Abstract
Purpose
To determine the rate of visual recovery following hyphema caused by traumatic blunt force injury in children.
Methods
The medical records of patients evaluated between July 2008 and July 2014 were reviewed retrospectively. Primary outcome measures included presenting and follow-up visual acuities.
Results
At total of 56 eyes of 55 children (<18 years of age) were diagnosed with hyphema following blunt force nonpenetrating injury. The average patient age was 10.3 ± 3.2 years. The majority of subjects were male (78%). Presenting visual acuities ranged from logMAR 0.0 (Snellen equivalent, 20/20) to light perception. Rebleeding occurred in 4 subjects (7.1%). Visual acuity demonstrated improvement over the first 28 days following injury, with 59% achieving visual acuity of logMAR 0.0 (Snellen equivalent, 20/20) and 82% recovering vision to logMAR 0.2 (Snellen equivalent 20/30) by day 28. All but 1 patient (43 of 44 eyes, 98%) had a best-corrected visual acuity of better than or equal to logMAR 0.2 at their last recorded follow-up.
Conclusions
There is good potential for visual recovery following uncomplicated traumatic hyphema in children. In our patient cohort, the majority of patients had significant improvement in visual acuity within the first 28 days; in some children visual acuity continued to improve beyond the first month.
Keywords: hyphema, traumatic hyphema, visual acuity, blunt ocular trauma, pediatric, complications, and follow-up
Trauma is a relatively common mechanism for the development of hyphema in children, with an estimated incidence of 17–20/100,000 cases of traumatic hyphema per year.1–3 Traumatic hyphemas are the result of the disruption of anterior ciliary body and iris vessels. Numerous complications are associated with traumatic hyphemas, including corneal bloodstaining, elevated intraocular pressure (IOP), and rebleeds.1–5 Perhaps secondary to participation in at-risk activities or due to the anatomic response of the eye to blunt injury, children are at higher risk than adults for sustaining traumatic hyphema.1,4 One report proposes that children younger than 6 years of age may be particularly susceptible to secondary hemorrhage,6 suggesting that the pediatric population may be at higher risk for long-term complications.
The initial decrease in visual acuity after the inciting injury can be worrisome for both patients and their families and results in frequent questions about visual potential and rate of recovery. Visual recovery after traumatic hyphema is multifactorial, varying with age, size of presenting hyphema, and the presence or development of complications including rebleeding, elevated IOP, and concomitant injury to adjacent structures.1,6–8 Prior studies have evaluated final visual acuity after treatment, with reports ranging from 71% to 88% of patients achieving a visual acuity of better than logMAR 0.3 (Snellen 20/30) in the outpatient setting,8 and 91% in the inpatient setting.1,5 Numerous studies have analyzed risk factors, complications, and final visual acuity in pediatric traumatic hyphema patients; however, to our knowledge, this is the first study to address the rate of visual recovery in this population. This study aimed to better define the typical visual recovery course in children suffering hyphema after blunt trauma injury.
Subjects and Methods
The medical records of all patients seen at Casey Eye Institute between July 1, 2008, and July 30, 2014 were reviewed retrospectively. The Oregon Health & Science University Institutional Review Board approved this study, which followed the tenets set forth by the Declaration of Helsinki and was fully compliant with the US Health Insurance Portability and Accountability Act of 1996. Medical records were searched performed using ICD-9 codes 364.41 (“hyphema of the iris and ciliary body”) and 921.3 (“contusion of eyeball”), and 921.9 (“eye trauma”). Subjects were included if they met the following criteria: blunt force mechanism of trauma, diagnosis of traumatic hyphema, evaluation by a Casey Eye Institute pediatric ophthalmologist, ability to complete Snellen visual acuity testing, and age <18 years at time of initial evaluation. To be included in the visual acuity recovery analysis, patients had to have a follow-up examination at least 1 week after initial injury. Patients with concurrent penetrating ocular injury, patients who sustained additional injuries precluding their participation in the ocular examination, and patients who presented more than 24 hours after the injury were excluded.
All participants initially underwent a complete ophthalmic examination, including dilated fundus examination. The initial examination was performed by either a comprehensive ophthalmologist on call (typically a resident physician with staffing) or by a pediatric ophthalmologist. All patients had follow-up by a pediatric ophthalmologist. All examinations included Snellen visual acuity testing, IOP measurement, and anterior segment examination. Dilated fundus examination and ancillary testing was left to the discretion of the treating ophthalmologist.
