Abstract
Cardiovascular diseases are still the primary cause of mortality worldwide, with high blood pressure and type 2 diabetes as major promoters. Over the past 3 decades, almost in parallel with the rise in cardiovascular disease incidence, the consumption of sugar-sweetened beverages (SSBs) has increased. In this context, SSBs are potential contributors to weight gain and increase the risk for elevations in blood pressure, type 2 diabetes, coronary heart disease, and stroke. Nevertheless, the mechanisms underlying the cardiovascular and metabolic responses to SSBs, in particular on blood pressure, are poorly understood. We discuss and propose potential mechanisms underlying differential effects of sugars on postprandial blood pressure regulation; provide evidence for additional molecular contributors, i.e., fibroblast growth factor 21, towards sugar-induced cardiovascular responses; and discuss potential cardiovascular neutral sugars. Furthermore, we explore whether pre-existing glucose intolerance in humans exacerbates the cardiovascular responses to SSBs, thus potentially aggravating the cardiovascular risk in already-susceptible individuals.
Keywords: cardiovascular disease, blood pressure, glucose intolerance, fructose, fibroblast growth factor 21
Introduction
Cardiovascular diseases (CVDs) are the number-one cause of mortality worldwide (1). A number of fundamental health issues (high blood pressure, cholesterol, and glucose levels) and health behaviors (overweight and obesity, smoking, physical inactivity, and poor diet) contribute to increased CVD risk (2). Although obesity is a potentially modifiable risk factor, the cause of obesity is multifactorial, and it is now well recognized that dietary excess, particularly in combination with a sedentary lifestyle, contributes significantly towards its development (3).
Over the past 3 decades, there has been a surge towards increased consumption of sugar-sweetened beverages (SSBs), especially among young US adults (aged 19–39 y) (4), which have been identified as the major source of added sugars in the US diet (5, 6). Globally, regions with the highest intake of SSBs include North America, Latin America, Australasia, and Western Europe (7), where Chile was identified as the region with the greatest increase in SSB consumption (7). The average daily calorie intake from SSBs in the US in 2011–2014 was 179 kcal for men and 113 kcal for women (8), with younger adults showing a greater intake of SSBs than older adults (8). Moreover, differences in the intake of SSBs have been found for US residents according to ethnicity, income, and behavioral characteristics (9, 10). However, it has been reported that in the US SSB intake in the form of soda consumption has declined, whereas intake of heavy sports and/or energy drinks has increased (11), thereby indicating a shift in consumer preferences.
SSBs are nonalcoholic drinks, which typically consist of water and sugar in the form of high-fructose corn syrup or sucrose with the addition of a flavor enhancer, and often caffeine. SSB consumption has been linked to elevations in blood pressure (12–14), weight gain (15), elevated blood lipid and blood glucose concentrations (13), increased risk of type 2 diabetes (T2DM) (16, 17), coronary heart disease (18), and stroke (particularly cerebral infarction) (19). Sucrose, the most common sweetener used in beverages in Europe, comprises the monosaccharides fructose and glucose, with the fructose component often being regarded as the more harmful moiety (20, 21). Indeed, there is compelling evidence in animals, and increasingly in humans, that chronically high consumption of fructose can lead to a more adverse lipid profile and greater risks for central obesity, diabetes, and CVD than high glucose consumption (21–24). For example, although sustained consumption of glucose-sweetened beverages for 10 wk led to similar weight gains in a cohort of overweight and obese adults as in those consuming beverages sweetened with fructose, dietary fructose specifically increased visceral adiposity and dyslipidemia and decreased insulin sensitivity (24). Furthermore, fructose, but not glucose, has been reported to increase postprandial systolic and diastolic blood pressure in healthy young adults (25, 26), findings which are in support of the notion that diets that include repeated fructose loads might over time contribute to an increased risk of CVD. However, the underlying mechanisms for this impact on blood pressure are still elusive, and whether the blood pressure–elevating effects of fructose would be exacerbated (and indeed those of sucrose unmasked) under conditions of glucose intolerance, which is often encountered in overweight or obese individuals, is unknown.
SSBs and their Impact on the Cardiovascular System
It was not until 2014 that the first systematic review on the impact of chronic SSB consumption on blood pressure was published (27). Malik and colleagues (27) included in their review 6 cross-sectional and 6 prospective cohort studies encompassing a total of 409,707 participants, and observed in 10 out of 12 studies a statistically significant, positive association between SSB consumption and blood pressure, whereas the other 2 presented a positive trend. More specifically, in response to SSB intake, 5 studies found an increase in systolic blood pressure (28–32), whereas 7 (14, 33–38) showed elevated OR values for incidence of hypertension in response to increasing SSB consumption (27). With the exception of 2 studies in which the sweetener used was not mentioned (32, 35), all other studies (14, 28–31, 33, 34, 36–38) investigated the impact of high-fructose corn syrup or a mixture of high-fructose corn syrup, glucose, and sucrose. Interestingly, the impact of SSB intake on blood pressure was reduced in younger subjects when compared with studies performed in older individuals, which could be because of differing endothelial and smooth muscle responses (27). As noted by Malik and colleagues (27), a caveat of the studies included in the review is the use of FFQs to assess SSB consumption. Although FFQs may provide valuable information, this dietary assessment method relies on accurate subject recall and is therefore prone to bias, which reduces the reliability of the collected data (39). Moreover, quantification of absolute intake of SSBs is not possible using FFQs (39).
In contrast to cross-sectional studies, randomized crossover trials offer advantages based on an evaluation within the same subject. This eliminates between-subject variability and provides insights into the mechanistic processes (40). In this context, a recent randomized crossover study investigated the cardiovascular responses of young and healthy adults to ingestion of various sugary drinks and concluded that the sucrose moiety does not seem to have an impact on blood pressure, whereas isoenergetic amounts of fructose raised the blood pressure substantially (26). Moreover, although sucrose comprises equivalent amounts of glucose and fructose, the cardiovascular responses were related more to the glucose than to the fructose (26). These findings led the study's authors to the conclusion that the blood pressure–elevating effects of fructose are attenuated in the presence of glucose through glucose-induced actions on vascular resistance (26). However, the underlying mechanisms by which sugary drinks affect the cardiovascular system, in particular blood pressure, remain elusive.
