Abstract
Objectives
Pain is a very common symptom of juvenile idiopathic arthritis (JIA). Disease activity alone cannot explain symptoms of pain in all children, suggesting other factors may be relevant. The objectives of this study were to describe the different patterns of pain experienced over time in children with JIA and to identify predictors of which children are likely to experience ongoing pain.
Methods
This study used longitudinal-data from patients (aged 1–16 years) with new-onset JIA. Baseline and up to 5-year follow-up pain data from the Childhood Arthritis Prospective Study (CAPS) were used. A two-step approach was adopted. First, pain trajectories were modelled using a discrete mixture model. Second, multinomial logistic regression was used to determine the association between variables and trajectories.
Results
Data from 851 individuals were included (4 years, median follow-up). A three-group trajectory model was identified: consistently low pain (n=453), improved pain (n=254) and consistently high pain (n=144). Children with improved pain or consistently high pain differed on average at baseline from consistently low pain. Older age at onset, poor function/disability and longer disease duration at baseline were associated with consistently high pain compared with consistently low pain. Early increases in pain and poor function/disability were also associated with consistently high pain compared with consistently low pain.
Conclusions
This study has identified routinely collected clinical factors, which may indicate those individuals with JIA at risk of poor pain outcomes earlier in disease. Identifying those at highest risk of poor pain outcomes at disease onset may enable targeted pain management strategies to be implemented early in disease thus reducing the risk of poor pain outcomes.
Keywords: pain, adolescent health, epidemiology, musculo-skeletal, rheumatology
What is already known on this topic?
Juvenile idiopathic arthritis (JIA) is the most common form of inflammatory arthritis in children and young people.
Pain is one of the most common symptoms reported by children and young people with JIA.
Pain in JIA is poorly understood and unsatisfactorily managed for children and young people.
What this study adds?
Children with JIA classify into three pain groups: consistently low pain, improved pain and consistently high pain. A clinically significant proportion of patients experience high pain that persists.
Factors at presentation including age at onset, disease duration, functional disability and pain are identified as associated with consistently high pain over time.
This study will help identify children at the highest risk of chronic pain, who should be targeted early with multidisciplinary pain management interventions.
Introduction
Inflammatory arthritis in children is a chronic and often disabling disease. With an annual incidence of approximately 33/100 000 children, juvenile idiopathic arthritis (JIA) represents the most common form of inflammatory arthritis in children.1 The disease is heterogeneous,2 its course variable with periods of activity and remission3 and can severely reduce quality of life.2 4 5 Up to a third of young people report active disease progressing into adult life.6
Pain is a commonly reported symptom in JIA7 8 and a recent study of illness perceptions in adolescents with JIA found that beliefs about their disease activity was influenced by their experience of pain.9 A study of individuals with polyarticular JIA found that pain was reported almost daily, with 31% reporting severe pain.10 Such levels of pain interfere with physical, educational, emotional and social activity, even when disease activity is controlled.11 12 Moreover, a significant number of patients continue to report pain into adulthood.13 This may explain the emerging consensus that the management of JIA needs to address more than active inflammation14 to minimise the long-term impact of the disease.
Active disease, although influential,15–17 accounts for small amounts of variance in pain in patients with JIA.15 18 Considerable variance in pain remains unaccounted for and increases as the disease progresses into adulthood.4 We know little about the different possible patterns of pain in JIA over time or which factors predict them. Previous studies were limited in their ability to provide greater understanding due to the nature and extent of the data collected, being either cross-sectional data or longitudinal data with small samples.19 20 They also focused on examining relationships between variables (variable-centred analyses). The aims of this analysis are to identify and group children with similar patterns of pain over time from baseline (person-centred analysis), and thereby predict patients with JIA at risk of poor pain outcomes.21
Method
Study population
The participants in this study were recruited to the Childhood Arthritis Prospective Study (CAPS). This longitudinal prospective inception cohort study of individuals with new-onset inflammatory arthritis, primarily JIA, was established in 2001, in the UK. Methodological details of this study have been published elsewhere.22 Patients are recruited into CAPS at first presentation to paediatric rheumatology (baseline). Written informed consent was provided by parent(s)/guardian(s) and patients (aged 16 years and older) in accordance with the Declaration of Helsinki.
Data collection
Data items used in the present analysis included the 10 cm pain visual analogue scale (VAS) (580 proxy reports and 271 child reports), active joint count (AJC) from 71 joints, 10 cm physician’s global assessment (PGA) VAS, 10 cm patient/proxy general evaluation (PGE) VAS, Child Health Assessment Questionnaire (CHAQ: functional disability) scored 0–3, Moods and Feelings Questionnaire (MFQ) scored 0–66 (self-report) and 0–68 (proxy-report) and the physician-assigned International League Against Rheumatism (ILAR) subtype. In addition, this analysis also included medication taken in the first year (eg, disease-modifying antirheumatic drugs (DMARDs), biologics and steroids). Data included in the analysis were collected at baseline (presentation), 6 months, 1 year and then annually up to 5 years. The data were extracted from hospital records and questionnaires.
