Abstract
Objective
Despite growing interest in children and young people’s (CYP) perspectives on healthcare, they continue to be excluded from many patient experience surveys. This study investigated the feasibility of, and additional information gained by, measuring CYP experiences of a recent hospital admission.
Design
Cross-sectional analysis of national survey data.
Setting
Inpatients aged 8–15 years in eligible National Health Service hospitals, July–September 2014.
Participants
6204 parents/carers completed the parent section of the survey. The CYP section of the survey was completed by CYP themselves (n=3592), parents (n=849) or jointly (n=1763).
Main outcome measures
Pain relief, involvement, quality of staff communication, perceived safety, ward environment, overall experience.
Analyses
Single-measures intraclass correlations (ICCs) were used to assess the concordance between CYP and parent responses about the same inpatient episode. Multilevel logistic regression models, adjusted for individual characteristics, were used to compare the odds of positive responses when the CYP section of the survey was completed by parents, by CYP themselves or jointly.
Results
The CYP section of the survey was completed independently by 57.8% of CYP. Agreement between CYP and parent responses was reasonably good for pain relief (ICC=0.61 (95% CI 0.58 to 0.63)) and overall experience (ICC=0.70 (95% CI 0.68 to 0.72)), but much lower for questions comparing professionals’ communication with CYP and with their parents (ICC range=0.28 (95% CI 0.24 to 0.32) to 0.51 (95% CI 0.47 to 0.54)). In the regression models, CYP were significantly less likely than parents to report feeling safe (adjusted OR (AOR)=0.54 (95% CI 0.38 to 0.76)), involvement in decisions (AOR=0.66 (95% CI 0.46 to 0.94)) or adequate privacy (AOR=0.68 (95% CI 0.52 to 0.89)).
Conclusions
Including CYP (8–15 years) in patient experience surveys is feasible and enhances what is known from parents’ responses.
Keywords: children, young people, patient perspective, inpatient experience, measurement
What is already known on this subject?
Data from patient experience surveys can help to empower patients, improve the quality and patient-centredness of care and make an important contribution to improving health outcomes.
Typically, children and young people below 16–18 years are either not included in patient experience surveys or their parents are asked to respond on their behalf.
What this study adds?
Including children and young people in patient experience surveys is feasible and enhances what is known from parents’ responses.
Background
Patients’ perspectives are essential to understanding the quality of healthcare services and delivering patient-centred care.1 2 Patient-centredness is recognised as a key pillar of health quality in its own right, and as an important determinant of health outcomes.3 4 Central to developing and monitoring such care has been an increase in the use of patient experience surveys, which are now administered routinely in many healthcare settings.4
Historically, most patient experience surveys have been restricted to adults.5 6 When children and young people’s (CYP) care is included in patient experience surveys, parents or caregivers (henceforth referred to as parents) are usually asked to respond on their behalf.5 7 Two reported reason for not asking CYP themselves have been concerns about gaining parental consent and lack of evidence about the feasibility of asking them to complete surveys.8 While it is clear that young children are unlikely to be able to provide detailed experience information, there is increasing evidence that young people may be willing to respond to age-appropriate surveys from the age of 8 onwards and that their healthcare priorities evolve and progressively diverge from those of their parents from the age of 12 onwards.9–11 However, it is not known whether, and from what age, it would be feasible to include CYP themselves in routine, large-scale programmes to measure patient experience. Lastly, it is not known whether asking CYP themselves would yield significant additional information about their experiences, over and above the information that can be obtained from parents answering on their behalf.
Data from the English Children and Young People’s Inpatient and Day Case Survey 201412 allow for investigation of these questions using a large, nationally representative sample of CYP who were recently discharged from hospital. This survey was administered in 137 acute and specialist NHS Hospital Trusts in England admitting paediatric patients. For CYP aged 8–15 years, child-friendly surveys were administered, which contained two sections: a CYP section for the child/young person to complete (with input from their parents where necessary), and a section for their parents.
The first aim of this study was to investigate the proportion and characteristics of CYP who completed the CYP section independently. The second aim was to study the agreement between reports by CYP and their parents on the same inpatient episode. Third, we investigated whether there were systematic differences in responses to the CYP section when it was completed by CYP, parents or jointly.
