Abstract
Background: The Massachusetts Childhood Obesity Research Demonstration (MA-CORD) project is a 2-year, multilevel, multisector community intervention to prevent and control obesity among children 2–12 years of age from two predominantly low-income communities in Massachusetts. MA-CORD includes evidence-based interventions in multiple sectors, including community health centers, early care and education centers, schools, afterschool programs, the Special Supplemental Nutrition Program for Women, Infants and Children, and the broader community. Currently, implementation of MA-CORD is complete and the final year of data collection is in progress. Here, the MA-CORD evaluation plan is described and baseline data are presented.
Methods/Design: The impact of MA-CORD on children's BMI, lifestyle behaviors, obesity-related care, and quality of life will be assessed using sector-specific, pre/post, time-series, and quasi-experimental designs. Change in the primary outcomes will be compared for intervention and comparison communities. Additionally, change in mean BMI and obesity prevalence in intervention school districts will be compared to similar districts throughout the state.
Results: At baseline in 2012, approximately 16% of preschool-aged and 25% of school-aged children were obese. Moreover, 15–40% of children consumed no vegetables on the previous day, 25–75% drank a sugar-sweetened beverage on the previous day, up to 87% had insufficient physical activity, 50–75% had a television in the room where they slept, and 50–80% obtained insufficient sleep.
Conclusions: There is ample room for improvement in BMI and health behaviors in children in MA-CORD communities. If successful, MA-CORD may serve as a model for multilevel, multisector approaches to childhood obesity prevention and control.
Introduction
Childhood obesity is one of the most pressing public health challenges of the times. In response to the complex etiology of obesity, there have been repeated calls for multilevel, multisector approaches to prevention and control of obesity.1 Such approaches are expected to have broad reach, thereby increasing their economic and social impact. A small number of studies have begun to provide an evidence base for multilevel, multisector whole-community interventions,2–6 but there remains a need for empirical evidence for such approaches in diverse settings in the United States. Consequently, the CDC funded the development and implementation of the Childhood Obesity Research Demonstration (CORD) project.7
Guided by the obesity chronic care model8 and targeting predominantly low-income children ages 2–12 years, CORD is one of the first large-scale, federally funded research efforts to integrate clinical and public health evidence-based approaches to promote healthy lifestyle behaviors and reduce rates of obesity among children.7 CORD has field sites in Texas, California, and Massachusetts, with a fourth site serving as the evaluation center.9 In contrast to the model of implementing a standardized intervention across multiple sites, a novel feature of CORD is that each site is encouraged to tailor the intervention to the needs of their specific community.9 In addition, coordinated by the CORD Evaluation Center, intervention sites use a combination of site-specific and standardized cross-site measures.10
Complex community interventions for childhood obesity prevention are commonly evaluated using quasi-experimental designs with outcomes measured for consented individuals, often a select subset of the target population.2,3,6 Less common is the use of existing electronic data.4 Integrating existing data into the evaluation design has several advantages; it reduces selection bias, minimizes participant and community burden, and supports intervention sustainability through continued quality improvement.11 The Massachusetts CORD project (MA-CORD) utilizes a novel evaluation design that integrates existing data across multiple sectors and supplements this with more in-depth information from a longitudinal cohort nested within the community. This article provides an overview of the MA-CORD evaluation plan and presents baseline data for the primary outcomes.
Methods
MA-CORD Interventions and the Participating Communities
The MA-CORD intervention design is outlined in detail by Taveras and colleagues.12 The 2-year project is built on existing state-wide public health infrastructure provided by Mass in Motion. With funding from the Massachusetts Department of Public Health, Mass in Motion provided minigrants and technical assistance to cities in Massachusetts to support policy, systems, and environmental changes to promote wellness and healthy living. Additional features of Mass in Motion included an executive order requiring BMI surveillance in schools for children in grades 1, 4, 7, and 10 (beginning in 2009) and revisions to school nutrition standards. Through various sources, as many as 33 Mass in Motion programs were funded with programs covering 52 Massachusetts cities and towns, including the MA-CORD intervention and comparison communities, and reaching up to one third of the state's population. Although children may have been affected by Mass in Motion activities, the state-wide program did not focus on children. MA-CORD served to expand obesity prevention activities in select Mass in Motion communities, with an explicit focus on children 2–12 years of age.
The MA-CORD intervention communities (Fitchburg and New Bedford) were selected from the pool of Mass in Motion communities through an internal request for proposals. The comparison community, also participating in Mass in Motion, was matched as much as feasible with the intervention communities on key demographic characteristics (e.g., race/ethnicity and percentage of families at 100% poverty). To ensure that common clinical data were available for the evaluation, the intervention and comparison communities were required to have a federally qualified community health center that was willing to share clinical data with evaluators. All three communities received the same Mass in Motion annual budget ($50K) to promote policy, systems, and environmental change locally; funds provided by MA-CORD were in addition to the original Mass in Motion funds.
The two intervention communities are small- to mid-size cities (population, 40,000–100,000) with predominantly non-Hispanic white (∼68%) and sizeable Hispanic (16–21%), populations (Table 1). The comparison community is a mid-size city (population, 106,000) whose residents are predominantly non-Hispanic white (53%) or Hispanic (17%). Mean income per capita is approximately $22,000 in MA-CORD intervention and comparison communities, which is lower than the state average of $35,000. Rates of poverty (23–27%) are approximately twice the rates noted in the state as a whole (12%).
Table 1.
Pre-Intervention Characteristics of MA-CORD Intervention and Control Communities
| Sociodemographic characteristics | Massachusetts | Fitchburg | New Bedford | Comparison community |
|---|---|---|---|---|
| Total populationa | 6,436,940 | 40,514 | 94,502 | 106,519 |
| % White (any race)a | 76.1 | 68.2 | 67.9 | 52.8 |
| % Black or African American (any race)a | 6.0 | 1.1 | 5.2 | 6.0 |
| % Hispanic or Latino (any race)a | 9.6 | 21.6 | 16.7 | 17.3 |
| Average per capita incomeb | $35,485 | $22,949 | $21,343 | $23,793 |
| % Families with children whose incomes are less 100% or more of the Federal Poverty Levelb | 12.0 | 23.5 | 27.1 | 19.9 |
2010 US Census.
2008–2012 American Community Survey 5-year estimates.
MA-CORD, Massachusetts Childhood Obesity Research Demonstration project.
