An intervention combining metacognitive strategy instruction with implementation intention training was found to be both feasible and potentially beneficial for adults with mild TBI.
Abstract
OBJECTIVE. We evaluated the feasibility of an intervention combining metacognitive strategy instruction (MSI) with training in implementation intentions for adults with mild traumatic brain injury (mTBI). Implementation intentions are written premade decision statements specifying when, where, and how goal behaviors are to be enacted.
METHOD. Two participants with mTBI received a six-session intervention that included setting a daily implementation intention for an occupational therapy goal. A scoring rubric was used to evaluate the quality of implementation intentions; goal achievement was measured using the Canadian Occupational Performance Measure (COPM) and goal attainment scaling.
RESULTS. All implementation intentions received perfect quality scores, suggesting participants learned to correctly craft implementation intentions. Improvements in COPM self-ratings exceeded minimal detectable change values; goal attainment levels indicated better-than-expected goal achievement.
CONCLUSION. An intervention combining MSI and implementation intention training appears to be feasible. As an adjunct to MSI, implementation intentions may contribute to clients’ ability to achieve their own occupational performance goals. Further study is needed.
Some people with mild traumatic brain injury (mTBI) experience executive dysfunction (Levine et al., 2011), which interferes with goal-directed behavior (Levine et al., 2000). In occupational therapy, these people may receive metacognitive strategy instruction (MSI; Radomski, Anheluk, Bartzen, & Zola, 2016). MSI involves teaching clients to learn to use new cognitive strategies (e.g., planning of routines, use of cognitive assistive technology) to meet therapy goals and ultimately improve occupational performance. However, successful use of new cognitive strategies in everyday life requires the learner to sustain conscious effort to recognize situations in which the newly learned strategies should be applied. This effortful attention is difficult for anyone to sustain (Salomon & Perkins, 1989), but especially so for people with mTBI. This difficulty may explain why people often act in ways that are contrary to their intentions (Gollwitzer, 1999). Therefore, MSI may not in and of itself advance enactment of goal behaviors, because successful strategy implementation is contingent on intact functioning of the impaired cognitive skills it is designed to circumvent (Clark-Wilson, Giles, & Baxter, 2014).
People who set implementation intentions in addition to goals appear to meet their goals more frequently than those who do not use implementation intentions (Gollwitzer, 1999). A goal describes a person’s commitment to a hoped-for endpoint (“I will lose 10 lb”) but does not specify how, when, or where goal-related behaviors will be performed (Gollwitzer & Brandstätter, 1997). Thus, goal achievement depends on self-monitoring and real-time problem solving, which are effortful and difficult to sustain (Levine et al., 2011). By including preestablished decisions about when, where, and how to enact specific goal behaviors, implementation intentions address the how-tos of goal achievement. Implementation intentions are developed as written if/when–then plans that link specific situational triggers with one-time actions that are aligned with the individual’s goals (e.g., “In Situation X, I will initiate Behavior Y”; Gollwitzer, 1999).
For example, to meet a 10-lb weight loss goal, the person might write the following implementation intention first thing in the morning: If I feel the urge to snack while watching TV (the if/when component), then I will eat some carrots (the then component). When the person encounters the situational trigger (feeling the urge to snack), the preestablished trigger action pairing of the implementation intention becomes activated, facilitating goal-directed action (eating carrots) with little or no conscious intent or effort (Bayer, Achtziger, Gollwitzer, & Moskowitz, 2009). This strategy reduces the demands of continuous, conscious goal oversight and increases the likelihood that people will act in accordance with their goals.
People who develop implementation intentions appear to perform better under stress (Scholz et al., 2009), improve their performance of prospective memory tasks (Burkard et al., 2014), and more frequently implement a wide range of health behaviors (e.g., Harris et al., 2014; Prestwich et al., 2012). Implementation intentions have been shown to increase performance speed for people with frontal lobe lesions (Lengfelder & Gollwitzer, 2001), to help people with anxiety use cognitive–behavioral techniques (Varley, Webb, & Sheeran, 2011), and to enhance memory performance for people with multiple sclerosis (Kardiasmenos, Clawson, Wilken, & Wallin, 2008).
