Abstract
Migratory dendritic cell (DC) subsets deliver tissue antigens to draining lymph nodes to either initiate or inhibit T cell-mediated immune responses. The signals mediating DC migration in response to tissue self antigen are largely unknown. Using a mouse model of inducible skin-specific self antigen expression, we demonstrate that CD103+ dermal DCs (DDCs) rapidly migrate from skin to skin-draining lymph nodes (SDLNs) within the first 48 hours after antigen expression. This window of time was characterized by the preferential activation of tissue-resident antigen-specific effector T cells (Teffs), with no concurrent activation of antigen-specific Teffs in SDLNs. Using genetic deletion and adoptive transfer approaches, we show that activation of skin-resident Teffs is required to drive CD103+ DDCs migration in response to tissue self antigen and this Batf3-dependent DC population is necessary to mount a fulminant autoimmune response in skin. Conversely, activation of antigen-specific Teffs in SDLNs played no role in DDC migration. Our studies reveal a crucial role for skin-resident T cell derived signals, originating at the site of self antigen expression, to drive DDC migration during the elicitation phase of an autoimmune response.
Introduction
The maintenance of immune homeostasis is dependent on the ability of tissue-resident immune cells to recognize and adequately respond to both foreign and self antigens. The skin is continuously exposed to exogenous and endogenous antigens and harbors a relatively high number of tissue-resident immune cells, largely composed of dendritic cells (DCs) and T cells (1, 2). Tissue residing DCs predominantly operate at the interface between innate and adaptive immunity, either promoting anti-pathogen immunity or facilitating tolerance to tissue antigens, both of which require their initial migration to tissue draining lymph nodes.
Migration of DCs from tissues is essential for presentation of tissue-derived antigens to T cells in secondary lymphoid organs. The mechanisms that govern DC migration under inflammatory contexts has been extensively studied (reviewed in (3)). Epidermal resident Langerhans cells (LC), characterized by expression of the C type Lectin CD207 (Langerin), are anchored to epithelial keratinocytes through E-cadherin–containing tight junctions, rendering them non-motile. Upon activation, LCs detach from keratinocytes via downregulation of E-cadherin and begin to upregulate CCR7 (4–6). While this pathway does not play a role in LC translocation from epidermis to dermis, CCR7 is required for the mobilization of all skin DC subsets towards terminal lymphatics (7). Following epicutaneous immunization, activated dermal DCs (DDC) arrive first to skin draining lymph nodes (SDLNs), and localize to distinct areas relative to slower migrating LCs (8). Recent evidence suggests that migratory LCs promote the maintenance of peripheral tolerance through deletion of self-reactive T cells, induction of regulatory T cell (Tregs) and promotion of IL-10 secretion (9–11). In contrast, dermal Langerin-expressing CD103+ DCs are specialized for cross-presentation of viral antigens, as well as uptake and delivery of Staphylococcus epidermidis derived antigens from skin to SDLNs for efficient induction of antigen-specific IL-17 producing CD8+ T cells (12–15). While many studies have addressed the functional specialization of migratory DC populations in response to viral, bacterial or allergic immune responses, the role of DC subsets in the early response to tissue self antigen and the signals that drive DC emigration from tissues during the initiation of an autoimmune response are less well defined.
To begin to address this, we utilized a previously established experimental model of skin autoimmunity. In this system, a model self antigen (ovalbumin, Ova), can be inducibly expressed in keratinocytes, resulting in a productive antigen-specific T cell-mediated immune response (16–18). The long-term kinetics of T cell recruitment, activation and regulation have been well characterized in this system, while the contribution of the major skin DC populations have not been assessed. This model of inducible and restricted Ova expression in epithelial cells permits detailed analysis of the accumulation and migratory behavior of different DC populations in the early events immediately following self antigen expression in skin. Herein, we report the observation of a robust and mass emigration of CD103+ DDCs from skin to SDLNs as early as 48h post-initiation of self antigen expression. Activation of skin resident, but not SDLN resident, antigen specific T cells coincided precisely with the rapid departure of CD103+ DDCs from skin. We further demonstrate that tissue resident T cells, but not SDLN resident T cells, are necessary for DDCs exit from the tissue early upon self antigen expression. These results elucidate a fundamental property of tissue-resident T cells and suggest that they play a role in shaping the migratory behavior of tissue DCs during the initiation phase of an autoimmune response.
Materials and Methods
Mice
TRE-TGO mice were crossed with K5-rtTA mice to generate mice with inducible epidermal expression of Ova. The TGO construct encodes a fusion protein linking the transferrin receptor transmembrane domain, GFP, and aa 230–359 of chicken ovalbumin. To create K5/TGO/DO11 mice, K5-rTA/TRE-TGO mice were crossed onto the DO11.10 TCR-transgenic background, as described (18). To induce expression of the TGO transgene, K5/TGO/DO11 mice were starved from all chow for 12 hours and then maintained on 1gm/kg doxycycline chow (i.e. Day 0) until sacrifice on day 2. Batf3−/− mice were purchased from The Jackson Laboratories and were bred in-house. A 16-point clinical scoring scale was utilized to quantify skin disease. Scaling, alopecia, loss of activity, and erythema were each given a score from 0 to 4. Individual scores were summed and mean scores per group are displayed. Hosts for adoptive transfer experiments were created by crossing K5/TGO mice with T cell receptor-alpha-deficient mice (TCRα−/−) on the Balb/c background. For adoptive transfer of DO11 T cells, DO11.10 TCR-transgenic mice were crossed onto Rag2−/−/CD90.1+ background. All mice were bred and maintained in a specific pathogen-free facility in accordance with the guidelines of the Laboratory Animal Resource Center of the University of California San Francisco. All mice used in experiments were socially housed under a 12 hr light/dark cycle.
