Abstract
Background
Knowledge about their past medical history is central for childhood cancer survivors to ensure informed decisions in their health management. Knowledge about information provision and information needs in this population is still scarce. We thus aimed to assess: (1) the information survivors reported to have received on disease, treatment, follow-up, and late effects; (2) their information needs in these four domains and the format in which they would like it provided; (3) the association with psychological distress and quality of life (QoL).
Procedure
As part of the Follow-up survey of the Swiss Childhood Cancer Survivor Study, we sent a questionnaire to all survivors (≥18 years) who previously participated to the baseline survey, were diagnosed with cancer after 1990 at an age of <16 years.
Results
Most survivors had received oral information only (on illness: oral: 82%, written: 38%, treatment: oral: 79%, written: 36%; follow-up: oral: 77%, written: 23%; late effects: oral: 68%, written: 14%). Most survivors who had not previously received any information rated it as important, especially information on late effects (71%). A large proportion of survivors reported current information needs and would like to receive personalized information especially on late effects (44%). Survivors with higher information needs reported higher psychological distress and lower QoL.
Conclusions
Survivors want to be more informed especially on possible late effects, and want to receive personalized information. Improving information provision, both qualitatively and quantitatively, will allow survivors to have better control of their health and to become better decision makers.
Keywords: childhood cancer survivors, cohort study, information needs, information provision, questionnaire survey
Introduction
Informing childhood cancer survivors about diagnosis, treatment received, the appropriate long-term care plan and the risk for co-morbidity is central for their understanding of the disease. Another important aspect beside information provision to patients is the concept of patients’ information needs, which is considered as the foundation from which to develop patient-centered services [1]. Information needs has been defined as the patient’s “recognition that the knowledge is inadequate to satisfy a goal, within the context/situation that they find themselves at a specific point in time” [2]. Cancer patients who are knowledgeable about their medical history are better decision makers, adhere more to the prescribed care-plan, show lower levels of distress and higher quality of life (QoL), have a greater sense of control and have less information needs [3,4]. A well informed patient is even more important in rare diseases, such as childhood cancer, where the patient needs to be able to actively interact with health care providers, who often lack specific knowledge and expertise due to the low prevalence of such diseases [5,6]. Patients’ information provision and needs in pediatric chronic diseases is fundamental for another reason. Often, due to the patient’s age, information is not directly given to them, but to the parents who are the child’s legal guardians. However, patients need to know about their past medical history to take over responsibility of their health once they reach adult age. Studies of Europe and North America showed that one in two childhood cancer survivors lacks the knowledge about the treatment they received and many are not even aware of their initial diagnosis [7–9].
Research investigating the information provision and the information needs in childhood cancer survivors is scarce. Two studies on this topic found that all childhood cancer survivors would like to receive more information on late effects (e.g., fertility) and survivorship [10,11]. One study assessing information needs in adolescent and young adult cancer survivors, reported that the majority wanted more information especially on late-effects and cancer recurrence [12]. Studies addressing the satisfaction with information in patients with adult cancers showed that patients are generally unsatisfied with the quality and amount of information received [13,14].
In the present study we aimed at extending the body of knowledge on the subject by looking at the situation in Switzerland. We had three main aims: (1) to assess the information survivors reported to have received from a medical professional at any time; and to compare survivors who received information with those who did not; (2) to assess survivors’ information needs at the time of study, and compare survivors with and without information needs; (3) determine whether information needs were associated with higher psychological distress and lower QoL.
Methods
Sample and Procedure
Since 1976 the population-based Swiss Childhood Cancer Registry (SCCR) has been collecting data on all cancer patients younger than 21 years at diagnosis who are diagnosed with leukemia, lymphoma, central nervous system (CNS) tumors, malignant solid tumors or Langerhans cell histiocytosis [15,16]. The Swiss Childhood Cancer Survivor Study (SCCSS) is a questionnaire survey which includes a baseline and a follow-up questionnaire (sent approximately 3 years apart) [17]. Inclusion criteria for the follow-up questionnaire were: having participated in the baseline survey, being diagnosed with childhood cancer after 1990, having survived ≥5 years and being older than 18 years at the time of the study. Eligible survivors received a questionnaire with a prepaid return envelope. If they did not reply within 2 months, non-responders received the questionnaire a second time with a reminder letter and another prepaid return envelope.
The follow-up questionnaire assessed various domains including follow up care, information provision, transition, psychological distress and QoL. The questionnaires were available in German and French. Ethics approval was provided through the general cancer registry permission of the SCCR (The Swiss Federal Commission of Experts for Professional Secrecy in Medical Research) and a non-obstat statement was obtained from the ethics committee of the Canton of Bern.
