Abstract
Objective
Treatment for Binge Eating Disorder (BED) – a condition associated with both excess adiposity and psychological distress – has not typically produced a significant weight loss despite reducing binge eating. Characterizing factors that promote or inhibit weight loss in individuals with co-occurring BED and obesity may help explain overall nonsignificant weight changes during treatment.
Methods
189 adults with BED participated in a randomized clinical trial evaluating the efficacy of 5M of cognitive behavioral therapy. Assessments included measured height and weight at baseline, midtreatment, end-of-treatment (EOT), and 6-month follow-up, the Eating Disorder Examination interview, and questionnaires.
Results
During treatment, there was a mean weight gain of 1.3±12.0 lbs. 22% of the sample lost ≥ 5 pounds and 25% of the sample gained ≥ 8 pounds. Results showed that baseline objective binge eating episodes (OBEs) predicted weight over treatment. Changes in weight were significantly positively related to concurrent changes in shape concern, weight concern, and disinhibition, but not binge eating episodes. Changes in OBEs from baseline to EOT were associated with changes in weight from EOT to follow-up.
Conclusions
Further investigation of eating behavior during BED treatment to understand the energy balance contributions to weight change or stability is warranted.
Keywords: weight change, binge eating, treatment, body weight, weight
Introduction
The majority of individuals with binge eating disorder (BED) have obesity or overweight1,2. In this population, both excess adiposity and psychological distress and impairment associated with binge eating increase risk for serious chronic health conditions and mortality3,4. Cognitive behavioral therapy (CBT) is the most widely studied and empirically-supported treatment for BED5. However, CBT for BED has not typically produced statistically significant weight reductions despite significant decreases in the frequency of binge-eating episodes6–8
Understanding how weight changes in response to BED treatment is critical because although decreasing frequency of binge eating leads to improvement in psychosocial functioning5, maintenance or worsening of obesity increases risk for chronic disease and mortality4,9. Few published studies have investigated energy balance in relationship to BED treatment, binge eating episode reductions, and lack of expected weight reduction. A recent study by Masheb and colleagues (2016) found that achieving abstinence from eating binges during treatment (about half of the sample) was associated with a 400-calorie deficit in intake compared to those who did not achieve abstinence from binge eating10; importantly, binge eating abstinence and the accompanying reported caloric deficit (measured by two random 24-hour recalls within the six month treatment period) also exhibited greater psychological improvements than those who did not achieve binge eating abstinence. This study did find a significant mean reduction in body mass index (BMI) of about 1 kg/m2 in the sample; however, changes in percent weight loss were not significantly different between those who did and did not achieve binge eating abstinence.
Characterizing factors that may promote or inhibit weight loss in individuals with co-occurring BED and obesity may inform the development of novel treatments designed to target both conditions. Relative to energy balance, if an individual decreases the number of calories consumed over the course of treatment and all other factors affecting energy balance remain stable, weight loss would be a predictable outcome of BED treatment. Psychological predictors have been well examined in the literature in reference to weight loss populations11; however, individuals with BED may represent a unique population and have been described as more similar to individuals with bulimia nervosa (e.g., in attitudes about shape and weight, psychiatric comorbidity,) than obesity without eating-related illness12.
This paper addresses a gap in the literature by exploring how individual variability in changes in binge eating behaviors and psychological variables during treatment for BED are associated with body weight change. This study has four primary objectives:
To describe variability in weight change during BED treatment;
To identify baseline predictors of weight change during BED treatment;
To explore concurrent changes in weight, binge eating episode frequency, and psychological factors during BED treatment; and
To determine whether change in binge eating episode frequency during treatment predicts change in weight during follow-up.
Methods
Participants and Procedure
This study utilized data from a larger randomized controlled clinical trial evaluating the effectiveness of different delivery methods of CBT (group-led, therapist led, or self-help)13. Waitlisted controls (N = 69) were included in the larger trial, but not the present analysis because they did not receive active treatment. Eligibility required meeting full criteria for DSM-IV BED and having a BMI ≥ 25 kg/m2. Exclusion criteria included pregnancy or lactation; lifetime diagnosis of bipolar or psychotic disorder; current diagnosis of substance abuse or substance dependence; medical or psychiatric instability including acute suicide risk; current psychotherapy; or current participation in a formal weight loss program. Participants completed measures at baseline, at a midpoint assessment (i.e., 10 weeks), at end of treatment (EOT; i.e., 20 weeks/5 months), and at a 6-month follow-up (approximately 11 months after baseline). Details regarding other aspects of the study have been described previously13. Ethical approval for the study was obtained from Institutional Review Boards at the University of Minnesota, University of North Dakota, and MeritCare/Sanford Health. The analytic sample for the present study included 189 adults who were randomized to one of three active treatment groups.