Flow cytometry
Preparation of single cell suspensions from SDLNs or full thickness skin for flow cytometry was performed as previously described (19). In brief, isolation of cells from axillary, brachial and inguinal lymph nodes (referred to as skin draining lymph nodes, SDLNs) for flow cytometry was performed by mashing tissue over 100 µm sterile filters. For all experiments, an equal area of mouse dorsal skin was harvested (~2 cm×3 cm). All experiments were designed such that negative and positive control groups were always included in parallel and in most cases data were not pooled between independent mouse harvests. For isolation of dorsal skin cells, mouse dorsal skin was harvested and lightly defatted. It was then minced finely with scissors and re-suspended in 3 ml of digestion mix (composed of 2mg/ml collagenase XI, 0.5mg/ml hyaluronidase and 0.1mg/ml DNase in RPMI with 1% Hepes, 1% penicillin-streptomycin and 10% fetal calf serum), followed by incubation in a shaking incubator at 37° C at 250 rpm for 1 hour. Single cell suspensions were then pelleted and re-suspended in PBS for cell counting and staining. The following antibodies were used for flow cytometry staining: Foxp3 eFluor 450, CD25 APC-eFluor 780, CD45 Alexa Fluor 700, MHC Class II (I-A/I-E) eFluor 450, Langerin (L31) PE, CD103 APC, KJ (DO11 TCR) FITC, and PD-1 PE-Cy7 (all from eBioscience); Brilliant Violet 605 CD8a, Brilliant Violet 650 CD4, Brilliant Violet 711 CD11b, Brilliant Violet 650 CD11c, and CD69 APC (all from BioLegend), CD3 PerCP, Purified Rat Anti-Mouse CD16/CD32, B220 PercP, CD11b FITC, CD90.1 PerCP, CD90.2 FITC, and MHC Class II (I-A/I-E) BV421 (all from BD Pharmingen); Ghost Dye Violet 510 Live/Dead Stain (Tonbo Biosciences).
Blockade of SDLN T cell egress
FTY720 (Selleck Chemicals) was dissolved in normal saline and administered to mice via intraperitoneal injection at a dose of 10 mg/kg on days -2, -1, and day 1. Control mice (age-matched littermates) were treated with equal volumes of normal saline according to the same schedule. All mice were harvested on day 2 for analysis of skin and SDLNs by flow cytometry.
In Vivo MHC Class II blockade
InVivoMAb anti-mouse MHC Class II (I-A/I-E) blocking antibody (clone M5/114) was purchased from BioXcell (West Lebanon, NH, USA). 250 µg was administered i.p on days -2, -1, and day 1. Mice were administered Doxycycline chow on day 0 and tissues harvested on day 2.
Adoptive transfer of T cells
Single cell suspensions from lymph nodes of DO11/Rag2−/−/CD90.1+ (i.e., DO11 T cells) mice were prepared and 2×106 LN cells adoptively transferred intravenously into gender-matched K5/TGO/TCRα−/− recipient mice, and mice were started on doxycycline chow the same day as adoptive transfer.
Statistical analyses
Statistical analyses were performed with Prism software package version 6.0 (GraphPad). P values were calculated using two-tailed unpaired or paired Student’s t-test. Sample size for animal experiments was determined based upon pilot experiments. Mice cohort size was designed to be sufficient to enable accurate determination of statistical significance. No animals were excluded from the statistical analysis, unless due to technical errors. Mice were randomly assigned to treatment or control groups, while ensuring inclusion criteria based on gender and age. Appropriate statistical analyses were applied, assuming a normal sample distribution. All in vivo experiments were conducted with at least two independent cohorts (as indicated in figure legends).
Results
CD103+ DDCs rapidly emigrate from skin in response to cutaneous self antigen expression
The experimental model of inducible self antigen expression we have developed comprises three transgenes (18). The first expresses membrane bound ovalbumin (Ova) under the control of a tetracycline response element, termed ‘TGO’, and the second carries a tetracycline transactivator driven by the keratin-5 (K5) promoter. These mice were further crossed with the DO11.10 T cell receptor (TCR)-transgenic strain. In the resultant K5/TGO/DO11 mice, expression of antigen in K5 expressing basal keratinocytes is dependent on administration of the tetracycline analog, doxycycline (Dox) (Fig. 1A). We have previously defined functional Ova expression in the thymus of K5/TGO/DO11 triple transgenic mice. Deletion of CD4+ DO11 T cells and increased production of Foxp3+CD4+DO11 regulatory T cells (Tregs) in K5/TGO/DO11 mice is a sensitive indicator of thymic Ova expression. K5/TGO/DO11 triple transgenic mice as well as TGO/DO11 double transgenic mice have modest deletion of CD4+ DO11 cells and a pronounced increase in DO11 Treg cells in the thymus, skin draining lymph nodes (SDLNs) and skin. Expression of Ova in this system largely mimics the pattern of tissue-restricted self antigen expression due to its constitutive expression in the thymus and tightly regulated induction in skin (16–18).
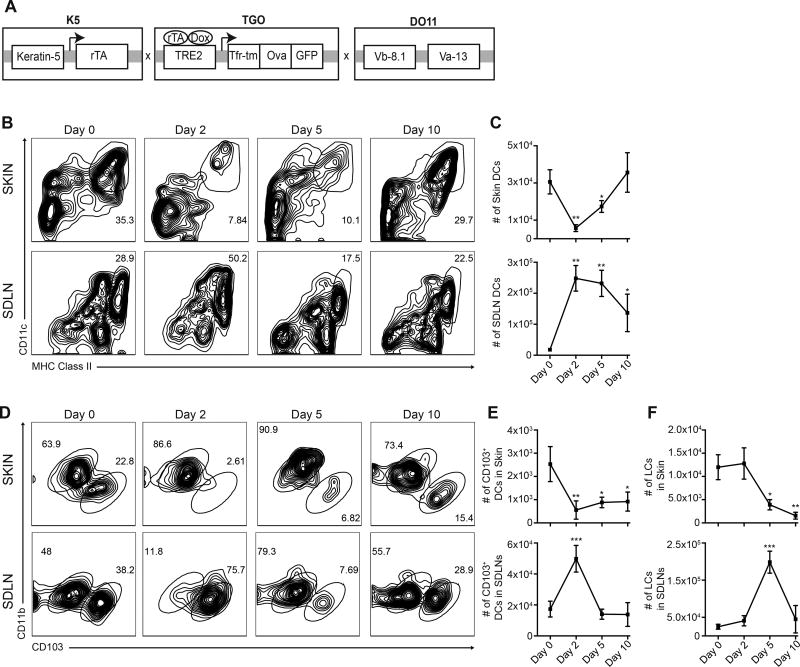
Figure 1. CD103+ DDCs rapidly emigrate from skin upon induction of self antigen expression.
(A) Construct for triple transgenic mice expressing ovalbumin (Ova) driven by the Keratin-5 promoter in a tetracycline inducible fashion. Mice were further crossed to the D011.10 T cell receptor (TCR)-transgenic strain to generate the K5/TGO/DO11 model. (B) Representative flow cytometric plots and (C) quantification of DC profiling in skin and skin draining lymph nodes (SDLNs) during the first 10 days after induction of antigen expression. (D) Representative flow cytometric plots and (E) quantification of CD103+ DDCs and (F) Langerhans cells (LCs) in skin and SDLNs. One representative experiment of four is shown. Data are mean ± s.e.m. ns = no significant difference. *P<0.05, **P<0.01 ***P<0.001, One-way ANOVA, day 0 vs, other time points (B, D, E).