A literature review conducted for this study failed to locate any prior study that described or evaluated an implementation intention intervention designed to help people with mTBI use implementation intentions in the context of self-selected goals. To address this evidentiary gap, we developed a six-session MSI intervention that incorporates training in implementation intentions called ACTION (AutomatiC iniTiation of IntentiONs). In preparation to conduct a small randomized controlled trial involving soldiers with mTBI, we evaluated the feasibility of our ACTION training methods on two civilians. Feasibility of the intervention was determined by answers to the following research question: Are civilians with mTBI who receive implementation intention training embedded in MSI (ACTION) able to learn to set implementation intentions specific to their self-selected occupational therapy goals, and do they achieve those goals?
Method
Design
We used a pretest–posttest case study design to answer the research question. Procedures were approved by the Quorum institutional review board; participants provided informed consent.
Participants
The coordinator at the Courage Kenny Rehabilitation Institute outpatient brain injury clinic evaluated current outpatients who were not already receiving occupational therapy for study eligibility, referring those who met the following inclusion criteria to the study: age ≥18 yr, brain injury–related executive function deficits on testing or evidenced by program goals, ability to transfer newly learned cognitive strategies from clinic sessions to home, ability to speak English, ability to see and hear (with or without correction or hearing device), ability to write or print responses on worksheets and questionnaires, and living independently in the community. Prospective participants were excluded if they had unstable mental health conditions that could interfere with engagement, learning, session participation, and adherence to home practice or if they required supervision or assistance to perform basic self-care tasks.
Prospective participants were further screened for inclusion by the principal investigator (Radomski) through a telephone interview in which they answered the eight questions that compose the PROMIS v1.0 Applied Cognition–Abilities Short Form 8a (National Institutes of Health, 2015). Those who answered sometimes, often, or very often to three of the four questions about problems with cognition-based occupational performance were invited to participate in the study.
Procedure and Data Collection
Each participant was seen in a private office by one of two occupational therapist investigators (Radomski and Zola), who administered assessments and provided the study intervention.
Measurement
The Canadian Occupational Performance Measure (COPM; Law et al., 1990) was administered before the intervention began to identify the three areas that participants most wanted to address in therapy. The COPM is a reliable and valid semistructured interview in which examinees rate their performance and satisfaction with performance specific to valued occupations (Eyssen, Beelen, Dedding, Cardol, & Dekker, 2005; Trombly, Radomski, & Davis, 1998). COPM average scores were calculated as the mean of the three individual scores on the Performance and Satisfaction domains.
Goal attainment scaling (GAS) provides a criterion-referenced measure of goal achievement that can be aggregated across participants who are receiving the same general intervention but who have different goals (Trombly et al., 1998). Each GAS outcome criterion is operationalized on a 5-point scale (–2 to +2) in which each point difference represents a plausible level of change. The GAS standardized score has a mean of 50 and a standard deviation of 10.
GAS criteria were developed by the participants’ occupational therapists with participant input for each of the three problem areas identified in the COPM interview. To assign postintervention GAS scores, the therapists interviewed the participants at a posttest session about the nature and frequency of goal-related behaviors and activities performed in the prior week. GAS scores were calculated using the equation described by Ottenbacher and Cusick (1990).
We used a scoring rubric based on work by van Osch, Lechner, Reubsaet, and De Vries (2010) to evaluate the quality of participants’ goal-related implementation intentions. This rubric uses two scales of 0–2 points to rate the specificity of (1) the if/when (trigger) and (2) the then (action) components of the implementation intention. Ratings on the two scales are added, resulting in up to 4 points total for each implementation intention. Higher scores signify sufficiently specific implementation intention statements, which are thought to be most effective in prompting action (van Osch et al., 2010). During data collection, the participants’ implementation intentions were transcribed from voicemail by their therapists. After data collection was completed, the two occupational therapists independently scored the quality of both participants’ implementation intentions. Scoring disagreements were resolved by discussion.