Methods
Data
Data from the Children and Young People’s Inpatient and Day Case Survey 2014 were analysed for patients aged 8–15 years (response rate=27%). Questionnaires were posted to consecutively discharged patients (overnight stays and day case admissions) between July and September 2014. Surveys comprised two sections: a section for their parent (n=6204) and a CYP section that could be completed by CYP themselves (n=3592), parents (n=849) or jointly (n=1763). Survey report and sampling procedures have been published previously.13 Further details on methodology are presented in the online supplementary appendix (Methods section).
archdischild-2017-313801supp001.docx (28.8KB, docx)
Variables and analyses
This study comprised three sets of analyses, corresponding to the three study aims.
Descriptive analysis of the sociodemographic and clinical characteristics of CYP in each category of respondent: by themselves, by their parents or jointly.
Analysis of CYP-parent dyads to compare the responses of CYP and their parents on the same inpatient admission, for CYP who responded by themselves.
Comparison of parent, CYP and joint responses to the CYP section (both unadjusted and adjusted for sociodemographic and clinical characteristics).
The details of each set of analyses are described in turn below.
Descriptive analysis of CYP respondents
The proportion of CYP surveys completed by the CYP, parent and jointly were calculated—both overall and disaggregated by patient characteristics (age group (8–11 vs 12–15 years), sex, ethnicity, elective vs emergency admission, number of admissions within the past year (1–3 vs ≥4) and presence of any long-standing illness or condition (see online supplementary appendix for wording of the questions and responses). Next, parental and joint responses were combined to create a dichotomised outcome of any parental involvement versus independent CYP response. Χ2 tests were used to assess the significance of differences in the rates of independent CYP responses between each sociodemographic and clinical group.
Analysis of CYP-parent dyads
Data from CYP-parent dyads were used to compare responses about the same inpatient admission from the two sections of the survey. Dyads were only included if the CYP completed his/her section independently.
For three questions (presence of pain, pain relief, overall experience), direct comparisons were possible between CYP self-reported experience and parent’s perceptions of his/her child’s experience. For an additional seven questions, CYP perceptions of how staff communicated with and involved them (as the child/patient) were compared with parental views of how staff communicated with and involved them (as the parent). The wording of the questions and dichotomised responses in the CYP and parent sections of the survey are presented in online supplementary appendix table A1 and table A2.
First, the single-measures intraclass correlation (ICC) was calculated, to assess the level of agreement between CYP and parent responses. These analyses made use of all response options. Next, using the dichotomised responses shown in table 1, the proportions of CYP and parents reporting a positive experience of care on each measure were calculated. Then, the degree of disagreement between dichotomised CYP and parent responses was calculated, using
The proportion of surveys where the CYP and parental responses differ and
The proportion where the CYP response was less positive than their parent’s response.
Table 1.
Respondents to the children and young people’s (CYP) section of the survey, by selected individual characteristics. Children and Young People’s Inpatient Survey, England, 2014
| Individual characteristics | N | CYP responses (%) | Parent responses (%) | Joint response (%) |
| Overall | 6204 | 57.9 | 13.7 | 28.4 |
| Male | 3247 | 53.6 | 15.2 | 31.2 |
| Female | 2957 | 62.6*** | 12.0 | 25.4 |
| 8–11 years | 2959 | 52.1 | 16.6 | 31.3 |
| 12–15 years | 3245 | 63.1*** | 11.1 | 25.8 |
| Any long-standing condition | 1906 | 50.4 | 20.8 | 28.8 |
| No long-standing condition | 3341 | 62.7*** | 9.4 | 27.9 |
| 1–3 admissions | 5467 | 58.9 | 13.3 | 27.9 |
| 4 or more admissions | 416 | 52.6* | 17.1 | 30.3 |
| White | 5090 | 60.4 | 12.1 | 27.5 |
| Asian/British Asian | 458 | 42.8*** | 23.4 | 33.8 |
| Black/Black British | 205 | 46.8*** | 16.6 | 36.6 |
| Mixed/other/not known | 450 | 50.0*** | 20.9 | 29.1 |
| Inpatient 1 | 2471 | 60.3 | 13.2 | 26.5 |
| Day case | 3732 | 56.4** | 14.0 | 29.6 |
| Children’s ward | 5569 | 57.9 | 13.9 | 28.2 |
| Adolescent ward | 342 | 64.0 | 9.9 | 26.0 |
| Adult ward 205 | 88 | 52.3 | 17.0 | 30.7 |
| Any procedure | 4172 | 59.3 | 12.4 | 28.3 |
| No procedure 84 | 1948 | 55.4** | 16.3 | 28.3 |
| Elective admission 1 | 3350 | 57.4 | 13.9 | 28.7 |
| Emergency admission | 2853 | 58.5 | 13.4 | 28.1 |
Column categories are based on responses to the item in the parent section of the survey ‘Who was the main person who answered the questions in the children and young people s section of the questionnaire?’
