland and West Virginia. Polypharmacy, by the authors' novel definition, was determined as simultaneous use of ≥5 drugs for a consecutive period of 60 days. Multimorbidity was defined as having ≥2 chronic conditions based on the US Department of Health and Human Services framework. The association between multimorbidity and polypharmacy was examined with chi-square tests and logistic regression. Polypharmacy prevalence was estimated at 50.9% using the novel definition, as compared to 16.7% and 64.9% for the 2 commonly used conventional measures, respectively. For all 3 definitions, individuals with multimorbidity were more likely to have polypharmacy than those without multimorbidity (P < 0.001). The authors also consistently found, using all definitions, that those who were older, female, white, and eligible for Medicaid because of cash assistance were more likely to have polypharmacy (all P < 0.001). Polypharmacy was highly prevalent and significantly associated with multimorbidity among Medicaid FFS enrollees irrespective of the definitions used. The new measure may provide a more comprehensive and accurate estimation of polypharmacy than the conventional measures. These findings suggest the need for a paradigm shift from disease-specific care to patient-centered collaborative care to manage patients with multimorbidity and polypharmacy.
Keywords: : Medicaid, polypharmacy, multimorbidity, multiple chronic conditions
Introduction
Polypharmacy, referred to as the concurrent use of multiple drugs, is an economic and public health issue that is related to the quality and efficiency of health care.1 Polypharmacy often needs to be considered in the context of multimorbidity, defined as the presence of ≥2 chronic diseases,2 to justify its appropriateness.3 A patient with multimorbidity very likely will receive multiple drugs from multiple prescribers. Current evidence-based clinical practice primarily follows single disease-specific treatment and prevention guidelines; however, this kind of practice paradigm may sometimes be detrimental and impractical for patients with multimorbidity.4,5 For example, in Boyd et al, if all recommendations from the clinical practice guideline of each disease were followed, a hypothetical 79-year-old patient with diabetes, hypertension, osteoporosis, osteoarthritis, and chronic obstructive pulmonary disease (COPD) would take 12 separate drugs at 5 times comprising almost 19 doses a day, which also raises issues such as drug-drug interactions and even contraindications.6 Therefore, though not all polypharmacy is inappropriate in the clinical context, often it still is associated with negative consequences, including harmful drug-drug interactions, hospital readmissions, and frequent emergency department visits.7,8
Historically, these issues were studied mostly in the elderly; recent studies suggest that multimorbidity and polypharmacy may extend to a more general population. According to Ornstein et al,9 the prevalence of multimorbidity in the United States is about 40% by age 50, and increases to 66% in the group who are ages 55–64. A geographic information system analysis of the prevalence of polypharmacy in Italy found that geographical differences were better explained by the distribution of the epidemiology of diseases and patients' health than by age.10 However, very few studies have examined this relationship in the non-elderly population. In addition, the Medicaid population, who are generally non-elderly with limited income and resources, may be more vulnerable to certain negative health outcomes including multimorbidity,11 which may lead to a high prevalence of polypharmacy as well. Exploring polypharmacy prevalence and patterns in different chronic conditions or combinations may suggest targets for future efforts to prevent negative consequences associated with polypharmacy and inappropriate use of medications in this population.
On the other hand, previous literature has not established a standard definition or measurement of polypharmacy, which leads to heterogeneous measurements of polypharmacy prevalence and outcomes across studies. In particular, there is no comprehensive operational definition of polypharmacy for research using administrative claims data, a method that is cost-effective and reflective of real-world clinical practice. An Italian study assessing geographic differences in polypharmacy defined polypharmacy as “the administration of five or more drugs during 1 month for at least 6 months (consecutive or not) in a year.”10 Moriarty et al's study on polypharmacy trends in Ireland defined polypharmacy as ≥5 regular medications in 1 year.5 These definitions used in claims data studies have taken into consideration the number of drugs used and duration of use, but another important aspect of polypharmacy is missing — the simultaneous use of drugs. Simultaneous polypharmacy, determined as the sum of drugs used concurrently on any given day, can provide comprehensive information on patients' medication use and detect transient changes in use, although more information and computation may be required to measure it.1,12
Therefore, the present study integrated the simultaneous polypharmacy approach established by Fincke et al that considers the number of drugs and duration of medication use to develop a novel operational definition for polypharmacy,12 which can be applied when using pharmacy claims data. The aim is to evaluate the association between multimorbidity and polypharmacy by both the novel and commonly-used conventional definitions of polypharmacy, using the West Virginia (WV) and Maryland (MD) Medicaid fee-for-service (FFS) claims data.
