Supplemental Digital Content is available in the text.
Keywords: resource allocation, efficiency, sustainability, health system strengthening, Gavi
Abstract
Background:
Despite the increase in Health System Strengthening (HSS) grants, there is no consensus among global health actors about how to maximize the efficiency and sustainability of HSS programs and their resulting gains. To formally analyze and compare the efficiency and sustainability of Gavi’s HSS grants, we investigated the factors, events and root causes that increased the time and effort needed to implement HSS grants, decreased expected outcomes and threatened the continuity of activities and the sustainability of the results gained through these grants in Cameron and Chad.
Methods:
We conducted 2 retrospective independent evaluations of Gavi’s HSS support in Cameroon and Chad using a mixed methodology. We investigated the chain of events and situations that increased the effort and time required to implement the HSS programs, decreased the value of the funds spent and hindered the sustainability of the implemented activities and gains achieved.
Results:
Root causes affecting the efficiency and sustainability of HSS grants were common to Cameroon and Chad. Weaknesses in health workforce and leadership/governance of the health system in both countries led to interrupting the HSS grants, reprogramming them, almost doubling their implementation period, shifting their focus during implementation toward procurements and service provision, leaving both countries without solid exit plans to maintain the results gained.
Conclusions:
To increase the efficiency and sustainability of Gavi’s HSS grants, recipient countries need to consider health workforce and leadership/governance prior, or in parallel to strengthening other building blocks of their health systems.
Health system strengthening (HSS) is needed to address the broader challenges affecting all 6 of World Health Organization’s (WHO) health system building blocks: leadership/governance, health workforce, health care financing, medical products and technologies, service delivery and health information systems, in a horizontal approach.1,2
Gavi, the Vaccine Alliance (Gavi) HSS grants were initially designed to increase vaccine coverage in recipient countries by strengthening the capacity of the health system to deliver immunization and other health services in a horizontal approach.3,4 Countries apply to receive this support to address priorities identified at the country level with a myriad of stakeholders. Gavi has committed 862.5 million $US to HSS for 2007–2017, while doubling its annual HSS disbursements between 2012 and 2013.5 Because HSS has a broader impact on health services, it is crucial that these funds be used as efficiently as possible and result in sustainable gains. Despite the increase in HSS funding, there is no consensus about how to maximize the efficiency and sustainability of HSS grants and their resulting gains. Efficiency and sustainability are 2 of the 5 domains that the Organization for Economic Cooperation and Development recommends assessing independently from relevance, effectiveness and impact when evaluating development assistance. Gavi has also adopted the use of these domains for evaluating its financial support to countries.6–9 An efficient program minimizes cost, effort and time required from people, and produces the maximum desired output.10 A sustainable program has the capacity to achieve long-term success and stability and to serve its recipients and consumers without interruption of services after external assistance ends.11
Cameroon and Chad are recipients of Gavi HSS support. Cameroon received Gavi HSS support in 2007. The funds were reprogrammed in 2013 after 2 years of interruption.12,13 Chad requested and was granted Gavi HSS funding in 2008.14 The program was scheduled to end in 2012, and was reprogrammed in 2012 and 2013 after the 2 years of interruption.15,16 Both countries’ programs were still ongoing at the end of 2015 with no formal independent evaluation.
Using WHO’s 6 health system building blocks, we hypothesized that unaddressed weaknesses in leadership/governance and health workforce were the major causes behind the decreased efficiency and sustainability of HSS in Cameroon and Chad. To verify this hypothesis, we (1) investigated the factors, events and root causes that increased the cost, time and effort needed to implement HSS grants and threatened the continuity of activities and sustainability of the results gained through HSS and (2) assigned them to the health system building blocks in the 2 countries.
MATERIALS AND METHODS
Two retrospective independent evaluations of Gavi HSS support in Cameroon and Chad were conducted using a mixed methodology.