Analysis
The primary outcome measure was the 10 cm pain VAS scores. Only children with a JIA subtype recorded at year 1 and pain scores recorded at baseline plus at least one additional follow-up pain score (up to 5 years postbaseline) were included in the analysis. A two-stage approach to this analysis was used.23 First, pain trajectories of patients were modelled using a form of discrete mixture-modelling called group-based trajectory analysis (GBTA).24 GBTA assigns each individual to a trajectory group, based on Bayesian posterior probabilities for group membership.21 Group-based trajectories were modelled in groups ranging from two to six trajectories. The optimal number of possible trajectories was determined by statistical fit (including Bayesian information criterion and model parsimony21) and the clinical relevance determined by the research team.
In the second step, multivariable multinomial logistic regression models were used to determine the association between possible predictors and membership in the trajectory groups.23 25 Predictors were chosen based on their salience to JIA and paediatric pain. They included baseline measures of age at onset, gender, pain, AJC, PGA, PGE, CHAQ, MFQ and disease duration (at baseline), plus early change measures of pain, AJC, PGA, PGE, CHAQ and medication. The predictors were entered into the model simultaneously. To deal with missing covariate data (table 1), multiple imputation (chained equations26) was used, with 50 datasets generated using the rule of thumb that the minimum number of imputations equated to the percentage of incomplete cases.26 Data analysis was conducted using STATA V.12.0, and user-written STATA modules Kwallis2 and TRAJ.27
Table 1.
Characteristics of the study population as a whole (n=851) and stratified by pain trajectory
| Variable | Available data, n (% missing) |
All patients | Consistently low pain, n=453 (50.2%) |
Improved pain, n=254 (31.9%) |
Consistently high pain, n=144 (17.9%) |
| Baseline | |||||
| Age, years* | 847 (0.5) | 7.6 (3.6–11.8) | 6.3 (2.9–10.9)†‡ | 8.6 (3.7–12.3)†§ | 10.8 (6.5–13.2)‡§ |
| Age at onset, years* | 843 (0.9) | 6.6 (2.7–10.8) | 5.6 (2.4–9.9)†‡ | 7.0 (3.0–11.1)†§ | 9.3 (4.5–11.8)‡§ |
| Gender n (%¶) | 851 (0.0) | ||||
| Female | 562 (66.0) | 288 (63.6)** | 184 (72.4)** | 90 (62.5)** | |
| Male | 289 (34.0) | 165 (36.4) | 70 (27.6) | 54 (37.5) | |
| Disease duration, months* | 839 (1.4) | 5.3 (2.7–10.7) | 4.7 (2.3–8.5)†‡ | 5.8 (2.8–12.8) †§ | 6.9 (3.7–17.6)‡§ |
| Disease duration from referral, weeks* | 793 (6.8) | 4 (1.3–7.7) | 4 (1.4–7.7) | 3.4 (1–7.1) | 4.6 (1.3–8.1) |
| PGA, cm* | 600 (29.5) | 3 (1.8, 5.4) | 2.6 (1.4, 4.8)†‡ | 3.5 (2, 5.7)† | 3.3 (2.1, 5.8)‡ |
| AJC* | 780 (8.3) | 2 (1–6) | 2 (1, 5)†‡ | 3 (1, 8)† | 3 (1, 8)‡ |
| PGE, cm* | 834 (2.0) | 2.1 (0.5, 5) | 0.8 (0.1, 2.4)†‡ | 4.6 (2.2, 6.2)† | 4.1 (2, 6.35)‡ |
| Pain, cm* | 851 (0.0) | 3 (0.8, 5.7) | 1 (0.2, 2.5)†‡ | 6 (4.5, 7.4)†§ | 5 (3, 6.9)‡§ |
| CHAQ* | 849 (0.2) | 0.6 (0.1–1.4) | 0.3 (0–0.9)†‡ | 1.1 (0.6–1.8)† | 1.1 (0.6–1.8)‡ |
| MFQ* | 312 (63.3) | 13 (6, 23) | 9 (4, 16) | 17 (9, 27) | 21 (13, 27) |
| Early change | |||||
| DMARDs 1st year n (%¶) | 851 (0.0) | ||||
| No | 434 (51) | 274 (60.5)** | 101 (39.8)** | 59 (41.0)** | |
| Yes | 417 (49) | 179 (39.5) | 153 (60.2) | 85 (59.0) | |
| Number of DMARDs 1st year n (%¶) | 851 (0.0) | ||||
| 1 | 381 (91.4) | 169 (94.4)** | 141 (92.2)** | 71 (83.5)** | |
| 2 | 31 (7.4) | 8 (4.5) | 10 (6.5) | 13 (15.3) | |
| 3 | 5 (1.2) | 2 (1.1) | 2 (1.3) | 1 (1.2) | |
| Biologics 1st year n (%¶) | 851 (0.0) | ||||
| No | 769 (90.4) | 430 (94.9)** | 222 (87.4)** | 117 (81.3)** | |