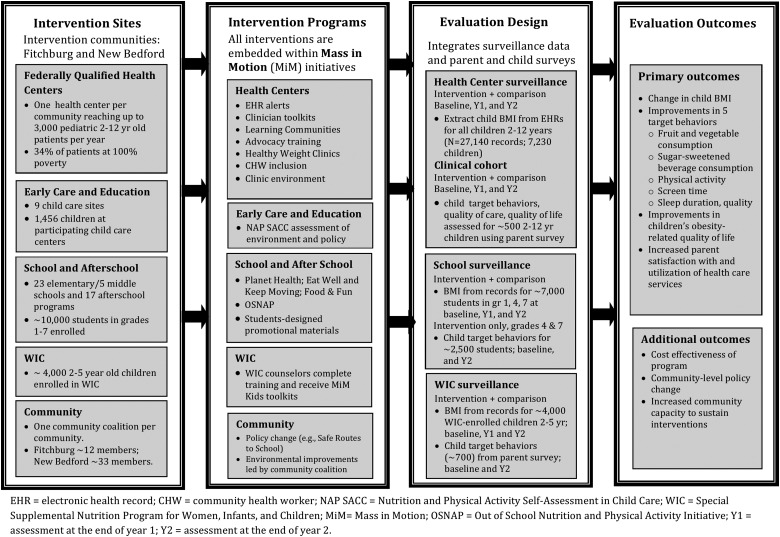
Figure 1 illustrates the key features of the MA-CORD intervention and its evaluation. Between August 2012 and August 2014, evidence-based interventions were implemented in the federally qualified health centers, early care and education (ECE) centers, public elementary and middle schools, afterschool programs, and the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) in the intervention communities.12 Intervention activities12 implemented in health centers include: (1) advanced training on clinical quality improvement and obesity prevention, assessment, and management through learning communities; (2) computerized, point-of-care decision support tools for clinicians through electronic health records (EHRs); (3) multidisciplinary weight management programs housed within the health center (i.e., healthy weight clinics); and (4) environmental changes within the health centers to support behavior change. Beyond these activities, community health workers acted as a link between primary care and other community resources.
Figure 1.
Summary of key intervention and evaluation components for the Massachusetts Childhood Obesity Research Demonstration (MA-CORD) project.
In ECECs, mentors were trained to provide support to staff to implement the Nutrition and Physical Activity Self-Assessment in Child Care protocol and establish and monitor action plans.13 In WIC clinics, nutrition counselors received intervention toolkits and were trained in behavioral counseling specific to the MA-CORD target behaviors. In all public elementary and middle schools, teachers were trained in the implementation of evidence-based obesity prevention curricula.14,15 Similar curricular, policy, and environmental changes were implemented in afterschool programs.16,17 Complementing these activities, students in schools and afterschool programs designed promotional materials—through video, posters, and song—to reflect their interpretation of the target behaviors. Finally, community-level components of MA-CORD included policy change (e.g., Safe Routes to School), improvements in the food, beverage, and PA environments achieved through activities led by a local coalition in each community (e.g., working with local restaurants and grocery stores to improve the selection of fruits and vegetables) and the coordination of messaging systems designed to provide cross-sector support for the sector-specific programs.
Evaluation Design
The evaluation of MA-CORD combines sector-specific, pre/post time-series and quasi-experimental designs, as shown in Figure 1 (column 3). With a focus on children ages 2–12 years, the primary outcomes include a reduction in mean child BMI and rates of child overweight and obesity along with five evidence-based behaviors that support obesity prevention and control in children,1 including increased consumption of fruits and vegetables and decreased consumption of sugar-sweetened beverages (SSBs), increased PA, decreased screen time, and improvements in sleep duration and quality. Additional outcomes, as specified by the grantor and outlined under the Children's Health Insurance Program Reauthorization Act of 2009, include quality of life and quality of care.7 Outcomes were measured at baseline and 1- and 2-years follow-up. In some instances, data for the primary outcomes will also be available 1–2 years preceding baseline.
A unique feature of the evaluation plan is the utilization of data from multiple surveillance systems, including EHRs, school records, and WIC records, coupled with supplemental data from families recruited through the health centers and WIC, as described below. This approach combines the strengths of internal validity gained from a within-person design with those of generalizability gained from the use of surveillance data. Because the evaluation utilizes pre-existing data systems, many of which are designed to collect data on virtually all individuals in a target population (i.e., school records and EHR), the risk of bias from selective nonparticipation is reduced. In addition, this approach minimizes respondent and community burden.
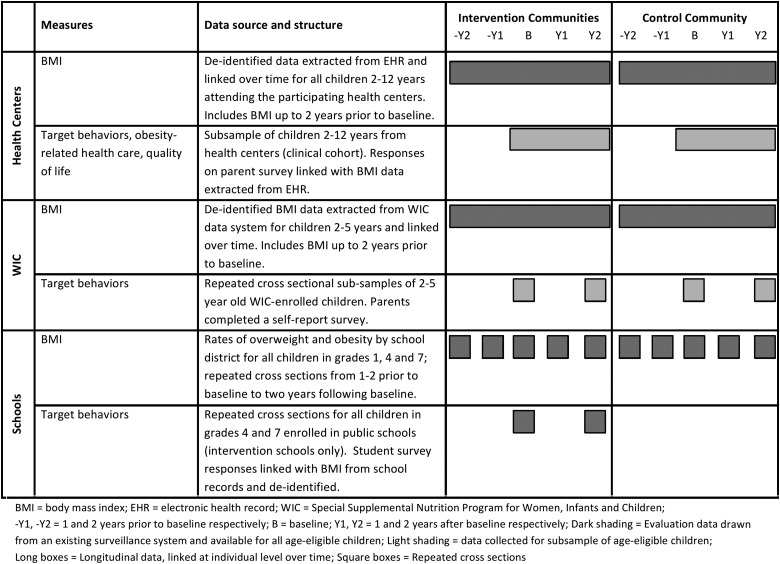
Figure 2 summarizes the data streams utilized in the health centers, WIC, and schools, including whether data are drawn from surveillance systems (dark shading) or a subsample of the target population (light shading) and whether data are independent at each time point reflecting repeated cross-sections (square boxes) or linked over time indicating a longitudinal design (long boxes). Complementing Figure 2, Table 2 illustrates variability in the data available within and across sectors by outcome (BMI and behavioral outcomes), school grade, assessment year, and for the majority versus a subsample of the target population.
Figure 2.
Summary of data streams utilized in the MA-CORD evaluation.
Table 2.
Summary of Body Mass Index and Behavioral Data Collected by Sector
| Intervention communities | Comparison community | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prebaselinea | Baseline | Year 1b | Year 2c | Prebaselinea | Baseline | Year 1b | Year 2c | ||||||||
| Federally qualified health centers | |||||||||||||||
| 2- to 12-year-old children (all) | BMI | → | BMI | → | BMI | → | BMI | → | BMI | → | BMI | → | BMI | → | BMI |
| 2- to 12-year-old children (subsample) | BMI | → | BMI+Beh | → | BMI+Beh | → | BMI+Beh | → | BMI | → | BMI+Beh | → | BMI+Beh | → | BMI+Beh |
| Public schoolsd | |||||||||||||||
| First-grade students (all) | BMI | BMI | BMI | BMI | BMI | BMI | BMI | BMI | |||||||
| Fourth-grade students (all) | BMI | BMI+Beh | BMI | BMI+Beh | BMI | BMI | BMI | BMI | |||||||
| Seventh-grade students (all) | BMI | BMI+Beh | BMI | BMI+Beh | BMI | BMI | BMI | BMI | |||||||
| WIC | |||||||||||||||
| 2- to 5-year-old children (all) | BMI | → | BMI | → | BMI | → | BMI | → | BMI | → | BMI | → | BMI | → | BMI |
| 2- to 5-year-old children (subsample) | BMI+Beh | BMI+Beh | BMI+Beh | BMI+Beh | |||||||||||
Arrow refers to longitudinal data (i.e., data linked for individuals over time).
Prebaseline=1–2 years preceding baseline.
Year 1=1 year after baseline.
Year 2=2 years after baseline (i.e., postintervention).
Rates of overweight and obesity by grade and gender and school district will be collected in the school sector; BMI is referenced in the table to streamline the presentation of information.