Potential Mechanisms Underlying Differential Effects of Sugars on Postprandial Blood Pressure
Differential insulin release and impact on blood pressure regulation in normal glucose tolerance
In response to glucose ingestion, the blood glucose concentration rises and induces a rapid increase in plasma insulin; this increase in plasma insulin is markedly lower in response to fructose ingestion (41–46), as fructose is converted to glucose slowly in the liver and is only partly released as glucose in the circulation (47). Glucose-induced insulin release is known to dose-dependently increase cardiac output (by increasing stroke volume and heart rate) and to reduce systemic vascular resistance (48) (Figure 1). This assertion is supported by previous findings that show increased heart rate, stroke volume, and cardiac output in response to glucose ingestion, but decreased total peripheral resistance (25, 26). These combined effects are accompanied by either no change (25) or a slight increase in blood pressure (26). However, despite this lack of significant overall change in blood pressure in response to glucose ingestion, a recent study observed a large inter-subject variability in overall (i.e., averaged over 120 min with baseline values subtracted) and peak (i.e., maximum response averaged over 10 min with baseline values subtracted) blood pressure changes (49). In this context, the study's authors suggested that the focus for future research should be on individual responses rather than on mean results in order not to neglect potential ‘treatment responders’ (49).
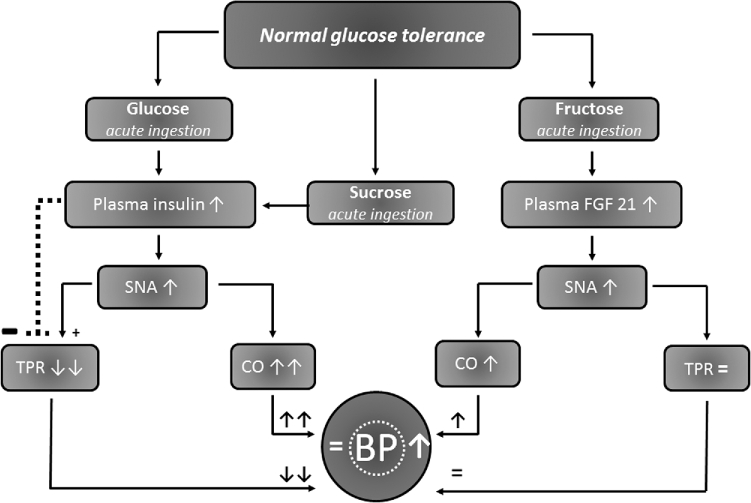
FIGURE 1.
Schematic depiction of the proposed mechanisms by which blood pressure is influenced in response to glucose, sucrose, and fructose ingestion in subjects with normal glucose tolerance. The main difference between sucrose—whose cardiovascular actions are more related to glucose than to fructose (26)—and fructose can best be explained by the actions of insulin, which, in response to sucrose, will dose-dependently increase CO by increasing stroke volume and heart rate owing to attenuated systemic vascular resistance (48), whereas the impact of fructose on the release of insulin is marginal (47). Therefore, sucrose- or glucose-induced reductions in TPR are largely offset by increases in CO, and consequently will not change the blood pressure. In contrast, acute fructose ingestion has only little overall effect on plasma insulin but increases plasma FGF-21, which increases SNA. This, in turn, leads to augmented CO, which, in combination with an unchanged or only slightly increased TPR, increases the overall BP. BP, blood pressure; CO, cardiac output; FGF-21, plasma fibroblast growth factor 21; SNA, sympathetic nerve activity; TPR, total peripheral resistance; ↓, decrease; ↑, increase; ↓↓, pronounced decrease; ↑↑, pronounced increase; —, inhibition; +, augmentation; =, unchanged.
Potential impact of glucose intolerance on blood pressure and cardiovascular responses to glucose
Impaired glucose tolerance, which usually precedes T2DM, substantially increases the risk for CVD (50), which raises the possibility that even early-stage alterations in glucose metabolism may affect the cardiovascular system. Impaired glucose tolerance comprises elevated concentrations of insulin and sympathetic neural activity at rest (51). Hence, it is probable that further stimulation of insulin secretion could cause additional increases in sympathetic nerve activity with a subsequent potential impact on total peripheral resistance (52). Indeed, Ferrannini and colleagues (52) surmised that insulin resistance could impact on blood pressure because of diminished vasodilation. Moreover, aside from the effects of elevated concentrations of insulin, it is plausible that impaired glucose tolerance concurrently affects the frequency and contraction force of the heart owing to higher levels of sympathetic nerve activity, which could override or substantially attenuate potential vasodilatory effects. Therefore, in such a scenario, impaired glucose tolerance would raise blood pressure owing to its impact on cardiac cells rather than peripheral effects on blood vessels (Figure 2).
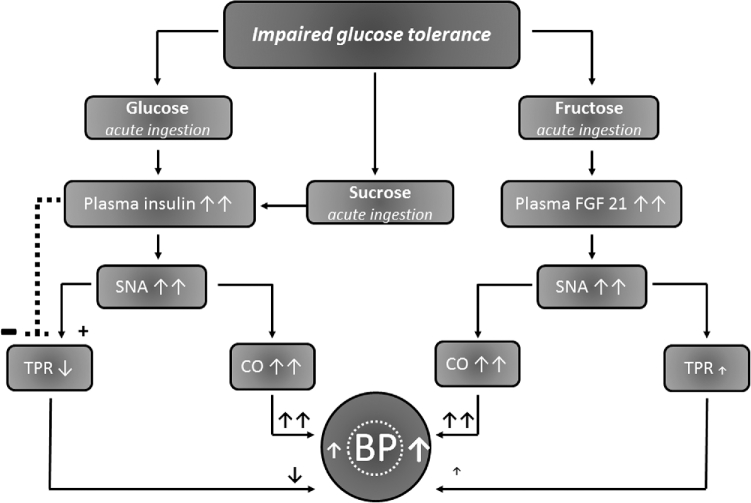
FIGURE 2.