Reported Information Received
In a first question survivors could indicate whether they had ever received information from a medical doctor on illness, treatment, follow-up care and late effects and, if they did, in which format they had received it (orally or written), or if they had not received any information. In case they had not received any information, they were asked to judge the importance this information would have had. They could rate the importance using a three-point scale ranging from “very important” to “not important” (Supplemental Table I).
Information Needs
In a second question survivors could indicate their information needs in four domains: on illness, treatment, follow-up and late effects. In particular, survivors could indicate whether they would like to receive (1) oral information from a doctor, (2) general written information, (3) personal written information, and (4) information online. Survivors could also indicate whether they did not wish to receive information. For the second part of the analysis we created a binary variable: has information needs (if answered affirmatively in one of the afore-mentioned four domains) versus no information needs (if answered negatively to all four domains) (Supplemental Table I).
Variables Extracted From the SCCR
Baseline demographic data and prospectively collected medical information on diagnosis and treatment of survivors were extracted from the Swiss Childhood Cancer Registry: age, gender, cancer diagnosis, year of diagnosis, age at diagnosis, cancer treatment, time since diagnosis and type of clinic.
The International Classification of Childhood Cancer—3rd Edition was utilized to classify diagnosis [18]. Treatment was classified as having had surgery (yes/no), having received chemotherapy (yes/no), having had radiotherapy (no radiotherapy, body and limb irradiation, cranio-spinal irradiation), and having had bone marrow transplantation (BMT; yes/no). Year of diagnosis was categorized in three categories (<1995, 1995–2000, ≥2001) chosen to evenly distribute data. Type of clinic was coded into big clinic if they had ≥35 cases per year and small clinic if they had <35 cases per year (Supplemental Figure 1).
Variables From the Baseline Questionnaire
Migration background was assessed by questionnaire. Participants were classified as having a migrant background if they were not Swiss citizens since birth, not born in Switzerland, or had at least one parent who was not Swiss citizen. We also assessed selfreported late-effects (yes/no) and asked whether they had received a checklist after discharge (yes/no) (Supplemental Figure 1).
Variables From the Follow-Up Questionnaire
Survivors’ education was divided into four categories: primary (compulsory schooling only); secondary (including vocational training, teachers, technical and commercial schools, etc.); tertiary (including university and university of applied sciences) and unknown education [19,20].
Psychological distress was assessed using the Brief Symptom Inventory-18 (BSI-18) [21]. The inventory yields three scales (somatization, depression, and anxiety) and a Global Severity Index (GSI). Patients were asked to report their degree of distress in the past 7 days using a 4-point scale ranging from “not at all” to “a lot.” To categorize individuals with psychological distress sum raw scores were standardized into T-scores (mean = 50, SD = 10). For the present study we used survivors’ T-scores on the three scales somatization, depression and anxiety. Higher scores on the BSI-18 refer to higher levels of distress.
Health related quality of life (HRQoL) was assessed using the Short-Form 12 (SF-12) [22]. The SF-12 yields two summary scores: physical component summary (PCS) and mental component summary (MCS). Scores were T-standardized with a mean of 50 and standard deviation of 10. Higher scores represented better HRQoL. The test showed good retest-reliability (between 0.76 and 0.89) and validity [22] (Supplemental Figure 1).
Statistical Analyses
We performed all analyses using Stata 12.0 (StataCorp, College Station, TX).
We computed Chi-square statistics for categorical variables and t-tests for continuous variables to compare questionnaire responders with non-responders. For both aims we used percentages to summarize our data and we calculated confidence intervals using Jeffrey’s method for small samples [23]. For group comparisons we used chi square statistics for categorical variables and t-tests for continuous variables. To assess the association between information needs and psychological distress and QoL we ran multivariable linear regressions adjusting for socio-demographic and clinical factors.
Results
Characteristics of the Study Population
Of the eligible 754 survivors we traced and contacted 720 (Supplemental Figure 2). Of those, 322 (45%) returned a questionnaire. In the final analysis we could include 319, after excluding 3 (0.5%) filled out by their parents. More participants (n = 319) compared to non-participants (n = 388; Table I) were female (56% vs. 42%; P = 0.001), were treated with chemotherapy (85% vs. 79%; P = 0.043) and reported to suffer from late effects (41% vs. 33%; P = 0.026; Table I). They did not differ by migration background, language region of Switzerland, surgery, radiotherapy, bone marrow transplantation, relapse status, type of treating clinic, age at study, age at diagnosis and time since diagnosis (Table I).