Beh, behavioral data (i.e., target behaviors); WIC, Special Supplemental Nutrition Program for Women, Infants and Children.
Data Collection Procedures
All data collection procedures were approved by the institutional review board (IRB) at the Massachusetts Department of Public Health. The Harvard School of Public Health and Massachusetts General Hospital for Children ceded IRB review to the Massachusetts Department of Public Health. A combination of passive and active consent procedures were used. Passive consent procedures were predominantly used when compiling deidentified data through existing surveillance systems. Active consent procedures were used when recruiting families for more-extensive measurement. To date, baseline and year 1 data collection are complete and year 2 data collection is in progress. Data extraction and cleaning for the health center and WIC electronic data (including prebaseline data), as described in greater detail below, is also in progress.
Federally qualified community health centers
In the federally qualified health centers, deidentified BMI data were extracted from EHRs for every child ages 2–12 years (∼7000 children) who resided and sought medical care in the intervention or comparison communities during the 2-year intervention period. In addition, where possible, BMI data for up to 2 years preceding the intervention will be extracted from EHRs to form an extended baseline. Thus, up to 6 years of BMI measurements will be available for each child (Table 2; Fig. 2). Additional variables include gender, visit date, and reason for the visit.
To complement the EHR data, a cohort of 515 families with children ages 2–12 years (referred to as the clinical cohort) was recruited at baseline through the participating health centers in the intervention and comparison communities. Trained research assistants recruited parents onsite following a well-child visit or by phone. In cases where more than 1 child per family was eligible, 1 child was randomly selected. At baseline, year 1, and year 2, parents completed a brief survey assessing the child's target behaviors, obesity-related quality of care, and quality of life. Parents also reported which school or ECEC their child attended to permit linkages across sectors. Behavioral data will be linked with the child's BMI data from the EHR.
Special Supplemental Nutrition Program for Women, Infants and Children (WIC)
Deidentified child BMI data were extracted from WIC records in the intervention and comparison communities for every child ages 2–5 years over the 2-year intervention period. When available, BMI data for up to 2 years preceding the intervention will be extracted along with these records. To complement these data, approximately 700 families with 2- to 5-year-old children enrolled in WIC were recruited at baseline; parents completed brief survey measuring their child's target behaviors. Parent responses will be linked with child BMI data from the WIC record system. A newly sampled group of families with age-eligible children are currently being recruited for the year 2 assessment. It was not feasible to recontact the original subsample of families to schedule follow-up. The behavioral data will not be linked over time and therefore will comprise two cross-sectional samples.
Schools
Massachusetts public schools are required to measure the heights and weights of all children in grades 1, 4, 7, and 10 on an annual basis and document rates of overweight and obesity by gender and grade.18 Height is measured to the nearest eighth of an inch, and weight is measured to the nearest quarter pound and recorded on the Massachusetts School Health Record form. In the intervention communities, a modified BMI measurement procedure was implemented at baseline and will be repeated for the year 2 assessment (fall 2014). All fourth and seventh graders (∼2500 students) from the intervention communities completed a self-report survey at the time of BMI measurement with oversight from a school nurse trained in survey administration procedures. The survey measures student demographic characteristics (age, gender, and race/ethnicity) and the five target behaviors. The BMI and survey data will be linked for each student through a common identification number, which cannot be traced back to the student (i.e., the data were deidentified). First-grade students did not complete the survey owing to concerns about their ability to report information accurately. The school nurse documented first-grade students' demographic information on the BMI assessment form using information from school records.
Aggregate district records will be used for the year 1 assessment. For the comparison community, overweight/obesity data for students in grades 1, 4, and 7 will be compiled from state and district records at each time point (baseline, year 1, and year 2). Overweight/obesity data will also be compiled from state records for a larger pool of comparison communities, as outlined in greater detail below. Given that state BMI mandates were introduced in 2009, school-based overweight/obesity data for all school districts in Massachusetts for the intervention period as well as up to 3 years preceding baseline (i.e., 2009–2011) will be available.18
Primary Outcome Measures
Table 3 summarizes the primary outcome measures by sector, along with the data sources and the timing of measurement. As previously noted, children's target behaviors were measured in the health centers and WIC based on parent report and in schools based on student self-report. The national CORD research team, including investigators from each site (Massachusetts, Texas, and California), the evaluation center, and the CDC adopted a consensus-driven approach to identify measures of the primary outcomes that would be utilized by all CORD sites as cross-site measures. For each outcome required by the legislative language, the CORD research team discussed, over 6–8 months, the best available evidence base, existing data against which results could be compared, whether the measure could be completed by children (10 years and older) in addition to parents, measures that each site were already using, and the feasibility of including the measure in CORD across multiple sectors and sites.
Table 3.
MA-CORD Primary Outcomes by Sector
| Intervention communities | Comparison community | |||||||
|---|---|---|---|---|---|---|---|---|
| Measures by sector | Example item | Source | B | Y1 | Y2 | B | Y1 | Y2 |
| Federally qualified health center | ||||||||
| Child BMIa | Measured height and weight | EHR extraction | Xa | X | X | Xa | X | X |
| Child diet Fruit, vegetables, SSB, 100% juice, water |
Yesterday, did your child eat any vegetables? | Parent survey, SPAN | X | X | X | X | X | X |
| Child physical activity No. of days active for 60 minutes |
During the past 7 days, on how many days was your child active for at least 60 minutes per day? | Parent survey, YRBS | X | X | X | X | X | X |
| Child screen time TV/DVDs, video games, Internet activities, TV where child sleeps |
On a typical day in the past week, how much time did your child spend watching TV/DVDs? Is there a television in the room where your child sleeps? |
Parent survey | X | X | X | X | X | X |
| Child sleep hygiene Daily hours of sleep, usual bedtime, time child goes to bed on school days |
In the past week, on average how much time did your child sleep during a usual 24-hour period? Does your child have a regular bedtime? What time does your child usually go to bed on a regular school day? |
Parent survey, PSQ | X | X | X | X | X | X |
| Child quality of care | Over the past year, when your child received healthcare, were you given a list of things your child could do to maintain a healthy weight? | Parent survey, PACIC | X | X | X | X | X | X |
| Child quality of life | In the past month, how often has your child had a problem with being teased by other children? | Parent survey, PedsQL | X | X | X | X | X | X |
| WIC | ||||||||
| Child BMI | Measured height and weight | WIC records | Xa | X | X | Xa | X | X |
| Child diet Fruit, vegetables, SSB |
Yesterday, did your child eat any vegetables? | Parent survey, SPAN | X | X | X | X | ||
| Child physical activity No. of days active for 60 minutes |
During the past 7 days, on how many days was your child active for at least 60 minutes per day? | Parent survey, YRBS | X | X | X | X | ||
| Child screen time TV where child sleeps |
Is there a television in the room where this child sleeps? | Parent survey | X | X | X | X | ||
| Child sleep Daily hours of sleep |
In the past week, on average how much time did your child sleep during a usual 24-hour period? | Parent survey, PSQ | X | X | X | X | ||
| Schools | ||||||||
| Child BMIa | Nurse measurement; grades 1, 4, and 7 | Nurse assessment School databases |
Xa | X | X | Xa | X | X |
| Child diet Fruit, vegetables, SSB, water |
Yesterday, did you eat any vegetables? | Student survey | X | X | ||||
| Child physical activity No. of days MVPA or outdoor play for 30 minutes |
Last week, on what days did you exercise or take part in physical activity that made your heart beat fast or made you breathe hard for at least 30 minutes (over entire day)? | Student survey, SPAN | X | X | ||||
| Child screen time TV/DVDs, video games, TV where child sleeps |
On a typical day in the past week, how much time did you spend watching TV/DVDs? | Student survey | X | X | ||||
| Child sleep hygiene Time go to bed on usual weekday, time wake up the next morning |
On a usual weekday this past week, when did you go to bed at night? When did you wake up the next morning? | Student survey | X | X | ||||
B=baseline; Y1=year 1, or 1 year after baseline; Y2=year 2, or 2 years after baseline.