| Yes | 82 (9.6) | 23 (5.1) | 32 (12.6) | 27 (18.7) | |
| Number of biologics 1st year n (%¶) | 851 (0.0) | ||||
| 1 | 75 (91.5) | 22 (95.6) | 28 (87.5) | 25 (92.6) | |
| 2 | 6 (7.3) | 1 (4.4) | 3 (9.4) | 2 (7.4) | |
| 3 | 1 (1.2) | 0 (0) | 1 (3.1) | 0 (0.0) | |
| All steroids 1st year n (%¶) | 851 (0.0) | ||||
| No | 207 (24.3) | 118 (26.1) | 56 (22.1) | 33 (22.9) | |
| Yes | 644 (75.7) | 335 (73.9) | 198 (77.9) | 111 (77.1) | |
| Change in AJC 6 months, cm*†† | 541 (36.4) | −1 (−4, 0) | −1 (−3, 0) | −1 (−5, 0) | −1 (−4, 0) |
| Change in PGA 6 months, cm*†† | 390 (54.2) | −1.9 (−3.9, –0.5) | −1.9 (−4.2, –0.7) | −1.9 (−3.4, –0.3) | −1.8 (−3.9, –0.2) |
| Change in PGE 6 months, cm*†† | 500 (41.2) | −0.5 (–2.4, 0.3) | −0.3 (–0.2, 0.1) | −1.2 (–3.5, 0.6)§ | −0.1 (–2, 1.5)§ |
| Change in CHAQ 1 year*†† | 702 (17.7) | −0.1 (–0.6, 0) | −0.1 (–0.6, 0)†‡ | −0.4 (–1, 0)†§ | 0 (–0.5, 0.4)‡§ |
| Change in pain 1 year, cm*†† | 691 (18.8) | −0.7 (–3.2, 0.2) | −0.4 (–1.9, 0)†‡ | −3.2 (–5.8, –0.3)†§ | 0.5 (–1.7, 2.6)‡§ |
All values are median (IQR) unless stated.
*Multiple comparisons of significant differences between trajectory groups using an adjusted P≤0.0083 from Kruskal-Wallis tests. n, number of children.
†Improved pain versus consistently low pain.
‡Consistently high pain versus consistently low pain.
§Consistently high pain versus improved pain.
¶Column.; PGA, Physician’s global assessment PGE, Parent’s/patient’s general evaluation of wellbeingwell-being VAS, visual analogue scale; CHAQ, Childhood Health Assessment Questionnaire.
**P≤0.05 from χ2 indicates a significant difference in proportions between the three trajectory groups.
††Minus denotes a decrease in the covariate.
AJC, active joint count; CHAQ, Childhood Health Assessment Questionnaire; n, number of children; nr, not reported; ns, non-significant; PGA, Physician’s Global Assessment; PGE, parent’s/patient’s general evaluation of well-being; VAS, visual analogue scale.
Results
Study population
In total, 851 patients were included in this analysis. The median age at diagnosis was 7.6 years (IQR 3.6, 11.8), the median age at disease onset was 6.6 years (IQR 2.7, 10.8) and median disease duration at presentation was 5.3 months (IQR 2.7, 10.7) (table 1); 66% were female. The most common ILAR subtype recorded at 1 year was persistent oligoarthritis (n=265, 42.7%) (table 2). There were negligible differences in characteristics between those who were included and excluded from this analysis (see online supplementary table 1).
Table 2.
Distribution of year 1 physician-assigned ILAR subtypes stratified by pain trajectory, n=851
| Variable | All patients n (%) | Consistently low pain, n=453 (50.2%) |
Improved pain, n=254 (31.9%) |
Consistently high pain, n=144 (17.9%) |
P value |
| Subtype at 1 year | 620 | 317 (51.1) | 198 (31.9) | 105 (16.9) | 0.001* |
| Systemic | 39 (6.3) | 16 (5.1)† (41.0) | 17 (8.6)† (43.6) | 6 (5.7)† (15.4) | |
| Oligoarthritis (persistent) | 265 (42.7) | 165 (52.1)† (62.3) | 64 (32.3)† (24.2) | 36 (34.3)† (13.6) | |
| Oligoarthritis (extended) | 33 (5.3) | 11 (3.5)† (33.3) | 14 (7.1)† (42.4) | 8 (7.6)† (24.2) | |
| Polyarthritis (RF–) | 158 (25.5) | 75 (23.7)† (47.5) | 59 (29.8)† (37.3) | 24 (22.9)† (15.2) | |
| Polyarthritis (RF+) | 23 (3.7) | 4 (1.3)† (17.4) | 13 (6.6)† (56.5) | 6 (5.7)† (26.1) | |
| Enthesitis-related arthritis | 33 (5.3) | 13 (4.1)† (39.4) | 10 (5.1)† (30.3) | 10 (9.5)† (30.3) | |
| Psoriatic arthritis | 52 (8.4) | 22 (6.9)† (42.3) | 16 (8.1)† (30.8) | 14 (13.3)† (26.9) | |
| Undifferentiated | 17 (2.7) | 11 (3.5)† (64.7) | 5 (2.5)† (29.4) | 1 (1.0)† (5.9) |
All values are n (column %) unless stated.
*P≤0.05 from χ2.
† % is for row.
