Abstract
Background
The clinical value of pedicle screws in spinal deformity surgery is well known; however, screw insertion is demanding and sometimes associated with complications. Navigation systems based on intraoperatively obtained three-dimensional (3-D) images were developed to minimize pedicle screw misplacements. However, there is a lack of data confirming superiority of navigation above other techniques. There are also concerns regarding increased radiation used during the procedure.
Questions/purposes
The purposes of this study were (1) to compare accuracy of the two methods of pedicle screws placement: intraoperative 3-D image navigation versus a freehand technique in patients with idiopathic scoliosis; and (2) to assess the radiation dose received by patients with both methods.
Methods
Between 2014 and 2016, 49 patients underwent posterior spinal fusion with all pedicle screw constructs for idiopathic scoliosis performed by two surgeons. The study design involved alternating the use of the freehand technique and navigation to position pedicle screws in consecutive patients, forming groups of 27 patients with 451 navigated screws and 22 patients with 384 screws positioned freehand. The two groups did not differ in age, sex, or magnitude of deformity. Two observers not involved in the treatment evaluated the position of the screws. The pedicle breach was assessed on intraoperatively obtained 3-D O-arm® scans according to a grading system: Grade 0 = no pedicle wall violation; Grade 1 = perforation ≤ 2 mm; Grade 2 = 2 to 4 mm; and Grade 3 = perforation > 4 mm. Grades 0 and 1 were considered properly positioned and Grades 2 and 3 represented malposition.
Results
In terms of accuracy, we found no differences, with the numbers available, between the freehand and navigated groups in terms of the proportion of screws that were properly positioned (96% freehand and 96% in the navigation group, respectively; p = 0.518). Grade 3 pedicle screws were observed only in the freehand group and were all located in the upper thoracic spine. Patients undergoing navigated pedicle screw placement received a greater mean radiation dose than those whose screws were placed freehand (1071 ± 447 mGy-cm versus 391 ± 53 mGy-cm; mean difference, 680 mGy-cm; 95% confidence interval, 217-2053 mGy-cm; p < 0.001).
Conclusions
In patients with moderate idiopathic scoliosis undergoing primary surgery, we did not observe benefits of pedicle screw placement with CT-based navigation, but the patients experienced greater exposure to radiation.
Level of Evidence
Level III, therapeutic study.
Introduction
Pedicle screws are helpful in the surgical treatment of spinal deformities, and they offer some advantages relative to hooks or wires [13, 33], particularly with respect to the biomechanics of spinal deformity correction; pedicle screws also are associated with a high likelihood of solid fusion [15, 17, 19]. However, placing these screws is demanding, and misplaced screws are associated with reduced biomechanical strength of the construct and less frequent but potentially severe complications like neurologic, visceral, or vascular injuries [8, 10]. Pedicle screw positioning in scoliosis surgery is particularly challenging because pedicles usually are smaller, sclerotic, and the spinal cord is in direct proximity to the pedicle on the concave side. Some prior research suggests that inappropriately placed implants occur more frequently in spinal deformities in the thoracic spine [10]. To prevent or at least minimize screw misplacements, navigation systems based on intraoperatively obtained three-dimensional (3-D) imaging were developed and seem promising [35].
However, available data are insufficient to confirm the superiority of navigation above other techniques [14]. Moreover, there are concerns regarding increased surgery time, costs of the necessary equipment, and particularly increased radiation to the patient [3, 14, 32]. This is a particular concern for patients with scoliosis, who are exposed to extensive radiation during deformity treatment owing to repetitive plain radiographs, intraoperative fluoroscopy, or CT. Although this is a concern for patients treated either nonsurgically or surgically, the patients having surgery receive particularly high doses of radiation [25]. Consequently, the question has been raised whether patients with scoliosis have an elevated risk of cancer developing [31].
The objectives of this study therefore were to (1) compare accuracy of two methods of pedicle screw placement: intraoperative 3-D image navigation versus a freehand technique in patients with idiopathic scoliosis; and (2) to assess the radiation dose for the patients with both methods.