We have previously demonstrated that induction of antigen expression in the epidermis results in a pronounced T cell dependent autoimmune dermatitis that peaks at 10 days (18). In order to determine how skin DCs respond to antigen expression in this model, we began by first defining the kinetics of total DC accumulation in skin and SDLNs by flow cytometry during the early window of time following Ova induction. In skin, DCs were identified as live, CD45Pos CD3neg CD8neg B220neg Class-IIPos CD11cPos cells, while migratory DCs present in SDLNS were defined as Class-IIHigh CD11cHigh cells, markers that have been previously shown to reliably distinguish migratory DCs from lymphoid resident DCs (20). Full gating strategies are shown in Supp Fig. 1. Within 2 days of initiation of Ova expression, we observed a significant reduction in the total number of DCs present in skin with a concomitant accumulation of migratory DCs in SDLNs (Fig. 1B & 1C), suggesting that these cells rapidly exit the skin upon initiation of self antigen expression in the epidermis. Migratory DC numbers gradually decreased in SDLNs with a concomitant re-accumulation in skin, returning to baseline levels in the tissue by day 10 (Fig. 1B & 1C). In skin, both CD103+ DDCs and epithelial resident LCs are found closely localized to keratinocytes residing in the basal layer of murine epidermis (21, 22). We examined the presence of these two subsets early after induction of antigen. Epidermal LCs and migratory LCs in SDLNs were identified in the DC gate as LangerinPos CD11bHigh CD103neg cells, while CD103+ DDCs were defined as LangerinPos CD11bLow CD103Pos cells (Supp Fig. 1). Strikingly, we observed a mass emigration of CD103+ DDCs from skin as early as day 2, with a ~4-fold reduction in the skin at this time point (Fig. 1D). The corresponding migratory CD103+ population accumulated in SDLNs at the same time point where their numbers initially peaked and returned to baseline thereafter (Fig. 1D & 1 E). In contrast, the absolute number of LCs present in both compartments was unchanged during this early time period (Fig. 1E). LCs exited the tissue with slightly delayed kinetics, as shown by an appreciable reduction in their absolute numbers in the tissue at day 5 post-antigen induction and a significant increase in their migratory counterparts in SDLNs (Fig. 1E). While the absolute number of Langerinneg DCs was also reduced in the skin at day 2 post-antigen induction, this represented a less marked emigration relative to CD103+ DDCs (Supp Fig. 2A & B). Similarly, the absolute number of SDLN resident DCs, characterized as CD11cHigh MHC Class IIIntermediate, remained unchanged during the first 48 hours post-antigen induction. While their numbers declined modestly thereafter, this failed to reach statistical significance (Supp Fig. 2C). These results demonstrate that CD103+ DDCs preferentially and rapidly exit the tissue early upon self antigen expression in skin.
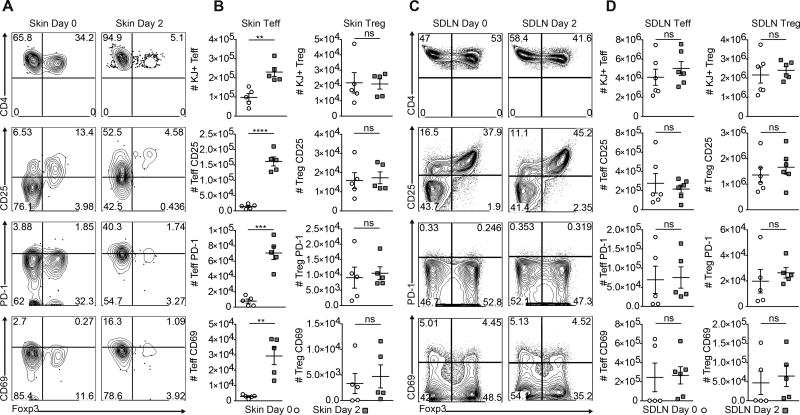
Activation of Skin resident T cells precedes that of SDLN T cells
Given the specialized ability of migratory CD103+ DDCs in eliciting functional responses to skin antigens (12–15), we attempted to elucidate the cellular signals that drive the mass emigration of this population. Importantly, this phenomenon occurs at a time point where we have previously been unable to detect any signs of clinical or cellular inflammation in skin (16–18). However, during the autoimmune response to Ova in K5/TGO/D011 mice, we have observed by immunofluorescent tissue staining of skin (17) that effector DO11 T cells localize close to CD11c+ cells diffusely throughout the dermis. This led us to hypothesize that T cells may be involved in facilitating the early migration of CD103+ DDCs upon antigen expression. We have previously characterized the T cell activation status in these mice over a long time-course (18), but not during the first 48 hours of Ova expression, when CD103+ DDCs exit skin. Antigen specific DO11 T cells were gated as SingletPosLivePosCD3PosCD4PosKJPos and then Foxp3Neg or Foxp3Pos for Teff and Treg cells, respectively. Comprehensive phenotypic analysis of DO11 T cells in skin on day 0 (i.e., no Dox treatment) and 2 days after initiation of antigen induction, revealed a 2-fold expansion of Foxp3 negative Teff cells with no change in the number of Foxp3 expressing Tregs (Fig. 2A & 2B). In addition, the activation status of skin DO11 cells, as evidenced by CD25, PD-1 and CD69 expression, revealed a significant up-regulation of all these markers in Teffs but not Tregs (Fig. 2A & 2B). In contrast, analysis of antigen-specific DO11 cells in SDLNs between day 0 and day 2 showed no differences in the absolute numbers of Teffs and Tregs. In addition, there was no evidence of activation of either of these populations (Fig. 2C & 2D). These results suggest that early after expression of self antigen in skin, antigen-specific Teffs are preferentially activated in the tissue with no evidence of activation of these cells in tissue-draining LNs.
Figure 2. Activation of skin resident T effector cells (Teffs) precedes that of SDLN Teff cells.
(A) Representative flow cytometric plots and (B) quantification of Teff and regulatory T cells (Tregs) in skin and skin draining lymph nodes (SDLNs) of K5/TGO/DO11 mice during the first 2 days of antigen expression. (C) Representative flow cytometric plots and (D) quantification of Teff and Treg cells in SDLNs. One representative experiment of three is shown. ns = no significant difference. Data are m-ean ± s.e.m. **P<0.01 ***P<0.001, ****P<0.0001, Student’s unpaired t-test (B, D).