Child BMI data are also available 1–2 years preceding baseline.
MA-CORD, Massachusetts Childhood Obesity Research Demonstration project; TV, television; DVDs, digital video discs; WIC, Special Supplemental Nutrition Program for Women, Infants and Children; EHR, electronic health record; PACIC, Patient Assessment of Chronic Illness Care survey; PedsQL, Pediatrics Quality of Life Inventory; PSQ, Pediatric Sleep Questionnaire; MVPA, moderate-to-vigorous physical activity; SPAN, School Physical Activity and Nutrition monitoring system; SSB, sugar-sweetened beverages; YRBS, Youth Risk Behavior Survey; BMI, body mass index.
Body mass index
Children's height and weight were used to calculate child BMI (weight[kg]/height[m]2) and age- and sex-specific BMI percentiles.19,20 In all sectors, children's standing height and weight were measured using a stadiometer and a Seca scale, respectively, by personnel trained in standardized BMI measurement procedures. Children were measured in a private setting, without shoes and hats, without heavy outer clothing (e.g., sweater), and after emptying their pockets of heavy objects (e.g., cell phones and iPods). Standard definitions of childhood overweight (BMI >85th to <95th percentile) and obesity (≥95th BMI percentile) were used.20
Dietary behaviors
Children's fruit, vegetable, SSB (i.e., regular nondiet sodas or soft drinks, including Malta, Penafiel, or Sumol, punch, Kool-Aid, Tampico, sports drinks, Goya juice, or other fruit-flavored drinks), and water consumption were assessed using six questions drawn from the School Physical Activity and Nutrition (SPAN) monitoring system.21,22 The SPAN monitoring system was used in the The Child and Adolescent Trial for Cardiovascular Health (CATCH) trial23 and has been validated for use by children in grade 4 and higher.21,22 Questions examine the child's behavior yesterday (see example item in Table 2) and include a 4-point response scale (e.g., 0=did not eat any vegetables, 1=ate vegetables 1 time yesterday, 2=ate vegetables 2 times yesterday, and 3=ate vegetables 3 or more times yesterday). Questions assessing the target behaviors match those used at the Texas (TX-CORD) and California (CA-CORD) CORD sites.10
Physical activity
In schools, children's recall of their PA was assessed using two items from the SPAN monitoring system.21,22 Items assess the number of days during the last week the child (1) participated in at least 30 minutes of moderate-to-vigorous PA (MVPA) and (2) played outdoors for at least 30 minutes outside of school time. In the health centers and WIC, parents' recall of their child's PA was assessed using one item drawn from the Youth Risk Behavior Survey (YRBS); this question examines the number of days in the past 7 days the child was physically active for a total of at least 60 minutes.24
Screen time
Children's weekly screen time was assessed in health centers, WIC, and schools using four questions focusing on time spent watching television/digital video discs (TV/DVDs) and time spent playing video games and computer games for a typical weekday and weekend day. In the health centers, time spent participating in Internet activities, such as social networking, e-mail, iPhone, or iPad applications (Apps) and YouTube (not including homework or games), were also measured. Additionally, the presence of a TV in the room where the child sleeps (yes/no) was assessed in health centers, WIC, and schools. Self-report surveys of screen time have been found to have moderate validity, compared with activity logs and 24-hour activity recalls.14,25
Sleep duration
Children's sleep time was assessed in health centers and WIC using a question from the Pediatric Sleep Questionnaire (PSQ).26 Responses were provided separately for weekdays and weekend days. Previous research supports the reliability and validity of the PSQ and its sensitivity to change in pediatric populations.26 In health centers, whether or not the child has a regular bedtime and the time the child goes to bed on school days were also assessed. In the school sector, children's sleep time was measured using a simplified format: Children recalled the times they go to bed and wake up the next morning on a usual weekday (which are used to calculate total sleep time) and the number of days in the past week they felt they needed more sleep.
Quality of life
Children's health-related quality of life was assessed in the health centers using 13 items from the Pediatrics Quality of Life Scale (PedsQL), which has demonstrated reliability and validity and is sensitive to change.27,28 Items assess the frequency over the past month that the child had problems: physical functioning (e.g., walking more than one block and participating in sports activity or exercise) and social functioning (e.g., getting along with other children or being teased by other children).
Quality of care
Children's quality of obesity-related care was assessed in the health centers using 8 modified questions from the Patient Assessment of Chronic Illness Care (PACIC).29 Previous research supports the reliability and validity of the PACIC.29
Proposed Analyses for the MA-CORD Outcome Evaluation
Following the collection and preparation of year 2 data, the impact of MA-CORD will be tested using a combination of within-person, between-person, and group-level analyses. All analyses will control for differences in demographic factors as necessary. Our primary analysis will involve change in BMI.30,31 Similar analyses will be performed for the target behaviors.
Within the health centers, repeated BMI measures will be available for all eligible children, including the clinical cohort at baseline, year 1, and year 2. With the individual as the unit of analysis, change in BMI for children in health centers in the intervention versus comparison communities will be compared using linear mixed models, where random effects are used to model the correlation of measurements from the same child. The parameter of interest is the interaction between intervention and time. Based on the enrollment of 2210 children ages 2–12 years in the intervention health centers and 3688 children enrolled in the comparison health center at baseline, there will be approximately 80% power to detect a change in BMI of 0.10 kg/m2. For the clinical cohort, based on 332 children enrolled in the cohort in the intervention communities and 183 children enrolled in the cohort in the comparison community at baseline, there will be approximately 80% power to detect a change in BMI of 0.35 kg/m2. In addition to examining change in BMI for the intervention versus comparison communities, it will be possible to assess links between change in the target behaviors and change in BMI in the clinical cohort along with effects of intervention exposure. Methods used to examine change in BMI for children enrolled in WIC in the intervention versus comparison communities will mimic those used for the health centers.
Within the school sector, repeated (baseline, year 1, and year 2) population cross-sections of child BMI will be available for all children in grades 1, 4, and 7 in the intervention communities and the comparison community. Using the school as the unit of analysis (measures for grades 1, 4, and 7 within each school), linear regression models will be used to examine change in mean BMI for schools in the intervention versus comparison communities, adjusting for school-level covariates, such as race/ethnicity and the proportion of children eligible for the free and reduced cost school meals program. Similar models using logistic regression will be performed to assess change rates of childhood overweight and obesity. Given that the dependent variable is the change in mean BMI or percentage of children who are overweight or obese, there will be three measurements per school, so we will adjust for any clustering within schools.