Where the proportion of CYP who responded independently differs significantly from the reference group (eg, females differ to males), this is indicated by *P<0·05, **P<0·01, ***P<0·001.
Where P values were between 0.001 and 0.05, exact values were as follows: 1–3 vs 4 or more admissions P=0.013; inpatient vs day case P=0.002; any vs no procedure P=0.004.
Row categories follow response options to each question in the survey.
Age, sex, ethnicity, type of admission were drawn from hospital records and had negligible missing data. Other characteristics were drawn from parent/carer responses, resulting in the following number of missing responses: presence of long-standing condition=957 (15.4%); any procedure=84 (1.4%); number of admissions=321 (5.2%); ward type=205 (3.3%).
Note that for the overall experience of care question, analyses of the dichotomised (or ‘top-box’) responses (0–8/10 vs 9–10/10) are presented in table 2; analyses of the exact scores were also performed and are presented separately. ICC values were assigned the following categories:<0.40=poor; 0.40–0.59=fair; 0.60–0.74=good; 0.75–1.00=excellent agreement.14
Table 2.
Agreement between reports of the same inpatient admission by children and young people (CYP) and their parent/carer. Children and Young People’s Inpatient Survey, England, 2014.
| N | CYP response Positive (%) |
Parent response Positive (%) |
CYP and parents’ non-concordant (%) | CYP response less positive than parent’s (%) | Single measures ICC (95% CI) | |
| Presence of pain (8–15 years) |
3470 | 65.9 | 68.4 | 11.9 | 4.7 | 0.73 (0.71 to 0.75)* |
| Pain relief (8–15 years) |
1888 | 80.0 | 78.4 | 18.6 | 8.4 | 0.61 (0.58 to 0.63)* |
| Overall experience (8–15 years) |
3394 | 55.8 | 59.3 | 23.5 | 13.5 | 0.70 (0.68 to 0.72)* |
| Involvement in decisions (12–15 years) |
1534 | 55.1 | 66.6 | 42.7 | 28.3 | 0.34 (0.29 to 0.39)† |
| Communication on arrival (8–15 years) |
3347 | 75.0 | 77.1 | 25.6 | 14.8 | 0.41 (0.38 to 0.44)‡ |
| Communication about care and treatment (8–15 years) |
3363 | 81.1 | 87.5 | 20.5 | 13.8 | 0.30 (0.26 to 0.33)† |
| Communication before operation/procedure (8–15 years) |
1923 | 91.4 | 89.7 | 13.7 | 6.2 | 0.28 (0.24 to 0.32)† |
| Communication after operation/procedure (8–15 years) |
1929 | 70.0 | 83.8 | 29.5 | 22.6 | 0.32 (0.25 to 0.38)† |
| Discharge communication (12–15 years) |
1459 | 60.5 | 69.5 | 34.4 | 22.3 | 0.47 (0.42 to 0.52)‡ |
| Advice on postdischarge care (12–15 years) |
1505 | 74.6 | 73.6 | 26.6 | 13.4 | 0.51 (0.47 to 0.54)‡ |
Columns 3–6 show analyses of dichotomised responses (see online supplementary appendix table A1 for details of response options and dichotomisation for each questionnaire item); N values differ, as some questions were not applicable to all patients and questions (eg, not all patients had an operation/procedure) and some questions were worded differently for younger patients (8 – 11 years) so direct comparison with parent responses is not possible. The first three questions compare the CYP’s response on their own experience with the parent’s response about their child’s experience. The next seven questions compare CYP perceptions of how staff communicated with them (as the child/ patient) to parental views of how staff communicated with them (as the parent).