Methods
Study design, study population, and data source
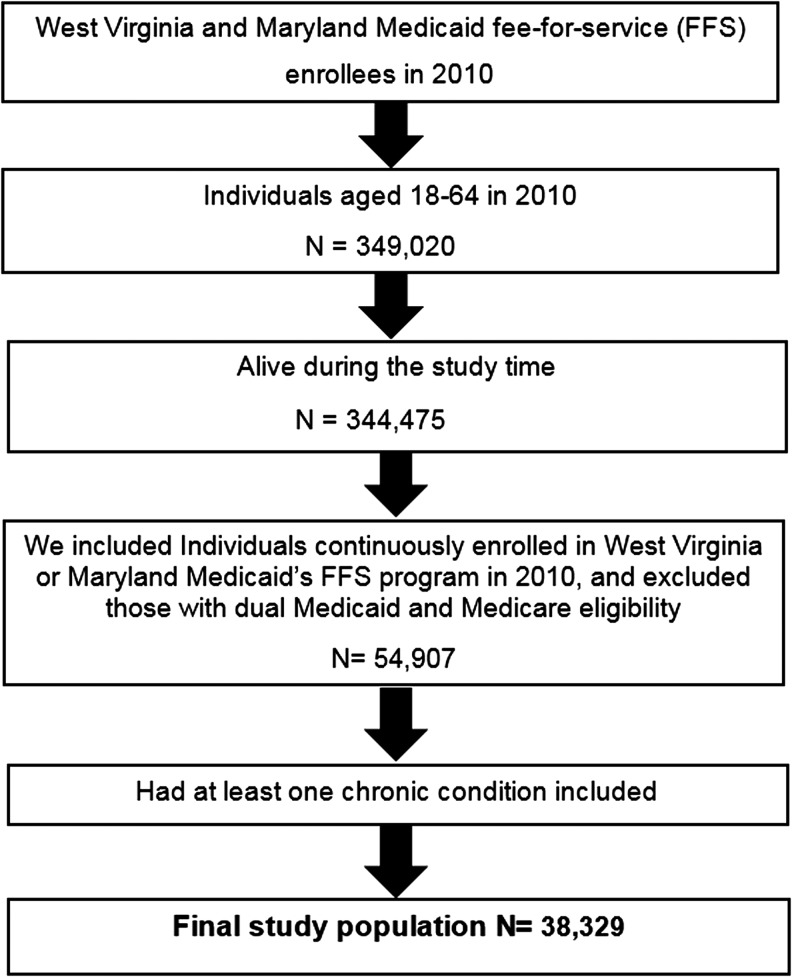
The research team conducted a cross-sectional study in 2010 using Medicaid Analytic eXtract (MAX) files. The data source was 2010 MAX data system for WV and MD. The team used person summary files to obtain demographic and enrollment data, inpatient files to identify hospital claims, prescription drug files for pharmacy claims, and other services files to identify the diagnosis codes from outpatient visits and other services. The team included adults who were alive and aged 18 to 64 in 2010, continuously enrolled in WV or MD Medicaid's FFS program, not eligible for Medicare, and with at least 1 of the chronic conditions based on the US Department of Health and Human Services (DHHS) framework,13 which included hypertension, congestive heart failure (CHF), coronary artery disease, cardiac arrhythmias, hyperlipidemia, stroke, arthritis, asthma, cancer, chronic kidney disease (CKD), COPD, dementia, depression, diabetes, hepatitis, HIV, osteoporosis, schizophrenia, and substance abuse disorders. Figure 1 shows the flowchart for obtaining the final study population. The study was approved by West Virginia University's Institutional Review Board (protocol number: 1511901393).
FIG. 1.
Flowchart for obtaining the final study population.