Intervention
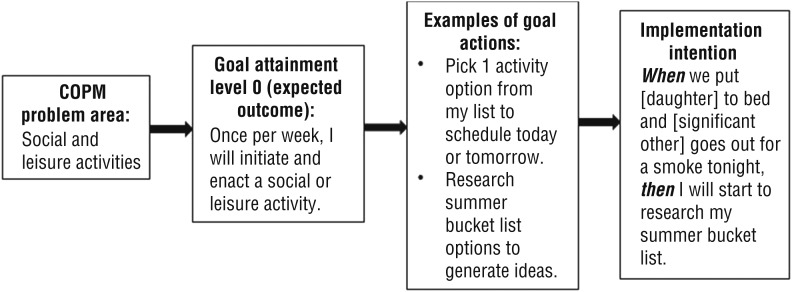
The manualized study intervention was composed of six 60-min sessions involving both individualized MSI and instruction in implementation intentions. During the MSI component, the occupational therapists helped the participants develop an array of feasible and desirable goal actions that aligned with their three COPM goal areas. Also, the therapists taught participants to use cognitive assistive technology, planning and prioritizing strategies, and new routines in the service of their goals. During the implementation intention component, the therapists provided explanation and structured activities to help participants learn to set implementation intentions for time-based, event-based, and emotion-based triggers. (Examples of implementation intentions training methods are available online at http://otjournal.net; navigate to this article, and click on “Supplemental.”) Participants were assigned to write an implementation intention related to one of their goals each day and to report it in a voicemail message to their therapist; the therapists provided feedback regarding homework follow-through and implementation intention quality. Figure 1 illustrates the relationship between one of the COPM problem areas, the goal specific to the expected outcome, possible actions in service of the goal, and an example of a related implementation intention.
Figure 1.
Example of the linkage between a problem area, goal, actions, and implementation intention.
Note. COPM = Canadian Occupational Performance Measure.
The occupational therapists adhered to the ACTION intervention as verified by checkoffs of key components in the administration manual. One participant attended two sessions per week over 3 wk as planned, and the other attended six sessions scheduled over 6 wk.
Results
Two women with mTBI enrolled in the study (Table 1). Both had completed some postsecondary education, sustained their injury in a motor vehicle crash, and were employed full time at the same position they had held before the mTBI (manager in a retail context and paraprofessional in a corporate context).
Table 1.
Participant Characteristics
| Characteristic | Participant 1 | Participant 2 |
| Age, yr | 42 | 40 |
| Time from onset of mild traumatic brain injury to study intervention | 2 yr, 9 mo | 1 yr, 6 mo |
Assessment Results
Both participants selected home and work management as among their top problem areas and priorities, but they had different specific concerns (Table 2). The participants improved on both COPM Performance and Satisfaction scores, as shown in Table 3 and exceeded minimal detectable change values (Davidson et al., 2015). Their posttest GAS scores of >50 (61.0 and 54.4) indicate better-than-expected goal achievement (Ottenbacher & Cusick, 1990).
Table 2.
Goal Areas for Which Participants Set Implementation Intentions
| Order of Importance | Goal Areas | |
| Participant 1 | Participant 2 | |
| 1 | Work (has difficulty managing multiple tasks; has unreliable follow-through despite long hours) | Social and leisure activities (doesn’t initiate activities) |
| 2 | Home management (is disorganized; is inconsistent in chores and errands) | Work (has no system for organizing work tasks; is overwhelmed and embarrassed about follow-through) |
| 3 | Energy (has no energy after work for self-care or socializing) | Home management (doesn’t perform routine chores) |
Table 3.
COPM, GAS, and Implementation Intention Quality Scores
| Measure | Participant 1 | Participant 2 |
| COPM average preintervention scores: Performance, Satisfaction | 3.7, 3.3 | 3.3, 1.3 |
| COPM average postintervention scores: Performance, Satisfaction | 6.0, 6.0 | 5.0, 3.3 |
| Change in COPM average pre- to postintervention scores: Performance, Satisfaction | 2.3, 2.7 | 1.7, 2.0 |
| Posttest GAS scores | 61.0 | 54.4 |
| Homework II scores: No. of IIs assigned 4 of 4 points | 9 of 9 | 11 of 11 |
| No. of Homework IIs set for each goal area: | ||
| 1 | 5 of 9 | 3 of 11 |
| 2 | 2 of 9 | 4 of 11 |
| 3 | 2 of 9 | 4 of 11 |
Note. COPM = Canadian Occupational Performance Measure; GAS = goal attainment scaling; II = implementation intention.
Implementation Intentions
Participant 1 generated most of her nine homework implementation intentions related to one primary goal area, managing work-related challenges, and Participant 2 distributed her 11 implementation intentions fairly evenly across all of her goals (Table 3). All homework implementation intentions received perfect scores (4/4 points), indicating that it was relatively easy for the participants to learn how to write implementation intentions with no observable learning curve.
In a posttest experience survey, both participants indicated that it was somewhat difficult to come up with implementation intentions related to their goals (7 and 8 on a 1–10 scale in which 10 = very difficult), but both found it useful to do so (7 and 8 on a 0–10 scale in which 10 = very useful).