The primary outcome measure for this study was the visual acuity of subjects treated for traumatic hyphema, including the rate of visual recovery along the treatment course. Secondary outcomes included the mechanism of injury, treatment methods (including choice of medications), complications, and the effect of any comorbidities on final visual acuity.
Baseline and follow-up characteristics were summarized with frequencies and percentages for all categorical variables. Snellen best-corrected visual acuities were converted to logarithm of the minimum angle of resolution (logMAR) values for analysis. Visual acuity of counting fingers was converted to a logMAR value of 2.0; hand motion, to logMAR of 3.0; and light perception to logMAR of 4.0. The proportion of patients recovering vision to logMAR 0, logMAR 0.2 and logMAR 0.3 during the initial 28 days following injury was calculated. Data compilation and statistical analysis were performed using Microsoft Excel software version 14.5.8 (Redmond, WA).
Results
A total of 56 eyes of 55 patients with traumatic hyphema met inclusion criteria on record review. Of these, the majority (78%) were male, and the average age of injury was 10.4 ± 3.2 years (range, 3.7–17.5 years). Parent-reported race was mostly white (86%); 2 patients identified as black (3.6%), 1 as Asian (1.8%), and 4 (7.3%) as multiracial. Of those who identified as white, 78% were non-Hispanic and 20% were Hispanic. One patient (1.8%) did not specify. The majority of patients (84%) had no prior ocular history. Seven (13%) had known refractive error, 2 (3.6%) had strabismus, and 1 (1.8%) had congenital glaucoma. Patient demographics are provided in Table 1.
Table 1.
Demographics and characteristics of patients with traumatic hyphema (N = 55)
| Number (%) | |
|---|---|
| Sex | |
| Male | 43 (78) |
| Female | 12 (22) |
| Race | |
| White | 47 (86) |
| Multiracial | 4 (7.3) |
| Black | 2 (3.6) |
| Asian | 1 (1.8) |
| Unknown | 1 (1.8) |
| Ethnicity | |
| Non-Hispanic | 47 (78) |
| Hispanic | 11 (20) |
| Other | 1 (1.8) |
| Past ocular history | |
| None | 46 (84) |
| Refractive error | 7 (13) |
| Strabismus | 2 (3.6) |
| Congenital glaucoma | 1 (1.8) |
| Total | 55 (100) |
The most common injury was sports related, followed by injuries from small projectiles sand elastic bands (Table 2). Corneal abrasion (38%) and commotio retinae (29%) were common presenting comorbidities at the time of hyphema diagnosis (Table 3). Hyphema treatment typically consisted of topical cycloplegia (98%) and prednisolone (77%), with only 3 patients (5.4%) requiring IOP-lowering treatment at initial presentation. No patients were treated with antifibrolytic therapy. One patient was hospitalized for observation due to loss of consciousness at the time of injury; otherwise, hyphema management was completed in the outpatient setting.
Table 2.
Mechanism of traumatic hyphema
| Mechanism of injury | Number (%) |
|---|---|
| Sports related (ball, hockey stick, jump rope) | 19 (35) |
| Small projectile (BB, airsoft pellet, paintball) | 10 (18) |
| Bungee cord/rubber band | 6 (11) |
| Stick/handle | 5 (9.1) |
| Rock | 3 (5.5) |
| Firework/bottle rocket | 3 (5.5) |
| Bottle cap | 2 (3.6) |
| Airbag | 1 (1.8) |
| Kick | 1 (1.8) |
| Other (hairbrush, apple, pencil, toy) | 5 (9.1) |
| Total | 55 (100) |
Table 3.
Ocular comorbidities associated with traumatic hyphemas at presentation and follow-up
| Complications (N = 56) | Number (%) |
|---|---|
| Corneal abrasion | 21 (38) |
| Commotio retinae | 16 (29) |
| Rebleed | 4 (7.1) |
| Anterior chamber washout | 1 (1.8) |
| Ocular hypertension requiring medication | 12 (21) |
| Traumatic cataract | 4 (7.1) |
| Retinal tear | 2 (3.6) |
| Scleral buckle | 1 (1.8) |
Five eyes developed rebleeds, which occurred 1–9 days after injury. Ten eyes had elevated IOP requiring treatment in addition to the 3 patients with elevated IOP at presentation. The average time to starting treatment was 6.6 days (range, 2–14 days). All patients were managed with topical medical therapy, and 4 patients received oral acetazolamide. IOP-lowering treatment could be discontinued in all cases. No patients required emergent glaucoma surgery; 1 patient who was lost to follow-up and had a rebleed of unknown duration eventually returned for care 3.5 years after his injury and required a trabeculectomy. One patient underwent anterior chamber washout after developing a complete hyphema with associated IOP elevation. In the first 14 days, the risk of rebleed was 7.1%; of IOP elevation requiring treatment, 23%.