Measures
Dependent variable: polypharmacy
Definition 1 (New definition): polypharmacy was defined as the simultaneous use of ≥5 different drug classes for a 60-day consecutive period. First, the research team identified drugs using the national drug codes and categorized them into therapeutic drug classes. Second, to measure the simultaneous use of drugs, the team extracted pharmacy claims, including information on prescription fill date and days of supply, and established separate data sets of pharmacy claims for each drug class. For each drug class data set, the team created a patient-level matrix marking all dates with the particular drug class taken. Then for each individual, all matrixes were merged together to obtain a final matrix that described the daily use of drug classes in the follow-up period. Third, to determine polypharmacy, the team marked the dates with ≥5 different drug classes for each patient on the final matrix. Then a 60-day consecutive period was chosen to indicate continuous use of drugs. In light of potential issues related to patient nonadherence to medications,12 the research team also allowed a gap in the consecutive period window. Given the widely-used cutoff point of 0.8 in medication adherence research using claims data, a 12-day gap was allowed in the consecutive use period. Therefore, polypharmacy was defined as an instance in which an individual took drugs from ≥5 different drug classes per day for at least 60 days out of 72 consecutive days in 2010.
The research team also applied the following 2 commonly-used, conventional definitions of polypharmacy in the previous literature:
Definition 2 (conventional definition): polypharmacy was referred to the average number of drug classes that was 1 standard deviation above the mean in a 90-day period.8,14,15
Definition 3 (conventional definition): polypharmacy was determined as >5 different drug classes used in an arbitrary 90-day period.16
Independent variable: multimorbidity
Multimorbidity was defined as the coexistence of ≥2 chronic conditions. These were identified in the medical claims using the International Classification of Diseases, Ninth Revision, Clinical Modification. The selection of chronic conditions was based on the DHHS framework.13
Covariates
Other covariates included age group (18–34, 35–44, 45–54, 55–64), sex (female, male), race (white, nonwhite), and Medicaid pathway to eligibility (cash assistance, other).
Statistical analyses
The research team presents descriptive statistics of total Medicaid enrollees and patients with polypharmacy by each definition with frequencies and percentages. The team compared the most prevalent combinations of comorbidities as well as polypharmacy prevalence by the novel and 2 conventional definitions. The bivariate association between polypharmacy and multimorbidity was assessed by chi-square tests. Multivariate logistic regression also was used to further examine the relationship between polypharmacy and multimorbidity after adjusting for other covariates. Analyses were conducted using SAS 9.4 (SAS Institute Inc., Cary, NC) and R 3.2.2 (R Foundation for Statistical Computing, Vienna, Austria).
Results
This study included a total of 38,329 Medicaid FFS enrollees, with 90.4% from WV and 9.6% from MD (Table 1). Most of the study subjects were female, white, and middle-aged (45–64 years old, 65.3%). Approximately 65% of the Medicaid population in this study had multimorbidity with the presence of ≥2 chronic conditions. The majority of patients with polypharmacy, regardless of definition, were female, older than 45 years of age, with cash assistance, from WV, and had multimorbidity.
Table 1.
Descriptive Statistics of 2010 Fee-for-Service Medicaid Enrollees in West Virginia and Maryland (n = 38,329)
| Polypharmacy patients, n (%)a | ||||
|---|---|---|---|---|
| Variables | All eligible patients, n (%) | Definition 1 | Definition 2 | Definition 3 |
| 38,329 (100) | 19,500 (50.9) | 6404 (16.7) | 24,882 (64.9) | |
| Sex | ||||
| Male | 15,636 (40.8) | 6937 (35.6) | 1568 (24.5) | 8670 (34.8) |