Table I. Characteristics of the Study Population, Comparing Survivor Participants and Non-Participants.
| Participants (n = 319) |
Non-participantsa (n = 388) |
|||||
|---|---|---|---|---|---|---|
| n | %c | n | %c | P-Valueb | ||
| Sex | ||||||
| Male | 140 | 44 | 223 | 58 | 0.001 | |
| Female | 179 | 56 | 165 | 42 | ||
| Language region | ||||||
| German | 238 | 75 | 290 | 75 | 0.967 | |
| French/Italian | 81 | 25 | 98 | 25 | ||
| Migration background | ||||||
| None (Swiss) | 293 | 92 | 349 | 90 | 0.422 | |
| Other countries | 25 | 8 | 37 | 10 | ||
| Education | ||||||
| Primary | 33 | 10 | 48 | 12 | 0.105 | |
| Secondary | 93 | 29 | 131 | 34 | ||
| Tertiary | 59 | 19 | 48 | 13 | ||
| Unknown | 134 | 42 | 161 | 41 | ||
| Diagnosis (ICCC-3) | ||||||
| I Leukemia | 115 | 36 | 121 | 31 | 0.648 | |
| II Lymphoma | 59 | 18 | 81 | 21 | ||
| III CNS tumor | 38 | 11 | 62 | 16 | ||
| IV Neuroblastoma | 8 | 4 | 12 | 5 | ||
| V Retinoblastoma | 5 | 2 | 9 | 2 | ||
| VI Renal tumor | 21 | 6 | 19 | 5 | ||
| VII Hepatic tumor | 1 | 1 | 2 | 1 | ||
| VIII Bone tumor | 22 | 7 | 23 | 6 | ||
| IX Soft tissue sarcoma | 20 | 6 | 18 | 5 | ||
| X Germ cell tumor | 9 | 3 | 17 | 3 | ||
| XI and XII Other tumord | 8 | 2 | 5 | 1 | ||
| Langerhans cell histiocytosis | 13 | 4 | 19 | 4 | ||
| Surgery | ||||||
| No | 95 | 30 | 99 | 26 | 0.206 | |
| Yes | 224 | 70 | 289 | 74 | ||
| Chemotherapy | ||||||
| No | 47 | 15 | 82 | 21 | 0.043 | |
| Yes | 272 | 85 | 306 | 79 | ||
| Radiotherapy | ||||||
| No radiotherapy | 195 | 61 | 260 | 67 | 0.741 | |
| Body and limbs radiation | 76 | 24 | 65 | 17 | ||
| Cranio-spinal radiation | 48 | 15 | 63 | 16 | ||
| Bone marrow transplantation | ||||||
| No | 302 | 95 | 363 | 94 | 0.533 | |
| Yes | 17 | 5 | 25 | 6 | ||
| Relapse | ||||||
| No | 281 | 88 | 354 | 91 | 0.168 | |
| Yes | 38 | 12 | 34 | 9 | ||
| Reported late-effects | ||||||
| No | 185 | 59 | 249 | 67 | 0.026 | |
| Yes | 130 | 41 | 123 | 33 | ||
| Treating clinic | ||||||
| University clinic | 239 | 75 | 290 | 75 | 0.956 | |
| Cranio-spinal radiation | 80 | 25 | 98 | 25 | ||
| Participants (n = 319) |
Non-participantsa (n = 388) |
|||||
| Mean | SD | Mean | SD | P-Valuee | ||
| Age at study | 21.3 | 4.1 | 21.7 | 3.8 | 0.852 | |
| Age at diagnosis | 8.9 | 4.7 | 8.9 | 4.5 | 0.512 | |
| Time since diagnosis | 12.5 | 3.8 | 12.8 | 3.6 | 0.857 | |
Note Percentages are based upon available data for each variable. CNS, Central Nervous System; ICCC-3, International Classification of Childhood Cancer—Third Edition.
Non-participants include: 375 survivors who did not respond, 13 who refused to participate (Supplemental Figure 1)
P-Value calculated from Chi-square statistics comparing survivor participants and survivor non-participants
Column percentages are given
Other malignant epithelial neoplasms, malignant melanomas and other or unspecified malignant neoplasms
P-Value calculated on two-sample mean-comparison test (t-test).
Information Received
Reported information received on illness, treatment, follow-up, and late effects
Most survivors reported to have received oral information (Table II). Considerably fewer survivors reported to have received any written information on illness (38%) and treatment (36%), and even fewer on follow-up (23%) or late effects (14%).
Table II. Reported Information Received on Illness, Treatment, Follow-Up and Late Effects by Format (Oral, Written, No Information).
| Type of information |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Oral information |
Written information |
No information |
|||||||
| n | (%) | 95% CIa | n | (%) | 95% CIa | n | (%) | 95% CIa | |
| Illness | 257 | 82 | 77–86 | 120 | 38 | 33–44 | 25 | 8 | 5–11 |
| Treatment | 248 | 79 | 74–83 | 112 | 36 | 31–40 | 34 | 11 | 8–15 |
| Follow-up | 241 | 77 | 72–81 | 72 | 23 | 18–28 | 35 | 11 | 8–14 |
| Late effects | 215 | 68 | 63–73 | 43 | 14 | 10–18 | 77 | 24 | 21–29 |
CI, confidence interval.