Discussion
The findings from this study suggest that the manualized MSI–implementation intention intervention was feasible to provide to people with mTBI. Two participants with mTBI demonstrated that they were able to learn to set implementation intentions related to three self-identified occupational therapy goals as evidenced by perfect quality scores on homework implementation intentions.. Additionally, both participants reported improved occupational performance as measured by the COPM and GAS after the intervention. Unlike most studies of implementation intentions that report on the effectiveness of implementation intentions in enhancing performance of a single goal behavior, typically designated by investigators (e.g., Prestwich et al., 2012), these two participants demonstrated competence in setting implementation intentions related to their own goals associated with real-world problems after mTBI.
One participant completed all six sessions within the planned 3-wk period; the other was unable to do so primarily because of the demands of full-time employment. With only 2 participants, we do not know whether extending the six sessions over a longer period of time had a positive or detrimental impact on outcome. Ultimately, both participants were readily able to write implementation intentions to a high standard, described the intervention as useful or very useful, and advanced their self-identified goals over the course of the ACTION intervention.
The study intervention combined MSI with training in implementation intentions; we cannot say whether one approach had more influence on outcomes than the other. It may be that the implementation intention and MSI approaches provided complementary benefits. The MSI component of the intervention enabled the participants to identify new strategies to address occupational performance problems, whereas the implementation intention component facilitated the implementation of the new strategy in daily life. For example, as part of the MSI intervention, both participants developed checklists to help them establish more effective household routines. They then developed implementation intentions to enable them to actually use the checklists on a given day. Even though the participants appeared to readily learn the mechanics of writing effective implementation intentions, they reported that it was difficult to do so in daily life because it was challenging to generate a wide array of daily actions that aligned with their ultimate goals and to anticipate triggers they were likely to encounter so as to implement the goal-directed behavior at the right time.
In general, MSI addresses changes in cognitive functioning by helping clients learn self-management skills, strategies, and behavioral routines (Tate et al., 2014). MSI is most effective when intervention supports the acquisition, real-life implementation, and generalization of new, goal-relevant skills, strategies, and routines (Geusgens, Winkens, van Heugten, Jolles, & van den Heuvel, 2007). By specifying the if/when (environmental or situational triggers) and then of new behaviors, implementation intentions may prove to extend MSI outcomes and client adaptation by facilitating the enactment of newly learned skills, strategies, and routines in varied life contexts.
Limitations and Future Research
This study represents a very preliminary step in examining the potential impact of teaching clients to use implementation intentions as a booster to goal achievement in occupational therapy. No control condition was used, and no attempt was made to disentangle the relative impact of the MSI and the implementation intention training on participant performance or the relative contributions of the subcomponents of the implementation intention-setting procedure. This feasibility study did little to elucidate the populations for whom the ACTION intervention is most appropriate.
We relied primarily on professionals from a brain injury clinic to determine whether participants met inclusion and exclusion criteria. The precise means by which the clinic coordinator assessed patients for potential study eligibility were unknown, and compliance with inclusion criteria could not be verified. Participants’ diagnostic or cognitive test scores also were unavailable to us. Therefore, it is possible that unspecified participant characteristics contributed to study outcomes more than the intervention, further limiting generalization of findings.
Finally, participants reported problems in both generating goal-relevant implementation intentions and determining the most appropriate triggers. Future versions of this intervention approach should include more and varied practice opportunities for anticipating and identifying triggers. Because successful use of implementation intentions appears to require self-awareness, anticipation, and the ability to generate new potential responses, this approach may not be appropriate for people with severe cognitive impairment (Clark-Wilson et al., 2014).
Future research must elucidate the potential benefit and clinical utility of combining implementation intention training with MSI as well as the critical instructional parameters (e.g., best candidates, dosage, duration). Future studies must also specify training of assessors to score the implementation intentions and interrater reliability if more than one rater is involved.
Implications for Occupational Therapy Practice
The results of this study have the following implications for occupational therapy practice:
Cognitive intervention that combines MSI with training in implementation intentions may enhance individualized goal setting and attainment in occupational therapy for clients with mTBI and can be considered as a treatment option.
Future research is needed to better define and develop the intervention, provide guidelines and options within the six-session intervention package, and rigorously evaluate its effectiveness in treating people with mTBI.
Conclusion
We present very preliminary evidence that a six-session intervention combining MSI and implementation intention training may help people with mTBI learn to set implementation intentions and make progress toward their own goals. Considerable work is still required to establish the effectiveness of implementation intention training as part of a package of occupational therapy interventions for people with mTBI-related cognitive impairment.