| Female | 22,693 (59.2) | 12,563 (64.4) | 4836 (75.5) | 16,212 (65.2) |
| Age group, years | ||||
| 18–34 | 6358 (16.6) | 1442 (7.4) | 273 (4.3) | 2533 (10.2) |
| 35–44 | 6945 (18.1) | 3012 (15.5) | 859 (13.4) | 4219 (17.0) |
| 45–54 | 13,121 (34.2) | 7335 (37.6) | 2425 (37.9) | 9193 (37.0) |
| 55–64 | 11,905 (31.1) | 7711 (39.5) | 2847 (44.5) | 8937 (35.9) |
| Race | ||||
| White | 34,706 (90.6) | 18,054 (92.6) | 6049 (94.5) | 22,971 (92.3) |
| Nonwhite | 3623 (9.5) | 1446 (7.4) | 355 (5.5) | 1911 (7.7) |
| State | ||||
| West Virginia | 34,662 (90.4) | 18,078 (92.7) | 6072 (94.8) | 23,037 (92.6) |
| Maryland | 3667 (9.6) | 1422 (7.3) | 332 (5.2) | 1845 (7.4) |
| Medicaid pathway to eligibility | ||||
| Cash eligibility | 31,451 (82.1) | 16,599 (85.1) | 5659 (88.4) | 20,882 (83.9) |
| Others | 6878 (17.9) | 2901 (14.9) | 745 (11.6) | 4000 (16.1) |
| No. of chronic conditionsb | ||||
| 1 chronic condition | 13,624 (35.5) | 3574 (18.3) | 493 (7.7) | 5392 (21.7) |
| 2 chronic conditions | 9891 (25.8) | 4979 (25.5) | 1046 (16.3) | 6577 (26.4) |
| 3 chronic conditions | 6705 (17.5) | 4445 (22.8) | 1390 (21.7) | 5463 (22.0) |
| ≥4 chronic conditions | 8109 (21.2) | 6502 (33.3) | 3475 (54.3) | 7450 (29.9) |
Definition-1 (new polypharmacy definition) is the simultaneous use of ≥5 different drug classes for a 60-day consecutive period; Definition-2 is the average number of drug classes that was 1 standard deviation above the mean in a 90-day period; Definition-3 is >5 different drug classes used in an arbitrary 90-day period.
Chronic conditions included in the list were: hypertension, congestive heart failure, coronary artery disease, cardiac arrhythmias, hyperlipidemia, stroke, arthritis, asthma, cancer, chronic kidney disease, chronic obstructive pulmonary disease, dementia, depression, diabetes, hepatitis, HIV, osteoporosis, schizophrenia, and substance abuse disorders.
In the study Medicaid population, the prevalence of polypharmacy identified by definition-1 (new definition) was 50.9%; prevalence rates determined by conventional definition-2 and definition-3 were 16.7% and 64.9%, respectively (Table 1). The new definition identified 99.2% of polypharmacy determined by commonly-used definition-2; approximately 58.8% of non-polypharmacy cases in definition-2 also were negative cases according to the new definition (Table 2). Similarly, when the new definition and conventional definition-3 were compared, the 2 statistics were 76.6% and 96.6%, respectively. These indicated fair to good agreement between the novel and conventional measures.
Table 2.
Comparisons of Polypharmacy Prevalence by Different Polypharmacy Definitions (n = 38,329)
| Definition 1 (novel definition) | |||
|---|---|---|---|
| Yes, n (%) | No, n (%) | P | |
| Definition 2 | <0.0001 | ||
| Yes | 6355 (99.2) | 49 (0.8) | |
| No | 13145 (41.2) | 18780 (58.8) | |
| Definition 3 | |||
| Yes | 19,048 (76.6) | 5834 (23.4) | <0.0001 |
| No | 452 (3.4) | 12,995 (96.6) | |
Definition-1 (new polypharmacy definition) is the simultaneous use of ≥5 different drug classes for a 60-day consecutive period; Definition-2 is the average number of drug classes that was 1 standard deviation above the mean in a 90-day period; Definition-3 is >5 different drug classes used in an arbitrary 90-day period.
The most prevalent comorbidity combinations (2 coexisting conditions) in this population were hypertension and hyperlipidemia (19.4%), following by hypertension and diabetes, and hypertension and depression (Table 3). They also were the most prevalent combinations among patients with polypharmacy, regardless of the definition used (Table 3). The comorbidity combinations (2 coexisting conditions) with the highest polypharmacy rate were CHF with osteoporosis for the new definition, CKD with COPD for definition-2, and CKD with osteoporosis for the definition-3 (data not shown). Throughout all definitions, patients with comorbidity combinations such as CKD with osteoporosis, CHF with osteoporosis, CKD with arthritis, and CHF with arthritis had particularly high prevalence of polypharmacy.
Table 3.