Patients and Methods
Forty-nine patients were included in this study from among the cohort of patients treated operatively for progressive idiopathic scoliosis between 2014 and 2016 in the Department of Orthopedics, University Hospital Wroclaw. Any of the following criteria excluded patients from the study: previous spinal surgeries, nonidiopathic curves, curves < 40° and > 95°, and applications of implants other than screws (hooks, wires, universal clamps). The patients who met the inclusion criteria, at the stage of addition to the surgeon’s waiting list (usually 3-6 months before the operation), were assigned to one of the two groups: screw insertion with a freehand technique or screw insertion with the aid of navigation. The patients were divided evenly, one assigned to freehand and the following to the navigated group until even groups of 30 patients were formed. Several dropouts in both groups appeared mostly resulting from intraoperative O-arm availability, rescheduling the patients’ operations for either medical or personal reasons. Therefore, in total 22 patients who had pedicle screws inserted freehand and 27 patients with navigated insertion of the screws were analyzed.
All pedicle screws were introduced exclusively by two orthopaedic surgeons experienced in spinal deformity (WU, WJ). Before the trial, both were confident in pedicle screw placement either with aid of navigation or freehand with each having performed > 50 surgeries per year in patients with adolescent idiopathic scoliosis. The distribution of cases was similar for both surgeons with either technique. In all cases, intraoperative neuromonitoring (motor-evoked potentials) was used and no pedicle screw-related disturbances of traces were noted in the series. Hardware constructs had a similar screw distribution in all patients regardless of the group: densely implanted concave side (90%-100%) and the convex side with pedicle screws at the bottom, the top, and apical levels.
In the navigation group, to cannulate the pedicles, a navigation system (StealthStationTM Surgical Navigation System; Medtronic, Minneapolis, MN, USA) based on 3-D imaging obtained with an O-arm® Multi-dimensional Surgical Imaging System (Medtronic) was used. The imaging was acquired after exposure of posterior elements of the spine in the operating room. A navigated straight pedicle finder was used to cannulate the pedicle. Then the tunnel was checked with a ball-tipped feeler to confirm whether the walls were intact and the screw eventually was mounted on a standard (nonnavigated) screwdriver and introduced.
In the freehand group, the technique popularized by Kim and Lenke [11] was used. A small hole was drilled with a matchstick-ended burr in the cortical bone. Subsequently, the pedicle was cannulated with a curved pedicle finder all the way down to the anterior vertebral body cortex. The integrity of the tunnel was confirmed with a ball-tipped feeler. In both groups, pedicles were rarely tapped when necessary (eg, sclerotic pedicles).
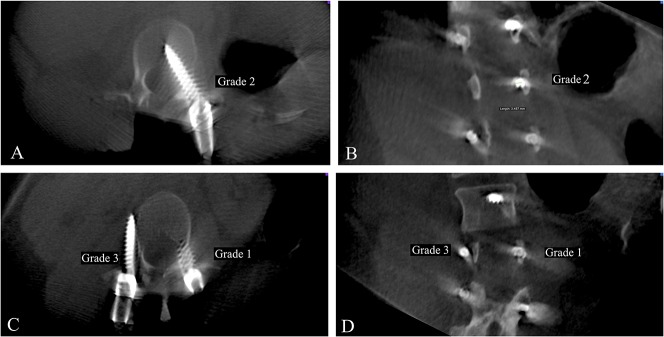
Two observers not involved in the treatment (MW, GM) conducted radiographic assessments. They independently assessed screw accuracy according to a grading system described by Gertzbein and Robbins [9] and in the case of disagreement, they discussed the criteria until a common consensus was reached. The pedicle wall violation was evaluated on CT scans obtained intraoperatively with the O-arm. The accuracy was described for each screw in sagittal (upper and lower wall breach) and horizontal (medial and lateral wall violation) planes (Fig. 1). The screws were assigned to one of four grades of pedicle breach: Grade 0 = no pedicle wall breach; Grade 1 = pedicle perforation of ≤ 2 mm; Grade 2 = wall perforation ≤ 4 mm; or Grade 3 = complete perforation of the pedicle (≥ 5 mm) [9]. Grades 0 and 1 were considered properly positioned screws and Grades 2 and 3 represented substantial wall violation resulting in screw malpositioning (Fig. 1) [1]. The pedicle screw accuracy, distribution of accuracy among levels, and distribution of breach localization were analyzed and compared between groups.