Acknowledgments
This pilot work was conducted as part of a larger study funded by the U.S. Army Medical Research Materiel Command (W81XWH-13-1-0198), which involved a small randomized controlled trial registered at clinicaltrials.gov (NCT02352441).
Contributor Information
Mary Vining Radomski, Mary Vining Radomski, PhD, OTR/L, FAOTA, is Senior Scientific Adviser, Courage Kenny Research Center, Minneapolis, MN; mary.radomski@allina.com.
Gordon Giles, Gordon Giles, PhD, OTR/L, FAOTA, is Professor, Samuel Merritt University, Oakland, CA.
Marsha Finkelstein, Marsha Finkelstein, MS, is Senior Scientific Adviser, Courage Kenny Research Center, Minneapolis, MN.
Jenny Owens, Jenny Owens, OTD, OTR/L, is Research Occupational Therapist, Oak Ridge Associated Universities, Oak Ridge, TN.
Mark Showers, Mark Showers, MSOT, OTR/L, is Lead Occupational Therapist, Fort Campbell Intrepid Spirit, Fort Campbell, KY.
Joette Zola, Joette Zola, OTR/L, is Occupational Therapist, Courage Kenny Rehabilitation Institute, Minneapolis, MN.
References
- Bayer U. C., Achtziger A., Gollwitzer P. M., & Moskowitz G. (2009). Responding to subliminal cues: Do if–then plans cause action preparation and initiation without conscious intent? Social Cognition, 27, 183–201. https://doi.org/10.1521/soco.2009.27.2.183 [Google Scholar]
- Burkard C., Rochat L., Blum A., Emmenegger J., Juillerat Van der Linden A. C., & Van der Linden M. (2014). A daily-life-oriented intervention to improve prospective memory and goal-directed behaviour in ageing: A pilot study. Neuropsychological Rehabilitation, 24, 266–295. https://doi.org/10.1080/09602011.2014.887023 [DOI] [PubMed] [Google Scholar]
- Clark-Wilson J., Giles G. M., & Baxter D. M. (2014). Revisiting the neurofunctional approach: Conceptualizing the core components for the rehabilitation of everyday living skills. Brain Injury, 28, 1646–1656. https://doi.org/10.3109/02699052.2014.946449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson L., Hammond C. S., Mashima P., Nitta L., Owens J., & Radomski M., . . . Zola J. (2015). Performance and self-management, work, social, and school roles. In Weightman M., Radomski M., Mashima P., & Roth C. (Eds.), Mild traumatic brain injury toolkit (pp. 335–448). Fort Sam Houston, TX: Borden Institute. [Google Scholar]
- Eyssen I. C. J. M., Beelen A., Dedding C., Cardol M., & Dekker J. (2005). The reproducibility of the Canadian Occupational Performance Measure. Clinical Rehabilitation, 19, 888–894. https://doi.org/10.1191/0269215505cr883oa [DOI] [PubMed] [Google Scholar]
- Geusgens C. A. V., Winkens I., van Heugten C. M., Jolles J., & van den Heuvel W. J. A. (2007). Occurrence and measurement of transfer in cognitive rehabilitation: A critical review. Journal of Rehabilitation Medicine, 39, 425–439. https://doi.org/10.2340/16501977-0092 [DOI] [PubMed] [Google Scholar]
- Gollwitzer P. M. (1999). Implementation intentions: Strong effects of simple plans. American Psychologist, 54, 493–503. https://doi.org/10.1037/0003-066X.54.7.493 [Google Scholar]
- Gollwitzer P. M., & Brandstätter V. (1997). Implementation intentions and effective goal pursuit. Journal of Personality and Social Psychology, 73, 186–199. https://doi.org/10.1037/0022-3514.73.1.186 [DOI] [PubMed] [Google Scholar]
- Harris P. R., Brearley I., Sheeran P., Barker M., Klein W. M., Creswell J. D., . . . Bond R. (2014). Combining self-affirmation with implementation intentions to promote fruit and vegetable consumption. Health Psychology, 33, 729–736. https://doi.org/10.1037/hea0000065 [DOI] [PubMed] [Google Scholar]
- Kardiasmenos K. S., Clawson D. M., Wilken J. A., & Wallin M. T. (2008). Prospective memory and the efficacy of a memory strategy in multiple sclerosis. Neuropsychology, 22, 746–754. https://doi.org/10.1037/a0013211 [DOI] [PubMed] [Google Scholar]
