Abstract
Objective
Individuals with overweight/obesity and loss-of-control eating (LOC) may experience poorer outcomes from behavioral weight loss (BWL) due to reactivity to internal (e.g., affective and physical) states that impact treatment adherence (e.g., dietary lapses). This study examined (1) whether the presence of LOC increased risk for dietary lapses and (2) the moderating role of LOC on the relation between internal states and dietary lapses.
Method
Individuals (n=189) with overweight and obesity completed ecological momentary assessment early in BWL.
Results
LOC was positively associated with dietary lapse. LOC did not moderate the relation between momentary changes in internal states and dietary lapses. However, the effect of average levels of internal states on lapses was attenuated for those with LOC.
Discussion
Results suggest that those with LOC are at higher risk of dietary lapse, while elevated average levels of internal states may contribute to early inadherence for those without LOC.
Keywords: loss-of-control eating, ecological momentary assessment, dietary lapses, behavioral weight loss, negative affect
Loss-of-control eating (LOC) is the hallmark characteristic of binge eating (BE) pathology and is associated with poor psychological and health outcomes, including excess weight (Goldschmidt, 2017; Wilfley, Wilson, & Agras, 2003). Research (although mixed) suggests that those with LOC may exhibit worse outcomes in behavioral weight loss (BWL) treatments (Munsch et al., 2007) possibly because BWL treatments do not adequately target factors that make it difficult for these individuals to control eating, resulting in poor adherence to BWL recommendations (e.g., staying under a calorie limit; Forman & Butryn, 2015). For example, standard BWL does not heavily emphasize strategies for coping with uncomfortable internal physical and affective states (e.g., negative mood, hunger). However, prior research has shown that BWL participants who report relatively higher average levels of numerous physical and affective states (i.e., sadness, loneliness, boredom, anger/irritation, stress, hunger, perceived deprivation, fatigue) are at greater risk of experiencing dietary lapses (i.e., discrete instances of non-adherence to a dietary prescription) (Forman et al., 2017). Additionally, risk for lapsing further increases at times when individuals experience greater hunger and perceived deprivation than is normal for them (Forman et al., 2017). Notably, many of these states robustly contribute to the occurrence of LOC and BE (Haedt-Matt & Keel, 2011). Thus, theoretically, those with LOC may be especially prone to react to uncomfortable internal states (such as negative emotions or hunger) by eating at an unintended time or a larger portion than planned, making adherence to BWL particularly difficult.
An important step in determining if or how to tailor BWL to individuals with LOC is to examine whether those with LOC indeed show decreased adherence to BWL and whether uncomfortable physical and affective states differentially predict treatment adherence among these individuals. In fact, no studies have directly examined these relationships using ecologically valid assessment. Adherence in a BWL program can be assessed via the occurrence of dietary lapses. Lapses may contribute to weight loss failure through increased caloric intake and degradation of motivation (Carels, Douglass, Cacciapaglia, & O’brien, 2004; Carels et al., 2001). Indeed, lapses have been shown to predict less weight loss both during early BWL and at one year (Forman et al., 2017), and early weight loss is related to longer-term success (Stotland & Larocque, 2005). It is especially important to identify early predictors of inadherence so that specialized intervention can be delivered to individuals as early as possible. Thus, examining whether the presence of LOC at baseline (1) is associated with increased dietary lapse risk and (2) moderates the relationship between affective/physical triggers and dietary lapses in BWL could help to identify individuals who may be more likely to experience long-term difficulties with weight control.