Fig. 1A-D.
Images from the O-arm were obtained after pedicle screw introduction with examples of misplaced screws. Axial (A) and coronal (B) views are presented with medial breech of the screw by 3.5 mm—Grade 2. Axial (C) and coronal (D) views show right-sided complete lateral screw misplacement—Grade 3 and left-sided medial breech by < 2 mm—Grade 1.
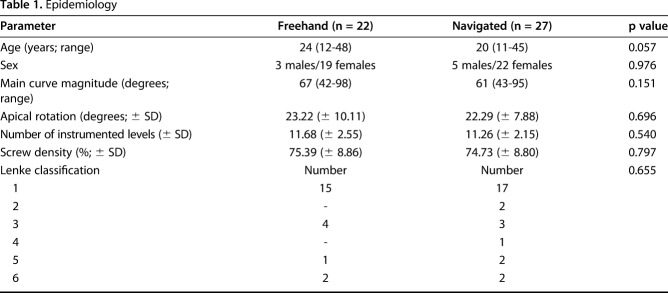
Patients in the navigated group were slightly younger than in the freehand group and the average curve magnitude was greater in the freehand group. Curve patterns according to the Lenke classification were similar in the freehand and navigated groups (Table 1) [18].
Table 1.
Epidemiology
In general, 835 pedicle screws were assessed in 49 patients. Four hundred fifty-one pedicle screws (27 patients) were introduced with the aid of navigation and 384 (22 patients) with the freehand technique. Six hundred thirty-one pedicle screws (298 freehand, 333 navigation) were placed in the thoracic vertebrae (T1-T12) and 204 (86 freehand, 118 navigation) in all lumbar levels.
All patients had ionizing radiation during surgery, either from a C-arm (BV Pulsera; Philips, Amsterdam, the Netherlands) or O-arm (Medtronic). Radiation doses were collected as dose reports obtained from both devices working in two-dimensional (2-D) imaging mode (C-arm and O-arm, mGy) and in 3-D imaging mode (O-arm, mGy-cm). Accuracy of the radiation exposure was tested routinely annually and the difference between measured and indicated values is < 20%. In the freehand group, the C-arm was used to check the instrumented levels and occasionally to observe the pedicle finder or feeler position in very narrow, deformed pedicles. In the navigated group, O-arm scans were obtained for navigation purposes. The number of 3-D scans performed depended on the patient’s size and instrumented spinal region. Usually one spin allows for comfortable navigation of four levels in the lumbar and lower thoracic spine and five to six levels in the middle and upper thoracic spine. Therefore, in smaller patients with Lenke Type 1A or 1B adolescent idiopathic scoliosis, only one scan was required. The majority of the patients had two spins, rarely three, and only one patient had four spins (tall, male patient with a Lenke Type 4 curve). Usually the same number of spins was necessary to observe the instrumented area and assess pedicle screw accuracy.
Once all the pedicle screws were inserted with either method, the protocol was the same in both groups. All patients underwent 3-D scans with the O-arm to check pedicle screw positions and to assess the accuracy of screw placement. Subsequently if malposition occurred, repositions were performed, but no additional 3-D scans were obtained (pedicle screws were checked with fluoroscopy if necessary). After corrective maneuvers, at the end of the operation, 2-D images were obtained using the O-arm to check spinal balance in all patients.
Malposition rates among levels, breach direction, radiation doses, and comparison between the freehand and navigated groups were statistically analyzed using Student’s t-test and Mann-Whitney tests. The U value of the Mann-Whitney test was used when both groups had < 20 measurements each, whereas the Z value of the Mann-Whitney test was used when one group had ≥ 20 measurements. In the situation of noncompliance, homogeneity of variance, and/or normal distribution (p > 0.05), Student’s t-test could not be used and thus the Mann-Whitney test was selected. A p value < 0.05 was considered statistically significant. The power analysis of presented material was performed. When true population effect size h is ≥ 0.2, an experiment based on two groups with sample sizes of 384 and 451 achieves at least 80% power to reject the null hypothesis of zero effect size between freehand and navigation using a two-sided Z test and significance level (α) is 0.05 (performed with software G*Power 3.0.10 [6]).