Schematic depiction of the proposed mechanisms by which blood pressure is hypothesized to affect glucose, sucrose, and fructose responses in subjects with impaired glucose tolerance. It is suggested that in a state of impaired glucose tolerance, which is characterized by elevated resting insulin and sympathetic nerve activity, an additional surge in insulin in response to the ingestion of sucrose will further raise SNA and therefore impact on TPR. This potentially raises blood pressure because of an attenuated vasodilatory effect of insulin on the vasculature owing to concurrently elevated SNA. Furthermore, in response to fructose ingestion, FGF-21 impacts centrally and raises SNA, and could therefore lead to further increases in CO and TPR. This, in turn, elevates the blood pressure to an even higher level than in glucose-tolerant subjects. BP, blood pressure; CO, cardiac output; FGF-21: plasma fibroblast growth factor 21; SNA: sympathetic nerve activity; TPR: total peripheral resistance; ↓, decrease; ↑, increase; ↓↓, pronounced decrease; ↑↑, pronounced increase; —, inhibition; +, augmentation; =, unchanged.
Despite an abundance of information on the fate of glucose and insulin in response to the oral glucose tolerance test (OGTT), which is supposedly the gold standard for diagnosing impaired glucose tolerance, little is known about concomitant changes in cardiovascular parameters. One study (53) has highlighted differences in blood pressure according to waist circumference in response to an OGTT: systolic and diastolic blood pressure were found to decrease (–6.3% and –9.4%, respectively) in response to an OGTT in subjects with a waist circumference <85 cm, whereas in those with a waist circumference >85 cm, systolic and diastolic blood pressure increased (+2% and +0.9%, respectively). Tabara and colleagues (54) measured brachial and central blood pressure responses to an OGTT in 1034 subjects and observed insulin sensitivity and insulin resistance as independent determinants of differences between peripheral and central (aortic) blood pressure. Central (aortic) blood pressure provides an indication of the true load imposed on target organs and thus is proposed to better predict cardiovascular events than peripheral (brachial) blood pressure (55).
An important outcome of a previous study (49) was the description and quantification of interindividual blood pressure responses: the peak systolic blood pressure of 63% of subjects was increased by >4 mm Hg following an OGTT. It would be of interest to know whether these blood pressure responses, in particular in so-called “responders,” who are defined by an increase of >4 mm Hg, could be repeated in the same individual. In this context, potential reproducible systolic blood pressure changes in response to oral glucose loads could be of importance for the development of a screening tool where susceptible individuals are followed over a longer period in order to verify the potential for later emergence of hypertension. Indeed, blood pressure intra-variability [i.e., variations in blood pressure over time within a single person (56, 57)] has been observed as an independent predictor for cardiovascular events (57). However, we are not aware of any study in adults in which reproducibility of intra-individual blood pressure changes was prospectively investigated in response to a standardized glucose drink.
Proposed mechanisms underlying the blood pressure response to sucrose and fructose in subjects with normal and impaired glucose tolerance
All of the above-mentioned studies investigated the effect of glucose only, but individuals generally prefer a beverage sweetened with sucrose or high-fructose corn syrup, i.e., combined glucose and fructose in equivalent or similar amounts. The main difference between sucrose and fructose can best be explained by the actions of insulin, which, in response to sucrose, will dose-dependently increase cardiac output by increasing the stroke volume and heart rate, and decreasing systemic vascular resistance (48); in contrast, the impact of fructose on the release of insulin is marginal (47). Therefore, sucrose-induced decreases in total peripheral resistance are largely offset by subsequent increases in cardiac output; consequently, they do not change the blood pressure. On the other hand, fructose ingestion elevates the heart rate to a greater extent than does glucose (25, 26) but causes little change in the total peripheral resistance (25, 26) and thus leads to elevations in blood pressure (Figure 1).
In contrast to the effect of sucrose in subjects with normal glucose tolerance (Figure 1), it is suggested that in subjects with impaired glucose tolerance, which is characterized by elevated resting insulin and sympathetic nerve activity, an additional surge in insulin will further raise sympathetic nerve activity and cardiac output. Thus, blood pressure will rise owing to the attenuated vasodilatory effect of insulin on the vasculature because of the increased sympathetic drive to resistance vessels and cardiac cells (Figure 2). Furthermore, in response to fructose ingestion, it has been observed that in individuals with the metabolic syndrome, fibroblast growth factor 21 (FGF-21) increased substantially more than in those without the metabolic syndrome (58). In this context, FGF-21 has been found to impact centrally and raises sympathetic nerve activity (59), and therefore, in a metabolic-syndrome scenario, may lead to further increases in cardiac output and total peripheral resistance. These, in turn, could elevate blood pressure to a higher level than in healthy individuals. To date, however, insulin and FGF-21 kinetics and their association with differential blood pressure and hemodynamic responses to sucrose, glucose, and fructose have not been investigated.
Circulating FGF-21: a potential link between fructose metabolism and sympathetic overactivity
Landsberg and Young (60), in reviewing the relation between dietary intake and sympathetic nervous system activity, concluded that insulin was able to enhance sympathetic activity. Moreover, in response to increasing insulin concentrations, obese men have been found to have comparable elevations in sympathetic activity to lean and insulin-sensitive subjects (61). Since fructose ingestion leads to only a marginal increase in circulating insulin concentrations (47), sympathetic neural responses to fructose are likely to be less dependent on the involvement of insulin than those to glucose (62). Interestingly, as pointed out by Young and colleagues (62), of all of the early human and animal studies examining sympathetic responses to fructose (63–69), the only reports demonstrating fructose-induced sympathetic activation were those in which fructose was given orally, and clearly not those (66–69) in which fructose was administered parentally. Young and colleagues (62) went on to propose that the afferent signal for sympathetic stimulation by fructose is likely to originate from peripheral chemoreceptors, possibly those located in the gastrointestinal tract and/or liver.