Current Study
First, we examined whether individuals who experienced any LOC episodes within the three months prior to starting treatment were more likely to experience dietary lapses during the first two weeks of a BWL program. Secondly, we examined whether the presence of LOC moderated the relationship between internal affective and physical states and dietary lapses. Given the difficulties with retrospective recall of dietary lapses and changing internal states, ecological momentary assessment (EMA; a data-collection method utilizing repeated sampling in a real-world context) is an ideal method through which to collect data on these experiences (Shiffman & Stone, 1998). We hypothesized that presence of LOC at baseline (measured by clinical interview) would be associated with increased risk for dietary lapses (measured via EMA) during the first two weeks of a BWL program, and that LOC would moderate the relationships between uncomfortable internal states (also measured by EMA) and dietary lapse occurrence. Specifically, we hypothesized that LOC would strengthen the relationship between average levels of uncomfortable states over the two weeks and lapse occurrence (i.e., those with greater average levels of uncomfortable states would be especially at risk for lapsing if they also had LOC; between-subjects effect). Additionally, we predicted that, controlling for average levels of internal states, LOC would strengthen the relationship between momentary increases in uncomfortable internal states and lapse occurrence (i.e., within-subjects effect). The present study is a secondary analysis of a larger EMA study of dietary lapses among BWL participants (Forman et al., 2017), which characterized the location and timing of lapses, examined the relationship between baseline lapse frequency and weight loss, and examined predictors of lapses. This study extends these findings by examining the potential influence of LOC status on lapse risk and triggers in early BWL.
METHODS
Participants
The sample consisted of 189 adults with overweight/obesity (BMI 27–50 kg/m2;MBMI=36.93 ±5.83 kg/m2; 82.0% female; 70.9% Caucasian; Mage= 51.81 ±9.76 years; ) participating in a BWL study (see Forman and colleagues (2016)). The intervention included 25 group sessions over 12 months, and included all features of standard BWL (e.g., tracking food consumption, reducing caloric intake). Although the larger treatment study compared the efficacy of standard and an acceptance-based BWL approach, data were collapsed across conditions for the present analyses, as conditions were identical for the first few weeks of treatment. Participants were recruited from the greater Philadelphia metropolitan community through various methods including radio advertisements, flyers, and primary care clinics.
Procedure
Participants were given an Android player (Samsung Galaxy Player 4.0) pre-loaded with a custom-designed EMA smartphone application (DrexelEMA). The EMA protocol occurred for 14 days within the first three weeks of treatment. Participants were given written and verbal instructions on how to use DrexelEMA and how to identify a dietary lapse. Participants received six prompts daily at semi-random intervals (i.e., ±30 minutes of 9:30 am, 12:00 pm, 2:30 pm, 5:00 pm, 7:15 pm, 9:30 pm) and were also instructed to initiate a survey whenever they experienced a dietary lapse. Time between the baseline assessment and start of treatment and the EMA protocol varied between 1–3 weeks. Procedures were approved by the Institutional Review Board of Drexel University.
Measures
LOC
The Overeating section of the Eating Disorder Examination (EDE) version 16, the gold standard for assessing for LOC (Grilo, Masheb, Lozano-Blanco, & Barry, 2004; Wilfley, Schwartz, Spurrell, & Fairburn, 1997), was administered to all participants. The EDE has demonstrated excellent psychometrics (Rizvi, Peterson, Crow, & Agras, 2000).
Ecological Momentary Assessment (EMA)
At each prompt, participants indicated whether they had experienced a dietary lapse since the last survey, with lapsing defined as “eating or drinking likely to cause weight gain, and/or put weight loss/maintenance at risk.” Based on an adapted version of the PANAS (Watson, Clark, & Tellegen, 1988), negative affect (sadness, irritation, loneliness, boredom, stress) and physical states (hunger, deprivation, fatigue) were measured on a 5-point Likert scale. To reduce burden, we did not include positive affect items. Given evidence that specific affective states are associated with dysregulated eating behavior (Berg et al., 2014), we used individual PANAS items rather than composite scores. For greater detail on the EMA protocol, see Forman et al (2017).
Statistical analyses
Separate generalized estimating equation (GEE) models based on a negative binomial distribution with a logit link function and a first-order autoregressive matrix structure were used to examine whether LOC predicted lapse occurrence at the next survey and whether each trigger’s impact on lapse occurrence was moderated by LOC. A model containing only LOC was used to examine the effect of LOC on lapse risk. All other models included between-subject effects (i.e., participants’ mean level across the two weeks) for each potential trigger, and lapse occurrence (yes/no) at the current survey. LOC was included as a predictor in each model and interactions between LOC and both between- and within-subject predictors were examined. All between-subjects variables were grand mean centered. Within-subjects effects were centered within person. Given the small number of males in the sample, we re-ran all analyses excluding males. Results were nearly identical. As such, for simplicity, we report results for analyses including both males and females.