Calculated for binomial distribution.
Rating of information
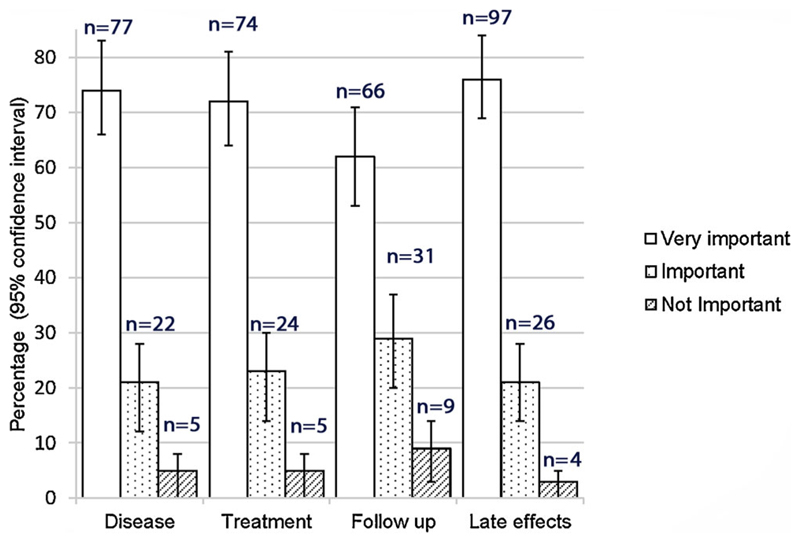
Thirteen survivors (4%) reported to have not received any information at all, 25 (8%) on illness, 34 (11%) on treatment, 35 (11%) on follow-up and 77 (24%) on late effects. When asked to rate the importance of such information, most of these survivors rated it as “very important” or “important” (Fig. 1) in all four domains, and late effects were considered by most as “very important” (76%) and “important” (21%). Only 2–4% rated the information as not important.
Fig. 1.
Survivors’ rating of the information they did not receive. The rating on illness, treatment, follow up, and late effects which they reported not to have received.
Compared to survivors who reported to have received information, survivors who reported not to have received information on treatment were more likely to be treated in a small clinic and to have been diagnosed before 1995 (Supplemental Table II). More survivors who reported not to have received information on follow-up were younger at study, treated in a small clinic and diagnosed before 1995 (Supplemental Table II). When looking at survivors who reported not to have received information on late effects they were more likely to be younger at study and fewer were diagnosed after 1995 and had received chemotherapy (Supplemental Table II).
Information Needs
The majority of survivors (n = 255; 80%) would like to receive more information on late effects irrespective of the format (Table III). Across all four domains most survivors would like to receive information in a written, personal manner (39–44%). The online format was chosen by the fewest participants (11–15%). Many survivors reported to have no need for more information especially on illness (31%), treatment (32%) and follow up (30%). Only 41 survivors (13%) reported not to want information on any topic and in any format. Among these survivors with no information needs, 93% reported to have received information on illness, 94% on treatment, 91% on follow-up and 83% on late effects. Survivors who had information needs in at least one domain did not differ from survivors who had no needs in any of the given domains (Supplemental Table III).
Table III. Information Needs on Illness, Treatment, Follow-Up and Late Effects.
| Overall | Type of information needs | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Any information | Oral information | Written general | Written personal | Online information | No information needs | |||||||
| n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | |
| Illness | 209 | 68 | 84 | 27 | 79 | 25 | 123 | 39 | 42 | 13 | 98 | 31 |
| Treatment | 204 | 64 | 76 | 24 | 69 | 22 | 124 | 39 | 37 | 12 | 100 | 32 |
| Follow-up | 213 | 67 | 92 | 29 | 75 | 24 | 97 | 31 | 33 | 11 | 94 | 30 |
| Late effects | 255 | 80 | 101 | 32 | 93 | 30 | 138 | 44 | 47 | 15 | 54 | 17 |
Information Needs, Psychological Distress and Quality of Life
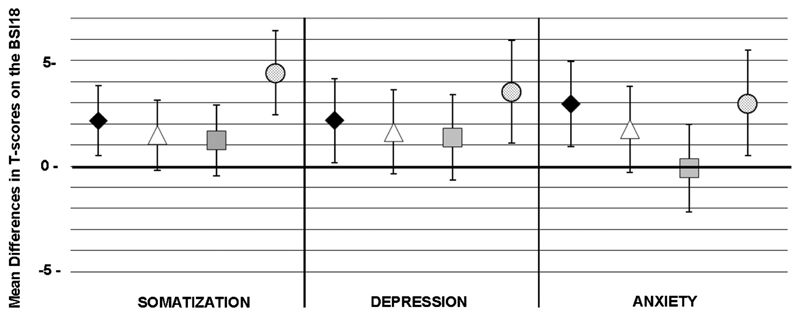
Compared to survivors who did not want to receive further information, survivors who were interested in more information on illness (mean difference Mdiff = 2.14; P = 0.011) and late effects (Mdiff = 4.43; P < 0.001) had significantly higher somatization scores depression scores (Mdiff = 2.17; P = 0.032, and Mdiff = 3.53; P = 0.005) and anxiety scores (Mdiff = 2.95; P = 0.004 and Mdiff = 2.31; P = 0.019) (Fig. 2).