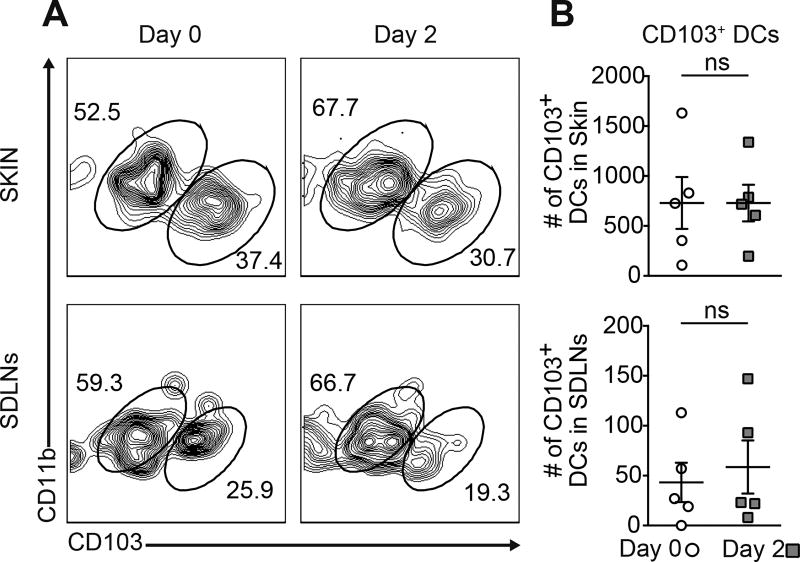
CD103+ DDCs fail to emigrate from skin in the absence of antigen specific T cells
Given the accumulation and robust activation of skin resident antigen-specific Teffs and the concurrent exit of CD103+ DDCs early after antigen induction, we sought to determine if T cells are required for DC emigration from skin. To this end, we utilized K5/TGO mice crossed onto a T cell receptor alpha-deficient (TCRα−/−) background to generate K5/TGO/TCRα−/− mice. In this model, administration of Dox will induce antigen expression in the absence of functional TCRα-expressing T cells, allowing characterization of CD103+ DDCs migration from skin in the absence of these cells. In K5/TGO/TCRα−/− mice, absolute numbers of CD103+ DDCs in both skin and SDLNS were unchanged between day 0 and day 2 post-Ova induction (Fig. 3). These results suggest that T cells are required for the migration of CD103+ DDCs early during the response to tissue self antigen.
Figure 3. T cells are required for CD103+ DDCs migration.
(A) Representative flow cytometric plots and (B) quantification of CD103+ DDCs in skin and SDLNs of K5/TGO/ TCRα−/− mice on day 0 and day 2 post antigen expression. One representative experiment of three is shown. ns = no significant difference. Data are m-ean ± s.e.m, Student’s unpaired t-test (B).
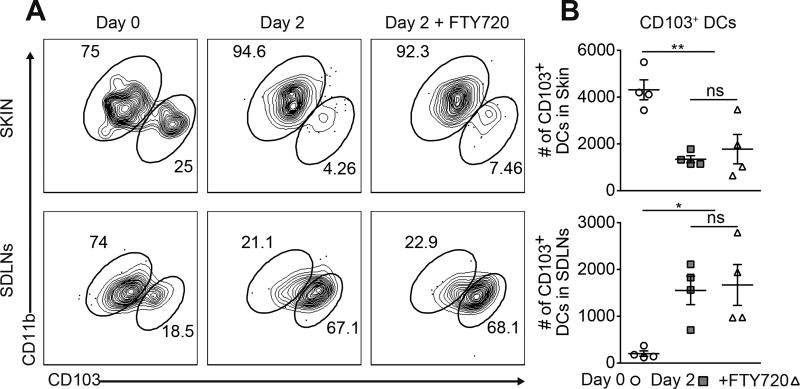
The migratory ability of CD103+ DDCs is dependent on the presence of skin resident T cells
The preferential activation of T cells in the tissue relative to SDLNs and the failure of DCs to migrate in T cell deficient mice, suggested that skin resident antigen-specific T cells might be the dominant drivers of CD103+ DDCs emigration from skin early after expression of tissue self antigen. To test the hypothesis that the accumulation of activated antigen-specific T cells in skin was not a result of a migratory T cell wave from secondary lymphoid organs, K5/TGO/DO11 mice were treated with the sphingosine 1-phosphate receptor antagonist, FTY720, from day -2 to day 1 post-antigen induction. FTY720 potently inhibits lymphocyte egress from lymphoid organs (23). In these experiments, CD103+ DDCs in FTY720 treated mice rapidly exited the tissue and accumulated in the SDLNS with similar kinetics to that observed in non-FTY720 treated animals (Fig. 4A). Furthermore, the absolute number of CD103+ DDCs in skin and SDLNs of FTY720-treated mice were equivalent to control mice on day 2 post-antigen induction (Fig. 4B), demonstrating that these cells retained the ability to emigrate from skin in the presence of FTY720. These results suggest that T cell egress from secondary lymphoid organs is not required for DDC tissue emigration, suggesting that tissue resident T cells may be the major drivers of this phenomenon.
Figure 4. Blockade of T cell egress from secondary lymphoid organs has no effect on CD103+ DDCs emigration from skin.
(A) Representative flow cytometric plots and (B) quantification of CD103+ DDCs in skin and SDLNs of K5/TGO/DO11 mice on day 0 and day 2 post-antigen expression in the presence or absence of FY720. One representative experiment of two is shown. Data are mean ± s.e.m. ns = no significant difference. *P<0.05, **P<0.01, One-way ANOVA (B).
Given that blockade of T cell egress from SDLN does not impact the migration of CD103+ DDCs from skin, we next sought to determine if the exclusive presence of T cells in the SDLNs (with relative absence in skin) was sufficient to promote DDC emigration. To this end, we utilized an adoptive transfer approach. Antigen specific T cells were isolated from CD90.1/DO11/Rag−/− mice (referred to as “DO11 cells”) and transferred intravenously into K5/TGO/ TCRα−/− hosts. Upon transfer, these cells stably engraft in secondary lymphoid organs well before they can be detected in skin (Fig 5A). Two days after adoptive transfer into K5/TGO/ TCRα−/− hosts, DO11 T cells (defined as CD90.1Pos CD4Pos KJPos) were readily detectable in SDLNs but undetectable in skin (Fig, 5A–B). Previous studies with this model have shown that DO11 cells begin to seed the skin no earlier than 5 days after Ova induction (16, 17), allowing a window for residence of antigen-specific DO11s exclusively in secondary lymphoid organs (and not in peripheral tissues). Activation profiling of adoptively transferred DO11 cells in the SDLNs on day 2 post-antigen induction showed no differences in the expression of PD-1, CD44 or CD69 between the Dox treated group and control mice that did not receive Dox (Fig. 5C). These results are consistent with the lack of SDLN T cell activation observed in the K5/TGO/DO11 model on day 2 post-antigen expression (Fig 2C & 2D). Notably, analysis of CD103+ DDCs revealed no changes in the absolute cell numbers of this population in both skin and SDLNs during this window of time (Fig. 5D & 5E), indicating a relative inability of these cells to emigrate from skin in this setting. Taken together, these findings suggest that T cell egress from SDLNs or the simple presence of antigen-specific T cells exclusively in secondary lymphoid organs is insufficient to drive migration of CD103+ DDCs from skin to SDLNs early after induction of tissue self antigen expression.