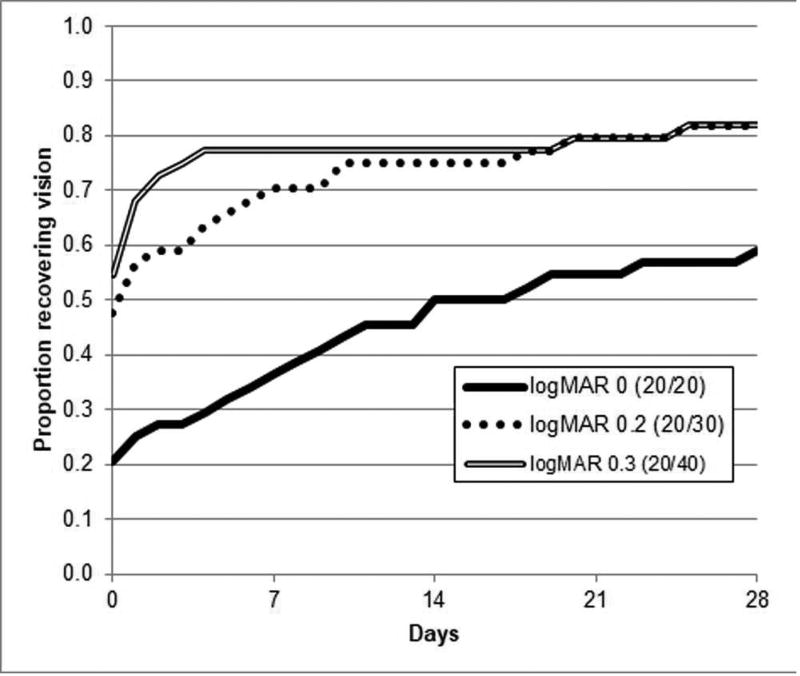
Data for 44 eyes of 43 patients was available for visual acuity recovery analysis. The average presenting best-corrected visual acuity was logMAR 0.91 (Snellen equivalent, 20/163), and 51% had a visual acuity of logMAR 0.2 or better (Snellen equivalent, 20/30; Figure 1). Visual acuity improved over the initial 28 days following injury, with half of the patients measuring logMAR 0 (Snellen equivalent, 20/20) acuity by 14 days and 59% achieving this acuity by 28 days (Figure 1); 82% showed visual acuity of logMAR 0.2 (Snellen equivalent, 20/30) by day 28; and 16% (7 children) had additional follow-up and improved visual acuity beyond the first month, and each ultimately achieving visual acuity of logMAR 0.2. The average final visual acuity was logMAR 0.14 (Snellen equivalent, 20/27). All but 1 patient (43 of 44 eyes [98%]) had a best-corrected visual acuity of logMAR 0.2 (Snellen equivalent, 20/30) or better at their last recorded follow-up. The 1 patient who did not improve had visual acuity of light perception and had very limited follow-up; this patient’s course was complicated by a rebleed of unknown duration prior to reestablishing care and subsequent development of glaucoma that required surgical intervention (trabeculectomy complicated by a choroidal hemorrhage and retinal detachment) 3.5 years later.
FIG 1.
Kaplan-Meir survival curve showing the proportion of patients achieving logMAR 0.0 (Snellen equivalent, 20/20), 0.2 (Snellen equivalent, 20/30), and 0.3 (Snellen equivalent 20/40) over the course of 28 days.
Discussion
Hyphemas are common in the pediatric population. Over the past decades, management has shifted from an inpatient to an outpatient basis without significant increase in rebleeds or other complications.8,9 In addition to activity restriction, many providers prescribe cycloplegics and topical steroids with frequent follow-up. There are several retrospective reports on the complication rate, rebleed rate, and final visual acuity.7,8,10 Coats and colleagues9 demonstrated that the majority of children (88%) end up with 20/40 vision or better. However, the rate of visual recovery can vary greatly among individuals.8 The uncertainty of visual recovery rate leads to anxiety by both parents and patients, especially while under activity restrictions.