Measures
Body mass index (BMI)
Anthropometric measurements of height and weight were collected. BMI was calculated using the standard formula for BMI14.
Eating Disorder Examination (EDE15)
The EDE is a semi-structured interview that assesses ED symptoms and psychopathology with a focus on the previous 28 days. The EDE assesses the frequency of different forms of overeating, including objective binge eating episodes (OBE; i.e., binge eating defined as unusually large quantities of food with a sense of loss of control), subjective binge eating episodes (SBE; i.e., episodes with a sense of loss of control while eating an amount of food that the individual considers to be large, but interviewer does not), and objective overeating episodes (OOE; i.e., episodes of consumption of unusually large quantities of food with no associated sense of loss of control). The EDE comprises four subscales: restraint (Cronbach’s alpha as baseline for this sample =0.65; EOT =0.49), eating concern (baseline =0.57; EOT=0.63), shape concern (baseline =0.67; EOT =0.81), and weight concern (baseline =0.61; EOT =0.73) as well as a combined global scale. Items are rated on 7-point forced-choice scales (range 0–6), with higher scores reflecting greater severity/frequency. The EDE has well-established inter-rater and test-retest reliability in individuals with BED16. Experienced graduate students administered the EDE and were blinded to participant’s treatment condition; interrater reliability was 0.955 and higher.13 For a detailed discussion of the EDE interviewer training, please refer to Peterson et al., (2009)13.
Three Factor Eating Questionnaire (TFEQ17)
In this study, the 51-item TFEQ was used to measure dietary restraint, defined as cognitive attempts to control food intake, and disinhibition, defined as a proclivity to eat in response to external cues as opposed to internal hunger/satiety signals. The restraint subscale has 21 items and the disinhibition subscale has 16 items; possible scores ranging from 0–21 and 0–16, respectively. The first 36 items of the TFEQ use a dichotomous response format of 0 (false) and 1 (true). Participants respond to the final 15 items using a four-point scale with response options varying for each question. Cronbach’s alphas for restraint and disinhibition were 0.76 and 0.46 at baseline and 0.75 and 0.76 at EOT in the current sample, respectively. Given the lower alpha for disinhibition at baseline, we opted not to include results pertaining to baseline disinhibition as a predictor of weight trajectory.
Inventory of Depressive Symptomatology (IDS18)
The IDS-SR is a 30-item scale that measures depressive symptoms (e.g., sadness, loss of interest). Participants rated items on a scale ranging from 0 to 3 with severity-based response options for each item, e.g., 0 (I do not feel sad), 1 (I feel sad less than half the time), 2 (I feel sad more than half the time), and 3 (I feel sad nearly all of the time); 28 of the 30 items are scored for a range of 0–84. Higher scores indicate more depressive symptoms. The IDS-SR is strongly associated with other established measures of depressive symptoms19. Cronbach’s alphas were 0.85 at baseline and 0.88 at EOT in the current sample.
Rosenberg Self-Esteem Scale (RSES20)
The RSES is the most widely used scale to assess global self-esteem. Participants respond to 10-items on a Likert scale ranging from 1 (strongly disagree) to 4 (strongly agree); total scores range from 0–30. A sample item is: “I take a positive attitude toward myself.” Higher scores indicate less self-esteem. The RSES has shown excellent psychometric properties (e.g.21). Cronbach’s alphas were 0.92 at baseline and 0.91 at EOT in the current sample.
Coping Scale for Bulimia Nervosa (CS-BN22)
The CS-BN was used to measure coping strategies specific to BED. The CS-BN was modified for use with individuals with BED by removing “purging” from items and replacing “BN” with “BED.” The CS-BN measures several dimensions of coping strategies including avoidant/alternative (e.g., avoided stressful situations), interpersonal (e.g., called a supportive friend), and cognitive (e.g., challenged unrealistic thoughts) strategies. Higher scores indicate greater use of coping strategies. Participants rated 36 items on a scale ranging from 0 (never) to 3 (frequently); scores range from 0 – 108. Cronbach’s alphas were 0.92 at baseline and 0.93 at EOT in the current sample.
Statistical Analysis
For Objective 1, descriptive statistics were calculated for study variables. For Objective 2, multilevel modeling was used to examine baseline values of predictors of weight change over time. Multilevel models were calculated separately for each predictor. Models included the baseline predictor, the linear and quadratic terms of time in days, and the interaction between the baseline predictor and the linear and quadratic terms of time. Because this study examined three separate treatments, we controlled for the effect of treatment type in analyses. For Objective 3, we examined associations between changes in predictor variables and changes in weight from baseline to EOT. Bivariate Pearson correlations (as the normality assumption was met) were used to examine how changes in eating patterns over the course of treatment were associated with changes in weight. For Objective 4, change in binge eating episodes from baseline to EOT was used as predictor of weight change during the follow-up period, using separate models for 6-month and 12-month follow-up. All analyses used SPSS version 23 and alpha was set to p < 0.05.