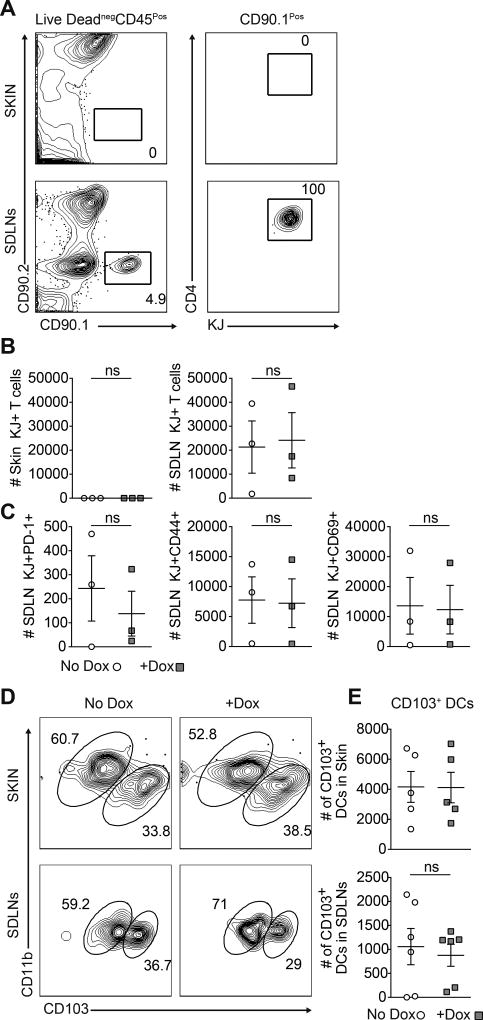
Figure 5. The presence of antigen-specific T cells in SDLNs is insufficient to drive CD103+ DDCs emigration from skin.
(A) Representative flow cytometric plots and (B) quantification of adoptively transferred DO11 cells in the skin and SDLNs of No Dox controls and Dox treated K5/TGO/TCRα−/− mice on day 2. (C) Quantification of activation marker expressing DO11 cells in the SDLNs. (D) Representative flow cytometric plots and (E) quantification of CD103+ DDCs in the skin and SDLNs of No Dox controls and Dox treated K5/TGO/ TCRα−/− mice on day 2. One representative experiment of three is shown. ns = no significant difference. Data are mean ± s.e.m, Student’s unpaired t-test (B. C, E).
The migratory ability of CD103+ DDCs is partially dependent on the MHC Class II pathway
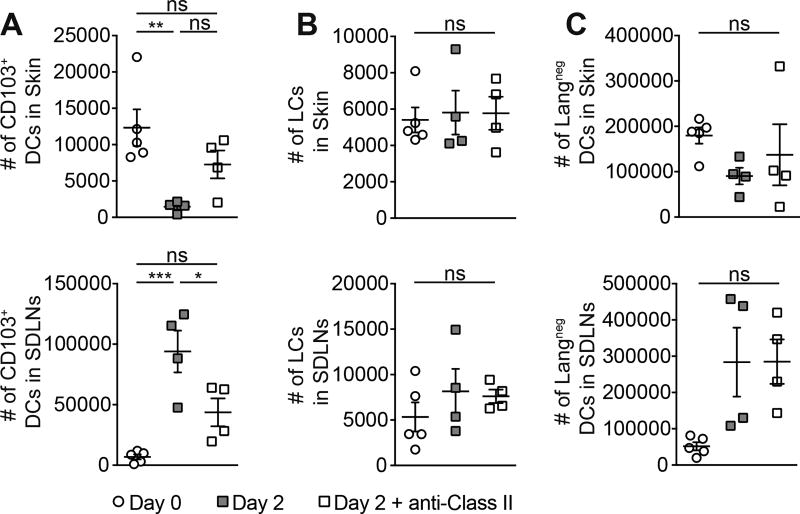
The requirement of skin resident T cells to induce CD103+ DDCs efflux suggested that prototypical cell surface interactions between the TCR and DC-expressed MHC class II may be an important driving factor. Also, given the rapid migration of CD103+ DDCs, we wanted to determine if innate-derived sensing or recognition through the antigen receptor plays a dominant role in the response to cutaneous self antigen expression in this defined time period. We therefore utilized an in vivo anti-MHC class II antibody blocking approach to assess the migratory ability of CD103+ DDCs during the first 2 days following induction of skin antigen expression. Under these conditions, the migratory ability of CD103+ DDCs was partially abrogated in skin, and was reflected in their reduced accumulation in SDLNs relative to control mice not receiving anti-MHC Class II antibody (Fig. 6A). In contrast, the numbers of LCs and Langerinneg DCs was unchanged in skin and SDLNs in the presence or absence of MHC Class II blockade (Fig. 6B &-6C). Partial abrogation of CD103+ DDC migration, but not other skin DC subsets, suggests that antigen-specific recognition through the MHC class II pathway plays a role in the induction of CD103+ DDC mobilization during the first 48 hours post-tissue self antigen expression. Because blockade of the MHC class II pathway only partially abrogated DDC migration, other signals may be required to synergize with antigen recognition in driving the migration of these cells from skin.
Figure 6. Emigration of CD103+ DDCs is partially MHC-Class II dependant.
Quantification of (A) CD103+ DDCs and (B) Langerhans cells (LCs), and (C) Langerinneg DCs in skin and skin draining lymph nodes (SDLNs) of K5/TGO/DO11 mice at day 0 or day 2 with and without anti-MHC Class II antibody blockade. One representative experiment of two is shown. Data are mean ± s.e.m. ns = no significant difference. *P<0.05, **P<0.01, ***P<0.001, One-way ANOVA.