ILAR, International League Against Rheumatism; RF, rheumatoid factor.
archdischild-2017-313337supp001.docx (33.5KB, docx)
Trajectory model
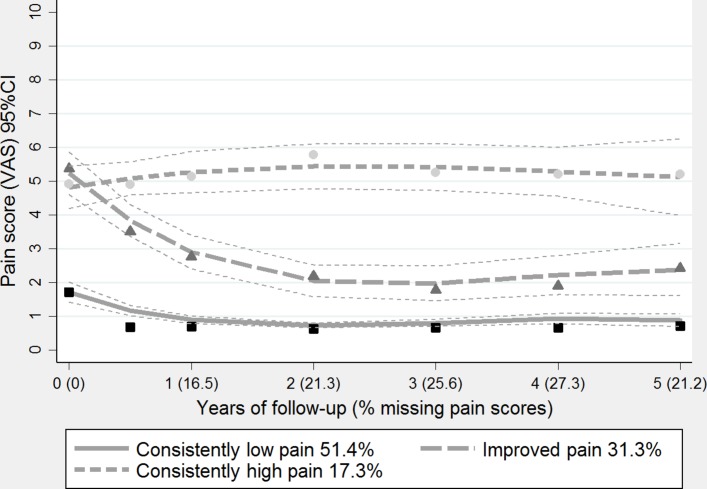
The three-group model of pain (figure 1) was selected as the most clinically and statistically satisfactory (see online supplementary table 2). Over 78% of children had a >0.7 probability of membership in their assigned trajectory groups. The averaged posterior probabilities of group membership for each of the subgroups were all high (>0.8) with the smallest trajectory group representing 17% of the study population.
Figure 1.
Pain trajectories from baseline to 5-year follow-up. VAS, visual analogue scale.
The largest group in the three-trajectory model was ‘consistently low’ pain, which accounted for half of the participants in this analysis (figure 1). This consisted of a horizontal trajectory undulating around the 1 cm point of the pain VAS (starting at 1.8 cm) throughout the 5-year period. The second group was ‘improved pain’, which accounted for almost a third of participants. This trajectory (starting at 5.5 cm) illustrated dramatic improvement in pain in the first year of follow-up, leading to a plateau for the subsequent 4 years. The third trajectory (starting at 4.9 cm) was ‘consistently high’ pain, which again was broadly horizontal, oscillating around the 5 cm point of the pain VAS throughout the 5-year follow-up.
Trajectory group characteristics
Subgroup analysis illustrated clear differences on average (median) between low persistent pain and the other pain trajectories across the majority of covariates (table 1). On average (median), older age at onset, older age at baseline, baseline pain, longer disease duration at baseline and early changes in PGE, pain and CHAQ, distinguished between trajectories with consistently high pain and improved pain (table 1).
Overall, 17% of the study cohort was in the consistently high pain group, this increased to approximately 25% for extended oligoarthritis (n=8, 24.2%), polyarthritis RF+ (n=6, 26.1%) and psoriatic arthritis (n=14, 26.9%) patients, and over 30% for children with enthesitis-related arthritis (n=10, 30.3%). While 42.7% of the study cohorts were classified with persistent oligoarthritis, this increased to over half of the children in the consistently low pain group and down to approximately one-third of the children in each of the other two groups.
Multinomial logistic regression
Variables associated with improved pain when compared with consistently low pain included being female, and longer disease duration, higher PGE and higher pain at baseline (table 3). In addition, associated early change factors included increased PGE in first 6 months, and increased CHAQ and pain in the first year (table 3). When comparing consistently high pain with consistently low pain, baseline factors of older age at onset, longer disease duration, higher PGE, higher CHAQ and higher pain were associated with consistently high pain membership, along with early change factors including treatment with biologics in the first year, increased PGE in the first 6 months and increased CHAQ and pain in the first year (table 3). Finally, when comparing consistently high pain with improved pain, the baseline factors of older age at onset and higher CHAQ were associated with consistently high pain, along with the early change factors of increased PGE in the first 6 months, and increased CHAQ and pain in the first year (table 3).
Table 3.
