Abstract
Background
Implant survivorship is reported to be lower and complications, particularly bearing dislocation, are reported to be more frequent in Asian than in Western patients with medial knee osteoarthritis (OA) undergoing Oxford® Phase III unicompartmental knee arthroplasty (UKA). To date, however, these complications have not been compared between these groups of patients.
Questions/purposes
The purpose of this study was to perform a meta-analysis comparing the standardized incidence rates of (1) all-cause reoperation; (2) reoperation related to bearing dislocation; and (3) reoperation related to progression of lateral compartment arthritis in Asian and Western patients with medial knee OA who underwent Oxford Phase III UKA.
Methods
We searched MEDLINE® (January 1, 1976, to May 31, 2017), EMBASE® (January 1, 1985, to May 31, 2017), and the Cochrane Library (January 1, 1987, to May 31, 2017) for studies that reported complications of Oxford Phase III UKAs. Studies were included if they reported reoperation rates attributable to bearing dislocation and/or progression of lateral knee OA after surgery with this implant. Twenty-seven studies were included in this systematic review and 16 studies with followups > 5 years were included in the meta-analysis. These rates were converted to standardized incidence rate (that is, reoperations per 100 observed component years) based on mean followup and number of involved knees in each study. After applying prespecified inclusion and exclusion criteria, the studies were categorized into two groups, Asian and Western, based on hospital location. Twenty-five studies, containing 3152 Asian patients and 5455 Western patients, were evaluated. Study quality was assessed by the modified Coleman Methodology score (MCMS). Although all studies were Level IV, their mean MCMS score was 66.92 (SD, 8.7; 95% confidence interval [CI], 63.5–70.3), indicating fair quality. Because the heterogeneity of all subgroup meta-analyses was high, a random-effects model was used with estimations using the restricted maximum likelihood method.
Results
There was no difference in the proportion of Asian patients versus Western patients undergoing reoperation for any cause calculated as 100 component observed years (1.022 of 3152 Asian patients; 95% CI, 0.810-1.235 versus 1.300 of 5455 Western patients; 95% CI, 1.067-1.534; odds ratio, 0.7839; 95% CI, 0.5323-1.1545; p = 0.178). The mean reoperation rate attributable to bearing dislocation per 100 observed years was higher in Asian than in Western patients (0.525; 95% CI, 0.407-0.643 versus 0.141; 95% CI, 0.116-0.166; odds ratio, 3.7378; 95% CI, 1.694-8.248; p = 0.001) Conversely, the mean reoperation rate attributable to lateral knee OA per 100 observed years was lower in Asian than in Western patients (0.093; 95% CI, 0.070-0.115 versus 0.298; 95% CI, 0.217-0.379; odds ratio, 0.3114; 95% CI, 0.0986-0.9840; p < 0.001).
Conclusions
Although total reoperation rates did not differ in the two populations, reoperation for bearing dislocation was more likely to occur in Asian than in Western patients, whereas reoperation for lateral knee OA progression was more likely to occur in Western than in Asian patients after Oxford Phase III UKA. Although possible explanations for these findings may be hypothesized, additional randomized, prospective comparative studies are needed. However, better survival outcomes after UKA may require consideration of ethnicity and lifestyle choices in addition to traditional surgical technique and perioperative care.
Level of Evidence
Level III, therapeutic study.
Introduction
Unicompartmental knee arthroplasty (UKA) is a treatment option for patients with medial or lateral compartment knee osteoarthritis (OA). UKA may provide advantages over TKA, including more natural kinematics, quicker recovery, lower postoperative morbidity rates, and greater preservation of bone stock, especially in relatively young patients [5, 12, 16, 27]. Fully congruent mobile-bearing UKA was devised to reduce bearing wear [44], one of the important factors affecting the long-term survival of UKA. The Oxford® Phase III (Zimmer Biomet Ltd, Swindon, UK) UKA is a design of congruent mobile-bearing UKA that has shown excellent long-term results in Europe and the United States [13, 29].
However, the risk of certain complications, particularly bearing dislocation, has been reported to be higher in Asian than in Western patients, raising questions on the survival of mobile-bearing UKA in Asian patients [4, 19, 28, 38]. The progression of lateral compartment OA after medial UKA is another common cause for reoperation after UKA. To our knowledge, no study to date has directly compared the survival and reoperation rates attributable to bearing dislocation and progression of lateral compartment OA of the Oxford Phase III UKA in Asian and Western patients with medial compartment knee OA.
This systematic review and meta-analysis therefore was designed to compare the standardized incidence rate of reoperation for (1) all-cause reoperation; (2) reoperation related to bearing dislocation; and (3) reoperation related to progression of lateral compartment arthritis in Asian and Western patients with medial knee OA who underwent Oxford Phase III UKA.
Materials and Methods
Literature Search
The study design was based on Cochrane Review Methods. In accordance with the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement [33, 34], multiple comprehensive databases, including MEDLINE® (January 1, 1976, to May 31, 2017), EMBASE® (January 1, 1985, to May 31, 2017), and the Cochrane Library (January 1, 1987, to May 31, 2017), were searched for studies that reported the complications of Oxford Phase III UKA. There were no restrictions on language or year of publication. Search terms used in the title, abstract, MeSH, and keyword fields included (Oxford) AND (unicompartmental knee replacement OR unicompartmental knee arthroplasty OR partial knee arthroplasty OR partial knee replacement OR unicondylar knee arthroplasty OR unicondylar knee replacement OR UKA) AND (oxford*) AND (reoperation OR revision OR survival analysis OR survival rate OR complication OR postoperative complication OR bearing dislocation OR dislocated bearing OR prosthesis failure OR progressive osteoarthritis OR lateral osteoarthritis). Relevant articles and their bibliographies were searched manually after the initial electronic search.