Although the use of a comparison community addresses the potential concern that secular trends explain pre/post intervention changes in BMI, there is still the possibility that temporal trends could differ among communities for reasons other than the intervention. This issue will be examined using school overweight/obesity data available for all school districts in the state to conduct a third type of analysis. Up to 20 school districts in Massachusetts will be selected that are similar to the intervention and comparison school districts' school demographic characteristics, preintervention obesity levels, and trends in rates of obesity prior to the intervention. Comparison schools are also expected to meet the following criteria: at least 500 students in grades 1, 4, and 7; fewer than 60% non-Hispanic white students; school BMI assessment beginning 2012 or earlier; and 80% or more of students weighed and measured in 2012. Based on an initial review of district BMI data, at least 22 school districts meet these criteria and are eligible for consideration. Upon selecting the comparison districts, multivariable regressions will be used to determine whether the intervention communities performed better than the comparison communities in terms of change from pre- to postintervention.
As illustrated in Figure 2, a subset of children in the health centers and WIC as well as a subset of schools will have BMI measures for 1–2 years preceding baseline. The above analyses for each sector will be rerun, including prebaseline data, to evaluate whether the BMI time trend before the intervention is different from the BMI time trend after the intervention for the intervention versus comparison communities.
Should evidence of intervention effects be found, an attempt will be made to disentangle the source of such effects by focusing on the data collected at health centers using information on the location of each child's school and/or ECEC as measured on the parent survey. Using these links, site-specific information from schools and child care centers can be pulled into the analysis. Pending IRB approval, the locations of schools and ECECs for children enrolled in the respective health centers, but who are not included in the clinical cohort, will be determined using geocodes along with the school and child care responses. Given that parents' selection of schools and ECECs are heavily influenced by geographic proximity, these additional data should increase our ability to estimate sector-specific impacts of MA-CORD interventions.
Analysis of the Baseline Data
To set the stage for the final outcome evaluation, an overview of the baseline data for the primary outcomes in the health centers, WIC, and schools is presented below. To facilitate interpretation of the data, behavioral data are dichotomized in all sectors, even though continuous variables will also be used in the final analyses. The figures reported in Tables 4–6 reflect the percentage of participants who did not meet minimally sufficient recommendations for the target behavior. Such recommendations include: (1) consuming fruits, vegetables, and water at least once a day, consuming juice one or fewer times a day, and consuming no SSBs (soda plus fruit drink)32; (2) reporting 6033 or 30 minutes34 of MVPA each day; (3) reporting no more than 2 hours of total screen time per day and not having a TV in the room where the child sleeps35; and (4) reporting at least 10 (ages 6–12 years) or 11 (ages 2–5 years) hours of sleep per day.36
Table 4.
Summary of Baseline (2012) Primary Outcome Data: Federally Qualified Health Centers
| Fitchburg % (N) | New Bedford % (N) | Intervention communities combined % (N) | Comparison community % (N) | |
|---|---|---|---|---|
| All children 2–12 years attending health center | N=452 | N=1758 | N=2210 | N=3688 |
| Overweight (BMI 85th to <95th percentile) | 16.4 (74) | 18.7 (329) | 18.2 (402) | 18.5 (682) |
| Obese (BMI ≥95th percentile) | 26.6 (120) | 25.7 (452) | 25.8 (570) | 23.5 (867) |
| Clinical cohort of children 2–12 years | N=93 | N=240 | N=333 | N=182 |
| Overweight (BMI 85th to <95th percentile) | 10.1 (9) | 16.3 (39) | 14.6 (49) | 16.6 (30) |
| Obese (BMI ≥95th percentile) | 28.1 (26) | 29.6 (71) | 29.2 (97) | 25.4 (46) |
| Diet (frequency consumed yesterday) | ||||
| Vegetables (consuming none) | 38.7 (36) | 30.8 (74) | 33.0 (110) | 37.9 (69) |
| Fruit (consuming none) | 30.1 (28) | 19.6 (47) | 22.5 (75) | 24.2 (44) |
| 100% juice (consuming >1) | 32.3 (30) | 38.3 (92) | 36.6 (122) | 35.7 (65) |
| SSB (soda and juice drinks; consuming ≥1) | 55.0 (51) | 43.3 (104) | 46.5 (155) | 50.0 (91) |
| Water (consuming none) | 10.8 (10) | 10.4 (25) | 10.5 (35) | 8.2 (15) |
| PA | ||||
| 60 minutes of PA (reporting <7 days) | 28.0 (26) | 27.9 (67) | 27.9 (93) | 25.3 (46) |
| Screen time | ||||
| Average daily hours screen (>2 hours) | 67.4 (63) | 52.7 (127) | 56.8 (189) | 73.6 (134) |
| TV where child sleeps (with TV) | 73.1 (68) | 60.8 (146) | 64.3 (214) | 61.0 (111) |
| Sleep | ||||
| Insufficient sleep (<11 hours/day for 2- to 5-year-olds, <10 hours/day for 6- to 12-year-olds) | 49.5 (46) | 61.9 (149) | 58.4 (195) | 62.8 (114) |
SSB, sugar-sweetened beverages; PA, physical activity; TV, television.
Table 5.
Summary of Baseline (2012) Primary Outcome Data: WIC
| Fitchburg | New Bedford | Intervention communities combined | Comparison community | |
|---|---|---|---|---|
| % (N) | % (N) | % (N) | % (N) | |
| All 2- to 5-year-old children | N=838 | N=2037 | N=2875 | N=2381 |
| Overweight (BMI 85th to <95th percentile) | 17.4 (146) | 17.3 (352) | 17.3 (497) | 11.0 (262) |
| Obese (BMI ≥95th percentile) | 15.4 (129) | 17.7 (361) | 17.0 (489) | 11.8 (281) |
| Subsample of 2- to 5-year-old children | N=206 | N=189 | N=395 | N=306 |
| Overweight (BMI 85th to <95th percentile) | 17.0 (35) | 15.9 (30) | 16.5 (65) | 14.7 (45) |
| Obese (BMI ≥95th percentile) | 17.5 (36) | 16.9 (32) | 17.2 (68) | 10.5 (32) |
| Diet (frequency consumed yesterday) | ||||
| Vegetables (consuming none) | 16.8 (35) | 20.7 (39) | 18.6 (74) | 15.1 (46) |
| Fruit (consuming none) | 10.0 (21) | 10.4 (20) | 10.2 (40) | 6.0 (18) |
| 100% juice (consuming >1) | 57.1 (118) | 70.2 (133) | 63.3 (250) | 46.3 (142) |
| SSB (soda and juice drinks; consuming ≥1) | 27.2 (56) | 31.8 (60) | 29.4 (116) | 17.0 (52) |
| PA | ||||
| 60 minutes of PA (reporting <7 days) | 35.5 (73) | 29.5 (56) | 32.6 (129) | 21.7 (66) |
| Screen time | ||||
| Average daily hours screen (reporting >2) | 31.1 (64) | 29.6 (56) | 30.4 (120) | 24.5 (75) |
| TV where child sleeps (with TV) | 49.0 (101) | 54.1 (102) | 51.4 (203) | 42.4 (130) |
| Sleep | ||||
| Insufficient sleep (<11 hours/day) | 50.8 (105) | 53.0 (100) | 51.8 (205) | 23.4 (72) |
WIC, Supplemental Program for Women, Infants, and Children; SSB, sugar-sweetened beverages; PA, physical activity; TV, television.