Association between variables and pain trajectories from a multivariable multinomial logistic regression using 50 multiple imputed datasets (n=851)
| Variable | Relative risk ratio (95% CI) | ||
| Improved versus Consistently low | Consistently high versus consistently low | Consistently high versus improved | |
| Baseline | |||
| Gender (base: female) | |||
| Male | 0.5 (0.3 to 0.9)* | 0.7 (0.4 to 1.4) | 1.5 (0.9 to 2.5) |
| Age at onset, per year | 1.1 (0.99 to 1.1) | 1.1 (1.1 to 1.2)* | 1.1 (1.0 to 1.2)* |
| PGA, per cm | 1.1 (0.9 to 1.3) | 1.1 (0.9 to 1.3) | 1.0 (0.8 to 1.2) |
| Disease duration, per month | 1.02 (1.0 to 1.04)* | 1.03 (1.0 to 1.1)* | 1.0 (0.99 to 1.0) |
| AJC, per joint | 0.9 (0.8 to 1.1) | 0.95 (0.8 to 1.1) | 1.0 (0.9 to 1.1) |
| PGE, per cm | 1.3 (1.0 to 1.5)* | 1.4 (1.1 to 1.7)* | 1.1 (0.9 to 1.3) |
| CHAQ, per 0.125 | 1.1 (0.96 to 1.1) | 1.2 (1.0 to 1.3)* | 1.1 (1.0 to 1.2)* |
| Pain, per cm | 3.2 (2.5 to 4.1)* | 3.1 (2.4 to 4.0)* | 1.0 (0.8 to 1.1) |
| MFQ, per 5% | 1.3 (0.7 to 2.5) | 1.3 (0.6 to 2.8) | 1.0 (0.6 to 1.7) |
| Early change | |||
| DMARDs in 1st year (base: no) | |||
| Yes | 1.2 (0.7 to 2.1) | 0.8 (0.4 to 1.5) | 0.6 (0.4 to 1.1)* |
| Biologics in 1st year (base: no) | |||
| Yes | 2.3 (0.8 to 6.1) | 3.0 (1.0 to 8.8)* | 1.3 (0.7 to 2.6) |
| Steroids in 1st year (base: no) | |||
| Yes | 1.0 (0.5 to 1.9) | 1.4 (0.7 to 3.1) | 1.4 (0.8 to 2.6) |
| Change in AJC in 1st 6 months, per joint increase | 0.9 (0.8 to 1.1) | 1.0 (0.8 to 1.1) | 1.0 (0.9 to 1.1) |
| Change in PGA in 1st 6 months, per cm increase | 1.2 (0.9 to 1.4) | 1.1 (0.9 to 1.4) | 1.0 (0.8 to 1.2) |
| Change in PGE in 1st 6 months, per cm increase | 1.3 (1.1 to 1.5)* | 1.4 (1.2 to 1.7)* | 1.1 (1.0 to 1.3)* |
| Change in CHAQ in 1st year, per 0.125 increase | 1.1 (1.01 to 1.2)* | 1.2 (1.1 to 1.3)* | 1.1 (1.0 to 1.1)* |
| Change pain in 1st year, per cm increase | 1.4 (1.2 to 1.7)* | 1.7 (1.4 to 2.1)* | 1.2 (1.1 to 1.3)* |
*P≤0.05.
CHAQ, Childhood Health Assessment Questionnaire; DMARDs, disease-modifying antirheumatic drugs; MFQ, Moods and Feelings Questionnaire; PGA, Physician’s Global Assessment; PGE, parent’s/patient’s general evaluation.
Discussion
Using GBTA, relatively novel in paediatric research, three distinct trajectories of pain in children and young people with JIA have been identified. Although a majority of children report low pain or pain which improves quickly during the first year following diagnosis, almost a fifth of children reported consistently high levels of pain over time. Pain at presentation is by far the strongest, but not only predictor of consistently high pain, consistent with previous research.20 28 Neither AJC nor PGA at presentation, nor early changes in AJC or PGA, were found to predict membership in either of the three trajectory groups. Consequently, a management approach focused primarily on disease activity may not necessarily lead to improvements in long-term pain. Children with consistently high pain were more likely to have been prescribed DMARDs and biologics compared with those in the other pain trajectories within the first 5 year of follow-up (see online supplementary table 3). This is consistent with findings reported by others that a significant proportion of patients with JIA treated with biologics including anti-TNF treatments still experienced pain12 29 with 19% of patients reporting severe pain.30 Similarly, this study found that being treated with biologics within the first year almost trebled a child’s likelihood of consistently high pain membership. Clinicians must address disease activity in their treatment decisions but must also address factors such as pain when considering the best management approach for JIA.31
A notable finding was that baseline measures of disease activity such as the AJC and PGA, did not predict children’s membership in any pain trajectory group. In contrast, baseline evaluations of patients or proxy (CHAQ, PGE and pain) scores did inform membership in the pain trajectories, as did early changes in those measures. Baseline functional disability (CHAQ) was a strong predictor of membership of the consistently high pain trajectory. Packham and Hall in their cross-sectional study found that functional disability contributed 18% of total variance explained in pain.4 Interestingly, an analysis of the CAPS cohort after a 1-year prospective follow-up found baseline pain to be a predictor of moderate-to-severe functional disability.32 These findings demonstrate the complex relationships between pain and functional disability, with experiences of one likely to contribute to the self-report of the other.
Age at onset also appears to have a relationship with trajectory group membership. Patients with consistently low pain were younger on average, those with improved pain were more commonly in the middle childhood age group at onset and those with consistently high pain were, on average, approaching early adolescence.14 Malleson et al 16 and Weiss et al found that older age was predictive of pain in patients with JIA.14 Patients who are older at onset may find it more difficult to adjust with the changes to their functioning than younger children33 and perceive the long-term consequences of JIA as more significant.34 Moreover, they may have to relearn and adjust to new ways of doing things rather than learning to do things for the first time as younger-onset children.35 Additionally, the psychological, social and emotional pressures experienced by those whose disease starts in adolescence such as conforming to peer-group expectations, increasing independence and burgeoning identity may magnify their experience of pain and functional disability when compared with those whose disease starts when they are younger.35
Disease duration at baseline was also associated with consistently high pain. One explanation for this may be due to the greater potential damage caused by JIA prior to its remission in consistently high pain owing to potential delays in appropriate treatment22 (with 21% of patients in this study waiting ≥1 year prior to presentation). Fantini et al found attaining remission decreases in proportion to delay in presenting to paediatric rheumatology.3 Oen et al found that time between onset and diagnosis was a prospective predictor of functional disability at follow-up.5 Parent’s unfamiliarity with the urgency of symptoms may delay seeking medical advice22; complicated by variables such as socioeconomic status.36 Therefore, their disease may go untreated for longer allowing functional disability to increase,22 potentially demonstrating why poor functional disability predicted consistently high pain. This may also lead to a greater probability of enhanced sensitivity to all pain-inducing stimuli beyond that induced by affected joints.7 This amplification in pain may persist beyond the resolution of inflammation leading to peripheral and central sensitisation,7 and lowered pain thresholds, pain tolerances37 and high chronic pain, as found in those in consistently high pain.