Results
Descriptive characteristics of the analytic sample are displayed in Table 1. For attrition rates at each study time point, please refer to Figure 1 in the main outcomes paper13. A series of one-way analyses of variance suggested no significant differences between the three groups in weight change during treatment, binge abstinence achieved during treatment, change in number of OBEs, OOEs or SBEs during treatment, or weight change during follow-up (all ps > 0.05).
Table 1.
Baseline characteristics of analytic sample
| Variable (unit, total n for variable) | Mean ± Standard Deviation or % |
|---|---|
| Age (Years, n = 189) | 46.7 ± 10.2 |
| Body Mass Index (kg/m2, n =189) | 39.3 ± 8.1 |
| Sex - Female (%, n = 189) | 89.9 % |
| Ethnicity - White (%, n = 181) | 95.8 % |
| Education – At least some college (%, n = 171) | 46.8 % |
| Eating Disorder Examination Interview (EDE), (n = 189) | |
| Restraint | 1.6 ± 1.3 |
| Eating Concern | 2.0 ± 1.2 |
| Shape Concern | 3.5 ± 1.0 |
| Weight Concern | 3.4 ± 1.1 |
| Global | 2.6 ± 0.9 |
| Objective Binge Eating Episodes/28 days | 23.0 ± 15.1 |
| Objective Overeating Episodes/28 days | 1.50 ± 6.0 |
| Subjective Binge Eating Episodes/28 days | 10.0 ± 15.1 |
| Three Factor Eating Questionnaire (TFEQ), (n = 176) | |
| Restraint | 6.7 ± 3.6 |
| Disinhibition | 13.9 ± 1.7 |
| Coping Scale for Bulimia Nervosa (CS-BN, adapted for BED), (n = 173) | |
| Cognitive Coping | 11.2 ± 5.9 |
| Interpersonal Coping | 3.7 ± 3.7 |
| Avoidant Coping | 11.2 ± 4.0 |
| Total Coping | 26.1 ± 11.5 |
| Inventory of Depressive Symptomatology (IDS), (n = 184) | 24.1 ± 11.0 |
| Rosenberg Self-Esteem (RSES), (n = 180) | 2.7 ± 2.0 |
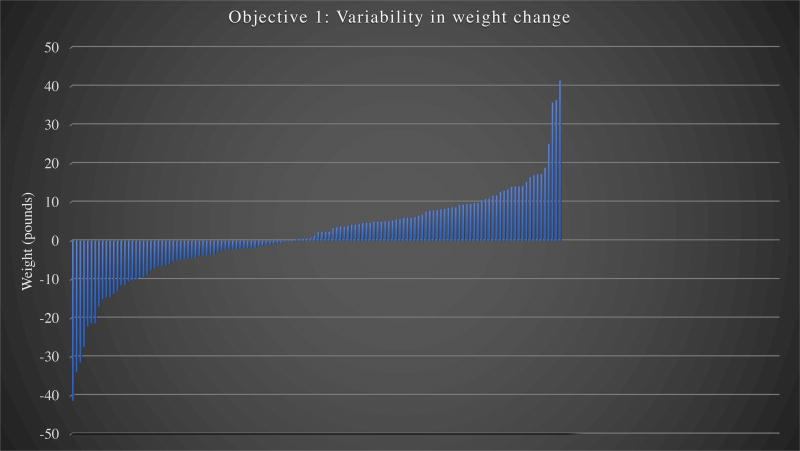
Figure 1. (Objective 1) Weight variability over 5 months of BED treatment (EOT minus BL).
Note. Each vertical line represents one individual participant. BED = Binge Eating Disorder; EOT = End of treatment; BL = Baseline
Objective 1: Variability of weight change during BED treatment1
During the five months of treatment, participants gained an average of 1.3 ± 12.0 lbs. Figure 1 highlights the variability in weight change during treatment by displaying each individual participant’s weight change. Twenty-five percent of the sample lost five pounds or more, and 25% of the sample gained at least eight pounds. Notably, 11 participants gained or lost over 20 pounds.