Results
Pedicle Screw Accuracy
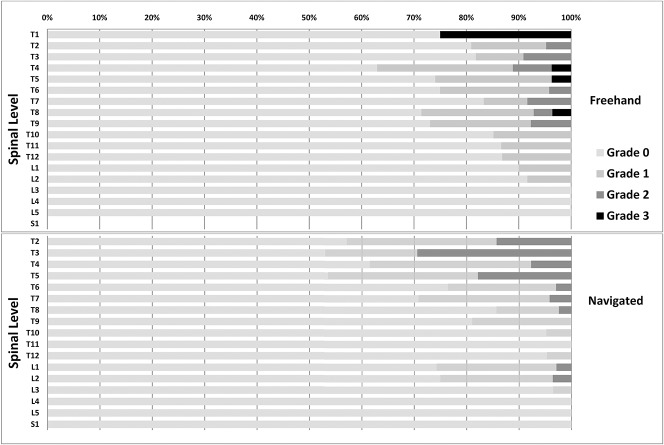
Of 384 pedicle screws inserted freehand, 315 were positioned with the whole screw in pedicle Grade 0. Fifty-five pedicle screws were considered Grade 1, still properly positioned, but there was minor pedicle wall breach (< 2 mm). Ten pedicle screws were assigned Grade 2 and four Grade 3. All Grade 3 pedicle screws were immediately repositioned. In the navigation group, of 451 pedicle screws, 374 were assigned to Grade 0, 58 to Grade 1, and 19 to Grade 2. There were no Grade 3 screws (Fig. 2). Therefore, with the numbers available, we observed no differences in accuracy of pedicle screw placement between the navigated and freehand groups (96% versus 96%; p = 0.5).
Fig. 2.
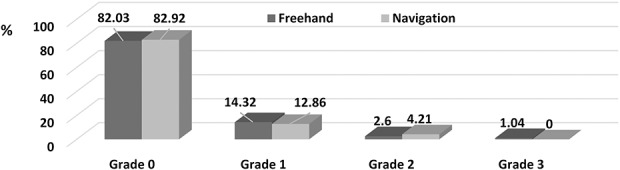
The percentage representation of pedicle screws in all grades is shown.
Most of the pedicle screws in Grade 2 in both groups were repositioned. Occasionally Grade 2 pedicle screws were left in place, for example, if the pedicles were very narrow, screw-related symptoms were unlikely, or the pedicle screws were laterally misplaced. Neither of the pedicle screws in the current series were symptomatic or required revision postoperatively.
The direction of misplacement also was assessed. In the freehand group, Grade 2 misplacements occurred in nine pedicle screws and only one pedicle screw breeched medially. Two pedicle screws were laterally displaced, one was medially displaced, and one was inferior to the pedicle in Grade 3 in the freehand group. Ten (55.5%) Grade 2 pedicle screws in the navigated group were displaced laterally, six were medially displaced, one was above the pedicle, and one was below the pedicle.
The lowest pedicle screw accuracy was across the upper thoracic spine (T1-T5, 82% navigated and 92% freehand screws were properly positioned) compared with the rest of the spine (T6-S1) (Fig. 3). For the navigated group, T1-T6 had a reduced accuracy of 17% (95% confidence interval [CI], 14%-18%; p = 0.047) and the freehand group had reduced accuracy of only 4% (95% CI, 4%-25%; p = 0.09).
Fig. 3.
The accuracy of pedicle screw on each instrumented level is shown. Percentage representation of each grade in both groups is shown.
Intraoperative Radiation
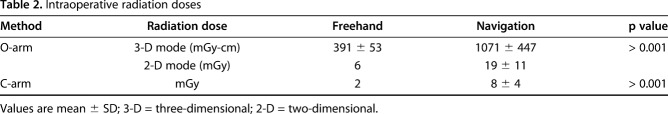
The radiation dose was higher in patients who underwent navigated pedicle screw placement than in the freehand group. The navigation group usually had two times more O-arm 3-D scans than the freehand group, which was reflected in higher radiation of 1071 ± 447 mGy-cm versus 391 ± 53 mGy-cm, respectively (mean difference, 680 mGy-cm; 95% CI, 217-2053 mGy-cm; p < 0.001). In addition, with 2-D imaging, patients were exposed to higher radiation in the navigated group (mean difference, 10 mGy; 95% CI, 2-40 mGy; p < 0.001) (Table 2).