The intraclass correlation coefficients (ICCs) in column seven are calculated using non-dichotomised responses. Following Cicchetti et al,22 ICC values were assigned the following categories: *0.60 – 0.74 — good agreement; †<0.40—poor agreement; ‡0.40– 0.59—fair agreement.
Analysis of differences between parent, CYP and joint responses to the CYP section
Data from the CYP section of the survey were used to compare responses according to who answered the survey: parent, CYP and joint responses. Thirteen dichotomised patient experience measures from the CYP section of the survey were analysed, which related to the hospital environment, staff attitudes and communication and overall care rating. The wording of all questions is presented in online supplementary appendix table A2. Unadjusted and adjusted logistic regression models were conducted; multilevel, adjusted models included all patient variables listed above (as fixed main effects at patient level) and admitting Hospital Trust (as a random effect at Trust level). Descriptive analyses were performed using SPSS V.23 and regression models created using MLwiN V.2.36.
Results
Descriptive analysis of CYP respondents
The majority (3592/6204=57.9%) of patients aged 8–15 years completed the CYP section of the survey themselves. Parents responded in 849 (13.7%) cases; the remaining 1763 (28.4%) were completed jointly by CYP and their parents.
Table 1 presents the response categories by selected individual variables. Surveys were more likely to be completed by CYP themselves (rather than by parents or jointly) when they were females versus males (62.6% vs 53.6%, P<0.001), older children (63.1% among 12–15 years vs 52.1% among 8–11 years, P<0.001), those with no long-standing condition (62.7% vs 50.4%, P<0.001), those with 1–3 versus four or more hospital admissions within the past 6 months (58.9% vs 52.6%, P=0.013) and those reporting white ethnicity (60.4%) versus black (46.8%, P<0.001), Asian (42.8%, P<0.001) or mixed/other/not known (50.0%, P<0.001). CYP were also more likely to respond themselves if they were admitted as an inpatient rather than a day case (60.3% vs 56.4%, P=0.002). Response rates did not differ significantly by ward type or elective versus emergency admission; regarding ward type, this may reflect the small number of patients admitted to adolescent or adult wards.
Analysis of CYP-parent dyads
Table 2 presents the proportion of positive responses and the agreement between responses by the CYP-parent dyads. Despite good overall agreement between CYP and parent responses regarding the presence of pain (ICC=0.73 (95% CI 0.71 to 0.75)), in 163 dyads (4.7%) CYP reported having had pain but their parents reported no pain, while the converse was true in 250 dyads (7.2%). Where both CYP and parents reported the CYP having had pain, the ICC value for good attention to pain control was 0.61 (95% CI 0.58 to 0.63), with CYP reporting poorer experience for pain management than their parents in 8.4% of cases. For overall experience, ICC was 0.70 (95% CI 0.68 to 0.72). Analysing dichotomised responses (as shown in the table), CYP were more positive than their parents regarding overall experience in 10.0% of cases, and less positive in 13.5%. Analysis of the exact scores (0–10) showed agreement in only 49.2% of dyads (see supplementary appendix table C and table D for further details).
Involvement in decisions about care was reported by 55.1% of CYP, by 66.6% of parents and by both in only 43.1% of dyads. There were considerable differences between CYP and their parents (ICC 0.34 (95% CI 0.29 to 0.39)), with disagreement in 42.7% of cases, and CYP reporting lower involvement than their parents in 28.3%. Similarly, low levels of agreement were seen between CYP and parental responses for the six indicators of communication (ICC range 0.28–0.51; non-concordance in 13.7%–34.4% of cases, with CYP reporting poorer experience of staff communication than their parents in 6.2%–22.6% of dyads).