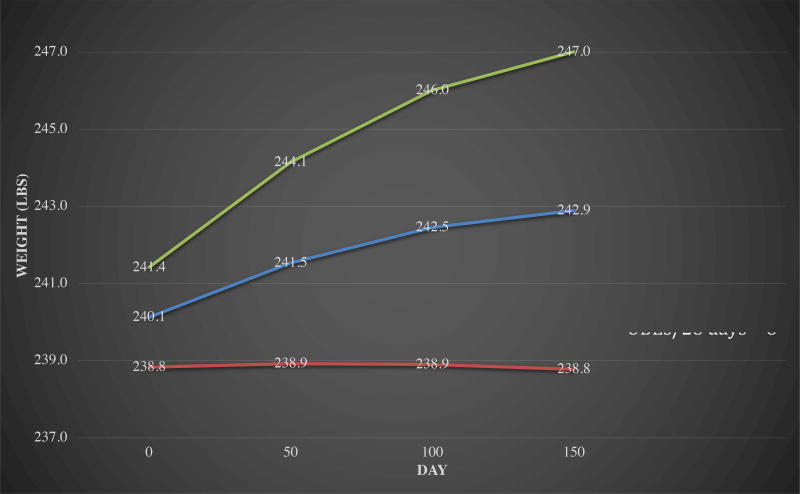
Objective 2: Baseline predictors of weight change over treatment2
Baseline restraint (measured by either the EDE or TFEQ), eating concern, shape concern, weight concern, global EDE score, OOEs, and SBEs were not significant predictors of weight trajectory over treatment. OBE episodes significantly predicted the trajectory of weight over the course of CBT. These relationships are displayed in Figure 2. Figure 2 illustrates the weight trajectory of mean OBE frequency at baseline and shows that those with higher reported OBEs predicted a steeper weight gain as compared to those with the mean level or low OBE frequency at baseline (low and high defined as one standard deviation above and below the mean).
Figure 2. (Objective 2) Baseline Objective Binge Episodes (OBEs) predicting weight trajectory over 5 m of BED treatment.
Note. Weight trajectories in this figure display the model-based predicted values at each of three time points based upon mixed model analyses. The top line is one standard deviation above the mean of baseline number of OBEs in past 28 days for this sample; the middle line is the mean level of baseline number of OBEs in past 28 days for this sample; the bottom line is one standard deviation below the mean of baseline number of OBEs in past 28 days for this sample.
Objective 3: Associations between change weight and change in binge episodes and psychological variables3
Associations between concurrent changes in weight and binge eating episodes/psychological variables are presented in Table 2. Shape concern, weight concern, and disinhibition were all positively and significantly related to weight change (Pearson rs = .18, .19, and .19 respectively, ps < .05). Weight change was not significantly associated with concurrent change in EDE-assessed eating behaviors, restraint, or psychological variables.
Table 2.
(Objective 3) Pearson correlations between change in weight and change in psych/behavioral variables during BED treatment. All change variables are EOT minus BL.
| Change in variable | Δ Weight |
|---|---|
| EDE-Restraint | 0.07 |
| EDE-Eating Concern | 0.08 |
| EDE-Shape Concern | 0.18* |
| EDE-Weight Concern | 0.19* |
| EDE-Total | 0.17 |
| EDE OBE | −0.12 |
| EDE OOE | 0.02 |
| EDE SBE | −0.01 |
| TFEQ-Restraint | −0.09 |
| TFEQ-Disinhibition | 0.19* |
| Coping-Cognitive | 0.11 |
| Coping-Interpersonal | 0.09 |
| Coping-Avoidant | −0.09 |
| Coping Total | 0.06 |
| Self-esteem | −0.01 |
| Depressive symptoms | 0.03 |
p < .05
Note. EOT = End-of-treatment; BL = Baseline; EDE = Eating Disorder Examination Interview; OBE = Objective Binge Episodes; OOE = Objective Overeating Episodes; SBE = Subjective Binge Episodes; TFEQ = Three Factor Eating Questionnaire
Objective 4: Changes in binge eating behaviors during treatment predicting weight change during follow-up4
Because expected significant relationships were not found between changes in weight and binge eating episodes (i.e. greater decreases in OBEs from baseline to end of treatment being associated with concurrent greater decreases in weight), we explored the possibility that changes in binge eating episodes during treatment may be related to change in weight during follow-up (defined separately as 6-month follow-up minus EOT weight and as 12-month follow-up minus EOT weight). Six months after EOT, the mean change in weight was −0.9 ± 12.72 lbs (range −59.40 to 36.80; n = 101). Twelve months after EOT, the mean change in weight was −6.85 ± 22.65 lbs (range = −88.00 to 31.20 lbs; n = 70). Changes in OBEs during treatment significantly positively predicted change in weight over the first 6-months after EOT(r = 0.198, p = 0.047), meaning that a greater decrease in OBEs during treatment was associated with a greater decrease in weight. Twelve months after treatment, this change was no longer significant. Changes in OOEs or SBEs during treatment did not significantly predict changes in weight 6 months or 12 months following treatment.