Table 2.
Intraoperative radiation doses
Discussion
Proper placement of pedicle screws in posterior scoliosis surgery is critical to avoid screw-related complications and to provide good fixation in the bone and stable spinal fixation. Proper insertion of pedicle screws is a demanding technique, particularly difficult in patients with scoliosis in whom anatomic landmarks often are distorted and in whom the pedicles are narrow and deformed owing to vertebral rotation [23, 29]. Therefore, various guidance systems have been introduced to facilitate pedicle screw placement and improve its accuracy. Intraoperative 3-D image-based navigation seems to have great potential and is becoming increasingly popular in spinal surgery [2, 16, 26, 30, 35]. However, it is associated with increased exposure to ionizing radiation, which is known for its adverse effects [28, 32]. Therefore, questions have been raised by the authors and other surgeons about how to balance the accuracy of pedicle screw introduction and minimize the necessary radiation and in what sort of situations it is justified to implement the technology [25, 31, 32]. In the current study, we assessed accuracy of pedicle screw insertion with 3-D based-image navigation and the freehand technique in patients with mild and moderate idiopathic scoliosis. We observed no advantage of navigation over the freehand method in terms of pedicle screw accuracy. Moreover, navigation substantially increased radiation exposure to the patients.
This study had several limitations. The assessed cohort consisted of a consecutive series of patients who had a preplanned method of screw introduction at the stage of being added to the waiting list. However, discrepancies in the numbers of patients between groups were attributable to patient dropouts as a result of surgery cancellations or rescheduling because of intraoperative O-arm availability on the day of the operation. Therefore, patients receiving the freehand technique without O-arm 3-D scans or who had cancelled or postponed operations had to be excluded and we felt adding patients not according to the study protocol, to make the groups even, might bias the results. However, ultimately the reduced number of patients in the groups did not result in underpowering the statistical analysis. The power analysis of the test based on presented sample sizes in both groups when significance level α = 0.05 showed that this kind of test can be used to distinguish true population differences between freehand and navigation with power of ≥ 80% if effect size h is ≥ 0.2.
The radiation dose collection using reports from the device (C-arm, O-arm) is not a very precise method of a patient’s exposure to radiation, and this may be considered a limitation. However, the considerable differences in radiation exposure between the groups provide solid confirmation of a substantial increase in radiation in the navigation group compared with the freehand group. Two observers independently assessed screw position for all patients in both groups; however, no intra- and interobserver reliability testing was performed, which may be considered a methodologic weakness.
In this study, similar accuracy of pedicle screw placement was observed in the navigated and freehand groups with a mean 96% of properly placed pedicle screws in either group (in the pedicle or < 2 mm breech). According to previous studies, use of 3-D imaging merged with navigation improves accuracy of pedicle screw placement in the deformed thoracolumbar spine with misplacement rates of 3% to 6% in navigated cases versus 9% to 24% for the freehand technique [2, 5, 10, 16, 21, 22, 27, 34, 35]. However, unlike our series, these studies often included patients with severe deformities [22] and different backgrounds of scoliosis [16], and multiple surgeons each using different methods or an imprecise system of screw position assessment [35]. It may all bias the results showing superiority of navigation. We have not found any report comparing screw introduction with navigation and freehand in a fairly homogenous group of patients operated on by the same surgeons with both methods. Moreover, greater accuracy with navigation compared with the freehand technique does not mean higher complication rates using the latter technique [14, 16, 30]. The incidence of pedicle screw placement-related complications in patients with scoliosis per screw is usually < 1% (most common are nerve root and dura injuries) [4, 7]. We observed a high misplacement rate in the upper thoracic spine (T1-T5 levels) of 17% with navigation versus 8% (nearly 3% in Grade 3) with the freehand technique. Thoracic pedicles in idiopathic scoliosis tend to be more anatomically variable and narrow [20], which might explain the reduced precision of placement. This also was reported by other authors [24, 26]. We believe there are two distinct reasons that may contribute to this observation: the first is related to difficulties in imaging of the upper thoracic region and the second concerns so-called “juxtapedicular” positioning. It signifies that large-diameter pedicle screws (we did not use pedicle screws < 5 mm in diameter in this series) in often small and narrow pedicles did not allow for true intraosseous positioning [12]. The reason for the poor outcome in the navigation group also may be the long distance from the reference frame and working area. The frame was mounted at the T8-T9 spinous processes, which resulted in up to 15 cm distance from the frame to the instrumented T2 level.