RESULTS
Compliance
Mean compliance with prompted EMA surveys was 82.4% (SD=13.3%). Based on visual examination of the data, participants with less than 40% compliance with prompted surveys (n=3) were excluded from analyses (Forman et al., 2017). Fourteen participants reported no lapses during the assessment period; thus, a total of 172 participants contributed data for analyses predicting lapses.
Descriptive information
A total of 13,402 baseline EMA recordings (14.0% [n=1,876] from those with LOC), representing 2,470 participant days, were obtained. See Table 1 for descriptives for groups with and without LOC.
Table 1.
Demographic and Clinical characteristics by group
| LOC Group* (n=21) | No-LOC Group* (n=152) | t | p | Effect sizea | |
|---|---|---|---|---|---|
| Age (yrs) | 47.77 (14.70) | 52.44 (9.10) | 1.50 | .15 | .38 |
| Body Mass Index (kg/m2) | 38.48 (7.12) | 36.79 (5.62) | −2.67 | .10 | .26 |
| Subjective binge episodes (past 28 days) | 2.67 (4.05) | 0.00 (0.00) | -- | -- | -- |
| Objective binge episodes (past 28 days) | 2.33 (3.77) | 0.00 (0.00) | -- | -- | -- |
LOC = Loss of control group
Data are shown as mean (SD)
Cohen’s d
Main effects and moderating role of LOC
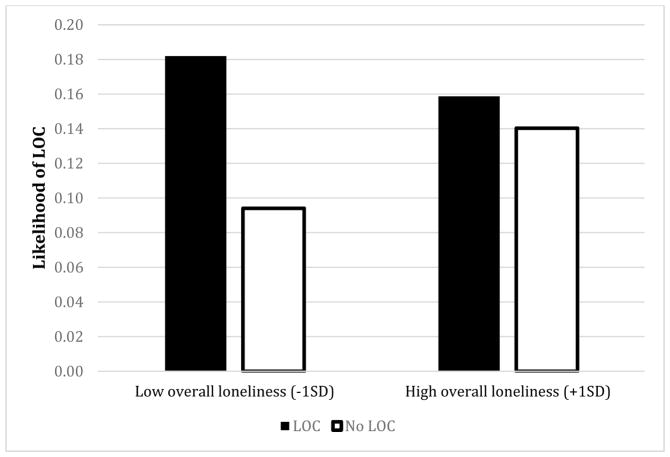
The presence of LOC at baseline was positively associated with overall risk for dietary lapses (B=.39, SE =.19, Waldχ2 =4.39, p=.04). Unexpectedly, LOC did not significantly moderate the effect of within-subjects (i.e., momentary changes, relative to one’s average level) increases in any facet of negative affect or physical states on dietary lapse occurrence at the next survey (Table 2). However, LOC significantly moderated the relation between several facets of between-subjects (i.e., one’s average level across the assessment period, relative to other participants’) negative affect/physical states (specifically, boredom, loneliness, irritation, hunger, and deprivation) and risk of lapsing at any given survey. The moderation effect was similar across variables such that those without LOC were at increased risk for lapsing when average levels of hunger, deprivation, boredom, irritation, and loneliness were higher, while those with LOC were at elevated risk for lapses regardless of average level of these variables (see Figure 1 for an example). Utilizing False Discovery Rate (Benjamini & Hochberg, 1995) for between-subjects interaction p-values, all statistically significant p-values remained < .05 when correcting for multiple comparisons.
Table 2.