Discussion
Although BED treatment targets binge eating episodes and has successfully been shown to decrease binge eating frequency, body weight is an important factor to consider in treatment and follow-up as obesity is associated with physiological and psychological co-morbidities. To this end, this study aimed to examine the variability of weight change during CBT treatment for BED. In this study, although there was a mean weight gain during treatment, we found substantial variability in weight change during the course of CBT treatment for BED (from losing 40 lbs to gaining 40 lbs). A substantial number of participants gained weight and a substantial number lost weight. This finding is not surprising given published studies finding heterogeneity in weight change in individuals with BED 12 months prior to treatment (from losing 40 lbs to gaining 62 lbs)23. Additionally, it has been shown that this heterogeneity in weight change is specific to individuals with comorbid overweight/obesity and BED as compared to individuals with overweight/obesity without BED24.
At baseline, greater self-reported OBEs significantly predicted weight gain during 5 months of treatment, which appears to begin leveling off by the end of treatment. Because individuals engaging in higher levels of OBEs/binge eating are consuming more calories, they may continue to gain weight during early stages of treatment, but weight gain levels off as binge eating behaviors improve. Longer term trials assessing BED and weight change are minimal; however, in one weight loss maintenance study that did not include treatment for binge eating, binge eating was associated with weight regain over time25, suggesting that the relationship between binge eating and weight gain or regain over time may be of importance.
Decreases in weight during treatment were significantly associated with concurrent decreases in shape concern, weight concern, and disinhibition. Weight and shape concerns are core symptoms associated with binge eating26, and are an important target in CBT for BED27. Reducing weight may be a possible mechanism for improving binge eating as well as preventing relapse through its relationship with decreasing weight and shape concerns, though the direction of causality is unclear (i.e. improving binge eating and weight and shape concerns is likely to lead to weight loss) and may be bi-directional. However, decreases in weight during treatment were not significantly related to decreases in OBEs, SBEs, or OOEs. Nonetheless, decreases in OBEs during treatment significantly predicted greater weight loss during six months of follow-up. A delay in energy balance effect is possible, such that the decrease in caloric intake from fewer OBEs does not produce a change in weight until after a few weeks or months, but future research is needed to determine the direction of causality and mechanisms associated with these changes.
Despite the aforementioned statically significant findings, Pearson correlation coefficients ranged from 0.18–0.20, evidencing small to medium effect sizes28. Additionally, some expected relationships were not significant (e.g. change in weight was not significantly associated with change in binge episodes during treatment). Most striking was the lack of relationship between changes in types of binge eating episodes and weight. The only significant finding, that change in OBEs during treatment predicted weight change over the 6 months after EOT, but not 12 months after EOT, is in the expected direction (as were the other nonsignificant findings), but a surprisingly small correlation.
There are several possible explanations for the lack of expected findings. First, other eating behaviors (e.g. snacking or ‘picking and nibbling’, an item later added to the EDE to address a possible shift from binge episodes to other eating behaviors) may increase concurrently as decreases in binge/overeating episodes are observed. To assess this possible explanation, post-hoc correlation analyses were run between changes in number of episodes of OBEs, OOEs, SBEs during treatment and changes in (1) the number of days of reported snacks (mid-morning, mid-afternoon, evening, or nocturnal) (2) a composite number of days on which snacking took place, and (3) the number of days of reported picking and nibbling. The only statistically significant correlation was between change in number of OBEs and change in number of days having an evening snack (Pearson r = 0.269; p <0.001), indicating that a greater change (either increase or decrease) in OBEs was associated with a greater change in number of evening snack days. Masheb, Roberto, and White (2013) also found a lack of relationship between binge episodes and picking and nibbling29; it is unclear whether decreases in binge eating are not associated with increases in picking and nibbling, or lack of findings reflect a measurement issue. Second, it is possible that the sample was underpowered to detect these effects; however, this is unlikely due to some expected effects emerging within the present sample. Recent published findings have suggested that a difference in caloric consumption may be more apparent between those achieving abstinence from binge eating versus those not achieving abstinence10, which, if continued over time, should equate to a difference in weight between those achieving and not achieving binge abstinence (assuming no marked change in physical activity). In this study, post-hoc analyses showed that at EOT, eighteen individuals reported not experiencing any OBE, OOE, or SBEs in the past 28 days. These 18 individuals lost an average of 0.58 ± 12.30 pounds, while the 112 who did not achieve abstinence from binge eating at EOT gained an average of 1.46 ± 11.84 pounds (t = 0.67, df = 128). While this difference was not statistically significant (p = 0.51), individuals who achieved abstinence from binge eating having an overall decrease in weight versus individuals not achieving abstinence having an average increase in weight is consistent with findings in recent literature10.