Recently, evidence has emerged that FGF-21 released by the liver could be linked to hepatic metabolism of fructose (58). In response to oral ingestion of 75 g fructose, FGF-21 was significantly increased above the baseline concentrations, with the peak response occurring at ∼120 min postprandially (58). These increases in circulating FGF-21 in response to fructose were more pronounced in patients with metabolic syndrome (58), which may be related to their high risk for glucose intolerance and insulin resistance. The time course for circulating FGF-21 seems similar to the blood pressure effects of a comparable amount of fructose (25), which raises the possibility that circulating FGF-21 could provide a link between hepatic fructose metabolism and the activation of sympathetic activity (Figures 1 and 2). In this context, studies in mice have shown that FGF-21 acts directly on the brain to stimulate sympathetic nerve activity (59). In addition to fructose, increases in plasma FGF-21 concentrations in mice have also been shown to occur in response to ingestion of 10% glucose or 10% sucrose, but not saccharin or water (70). In humans, excess dietary carbohydrate intake (80% of energy, with a glucose:fructose ratio of 1:1) for 3 d resulted in an 8-fold increase in FGF-21 concentrations compared with a control diet (71), whereas ingestion of 75 g sucrose doubled FGF-21 concentrations in healthy subjects, with peak responses occurring 120 min after ingestion (72). In contrast, glucose only, provided as part of an OGTT, resulted in no overall change in FGF-21 concentrations (73, 74). It is therefore possible that increasing concentrations of FGF-21 are triggered by fructose or a combination of glucose and fructose, and may be involved in blood pressure elevation. Moreover, higher FGF-21 blood concentrations in patients with metabolic syndrome (58) could be speculated to exacerbate fructose-induced elevations in blood pressure.
Potential Cardiovascular Neutral Sugars
Galactose
Lactose is a disaccharide comprising of the monosaccharides glucose and galactose, at which galactose has received much attention as a low–glycemic index sugar, with only small increases in plasma glucose and insulin in response to its ingestion (46, 75, 76). Recently, the cardiovascular effects of galactose have also been explored (77). In this context, acute cardiovascular responses to the ingestion of 60 g galactose were investigated and compared with the same quantity of fructose or glucose with the use of a randomized crossover study design (77). This study observed that glucose and galactose had minor effects on blood pressure, which contrasted to the blood-pressure-elevating effect of fructose. Moreover, galactose affected cardiac workload to a significantly lesser extent than glucose. Therefore, the benefits of galactose appear to be 2-fold: 1) it is a low–glycemic index sugar and 2) it appears to induce milder cardiovascular effects than either fructose or glucose. Future studies are needed to investigate the cardiovascular effect of chronic galactose consumption alone and in combination with other sugars in healthy individuals, as well as in those with impaired glucose tolerance.
Artificial sweeteners
The increasing consumption of added sugars, i.e., dietary carbohydrates that are artificially added to edible food items during processing or preparation, particularly in the form of liquid sugars, is deemed to be an important contributor to weight gain (38, 78–80). These findings have been strengthened by a randomized controlled trial in which changes in body weight associated with sucrose intake seemed to be attributable to changes in energy intake rather than energy expenditure (81). As a result, the American Heart Association recommends limiting added sugar intake to no more than 100 kcal (∼25 g)/d for women and 150 kcal (∼38 g)/d for men (82).
Knowledge of the potential detrimental health effects associated with SSB consumption has driven an increase in the consumption of low-calorie sweeteners (LCSs) (83, 84), often consumed in the form of reduced-calorie beverages (i.e., beverages containing calories and which are sweetened with LCS) (83). LCSs are food additives containing practically no calories, which are associated with an intense sweetness and are mostly used to artificially sweeten food and beverages (85). The most popular and commonly used artificial sweeteners include aspartame, acesulphame-K, saccharin, sucralose, and cyclamate. The effect of artificial sweeteners on body weight and metabolic risk markers has been reviewed and, when compared with sucrose-sweetened drinks, LCSs were found to have beneficial effects on body weight, glycemia, and insulinemia (86). Maersk and colleagues (87) observed that ingestion of 1 L/d of a sucrose-sweetened soft drink (regular cola) over a 6-mo period resulted in augmented liver-, skeletal-, and visceral fat, and increased plasma triglycerides and total cholesterol, which were not seen when drinking the same amount of an aspartame-sweetened soft drink (diet cola) or water (87). Similarly, a 10-wk parallel intervention study found significant increases in body weight and fat mass, as well as systolic and diastolic blood pressure, among overweight subjects consuming sucrose, but not in those consuming artificial sweeteners (88).
Additional interesting LCSs include stevioside, approved by the European Food Safety Authority (89), and erythritol, a commonly used polyol sweetener, both of which are used as alternatives to aspartame, acesulfame-K, sucralose, and saccharin. However, clinical data on stevia (derived from the leaves of Stevia rebaudiana) and its potential cardiovascular effects are scarce and inconclusive. Stevia has been shown to reduce blood glucose concentrations by 18% in individuals with T2DM compared with a cornstarch meal (90), but chronic use of stevia (1000 mg rebaudioside A or placebo over 16 wk) did not alter glucose homeostasis or blood pressure in patients with T2DM (91). With respect to erythritol, one study investigated the effect of acute (24 g) and chronic (36 g/d × 4 wk) erythritol supplementation in beverage form and found improved endothelial function in patients with T2DM (92). In a post hoc analysis, Flint and colleagues (92) observed that in patients with brachial systolic blood pressure >130 mm Hg, chronic treatment with erythritol lowered the central pulse pressure (i.e., aortic systolic blood pressure minus aortic diastolic blood pressure), which suggests a central (aortic) antihypertensive effect (92). Unfortunately, this study lacked a control group and raises concerns about multiple testing. Future cardiovascular research should focus on potential interaction effects of LCSs with sucrose and/or caffeine because of the widespread use of such beverages (i.e., diet beverages sweetened with sucrose and LCS, with or without caffeine).