Most Prevalent Dual Comorbidities and the Dual Comorbidities with Top Polypharmacy Rate
| Most prevalent dual comorbidities among the total enrollees and polypharmacy patients | ||||||||
|---|---|---|---|---|---|---|---|---|
| Total | Polypharmacy | |||||||
| Rank | n (%) | Definition 1 | n (%) | Definition 2 | n (%) | Definition 3 | n (%) | |
| 1 | Hypertension + hyperlipidemia | 7453 (19.4) | Hypertension + diabetes | 5664 (29.1) | Hypertension + diabetes | 2746 (42.9) | Hypertension + diabetes | 6407 (25.8) |
| 2 | Hypertension + diabetes | 7210 (18.8) | Hypertension + hyperlipidemia | 5598 (28.7) | Hypertension + hyperlipidemia | 2345 (36.6) | Hypertension + hyperlipidemia | 6402 (25.7) |
| 3 | Hypertension + depression | 5263 (13.7) | Hypertension + depression | 3957 (20.3) | Hypertension + COPD | 1910 (29.8) | Hypertension + depression | 4662 (18.7) |
| 4 | Diabetes + hyperlipidemia | 4848 (12.7) | Diabetes + hyperlipidemia | 3832 (19.7) | Hypertension + depression | 1906 (29.8) | Diabetes + hyperlipidemia | 4322 (17.4) |
| 5 | Hypertension + COPD | 4406 (11.5) | Hypertension + COPD | 3452 (17.7) | Diabetes + hyperlipidemia | 1865 (29.1) | Hypertension + COPD | 3988 (16.0) |
Definition-1 (new polypharmacy definition) is the simultaneous use of ≥5 different drug classes for a 60-day consecutive period; Definition-2 is the average number of drug classes that was 1 standard deviation above the mean in a 90-day period; Definition-3 is >5 different drug classes used in an arbitrary 90-day period.
COPD, chronic obstructive pulmonary disease.
Univariate analysis results show that individuals with a greater number of chronic conditions had higher rates of polypharmacy under all 3 definitions (all P < 0.001) (data not shown). The significantly positive relationship between polypharmacy and multimorbidity also was demonstrated in the multivariable logistic models (Table 4). The likelihood of polypharmacy, regardless of definition, increased with the number of chronic conditions (all P < 0.001). The research team also consistently found, using all definitions, that those who were older, female, white, and eligible for Medicaid because of cash assistance were more likely to have polypharmacy (all P < 0.001).
Table 4.
Multivariate Logistic Regression of the Association Between Polypharmacy and Multimorbidity Among Medicaid Enrollees (n = 38,329)
| Polypharmacy | |||
|---|---|---|---|
| Definition 1 | Definition 2 | Definition 3 | |
| AOR (95% CI) | AOR (95% CI) | AOR (95% CI) | |
| Multimorbidity | |||
| 2 conditions vs. 1 | 2.47 (2.33–2.61) | 2.73 (2.44–3.05) | 2.78 (2.63–2.94) |
| 3 conditions vs. 1 | 4.59 (4.30–4.90) | 5.84 (5.24–6.52) | 6.07 (5.64–6.53) |
| ≥4 conditions vs. 1 | 8.88 (8.28–9.51) | 16.49 (14.87–18.29) | 14.93 (13.65–16.34) |
| Age group | |||
| 35–44 vs. 18–34 | 1.93 (1.78–2.10) | 1.92 (1.65–2.23) | 1.68 (1.55–1.81) |
| 45–54 vs. 18–34 | 2.70 (2.51–2.90) | 2.40 (2.09–2.75) | 2.07 (1.93–2.22) |
| 55–64 vs. 18–34 | 3.31 (3.07–3.58) | 2.69 (2.35–3.09) | 2.12 (1.97–2.28) |
| Sex (female vs. male) | 1.41 (1.35–1.48) | 2.29 (2.14–2.45) | 1.96 (1.87–2.06) |
| Race (White vs. Nonwhite) | 1.80 (1.66–1.95) | 2.13 (1.88–2.41) | 1.97 (1.81–2.14) |
| Medicaid pathway-to-eligibility (cash eligibility vs. others) | 1.40 (1.32–1.49) | 1.64 (1.51–1.81) | 1.30 (1.22–1.38) |
Definition-1 (new definition) is the simultaneous use of ≥5 different drug classes for a 60-day consecutive period; Definition-2 is the average number of drug classes that was 1 standard deviation above the mean in a 90-day period; Definition-3 is >5 different drug classes used in an arbitrary 90-day period.