In the weight loss literature, behavioral weight loss often produces an increase in dietary restraint associated with a decrease in weight (e.g.30). However, in response to BED treatment, there is variability in weight change such that some gain weight while others lose, possibly resulting in a net weight change not significantly different from zero. The finding that increases in dietary restraint are associated with decreases in weight does not necessarily mean that increases in weight are associated with decreases in dietary restraint. The net change in this study was close to one pound gained, and we would not expect a weight change of that magnitude to be associated with a change in restraint score. Furthermore, CBT for BED does not focus on dietary restraint; in fact, it discourages dietary restraint based on the presumed link between dietary restraint (i.e., strict, rigid rules regarding food intake) and binge eating31. Additionally, as is common in BED samples, because participants’ mean level of dietary restraint was low to begin with (EDE restraint = 1.6; TFEQ restraint = 6.7), we would not expect further significant decrease.
This study is limited by its primarily Caucasian and female sample. In addition, three treatment groups were combined in this secondary analysis. All treatment groups were CBT-focused, but the method of intervention delivery differed (therapist-assisted group (n = 60), therapist-led group (n = 62), or self-help group (n = 67)). Although there were significant differences noted in the outcomes reported in the main paper13 (i.e. % of women randomized to each group, greater percentage of binge abstinence achieved in therapist-led versus self-help or control groups during treatment), due to absence of significant differences between the groups for weight loss over treatment or follow-up, and the fact that identical content was presented to each of the three groups13, we combined groups. Other individual difference variables (e.g. personality factors) may be significantly related to weight change during treatment and were not explored. Further research is necessary to determine if these results are generalizable to other BED samples.
This research offers several avenues for research on energy balance and weight within the context of BED. Improved measurement of variables impacting energy balance would allow for a more nuanced understanding of caloric balance during and after treatment for BED. Currently, treatment trials for BED rarely include energy balance assessments in their research protocols. Random 24-hour dietary recalls as well as novel ecological momentary assessment approaches could be used to quantify caloric intake along with self-reported OBE, OOE, and SBE episodes. Further, although physical activity has often not been reported in BED treatment trials, the importance of physical activity in energy balance make this variable critical to measure. Finally, investigation of other potential predictors response to BED treatment, including biological and physiological markers (i.e., weight suppression, weight regulatory hormones) is warranted due to the consequences of potential weight gain during treatment. In addition, there may be clinical utility of adding other approaches to binge eating treatments such as physical activity and nutritional components in order to increase weight loss and improve targeted outcomes (e.g., improvements in weight and shape concerns, decreases in binge eating). For example, one study found that the addition of exercise and nutritional counseling to CBT was associated with greater weight loss in patients with co-occurring obesity and BED32. Adding physical activity components to BED treatment may be effective in enhancing weight loss as well as improving mental health symptoms. Physical activity may help decrease weight both directly33 and indirectly by improving emotional health34, which is a common trigger of binge eating35. Given that participants in BED treatment trials often express a desire to lose weight, adding these components to treatment may also increase treatment acceptability and retention.
In conclusion, findings from this study suggest that there is substantial variability in weight change during CBT treatment for BED in adults with overweight/obesity. Although decreases in binge eating behavior frequency were not significantly associated with concurrent decreases in weight during treatment, greater decreases in OBEs during treatment significantly predicted greater decreases in weight during six months of follow-up. It may be useful to provide additional treatment and support for those at risk of weight gain during BED treatment (i.e. those with greater baseline OBEs) to prevent this outcome given the medical complications associated with further weight gain and obesity.
What is already known about this subject
Obesity and Binge Eating Disorder (BED) are comorbid conditions
Having both illnesses is associated with marked distress and impairment
Cognitive Behavioral Therapy (CBT) for BED does not consistently produce a reduction in weight
What this study adds
Weight change in response to CBT for BED is highly variable, ranging from a loss of 41.3 pounds to a gain of 41.5 pounds over five months of treatment in this sample
A high number of objective binge eating episodes at baseline predicted steeper weight gain during treatment
Greater reductions in objective binge eating episodes during treatment predicted greater weight loss during follow-up
Acknowledgments
FUNDING: NIH Grants: DK 61912, DK 61973, P30 DK 60456, K02 MH65919, T32 MH 082761
Footnotes
CLINICAL TRIAL REGISTRATION: NCT00041743
DISCLOSURE: The authors declared no conflict of interest.