Conclusion
High consumption of SSBs has been implicated in the development of hypertension, hyperlipidemia and obesity, all of which are involved in the pathogenesis of CVD. This review provides an important mechanistic understanding of how sweetened beverages affect cardiovascular responses, with particular reference to the regulation of blood pressure, which is a key contributor to increased CVD risk. Overweight and obesity, particularly abdominal fat accumulation, negatively impact insulin sensitivity, and in this context it is hypothesized that impaired glucose tolerance resulting from altered insulin action is contributing to altered blood pressure regulation. Another potential mechanism whereby SSBs may increase CVD risk is sympathetic activation, which is potentially driven by FGF-21 in response to orally ingested fructose. In contrast to fructose and glucose, galactose appears to induce milder cardiovascular effects, while artificial sweeteners either have no effect on cardiovascular parameters or are beneficial. Finally, we have identified a need for further research to elucidate whether (and how) pre-existing glucose intolerance in individuals may exacerbate the postprandial cardiovascular responses to sugary drinks, thus aggravating cardiovascular risk in already susceptible individuals.
Acknowledgments
Both authors read and approved the final manuscript.
Notes
Author disclosures: CRM and EKG, no conflicts of interest and no competing financial interests.
Perspectives articles allow authors to take a position on a topic of current major importance or controversy in the field of nutrition. As such, these articles could include statements based on author opinions or points of view. Opinions expressed in Perspectives articles are those of the author and are not attributable to the funder(s) or the sponsor(s) or the publisher, Editor, or Editorial Board of Advances in Nutrition. Individuals with different positions on the topic of a Perspective are invited to submit their comments in the form of a Perspectives article or in a Letter to the Editor.
The authors reported no funding received for this study.
Abbreviations used:
- CVD
cardiovascular disease
- FGF-21
fibroblast growth factor 21
- LCS
low-calorie sweetener
- OGTT
oral glucose tolerance test
- SSB
sugar-sweetened beverage
- T2DM
type 2 diabetes
References
- 1. GBD 2013 Mortality and Causes of Death Collaborators Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;385:117–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, de Ferranti SD, Floyd J, Fornage M, Gillespie C. et al. Heart disease and stroke statistics—2017 update: a report from the American Heart Association. Circulation 2017;135:e146–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Speakman JR, Levitsky DA, Allison DB, Bray MS, de Castro JM, Clegg DJ, Clapham JC, Dulloo AG, Gruer L, Haw S. et al. Set points, settling points and some alternative models: theoretical options to understand how genes and environments combine to regulate body adiposity. Dis Model Mech 2011;4:733–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nielsen SJ, Popkin BM. Changes in beverage intake between 1977 and 2001. Am J Prev Med 2004;27:205–10. [DOI] [PubMed] [Google Scholar]
- 5. Kumar GS, Pan L, Park S, Lee-Kwan SH, Onufrak S, Blanck HM. Sugar-sweetened beverage consumption among adults – 18 states, 2012. MMWR Morb Mortal Wkly Rep 2014;63:686–90. [PMC free article] [PubMed] [Google Scholar]
- 6. Welsh JA, Sharma AJ, Grellinger L, Vos MB. Consumption of added sugars is decreasing in the United States. Am J Clin Nutr 2011;94:726–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Popkin BM, Hawkes C. Sweetening of the global diet, particularly beverages: patterns, trends, and policy responses. Lancet Diabetes Endocrinol 2016;4:174–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rosinger A, Herrick K, Gahche J, Park S. Sugar-sweetened beverage consumption among U.S. adults, 2011–2014. NCHS Data Brief 2017;270:1–8. [PubMed] [Google Scholar]
- 9. Ogden CL, Kit BK, Carroll MD, Park S. Consumption of sugar drinks in the United States, 2005–2008. NCHS Data Brief 2011;71:1–8. [PubMed] [Google Scholar]
- 10. Park S, Pan L, Sherry B, Blanck HM. Consumption of sugar-sweetened beverages among US adults in 6 States: behavioral risk factor surveillance system, 2011. Prev Chronic Dis 2014;11:E65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Han E, Powell LM. Consumption patterns of sugar-sweetened beverages in the United States. J Acad Nutr Diet 2013;113:43–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Te Morenga LA, Howatson AJ, Jones RM, Mann J. Dietary sugars and cardiometabolic risk: systematic review and meta-analyses of randomized controlled trials of the effects on blood pressure and lipids. Am J Clin Nutr 2014;100:65–79. [DOI] [PubMed] [Google Scholar]
- 13. Keller A, Heitmann BL, Olsen N. Sugar-sweetened beverages, vascular risk factors and events: a systematic literature review. Public Health Nutr 2015;18:1145–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Duffey KJ, Gordon-Larsen P, Steffen LM, Jacobs DR, Popkin BM. Drinking caloric beverages increases the risk of adverse cardiometabolic outcomes in the Coronary Artery Risk Development in Young Adults (CARDIA) Study. Am J Clin Nutr 2010;92:954–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Malik VS, Schulze MB, Hu FB. Intake of sugar-sweetened beverages and weight gain: a systematic review. Am J Clin Nutr 2006;84:274–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. de Koning L, Malik VS, Rimm EB, Willett WC, Hu FB. Sugar-sweetened and artificially sweetened beverage consumption and risk of type 2 diabetes in men. Am J Clin Nutr 2011;93:1321–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Imamura F, O'Connor L, Ye Z, Mursu J, Hayashino Y, Bhupathiraju SN, Forouhi NG. Consumption of sugar sweetened beverages, artificially sweetened beverages, and fruit juice and incidence of type 2 diabetes: systematic review, meta-analysis, and estimation of population attributable fraction. BMJ 2015;351:h3576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. de Koning L, Malik VS, Kellogg MD, Rimm EB, Willett WC, Hu FB. Sweetened beverage consumption, incident coronary heart disease, and biomarkers of risk in men. Circulation 2012;125:1735–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Larsson SC, Akesson A, Wolk A. Sweetened beverage consumption is associated with increased risk of stroke in women and men. J Nutr 2014;144:856–60. [DOI] [PubMed] [Google Scholar]