Batf3-dependent DDCs play a major role in mediating skin inflammation
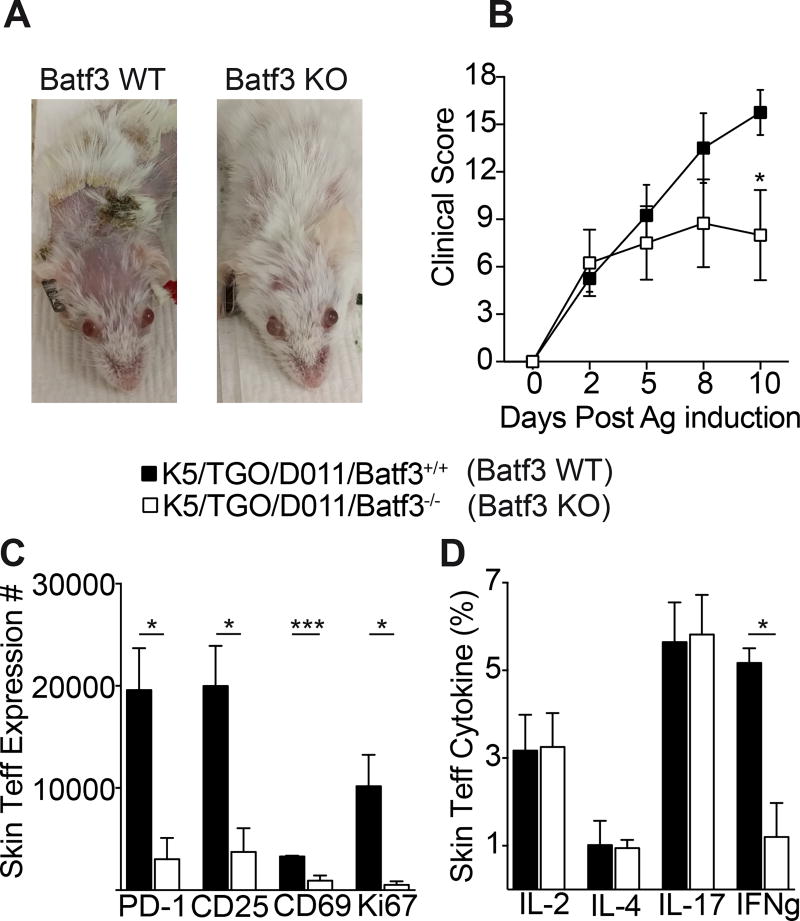
To determine if Batf3-dependant CD103+ DDCs play a functional role in the response to cutaneous self antigen, K5/TGO/DO11 mice were crossed onto a Batf3−/− background. These mice lack CD103+ DCs (24). This allowed us to generate K5/TGO/DO11/Batf3−/− (Batf3 KO) and control K5/TGO/DO11/Batf3+/+ (Batf3 WT) mice. Induction of cutaneous Ova expression in Batf3 WT mice resulted in a pronounced inflammatory dermatitis, peaking by day 10 (Fig. 7). Disease was characterized and scored by the development of erythema, scaling, and alopecia (Fig. 7A). In Batf3 KO mice, disease induction in the first five days was similar to Batf3 WT mice, whereas clinical severity was significantly attenuated by day 10 post-antigen expression (Fig. 7A).
Figure 7. Batf3-dependent DDCs play a major role in mediating skin inflammation.
(A) Representative clinical photos at day 10 and (B) clinical scoring of control K5/TGO/DO11/Batf3+/+ (Batf3 WT) and K5/TGO/DO11/Batf3−/− (Batf3 KO) mice. Skin Teff cell (C) quantification of PD-1, CD5, CD69, and Ki67 expression, and (D) cytokine expression in Batf3 WT and Batf3 KO mice at day 10 post antigen induction. One representative experiment of two is shown. Data are mean ± s.e.m. *P<0.05, ***P<0.001, Two way ANOVA (B), One-way ANOVA (C and D).
Attenuated severity of disease in Batf3 KO mice was associated with a reduction in the absolute number of PD-1, CD25, CD69, and Ki67 expressing antigen specific Teff cells in skin (Fig. 7C). In addition, Teff production of the cytokine IFN-gamma, but not IL-2, IL-4, or IL-17, was significantly reduced in Batf3 KO mice relative to control Batf3 WT mice (Fig. 7D). Taken together, these results indicate that CD103+ DDCs play a major role for antigen-specific T cell activation and the development of fulminant skin inflammation in our model.
Discussion
To permit efficient induction of an acquired immune response, non-lymphoid tissue resident DCs not only need to undergo a sequence of functional maturation, but also must relocate from peripheral tissues to tissue-draining lymph nodes. By virtue of their migratory potential and specialized capacity to acquire and process tissue derived antigens, DCs efficiently direct the primary antigen specific T cell response. Studies on the pathways responsible for DC mobilization from peripheral tissues have focused on experimental models of inflammation, but to date, none have elucidated the cellular signals that drive DC migration upon expression of a tissue self antigen. To our knowledge, we demonstrate for the first time a requirement of activated antigen-specific CD4+ T cells to be present in the tissue to drive the emigration of CD103+ DDCs during the initiation of skin autoimmunity. Interestingly, this occurs at an early time point post-epidermal antigen induction where there are no signs of clinical or cellular inflammation in the tissue. This suggests that the classical signals promoting the morphological and phenotypic changes associated with DC migration, such as activation induced via the Toll like Receptor pathway or cytokine-induced MHC Class II up-regulation, may not be the primary drivers of CD103+ DDC emigration from skin. In the context of OVA infection of the female reproductive tract (FRT), re-activated antigen specific CD8+ T resident-memory (TRM) cells are required for triggering local DC maturation, as evidenced by induced expression of costimulatory molecules CD80, CD86, CD40, as well as the lymphoid organ homing receptor CCR7 (25). This effect was largely attributed to CD8+ TRM-derived TNF-alpha in the FRT. While this study did not determine the contribution of tissue resident CD8+ cells during an autoimmune response nor directly assess the migratory ability of activated DCs in the FRT, it is highly suggestive that the presence of cognate-antigen specific T cells at tissue sites can serve as potent modulators of the immune response to tissue antigen. Our study also raises the notion that the early activation of tissue-resident CD4+ dermal T cells may represent local sensing of previously encountered antigens other than self antigens (i.e., commensal microbes or foreign pathogens) that precipitate innate-like signals to draw circulating effector T cells into the cutaneous microenvironment.
More recently, it has been demonstrated that DDCs can form clusters with effector T cells in perivascular areas of the dermis upon epicutaneous antigen challenge (26). Accordingly, we demonstrate that tissue resident antigen-specific T cells are necessary for DC flux shortly after tissue self antigen expression, and do so in an MHC-Class II dependent manner. Whether dermal T cell-DC clusters are an essential structure for eliciting DC migration and autoimmunity in skin is yet to be determined. This also raises the question of whether or not T cells, or a subset thereof, residing in other tissue sites also have the capacity to regulate migratory DC mobilization in the face of self antigen induction.