(n = 132)
(n = 119 – 130 depending upon completeness of data)
(n = 119 – 130 depending upon completeness of data)
(n = 101 at 6 months, n = 70 at 12 months)
References
- 1.Kessler RC, Berglund PA, Chiu WT, et al. The prevalence and correlates of binge eating disorder in the World Health Organization World Mental Health Surveys. Biol Psychiatry. 2013;73(9):904–914. doi: 10.1016/j.biopsych.2012.11.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Zwaan M. Binge eating disorder and obesity. Int J Obes Relat Metab Disord J Int Assoc Study Obes. 2001;25(Suppl 1):S51–55. doi: 10.1038/sj.ijo.0801699. [DOI] [PubMed] [Google Scholar]
- 3.Kalarchian MA, Marcus MD, Levine MD, et al. Psychiatric disorders among bariatric surgery candidates: relationship to obesity and functional health status. Am J Psychiatry. 2007;164(2):328–334. doi: 10.1176/ajp.2007.164.2.328. [DOI] [PubMed] [Google Scholar]
- 4.Flegal KM, Kit BK, Orpana H, Graubard BI. Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. Jama. 2013;309(1):71–82. doi: 10.1001/jama.2012.113905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Iacovino JM, Gredysa DM, Altman M, Wilfley DE. Psychological treatments for binge eating disorder. Curr Psychiatry Rep. 2012;14(4):432–446. doi: 10.1007/s11920-012-0277-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brownley KA, Berkman ND, Sedway JA, Lohr KN, Bulik CM. Binge eating disorder treatment: a systematic review of randomized controlled trials. Int J Eat Disord. 2007;40(4):337–348. doi: 10.1002/eat.20370. [DOI] [PubMed] [Google Scholar]
- 7.Grilo CM, Reas DL, Mitchell JE. Combining pharmacological and psychological treatments for binge eating disorder: current status, limitations, and future directions. Curr Psychiatry Rep. 2016;18(6):1–11. doi: 10.1007/s11920-016-0696-z. [DOI] [PubMed] [Google Scholar]
- 8.Palavras MA, Hay P, Filho CADS, Claudino A. The Efficacy of Psychological Therapies in Reducing Weight and Binge Eating in People with Bulimia Nervosa and Binge Eating Disorder Who Are Overweight or Obese-A Critical Synthesis and Meta-Analyses. Nutrients. 2017;9(3) doi: 10.3390/nu9030299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cecchini M, Sassi F, Lauer JA, Lee YY, Guajardo-Barron V, Chisholm D. Tackling of unhealthy diets, physical inactivity, and obesity: health effects and cost-effectiveness. Lancet Lond Engl. 2010;376(9754):1775–1784. doi: 10.1016/S0140-6736(10)61514-0. [DOI] [PubMed] [Google Scholar]
- 10.Masheb RM, Dorflinger LM, Rolls BJ, Mitchell DC, Grilo CM. Binge abstinence is associated with reduced energy intake after treatment in patients with binge eating disorder and obesity. Obesity. 2016;24(12):2491–2496. doi: 10.1002/oby.21664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lasikiewicz N, Myrissa K, Hoyland A, Lawton CL. Psychological benefits of weight loss following behavioural and/or dietary weight loss interventions. A systematic research review. Appetite. 2014;72:123–137. doi: 10.1016/j.appet.2013.09.017. [DOI] [PubMed] [Google Scholar]
- 12.Dingemans AE, Bruna MJ, Van Furth EF. Binge eating disorder: a review. Int J Obes. 2002;26(3):299. doi: 10.1038/sj.ijo.0801949. [DOI] [PubMed] [Google Scholar]
- 13.Peterson CB, Mitchell JE, Crow SJ, Crosby RD, Wonderlich SA. The Efficacy of Self-Help Group Treatment and Therapist-Led Group Treatment for Binge Eating Disorder. Am J Psychiatry. 2009;166(12):1347–1354. doi: 10.1176/appi.ajp.2009.09030345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keys A, Fidanza F, Karvonen MJ, Kimura N, Taylor HL. Indices of relative weight and obesity. J Chronic Dis. 1972;25(6):329–343. doi: 10.1016/0021-9681(72)90027-6. [DOI] [PubMed] [Google Scholar]
- 15.Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge Eating: Nature, Assessment, and Treatment. 12. New York, NY: Guilford Press; 1993. pp. 317–360. [Google Scholar]
- 16.Grilo CM, Masheb RM, Lozano-Blanco C, Barry DT. Reliability of the Eating Disorder Examination in patients with binge eating disorder. Int J Eat Disord. 2004;35(1):80–85. doi: 10.1002/eat.10238. [DOI] [PubMed] [Google Scholar]
- 17.Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. 1985;29(1):71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- 18.Rush AJ, Giles DE, Schlesser MA, Fulton CL, Weissenburger J, Burns C. The inventory for depressive symptomatology (IDS): Preliminary findings. Psychiatry Res. 1986;18(1):65–87. doi: 10.1016/0165-1781(86)90060-0. [DOI] [PubMed] [Google Scholar]
- 19.Rush AJ, Trivedi M, Carmody TJ, et al. One-year clinical outcomes of depressed public sector outpatients: a benchmark for subsequent studies. Biol Psychiatry. 2004;56(1):46–53. doi: 10.1016/j.biopsych.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 20.Rosenberg M. [Accessed November 2, 2016];Society and the adolescent self-image. 1965 http://psycnet.apa.org/journals/ort/36/3/560.pdf%26productCode=pa.