Table 6.
Summary of Baseline (2012) Primary Outcome Data: Schools
| Fitchburg | New Bedford | Intervention communities combined | Comparison community | |
|---|---|---|---|---|
| % (N) | % (N) | % (N) | % (N) | |
| First-, fourth-, and seventh-grade students | N=1137 | N=2974 | N=4092 | N=3022 |
| Overweight (BMI 85th to <95th percentile) | 16.8 (191) | 18.8 (559) | 18.3 (749) | 15.8 (478) |
| First grade | 15.1 (172) | 18.2 (541) | 17.5 (716) | 13.5 (408) |
| Fourth grade | 17.7 (201) | 19.3 (574) | 18.9 (773) | 17.4 (526) |
| Seventh grade | 18.1 (206) | 19.1 (568) | 18.8 (769) | 16.9 (511) |
| Obese (BMI ≥95th percentile) | 25.3 (288) | 27.6 (821) | 27.0 (1105) | 20.0 (604) |
| First grade | 20.6 (234) | 24.6 (732) | 23.6 (966) | 16.8 (508) |
| Fourth grade | 24.2 (275) | 29.5 (877) | 28.1 (1150) | 22.1 (668) |
| Seventh grade | 32.5 (370) | 30.0 (892) | 30.8 (1260) | 21.5 (650) |
| Fourth- and seventh-grade studentsa | N=703 | N=1753 | N=2456 | N/A |
| Diet (frequency consumed yesterday) | ||||
| Vegetables (consuming none) | 35.9 (252) | 41.8 (733) | 40.1 (985) | N/A |
| Fruit (consuming none) | 25.1 (175) | 29.6 (519) | 28.3 (695) | N/A |
| 100% juice (consuming >1) | 30.6 (215) | 26.3 (461) | 27.5 (675) | N/A |
| Juice drinks (consuming ≥1) | 55.9 (393) | 53.0 (929) | 53.8 (1321) | N/A |
| SSB (soda and juice drinks; consuming ≥1) | 74.1 (521) | 70.8 (1241) | 71.8 (1763) | N/A |
| Water (consuming none) | 14.3 (101) | 17.7 (310) | 16.8 (413) | N/A |
| Physical activity | ||||
| 30 minutes of MVPA (reporting <7 days) | 86.2 (606) | 87.8 (1539) | 87.3 (2144) | N/A |
| 30 minutes outdoors (reporting <7 days) | 87.9 | 88.7 | 88.5 | N/A |
| Screen time | ||||
| Daily hours screen (≥2 hours) | 62.2 | 65.5 | 64.5 | N/A |
| TV where child sleeps (with TV) | 72.4 | 76.2 | 75.1 | N/A |
| Sleep | ||||
| Insufficient sleep (<10 hours/day) | 59.1 | 62.5 | 61.5 | N/A |
| First grade | N/A | N/A | N/A | N/A |
| Fourth grade | 38.7 | 50.5 | 47.4 | N/A |
| Seventh grade | 81.0 | 78.9 | 79.5 | N/A |
Sample size may vary owing to missing data.
SSB, sugar-sweetened beverage; MVPA, moderate-to-vigorous physical activity; TV, television; N/A, not available.
Results
At baseline, approximately 23–25% of 2- to 12-year-old children enrolled in a participating health center in the MA-CORD communities were obese (Table 4). Among preschool-aged children enrolled in WIC, the baseline prevalence of obesity ranged between 12% and 17% across communities (Table 5). Obesity prevalence in school-aged children varied by school grade with 17–24% of first-grade children, 22–28% of fourth-grade children, and 22–30% of seventh-grade children in the MA-CORD communities classified as obese (Table 6). Overall, rates of obesity appeared to be slightly higher in the comparison community, compared with the intervention communities.
For the target behaviors, approximately 15% of preschool-aged children at baseline consumed no vegetables the previous day, 50% had a TV in the room where they slept, and 17–30% consumed an SSB (Table 5). Within the health clinics, approximately 35% of children consumed no vegetables the previous day, 50% consumed an SSB the previous day, 25% had insufficient PA, 60% had a TV in the room where they slept, and 60% had insufficient sleep (Table 4). Among school-aged children, approximately 40% consumed no vegetables and 70% consumed an SSB the previous day (Table 6). In addition, approximately 75% had a TV in the room where they slept, 85% had insufficient levels of PA, and 45–80% reported insufficient sleep with higher rates of insufficient sleep observed among seventh graders, compared with fourth graders.
Discussion
MA-CORD is a complex community intervention to prevent and control childhood obesity in two predominantly low-income cities in Massachusetts. The MA-CORD communities are at high risk of childhood obesity, with obesity rates at baseline being notably higher than those observed in the US population where approximately 17% of children ages 2–19 years in 2011–2012 were obese.37 The evaluation design integrates information across multiple communities, intervention levels, and sectors and takes advantage of both existing surveillance systems and new data collection. This permits the compellation of data for the primary outcomes for a substantial number of children ages 2–12 years from the intervention and comparison communities, including over 7000 children in the health centers, 7000 children in schools, and 4000 children enrolled in WIC.
Development and implementation of the evaluation plan capitalizes on the strengths of MA-CORD's interdisciplinary team with expertise in measurement and program evaluation in clinical, school, afterschool, and ECE settings. Intervention and evaluation strategies were informed by research previously undertaken by our research team.15,17,38,39 Collaboration among researchers, the Massachusetts Department of Public Health, and community partners make such large-scale data collection possible. Supplemental grants enable additional assessments across sectors, facilitating the collection of qualitative and quantitative data for process evaluations, which will be presented in follow-up publications. For example, as outlined by Chuang and colleagues,40 a supplemental grant supported semistructured interviews with community stakeholders at baseline and year 1 to assess factors hypothesized to affect implementation effectiveness across multiple CORD sites based on an overarching implementation model.
MA-CORD and the broader CORD consortium are designed with sustainability in mind. Intervention activities are implemented by the community; thus, all key decisions about implementation are made within the community. The sustainability of MA-CORD's potential impact is further enhanced by policy and environmental changes across sectors (e.g., development of policies in afterschool settings to limit screen time and improve nutritional standards for snacks), as well as changes in practice and systems that can be readily maintained (e.g., integration into the EHR of computerized support tools and, in schools, adoption of health education lessons easily incorporated into existing school curricula).
In the context of such a large study requiring consistent measures across multiple sectors and communities, the choice of assessment methods was constrained by participant burden, cost, and logistical considerations. Therefore, the assessment of behavioral outcomes relied largely on self- or parent-reported measures with evidence of validity and/or reliability, or which have been used in previous large-scale studies, in lieu of instruments that may be less prone to reporting biases. For instance, though 24-hour dietary recalls, diet records, or direct observation may have yielded complete and potentially more accurate estimates of diet, the costs of administering and coding such measures, along with the need to obtain administrative permission to conduct these measures during the school day, were prohibitive. Likewise, the use of accelerometry and actigraphy as primary measures of PA and sleep would have been less prone to social desirability bias and recall error, but were not feasible owing to financial or logistical barriers.