In this study, increased ionizing radiation was observed in the group of patients having navigated pedicle screw placement versus the freehand technique. Dabaghi et al. [3] and Su et al. [32] reported analogous results, showing substantially higher mean effective radiation doses when intraoperative CT-based navigation was used compared with the freehand technique. However, the use of navigation reduces radiation exposure to the surgeon and operating room staff [36]. Adverse effects of radiation are well known and it has been shown that radiation may cause infertility, spontaneous abortion, and also increase the risk of cancer [28, 31]. Simony et al. [31] reported a five times higher incidence of cancer development (mainly breast and endometrial) in patients with adolescent idiopathic scoliosis treated either surgically or with a brace. Ronckers et al. [28] reported increased cancer risk and an 8% higher mortality rate from cancer in patients with scoliosis.
In the current study, in patients with moderate idiopathic scoliosis, accuracy of pedicle screw introduction was not different with navigation and the freehand technique, and overall accuracy of screw placement was high in both groups of patients. We observed an increased radiation dose in patients whose procedures were navigated and that appeared to provide at least a radiographic benefit, because Grade 3 screws were observed only with the freehand technique. However, intraoperative CT-based navigation does not eliminate misplacement. A noticeable risk still was observed, particularly in the upper thoracic spine. Therefore, it is essential to balance between the accuracy of placing pedicle screws and the increase in adverse ionizing radiation. We believe that use of CT-based navigation is only slightly justified in patients with mild or moderate idiopathic scoliosis during primary surgery. Further research is needed to confirm the usefulness of CT-based navigation in complex spinal cases (eg, severe deformity, revisions, congenital abnormalities), because additional substantial radiation may be acceptable in these cases. It also may have a role in education of spine surgeons, but this will need to be established in future studies, and the increased radiation dose to patients may be difficult to justify in the name of education.
Footnotes
Each author certifies that neither he, nor any member of his immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his institution waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This study was performed at the Department of Orthopaedics and Traumatology, University Hospital Wroclaw, Wroclaw, Poland.
References
- 1.Aoude AA, Fortin M, Figueiredo R, Jarzem P, Ouellet J, Weber MH. Methods to determine pedicle screw placement accuracy in spine surgery: a systematic review. Eur Spine J. 2015;24:990–1004. [DOI] [PubMed] [Google Scholar]
- 2.Cui G, Wang Y, Kao TH, Zhang Y, Liu Z, Liu B, Li J, Zhang X, Zhu S, Lu N, Mao K, Wang Z, Zhang X, Yuan X, Dong T, Xiao S. Application of intraoperative computed tomography with or without navigation system in surgical correction of spinal deformity: a preliminary result of 59 consecutive human cases. Spine (Phila Pa 1976). 2012;37:891–900. [DOI] [PubMed] [Google Scholar]
- 3.Dabaghi RA, Christodoulou E, Li Y, Caird MS, Jong N, Farley FA. Comparison of effective dose of radiation during pedicle screw placement using intraoperative computed tomography navigation versus fluoroscopy in children with spinal deformities. J Pediatr Orthop. 2016;36:530–533. [DOI] [PubMed] [Google Scholar]
- 4.Dede O, Ward WT, Bosch P, Bowles AJ, Roach JW. Using the freehand pedicle screw placement technique in adolescent idiopathic scoliosis surgery: what is the incidence of neurological symptoms secondary to misplaced screws? Spine (Phila Pa 1976). 2014;39:286–290. [DOI] [PubMed] [Google Scholar]