AOR, adjusted odds ratio; CI, confidence interval.
Discussion
Most current definitions of polypharmacy used in research with claims data are limited because they do not account for daily use of multiple medications. By incorporating 3 important components used to define polypharmacy –number of drugs, simultaneous use of drugs on a daily base, and duration of use – the research team developed a novel measure to assess polypharmacy using Medicaid claims data. Using this definition, the team found that polypharmacy was highly prevalent (50.9%) in WV and MD Medicaid populations who have at least 1 chronic condition, and was significantly associated with multimorbidity, implying considerable burdens of polypharmacy and multimorbidity among the Medicaid population in these 2 states.
The new and old measures were broadly concordant. The new measure identified more than 99% or 76.6% of polypharmacy cases defined by 2 conventional measures; approximately 59% or 97% of the non-polypharmacy patients by the 2 measures also were negative cases as determined by the new definition. This suggests good agreement between the novel and conventional measures. Additionally, the positive relationship between polypharmacy and multimorbidity was corroborated by the univariate and multivariate analyses using all measures.
Nevertheless, compared to the conventional measures, the new measure provides a clearer and more comprehensive view of polypharmacy. Incorporating daily drug use and other important components into the new definition provides a more accurate estimation of polypharmacy burden and can capture transient and longitudinal changes, which can help us to better understand the antecedents and consequences associated with polypharmacy issues. The new measure also is flexible and feasible to use with claims data, as it can be applied to different levels of drug classes, number of drug classes, and assessment periods.
The analyses showed that polypharmacy was not only positively associated with number of chronic conditions in the Medicaid population, but also varied among different disease combinations. It was found that patients with CKD and musculoskeletal conditions as well as CHF and musculoskeletal conditions had considerable polypharmacy burdens. First, patients with CKD with or without other conditions may be particularly at risk of polypharmacy. Multimorbidity and multiple drug use may contribute to the physiological decline in renal function.17 As renal function deteriorates, it is necessary to add more drugs to manage the complications or comorbidities including cardiometabolic conditions, musculoskeletal conditions, and anemia,17,18 which further complicate medication regimens.19,20 For patients with CHF, multimorbidity also is exceedingly common across all ages, which leads to overwhelmingly significant burdens from the diseases and treatments with high complexity.21,22 It has even been suggested that nonpharmacological treatments be prioritized and polypharmacy reduced to alleviate the treatment burden in patients with CHF.22 In terms of musculoskeletal conditions such as arthritis, the management of the disease itself demands multiple drugs such as analgesics, anti-inflammatory drugs, corticosteroids, or biologics, as well as other drugs to treat comorbidities. Therefore, the literature has often documented a high prevalence of polypharmacy in patients with CKD and musculoskeletal conditions.23–26 Nevertheless, future research may be warranted to further examine the differences in polypharmacy and inappropriate medication use across various types of chronic conditions or combinations among different populations.
The present study had several limitations. First, the cross-sectional study design limits the ability to establish causality in the findings. Second, the main therapeutic drug classes were used to measure polypharmacy instead of the single active ingredient; therefore, this study is only able to estimate polypharmacy from different drug classes but not within the drug classes. This may lead to underestimation of polypharmacy rates, but the measurement may be more feasible to implement with claims data given the tremendous amount of data and computation challenges. Third, measurement of polypharmacy did not fully address early refill issues. But allowing for a 12-day gap in the calculation might mitigate this potential issue to some extent. Fourth, the data source had limited ability to capture patients' actual medication-taking behavior, over-the-counter medications, accurate drug indications, and disease severity, which may influence either the accuracy of estimation or the differentiation between appropriate and inappropriate polypharmacy. Fifth, only 19 chronic conditions were included in the analyses, which also may result in the underestimation of multimorbidity in the study population. Lastly, the population was adult Medicaid FFS program enrollees in WV and MD in 2010; thus, the findings may not be generalizable to populations in other regions or with other health care plans, or may not reflect the most updated situation in the study population.