To control the development of autoimmunity, multiple mechanisms of peripheral tolerance are present, including both activating and inhibitory T cell costimulatory pathways. By definition, costimulatory ligands expressed on antigen presenting cells (including DCs) engage their cognate receptors on T cells, the result of which dictates T cell differentiation and function. The costimulatory pathway consisting of the programmed death-1 (PD-1) receptor and its ligands, PD-L1 and PD-L2, delivers inhibitory signals that regulate T cell activation, tolerance and immune-mediated tissue damage. This pathway exerts critical inhibitory functions in the context of persistent antigen expression, such as that occurring during chronic infections (27–30). We have previously shown in the K5/TGO/DO11 model that the single best indicator of a self antigen experienced tissue resident T cell is the upregulation of PD-1. In this study, we also demonstrate that as early as 2-days post-antigen induction, antigen-specific T cells in the skin increase expression of PD-1, while its expression is unchanged in the SDLNs, suggesting that tissue T cell recognition of self antigen precedes that of secondary lymphoid residing T cells. Whether or not the PDL1-PD-1 pathway is functionally relevant for DC-T cell interactions, and thus DC migration in this system, is yet to be determined.
In addition to self antigen induced migration, the homeostatic signals that mediate DC trafficking from peripheral tissues in the steady-state is poorly understood. It will be important to determine if cutaneous T cells are also involved in the regulation of DC migration in this context, as well as in tissue sites other than skin. Elucidating the molecular pathways governing tissue resident T cell-induced DC migration will be critical, as these may provide novel avenues for targeting the T cell priming stage of autoimmune disease.
Supplementary Material
Acknowledgments
We thank C. Benetiz for assistance with animal husbandry.
Funding Sources:
Flow Cytometry data was generated in the UCSF Parnassus Flow Cytometry Core which is supported by the Diabetes Research Center (DRC) grant, NIH P30 DK063720. N.A. received support as a Marie Curie International Outgoing Fellow: FP7-PEOPLE-2012-IOF, Project No. 327244. This work was primarily funded by M.D.R. grants: NIH K08-AR062064, Burroughs Wellcome Fund CAMS-1010934, NIH DP2-AR068130, NIH R21-AR066821, Scleroderma Research Foundation grant, a National Psoriasis Foundation Translational Grant and a Dermatology Foundation Stiefel Scholar Award in Autoimmune & Connective Tissue Diseases.
Footnotes
Author Contributions:
N.A. designed the studies, performed the experiments, analyzed the data, and wrote the manuscript. B.Z, H.T, and M.M. assisted with mouse experiments. I.K.G and A.K.A. were involved in study design. M.D.R. oversaw all study design, data analysis, and manuscript writing.
References
- 1.Malissen B, Tamoutounour S, Henri S. The origins and functions of dendritic cells and macrophages in the skin. Nat. Rev. Immunol. 2014;14:417–428. doi: 10.1038/nri3683. [DOI] [PubMed] [Google Scholar]
- 2.Clark RA, Chong B, Mirchandani N, Brinster NK, Yamanaka K-I, Dowgiert RK, Kupper TS. The vast majority of CLA+ T cells are resident in normal skin. J. Immunol. Baltim. Md 1950. 2006;176:4431–4439. doi: 10.4049/jimmunol.176.7.4431. [DOI] [PubMed] [Google Scholar]
- 3.Worbs T, Hammerschmidt SI, Förster R. Dendritic cell migration in health and disease. Nat. Rev. Immunol. 2017;17:30–48. doi: 10.1038/nri.2016.116. [DOI] [PubMed] [Google Scholar]
- 4.Borkowski TA, Van Dyke BJ, Schwarzenberger K, McFarland VW, Farr AG, Udey MC. Expression of E-cadherin by murine dendritic cells: E-cadherin as a dendritic cell differentiation antigen characteristic of epidermal Langerhans cells and related cells. Eur. J. Immunol. 1994;24:2767–2774. doi: 10.1002/eji.1830241129. [DOI] [PubMed] [Google Scholar]
- 5.Jakob T, Udey MC. Regulation of E-cadherin-mediated adhesion in Langerhans cell-like dendritic cells by inflammatory mediators that mobilize Langerhans cells in vivo. J. Immunol. Baltim. Md 1950. 1998;160:4067–4073. [PubMed] [Google Scholar]
- 6.Schwarzenberger K, Udey MC. Contact allergens and epidermal proinflammatory cytokines modulate Langerhans cell E-cadherin expression in situ. J. Invest. Dermatol. 1996;106:553–558. doi: 10.1111/1523-1747.ep12344019. [DOI] [PubMed] [Google Scholar]
- 7.Weber M, Hauschild R, Schwarz J, Moussion C, de Vries I, Legler DF, Luther SA, Bollenbach T, Sixt M. Interstitial dendritic cell guidance by haptotactic chemokine gradients. Science. 2013;339:328–332. doi: 10.1126/science.1228456. [DOI] [PubMed] [Google Scholar]
- 8.Kissenpfennig A, Henri S, Dubois B, Laplace-Builhé C, Perrin P, Romani N, Tripp CH, Douillard P, Leserman L, Kaiserlian D, Saeland S, Davoust J, Malissen B. Dynamics and function of Langerhans cells in vivo: dermal dendritic cells colonize lymph node areas distinct from slower migrating Langerhans cells. Immunity. 2005;22:643–654. doi: 10.1016/j.immuni.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 9.Flacher V, Tripp CH, Mairhofer DG, Steinman RM, Stoitzner P, Idoyaga J, Romani N. Murine Langerin+ dermal dendritic cells prime CD8+ T cells while Langerhans cells induce cross-tolerance. EMBO Mol. Med. 2014;6:1191–1204. doi: 10.15252/emmm.201303283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gomez de Agüero M, Vocanson M, Hacini-Rachinel F, Taillardet M, Sparwasser T, Kissenpfennig A, Malissen B, Kaiserlian D, Dubois B. Langerhans cells protect from allergic contact dermatitis in mice by tolerizing CD8(+) T cells and activating Foxp3(+) regulatory T cells. J. Clin. Invest. 2012;122:1700–1711. doi: 10.1172/JCI59725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shklovskaya E, O’Sullivan BJ, Ng LG, Roediger B, Thomas R, Weninger W, Fazekas de St Groth B. Langerhans cells are precommitted to immune tolerance induction. Proc. Natl. Acad. Sci. U. S. A. 2011;108:18049–18054. doi: 10.1073/pnas.1110076108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bedoui S, Whitney PG, Waithman J, Eidsmo L, Wakim L, Caminschi I, Allan RS, Wojtasiak M, Shortman K, Carbone FR, Brooks AG, Heath WR. Cross-presentation of viral and self antigens by skin-derived CD103+ dendritic cells. Nat. Immunol. 2009;10:488–495. doi: 10.1038/ni.1724. [DOI] [PubMed] [Google Scholar]