Qualitative Methods
Document Review
A document review (DR) was conducted to refine the research questions, identify key informants (KIs) and develop KI interview (KII) topic guides and guide the quantitative analysis.17 Documents were selected as they pertain to Gavi HSS programs in Cameroon and Chad.18 We searched for (1) documents relevant to HSS assessment, such as Gavi HSS country proposals and accompanying responses, HSS documentation provided by Gavi, Gavi HSS policies and procedures, strategic plans such as annual plans of the Expanded Program on Immunization and national health plans and (2) evaluations, either internal or external, that addressed relevance and achievement of results such as other countries’ end-of-grant Gavi HSS evaluations, annual progress reports, Millennium Development Goals progress reports and academic evaluations of Gavi HSS grants.
Key Informant Interviews
KIs were selected through a purposive sampling strategy (Table 1). These were stakeholders from the Ministries of Health and their various directorates, the Expanded Program on Immunization, WHO, United Nations Children’s Fund (UNICEF), bilateral donors, local partners involved in the Gavi HSSs and representatives from Gavi Secretariat and Gavi Independent Review Committee.
TABLE 1.
Participants in Gavi HSS Evaluations in Cameroon and Chad by Category and Method of Data Collection

A general structured KII topic guide was developed after DR and consultations with the Gavi Secretariat monitoring and evaluation team. The general topic guide was tailored toward each audience based on their knowledge of various parts of the HSS grant in the country.
Questionnaires
We visited a sample of health areas, districts, and facilities and collected data on Gavi HSS grant implementation using questionnaires (Q) developed based on HSS activities. The Gavi HSS grant proposes different activities for the central, regional, district and health facility levels (Tables, Supplemental Digital Content 1 and 2, http://links.lww.com/INF/C914; http://links.lww.com/INF/C915). Qs were developed to assess and verify the implementation of all activities at each of the 4 levels during the field visits. Stakeholders at the central, regional and district levels interviewed through the KII technique were the same as those interviewed using these standardized Qs. Table 1 represents study participants by category and method of data collection.
Data collection was completed face-to-face during June–July 2015, and September–October 2015 in Chad and Cameroon, respectively. Collected data were transferred electronically to a secure server. Verbal consent was obtained at the beginning of each interview and both studies were deemed exempt from institutional review board approval. Data from KIIs were analyzed through recursive abstraction.19
Quantitative Methods
Financial Analysis
We analyzed HSS grant disbursements by comparing budgets to expenditures. Each Gavi HSS grant proposal includes an original budget for funds expenditure over the duration of the program. During each funding year, the country submits a planned budget for the upcoming year within the Annual Progress Report. This planned budget can include variations of <15% from the originally proposed budget, as well as details of the expenditures that occurred during the last year. A financial analysis (FA) was conducted to compare proposed expenditures in the HSS grant proposal budget, planned expenditures in the Gavi HSS annual progress reports and actual expenditures. This allowed us to assess adherence to the expenditures in proposed and approved budgets.20–28 For each category of expenditures, we calculated percent deviation from the proposed budget and summed all changes.
Root-cause Analysis
Data generated from all quantitative and qualitative methods were triangulated through a root-cause analysis, a particularly useful approach in the study of complex interventions like HSS.29–31 We investigated the chain of events and situations that increased the effort and time required to implement the HSS program, decreased the value of the funds spent and hindered the sustainability of the implemented activities and gains achieved.
RESULTS
The results section presents the root-cause analysis combining data from all methods used (Fig. 1). At the end of each paragraph, we indicate the method that generated the result presented [DR, KIIs, Qs, FA].
FIGURE 1.

Root-cause analysis behind the decreased efficiency and sustainability of Gavi HSS grants in Cameroon and Chad.