Despite the limitations, the study findings have implications for researchers, clinicians, and policy makers. This study found that even in the Medicaid population, a majority of whom are not elderly, multimorbidity and polypharmacy are prevalent and highly correlated. There is limited clinical evidence or guidelines for multimorbidity,4 and most clinical trials exclude patients with multimorbidity and polypharmacy.27 Furthermore, physicians tend to adhere to single-disease guidelines when prescribing medications as recommended.28,29 Therefore, there is a need for more evidence on managing patients with multimorbidity and polypharmacy, which can lead to more comprehensive guidelines for these high-risk patients. Moreover, in a system such as FFS, which lacks financial incentives for care coordination, a patient with multimorbidity very likely will receive multiple medications from multiple prescribers without adequate review or monitoring of medications.16 Interventions or policies directed at reducing inappropriate polypharmacy must consider fostering collaboration among different health care professionals to review and monitor all medications taken to ensure the appropriateness and safety of drugs with the support of a sustainable financial model. The new definition of polypharmacy presented here may provide a feasible and cost-effective way to use claims data to identify targeted populations such as those with polypharmacy or multimorbidity, and those using high-risk drugs or drug combinations, ultimately achieving the goal of reducing preventable medication-related harm to patients as well as associated excessive costs.
Conclusion
In this study, polypharmacy was highly prevalent and significantly associated with multimorbidity among Medicaid FFS enrollees, irrespective of the definition used. The new measure developed to be applied to claims data may provide a more comprehensive and accurate estimation of polypharmacy compared to conventional measures. Patients with certain chronic conditions or combinations, such as a chronic kidney condition or heart failure with musculoskeletal conditions, may be at higher risk of polypharmacy. This study's findings suggest the need for a paradigm shift from disease-specific care to patient-centered collaborative care to manage patients with multimorbidity and polypharmacy.
Author Disclosure Statement
All authors declared that there are no conflicts of interest. The project described was supported by the West Virginia University–Marshall University Health Grants Partnership. The content is solely the responsibility of the authors and does not necessarily represent the official views of West Virginia University or Marshall University.
References
- 1.Monégat M, Sermet C, Perronnin M, Rococo E. Polypharmacy: definitions, measurement and stakes involved. Review of the literature and measurement tests. 2014. www.irdes.fr/english/issues-in-health-economics/204-polypharmacy-definitions-measurement-and-stakes-involved.pdf Accessed April5, 2017
- 2.Karlamangla A, Tinetti M, Guralnik J, Studensky S, Wetle T, Reuben D. Comorbidity in older adults: nosology of impairments, diseases, and conditions. J Gerontol 2007;62A:296–300 [DOI] [PubMed] [Google Scholar]
- 3.Cadogan CA, Ryan C, Hughes CM. Appropriate polypharmacy and medicine safety: when many is not too many. Drug Saf 2016;39:109–116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Uhlig K, Leff B, Kent D, et al. A framework for crafting clinical practice guidelines that are relevant to the care and management of people with multimorbidity. J Gen Intern Med 2014;29:670–679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moriarty F, Hardy C, Bennett K, Smith SM, Fahey T. Trends and interaction of polypharmacy and potentially inappropriate prescribing in primary care over 15 years in Ireland: a repeated cross-sectional study. BMJ Open 2015;5:e008656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance. JAMA 2005;294:716–724 [DOI] [PubMed] [Google Scholar]
- 7.Ruiz B, García M, Aguirre U, Aguirre C. Factors predicting hospital readmissions related to adverse drug reactions. Eur J Clin Pharmacol 2008;64:715–722 [DOI] [PubMed] [Google Scholar]
- 8.Agarwal P, Bias TK, Sambamoorthi U. Longitudinal patterns of emergency department visits: a multistate analysis of Medicaid beneficiaries. Health Serv Res 2016. [Epub ahead of print]; DOI: 10.1111/1475-6773.12584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ornstein SM, Nietert PJ, Jenkins RG, Litvin CB. The prevalence of chronic diseases and multimorbidity in primary care practice: a PPRNet report. J Am Board Fam Med 2013;26:518–524 [DOI] [PubMed] [Google Scholar]