Analysis of differences between parent, CYP and joint responses to the CYP section
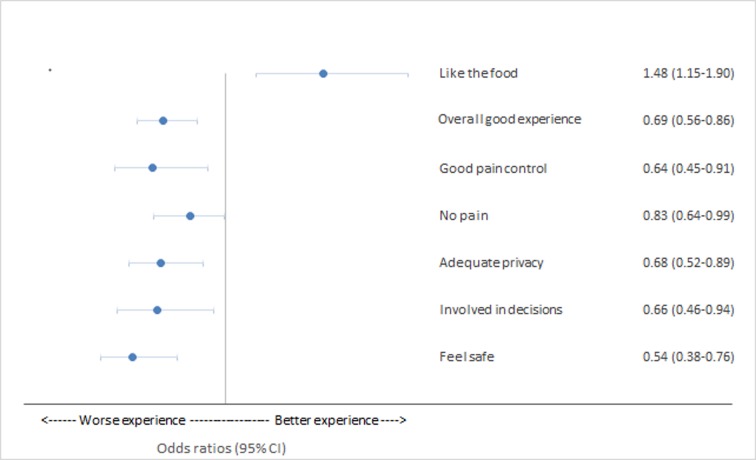
The proportions of positive responses to each question by CYP, parents and jointly are shown in online supplementary appendix table B. In table 3, data from the CYP section show the ORs of positive responses for CYP and joint responses, compared with parental responses; the adjusted ORs (AOR) for selected questions are also shown in figure 1.
Table 3.
ORs of positive reported patient experience in surveys completed by children and young people (CYP) themselves or jointly, compared with surveys completed by parents/carers. Children and Young People’s Inpatient Survey, England, 2014
| OR (95% CI) | P value | Adjusted OR (95% CI) | P value | |
| Did you feel safe on the hospital ward? (8–15 years) | ||||
| CYP | 0.84 (0.62 to 1.13) | 0.24 | 0.54 (0.38 to 0.76) | <0.001 |
| Joint | 1.09 (0.78 to 1.53) | 0.60 | 0.78 (0.54 to 1.12) | 0.18 |
| Did hospital staff play with you or do any activities with you while you were in hospital? (8–11 years) | ||||
| CYP | 0.81 (0.47 to 1.02) | 0.06 | 0.70 (0.45 to 1.07) | 0.10 |
| Joint | 1.06 (0.71 to 1.58) | 0.80 | 1.05 (0.68 to 1.61) | 0.83 |
| Were there enough things for someone of your age to do on the ward? (12–15 years) | ||||
| CYP | 0.87 (0.61 to 1.24) | 0.44 | 0.91 (0.61 to 1.35) | 0.62 |
| Joint | 1.26 (0.86 to 1.85) | 0.24 | 1.26 (0.83 to 1.92) | 0.28 |
| Did you like the hospital food? (8–15 years) | ||||
| CYP | 1.43 (1.13 to 1.79) | 0.002 | 1.48 (1.15 to 1.90) | 0.002 |
| Joint | 1.27 (0.99 to 1.63) | 0.06 | 1.27 (0.97 to 1.65) | 0.08 |
| Did hospital staff talk to you about how they were going to care for you, in a way that you could understand? (8–15 years) | ||||
| CYP | 1.23 (0.98 to 1.54) | 0.07 | 0.80 (0.62 to 1.04) | 0.10 |
| Joint | 1.37 (1.06 to 1.76) | 0.02 | 0.98 (0.74 to 1.29) | 0.88 |
| Were you involved in decisions about your care? (12–15 years) | ||||
| CYP | 0.87 (0.60 to 1.10) | 0.18 | 0.66 (0.46 to 0.94) | 0.02 |
| Joint | 0.97 (0.69 to 1.35) | 0.84 | 0.81 (0.56 to 1.18) | 0.27 |
| If you had any worries, did someone at the hospital talk with you about them? (8–15 years) | ||||
| CYP | 1.26 (1.00 to 1.58) | 0.048 | 0.92 (0.71 to 1.20) | 0.54 |
| Joint | 1.59 (1.22 to 2.05) | <0.001 | 1.24 (0.94 to 1.64) | 0.14 |
| Did staff talk to each other about you as if you were not there? (8–15 years) | ||||
| CYP | 0.85 (0.60 to 1.20) | 0.36 | 1.02 (0.68 to 1.54) | 0.93 |
| Joint | 0.62 (0.42 to 0.93) | 0.02 | 0.70 (0.45 to 1.09) | 0.11 |
| Were you given enough privacy when you were receiving care and treatment? (8–15 years) | ||||
| CYP | 0.82 (0.64 to 1.03) | 0.09 | 0.68 (0.52 to 0.89) | 0.005 |
| Joint | 1.07 (0.82 to 1.40) | 0.60 | 0.93 (0.70 to 1.24) | 0.62 |
| Did your condition ever cause you pain when you were in hospital? (8–15 years) | ||||
| CYP | 1.33 (1.10 to 1.61) | 0.004 | 1.21 (1.01 to 1.56) | 0.04 |
| Joint | 1.20 (0.98 to 1.49) | 0.08 | 1.19 (0.94 to 1.49) | 0.15 |
| Do you think the hospital staff did everything they could to help your pain? (8–15 years) | ||||
| CYP | 0.86 (0.63 to 1.17) | 0.33 | 0.64 (0.45 to 0.91) | 0.01 |
| Joint | 1.13 (0.80 to 1.59) | 0.50 | 0.90 (0.62 to 1.30) | 0.56 |
| Do you feel that the people looking after you listened to you? (8–15 years) | ||||