Fig. 2.
Association between psychological distress and information needs on illness, treatment, follow up, and late effects. Mean differences in T-scores and 95% confidence intervals on the three BSI-18 scales (somatization, depression, and anxiety) between survivors with information needs on illness (black diamond), treatment (white triangle), follow-up (gray square), and late effects (dotted circle) versus survivors without information needs. Higher scores indicate higher distress. Means were adjusted for sex, age, language, and diagnosis.
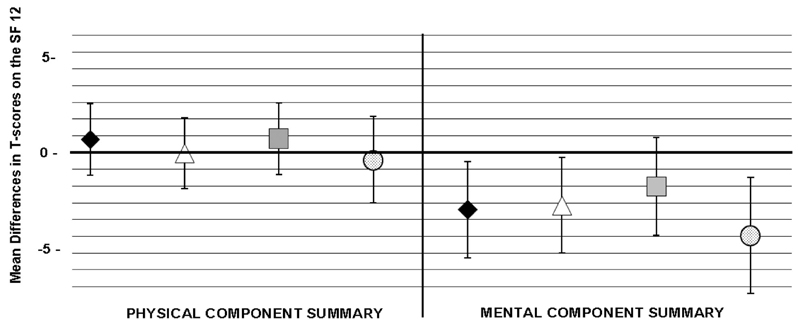
Survivors who did not want more information did not differ from survivors who wished to receive more information on the PCS (Fig. 3). However, on the MCS, survivors who wished to have more information on illness (Mdiff = −3.40; P = 0.020), treatment (Mdiff = −3.16; P = 0.030) and late-effects (Mdiff = −4.94; P = 0.006) had significantly lower scores (Fig. 3).
Fig. 3.
Association between health related quality of life (HRQoL) and information needs on illness, treatment, follow up and late effects. Mean differences in T-scores and 95% confidence intervals on the three SF 12 summary scores scales (Physical component summary, Mental component summary) between survivors with information needs on illness (black diamond), treatment (white triangle), follow-up (gray square) and late effects (dotted circle) versus without information needs. Lower scores indicate lower HRQoL. Means were adjusted for sex, age, language, and diagnosis.
Discussion
In the present study survivors reported to have mostly received oral information or a lack of information on late effects. Those reporting not to have received any information rated it as important independent of the topic. Survivors wished to receive more information especially written and in a more personal manner. Interestingly, not many survivors indicated that they would like to receive information online, and a substantial proportion of survivors did not want to have more information on certain topics. However, the latter group was composed of survivors who reported to have receive information previously (both orally and written). Information need was associated with higher levels of psychological distress and lower QoL.
A major strength of this study is the population-based sample of survivors with prospectively collected data on the cancer-related factors from the Swiss Childhood Cancer Registry and data available from the baseline and follow-up questionnaires from the Swiss Childhood Cancer Survivor Study. A limitation might be self-selection because survivors of specific groups may have been more reluctant to complete the questionnaire, especially after having filled in the baseline questionnaire. Other groups may not have been in the position to complete it due to severe late-effects or impairments or due to the lack of interest in the topic. The response rate was 45%. Although this could be a major limitation in a recent study it was shown that a low response rate does not seem to introduce non-response bias in this population [24]. When assessing the information a patient reported to have received, we have to take into account that the person might have received it, but did not understand it, forgot it or the information might have been given to parents. Caution is required when drawing conclusions with such data.
This is a relatively new field of research with few studies having been published on the subject in pediatric oncology. We found two studies which assessed information needs in childhood cancer survivors. One is a mixed methods study [11] assessing the information needs of families within the first year post-treatment. Participants were mostly unsatisfied with the information they received about fertility and long-term coping with survivorship. They also found that a considerable proportion of survivors had no need for further information to prepare for the post-treatment phase, which is in line with our results. The other study [10] showed that information on late-effects (how to recognize late effects, personalized information) is a high priority for survivors. However, this study may be difficult to generalize because all participants were recruited within a follow-up program and are thus probably more interested in such matters than survivors who were lost to follow-up or did not agree to participate.