Efficiency
Funds Allocation
The first disbursement of funds was delayed in both countries because of, among other things, the countries’ late response to the Gavi Independent Review Committee’s requests for clarifications concerning HSS proposals—usually caused by high staff turnover—and internal procedures at Gavi. A lack of planning for this scenario created a need to implement a large number of activities within a shorter period of time during the first year. A combination of inflexible fiscal laws and the late arrival of funds in country meant that these funds could not be effectively used within the annual budget cycle. This planning deficit stemmed from a shortage of appropriate health workforce, combined with delays of HSS disbursements. Both countries were not prepared for the delays and had no alternative implementation plans or financial management guidelines (DR, KII).
The Gavi Secretariat requires HSS expenditures adhere to approved budgets. Any deviations exceeding 15% of originally approved budgets requires approval from the Gavi Secretariat.
In Cameroon, the technical secretariat, made up of a handful of people, designed and implemented the HSS program unsupervised by any other national entity or the health partners. Funds were mostly spent on day-to-day planning and monitoring operations, resulting in 52% of actual expenditures deviating from the proposed ones. A positive outcome in Cameroon was the birth of a planning culture which had not been the common practice (DR, KII). The proportion of expenditures received in this domain was almost the same as proposed. However, no funds were spent on coordination activities, which were supposed to make up 26% of the expenditure, while more funds were spent on monitoring and supervision, increases of 133% and 150%, respectively (KII, FA).
In Chad, several factors contributed to the weak management of funds and deviation of expenditures: a serious archiving problem, a lack of institutional memory and high staff turnover, including the appointment of a new HSS manager after a change of the Minister of Health (DR, KII). Most of the funds in Chad were spent on procurement of medicines and vehicles for supervision during a shorter period of time than originally planned, resulting in 38% of actual expenditures having deviated from proposed spending and triggering conflict with Gavi about these expenditures. The proportion of expenditures increased by 160% and 20% for HSS program management and organization and management of health services, respectively. However, no funds were spent on human resources, and expenditures on management of medicine and medical products decreased by 43% (KII, FA).
Figures 2 and 3 show the proposed, planned and actual expenditures of the first HSS disbursements in Cameroon and Chad.
FIGURE 2.

Proposed, planned and actual expenditures of HSS funds, Cameroon, 2007–2011.
FIGURE 3.
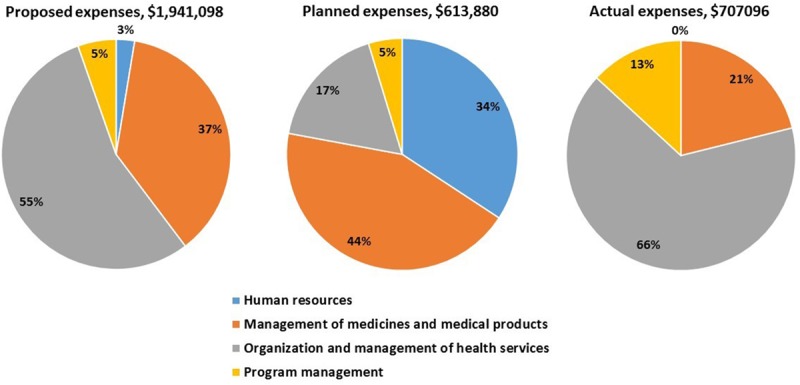
Proposed, planned and actual expenditures of the first HSS funds, Chad, 2008–2010.
Interruption and Reprogramming of Funds
Expenditures detailed in the yearly progress reports led the Gavi Secretariat to conduct a series of independent audits and investigations on the financial management of HSS in both countries. The auditors found irregularities in spending, and consequently, the Gavi Secretariat decided to suspend the funds in both countries, interrupting all ongoing HSS activities. After a period of negotiations, funds were reprogrammed in both countries. In each of the countries, this resulted in more than 2 years of auditing, investigating and reprogramming of funds that required additional human effort and material resources (DR, KII).