Contrary to previous research, depression was not found to predict any pain trajectory.28 38 In this study, depression was correlated positively with pain (see online supplementary table 4). An explanation for the findings may be that PGE, which is a measure of well-being, occupies similar variance associated with depression, thereby reducing its uniquely associated contribution. Higher PGE scores were found to predict consistently high pain. Patients and/or their parents more readily view pain as an indicator of arthritis9 39 than do clinicians. Therefore, PGE scores would provide a more accurate indicator of pain experiences over time than PGA, as it takes into account pain experience.
The findings from this study have a number of implications for pain management in children presenting for the first time to paediatric rheumatology. Alongside objective markers of disease activity, this study suggests that clinicians should ensure that pain is also addressed, particularly among those presenting with higher levels of pain and PGE, poor functional ability, older onset and/or longer disease duration. Importantly, early increases in PGE, poor functional ability and pain are also independently associated with consistently high pain, indicating that delays in pain management may only serve to increase the risk of a child developing consistently high pain. Hence, pain management should be prioritised early in children with JIA. Furthermore, medications such as DMARDs, biologics and steroids, which are used to reduce disease activity, may be less efficacious in reducing pain in some patients. Therefore, an integrated management approach in which pain is assessed and managed alongside disease activity is needed to reduce the prospect of poor long-term pain outcomes.
Limitations
These findings must be viewed in the context of some limitations. The pain, PGE, CHAQ and MFQ score was reported by a parent for children under the age of 11 and were self-reported by children aged ≥11 years. The potential limitations of such strategies of data collection have been identified previously.40 However, this strategy reflects the routine collection of data in the UK paediatric rheumatology. Therefore, the baseline covariates in this study correspond with data that were available to paediatric rheumatologists. Furthermore, information on pain management was not examined, which may highlight that if interventions were used they were not adequate in reducing pain in at least a fifth of the cohort.
Conclusion
This study has used clinical data which are routinely collected from patients with JIA to classify pain trajectories into three categories. Factors which contributed to pain patterns included disease features (eg, duration, age at onset, etc), which would enable children with JIA at an increased risk of consistently high pain over time to be identified early in disease. It is important for children with JIA that integrated pain management strategies are used in addition to pharmacological therapy aimed to control inflammation, and targeted at those most at risk, as soon as possible after diagnosis to improve important long-term pain outcomes.
Acknowledgments
The authors would also like to thank all local research coordinators and principal investigators who have made this research possible as well as members of the research team at University of Manchester. The members who contributed were as follows: Alder Hey Children’s Hospital: E Baildam, C Lydon; Great Ormond Street Hospital: L Wedderburn, C Johnson; Royal Hospital for Sick Children (NHS Lothian): J Davidson, J Baggott; Royal Hospital for Children (Glasgow): J Davidson, R Boyle; Royal Manchester Children’s Hospital: A Chieng, A McGovern, A Duggan; Royal Victoria Hospital (Newcastle): F McErlane, K Devine, S Crulley; University College London Hospital: Y Ioannou, L Suffield and the research team at the University of Manchester: W Thomson, KL Hyrich, R Carrasco, P Gilbert, A Smith. The authors would also like to thank Dr Bo Fu for his statistical advice. In the end, the authors would like to thank all of the patients and their families who contributed to the Childhood Arthritis Prospective Study.
Footnotes
Contributors: AR, RC, LC, SMMV, KLH and WT were responsible for data cleaning and data analysis. HEF, EB, AC, JED, LRW, YI and FM were responsible for data collection and contribution to the final analysis.
Funding: The ‘Childhood Arthritis Prospective Study (CAPS)’ is supported by the Arthritis Research UK Special Strategic (grant number 20542); Arthritis Research UK Centre for Epidemiology (grant number 20380 to AR, LC, RC, SMMV, KLH and WT); National Institute for Health Research Manchester Musculoskeletal Biomedical Research Unit to AR, SMMV, KLH and WT; Arthritis Research UK Centre for Genetics and Genomics (grant number 20385 to WT); National Institute for Health Research University College London Hospitals Biomedical Research Centre to YI and LRW and Arthritis Research UK (grant number 20164 to YI and LRW). LW is supported by Arthritis Research UK Grant 20164, and the NIHR Great Ormond Street Hospital Biomedical Research Centre. This work is also supported by the National Institute for Health Research Biomedical Research Centre Funding Scheme and is adopted into the NIHR Clinical Research Network Portfolio (CRN Study ID: 2635).
Competing interests: KLH has received honoraria from Pfizer and AbbVie for work unrelated to the present article.