When looking at research outside pediatric oncology, we see that information provision is a matter of interest also in other disciplines. A study on survivors of endometrial cancer [14] reported that a considerable number of survivors was not aware having received information on possible side effects and aftercare. Another study [13] assessing information satisfaction in a group of survivors of lymphoma and multiple myeloma found that the majority was satisfied but one third still had unmet needs for information. In line with our findings, a systematic review [3] assessing the relation between information provision and psychological distress and QoL, showed that dissatisfaction with information provision is associated with higher levels of depression and anxiety, and, to a lower extent, with reduced QoL.
In this study we showed that survivors are not completely uninformed, but there is considerable room for improvement. The majority of survivors seem to receive oral information, a format which has its limits. While it is excellent for making the communication informal and more personal it might be short lived. Orally communicated information on treatment and disease is likely to be forgotten within no time by the majority of lay persons. Moreover, in the pediatric oncology setting, information is mostly communicated to parents and not to the patients themselves, especially if the children are young. This could explain the wish of many survivors to receive personalized written information. The disease by itself and its treatment seem to be the two topics which already receive more attention. Information on follow up and especially on late effects is still lacking. Interestingly only a minority of survivors would like to find more information on the internet. This might be due to a lack of individualized information, the difficulty of retrieving trustworthy information in the plethora of online offers or the lack of internet access. The plethora of information available online makes it hard to distinguish between credible and less reliable sources. However, this will probably be the format chosen in the future because of its accessibility, lower costs and broad availability. Professionals caring for survivors should develop official online platforms with credible high quality health information, which can be easily traced and trusted by interested patients.
In the group of survivors without any information needs, almost all reported to have received information. This shows that information should be tailored to the different groups, according to the various stages of survivorship and their personal wishes [25]. Like other studies, we showed that survivors who did not receive information did not differ socio-demographically or clinically from survivors who did receive information. Caution is required because these findings might have been influenced by the small sample size of the present study. The same was found when comparing survivors not wanting more information with survivors who wished to receive additional information.
Finally, we showed that survivors with information needs tend to have higher levels of psychological distress and lower QoL [25]. These results confirm what previous research [3] has shown on the role of information provision in improving quality of survivorship.
Information provision should be improved because it is through patients’ education that better adherence to follow-up care can be achieved [26] and quality of survivorship increased. The importance of information provision is advocated in several guidelines [27,28]. An open question remains about who should be providing the information, in which format and at which time point (e.g., at treatment completion, at discharge or when the patient reaches adult age). Because the number of long-term survivors is rapidly growing, pediatric oncologists are progressively lacking resources for assuming both further improvements in survival for newly diagnosed patients and better quality of follow-up care for survivors [11]. In the future, other groups of professionals (e.g., nurses, social workers, and psychologists) or internet-based resources could take over this important duty of offering improved long-term care to survivors, at least in part. Pediatric oncologists will still need to inform patients and families orally, because of their specific knowledge of potential late effects in their former patients. We suggest them developing written and personalized information about diagnosis, treatment received and expected late effects as well as a follow-up plan in the format of a “survivorship passport” or on the internet in a members’ area of a dedicated webpage. This would allow survivors to gain independence, self-control and motivation to follow a healthy life-style. This is particularly important during the critical time of transition to adult care when survivors start taking over responsibility for their health because if not well informed and aware of the importance of continued medical care, the patients may be lost to follow up. An informed patient can also be more interactive with the new adult caregiver and this may help the latter to further motivate the patient to adhere to follow up visits and to promote healthy lifestyles. Finally, information provision should reach the whole population of survivors, even those in the lowest risk groups [29].
Survivors want to be more informed especially on possible late effects and want to receive personalized information in a written format. Improving information provision, both in quality and quantity, will allow survivors to have better control of their health and become better decision makers and, consequently, have higher QoL.
Supplementary Material
Additional Supporting Information may be found in the online version of this article at the publisher’s web-site.
Acknowledgements
We thank all survivors and their families for participating in our survey. We thank Anna Hohn and Zina Heg-Bachar for their help with the questionnaire survey. This study was supported by the Swiss National Science Foundation (GM: Ambizione Fellowship grant PZ00P3_121682/1 and PZ00P3_141722; SE: MD-PhD fellowship grant 323630-133897). Swiss Cancer League (KLS-01605-10-2004, KLS-2215-02-2008, KLS-02783-02-2011), Cancer Research Switzerland (02606-06-2010 and 02631-08-2010), Cancer League Aargau, Cancer League Zurich, Swiss Bridge and Stiftung zur Krebsbekämpfung. The work of the Swiss Childhood Cancer Registry is supported by the Swiss Paediatric Oncology Group, Kinderkrebshilfe Schweiz, Stiftung für krebskranke Kinder Regio Basiliensis, Schweizerische Konferenz der kantonalen Gesundheitsdirektorinnen und—direktoren (GDK) and numerous other sponsors.