Study Selection
Two reviewers (K-HR, WJJ) evaluated the titles and abstracts of all retrieved papers and selected relevant studies for full review. If the abstract did not provide sufficient data to make a decision, the full text of the article was reviewed. Studies were included in the systematic review if they (1) involved patients who underwent primary UKA using Oxford Phase III prostheses for medial OA of the knee; (2) evaluated patients undergoing reoperation surgery after the primary UKA; and (3) if they fully reported the numbers of patients and involved knees, mean followup, and reasons for reoperation, enabling calculations of the number and proportion of knees with bearing dislocation and the progression of knees with lateral OA. Studies not clearly reporting reoperation data, biomechanical and cadaveric studies, technical notes, letters to the editor, expert opinions, review articles, meta-analyses, scientific conference abstracts, other unpublished work, studies published in nonindexed journals, and case reports were excluded. Although Clinical Orthopaedics and Related Research® normally does not allow meta-analysis (data pooling) from retrospective sources, this was permitted in the current study because the research questions (comparing survivorship of UKA between Asian and Western patients and different reasons for reoperations between those populations) have never been—and are unlikely ever to be—explored in the context of randomized or even prospective trials.
Studies of cohorts undergoing UKA for extraordinary conditions, studies of patients who underwent primary UKA for lateral OA, and studies with short-term followup (< 2 years) also were excluded. In assessing and organizing pooled studies, the country and city of the hospital or institution where the UKA was performed, and the evaluation period, were checked to exclude duplicate groups of patients. If the same patient cohort was evaluated in more than one study, the study published last with the longest followup was included, whereas the others were excluded. Two studies [4, 38] included patients who underwent surgery at the same hospital during a similar period, but none of the patients included in the latter published study [4] had been included in previous survival analyses at that institution; therefore, both studies were included.
Studies were categorized into two groups, Asian and Western, based on hospital location. Studies involving international clinics and those mentioning the inclusion of nonresident patients who underwent reoperation after UKA were excluded. None of the studies reported the number or proportion of domestic patients who underwent surgery. Patient regions of origin in each study were classified as Asian or Western based not only on geography, but on sociocultural environment, including floor-based lifestyle or religious activities. The meta-analysis assumed that (1) most patients who underwent UKA were older rather than younger and had lived in the country of operation for some time, even if they were born elsewhere; and (2) few patients would be nonresidents of the country of operation. For example, although ethnic Asians live in the United States and the United Kingdom, many have adopted more Western lifestyles. Traditional Asian floor-based lifestyles are less commonly practiced by Asians in Western countries, except for a small minority who practice Islam. Therefore, studies performed outside Asia were regarded as consisting entirely of Western patients.
In terms of classifying the region of origin as Asian or Western, we considered not only the geographic, but also the sociocultural environment, because both may influence knee motion and stress after UKA. This classification was difficult for two studies, one from Turkey [7] and the other from Israel [17]. Although both of these countries are in the Middle East, which are geographically Asian, their religions and cultures differ from those in East Asian countries making their classification more difficult. Therefore, to clearly differentiate between Asian and Western subjects, these studies were excluded from this meta-analysis. Institutional review board approval and patient informed consent (written or oral) were not required because all analyses were based on previously published studies.
Data Extraction
Two investigators (K-HR, J-WH) independently recorded data from each study using a predefined data extraction form. Any disagreements unresolved by discussion by these investigators were reviewed by a third investigator (D-HL) as needed. Complications recorded included those undergoing reoperation after the medial UKA. Patients with intraoperative complications and postoperative complications rho did not undergo reoperation were not analyzed. Demographic characteristics included the total numbers of patients and knees, age, sex, ethnicity, and followup period.
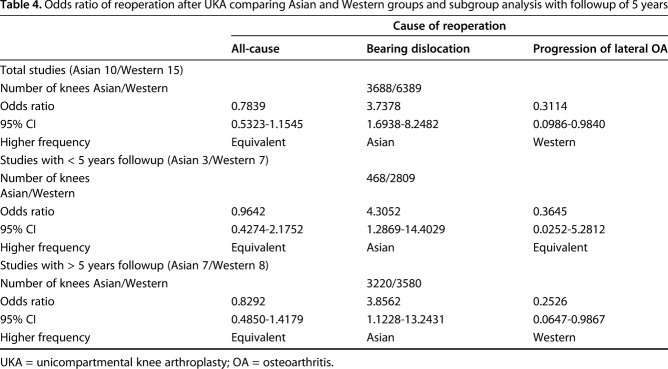
Identification of Studies
An electronic search yielded 154 studies in PubMed (MEDLINE), 120 in EMBASE, and 18 in the Cochrane Library (Fig. 1). After removing 118 duplicates, and adding seven additional publications identified through manual searches, 181 studies remained; of these, 73 were excluded based on review of their titles and abstracts. An additional 83 studies were excluded after reading their full texts showed that they did not contain usable information or included irrelevant data. Finally, 25 studies [3, 4, 6, 9, 10, 13, 15, 19, 22-24, 28-32, 36, 38, 39, 43, 44, 46, 51, 52, 54] were included in this systematic review.
Fig. 1.
The PRISMA flow diagram used in our study is shown. The initial search criteria identified 292 articles. After application of all exclusion criteria, 25 studies were identified for analysis.
Quality Appraisal
The original Coleman methodology score [11] uses 10 criteria to assess the methodology of a given study, resulting in total scores between 0 and 100 with a score of 100 indicating that the study largely avoids important systemic sources of bias and other confounding factors. The subsections that compose the Coleman methodology score are based on the subsections of the Consolidated Standards of Reporting Trials (CONSORT) statement for randomized controlled trials [1] but were modified to allow for other study designs [37]. The original Coleman methodology score, which was developed for surgical treatment of tendinopathy [11], was modified for arthroplasty of the knee [20]. The quality of each included study was evaluated by two independent investigators (K-HR, J-WH) using the modified Coleman methodology score. Quality was also assessed using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist [47], which contains 22 numbered items with several multiple subitems. Because all studies were case series with Level IV evidence, relevant items or STROBE was used for case series, as described previously [2]. Differences in subsections were resolved by consensus or, if necessary, by a third senior investigator (D-HL). The quality of studies was compared between groups using Student’s t-tests with statistical significance set at a probability < 0.05.