In Cameroon, HSS reprogramming occurred once and involved several changes to the way the grant was supposed to strengthen the system and lead to the desired outcomes. During the first stage, activities were focused on governance and leadership of the health system. After reprogramming, activities were focused on service delivery, logistics and demand generation, with most of the funds covering day-to-day operational costs. The changes in the new proposal were based on an assessment of the Expanded Program on Immunization specifically instead of the whole health system. Among governance and leadership activities, one had substantial potential for sustainability: developing a manual or system for financial management of HSS funds (DR, KII).
In Chad, HSS was reprogrammed twice. Although the program’s strategy was retained, with each reprogramming, the focus of activities shifted. Specifically, an increasing number of activities targeted health workforce, logistics and procurement, while activities targeting governance and leadership of the health system were cancelled (DR, KII).
A positive consequence of the suspension and reprogramming of HSS in Chad was that the funds were spent with almost total adherence to the proposed and approved budgets. However, this meant considerable spending on day-to-day operational costs, procurements and service delivery (DR, FA). The use of reprogrammed funds was also inefficient. For example, the majority of the procurements had not yet been distributed by the end of our evaluation, and thus did not reach the point of care. However, it is important to note that the implementation period was still ongoing when the evaluation was conducted (KII, Q).
Delayed Implementation
Implementation of reprogrammed HSS activities was delayed for over a year in both countries for different reasons, including the delay of fund disbursement. Lacking financial management guidelines, Cameroon opted for the financial management of the funds through a third party. A “mirror”‘ team was created within the Ministry of Health with the objective of transferring knowledge to the local team and building the financial management capacity at the Ministry. However, this increased the cost of program management, thereby consuming funds that could have been used to fund additional activities. Further, hiring of the local team was delayed for approximately 2 months, and its members changed during the program implementation. In parallel, Cameroon suffered a poliomyelitis epidemic that required 14 vaccination campaigns managed financially by the same third party. The shortage of staff and capacity at the Ministry of Health meant that the receipts from these campaigns were delayed for almost 3 months. This caused the third party responsible for the financial management of HSS to block all disbursements, including HSS funds, until all receipts were received, which took about 4 months. On the other hand, this situation forced the accounting system at the Ministry to improve, which had the effect of creating a culture of fiscal accountability. In Chad, in addition to reprogramming of funds and 2 delays in disbursement, the Directorate of Planning in charge of HSS management and implementation suffered from staff shortages that slowed the implementation process significantly (DR, KII, Q).
On Sustainability
Sustainability was a challenge in both countries. In Cameroon, the reprogramming resulted in a substantial change to the HSS strategy and an interruption of the planning culture born during the first phase. This interruption resulted from the tensions surrounding the investigations and suspension of HSS before the reprogramming. Further, the change of the local HSS management team during the second implementation phase hindered the capacity built in strengthening the health workforce at the ministry. Even more, by the end of the evaluation, Cameroon had not yet developed a financial management manual to help institutionalize the newly born culture of accountability (DR, KII, Q).
In Chad, governance and management manuals were not developed, as the reprogrammed funds were spent mostly on procurement and daily operational costs which, unlike manuals, require continued funding for maintenance and execution (DR, KII, Q).
In both countries, many HSS activities related to service delivery had no exit plan for their financing. Cameroon and Chad were preparing proposals for a second HSS to continue financing these and additional activities (DR, KII).
DISCUSSION
While others have evaluated different aspects of efficiency and sustainability of Gavi HSS grants, this is the first study to evaluate these 2 domains in relation to bottlenecks by building blocks of the health system. HSS grants in Cameroon and Chad faced some challenges that led to reduced efficiency and perhaps sustainability. As a result, a 5-year program was conducted in 8 years, putting strain on resources and increasing effort. Our findings suggest that these challenges could be avoided through stronger governance and leadership and a more adequate health workforce, hence the importance of prioritizing these 2 building blocks through HSS.
