Abstract
The double Maddox rod test is often use to measure cyclodeviations and to monitor change over time. The purpose of this study was to estimate test–retest reliability and the amount of cyclodeviation that would be considered real change using 95% limits of agreement. We retrospectively studied 86 clinically stable patients with double Maddox rod measurements 5–175 days apart (median, 69 days). The range of cyclodeviation at the first measurement was 6° incyclodeviation to 15° excyclodeviation. We calculated the half width of the 95% limits of agreement to be 4.7°, which means that a change of ≥5° in cyclodeviation would be considered a real change. The threshold of 5° should be used when assessing change between two measurements made with double Maddox rods.
Determining the degree and direction of a cyclodeviation is important for the diagnosis and management of certain types of strabismus. Currently, one of the most frequently used methods of measuring cyclodeviations subjectively in clinic is the double Maddox rod test. This test has often been used as an outcome measure in previous studies, for example, when comparing the effectiveness of different torsional surgical procedures in patients with superior oblique palsy1 or to assess torsional side effects.2 Nevertheless, test–retest data for the double Maddox rod test are not available in the literature. The present study aimed to quantify test–retest variability in two consecutive double Maddox rod measurements.
Subjects and Methods
This study was approved by the Mayo Clinic Institutional Review Board. All procedures and data collection were conducted in a manner compliant with the US Health Insurance Portability and Accountability Act of 1996 and all research procedures adhered to the tenets of the Declaration of Helsinki.
The medical records of patients seen at the Mayo Clinic from September 2004 to October 2016 were reviewed retrospectively to identify a cohort of stable strabismus patients, with measures of ocular alignment by distance and near prism and alternate cover test on two examinations at least 1 day but no more than 180 days apart and measures of torsion by double Maddox rod. Stable ocular alignment was defined as distance and near measures within 5Δ on each examination (and no change in direction of the vertical deviation). This 5Δ limit is well within previous reports of test–retest variability for prism and alternate cover test strabismus measurements.3 Patients with any level of visual acuity were included, but patients were excluded if both streaks of the double Maddox rod test could not be seen simultaneously. Patients whose history included any of the following during the previous 5 years were excluded: head trauma, neurosurgery, unstable neurologic conditions (chronic progressive external ophthalmoplegia, myasthenia, multiple sclerosis, superior oblique myokymia), or eye surgery possibly affecting cyclodeviation (strabismus, orbital decompression, cataract, trabeculectomy/glaucoma drainage device, orbital fracture repair, vitreoretinal surgery, ptosis or lid surgery, botulinum toxin). Patients diagnosed with trochleitis and oscillopsia were also excluded.. Nonsurgical treatments (eg, prism) were allowed, with the exception of prolonged full-time occlusion.4
Assessment of Torsion
Cyclodeviation was assessed using the double Maddox rod test at both examinations by the same examiner. The examiner routinely performed the test as essentially masked, not reviewing the results of previous examinations until all testing was completed. The patient was tested in a sitting position, wearing a full trial frame (eFigure 1), with the red lens placed in front of the right eye and the white lens placed in front of the left eye. A muscle light was then presented in the straight ahead position, and the patient was asked whether or not they saw two horizontal streaks. The lenses were then deliberately offset by the examiner, with the red lens at approximately 105° and the white at approximately 75°, and the patient was instructed to adjust the knobs of the trial frame slowly (right lens and then left lens) until the perceived two horizontal streaks were “parallel to the floor” and “running like train tracks” or “together as one line.” The torsional deviation was read on the trial frame to the nearest single degree (estimating number of degrees between the 5° markings on trial frame), and the sum from both eyes was recorded as the net cyclodeviation. For example, 5° incyclodeviation on the right and 7° excyclodeviation on the left would be read as 2° excyclodeviation.
Analysis
Differences between test and retest were calculated for each individual. The 95% limits of agreement and the 95% confidence intervals around the 95% limits of agreement were calculated. Test–retest data were also presented as a Bland-Altman plot.5
Results
A total of 86 patients (mean age, 52 years; range, 14–86 years) met inclusion criteria. Demographics and clinical characteristics are presented in Table 1.
Table 1.
Demographic and clinical characteristics
| Characteristic | N (%) |
|---|---|
| Sex | |
| Female | 48 (56) |
| Male | 38 (44) |
| Race | |
| White (including Hispanic/Latino) | 84 (98) |
| Black/African American | 1 (1) |
| Unknown/not reported | 1 (1) |
| Ethnicity | |
| Not Hispanic or Latino | 85 (99) |
| Unknown/not reported | 1 (1) |
| VA in better-seeing eye | |
| 20/20 | 68 (79) |
| 20/25 to 20/40 | 18 (21) |
| VA in worse-seeing eye | |
| 20/20 | 44 (51) |
| 20/25 to 20/40 | 32 (37) |
| 20/50 to 20/200 | 10 (12) |
| Diagnosis | |
| Oculomotor nerve palsy | 3 (3) |
| Trochlear nerve palsy | 46 (53) |
| Abducens nerve palsy | 2 (2) |
| Brown syndrome | 4 (5) |
| Convergence insufficiency | 2 (2) |
| Consecutive XT | 3 (3) |
| Divergence insufficiency | 6 (7) |
| Duane syndrome | 1 (1) |
| Epiretinal membrane | 3 (3) |
| Esotropia (idiopathic) | 2 (2) |
| Graves eye disease | 1 (1) |
| Intermittent exotropia | 3 (3) |
| Lost muscle | 1 (1) |
| Mechanical strabismus after scleral buckle | 1 (1) |
| Sagging eye syndrome | 3 (3) |
| Exotropia (idiopathic) | 5 (6) |
| Type of cyclodeviation at first exam | |
| Excyclodeviation | 56 (65) |
| Incyclodeviation | 15 (17) |
| None | 15 (17) |
| Cyclodeviation, degrees at first exam | |
| 0 | 15 (17) |
| 1–4 | 36 (42) |
| 5–9 | 27 (31) |
| 10–15 | 8 (9) |
VA, visual acuity; XT, exotropia.