Study Characteristics and Quality
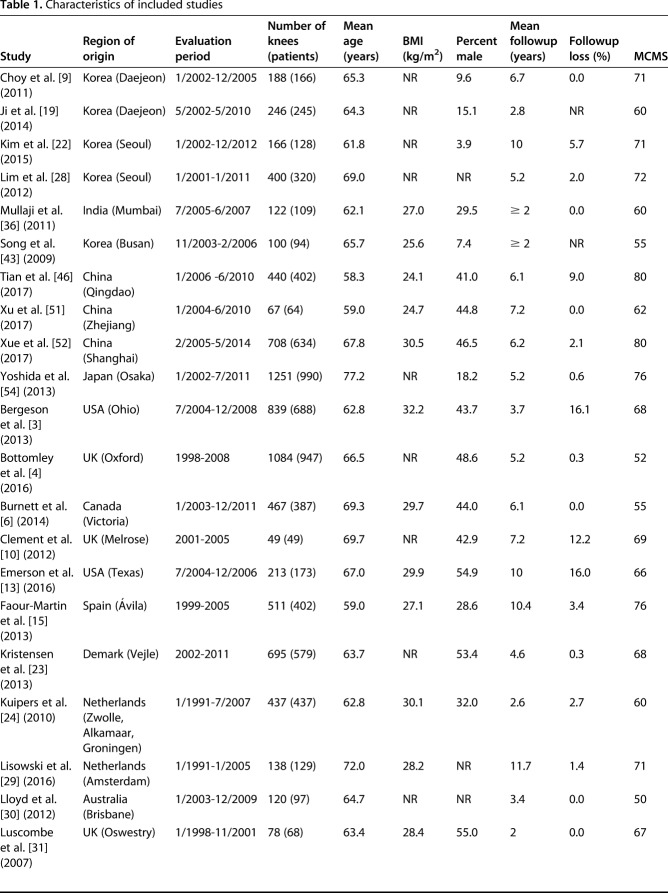
Patient characteristics, including region of origin, evaluation period, mean age, duration of followup, body mass index, sex distribution, and modified Coleman methodology score, are summarized (Table 1). The 25 included studies evaluated 10,077 knees of 8607 patients who underwent Oxford Phase III UKA. Ten studies included 3688 knees of 3152 Asian patients, and 15 studies included 6389 knees of 5455 Western patients. Seven studies of Asian patients and eight of Western patients reported followup > 5 years. Although all studies were Level IV, their total mean modified Coleman methodology score was 66.92 (SD, 8.7; 95% confidence interval [CI], 63.5-70.3) of 100, regarded as fair quality. Of the 25 studies, nine had mean modified Coleman methodology scores > 70, whereas two had scores < 55. The mean modified Coleman methodology scores of the 15 studies included in the subgroup meta-analysis group [4, 6, 9, 10, 13, 15, 22, 28, 29, 38, 44, 46, 51, 52, 54] were 70.3 (SD, 8.6; 95% CI, 65.9-74.6), 73.9 (SD, 6.3; 95% CI, 69.2-78.5) in seven studies of Asian patients [9, 22, 28, 46, 51, 52, 54] and 67.1 (SD, 9.6; 95% CI, 60.7–73.4) in eight studies of Western patients [4, 6, 10, 13, 15, 29, 38, 44], a difference that was not statistically significant (p = 0.468). Assessment of quality using the STROBE checklist showed that Outcome data (Item 15) were well described, shown as (+) in all studies. Setting (Item 5), Participants (Item 6), and Variables (Item 7) were also generally well described, whereas Statistical methods (Item 12) had the lowest score among all items of the checklist. Of the 25 studies, 13 were regarded as well described, nine as partly described (+/-), and three as poorly/not described (-) (Table 2).
Table 1.
Characteristics of included studies
Table 2.
Quality assessment by Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist for the case series
Statistical Analysis
Reoperation data recorded in the studies included in this analysis were pooled. Because the need for reoperation was relatively rare and could be biased by differences in followup periods, reoperation rates were converted to a standardized incidence rate (ie, reoperations per 100 observed component years) based on the mean followup and number of involved knees in each study [26]. To allow for inclusion of studies with a 0% incidence of reoperations, a 0.5 correction was used.
Most reoperations after UKA occurred within 5 years of surgery. However, studies with a followup > 5 years reported a substantial rate of reoperation > 5 years after UKA. Subgroup analysis of studies with a followup > 5 years was performed to determine midterm results and to determine whether these results differed from those of the meta-analysis that included all studies. Reoperation rates per 100 observed years were compared in Asian and Western populations using independent t-tests. Analyses were performed using the Comprehensive Meta-Analysis statistical software (Biostat, Englewood, NJ, USA) and R statistical software Version 3.4.0 (the metafor Package: a Meta-Analysis Package for R; R Foundation for Statistical Computing, Vienna, Austria) [48]. Because the heterogeneity of all subgroup meta-analyses was high, a random-effects model, with estimations using the restricted maximum likelihood method, was used. This model has been shown to allow greater generalization of conclusions for variable patient populations and different surgical techniques are grouped [18]. A summary odds ratio (OR) was calculated using a two-by-two contingency table (George Wilson University, Fairfax, VA, USA). The reoperation rates and 95% CIs for each study and the overall random-effects pooled estimate for each UKA group and its 95% CI were constructed for forest plots, which were constructed using Open Meta-Analyst (http://www.cebm.brown.edu/openmeta) [49]. We set statistical significance at a probability < 0.05.