The suboptimal qualifications and shortages in the health workforce, as well as the poor governance and leadership in the 2 countries, limited the efficiency of HSS funds. The deviation in funds allocation has led to several consequences that have also affected efficiency: the implementation extended 3 years beyond the original plan, additional resources were required on the part of the countries and the Gavi Secretariat to investigate the irregular expenditures, reprogram and manage the funds. With the reprogramming, activities with a longer-term health impact were eliminated as well. At the conclusion of Gavi HSS funding, most services were interrupted, and there were no financial plans to support maintenance of procured logistics and equipment. Once again, both countries counted on a second HSS program that was not yet in place to continue funding of activities. This is another failure on the part of all stakeholders with regard to adherence to the Paris declaration for aid effectiveness, which (1) stresses that countries should mobilize their domestic resources and (2) serves as the basis for Gavi’s HSS support.5,32 Unfortunately, specifically in Cameroon, the sustainability problem is more pronounced with the loss of the planning culture born during the first phase, before the suspension of HSS funds. Similarly, the accountability culture born during the implementation of the reprogrammed funds is threatened, as it was not institutionalized through a system that would ensure its continuity.
Many of the hurdles encountered with the HSS grants in Cameroon and Chad could have been avoided if Gavi, the health partners, and country stakeholders had followed more closely the Paris declaration for aid effectiveness, specifically around leadership and governance.32 Under the principles of ownership, alignment and mutual accountability, the declaration requires countries to mobilize their domestic resources, strengthen their fiscal sustainability, publish in a timely manner, provide transparent and reliable reporting on budget execution and take leadership of the public financial management reform process. In parallel, donors are required to respect partner country leadership and help strengthen their capacity to exercise it, rely to the maximum extent possible on transparent partner government budget and accounting mechanisms, disburse aid in a timely and predictable fashion according to agreed schedules and provide timely, transparent and comprehensive information on aid flows. As discussed above, these principles have all been hindered through the design and implementation of HSS in Cameroon and Chad. Gavi has started addressing these issues and, since 2016, has adopted the partners’ engagement framework which stipulates sustainability as a strategic focus area.33 This framework aims to align timelines and planning with country needs to improve vaccine coverage. It leverages targeted technical assistance to strengthen data, supply chain and sustainability. Through 2016, funds from Gavi have enabled partner organizations to strengthen their capacity and provide host countries with continuous support in critical areas.34 The ultimate goal is to transfer skills and strengthen country capacities to manage and implement their programs through their own staff.
Our study is subject to some limitations. First, some important documents were not accessible. Second, a number of KIs who played important roles at the beginning of HSS were not available. Finally, recall bias was also a limitation with some KIs. Nevertheless, our study is based on a mixed methodology that triangulated data from different sources, and allowed us to provide more robust findings and conclusions. Given the mostly-qualitative nature of our methods, we do not measure the robustness of our conclusions from a reliability and validity stand point, but emphasize the richness of our data, the high convergence of themes between KI, and between the different methods, specifically between KII and DR, or the FA. For example, and despite the sensitivity of the HSS interruption topic, in-country KI reported the percent of deviation in expenditure almost exactly to what the FA showed.
For more efficient and sustainable HSS programs, we recommend that countries that are similar to Cameroon and Chad, and are requesting financial support for HSS, phase their HSS activities by first targeting weaknesses in their system’s governance, leadership and health workforce before moving to service delivery and logistics and medical products, especially if no other funds have been secured for the continuity of activities. Once the appropriate norms, rules, leadership/governance and health care workforce are in place, actors of the health system can start acquiring and providing the needed logistics and medical products and services. This will ensure that health care actors follow strong rules and norms, that undesirable trends and distortions will be detected and corrected, that transparent and effective accountability mechanisms will be established, that skilled health workers will be available to deliver services effectively.
In parallel, to ensure that countries design appropriate HSS programs and know the procedures to be followed in the financial management and implementation of HSS, we recommend that the Gavi Secretariat be present throughout the process of selecting activities and implementing the program, alert countries requesting HSS support to the time needed between the approval and the first disbursement of funds and clarify the steps that countries should follow in case of a delay or a division of disbursements in the HSS guidelines and applications.