First measurement of cyclodeviation ranged from 6° incyclodeviation to 15° excyclodeviation. The second measurement ranged from 10° incyclodeviation to 17° excyclodeviation. The range of difference was 5° incyclodeviation to 7° excyclodeviation, with a mean of 0.5° excyclodeviation. Bland-Altman plots are presented in Figure 1, showing no evidence of increasing variability with increasing magnitude. The half-width of the 95% limits of agreement was 4.7° (95% CI, 3.8°–5.5°), with 95% limits of agreement of 4.2° incyclodeviation to 5.2° excyclodeviation.
FIG. 1.
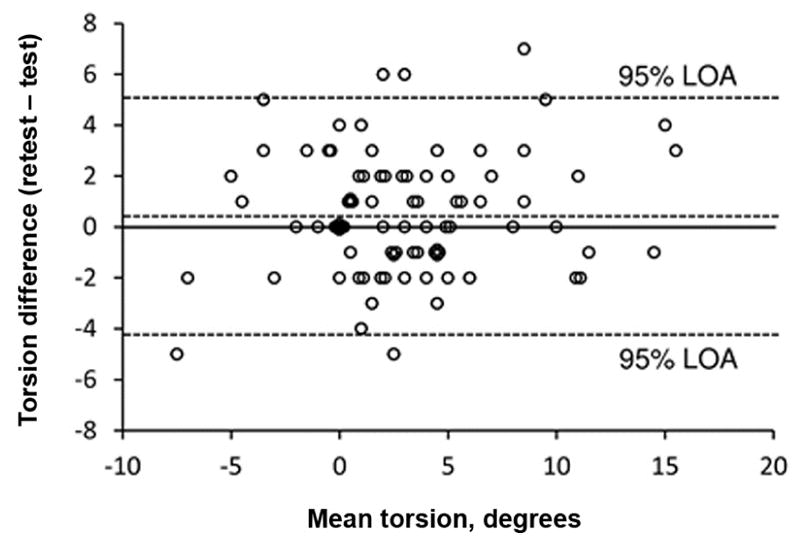
Bland–Altman plot showing 95% limits of agreement for the difference between 2 measurements of cyclodeviation using the double Maddox rod to be 4.7°. Middle dotted line represents the mean of test–retest differences (0.5°).
Discussion
In the present test–retest variability study of cyclodeviation using the double Maddox rod test, the half-width of the 95% limits of agreement was 4.7°. Therefore, to be confident that a real change in cyclodeviation has occurred, a change of 5° between examinations would be needed, acknowledging that any difference in measurements has both a component of measurement error and possible real change.
We are unaware of previous studies calculating test–retest variability for subjective cyclodeviation using the double Maddox rod test in patients. In a recent study of the single Maddox rod test (using the average of 3 measurements on each examination) in 20 subjects,6 the 95% limits of agreement (calculated from the author’s published averages from each patient) was 4.7°, which is essentially the same as that of the present study using the double Maddox rod.
Some limitations to the double Maddox rod test for measuring cyclodeviation have been previously reported.7 The Maddox rods are somewhat challenging to measure to the single degree, because the trial frames are graduated in 5° increments. In addition, we did not study test–retest variability within a single examination; nevertheless, we believe our study of test–retest variability between examinations is clinically useful.
Supplementary Material
Acknowledgments
Financial support: Supported by National Institutes of Health Grants EY018810 (JMH), EY024333 (JMH), Research to Prevent Blindness, New York, New York (unrestricted grant to the Department of Ophthalmology, Mayo Clinic), and Mayo Foundation, Rochester, Minnesota. None of the sponsors or funding organizations had a role in the design or conduct of this research. No authors have any financial/conflicting interests to disclose.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Arici C, Oguz V. The effect of surgical treatment of superior oblique muscle palsy on ocular torsion. J AAPOS. 2012;16:21–5. doi: 10.1016/j.jaapos.2011.09.015. [DOI] [PubMed] [Google Scholar]
- 2.Holmes JM, Hatt SR, Leske DA. Intraoperative monitoring of torsion to prevent vertical deviations during augmented vertical rectus transposition surgery. J AAPOS. 2012;16:136–40. doi: 10.1016/j.jaapos.2011.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pediatric Eye Disease Investigator Group. Interobserver reliability of the prism and alternate cover test in children with esotropia. Arch Ophthalmol. 2009;127:59–65. doi: 10.1001/archophthalmol.2008.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Graf EW, Maxwell JS, Schor CM. Changes in cyclotorsion and vertical eye alignment during prolonged monocular occlusion. Vision Res. 2002;42:1185–94. doi: 10.1016/s0042-6989(02)00047-0. [DOI] [PubMed] [Google Scholar]
- 5.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10. [PubMed] [Google Scholar]
- 6.Flodin S, Karlsson P, Andersson Grönlund M. Cyclotorsion measured in a patient population using three different methods: a comparative study. Strabismus. 2016;24:28–36. doi: 10.3109/09273972.2015.1135967. [DOI] [PubMed] [Google Scholar]
- 7.Marsh JD, Durkin MW, Hack AE, Markowitz BB, Cheeseman EW. Accuracy of double Maddox rod with induced hypertropia in normal subjects. Am Orthopt J. 2014;64:76–80. doi: 10.3368/aoj.64.1.76. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