- 5.Esses SI, Sachs BL, Dreyzin V. Complications associated with the technique of pedicle screw fixation: a selected survey of ABS members. Spine (Phila Pa 1976). 1993;18:2231–2238; discussion 2238–2239. [DOI] [PubMed] [Google Scholar]
- 6.Faul F, Erdfelder E, Lang A-G, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods. 2007;39:175–191. [DOI] [PubMed] [Google Scholar]
- 7.Fujimori T, Yaszay B, Bartley CE, Bastrom TP, Newton PO. Safety of pedicle screws and spinal instrumentation for pediatric patients. Spine (Phila Pa 1976). 2014;39:541–549. [DOI] [PubMed] [Google Scholar]
- 8.Gautschi OP, Schatlo B, Schaller K, Tessitore E. Clinically relevant complications related to pedicle screw placement in thoracolumbar surgery and their management: a literature review of 35,630 pedicle screws. Neurosurg Focus. 2011;31:E8. [DOI] [PubMed] [Google Scholar]
- 9.Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine (Phila Pa 1976). 1990;15:11–14. [DOI] [PubMed] [Google Scholar]
- 10.Hicks JM, Singla A, Shen FH, Arlet V. Complications of pedicle screw fixation scoliosis surgery: a systematic review. Spine (Phila Pa 1976). 2010;35:E465–470. [DOI] [PubMed] [Google Scholar]
- 11.Kim YJ, Lenke LG. Thoracic pedicle screw placement: free-hand technique. Neurol India. 2005;53:512–519. [DOI] [PubMed] [Google Scholar]
- 12.Kim YJ, Lenke LG, Cheh G, Riew KD. Evaluation of pedicle screw placement in the deformed spine using intraoperative plain radiographs: a comparison with computerized tomography. Spine (Phila Pa 1976). 2005;30:2084–2088. [DOI] [PubMed] [Google Scholar]
- 13.Kim YJ, Lenke LG, Kim J, Bridwell KH, Cho SK, Cheh G, Sides B. Comparative analysis of pedicle screw versus hybrid instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2006;31:291–298. [DOI] [PubMed] [Google Scholar]
- 14.Kraus M, Weiskopf J, Dreyhaupt J, Krischak G, Gebhard F. Computer-aided surgery does not increase the accuracy of dorsal pedicle screw placement in the thoracic and lumbar spine: a retrospective analysis of 2,003 pedicle screws in a level I trauma center. Global Spine J. 2015;5:93–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kuklo TR, Potter BK, Lenke LG, Polly DW, Jr, Sides B, Bridwell KH. Surgical revision rates of hooks versus hybrid versus screws versus combined anteroposterior spinal fusion for adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2007;32:2258–2264. [DOI] [PubMed] [Google Scholar]
- 16.Larson AN, Polly DW, Jr, Guidera KJ, Mielke CH, Santos ER, Ledonio CG, Sembrano JN. The accuracy of navigation and 3D image-guided placement for the placement of pedicle screws in congenital spine deformity. J Pediatr Orthop. 2012;32:e23–29. [DOI] [PubMed] [Google Scholar]
- 17.Lee SM, Suk SI, Chung ER. Direct vertebral rotation: a new technique of three-dimensional deformity correction with segmental pedicle screw fixation in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2004;29:343–349. [DOI] [PubMed] [Google Scholar]
- 18.Lenke LG, Edwards CC, 2nd, Bridwell KH. The Lenke classification of adolescent idiopathic scoliosis: how it organizes curve patterns as a template to perform selective fusions of the spine. Spine (Phila Pa 1976). 2003;28:S199–207. [DOI] [PubMed] [Google Scholar]
- 19.Lenke LG, Kuklo TR, Ondra S, Polly DW., Jr Rationale behind the current state-of the-art treatment of scoliosis (in the pedicle screw era). Spine (Phila Pa 1976). 2008;33:1051–1054. [DOI] [PubMed] [Google Scholar]
- 20.Liljenqvist UR, Link TM, Halm HFH. Morphometric analysis of thoracic and lumbar vertebrae in idiopathic scoliosis. Spine (Phila Pa 1976). 2000;25:1247–1253. [DOI] [PubMed] [Google Scholar]