ACKNOWLEDGMENTS
The authors thank all key informants who participated in this study, as well as Sofia Cababa Wood, for graphics, and Kevin O’Rourke, for copyediting, from the Institute for Health Metrics and Evaluation.
IFORD group includes Hénoque Blaise Nguendo Yongsi, PhD, Julien Guy Ewos Bomba, MD, MPH, Léopold Cyriaque Donfack Mbasso, MD, MPH, Mariane Kenmegni Omgba, PhD, Patrice Tanang Tchouala, MSc, Vivien Meli Meli, PhD, from the Institut de Formation et de Recherche Démographiques, University of Yaoundé II, Yaoundé, Cameroon.
UND group includes Alexis Ngarmbatedjimal, MSc, Haroun Koumakoi, MSc, Djimet Seli, PhD, from the University of N’Djamena, N’Djamena, Chad.
Supplementary Material
Footnotes
Supported by the Gavi, the Vaccine Alliance [PP45680815A4, PO006331].
The authors have no conflicts of interest to disclose.
The authors Mimche and Squires contributed equally to this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (www.pidj.com).
REFERENCES
- 1.Reich MR, Takemi K, Roberts MJ, et al. Global action on health systems: a proposal for the Toyako G8 summit. Lancet. 2008;371:865–869.. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies. 2010WHO. [Google Scholar]
- 3.HLSP. GAVI Health Systems Strengthening Support Evaluation 2009. Mott MacDonald; Report No.: RFP-0006-08. [Google Scholar]
- 4.Storeng KT. The GAVI Alliance and the ‘Gates approach’ to health system strengthening. Glob Public Health. 2014;9:865–879.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gavi Alliance. Health system strengthening support [Internet]. Health system strengthening support. 2016. Available from: http://www.gavi.org/support/hss/. Accessed July 5, 2016.
- 6.Hafner T, Shiffman J. The emergence of global attention to health systems strengthening. Health Policy Plan. 2013;28:41–50.. [DOI] [PubMed] [Google Scholar]
- 7.van Olmen J, Marchal B, Van Damme W, et al. Health systems frameworks in their political context: framing divergent agendas. BMC Public Health. 2012;12:774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adam T, Hsu J, de Savigny D, Lavis JN, Røttingen J-A, Bennett S. Evaluating health systems strengthening interventions in low-income and middle-income countries: are we asking the right questions? Health Policy Plan. 2012;27(suppl_4):iv9–iv19.. [DOI] [PubMed] [Google Scholar]
- 9.Development Assistance Committee. DAC principles for evaluation of development assistance [Internet]. Organization for Economic Co-Operation and Development.. 1991. Available from: https://www.oecd.org/development/evaluation/2755284.pdf. Accessed August 8, 2017.
- 10.Southern California Evidence-based Practice Center - RAND Corporation. Identifying, categorizing, and evaluating health care efficiency measures. 2008 Apr. Rockville, MD: AHRQ; Report No.: 08-0030. [Google Scholar]
- 11.USAID. From aid to investment [Internet]. From aid to investment. 2016. Available from: https://www.usaid.gov/what-we-do/global-health/hiv-and-aids/technical-areas/aid-investment. Accessed July 5, 2016.
- 12.Comite de Coordination Inter-Agences (CCIA). Cameroon Immunization Services, Health System Strengthening and Injection Safety Proposal. 2006. [Google Scholar]
- 13.The government of Cameroon. Provisional proposal for reprogramming based on part 9 of the Annual Progress Report: Cash support for Health System Strengthening Support (HSS). 2013.
- 14.Chad Ministry of Public Health. Chad proposal with a view to obtaining support from the GAVI Alliance for Health System Strengthening (HSS). 2008.