Grant sponsor: Swiss National Science Foundation; Grant numbers: PZ00P3_121682/1; PZ00P3_141722; 323630-133897; Grant sponsor: Swiss Cancer League; Grant numbers: KLS-01605-10-2004; KLS-2215-02-2008; KLS-02783-02-2011; Grant sponsor: Cancer Research Switzerland; Grant number: 02606-06-2010; Grant sponsor: KFS; Grant number: 02631-08-2010; Grant sponsor: Cancer League Aargau; Grant sponsor: Cancer League Zurich; Grant sponsor: Swiss Bridge; Grant sponsor: Stiftung zur Krebsbekämpfung; Grant sponsor: Swiss Childhood Cancer Registry; Grant sponsor: Swiss Paediatric Oncology Group; Grant sponsor: Kinderkrebshilfe Schweiz; Grant sponsor: Stiftung für krebskranke Kinder Regio Basiliensis; Grant sponsor: Schweizerische Konferenz der kantonalen Gesundheitsdirektorinnen und –direktoren
Swiss Paediatric Oncology Group (SPOG) Scientific Committee: Prof. Dr. med. R. Ammann, Bern; Dr. med. R. Angst, Aarau; Dr. med. Marc Ansari; PD Dr. med. M. Beck Popovic, Lausanne; Dr. med. E. Bergstraesser, Zurich; Dr. med. P. Brazzola, Bellinzona; Dr. med. J. Greiner, St. Gallen; Prof. Dr. med. M. Grotzer, Zurich; Dr. med. H. Hengartner, St. Gallen; Prof. Dr. med. T. Kuehne, Basel; Prof. Dr. med. K. Leibundgut, Bern; Prof. Dr. med.F. Niggli, Zurich; PD Dr. med. J. Rischewski, Lucerne; Prof. Dr. med. N. von der Weid, Basel.
Footnotes
Conflict of interest: Nothing to declare.
References
- 1.David A. People at the Centre of Health Care: Harmonizing mind and body, people and systems. New Delhi: World Health Organization Regional Office for the Western Pacific; 2007. [Google Scholar]
- 2.Ormandy P. Defining information need in health—Assimilating complex theories derived from information science. Health Expect. 2011;14:92–104. doi: 10.1111/j.1369-7625.2010.00598.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Husson O, Mols F, van de Poll-Franse LV. The relation between information provision and health-related quality of life, anxiety and depression among cancer survivors: A systematic review. Ann Oncol. 2011;22:761–772. doi: 10.1093/annonc/mdq413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jenkins V, Fallowfield L, Saul J. Information needs of patients with cancer: Results from a large study in UK cancer centres. Br J Cancer. 2001;84:48–51. doi: 10.1054/bjoc.2000.1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Budych K, Helms TM, Schultz C. How do patients with rare diseases experience the medical encounter? Exploring role behavior and its impact on patient-physician interaction. Health Policy. 2012;105:154–164. doi: 10.1016/j.healthpol.2012.02.018. [DOI] [PubMed] [Google Scholar]
- 6.Singer S, Gianinazzi ME, Hohn A, et al. General practitioner involvement in follow-up of childhood cancer survivors: A systematic review. Pediatr Blood Cancer. 2013;60:1565–1573. doi: 10.1002/pbc.24586. [DOI] [PubMed] [Google Scholar]
- 7.Byrne J, Lewis S, Halamek L, et al. Childhood cancer survivors’ knowledge of their diagnosis and treatment. Ann Intern Med. 1989;110:400–403. doi: 10.7326/0003-4819-110-5-400. [DOI] [PubMed] [Google Scholar]
- 8.Bashore L. Childhood and adolescent cancer survivors’ knowledge of their disease and effects of treatment. J Pediatr Oncol Nurs. 2004;21:98–102. doi: 10.1177/1043454203262754. [DOI] [PubMed] [Google Scholar]
- 9.Maeda N, Horibe K, Kato K, et al. Survey of childhood cancer survivors who stopped follow-up physician visits. Pediatr Int. 2010;52:806–812. doi: 10.1111/j.1442-200X.2010.03158.x. [DOI] [PubMed] [Google Scholar]
- 10.Knijnenburg SL, Kremer LC, van den Bos C, et al. Health information needs of childhood cancer survivors and their family. Pediatr Blood Cancer. 2010;54:123–127. doi: 10.1002/pbc.22207. [DOI] [PubMed] [Google Scholar]
- 11.Wakefield CE, Butow P, Fleming CAK, et al. Family information needs at childhood cancer treatment completion. Pediatr Blood Cancer. 2012;58:621–626. doi: 10.1002/pbc.23316. [DOI] [PubMed] [Google Scholar]