- 13.Henri S, Poulin LF, Tamoutounour S, Ardouin L, Guilliams M, de Bovis B, Devilard E, Viret C, Azukizawa H, Kissenpfennig A, Malissen B. CD207+ CD103+ dermal dendritic cells cross-present keratinocyte-derived antigens irrespective of the presence of Langerhans cells. J. Exp. Med. 2010;207:189–206. doi: 10.1084/jem.20091964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Murphy TL, Tussiwand R, Murphy KM. Specificity through cooperation: BATF-IRF interactions control immune-regulatory networks. Nat. Rev. Immunol. 2013;13:499–509. doi: 10.1038/nri3470. [DOI] [PubMed] [Google Scholar]
- 15.Naik S, Bouladoux N, Linehan JL, Han S-J, Harrison OJ, Wilhelm C, Conlan S, Himmelfarb S, Byrd AL, Deming C, Quinones M, Brenchley JM, Kong HH, Tussiwand R, Murphy KM, Merad M, Segre JA, Belkaid Y. Commensal-dendritic-cell interaction specifies a unique protective skin immune signature. Nature. 2015;520:104–108. doi: 10.1038/nature14052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gratz IK, Rosenblum MD, Maurano MM, Paw JS, Truong H-A, Marshak-Rothstein A, Abbas AK. Cutting edge: Self-antigen controls the balance between effector and regulatory T cells in peripheral tissues. J. Immunol. Baltim. Md 1950. 2014;192:1351–1355. doi: 10.4049/jimmunol.1301777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gratz IK, Truong H-A, Yang SH-Y, Maurano MM, Lee K, Abbas AK, Rosenblum MD. Cutting Edge: memory regulatory t cells require IL-7 and not IL-2 for their maintenance in peripheral tissues. J. Immunol. Baltim. Md 1950. 2013;190:4483–4487. doi: 10.4049/jimmunol.1300212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rosenblum MD, Gratz IK, Paw JS, Lee K, Marshak-Rothstein A, Abbas AK. Response to self antigen imprints regulatory memory in tissues. Nature. 2011;480:538–542. doi: 10.1038/nature10664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ali N, Zirak B, Rodriguez RS, Pauli ML, Truong H-A, Lai K, Ahn R, Corbin K, Lowe MM, Scharschmidt TC, Taravati K, Tan MR, Ricardo-Gonzalez RR, Nosbaum A, Bertolini M, Liao W, Nestle FO, Paus R, Cotsarelis G, Abbas AK, Rosenblum MD. Regulatory T Cells in Skin Facilitate Epithelial Stem Cell Differentiation. Cell. 2017;169:1119–1129.e11. doi: 10.1016/j.cell.2017.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Idoyaga J, Fiorese C, Zbytnuik L, Lubkin A, Miller J, Malissen B, Mucida D, Merad M, Steinman RM. Specialized role of migratory dendritic cells in peripheral tolerance induction. J. Clin. Invest. 2013;123:844–854. doi: 10.1172/JCI65260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bursch LS, Wang L, Igyarto B, Kissenpfennig A, Malissen B, Kaplan DH, Hogquist KA. Identification of a novel population of Langerin+ dendritic cells. J. Exp. Med. 2007;204:3147–3156. doi: 10.1084/jem.20071966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Poulin LF, Henri S, de Bovis B, Devilard E, Kissenpfennig A, Malissen B. The dermis contains langerin+ dendritic cells that develop and function independently of epidermal Langerhans cells. J. Exp. Med. 2007;204:3119–3131. doi: 10.1084/jem.20071724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Matloubian M, Lo CG, Cinamon G, Lesneski MJ, Xu Y, Brinkmann V, Allende ML, Proia RL, Cyster JG. Lymphocyte egress from thymus and peripheral lymphoid organs is dependent on S1P receptor 1. Nature. 2004;427:355–360. doi: 10.1038/nature02284. [DOI] [PubMed] [Google Scholar]
- 24.Hildner K, Edelson BT, Purtha WE, Diamond M, Matsushita H, Kohyama M, Calderon B, Schraml BU, Unanue ER, Diamond MS, Schreiber RD, Murphy TL, Murphy KM. Batf3 deficiency reveals a critical role for CD8alpha+ dendritic cells in cytotoxic T cell immunity. Science. 2008;322:1097–1100. doi: 10.1126/science.1164206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schenkel JM, Fraser KA, Beura LK, Pauken KE, Vezys V, Masopust D. T cell memory. Resident memory CD8 T cells trigger protective innate and adaptive immune responses. Science. 2014;346:98–101. doi: 10.1126/science.1254536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Natsuaki Y, Egawa G, Nakamizo S, Ono S, Hanakawa S, Okada T, Kusuba N, Otsuka A, Kitoh A, Honda T, Nakajima S, Tsuchiya S, Sugimoto Y, Ishii KJ, Tsutsui H, Yagita H, Iwakura Y, Kubo M, guan Ng L, Hashimoto T, Fuentes J, Guttman-Yassky E, Miyachi Y, Kabashima K. Perivascular leukocyte clusters are essential for efficient activation of effector T cells in the skin. Nat. Immunol. 2014;15:1064–1069. doi: 10.1038/ni.2992. [DOI] [PubMed] [Google Scholar]
- 27.Keir ME, Butte MJ, Freeman GJ, Sharpe AH. PD-1 and its ligands in tolerance and immunity. Annu. Rev. Immunol. 2008;26:677–704. doi: 10.1146/annurev.immunol.26.021607.090331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nurieva RI, Liu X, Dong C. Yin-Yang of costimulation: crucial controls of immune tolerance and function. Immunol. Rev. 2009;229:88–100. doi: 10.1111/j.1600-065X.2009.00769.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Okazaki T, Honjo T. PD-1 and PD-1 ligands: from discovery to clinical application. Int. Immunol. 2007;19:813–824. doi: 10.1093/intimm/dxm057. [DOI] [PubMed] [Google Scholar]
- 30.Sharpe AH, Wherry EJ, Ahmed R, Freeman GJ. The function of programmed cell death 1 and its ligands in regulating autoimmunity and infection. Nat. Immunol. 2007;8:239–245. doi: 10.1038/ni1443. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.