Ethics approval: The study was approved by the North West Multicentre Research Ethics Committee and all participants gave written informed consent.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Thierry S, Fautrel B, Lemelle I, et al. . Prevalence and incidence of juvenile idiopathic arthritis: a systematic review. Joint Bone Spine 2014;81:112–7. 10.1016/j.jbspin.2013.09.003 [DOI] [PubMed] [Google Scholar]
- 2. Armon K. Outcomes for juvenile idiopathic arthritis. Paediatr Child Health 2014;24:64–71. 10.1016/j.paed.2013.07.008 [DOI] [Google Scholar]
- 3. Fantini F, Gerloni V, Gattinara M, et al. . Remission in juvenile chronic arthritis: a cohort study of 683 consecutive cases with a mean 10 year followup. J Rheumatol 2003;30:579–84. [PubMed] [Google Scholar]
- 4. Packham JC, Hall MA. Long-term follow-up of 246 adults with juvenile idiopathic arthritis: education and employment. Rheumatology 2002;41:1436–9. 10.1093/rheumatology/41.12.1436 [DOI] [PubMed] [Google Scholar]
- 5. Oen K, Tucker L, Huber AM, et al. . Predictors of early inactive disease in a juvenile idiopathic arthritis cohort: results of a Canadian multicenter, prospective inception cohort study. Arthritis Rheum 2009;61:1077–86. 10.1002/art.24539 [DOI] [PubMed] [Google Scholar]
- 6. Duffy CM. Health outcomes in pediatric rheumatic diseases. Curr Opin Rheumatol 2004;16:102–8. 10.1097/00002281-200403000-00005 [DOI] [PubMed] [Google Scholar]
- 7. La Hausse de Lalouvière L, Ioannou Y, Fitzgerald M. Neural mechanisms underlying the pain of juvenile idiopathic arthritis. Nat Rev Rheumatol 2014;10:1–7. 10.1038/nrrheum.2014.4 [DOI] [PubMed] [Google Scholar]
- 8. Oen K, Reed M, Malleson PN, et al. . Radiologic outcome and its relationship to functional disability in juvenile rheumatoid arthritis. J Rheumatol 2003;30:832–40. [PubMed] [Google Scholar]
- 9. Ghio D, Thomson W, Calam R, et al. . Development and preliminary validation of the pain perceptions questionnaire for young people with juvenile arthritis, 2016. [Google Scholar]
- 10. Schanberg LE, Anthony KK, Gil KM, et al. . Daily pain and symptoms in children with polyarticular arthritis. Arthritis Rheum 2003;48:1390–7. 10.1002/art.10986 [DOI] [PubMed] [Google Scholar]
- 11. Consolaro A, Ravelli A. Paediatric rheumatology: Juvenile idiopathic arthritis–are biologic agents effective for pain? Nat Rev Rheumatol 2013;9:447–8. 10.1038/nrrheum.2013.108 [DOI] [PubMed] [Google Scholar]
- 12. Lomholt JJ, Thastum M, Herlin T. Pain experience in children with juvenile idiopathic arthritis treated with anti-TNF agents compared to non-biologic standard treatment. Pediatr Rheumatol Online J 2013;11:21 10.1186/1546-0096-11-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Selvaag AM, Aulie HA, Lilleby V, et al. . Disease progression into adulthood and predictors of long-term active disease in juvenile idiopathic arthritis. Ann Rheum Dis 2016;75:190–5. 10.1136/annrheumdis-2014-206034 [DOI] [PubMed] [Google Scholar]
- 14. Weiss PF, Beukelman T, Schanberg LE, et al. . Enthesitis-related arthritis is associated with higher pain intensity and poorer health status in comparison with other categories of juvenile idiopathic arthritis: the childhood arthritis and rheumatology research alliance registry. J Rheumatol 2012;39:2341–51. 10.3899/jrheum.120642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ilowite NT, Walco GA, Pochaczevsky R. Assessment of pain in patients with juvenile rheumatoid arthritis: relation between pain intensity and degree of joint inflammation. Ann Rheum Dis 1992;51:343–6. 10.1136/ard.51.3.343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Malleson PN, Oen K, Cabral DA, et al. . Predictors of pain in children with established juvenile rheumatoid arthritis. Arthritis Rheum 2004;51:222–7. 10.1002/art.20238 [DOI] [PubMed] [Google Scholar]
- 17. Varni JW, Thompson KL, Hanson V. The varni/thompson pediatric pain questionnaire. I. chronic musculoskeletal pain in juvenile rheumatoid arthritis. Pain 1987;28:27–38. 10.1016/0304-3959(87)91056-6 [DOI] [PubMed] [Google Scholar]
- 18. Schanberg LE, Lefebvre JC, Keefe FJ, et al. . Pain coping and the pain experience in children with juvenile chronic arthritis. Pain 1997;73:181–9. 10.1016/S0304-3959(97)00110-3 [DOI] [PubMed] [Google Scholar]
- 19. Bromberg MH, Gil KM, Schanberg LE. Daily sleep quality and mood as predictors of pain in children with juvenile polyarticular arthritis. Health Psychol 2012;31:202–9. 10.1037/a0025075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Thastum M, Herlin T. Pain-specific beliefs and pain experience in children with juvenile idiopathic arthritis: a longitudinal study. J Rheumatol 2011;38:155–60. 10.3899/jrheum.091375 [DOI] [PubMed] [Google Scholar]
- 21. Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol 2010;6:109–38. 10.1146/annurev.clinpsy.121208.131413 [DOI] [PubMed] [Google Scholar]