Results
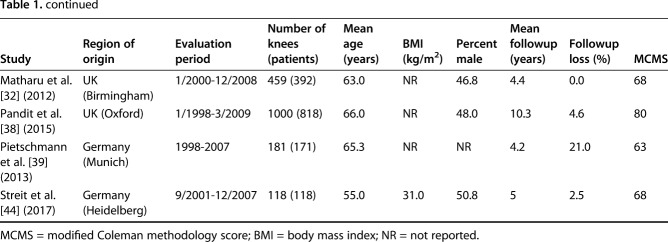
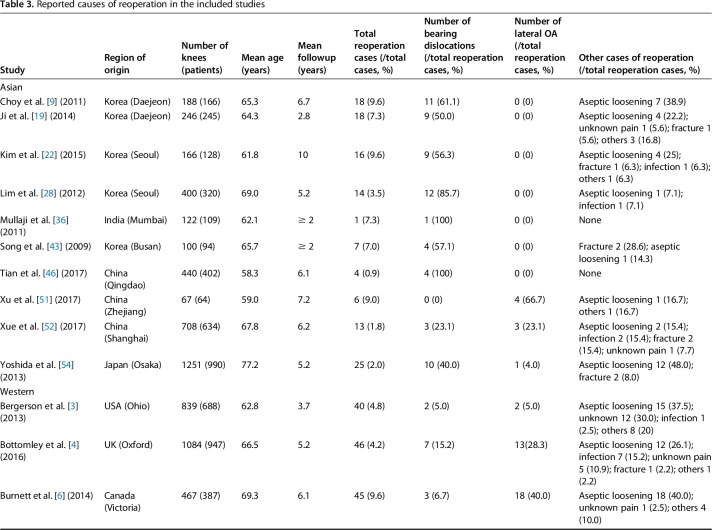
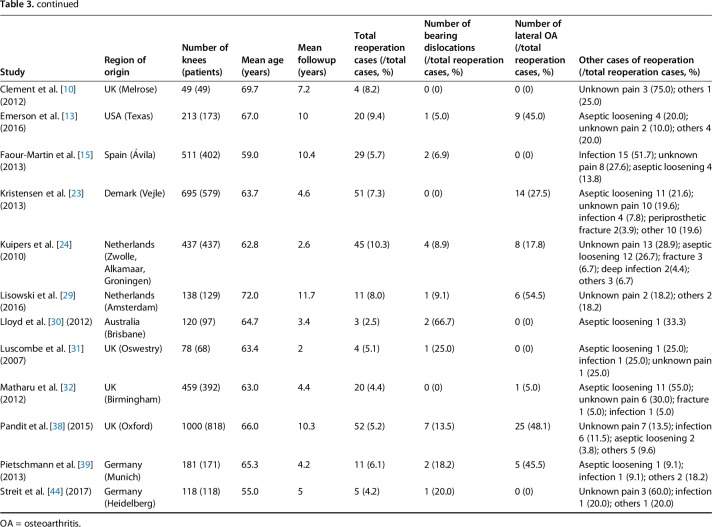
Reported causes of reoperations in the included studies were summarized. Total reoperation rates in these studies ranged from 0.9% to 10.3% (Table 3). Of the 10 studies of Asian patients, nine reported bearing dislocations after UKA, but only three reported the progression of lateral OA. In contrast, of the 15 studies of Western patients, 12 reported bearing dislocations after UKA, and 10 reported the progression of lateral OA.
Table 3.
Reported causes of reoperation in the included studies
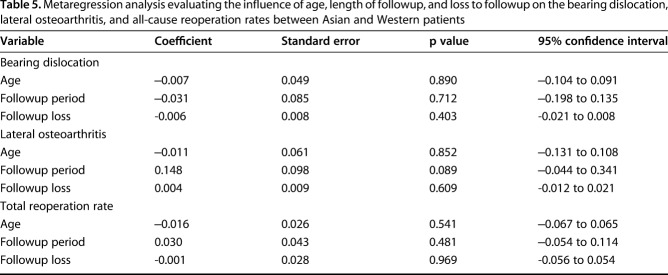
All-cause Reoperations
The mean reoperation rates per 100 observed component years for any cause after UKA were similar in the 3152 Asian patients (1.02; 95% CI, 0.81–1.23) and the 5455 Western patients (1.30; 95% CI, 1.07–1.53; p = 0.178; OR, 0.78; 95% CI, 0.53–1.15) (Fig. 2; Table 4). In a subgroup meta-analysis of patients followed up for > 5 years, the OR of mean reoperation rates per 100 observed component years was not different between Asian and Western patients (0.73 of 3220 Asian patients; 95% CI, 0.52-0.94 versus 0.88 of 3580 Western patients; 95% CI, 0.68-1.08; p = 0.58; OR, 0.83; 95% CI, 0.49-1.42) (Table 4).
Fig. 2.
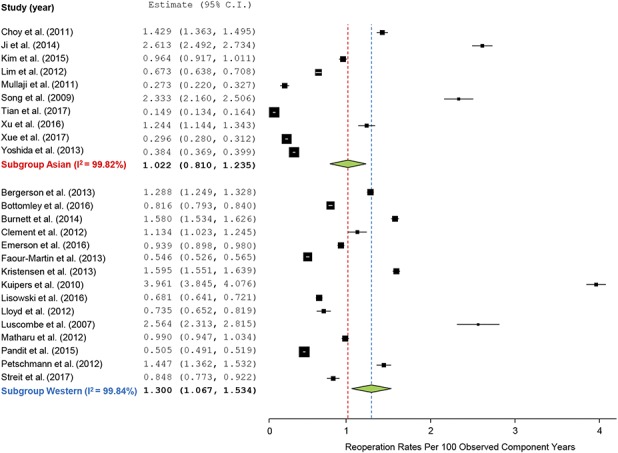
The forest plot of all-cause revision is shown. The mean reoperation rates per 100 observed component years for any cause after UKA were not different between 10 studies of the Asian group and 15 studies of the Western group showed no difference (1.022 of 3152 Asian patients; 95% CI, 0.810-1.235 versus 1.300 of 5455 western patients; 95% CI, 1.067-1.534; p = 0.178).
Table 4.
Odds ratio of reoperation after UKA comparing Asian and Western groups and subgroup analysis with followup of 5 years
Reoperation for Bearing Dislocation
The mean reoperation rates per 100 observed component years for bearing dislocation after UKA were higher in Asian (0.53; 95% CI, 0.41–0.64) than in Western (0.14; 95% CI, 0.12–0.17) patients (p = 0.001; OR, 3.7; 95% CI, 1.7–8.2) (Fig. 3; Table 4). Subgroup meta-analysis of patients followed up for > 5 years also showed that the OR of the mean bearing dislocation rate for patients undergoing reoperation per 100 observed years was higher in Asian than in Western patients (0.35 of 3220 Asian patients; 95% CI, 0.23-0.47 versus 0.09 of 3580 Western patients; 95% CI, 0.07-0.12; p = 0.027; OR, 3.9; 95% CI, 1.2-13.2) (Table 4).
Fig. 3.