- 21.Sinclair SJ, Blais MA, Gansler DA, Sandberg E, Bistis K, LoCicero A. Psychometric properties of the Rosenberg Self-Esteem Scale: overall and across demographic groups living within the United States. Eval Health Prof. 2010;33(1):56–80. doi: 10.1177/0163278709356187. [DOI] [PubMed] [Google Scholar]
- 22.Binford RB, Mussell MP, Crosby RD, Peterson CB, Crow SJ, Mitchell JE. Coping Strategies in Bulimia Nervosa Treatment: Impact on Outcome in Group Cognitive-Behavioral Therapy. J Consult Clin Psychol. 2005;73(6):1089–1096. doi: 10.1037/0022-006X.73.6.1089. [DOI] [PubMed] [Google Scholar]
- 23.Barnes RD, Blomquist KK, Grilo CM. Exploring pretreatment weight trajectories in obese patients with binge eating disorder. Compr Psychiatry. 2011;52(3):312–318. doi: 10.1016/j.comppsych.2010.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ivezaj V, Kalebjian R, Grilo CM, Barnes RD. Comparing weight gain in the year prior to treatment for overweight and obese patients with and without binge eating disorder in primary care. J Psychosom Res. 2014;77(2):151–154. doi: 10.1016/j.jpsychores.2014.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pacanowski CR, Senso MM, Oriogun K, Crain AL, Sherwood NE. Binge Eating Behavior and Weight Loss Maintenance over a 2-Year Period. J Obes. 2014;2014:e249315. doi: 10.1155/2014/249315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stice E, Shaw HE. Role of body dissatisfaction in the onset and maintenance of eating pathology: a synthesis of research findings. J Psychosom Res. 2002;53(5):985–993. doi: 10.1016/s0022-3999(02)00488-9. [DOI] [PubMed] [Google Scholar]
- 27.Fairburn CG, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders: a “transdiagnostic” theory and treatment. Behav Res Ther. 2003;41(5):509–528. doi: 10.1016/s0005-7967(02)00088-8. [DOI] [PubMed] [Google Scholar]
- 28.Cohen J. A power primer. Psychol Bull. 1992;112(1):155. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 29.Masheb RM, Roberto CA, White MA. Nibbling and picking in obese patients with Binge Eating Disorder. Eat Behav. 2013;14(4):424–427. doi: 10.1016/j.eatbeh.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Björvell H, Rössner S, Stunkard A. Obesity, weight loss, and dietary restraint. Int J Eat Disord. 1986;5(4):727–734. [Google Scholar]
- 31.Fairburn C. Cognitive Behavior Therapy and Eating Disorders. Guilford Press; 2008. [Google Scholar]
- 32.Fossati M, Amati F, Painot D, Reiner M, Haenni C, Golay A. Cognitive-behavioral therapy with simultaneous nutritional and physical activity education in obese patients with binge eating disorder. Eat Weight Disord EWD. 2004;9(2):134–138. doi: 10.1007/BF03325057. [DOI] [PubMed] [Google Scholar]
- 33.Jeffery RW, Wing RR, Sherwood NE, Tate DF. Physical activity and weight loss: does prescribing higher physical activity goals improve outcome? Am J Clin Nutr. 2003;78(4):684–689. doi: 10.1093/ajcn/78.4.684. [DOI] [PubMed] [Google Scholar]
- 34.Penedo FJ, Dahn JR. Exercise and well-being: a review of mental and physical health benefits associated with physical activity. Curr Opin Psychiatry. 2005;18(2):189–193. doi: 10.1097/00001504-200503000-00013. [DOI] [PubMed] [Google Scholar]
- 35.Haedt-Matt AA, Keel PK. Revisiting the Affect Regulation Model of Binge Eating: A Meta-Analysis of Studies using Ecological Momentary Assessment. Psychol Bull. 2011;137(4):660–681. doi: 10.1037/a0023660. [DOI] [PMC free article] [PubMed] [Google Scholar]