- 22. Adib N, Hyrich K, Thornton J, et al. . Association between duration of symptoms and severity of disease at first presentation to paediatric rheumatology: results from the Childhood Arthritis Prospective Study. Rheumatology 2008;47:991–5. 10.1093/rheumatology/ken085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lewis KN, Heckman BD, Himawan L. Multinomial logistic regression analysis for differentiating 3 treatment outcome trajectory groups for headache-associated disability. Pain 2011;152:1718–26. 10.1016/j.pain.2011.02.001 [DOI] [PubMed] [Google Scholar]
- 24. Nagin DS, Tremblay RE. Developmental trajectory groups: fact or a useful statistical fiction?. Criminology 2005;43:873–904. 10.1111/j.1745-9125.2005.00026.x [DOI] [Google Scholar]
- 25. Nagin DS. Group-based trajectory modeling an overview In: Piquero AR, Weisburd D, eds Handbook of quantitative criminology. New York, 2010:53–67. doi. [Google Scholar]
- 26. White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med 2011;30:377–99. 10.1002/sim.4067 [DOI] [PubMed] [Google Scholar]
- 27. Jones BL, Nagin DS. A Note on a Stata Plugin for Estimating Group-based Trajectory Models. Sociol Methods Res 2013;42:608–13. 10.1177/0049124113503141 [DOI] [Google Scholar]
- 28. Packham JC, Hall MA, Pimm TJ. Long-term follow-up of 246 adults with juvenile idiopathic arthritis: predictive factors for mood and pain. Rheumatology 2002;41:1444–9. 10.1093/rheumatology/41.12.1444 [DOI] [PubMed] [Google Scholar]
- 29. Bromberg MH, Connelly M, Anthony KK, et al. . Self-reported pain and disease symptoms persist in juvenile idiopathic arthritis despite treatment advances: an electronic diary study. Arthritis Rheumatol 2014;66:462–9. 10.1002/art.38223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Boiu S, Marniga E, Bader-Meunier B, et al. . Functional status in severe juvenile idiopathic arthritis in the biologic treatment era: an assessment in a French paediatric rheumatology referral centre. Rheumatology 2012;51:1285–92. 10.1093/rheumatology/kes004 [DOI] [PubMed] [Google Scholar]
- 31. Guzman J, Gómez-Ramírez O, Jurencak R, et al. . What matters most for patients, parents, and clinicians in the course of juvenile idiopathic arthritis? A qualitative study. J Rheumatol 2014;41:2260–9. 10.3899/jrheum.131536 [DOI] [PubMed] [Google Scholar]
- 32. Hyrich KL, Lal SD, Foster HE, et al. . Disease activity and disability in children with juvenile idiopathic arthritis one year following presentation to paediatric rheumatology. Results from the Childhood Arthritis Prospective Study. Rheumatology 2010;49:116–22. 10.1093/rheumatology/kep352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. April KT, Cavallo S, Feldman DE. Children with juvenile idiopathic arthritis: are health outcomes better for those diagnosed younger? Child Care Health Dev 2013;39:442–8. 10.1111/j.1365-2214.2012.01386.x [DOI] [PubMed] [Google Scholar]
- 34. Beales JG, Keen JH, Holt PJ. The child’s perception of the disease and the experience of pain in juvenile chronic arthritis. J Rheumatol 1983;10:61–5. [PubMed] [Google Scholar]
- 35. Jacobson CJ, Farrell JE, Kashikar-Zuck S, et al. . Disclosure and self-report of emotional, social, and physical health in children and adolescents with chronic pain–a qualitative study of PROMIS pediatric measures. J Pediatr Psychol 2013;38:82–93. 10.1093/jpepsy/jss099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Verstappen SMM, Cobb J, Foster HE, et al. . The association between low socio-economic status with high physical limitations and low illness self-perception in patients with juvenile idiopathic arthritis: Results from the childhood arthritis prospective study. Arthritis Care Res 2015;67:382–9. 10.1002/acr.22466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cornelissen L, Donado C, Kim J, et al. . Pain hypersensitivity in juvenile idiopathic arthritis: a quantitative sensory testing study. Pediatr Rheumatol Online J 2014;12:39 10.1186/1546-0096-12-39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Connelly M, Bromberg MH, Anthony KK, et al. . Emotion regulation predicts pain and functioning in children with juvenile idiopathic arthritis: an electronic diary study. J Pediatr Psychol 2012;37:43–52. 10.1093/jpepsy/jsr088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Armbrust W, Kaak JG, Bouma J, et al. . Assessment of disease activity by patients with juvenile idiopathic arthritis and the parents compared to the assessment by pediatric rheumatologists. Pediatr Rheumatol Online J 2013;11:48 10.1186/1546-0096-11-48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lal SD, McDonagh J, Baildam E, et al. . Agreement between proxy and adolescent assessment of disability, pain, and well-being in juvenile idiopathic arthritis. J Pediatr 2011;158:307–12. 10.1016/j.jpeds.2010.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
archdischild-2017-313337supp001.docx (33.5KB, docx)