Interactions between internal states and loss-of-control on likelihood of dietary lapse
| B | SE | 95% CI | Wald χ2 | P | OR | |
|---|---|---|---|---|---|---|
| Between-subjects x LOC interaction effects | ||||||
| Sadness | −.27 | .25 | [−.76, .21] | 1.23 | .27 | .76 |
| Loneliness | −.68 | .25 | [−1.16, −.20] | 7.58 | .01a | .50 |
| Boredom | −.76 | .33 | [−1.42, −.11] | 5.17 | .02a | .47 |
| Anger/Irritation | −.62 | .24 | [−1.10, −.13] | 6.09 | .01a | .54 |
| Stress | −.26 | .18 | [−.63, .10] | 2.10 | .15 | .77 |
| Hunger | −.83 | .34 | [−1.50, −.16] | 5.94 | .02a | .44 |
| Deprivation | −.50 | .22 | [−.93, −.06] | 5.02 | .03a | .61 |
| Fatigue | −.14 | .16 | [−.47, .18] | .77 | .39 | .87 |
| Within-subjects x LOC interaction effects | ||||||
| Sadness | .21 | .33 | [−.45, .86] | 3.79 | .54 | 1.23 |
| Loneliness | −.11 | .13 | [−.36, .14] | .75 | .39 | .90 |
| Boredom | .14 | .17 | [−.20, .48] | .64 | .42 | 1.15 |
| Anger/Irritation | −.13 | .12 | [−.36, .11] | 1.09 | .30 | .88 |
| Stress | .13 | .11 | [−.07, .33] | 1.60 | .21 | 1.13 |
| Hunger | .07 | .09 | [−.10, .24] | .70 | .41 | 1.07 |
| Deprivation | .07 | .12 | [−.17, .31] | .34 | .56 | 1.07 |
| Fatigue | −.10 | .09 | [−.28, .08] | 1.18 | .28 | .90 |
LOC = Loss of control
CI = Confidence interval
SE = Standard error
OR=Odds Ratio
Remained statistically significant when using False Discovery rate to correct for multiple comparisons
Note: Within-person x LOC and between-person x LOC interaction terms were included in the same statistical model for each trigger.
Figure 1.
Moderating role of loss-of-control eating on the relation between overall loneliness and risk for dietary lapse
DISCUSSION
This is the first study to examine whether presence of LOC predicted lapse risk among adults beginning BWL treatment, as well as whether LOC moderated the relationship between uncomfortable internal states and dietary lapses using EMA. As hypothesized, presence of LOC was associated with greater risk of lapse at any given survey, indicating that individuals with LOC may experience greater difficulty with adherence to dietary goals early in treatment. In particular, tendency to experience LOC may lead to instances of eating high-calorie foods and/or eating at unplanned times, potentially leading to greater difficulties with staying under a calorie recommendation, even at the beginning of treatment, when motivation is typically highest (Webber, Tate, Ward, & Bowling, 2010). Some research has suggested that individuals with LOC display poorer outcomes in behavioral weight loss treatment (Munsch et al., 2007), although results are mixed. As such, these results suggest that early adherence may be a useful intervention target for individuals with LOC.
The second aim of the study was to examine whether those with LOC were more prone to dietary lapse due to increased reactivity to internal states. Specifically, we posited that individuals with loss of control may be more prone to lapse in attempt to relieve or distract from negative affective states, which would be consistent with a body of literature linking increases in negative momentary affective states with episodes of LOC and BE (Haedt-Matt & Keel, 2011). While several momentary (i.e., within-subjects) increases in uncomfortable internal states have been shown to predict subsequent dietary lapses (Forman et al., 2017), LOC did not moderate any of these relationships. However, LOC did moderate the relationship between participants’ average levels (between-subjects) of hunger, deprivation, boredom, irritation, and loneliness. Interestingly and unexpectedly, results revealed that individuals with LOC were at elevated likelihood of lapsing regardless of average levels of these states, while individuals without LOC experienced increased lapse likelihood only at higher average levels of these states. These findings indicate that momentary increases or higher average levels (over the two weeks) of uncomfortable states do not confer additional risk for lapsing in individuals with LOC. Instead, presence of LOC appears to be a risk factor for lapsing independent of the average or momentary level of several internal states. However, increasing average levels of uncomfortable internal experiences are associated with increased lapse risk among individuals without LOC. It is possible that LOC itself is a powerful enough driver of lapses that overall levels of negative affect play less of a role for these individuals. While LOC may be driven by a desire to distract from or relieve negative affect states (Smyth et al., 2007), perhaps not all eating categorized as “lapsing” serves the same function as LOC, consistent with literature demonstrating that LOC is a distinct subtype of eating from other types of overeating (Latner, Hildebrandt, Rosewall, Chisholm, & Hayashi, 2007).