- 10.Franchi C, Cartabia M, Risso P, et al. Geographical differences in the prevalence of chronic polypharmacy in older people: eleven years of the EPIFARM-Elderly Project. Eur J Clin Pharmacol 2013;69:1477–1483 [DOI] [PubMed] [Google Scholar]
- 11.Agborsangaya CB, Lau D, Lahtinen M, Cooke T, Johnson JA. Multimorbidity prevalence and patterns across socioeconomic determinants: a cross-sectional survey. BMC Public Health 2012;12:201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fincke BG, Snyder K, Cantillon C, et al. Three complementary definitions of polypharmacy: methods, application and comparison of findings in a large prescription database. Pharmacoepidemiol Drug Saf 2005;14:121–128 [DOI] [PubMed] [Google Scholar]
- 13.Goodman RA, Posner SF, Huang ES, Parekh AK, Koh HK. Defining and measuring chronic conditions: imperatives for research, policy, program, and practice. Prev Chronic Dis 2013;10:120239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goldberg JF, Brooks JO, 3rd, Kurita K, et al. Depressive illness burden associated with complex polypharmacy in patients with bipolar disorder: findings from the STEP-BD. J Clin Psychiatry 2009;70:155–162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bhattacharya R, Zhou S, Wei W, Ajmera M, Sambamoorthi U. A real‐world study of the effect of timing of insulin initiation on outcomes in older Medicare beneficiaries with type 2 diabetes mellitus. J Am Geriatr Soc 2015;63:893–901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vyas A, Pan X, Sambamoorthi U. Chronic condition clusters and polypharmacy among adults. Int J Fam Med 2012;2012:193168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sutaria A, Liu L, Ahmed Z. Multiple medication (polypharmacy) and chronic kidney disease in patients aged 60 and older: a pharmacoepidemiologic perspective. Ther Adv Cardiovasc Dis 2016;10:242–250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mason NA. Polypharmacy and medication related complications in the chronic kidney disease patient. Curr Opin Nephrol Hypertens 2011;20:492–497 [DOI] [PubMed] [Google Scholar]
- 19.Ponticelli C, Sala G, Glassock RJ. Drug management in the elderly adult with chronic kidney disease: a review for the primary care physician. Mayo Clin Proc 2015;90:633–645 [DOI] [PubMed] [Google Scholar]
- 20.Reese PP, Cappola AR, Shults J, et al. Physical performance and frailty in chronic kidney disease. Am J Nephrol 2013;38:307–315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wong CY, Chaudhry SI, Desai MM, Krumholz HM. Trends in comorbidity, disability, and polypharmacy in heart failure. Am J Med 2011;124:136–143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dharmarajan K, Dunlay SM. Multimorbidity in older adults with heart failure. Clin Geriatr Med 2016;32:277–289 [DOI] [PubMed] [Google Scholar]
- 23.Chakraborty S, Ghosh S, Banerjea A, De RR, Hazra A, Mandal SK. Prescribing patterns of medicines in chronic kidney disease patients on maintenance hemodialysis. Indian J Pharmacol 2016;48:586–590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Meraya AM, Dwibedi N, Sambamoorthi U. Polypharmacy and health-related quality of life among US adults with arthritis, Medical Expenditure Panel Survey, 2010–2012. Prev Chronic Dis 2016;13:E132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Treharne GJ, Douglas KM, Iwaszko J, et al. Polypharmacy among people with rheumatoid arthritis: the role of age, disease duration and comorbidity. Musculoskeletal Care 2007;5:175–190 [DOI] [PubMed] [Google Scholar]
- 26.Wallace JL. Polypharmacy of osteoarthritis: the perfect intestinal storm. Dig Dis Sci 2013;58:3088–3093 [DOI] [PubMed] [Google Scholar]
- 27.Van Spall HG, Toren A, Kiss A, Fowler RA. Eligibility criteria of randomized controlled trials published in high-impact general medical journals: a systematic sampling review. JAMA 2007;297:1233–1240 [DOI] [PubMed] [Google Scholar]
- 28.Veehof LJG, Meyboom-de Jong B, Haaijer-Rasamp FM. Polypharmacy in the elderly—a literature review. Eur J Gen Pract 2000;6:98–106 [Google Scholar]
- 29.Mannucci PM, Nobili A. REPOSI Investigators. Multimorbidity and polypharmacy in the elderly: lessons from REPOSI. Intern Emerg Med 2014;9:723–734 [DOI] [PubMed] [Google Scholar]