| CYP | 1.25 (1.01 to 1.55) | 0.04 | 1.06 (0.83 to 1.36) | 0.65 |
| Joint | 1.28 (1.01 to 1.63) | 0.04 | 1.07 (0.83 to 1.39) | 0.60 |
| Do you feel that the people looking after you were friendly? (8–15 years) | ||||
| CYP | 1.20 (0.91 to 1.57) | 0.20 | 1.05 (0.77 to 1.43) | 0.76 |
| Joint | 1.24 (0.92 to 1.67) | 0.17 | 1.07 (0.77 to 1.48) | 0.71 |
| Overall experience (8–15 years) | ||||
| CYP | 0.73 (0.60 to 0.89) | 0.002 | 0.69 (0.56 to 0.86) | 0.001 |
| Joint | 1.03 (0.83 to 1.27) | 0.81 | 0.96 (0.77 to 1.20) | 0.71 |
All experience measures were dichotomised. See online supplementary appendix table A2 for details.
Adjusted ORs were derived from logistic regression models that adjusted for trust (as a random effect at trust level) and the following variables as fixed effects at patient level: age, sex, ethnicity, reason for admission (elective vs emergency), whether had operation/procedure, day case vs overnight stay, previous experience of inpatient or day case care (1–3 vs 4+ admissions within the past 6 months), presence of any long-standing condition, ward type (children’s/adolescent/adult).
Figure 1.
Adjusted ORs of good experience, children and young people (CYP) vs parent responses. Selected indicators from CYP Inpatient Survey, England, 2014.
CYP were significantly more likely than their parents to report pain (AOR 1.21 (95% CI 1.01 to 1.56), P=0.04). CYP were less likely to report that staff did all they could to help ease the pain (AOR 0.64 (95% CI 0.45 to 0.91), P=0.01); they felt safe on the ward (AOR 0.54 (95% CI 0.38 to 0.76), P<0.001); they were involved in decisions about their care (AOR 0.66 (95% CI 0.46 to 0.94), P=0.02) or they were given enough privacy (AOR 0.68 (95% CI 0.52 to 0.89), P=0.005). The likelihood of a good overall care rating (9-10/10) was also lower for CYP AOR=0.69 (95% CI 0.56 to 0.86), P=0.001). Conversely, there were significantly higher odds of positive responses about hospital food when the survey was completed by CYP themselves, rather than by their parents (AOR 1.48 (95% CI 1.15 to 1.90), P=0.002). There were no significant differences between CYP and parental responses in the odds of responding positively to the other questions, and no significant differences between parent and joint responses.
Discussion
Although many have argued against collecting patient experience data from CYP because they would fail to complete surveys or give answers that matched their parent’s responses, this study shows that CYP will indeed respond and provide information that enhances what is known from their parents. Direct comparisons of the experiences of CYP and their parents during the same inpatient admission showed that parents’ responses often do not capture important aspects of CYP’s experience relating to pain, involvement and communication. Overall care ratings by CYP and parents differed in about one-quarter (24%) of families (using dichotomised or ‘top-box’ scores) and over half (51%) of families when comparing the exact rating. Comparing surveys completed by CYP and parents, and adjusting for patient characteristics, CYP responses were less positive than parents’ responses regarding safety, pain relief, involvement in decisions, privacy and overall care rating.