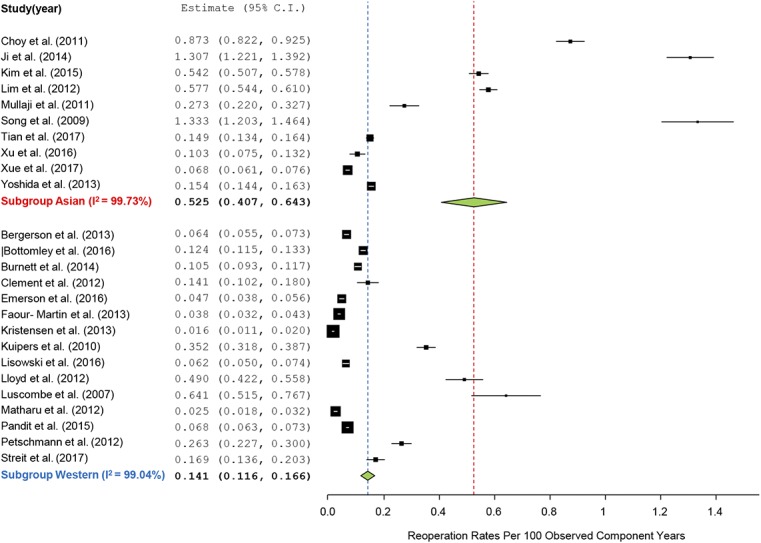
The forest plot of reoperation rates for bearing dislocation is shown. The mean reoperation rates per 100 observed component years for the bearing dislocation after UKA were higher in seven studies of the Asian group than eight studies of the Western group (0.525 of 3152 Asian patients; 95% CI, 0.407-0.643 versus 0.141 of 5455 Western patients; 95% CI, 0.116-0.166; p = 0.001).
Reoperation for Progression of Lateral OA
The mean reoperation rates per 100 observed component years for the progression of lateral OA after UKA were lower in Asian patients than Western patients (0.09 of 3152 Asian patients; 95% CI, 0.07-0.12 versus 0.30 of 5455 Western patients; 95% CI, 0.22-0.38; p < 0.001; OR, 0.31; 95% CI, 0.098-0.984) (Fig. 4; Table 4). Likewise, subgroup meta-analysis of patients followed up for > 5 years showed that the mean rate of progressive lateral OA in patients undergoing reoperations per 100 observed years was significantly lower in Asian than in Western patients (0.08 of 3220 Asian patients; 95% CI, 0.055-0.104 versus 0.27 of 3580 Western patients; 95% CI, 0.134-0.469; p = 0.017; OR, 0.25; 95% CI, 0.065-0.99) (Table 4).
Fig. 4.
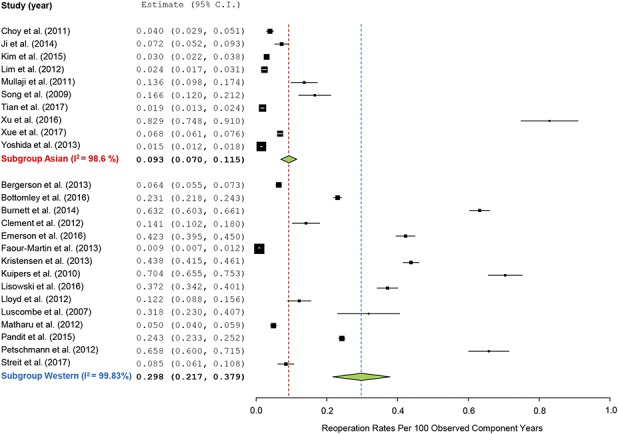
The forest plot of reoperation rates for progression of lateral OA is shown. The mean reoperation rates per 100 observed component years for the progression of lateral OA after UKA were lower in seven studies of the Asian group than eight studies of the Western group (0.093 of 3152 Asian patients; 95% CI, 0.070-0.115 versus 0.298 of 5455 Western patients; 95% CI, 0.217-0.379; p < 0.001).
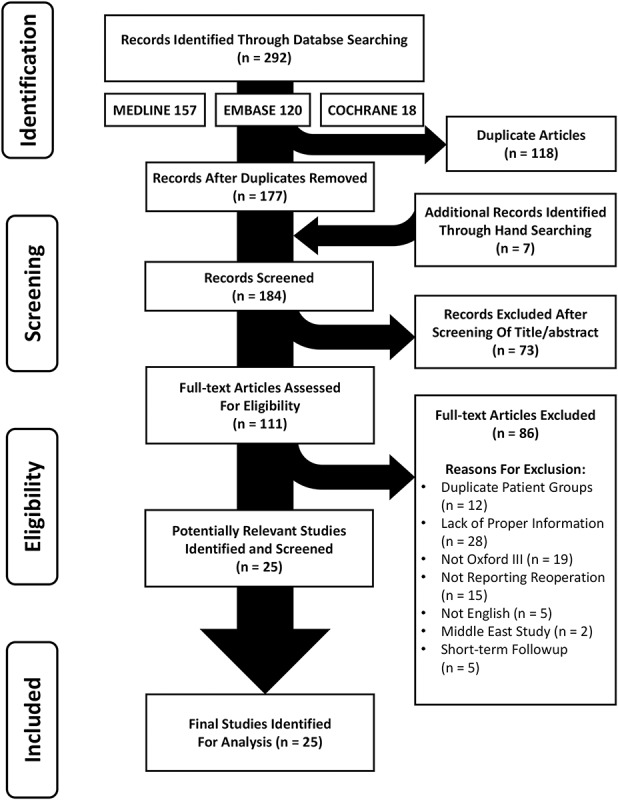
Metaregression Analyses
The results of metaregression analyses are reported (Table 5). The age and the length of or loss to followup was not significantly associated with rates of bearing dislocation, lateral compartment OA, and reoperation as a result of any reason.
Table 5.
Metaregression analysis evaluating the influence of age, length of followup, and loss to followup on the bearing dislocation, lateral osteoarthritis, and all-cause reoperation rates between Asian and Western patients
Discussion
Many case series, differing in length of followup and patient origin, have reported outcomes after UKA. Differences in specific causes of reoperation have been observed in studies of patients from both Asian and Western countries. Because randomized and comparative studies are lacking, we designed this meta-analysis to compare the standardized incidence rates of reoperation for all causes, for bearing dislocation and for progression of lateral compartment arthritis in Asian and Western patients with medial knee OA who underwent Oxford Phase III UKA. The most important findings of this systematic review and meta-analysis were that reoperations for bearing dislocation after UKA are more likely to occur in Asian than Western populations, but that reoperation for progression of lateral OA is more predominant in Western than Asian patients.