Although replication with larger samples of individuals with LOC is needed, the present study indicates that individuals with LOC (vs. without) are at greater risk of lapsing even at lower average levels of certain internal states. These results are consistent with restraint theory (Fairburn, Cooper, & Shafran, 2003), which states that individuals with LOC or BE pathology are more likely to see an increase in deleterious eating behaviors when rigid dietary restraint is high (due to deprivation, hunger and cravings), as it is during BWL. Consequently, it may be beneficial to attempt to target LOC directly (vs. targeting negative affect) to improve adherence in early BWL among these individuals. For example, those with LOC could be delivered targeted interventions from cognitive behavioral treatment known to reduce rigid dietary restraint and improve LOC (e.g., engaging in regular eating and engaging in alternative activities during urges; Fairburn, Cooper, & Shafran, 2003). These strategies, which aim to limit excessive dietary restraint while still inducing a negative calorie balance, could be integrated into standard BWL. Additionally, individuals without LOC who report high average levels of hunger, deprivation, boredom, irritation, and loneliness may benefit from interventions that aim to reduce or provide additional skills for coping with these experiences to improve adherence.
Study strengths include use of EMA to examine prospective relationships between internal experiences and lapse occurrence as measured in real-time, as well as examination of these relationships in a treatment-seeking sample. Key limitations include a relatively small subsample who endorsed LOC (which may have precluded our ability to detect differences), and failure to assess other internal experiences (e.g., positive affect) or social situations (e.g., parties) that may lead to lapses and may differentially relate to LOC. Additionally, while showing distinct advantages over traditional self-report, EMA still involves individuals reporting on their own behavior. As such, there may have been problems with recall bias and some level of subjectivity with lapse identification (i.e. in deciding what put one’s weight loss goals at risk). It is also important to note that LOC and binge episodes were not collected via EMA. Future research should examine whether LOC severity (e.g., frequency and size of LOC episodes, diagnosis of binge eating disorder) impacts these relationships, and should examine differential predictors of both LOC/binge episodes (as measured via EMA) and dietary lapses within individuals in BWL. Additionally, given the poor long-term outcomes of BWL (Wadden & Butryn, 2003), it will also be important to examine factors that drive dietary lapses later on in treatment.
Overall, this study suggests that LOC differentially impacts dietary adherence during early BWL treatment. Given research that early performance in BWL predicts later outcomes (Stotland & Larocque, 2005), these findings highlight need for additional investigation of momentary correlates of inadherence to dietary prescriptions.
Acknowledgments
This study was funded by grants from the National Institute for Diabetes and Digestive and Kidney Diseases (R01 DK095069) to Dr. Forman and the National Institute of Mental Health (F31 MH108279, K23MH105680) to Drs. Manasse and Juarascio, respectively.
Funding Agencies: National Institute for Diabetes and Digestive and Kidney Diseases (R01 DK095069; PI: Forman), National Institute of Mental Health (F31 MH108279, PI: Manasse)
References
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the royal statistical society. Series B (Methodological) 1995:289–300. [Google Scholar]
- Berg KC, Peterson CB, Crosby RD, Cao L, Crow SJ, Engel SG, Wonderlich SA. Relationship between daily affect and overeating-only, loss of control eating-only, and binge eating episodes in obese adults. Psychiatry research. 2014;215(1):185–191. doi: 10.1016/j.psychres.2013.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carels RA, Douglass OM, Cacciapaglia HM, O’brien WH. An ecological momentary assessment of relapse crises in dieting. Journal of consulting and clinical psychology. 2004;72(2):341. doi: 10.1037/0022-006X.72.2.341. [DOI] [PubMed] [Google Scholar]