- 21.Lonstein JE, Denis F, Perra JH, Pinto MR, Smith MD, Winter RB. Complications associated with pedicle screws. J Bone Joint Surg Am. 1999;81:1519–1528. [DOI] [PubMed] [Google Scholar]
- 22.Modi HN, Suh SW, Hong JY, Yang JH. Accuracy of thoracic pedicle screw using ideal pedicle entry point in severe scoliosis. Clin Orthop Relat Res. 2010;468:1830–1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.O’Brien MF, Lenke LG, Mardjetko S, Lowe TG, Kong Y, Eck K, Smith D. Pedicle morphology in thoracic adolescent idiopathic scoliosis: is pedicle fixation an anatomically viable technique? Spine (Phila Pa 1976). 2000;25:2285–2293. [DOI] [PubMed] [Google Scholar]
- 24.Parker SL, McGirt MJ, Farber SH, Amin AG, Rick AM, Suk I, Bydon A, Sciubba DM, Wolinsky JP, Gokaslan ZL, Witham TF. Accuracy of free-hand pedicle screws in the thoracic and lumbar spine: analysis of 6816 consecutive screws. Neurosurgery. 2011;68:170–178 [DOI] [PubMed] [Google Scholar]
- 25.Presciutti SM, Karukanda T, Lee M. Management decisions for adolescent idiopathic scoliosis significantly affect patient radiation exposure. Spine J. 2014;14:1984–1990. [DOI] [PubMed] [Google Scholar]
- 26.Rivkin MA, Yocom SS. Thoracolumbar instrumentation with CT-guided navigation (O-arm) in 270 consecutive patients: accuracy rates and lessons learned. Neurosurg Focus. 2014;36:E7. [DOI] [PubMed] [Google Scholar]
- 27.Rodrigues LM, Nicolau RJ, Milani C. Computed tomographic evaluation of thoracic pedicle screw placement in idiopathic scoliosis. J Pediatr Orthop B. 2011;20:195–198. [DOI] [PubMed] [Google Scholar]
- 28.Ronckers CM, Land CE, Miller JS, Stovall M, Lonstein JE, Doody MM. Cancer mortality among women frequently exposed to radiographic examinations for spinal disorders. Radiat Res. 2010;174:83–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schulze CJ, Munzinger E, Weber U. Clinical relevance of accuracy of pedicle screw placement: a computed tomographic-supported analysis. Spine (Phila Pa 1976). 1998;23:2215–2220. [DOI] [PubMed] [Google Scholar]
- 30.Shin BJ, James AR, Njoku IU, Härtl R. Pedicle screw navigation: a systematic review and meta-analysis of perforation risk for computer-navigated versus freehand insertion. A review. J Neurosurg Spine. 2012;17:113–122. [DOI] [PubMed] [Google Scholar]
- 31.Simony A, Hansen EJ, Christensen SB, Carreon LY, Andersen MO. Incidence of cancer in adolescent idiopathic scoliosis patients treated 25 years previously. Eur Spine J. 2016;25:3366–3370. [DOI] [PubMed] [Google Scholar]
- 32.Su AW, McIntosh AL, Schueler BA, Milbrandt TA, Winkler JA, Stans AA, Larson AN. How does patient radiation exposure compare with low-dose O-arm versus fluoroscopy for pedicle screw placement in idiopathic scoliosis? J Pediatr Orthop. 2017;37:171–177. [DOI] [PubMed] [Google Scholar]
- 33.Suk SI, Kim JH, Kim SS, Lim DJ. Pedicle screw instrumentation in adolescent idiopathic scoliosis (AIS). Eur Spine J. 2012;21:13–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Takahashi J, Hirabayashi H, Hashidate H, Ogihara N, Kato H. Accuracy of multilevel registration in image-guided pedicle screw insertion for adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2010;35:347–352. [DOI] [PubMed] [Google Scholar]
- 35.Ughwanogho E, Patel NM, Baldwin KD, Sampson NR, Flynn JM. Computed tomography guided navigation of thoracic pedicle screws for adolescent idiopathic scoliosis results in more accurate placement and less screw removal. Spine (Phila Pa 1976). 2012;37:E473–478. [DOI] [PubMed] [Google Scholar]
- 36.Villard J, Ryang YM, Demetriades AK, Reinke A, Behr M, Preuss A, Meyer B, Ringel F. Radiation exposure to the surgeon and the patient during posterior lumbar spinal instrumentation a prospective randomized comparison of navigated versus non-navigated freehand techniques Spine (Phila Pa 1976). 2014;39:1004–1009. [DOI] [PubMed] [Google Scholar]