- 20. Tappy L, Le K-A. Metabolic effects of fructose and the worldwide increase in obesity. Physiol Rev 2010;90:23–46. [DOI] [PubMed] [Google Scholar]
- 21. Brown CM, Dulloo AG, Montani J-P. Sugary drinks in the pathogenesis of obesity and cardiovascular diseases. Int J Obes 2008;32:S28–34. [DOI] [PubMed] [Google Scholar]
- 22. Bray GA, Nielsen SJ, Popkin BM. Consumption of high-fructose corn syrup in beverages may play a role in the epidemic of obesity. Am J Clin Nutr 2004;79:537–43. [DOI] [PubMed] [Google Scholar]
- 23. Fung TT, Malik V, Rexrode KM, Manson JE, Willett WC, Hu FB. Sweetened beverage consumption and risk of coronary heart disease in women. Am J Clin Nutr 2009;89:1037–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Stanhope KL, Schwarz JM, Keim NL, Griffen SC, Bremer AA, Graham JL, Hatcher B, Cox CL, Dyachenko A, Zhang W. et al. Consuming fructose-sweetened, not glucose-sweetened, beverages increases visceral adiposity and lipids and decreases insulin sensitivity in overweight/obese humans. J Clin Invest 2009;119:1322–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Brown CM, Dulloo AG, Yepuri G, Montani JP. Fructose ingestion acutely elevates blood pressure in healthy young humans. Am J Physiol Regul Integr Comp Physiol 2008;294:R730–7. [DOI] [PubMed] [Google Scholar]
- 26. Grasser EK, Dulloo A, Montani JP. Cardiovascular responses to the ingestion of sugary drinks using a randomised cross-over study design: does glucose attenuate the blood pressure-elevating effect of fructose? Br J Nutr 2014;112:183–92. [DOI] [PubMed] [Google Scholar]
- 27. Malik AH, Akram Y, Shetty S, Malik SS, Yanchou Njike V. Impact of sugar-sweetened beverages on blood pressure. Am J Cardiol 2014;113:1574–80. [DOI] [PubMed] [Google Scholar]
- 28. Brown IJ, Stamler J, Van Horn L, Robertson CE, Chan Q, Dyer AR, Huang C-C, Rodriguez BL, Zhao L, Daviglus ML. et al. Sugar-sweetened beverage, sugar intake of individuals, and their blood pressure: international study of macro/micronutrients and blood pressure. Hypertension 2011;57:695–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Chen L, Caballero B, Mitchell DC, Loria C, Lin P-H, Champagne CM, Elmer PJ, Ard JD, Batch BC, Anderson CAM. et al. Reducing consumption of sugar-sweetened beverages is associated with reduced blood pressure: a prospective study among United States adults. Circulation 2010;121:2398–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Nguyen S, Choi HK, Lustig RH, Hsu C. Sugar-sweetened beverages, serum uric acid, and blood pressure in adolescents. J Pediatr 2009;154:807–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bremer AA, Auinger P, Byrd RS. Relationship between insulin resistance-associated metabolic parameters and anthropometric measurements with sugar-sweetened beverage intake and physical activity levels in US adolescents: findings from the 1999–2004 National Health and Nutrition Examination Survey. Arch Pediatr Adolesc Med 2009;163:328–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ambrosini GL, Oddy WH, Huang RC, Mori TA, Beilin LJ, Jebb SA. Prospective associations between sugar-sweetened beverage intakes and cardiometabolic risk factors in adolescents. Am J Clin Nutr 2013;98:327–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jalal DI, Smits G, Johnson RJ, Chonchol M. Increased fructose associates with elevated blood pressure. J Am Soc Nephrol 2010;21:1543–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kim YH, Abris GP, Sung M-K, Lee JE. Consumption of sugar-sweetened beverages and blood pressure in the United States: the national health and nutrition examination survey 2003–2006. Clin Nutr Res 2012;1:85–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Tayel DI, El-Sayed NA, El-Sayed NA. Dietary pattern and blood pressure levels of adolescents in Sohag, Egypt. J Egypt Public Health Assoc 2013;88:97–103. [DOI] [PubMed] [Google Scholar]
- 36. Winkelmayer WC, Stampfer MJ, Willett WC, Curhan GC. Habitual caffeine intake and the risk of hypertension in women. JAMA 2005;294:2330. [DOI] [PubMed] [Google Scholar]
- 37. Cohen L, Curhan G, Forman J. Association of sweetened beverage intake with incident hypertension. J Gen Intern Med 2012;27:1127–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Dhingra R, Sullivan L, Jacques PF, Wang TJ, Fox CS, Meigs JB, D'Agostino RB, Gaziano JM, Vasan RS. Soft drink consumption and risk of developing cardiometabolic risk factors and the metabolic syndrome in middle-aged adults in the community. Circulation 2007;116:480–8. [DOI] [PubMed] [Google Scholar]
- 39. Ambrosini GL, de Klerk NH, O'Sullivan TA, Beilin LJ, Oddy WH. The reliability of a food frequency questionnaire for use among adolescents. Eur J Clin Nutr 2009;63:1251–9. [DOI] [PubMed] [Google Scholar]
- 40. Mills EJ, Chan AW, Wu P, Vail A, Guyatt GH, Altman DG. Design, analysis, and presentation of crossover trials. Trials 2009;10:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Chong MF-F, Fielding BA, Frayn KN. Mechanisms for the acute effect of fructose on postprandial lipemia. Am J Clin Nutr 2007;85:1511–20. [DOI] [PubMed] [Google Scholar]