These analyses used questions that had undergone a rigorous process of piloting and cognitive testing with their relevant age groups and the survey sample has previously been shown to be broadly representative of the NHS inpatient population in this age group.12 13 The overall response rate of 27% was similar to other paediatric surveys that are only addressed to parents,7 but the risk of differential non-response limits our ability to generalise the first set of findings to all NHS patients in this age group.
The analyses investigating whether CYP and parent responses differ are also subject to limitations. It is possible that minor wording differences and/or differences in interpretation may have influenced the degree of agreement between CYP and parent responses. It was also not possible to compare parent and CYP responses directly for the majority of questions. Lastly, while our regression models were able to adjust for a number of important potential confounders, we cannot exclude unseen confounding by factors not included in our models. In particular, no data were available to indicate how many patients were not able to respond independently due to cognitive impairment, or due to additional physical or communication needs.
Research and policy context
WHO has recommended as a key research priority developing better ways of understanding and monitoring the views of young people.14 To our knowledge, this is the first national study to report detailed characteristics of CYP who complete a patient experience survey. Although previous literature is sparse, we report a larger number of CYP responding independently than the previous English survey in 2004, when a minority (38%) of CYP aged 12–15 years and very few below the age of 12 years completed the survey themselves.15 This may reflect the extensive work that has been done to develop a questionnaire that is designed specifically for CYP. There may also be an increasing level of willingness among CYP to express their views and a greater expectation that their views will be listened to.16 17
Although responses from CYP have long been used in the diagnosis and management of some paediatric conditions,18 we are not aware of other national-level studies that investigate the additional benefit of CYP reporting their patient experience (rather than relying on parent responses). It confirms and extends the findings of smaller, single-centre studies, which have shown that parent and CYP responses to patient experience surveys often differ, with a tendency for CYP to be less positive about the quality of care they have received.19 20 Lastly, our findings extend previous research with parents, which showed that the quality of communication with CYP and with parents are distinct aspects of paediatric care and should be evaluated separately.7
Conclusion
The Royal College of Paediatrics and Child Health has stated that ‘no-one is better qualified to comment on the care provided by a paediatric centre than the CYP receiving that care’.21 Yet, in practice, CYP are rarely given the opportunity to express their views or report their experience of healthcare. Our findings demonstrate that it is feasible to collect the views of CYP (8–15 years) and that doing so yields important additional information, beyond what is possible from parent surveys alone.
A key research question for the future is whether monitoring and improving CYP experience of healthcare could promote more patient-centred care for this age group, which may in turn promote healthier behaviour, including adherence to treatment regimens, and improve long-term health outcomes. There is also a need for research into whether administering the questionnaire electronically, and/or using shorter versions of questionnaires could improve response rates and provide more timely information with which to improve services.
Footnotes
Contributors: DSH, SS, JP, AT, RMV conceived and designed the study. SS performed all analyses. All authors critically reviewed the manuscript. SS and DSH are the guarantors. DSH affirms that the manuscript is an honest, accurate and transparent account of the study being reported; that no important aspects of the study have been omitted and that any discrepancies from the study as planned (and, if relevant, registered) have been explained. All authors, external and internal, had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Competing interests: SS, AT and BH are employed by Picker Institute Europe, which provides survey coordination services for the NHS patient surveys under contract to the Care Quality Commission. DSH is supported by the Health Foundation.