Identifying an appropriate comparison community presented a number of challenges. The two target communities are quite different, thus making it difficult to identify a single comparison community that matched both target communities. It was not feasible to include multiple comparison communities. In addition, to ensure that all MA-CORD communities had a similar level of infrastructure and community support for obesity prevention, the comparison community (as with the intervention communities) was required to be a Mass in Motion participant community. The result of this requirement is that it limited the pool of comparison communities and further limited the feasibility of identifying a well-matched comparison community. Baseline differences in the target outcomes for the intervention and comparison communities were expected. To the extent possible, these differences will be taken into account in the final analyses.
There is also uncertainty around the length of time required to detect clinically meaningful changes in BMI in the context of a community intervention. Relative to smaller, targeted interventions, the dose received by most participants in MA-CORD was likely to have been diffuse. As a result, 2 years may be insufficient to detect changes in child BMI. However, significant changes in adiposity have been detected previously in the context of a 2-year community intervention. Shape Up Somerville, a policy-focused intervention in diverse cities in Massachusetts, resulted in a 2-year reduction in BMIz of children in the intervention community (change in BMIz=−0.06; p<0.01), compared to controls.3 Moreover, recent research documents that approximately 80% of expected weight change resulting from a given behavioral change is observed within 2 years.41,42 Finally, the use of existing surveillance systems for the evaluation of MA-CORD permits continued assessment of potential intervention impacts beyond two years.
Conclusion
Despite their inherent challenges, multisector whole-community interventions hold tremendous promise for addressing childhood obesity and reaching underserved populations. Improvements in at least one measure of adiposity or population-level prevalence of childhood obesity have been observed in several multisector community interventions.2–6,43,44 However, most of these interventions have taken place in outside the United States. MA-CORD is part of a consortium of demonstration projects that distinguish themselves from previous community interventions through their integrated focus on healthcare and clinical-community partnerships and their emphasis on sustainability.10 If successful, MA-CORD and the broader CORD consortium will serve as a best practices model for accelerating progress in reversing childhood obesity.
Appendix
The following investigators and institutions constitute the MA-CORD Study Group: Massachusetts Department of Public Health: Thomas Land, PhD; Commissioner Cheryl Bartlett, RN; Lea Susan Ojamaa, MPH; Craig Andrade, DrPH; Jo-Ann Kwass, MS; Jaime Corliss, MPH; James Buszkiewicz, MPH; Judy Hause, MPH; Rachel Colchamiro, MPH, RD; Peggy Leung-Strle, MS, RD; Suzanne Crowther, MPH; Donna Salloom. Massachusetts Department of Early Education and Care: Anne Hemmer, RD, MS. Fitchburg Mass in Motion: Mary Giannetti, MS, RD; Pamela Rivers, RN, MPH. New Bedford Mass in Motion: Pauline Hamel, EdD; Kim Ferreira, MS; Sarah Clermont, MPH; Karen Regan, RN, MSN. Massachusetts General Hospital for Children/Harvard Medical School: Elsie M. Taveras, MD, MPH; Meghan Perkins, MPH; Jennifer Woo Baidal, MD, MPH; Lauren Fiechtner, MD, MPH; Courtney Cunningham MPH; Savannah Vicente, BS; Gabriella De Paz, BS. Harvard School of Public Health: Kirsten Davison, PhD; Steven Gortmaker, ScD; Walter Willett, MD, DrPH; Lilian Cheung, DSc; Steven Miller; Catherine Giles, MPH; Rebecca L. Franckle, MPH; Claudia Ganter, MPH; Rachel E. Blaine, MPH, RD; Jennifer Falbe, ScD, MPH, Shaniece Criss, MPH; Alyssa Aftosmes-Tobio, MPH; Jo Charles, BS; Alvin Tran, MPH. National Initiative for Children's Healthcare Quality: Shikha Anand, MD, MPH; Lauren Smith, MD, MPH; Charles Homer, MD, MPH; Lexi Abel, MPH. MORE Advertising: Megan Palamé, MA. Harvard Pilgrim Health Care Institute: Martin Kuldorff, PhD; Matthew Gillman, MD, SM. University of California, Berkeley: Jennifer Falbe, PhD. Centers for Disease Control and Prevention: Carrie A. Dooyema, MPH, MSN, RN; Brook Belay, MD, MPH; Jennifer L. Foltz, MD, MPH; Nancy Williams, MSPH; Heidi M. Blanck, PhD. University of Houston Evaluation Center: Daniel O'Connor, PhD; Paras Mehta, PhD.
Contributor Information
Collaborators: the MA-CORD Study Group
Acknowledgments
This study was supported by the CDC, National Center for Chronic Disease Prevention and Health Promotion (award no.: U18DP003370). The work is solely the responsibility of the authors and does not represent official views of the CDC. The authors thank the families, institutions, faculty, research staff, and students that are participating in the MA-CORD study.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Institute of Medicine. Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. The National Academies Press: Washington, DC, 2012. Available at www.iom.edu/Reports/2012/Accelerating-Progress-in-Obesity-Prevention.aspx Last accessed November11, 2014 [PubMed] [Google Scholar]
- 2.Sanigorski AM, Bell AC, Kremer PJ, et al. Reducing unhealthy weight gain in children through community capacity-building: Results of a quasi-experimental intervention program, Be Active Eat Well. Int J Obes (Lond) 2008;32:1060–1067 [DOI] [PubMed] [Google Scholar]
- 3.Economos CD, Hyatt RR, Must A, et al. Shape Up Somerville two-year results: A community-based environmental change intervention sustains weight reduction in children. Prev Med 2013;57:322–327 [DOI] [PubMed] [Google Scholar]
- 4.de Silva-Sanigorski AM, Bell AC, Kremer P, et al. Reducing obesity in early childhood: Results from Romp & Chomp, an Australian community-wide intervention program. Am J Clin Nutr 2010;91:831–840 [DOI] [PubMed] [Google Scholar]
- 5.Pettman T, Magarey A, Mastersson N, et al. Improving weight status in childhood: Results from the eat well be active community programs. Int J Public Health 2014;59:43–50 [DOI] [PubMed] [Google Scholar]
- 6.Kremer P, Waqa G, Vanualailai N, et al. Reducing unhealthy weight gain in Fijian adolescents: Results of the Healthy Youth Healthy Communities study. Obes Rev 2011;12(Suppl 2):29–40 [DOI] [PubMed] [Google Scholar]
- 7.Dooyema CA, Belay B, Foltz JL, et al. The childhood obesity research demonstration project: A comprehensive community approach to reduce childhood obesity. Child Obes 2013;9:454–459 [DOI] [PubMed] [Google Scholar]
- 8.Dietz W, Lee J, Wechsler H, et al. Health plans' role in preventing overweight in children and adolescents. Health Aff 2007;26:430–440 [DOI] [PubMed] [Google Scholar]
- 9.Foltz J, Dooyema C, Belay B, et al. Overarching conceptual approach to the design and implementation of the Childhood Obesity Research Demonstration (CORD). Child Obes 2015;11:4–1025679059 [Google Scholar]
- 10.O'Connor D, Lee R, Mehta P, et al. Childhood Obesity Research Demonstration (CORD) project: Cross-site evaluation methods. Child Obes 2015;11:92–103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Glasgow RE, Davidson KW, Dobkin PL, et al. Practical behavioral trials to advance evidence-based behavioral medicine. Ann Behav Med 2006;31:5–13 [DOI] [PubMed] [Google Scholar]