- Carels RA, Hoffman J, Collins A, Raber AC, Cacciapaglia H, O’Brien WH. Ecological momentary assessment of temptation and lapse in dieting. Eating Behaviors. 2001;2(4):307–321. doi: 10.1016/s1471-0153(01)00037-x. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z, Shafran R. Cognitive behaviour therapy for eating disorders: A “transdiagnostic” theory and treatment. Behaviour research and therapy. 2003;41(5):509–528. doi: 10.1016/s0005-7967(02)00088-8. [DOI] [PubMed] [Google Scholar]
- Forman EM, Butryn ML. A new look at the science of weight control: how acceptance and commitment strategies can address the challenge of self-regulation. Appetite. 2015;84:171–180. doi: 10.1016/j.appet.2014.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman EM, Butryn ML, Manasse SM, Crosby RD, Goldstein SP, Wyckoff EP, Thomas JG. Acceptance-based versus standard behavioral treatment for obesity: Results from the mind your health randomized controlled trial. Obesity. 2016;24(10):2050–2056. doi: 10.1002/oby.21601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman EM, Schumacher LM, Crosby R, Manasse SM, Goldstein SP, Butryn ML, … Thomas JG. Ecological Momentary Assessment of Dietary Lapses Across Behavioral Weight Loss Treatment: Characteristics, Predictors, and Relationships with Weight Change. Annals of Behavioral Medicine. 2017:1–13. doi: 10.1007/s12160-017-9897-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldschmidt AB. Are loss of control while eating and overeating valid constructs? A critical review of the literature. Obesity Reviews. 2017;18(4):412–449. doi: 10.1111/obr.12491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Lozano-Blanco C, Barry DT. Reliability of the Eating Disorder Examination in patients with binge eating disorder. International journal of eating disorders. 2004;35(1):80–85. doi: 10.1002/eat.10238. [DOI] [PubMed] [Google Scholar]
- Haedt-Matt AA, Keel PK. Revisiting the affect regulation model of binge eating: a meta-analysis of studies using ecological momentary assessment. Psychological bulletin. 2011;137(4):660. doi: 10.1037/a0023660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latner JD, Hildebrandt T, Rosewall JK, Chisholm AM, Hayashi K. Loss of control over eating reflects eating disturbances and general psychopathology. Behaviour research and therapy. 2007;45(9):2203–2211. doi: 10.1016/j.brat.2006.12.002. [DOI] [PubMed] [Google Scholar]
- Munsch S, Biedert E, Meyer A, Michael T, Schlup B, Tuch A, Margraf J. A randomized comparison of cognitive behavioral therapy and behavioral weight loss treatment for overweight individuals with binge eating disorder. International journal of eating disorders. 2007;40(2):102–113. doi: 10.1002/eat.20350. [DOI] [PubMed] [Google Scholar]
- Rizvi SL, Peterson CB, Crow SJ, Agras WS. Test-retest reliability of the eating disorder examination. International journal of eating disorders. 2000;28(3):311–316. doi: 10.1002/1098-108x(200011)28:3<311::aid-eat8>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Stone AA. Ecological momentary assessment: A new tool for behavioral medicine research. Technology and methods in behavioral medicine. 1998:117–131. [Google Scholar]
- Smyth JM, Wonderlich SA, Heron KE, Sliwinski MJ, Crosby RD, Mitchell JE, Engel SG. Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. Journal of consulting and clinical psychology. 2007;75(4):629. doi: 10.1037/0022-006X.75.4.629. [DOI] [PubMed] [Google Scholar]
- Stotland S, Larocque M. Early treatment response as a predictor of ongoing weight loss in obesity treatment. British journal of health psychology. 2005;10(4):601–614. doi: 10.1348/135910705X43750. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Butryn ML. Behavioral treatment of obesity. Endocrinology and Metabolism Clinics. 2003;32(4):981–1003. doi: 10.1016/s0889-8529(03)00072-0. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of personality and social psychology. 1988;54(6):1063. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Webber KH, Tate DF, Ward DS, Bowling JM. Motivation and its relationship to adherence to self-monitoring and weight loss in a 16-week Internet behavioral weight loss intervention. Journal of nutrition education and behavior. 2010;42(3):161–167. doi: 10.1016/j.jneb.2009.03.001. [DOI] [PubMed] [Google Scholar]
- Wilfley DE, Schwartz MB, Spurrell EB, Fairburn CG. Assessing the specific psychopathology of binge eating disorder patients: Interview or self-report? Behaviour Research and Therapy. 1997;35(12):1151–1159. [PubMed] [Google Scholar]
- Wilfley DE, Wilson GT, Agras WS. The clinical significance of binge eating disorder. International journal of eating disorders. 2003;34(S1):S96–S106. doi: 10.1002/eat.10209. [DOI] [PubMed] [Google Scholar]