Ethics approval: These were secondary analyses of anonymised data and were approved by the Care Quality Commission. The survey implementation itself was given a favourable ethical opinion by NRES Committees—North of Scotland ref 14/NS/0006.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. World Health Organisation. WHO global strategy on people-centred and integrated health services. Geneva: World Health Organisation, 2015. [Google Scholar]
- 2. Agency for Healthcare Research and Quality (AHRQ). Understanding quality measurement. Rockville MD: Agency for Healthcare Research and Quality (AHRQ), 2012. [Google Scholar]
- 3. Stewart M, Brown JB, Donner A, et al. The impact of patient-centered care on outcomes. J Fam Pract 2000;49:796–804. [PubMed] [Google Scholar]
- 4. World Health Organisation. People-centred and integrated health services: an overview of the evidence. Geneva: World Health Organisation, 2015. [Google Scholar]
- 5. Hargreaves DS, Viner RM. Children’s and young people’s experience of the National Health Service in England: a review of national surveys 2001-2011. Arch Dis Child 2012;97:661–6. 10.1136/archdischild-2011-300603 [DOI] [PubMed] [Google Scholar]
- 6. Hargreaves DS, Greaves F, Levay C, et al. Comparison of Health Care Experience and Access Between Young and Older Adults in 11 High-Income Countries. J Adolesc Health 2015;57:413–20. 10.1016/j.jadohealth.2015.05.015 [DOI] [PubMed] [Google Scholar]
- 7. Toomey SL, Zaslavsky AM, Elliott MN, et al. The Development of a Pediatric Inpatient Experience of Care Measure: Child HCAHPS. Pediatrics 2015;136:360–9. 10.1542/peds.2015-0966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Department of Health. Improving Children and Young People’s Health Outcomes: a system wide response, 2013. [Google Scholar]
- 9. Bensted R, Hargreaves DS, Lombard J, et al. Comparison of healthcare priorities in childhood and early/late adolescence: analysis of cross-sectional data from eight countries in the Council of Europe Child-friendly Healthcare Survey, 2011. Child Care Health Dev 2015;41:160–5. 10.1111/cch.12169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ambresin AE, Bennett K, Patton GC, et al. Assessment of youth-friendly health care: a systematic review of indicators drawn from young people’s perspectives. J Adolesc Health 2013;52:670–81. 10.1016/j.jadohealth.2012.12.014 [DOI] [PubMed] [Google Scholar]
- 11. Santelli JS, Rosenfeld WD, DuRant RH, et al. Guidelines for Adolescent Health Research. Journal of Adolescent Health 1995;17:270–6. 10.1016/1054-139X(95)00181-Q [DOI] [PubMed] [Google Scholar]
- 12. Care Quality commission. Children and young people’s survey 2016. 2016. http://www.cqc.org.uk/content/children-and-young-peoples-survey-2014
- 13. Care Quality Commission. Children and young people’s inpatient and day case survey 2014, 2015. [Google Scholar]
- 14. World Health Organization. Adolescent Health Research Priorities: Report of a Technical Consultation. WHO/FWC/MCA/15/07. Geneva: World Health Organization, 2015. [Google Scholar]
- 15. Healthcare Commission. Patient survey report 2004 - young patients, 2004. [Google Scholar]
- 16. Hopwood B, Tallett A. Little voice: giving young patients a say. Nurs Times 2011;107(49-50):18–20. [PubMed] [Google Scholar]
- 17. Weil LG, Lemer C, Webb E, et al. The voices of children and young people in health: where are we now? Arch Dis Child 2015;100:915–7. 10.1136/archdischild-2014-307492 [DOI] [PubMed] [Google Scholar]
- 18. Achenbach TM, Ruffle TM. The Child Behavior Checklist and related forms for assessing behavioral/emotional problems and competencies. Pediatr Rev 2000;21:265–71. 10.1542/pir.21-8-265 [DOI] [PubMed] [Google Scholar]
- 19. Mah JK, Tough S, Fung T, et al. Adolescent quality of life and satisfaction with care. J Adolesc Health 2006;38:607.e1–607.e7. 10.1016/j.jadohealth.2005.08.004 [DOI] [PubMed] [Google Scholar]
- 20. Chesney M, Lindeke L, Johnson L, et al. Comparison of child and parent satisfaction ratings of ambulatory pediatric subspecialty care. J Pediatr Health Care 2005;19:221–9. 10.1016/j.pedhc.2005.02.003 [DOI] [PubMed] [Google Scholar]
- 21. Royal College of Paediatrics and Child Health. Service level quality improvement measures for acute general paediatrics service (SLQMAPS): RCPCH, 2016. [Google Scholar]
- 22. Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. USA: American Psychological Association, 1994:284–90. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
archdischild-2017-313801supp001.docx (28.8KB, docx)