- 42. Tappy L, Randin JP, Felber JP, Chiolero R, Simonson DC, Jequier E, DeFronzo RA. Comparison of thermogenic effect of fructose and glucose in normal humans. Am J Physiol 1986;250:E718–24. [DOI] [PubMed] [Google Scholar]
- 43. Blaak EE, Saris WH. Postprandial thermogenesis and substrate utilization after ingestion of different dietary carbohydrates. Metabolism 1996;45:1235–42. [DOI] [PubMed] [Google Scholar]
- 44. Fukagawa NK, Veirs H, Langeloh G. Acute effects of fructose and glucose ingestion with and without caffeine in young and old humans. Metabolism 1995;44:630–8. [DOI] [PubMed] [Google Scholar]
- 45. Schwarz JM, Schutz Y, Froidevaux F, Acheson KJ, Jeanprêtre N, Schneider H, Felber JP, Jéquier E. Thermogenesis in men and women induced by fructose vs glucose added to a meal. Am J Clin Nutr 1989;49:667–74. [DOI] [PubMed] [Google Scholar]
- 46. Rebello T, Hodges RE, Smith JL. Short-term effects of various sugars on antinatriuresis and blood pressure changes in normotensive young men. Am J Clin Nutr 1983;38:84–94. [DOI] [PubMed] [Google Scholar]
- 47. Hallfrisch J. Metabolic effects of dietary fructose. FASEB J 1990;4:2652–60. [DOI] [PubMed] [Google Scholar]
- 48. Baron AD, Brechtel G. Insulin differentially regulates systemic and skeletal muscle vascular resistance. Am J Physiol 1993;265:E61–7. [DOI] [PubMed] [Google Scholar]
- 49. Monnard CR, Fellay B, Scerri I, Grasser EK. Substantial inter-subject variability in blood pressure responses to glucose in a healthy, non-obese population. Front Physiol 2017;8:507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. DeFronzo RA, Abdul-Ghani M. Assessment and treatment of cardiovascular risk in prediabetes: impaired glucose tolerance and impaired fasting glucose. Am J Cardiol 2011;108:3B–24B. [DOI] [PubMed] [Google Scholar]
- 51. Rowe JW, Young JB, Minaker KL, Stevens AL, Pallotta J, Landsberg L. Effect of insulin and glucose infusions on sympathetic nervous system activity in normal man. Diabetes 1981;30:219–25. [DOI] [PubMed] [Google Scholar]
- 52. Ferrannini E, Natali A, Capaldo B, Lehtovirta M, Jacob S, Yki-Järvinen H. Insulin resistance, hyperinsulinemia, and blood pressure: role of age and obesity. European Group for the Study of Insulin Resistance (EGIR). Hypertension 1997;30:1144–9. [DOI] [PubMed] [Google Scholar]
- 53. Nakatsuji H, Kishida K, Kitamura T, Nakajima C, Funahashi T, Shimomura I. Dysregulation of glucose, insulin, triglyceride, blood pressure, and oxidative stress after an oral glucose tolerance test in men with abdominal obesity. Metabolism 2010;59:520–6. [DOI] [PubMed] [Google Scholar]
- 54. Tabara Y, Saito I, Nishida W, Kohara K, Sakurai S, Kawamura R, Onuma H, Takata Y, Osawa H, Miki T. et al. Relatively lower central aortic pressure in patients with impaired insulin sensitivity and resistance: the Toon Health Study. J Hypertens 2011;29:1948–54. [DOI] [PubMed] [Google Scholar]
- 55. Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D. et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J 2006;27:2588–605. [DOI] [PubMed] [Google Scholar]
- 56. Mancia G, Ferrari A, Gregorini L, Parati G, Pomidossi G, Bertinieri G, Grassi G, di Rienzo M, Pedotti A, Zanchetti A. Blood pressure and heart rate variabilities in normotensive and hypertensive human beings. Circ Res 1983;53:96–104. [DOI] [PubMed] [Google Scholar]
- 57. Mancia G. Short- and long-term blood pressure variability: present and future. Hypertension 2012;60:512–7. [DOI] [PubMed] [Google Scholar]
- 58. Dushay JR, Toschi E, Mitten EK, Fisher FM, Herman MA, Maratos-Flier E. Fructose ingestion acutely stimulates circulating FGF21 levels in humans. Mol Metab 2015;4:51–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Owen BM, Ding X, Morgan DA, Coate KC, Bookout AL, Rahmouni K, Kliewer SA, Mangelsdorf DJ. FGF21 acts centrally to induce sympathetic nerve activity, energy expenditure, and weight loss. Cell Metab 2014;20:670–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Landsberg L, Young JB. Insulin-mediated glucose metabolism in the relationship between dietary intake and sympathetic nervous system activity. Int J Obes 1985;9 Suppl 2:63–8. [PubMed] [Google Scholar]
- 61. Landsberg L. Diet, obesity and hypertension: an hypothesis involving insulin, the sympathetic nervous system, and adaptive thermogenesis. Q J Med 1986;61:1081–90. [PubMed] [Google Scholar]
- 62. Young JB, Weiss J, Boufath N. Effects of dietary monosaccharides on sympathetic nervous system activity in adipose tissues of male rats. Diabetes 2004;53:1271–8. [DOI] [PubMed] [Google Scholar]
- 63. Walgren MC, Young JB, Kaufman LN, Landsberg L. The effects of various carbohydrates on sympathetic activity in heart and interscapular brown adipose tissue of the rat. Metabolism 1987;36:585–94. [DOI] [PubMed] [Google Scholar]
- 64. Jansen RW, Penterman BJ, van Lier HJ, Hoefnagels WH. Blood pressure reduction after oral glucose loading and its relation to age, blood pressure and insulin. Am J Cardiol 1987;60:1087–91. [DOI] [PubMed] [Google Scholar]
- 65. Van Gaal L, Mertens I, Vansant G, De Leeuw I. Carbohydrate-induced thermogenesis in obese women. Effect of insulin and catecholamines. J Endocrinol Invest 1999;22:109–14. [DOI] [PubMed] [Google Scholar]
- 66. Schwarz JM, Acheson KJ, Tappy L, Piolino V, Müller MJ, Felber JP, Jéquier E. Thermogenesis and fructose metabolism in humans. Am J Physiol 1992;262:E591–8. [DOI] [PubMed] [Google Scholar]
- 67. Vollenweider P, Tappy L, Randin D, Schneiter P, Jéquier E, Nicod P, Scherrer U. Differential effects of hyperinsulinemia and carbohydrate metabolism on sympathetic nerve activity and muscle blood flow in humans. J Clin Invest 1993;92:147–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Niijima A. Effect of glucose and other hexoses on efferent discharges of brown adipose tissue nerves. Am J Physiol 1986;251:R240–2. [DOI] [PubMed] [Google Scholar]