To our knowledge, this study is the first to analyze visual acuity recovery with time. The mean final visual acuity is logMAR 0.14 (Snellen equivalent 20/27). The majority of visual acuity recovery occurs within the first 14 days, but some subjects are slower to recover; 16% continued to have gradual visual recovery beyond 1 month.
There are several recognized weaknesses of the study. First, this study represents a small population, one typical of the predominantly white population in Oregon. As a retrospective review, there is significantly varied follow-up, including duration and frequency. One patient in particular who missed numerous appointments and had limited follow-up ended up with visual acuity of light perception after a rebleed of unknown duration. Another study weakness lies in the initial examination; like many institutions, call is shared by numerous providers and is limited in the available equipment. Often, bedside visual acuities were measured using near cards, which may overestimate presenting visual acuity. To minimize this, patients were only included in the study if they had prompt follow-up with an outpatient pediatric ophthalmologist specialist. Lastly, our study restricts evaluation to a pediatric population. Results may significantly differ in older patients or one with degenerative concomitant disease.
Table 4.
Management of traumatic hyphemas
| Initial treatment | Number (%) |
|---|---|
| Cycloplegia | 55 (98) |
| Steroid | 43 (77) |
| Antifibrolytic | 0 (0) |
| IOP-lowering medication | 3 (5.4) |
| Hospital admission Sickle cell testing | 1 (1.8) |
| Known history | 0 (0) |
| Tested | 5 (9.1) |
| Positive test | 1 (1.8) |
Acknowledgments
Funding support: Unrestricted grant from Research to Prevent Blindness; NIH/NEI Core Grant (P30EY010572); The Heed Ophthalmic Foundation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presented at the Annual Meeting of the Association for Research in Vision and Ophthalmology, Orlando, Florida, May 4–8, 2014.
References
- 1.Agapitos PJ, Noel LP, Clarke WN. Traumatic hyphema in children. Ophthalmology. 1987;94:1238–41. doi: 10.1016/s0161-6420(87)80006-4. [DOI] [PubMed] [Google Scholar]
- 2.Walton W, Von Hagen S, Grigorian R, Zarbin M. Management of traumatic hyphema. Surv Ophthalmol. 2002;47:297–334. doi: 10.1016/s0039-6257(02)00317-x. [DOI] [PubMed] [Google Scholar]
- 3.Kennedy RH, Brubaker RF. Traumatic hyphema in a defined population. Am J Ophthalmol. 1988;106:123–30. doi: 10.1016/0002-9394(88)90822-7. [DOI] [PubMed] [Google Scholar]
- 4.Spoor TC, Kwitko GM, O’Grady JM, Ramocki JM. Traumatic hyphema in an urban population. Am J Ophthalmol. 1990;109:23–7. doi: 10.1016/s0002-9394(14)75573-4. [DOI] [PubMed] [Google Scholar]
- 5.Recchia FM, Saluja RK, Hammel K, Jeffers JB. Outpatient management of traumatic microhyphema. Ophthalmology. 2002;109:1465–70. doi: 10.1016/s0161-6420(02)01091-6. [DOI] [PubMed] [Google Scholar]
- 6.Crouch ER, Jr, Crouch ER. Management of traumatic hyphema: therapeutic options. J Pediatr Ophthalmol Strabismus. 1999;36:238–50. doi: 10.3928/0191-3913-19990901-04. [DOI] [PubMed] [Google Scholar]
- 7.Cho J, Jun BK, Lee YJ, Uhm KB. Factors associated with the poor final visual outcome after traumatic hyphema. Korean J Ophthalmol. 1998;12:122–9. doi: 10.3341/kjo.1998.12.2.122. [DOI] [PubMed] [Google Scholar]
- 8.Rocha KM, Martins EN, Melo LA, Jr, Moraes NS. Outpatient management of traumatic hyphema in children: prospective evaluation. J AAPOS. 2004;8:357–61. doi: 10.1016/j.jaapos.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 9.Coats DK, Viestenz A, Paysse EA, Plager DA. Outpatient management of traumatic hyphemas in children. Binocul Vis Strabismus Q. 2000;15:169–74. [PubMed] [Google Scholar]
- 10.SooHoo JR, Davies BW, Braverman RS, Enzenauer RW, McCourt EA. Pediatric traumatic hyphema: a review of 138 consecutive cases. J AAPOS. 2013;17:565–7. doi: 10.1016/j.jaapos.2013.07.007. [DOI] [PubMed] [Google Scholar]