- 12.Keegan TH, Lichtensztajn DY, Kato I, et al. Unmet adolescent and young adult cancer survivors information and service needs: A population-based cancer registry study. J Cancer Surviv. 2012;6:239–250. doi: 10.1007/s11764-012-0219-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oerlemans S, Husson O, Mols F, et al. Perceived information provision and satisfaction among lymphoma and multiple myeloma survivors-results from a Dutch population-based study. Ann Hematol. 2012;91:1587–1595. doi: 10.1007/s00277-012-1495-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nicolaije KAH, Husson O, Ezendam NPM, et al. Endometrial cancer survivors are unsatisfied with received information about diagnosis, treatment and follow-up: A study from the population-based PROFILES registry. Patient Educ Couns. 2012;88:427–435. doi: 10.1016/j.pec.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 15.Michel G, von der Weid NX, Zwahlen M, et al. The Swiss Childhood Cancer Registry: Rationale, organisation and results for the years 2001–2005. Swiss Medical Wkly. 2007;137:502–509. doi: 10.4414/smw.2007.11875. [DOI] [PubMed] [Google Scholar]
- 16.Michel G, von der Weid NX, Zwahlen M, et al. Incidence of childhood cancer in Switzerland: The Swiss childhood cancer registry. Pediatr Blood Cancer. 2008;50:46–51. doi: 10.1002/pbc.21129. [DOI] [PubMed] [Google Scholar]
- 17.Kuehni CE, Rueegg CS, Michel G, et al. Cohort profile: The Swiss Childhood Cancer Survivor Study. Int J Epidemiol. 2011;41:1553–1564. doi: 10.1093/ije/dyr142. [DOI] [PubMed] [Google Scholar]
- 18.Steliarova-Foucher E, Stiller C, Lacour B, et al. International classification of childhood cancer, third edition. Cancer. 2005;103:1457–1467. doi: 10.1002/cncr.20910. [DOI] [PubMed] [Google Scholar]
- 19.Kuehni CE, Strippoli M-PF, Rueegg CS, et al. Educational achievement in Swiss childhood cancer survivors compared with the general population. Cancer. 2011;118:1439–1449. doi: 10.1002/cncr.26418. [DOI] [PubMed] [Google Scholar]
- 20.German U. Abschlussbericht zur Volkszählung 2000. Neuchâtel: Bundesamt für Statistik; 2005. [Google Scholar]
- 21.Derogatis LR. BSI-18 administration, scoring, and procedures manual. Minneapolis, MN: National Computer Services; 2000. [Google Scholar]
- 22.Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Brown Lawrence D, Cai Tony C, Anirban D. Interval estimation for a binomial proportion. Statist Sci. 2001;16:101–133. [Google Scholar]
- 24.Ojha RP, Oancea SC, Ness KK, et al. Assessment of potential bias from non-participation in a dynamic clinical cohort of long-term childhood cancer survivors: Results from the St. Jude lifetime cohort study. Pediatr Blood Cancer. 2012;28:24348. doi: 10.1002/pbc.24348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Michel G, Greenfield D, Absolom K, et al. Satisfaction with follow-up consultations among younger adults treated for cancer: The role of quality of life and psychological variables. Psychooncology. 2011;20:813–822. doi: 10.1002/pon.1783. [DOI] [PubMed] [Google Scholar]
- 26.Haddad M, Inch C, Glazier RH, et al. Patient support and education for promoting adherence to highly active antiretroviral therapy for HIV/AIDS. Cochrane Database Syst Rev. 2000 doi: 10.1002/14651858.CD001442. CD001442. [DOI] [PubMed] [Google Scholar]
- 27.Children’s Oncology Group. Long-Term Follow-Up Guidelines for Survivors of Childhood, Adolescent, and Young Adult Cancers V3.0. 2008 [Google Scholar]
- 28.Jacobsen PB. Clinical practice guidelines for the psychosocial care of cancer survivors: Current status and future prospects. Cancer. 2009;115:4419–4429. doi: 10.1002/cncr.24589. [DOI] [PubMed] [Google Scholar]
- 29.Wallace WHB, Blacklay A, Eiser C, et al. Developing strategies for long term follow up of survivors of childhood cancer. Br Med J. 2001;323:271–274. doi: 10.1136/bmj.323.7307.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.