- 15.Chad Ministry of Public Health. Proposal from Chad for Gavi Alliance Support for Health System Strengthening (HSS): Reprogramming of Interventions for the period from January 2013 to June 2014. 2012.
- 16.Ministère de la Santé Publique, Republique du Tchad. Reprogrammation 2,2 Millions GAVI RSS_2014. 2013.
- 17.Centers for Disease Control and Prevention. Data Collection Methods for Evaluation: Document Review [Internet].. 2009. Available from: https://www.cdc.gov/healthyyouth/evaluation/pdf/brief18.pdf. Accessed April 4, 2017.
- 18.Multilateral Organisation Performance Assessment Network. MOPAN common approach: document review guide [Internet]. 2014. Available from: http://www.oecd.org/callsfortenders/MOPAN%202014_Document%20Review%20Guide_Draft_April%201.pdf. Accessed April 4, 2017.
- 19.Polkinghorne M, Arnold A. A Six Step Guide to Using Recursive Abstraction Applied to the Qualitative Analysis of Interview Data [Internet]. 2014. Bournemouth University; Available from: http://eprints.bournemouth.ac.uk/21367/1/ISBN%20978-1-85899-296-9.pdf. Accessed April 4, 2017. [Google Scholar]
- 20.The government of Cameroon. Annual Progress Report 2008. 2009Gavi: The Vaccine Alliance. [Google Scholar]
- 21.The government of Cameroon. Annual Progress Report 2009. 2010Gavi: The Vaccine Alliance. [Google Scholar]
- 22.The government of Cameroon. Annual Progress Report 2010. 2011Gavi: The Vaccine Alliance. [Google Scholar]
- 23.The government of Cameroon. Annual Progress Report 2011. 2012Gavi: The Vaccine Alliance. [Google Scholar]
- 24.The government of Cameroon. Annual Progress Report 2014. 2015Gavi: The Vaccine Alliance. [Google Scholar]
- 25.The government of the Republic of Chad. Annual Progress Report 2008. 2009Gavi: The Vaccine Alliance. [Google Scholar]
- 26.The government of the Republic of Chad. Annual Progress Report 2009. 2010Gavi: The Vaccine Alliance. [Google Scholar]
- 27.The government of the Republic of Chad. Annual Progress Report 2010. 2011Gavi: The Vaccine Alliance. [Google Scholar]
- 28.The government of the Republic of Chad. Annual Progress Report 2013. 2014Gavi: The Vaccine Alliance. [Google Scholar]
- 29.Department of Energy. Root cause analysis guidance document [Internet]. 1992. Available from: https://energy.gov/sites/prod/files/2013/07/f2/nst1004.pdf. Accessed April 4, 2017.
- 30.Rooney JJ, Vanden Heuvel LN. Root cause analysis for beginners [Internet]. 2004. Available from: https://www.env.nm.gov/aqb/Proposed_Regs/Part_7_Excess_Emissions/NMED_Exhibit_18-Root_Cause_Analysis_for_Beginners.pdf. Accessed April 4, 2017.
- 31.Spath PL. Error reduction in health care. In: A Systems Approach to Improving Patient Safety. 20112nd ed San Francisco, CA: John Wiley & Sons, Inc. Jossey-Bass. [Google Scholar]
- 32.Organisation for Economic Co-operation and Development. Paris Declaration on Aid Effectiveness [Internet]. 2005. Available from: http://www.mfdr.org/sourcebook/2-1paris.pdf. Accessed April 5, 2017.
- 33.GAVI, the Vaccine Alliance. Partners’ engagement framework [Internet]. Available from: http://www.gavi.org/support/pef/. Accessed August 21, 2017.
- 34.De Chaisemartin A, Dubois C, Murray-Lopez M, Hansen P. Partners’ engagement framework & alliance accountability framework. 2016. Geneva: Gavi, the Vaccine Alliance; Report No.: 13. [Google Scholar]