- 69. Niijima A. The effect of glucose and other sugars on the efferent activity of the sympathetic nerves innervating the fatty tissue. Jpn J Physiol 1997;47 Suppl 1:S40–2. [PubMed] [Google Scholar]
- 70. von Holstein-Rathlou S, BonDurant LD, Peltekian L, Naber MC, Yin TC, Claflin KE, Urizar AI, Madsen AN, Ratner C, Holst B. et al. FGF21 mediates endocrine control of simple sugar intake and sweet taste preference by the liver. Cell Metab 2016;23:335–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Lundsgaard A-M, Fritzen AM, Sjøberg KA, Myrmel LS, Madsen L, Wojtaszewski JFP, Richter EA, Kiens B. Circulating FGF21 in humans is potently induced by short term overfeeding of carbohydrates. Mol Metab 2017;6:22–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Søberg S, Sandholt CH, Jespersen NZ, Toft U, Madsen AL, von Holstein-Rathlou S, Grevengoed TJ, Christensen KB, Bredie WLP, Potthoff MJ. et al. FGF21 is a sugar-induced hormone associated with sweet intake and preference in humans. Cell Metab 2017;25:1045–53. [DOI] [PubMed] [Google Scholar]
- 73. Schmid A, Leszczak S, Ober I, Karrasch T, Schäffler A. Short-term and divergent regulation of FGF-19 and FGF-21 during oral lipid tolerance test but not oral glucose tolerance test. Exp Clin Endocrinol Diabetes 2015;123:88–94. [DOI] [PubMed] [Google Scholar]
- 74. Zhang M, Liu Y, Xiong Z, Deng Z, Song H, An Z. Changes of plasma fibroblast growth factor-21 (FGF-21) in oral glucose tolerance test and effects of metformin on FGF-21 levels in type 2 diabetes mellitus. Endokrynol Pol 2013;64:220–4. [PubMed] [Google Scholar]
- 75. Ganda OP, Soeldner JS, Gleason RE, Cleator IG, Reynolds C. Metabolic effects of glucose, mannose, galactose, and fructose in man. J Clin Endocrinol Metab 1979;49:616–22. [DOI] [PubMed] [Google Scholar]
- 76. Coss-Bu JA, Sunehag AL, Haymond MW. Contribution of galactose and fructose to glucose homeostasis. Metabolism 2009;58:1050–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Charrière N, Loonam C, Montani JP, Dulloo AG, Grasser EK. Cardiovascular responses to sugary drinks in humans: galactose presents milder cardiac effects than glucose or fructose. Eur J Nutr 2017;56:2105–13. [DOI] [PubMed] [Google Scholar]
- 78. Mattes RD, Shikany JM, Kaiser KA, Allison DB. Nutritively sweetened beverage consumption and body weight: a systematic review and meta-analysis of randomized experiments. Obes Rev 2011;12:346–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med 2011;364:2392–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Te Morenga L, Mallard S, Mann J. Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies. BMJ 2012;346:e7492. [DOI] [PubMed] [Google Scholar]
- 81. Sørensen LB, Vasilaras TH, Astrup A, Raben A. Sucrose compared with artificial sweeteners: a clinical intervention study of effects on energy intake, appetite, and energy expenditure after 10 wk of supplementation in overweight subjects. Am J Clin Nutr 2014;100:36–45. [DOI] [PubMed] [Google Scholar]
- 82. Johnson RK, Appel LJ, Brands M, Howard BV, Lefevre M, Lustig RH, Sacks F, Steffen LM, Wylie-Rosett J, American Heart Association Nutrition Committee of the Council on Nutrition, Physical Activity, and Metabolism and the Council on Epidemiology and Prevention Dietary sugars intake and cardiovascular health: a scientific statement from the American Heart Association. Circulation 2009;120:1011–20. [DOI] [PubMed] [Google Scholar]
- 83. Sylvetsky AC, Welsh JA, Brown RJ, Vos MB. Low-calorie sweetener consumption is increasing in the United States. Am J Clin Nutr 2012;96:640–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Popkin BM, Nielsen SJ. The sweetening of the world's diet. Obes Res 2003;11:1325–32. [DOI] [PubMed] [Google Scholar]
- 85. Gibson S, Drewnowski A, Hill J, Raben AB, Tuorila H, Widström E. Consensus statement on benefits of low-calorie sweeteners. Nutr Bull 2014;39:386–9. [Google Scholar]
- 86. Raben A, Richelsen B. Artificial sweeteners: a place in the field of functional foods? Focus on obesity and related metabolic disorders. Curr Opin Clin Nutr Metab Care 2012;15:597–604. [DOI] [PubMed] [Google Scholar]
- 87. Maersk M, Belza A, Stødkilde-Jørgensen H, Ringgaard S, Chabanova E, Thomsen H, Pedersen SB, Astrup A, Richelsen B. Sucrose-sweetened beverages increase fat storage in the liver, muscle, and visceral fat depot: a 6-mo randomized intervention study. Am J Clin Nutr 2012;95:283–9. [DOI] [PubMed] [Google Scholar]
- 88. Raben A, Møller BK, Flint A, Vasilaris TH, Christina Møller A, Juul Holst J, Astrup A. Increased postprandial glycaemia, insulinemia, and lipidemia after 10 weeks’ sucrose-rich diet compared to an artificially sweetened diet: a randomised controlled trial. Food Nutr Res 2011;55:5961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. ANS, EFSA Panel on Food Additives and Nutrient Sources Added to Food Scientific opinion on the safety of steviol glycosides for the proposed uses as a food additive. EFSA J 2010;8:1537. [Google Scholar]
- 90. Gregersen S, Jeppesen PB, Holst JJ, Hermansen K. Antihyperglycemic effects of stevioside in type 2 diabetic subjects. Metabolism 2004;53:73–6. [DOI] [PubMed] [Google Scholar]
- 91. Maki KC, Curry LL, Reeves MS, Toth PD, McKenney JM, Farmer M V, Schwartz SL, Lubin BC, Boileau AC, Dicklin MR. et al. Chronic consumption of rebaudioside A, a steviol glycoside, in men and women with type 2 diabetes mellitus. Food Chem Toxicol 2008;46 Suppl 7:S47–53. [DOI] [PubMed] [Google Scholar]
- 92. Flint N, Hamburg NM, Holbrook M, Dorsey PG, LeLeiko RM, Berger A, de Cock P, Bosscher D, Vita JA. Effects of erythritol on endothelial function in patients with type 2 diabetes mellitus: a pilot study. Acta Diabetol 2014;51:513–6. [DOI] [PMC free article] [PubMed] [Google Scholar]