The present study had several limitations. Although we observed associations between common causes of reoperation after UKA and geographic group, we could not determine a clear causal relationship. Bearing dislocation or the progression of lateral OA may be influenced by lifestyle, but may also be influenced by biologic factors or differences in knee morphology. Although our findings yield important implications regarding postoperative clinical care and radiologic evaluation, this may be difficult to apply to patients who maintain their ethnic cultural lifestyle in a foreign country with a different cultural lifestyle and patients who live in geographic areas not considered Asian or Western such as the Middle East. Second, because most studies did not report patient-level information about the number of Asian and Western patients, we could not determine the ethnic homogeneity of patients in each study. However, we assumed that patients adopted the lifestyle of their native country, not their country of origin. Studies involving a single center or many centers within a single nation would be required to assess the effects of patient ethnicity. Third, because the research questions have never been explored in the context of randomized or even prospective trials, our meta-analysis was based on studies with Level IV evidence. Thus, our meta-analysis has all of the limitations of retrospective, literature-based studies, including differences in surgical techniques, sample sizes, and other possible confounders. However, the development of meta-analytic methods has led to the analysis of many single-armed studies. Moreover, we expect that the results of our meta-analysis might contribute to the establishment of Level I or II evidence. Another possible limitation was the potential risk of bias caused by differences in followup periods or loss to followup among studies. To mitigate the possible confounding effects of differences in sample sizes and length of postsurgical followup, we performed a subgroup meta-analysis of studies with followup durations > 5 years and reported rates of bearing dislocation and lateral OA after UKA as standardized rates (reoperation rate per 100 observed component years). This parameter, which averages sample size and followup durations, is a reliable indicator of studies with differences in these two parameters. In assessing the effects of loss to followup, we evaluated the rate in each study and performed metaregression analysis, finding no significant difference in reoperation rates after UKA. Finally, despite efforts to reduce possible bias such as the inclusion of only those studies in which patients underwent Oxford Phase III UKAs, significant heterogeneity was observed.
Although common causes of reoperation differed between Asian and Western patients, the rate of all-cause reoperation after UKA did not differ significantly. The reported reoperation rate in all included studies with a minimum 2-year followup ranged from 0.9% to 11.9%. Many patients underwent reoperation within 5 years, although some required reoperation after > 5 years. For example, one study reported that 25 of 1000 knees underwent reoperation for lateral OA at a mean 7.0 years and a second study reported that six of 129 knees underwent late reoperation as a result of symptomatic lateral OA after a mean followup of 7.5 years. A study from China reported that 13 knees required reoperation, six occurring after 5 years, including one for bearing dislocation and two for lateral OA. These rates of late reoperation suggested the need for subgroup analysis after a followup > 5 years. However, a comparison of the seven Asian and eight Western studies with > 5-year followup found no difference in all-cause reoperation rate. Individual causes of midterm to long-term reoperation, including aseptic loosening, pain of unknown origin, and periprosthetic fracture, require further analysis.
We found a higher rate of reoperation for bearing dislocation in Asian than in Western patients in this systematic review and meta-analysis. Several factors may explain the higher rate of bearing dislocation after UKA in Asian than in Western populations. The most important factor is likely lifestyle. People living in many parts of Asia kneel, squat, sit crosslegged, or sit on the floor during activities of daily living or while performing religious activities. These positions demand a greater range of knee motion than those typically used by Western populations [25, 35]. Hyperflexion, common to daily activities of Asia populations, increases anterior cruciate ligament (ACL) force [40] and may strain the ACL, resulting in anterior subluxation of the proximal tibia [36]. Exposure of knees to the biomechanical environment of deep squatting may induce slight anterior subluxation of the proximal tibia, increasing wear on posterior polyethylene bearings, whereas more limited flexion may have little or no effect [21]. A dislocated bearing may induce deformation of a reduced posterior lip while the intact ACL remains intact [9]. These results suggest that deformation of the posterior lip during deep squatting may lead to bearing dislocation. In addition, the remaining meniscus or osteophytes may impinge on the posterior femoral condyle during repetitive deep squatting with knee hyperflexion exacerbating bearing dislocation [54].
Anthropometric differences between Asian and Western populations also may predispose Asians to higher bearing dislocation rates. In particular, tibias are smaller in East Asian than in Western populations [19]. The design of the Oxford tibial component in Asians showed a tendency toward mediolateral overhang of the resected area of the medial tibial condyle. As the AP dimension of the resected medial tibial condyle increases, so does the mediolateral dimension. However, the relative increase in this dimension is of lower magnitude in Asian than in Western populations [45]. Overhang of the tibial component could lead to a size mismatch between the resected surface of the medial tibial condyle area and the geometry of the tibial component, introducing a space between the implant and soft tissue envelopes. This extra space may increase the likelihood of a bearing dislocation because of the greater possibility of impingement between mobile-bearing and soft tissues or remaining osteophytes [42]. In addition, this space may make the knee environment more susceptible to soft tissue imbalance, one of the most frequent causes of bearing dislocation in UKA. These knees may be susceptible to widening of the medial gap, even after minimal changes in tension on medial soft tissue owing to the inadvertent or overly aggressive release of medial collateral ligaments [14].
We also found that the incidence of progression of lateral OA after UKA was higher in Western than in Asian patients. This finding may be attributable, at least in part, to the higher prevalence of constitutional varus in Asians than in Western patients. This higher prevalence in Asians than in Western patients may, in turn, result from the higher rate of increased femoral varus (lateral) bowing in Asians [42]. Intense knee flexion by Asians during kneeling and deep squatting occurring at the end of their growth spurt, retarding growth of the physis and increasing compression on the medial knee compartment [8, 50, 53], may result in a higher prevalence of varus alignment in Asians than in Western patients. The incidence of constitutional varus alignment has been reported to be approximately 10% higher in Asians than in Western patients (35% versus 25%). This higher rate of constitutional varus in Asians could at least partially offset the valgus alignment occurring after UKA in Asians [41, 42, 55]. Conversely, Western patients show a greater tendency than Asians to have neutral or valgus lower limb alignment. Therefore, after UKA, Asians are less likely to have valgus alignment develop than Western patients, which may explain, at least in part, our finding that the rate of lateral knee OA was higher in Western than in Asian patients.