- Law M., Baptiste S., McColl M., Opzoomer A., Polatajko H., & Pollock N. (1990). The Canadian Occupational Performance Measure: An outcome measure for occupational therapy. Canadian Journal of Occupational Therapy, 57, 82–87. https://doi.org/10.1177/000841749005700207 [DOI] [PubMed] [Google Scholar]
- Lengfelder A., & Gollwitzer P. M. (2001). Reflective and reflexive action control in patients with frontal brain lesions. Neuropsychology, 15, 80–100. https://doi.org/10.1037/0894-4105.15.1.80 [DOI] [PubMed] [Google Scholar]
- Levine B., Robertson I. H., Clare L., Carter G., Hong J., & Wilson B. A., . . . Stuss D. T. (2000). Rehabilitation of executive functioning: An experimental–clinical validation of Goal Management Training. Journal of the International Neuropsychological Society, 6, 299–312. https://doi.org/10.1017/S1355617700633052 [DOI] [PubMed] [Google Scholar]
- Levine B., Schweizer T. A., O’Connor C., Turner G., Gillingham S., Stuss D. T., . . . Robertson I. H. (2011). Rehabilitation of executive functioning in patients with frontal lobe brain damage with Goal Management Training. Frontiers in Human Neuroscience, 5, 9 https://doi.org/10.3389/fnhum.2011.00009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institutes of Health. (2015). PROMIS Applied Cognition–Abilities. Retrieved from https://www.assessmentcenter.net/documents/PROMIS%20Applied%20Cognitive%20Abilities%20Scoring%20Manual.pdf
- Ottenbacher K. J., & Cusick A. (1990). Goal attainment scaling as a method of clinical service evaluation. American Journal of Occupational Therapy, 44, 519–525. https://doi.org/10.5014/ajot.44.6.519 [DOI] [PubMed] [Google Scholar]
- Prestwich A., Conner M. T., Lawton R. J., Ward J. K., Ayres K., & McEachan R. R. (2012). Randomized controlled trial of collaborative implementation intentions targeting working adults’ physical activity. Health Psychology, 31, 486–495. https://doi.org/10.1037/a0027672 [DOI] [PubMed] [Google Scholar]
- Radomski M. V., Anheluk M., Bartzen M. P., & Zola J. (2016). Effectiveness of interventions to address cognitive impairments and improve occupational performance after traumatic brain injury: A systematic review. American Journal of Occupational Therapy, 70, 7003180050 https://doi.org/10.5014/ajot.2016.020776 [DOI] [PubMed] [Google Scholar]
- Salomon G., & Perkins D. N. (1989). Rocky roads to transfer: Rethinking mechanisms of a neglected phenomenon. Educational Psychologist, 24, 113–142. https://doi.org/10.1207/s15326985ep2402_1 [Google Scholar]
- Scholz U., La Marca R., Nater U. M., Aberle I., Ehlert U., Hornung R., . . . Kliegel M. (2009). Go no-go performance under psychosocial stress: Beneficial effects of implementation intentions. Neurobiology of Learning and Memory, 91, 89–92. https://doi.org/10.1016/j.nlm.2008.09.002 [DOI] [PubMed] [Google Scholar]
- Tate R., Kennedy M., Ponsford J., Douglas J., Velikonja D., Bayley M., & Stergiou-Kita M. (2014). INCOG recommendations for management of cognition following traumatic brain injury, Part III: Executive function and self-awareness. Journal of Head Trauma Rehabilitation, 29, 338–352. https://doi.org/10.1097/HTR.0000000000000068 [DOI] [PubMed] [Google Scholar]
- Trombly C. A., Radomski M. V., & Davis E. S. (1998). Achievement of self-identified goals by adults with traumatic brain injury: Phase I. American Journal of Occupational Therapy, 52, 810–818. https://doi.org/10.5014/ajot.52.10.810 [DOI] [PubMed] [Google Scholar]
- van Osch L., Lechner L., Reubsaet A., & De Vries H. (2010). From theory to practice: An explorative study into the instrumentality and specificity of implementation intentions. Psychology and Health, 25, 351–364. https://doi.org/10.1080/08870440802642155 [DOI] [PubMed] [Google Scholar]
- Varley R., Webb T. L., & Sheeran P. (2011). Making self-help more helpful: A randomized controlled trial of the impact of augmenting self-help materials with implementation intentions on promoting the effective self-management of anxiety symptoms. Journal of Consulting and Clinical Psychology, 79, 123–128. https://doi.org/10.1037/a0021889 [DOI] [PubMed] [Google Scholar]