- 12.Taveras E, Blaine R, Davison K, et al. Design of the Massachusetts Childhood Obesity Research Demonstration (MA-CORD) project. Child Obes 2015;11:11–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Benjamin S, Ammerman A, Sommers J, et al. Nutrition and physical activity self-assessment for child care (NAP SACC): Results from a pilot intervention. J Nutr Educ Behav 2007;39:142–149 [DOI] [PubMed] [Google Scholar]
- 14.Gortmaker S, Cheung L, Peterson K, et al. Impact of a school-based interdisciplinary intervention on diet and physical activity among urban primary school children: Eat well and keep moving. Arch Pediatr Adolesc Med 1999;153:975–983 [DOI] [PubMed] [Google Scholar]
- 15.Gortmaker SL, Peterson K, Wiecha J, et al. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adol Med 1999;153:409–418 [DOI] [PubMed] [Google Scholar]
- 16.Gortmaker S, Lee R, Mozaffarian R, et al. Effect of an after-school intervention on increases in children's physical activity. Med Sci Sports Exerc 2012;44:450–457 [DOI] [PubMed] [Google Scholar]
- 17.Giles CM, Kenney EL, Gortmaker SL, et al. Increasing water availability during afterschool snack: Evidence, strategies, and partnerships from a group randomized trial. Am J Prev Med 2012;43:S136–S142 [DOI] [PubMed] [Google Scholar]
- 18.Leibowitz R, Foley M, Gapinski M, et al. The status of childhood weight in Massachusetts: Preliminary results from body mass index screening in Massachusetts public school districts, 2009–2011. Available at www.mass.gov/eohhs/docs/dph/com-health/school/status-childhood-obesity-2011.pdf Last accessed September3, 2014
- 19.Ogden CL, Flegal KM. Changes in terminology for childhood overweight and obesity. Natl Health Stat Rep 2010:1–5. Available at www.cdc.gov/nchs/data/nhsr/nhsr025.pdf Last accessed September3, 2014 [PubMed]
- 20.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, et al. CDC growth charts: United States. Adv Data 2000:1–27 [PubMed] [Google Scholar]
- 21.Hoelscher D, Day R, Kelder S, et al. Reproducibility and validity of the secondary level School-Based Nutrition Monitoring student questionnaire. J Am Diet Assoc 2003;103:186–194 [DOI] [PubMed] [Google Scholar]
- 22.Thiagarajah K, Fly A, Hoelscher D, et al. Validating the food behavior questions from the elementary school SPAN questionnaire. J Nutr Educ Behav 2008;40:305–310 [DOI] [PubMed] [Google Scholar]
- 23.Edmundson E, Parcel G, Feldman H, et al. The effects of the Child and Adolescent Trial for Cardiovascular Health upon psychosocial determinants of diet and physical activity behavior. Prev Med 1996;25:442–454 [DOI] [PubMed] [Google Scholar]
- 24.Helmerhorst HJ, Brage S, Warren J, et al. A systematic review of reliability and objective criterion-related validity of physical activity questionnaires. Int J Behav Nutr Physc Act 2012;9:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schmitz KH, Harnack L, Fulton JE, et al. Reliability and validity of a brief questionnaire to assess television viewing and computer use by middle school children. J Sch Health 2004;74:370–377 [DOI] [PubMed] [Google Scholar]
- 26.Chervin RD, Hedger K, Dillon JE, et al. Pediatric sleep questionnaire (PSQ): Validity and reliability of scales for sleep-disordered breathing, snoring, sleepiness, and behavioral problems. Sleep Med 2000;1:21–32 [DOI] [PubMed] [Google Scholar]
- 27.Varni JW, Burwinkle TM, Seid M, et al. The PedsQL 4.0 as a pediatric population health measure: Feasibility, reliability, and validity. Ambul Pediatr 2003;3:329–341 [DOI] [PubMed] [Google Scholar]
- 28.Varni JW, Seid M, Smith Knight T, et al. The PedsQL in pediatric rheumatology: Reliability, validity, and responsiveness of the Pediatric Quality of Life Inventory Generic Core Scales and Rheumatology Module. Arthritis Rheum 2002;46:714–725 [DOI] [PubMed] [Google Scholar]
- 29.Glasgow RE, Wagner EH, Schaefer J, et al. Development and validation of the Patient Assessment of Chronic Illness Care (PACIC). Med Care 2005;43:436–444 [DOI] [PubMed] [Google Scholar]
- 30.Cole TJ, Faith MS, Pietrobelli A, et al. What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile? Eur J Clin Nutr 2005;59:419–425 [DOI] [PubMed] [Google Scholar]
- 31.Berkey CS, Colditz GA. Adiposity in adolescents: Change in actual BMI works better than change in BMI z score for longitudinal studies. Ann Epidemiol 2007;17:44–50 [DOI] [PubMed] [Google Scholar]
- 32.US Department of Agriculture, US Department of Health and Human Services. Dietary Guidelines for Americans, 2010. 7th edition. US Government Printing Office: Washington, DC, 2010 [Google Scholar]
- 33.US Department of Health and Human Services. 2008 physical activity guidelines for Americans. 2008. Available at www.health.gov/paguidelines/guidelines/default.aspx Last accessed September3, 2014
- 34.Pate R, Pratt M, Blair S, et al. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA 1995;273:402–407 [DOI] [PubMed] [Google Scholar]
- 35.American Academy of Pediatrics Committee on Public Education. Children, adolescents, and television. Pediatrics 2001;107:423–426 [DOI] [PubMed] [Google Scholar]
- 36.US Department of Health and Human Services and the National Institutes of Health. Your Guide to Healthy Sleep. 2011. www.nhlbi.nih.gov/health/public/sleep/healthy_sleep.pdf Last accessed September3, 2014
- 37.Ogden C, Carroll M, Kit B, et al. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014;311:806–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Taveras EM, Gortmaker SL, Hohman KH, et al. Randomized controlled trial to improve primary care to prevent and manage childhood obesity: The High Five for Kids study. Arch Pediatr Adolesc Med 2011;165:714–722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Taveras EM, Marshall R, Horan CM, et al. Rationale and design of the STAR randomized controlled trial to accelerate adoption of childhood obesity comparative effectiveness research. Contemp Clin Trials 2013;34:101–108 [DOI] [PubMed] [Google Scholar]
- 40.Chuang E, Ayala G, Schmied E, et al. Evalaution protocol to assess an integrated framework for the implementation of the Childhood Obesity Research Demonstration project at the California (CA-CORD) and Massachusetts (MA-CORD) sites. Child Obes 2015;11:48–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hall KD, Butte NF, Swinburn BA, et al. Dynamics of childhood growth and obesity: Development and validation of a quantitative mathematical model. Lancet Diabetes Endocrinol 2013;1:97–105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hall KD, Sacks G, Chandramohan D, et al. Quantification of the effect of energy imbalance on bodyweight. Lancet 2011;378:826–837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Romon M, Lommez A, Tafflet M, et al. Downward trends in the prevalence of childhood overweight in the setting of 12-year school- and community-based programmes. Public Health Nutr 2009;12:1735–1742 [DOI] [PubMed] [Google Scholar]
- 44.Chomitz VR, McGowan RJ, Wendel JM, et al. Healthy Living Cambridge Kids: A community-based participatory effort to promote healthy weight and fitness. Obesity (Silver Spring) 2010;18(Suppl 1):S45–S53 [DOI] [PubMed] [Google Scholar]