In conclusion, the current study showed that reoperation for bearing dislocation after UKA was more likely to occur in Asian than in Western populations. Furthermore, reoperation attributable to progression or lateral OA was more frequent in Western than in Asian patients. Nevertheless, total reoperation rates after UKA were similar in Asian and Western populations, perhaps reflecting offsetting of these two revision indications. Although we have offered some possible explanations for these findings, additional randomized, prospective comparative studies are needed. However, better survival outcomes after UKA may require consideration of ethnicity and lifestyle choices in addition to traditional surgical technique and perioperative care.
Acknowledgments
We thank Woo Joo Jeon MD, PhD, of the Department of Orthopaedic Surgery at Bon-Bridege Hospital, Seoul, Korea, for searching relevant studies and reviewing their titles and abstracts.
Footnotes
Each author certifies that neither he, nor any member of his immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
References
- 1.Altman DG, Schulz KF, Moher D, Egger M, Davidoff F, Elbourne D, Gotzsche PC, Lang T. The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Ann Intern Med. 2001;134:663–694. [DOI] [PubMed] [Google Scholar]
- 2.Baauw M, van Hooff ML, Spruit M. Current construct options for revision of large acetabular defects: a systematic review. JBJS Rev. 2016;4. [DOI] [PubMed] [Google Scholar]
- 3.Bergeson AG, Berend KR, Lombardi AV, Jr, Hurst JM, Morris MJ, Sneller MA. Medial mobile bearing unicompartmental knee arthroplasty: early survivorship and analysis of failures in 1000 consecutive cases. J Arthroplasty. 2013;28:172–175. [DOI] [PubMed] [Google Scholar]
- 4.Bottomley N, Jones LD, Rout R, Alvand A, Rombach I, Evans T, Jackson WF, Beard DJ, Price AJ. A survival analysis of 1084 knees of the Oxford unicompartmental knee arthroplasty: a comparison between consultant and trainee surgeons. Bone Joint J. 2016;98:22–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brown NM, Sheth NP, Davis K, Berend ME, Lombardi AV, Berend KR, Della Valle CJ. Total knee arthroplasty has higher postoperative morbidity than unicompartmental knee arthroplasty: a multicenter analysis. J Arthroplasty. 2012;27:86–90. [DOI] [PubMed] [Google Scholar]
- 6.Burnett RS, Nair R, Hall CA, Jacks DA, Pugh L, McAllister MM. Results of the Oxford Phase 3 mobile bearing medial unicompartmental knee arthroplasty from an independent center: 467 knees at a mean 6-year follow-up: analysis of predictors of failure. J Arthroplasty. 2014;29:193–200. [DOI] [PubMed] [Google Scholar]
- 7.Cepni SK, Arslan A, Polat H, Yalcin A, Parmaksizoglu AS. Mid-term results of Oxford Phase 3 unicompartmental knee arthroplasty in obese patients. Acta Orthop Traumatol Turc. 2014;48:122–126. [DOI] [PubMed] [Google Scholar]
- 8.Cheng JC, Chan PS, Chiang SC, Hui PW. Angular and rotational profile of the lower limb in 2,630 Chinese children. J Pediatr Orthop. 1991;11:154–161. [DOI] [PubMed] [Google Scholar]
- 9.Choy WS, Kim KJ, Lee SK, Yang DS, Lee NK. Mid-term results of Oxford medial unicompartmental knee arthroplasty. Clin Orthop Surg. 2011;3:178–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clement ND, Duckworth AD, MacKenzie SP, Nie YX, Tiemessen CH. Medium-term results of Oxford phase-3 medial unicompartmental knee arthroplasty. J Orthop Surg (Hong Kong). 2012;20:157–161. [DOI] [PubMed] [Google Scholar]
- 11.Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. 2000;10:2–11. [DOI] [PubMed] [Google Scholar]
- 12.Dalury DF, Fisher DA, Adams MJ, Gonzales RA. Unicompartmental knee arthroplasty compares favorably to total knee arthroplasty in the same patient. Orthopedics. 2009;32. [PubMed] [Google Scholar]
- 13.Emerson R, Alnachoukati O, Barrington J, Ennin K. The results of Oxford unicompartmental knee arthroplasty in the United States: a mean ten-year survival analysis. Bone Joint J. 2016;98:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Emerson RH., Jr Unicompartmental mobile-bearing knee arthroplasty. Instr Course Lect. 2005;54:221–224. [PubMed] [Google Scholar]
- 15.Faour-Martin O, Valverde-Garcia JA, Martin-Ferrero MA, Vega-Castrillo A, de la Red Gallego MA, Suarez de Puga CC, Amigo-Linares L. Oxford phase 3 unicondylar knee arthroplasty through a minimally invasive approach: long-term results. Int Orthop. 2013;37:833–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fisher DA, Dalury DF, Adams MJ, Shipps MR, Davis K. Unicompartmental and total knee arthroplasty in the over 70 population. Orthopedics. 2010;33:668. [DOI] [PubMed] [Google Scholar]
- 17.Heller S, Fenichel I, Salai M, Luria T, Velkes S. The Oxford unicompartmental knee prosthesis for the treatment of medial compartment knee disease: 2 to 5 year follow-up. Isr Med Assoc J. 2009;11:266–268. [PubMed] [Google Scholar]
- 18.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ji JH, Park SE, Song IS, Kang H, Ha JY, Jeong JJ. Complications of medial unicompartmental knee arthroplasty. Clin Orthop Surg. 2014;6:365–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khanna A, Gougoulias N, Longo UG, Maffulli N. Minimally invasive total knee arthroplasty: a systematic review. Orthop Clin North Am. 2009;40:479–489, viii. [DOI] [PubMed] [Google Scholar]
- 21.Kim JM, Moon MS. Squatting following total knee arthroplasty. Clin Orthop Relat Res. 1995;313:177–186. [PubMed] [Google Scholar]
- 22.Kim KT, Lee S, Kim JH, Hong SW, Jung WS, Shin WS. The survivorship and clinical results of minimally invasive unicompartmental knee arthroplasty at 10-year follow-up. Clin Orthop Surg. 2015;7:199–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kristensen PW, Holm HA, Varnum C. Up to 10-year follow-up of the Oxford medial partial knee arthroplasty: 695 cases from a single institution. J Arthroplasty. 2013;28:195–198. [DOI] [PubMed] [Google Scholar]
- 24.Kuipers BM, Kollen BJ, Bots PC, Burger BJ, van Raay JJ, Tulp NJ, Verheyen CC. Factors associated with reduced early survival in the Oxford phase III medial unicompartment knee replacement. Knee. 2010;17:48–52. [DOI] [PubMed] [Google Scholar]
- 25.Kurosaka M, Yoshiya S, Mizuno K, Yamamoto T. Maximizing flexion after total knee arthroplasty: the need and the pitfalls. J Arthroplasty. 2002;17:59–62. [DOI] [PubMed] [Google Scholar]
- 26.Labek G, Thaler M, Janda W, Agreiter M, Stockl B. Revision rates after total joint replacement: cumulative results from worldwide joint register datasets. J Bone Joint Surg Br. 2011;93:293–297. [DOI] [PubMed] [Google Scholar]
- 27.Laurencin CT, Zelicof SB, Scott RD, Ewald FC. Unicompartmental versus total knee arthroplasty in the same patient. A comparative study. Clin Orthop Relat Res. 1991;273:151–156. [PubMed] [Google Scholar]
- 28.Lim HC, Bae JH, Song SH, Kim SJ. Oxford phase 3 unicompartmental knee replacement in Korean patients. J Bone Joint Surg Br. 2012;94:1071–1076. [DOI] [PubMed] [Google Scholar]
- 29.Lisowski LA, Meijer LI, Bekerom MP, Pilot P, Lisowski AE. Ten- to 15-year results of the Oxford Phase III mobile unicompartmental knee arthroplasty: a prospective study from a non-designer group. Bone Joint J. 2016;98:41–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lloyd JM, Watts MC, Stokes AP, Peden SA, McMeniman PJ, Myers PT. Medium term results of per-operative knee arthroscopy in confirming suitability for unicompartmental arthroplasty. Knee. 2012;19:908–912. [DOI] [PubMed] [Google Scholar]
- 31.Luscombe KL, Lim J, Jones PW, White SH. Minimally invasive Oxford medial unicompartmental knee arthroplasty. A note of caution! Int Orthop. 2007;31:321–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Matharu G, Robb C, Baloch K, Pynsent P. The Oxford medial unicompartmental knee replacement: survival and the affect of age and gender. Knee. 2012;19:913–917. [DOI] [PubMed] [Google Scholar]
- 33.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–341. [DOI] [PubMed] [Google Scholar]
- 34.Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mulholland SJ, Wyss UP. Activities of daily living in non-Western cultures: range of motion requirements for hip and knee joint implants. Int J Rehabil Res. 2001;24:191–198. [DOI] [PubMed] [Google Scholar]
- 36.Mullaji AB, Shetty GM, Kanna R. Postoperative limb alignment and its determinants after minimally invasive Oxford medial unicompartmental knee arthroplasty. J Arthroplasty. 2011;26:919–925. [DOI] [PubMed] [Google Scholar]
- 37.Oiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37:1434–1443. [DOI] [PubMed] [Google Scholar]
- 38.Pandit H, Hamilton TW, Jenkins C, Mellon SJ, Dodd CA, Murray DW. The clinical outcome of minimally invasive Phase 3 Oxford unicompartmental knee arthroplasty: a 15-year follow-up of 1000 UKAs. Bone Joint J. 2015;97:1493–1500. [DOI] [PubMed] [Google Scholar]
- 39.Pietschmann MF, Wohlleb L, Weber P, Schmidutz F, Ficklscherer A, Gulecyuz MF, Safi E, Niethammer TR, Jansson V, Muller PE. Sports activities after medial unicompartmental knee arthroplasty Oxford III—what can we expect? Int Orthop. 2013;37:31–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Senter C, Hame SL. Biomechanical analysis of tibial torque and knee flexion angle: implications for understanding knee injury. Sports Med. 2006;36:635–641. [DOI] [PubMed] [Google Scholar]
- 41.Shetty GM, Mullaji A, Bhayde S, Nha KW, Oh HK. Factors contributing to inherent varus alignment of lower limb in normal Asian adults: role of tibial plateau inclination. Knee. 2014;21:544–548. [DOI] [PubMed] [Google Scholar]
- 42.Song M-H, Yoo S-H, Kang S-W, Kim Y-J, Park G-T, Pyeun Y-S. Errata to ‘Coronal Alignment of the Lower Limb and the Incidence of Constitutional Varus Knee in Korean Females.’ Knee Surg Relat Res. 2015;27:197–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Song MH, Kim BH, Ahn SJ, Yoo SH, Lee MS. Early complications after minimally invasive mobile-bearing medial unicompartmental knee arthroplasty. J Arthroplasty. 2009;24:1281–1284. [DOI] [PubMed] [Google Scholar]
- 44.Streit MR, Streit J, Walker T, Bruckner T, Philippe Kretzer J, Ewerbeck V, Merle C, Aldinger PR, Gotterbarm T. Minimally invasive Oxford medial unicompartmental knee arthroplasty in young patients. Knee Surg Sports Traumatol Arthrosc. 2017;25:660–668. [DOI] [PubMed] [Google Scholar]
- 45.Surendran S, Kwak DS, Lee UY, Park SE, Gopinathan P, Han SH, Han CW. Anthropometry of the medial tibial condyle to design the tibial component for unicondylar knee arthroplasty for the Korean population. Knee Surg Sports Traumatol Arthrosc. 2007;15:436–442. [DOI] [PubMed] [Google Scholar]
- 46.Tian S, Liu J, Yuan W, Wang Y, Ha C, Liu L, Li Q, Yang X, Sun K. Minimally invasive unicompartmental knee replacement: Midterm clinical outcome. PLoS One. 2017;12:e0176082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vandenbroucke JP, von Elm E, Altman DG, Gotzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology. 2007;18:805–835. [DOI] [PubMed] [Google Scholar]
- 48.Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. 2010;36:1–48. [Google Scholar]
- 49.Wallace BC, Dahabreh IJ, Trikalinos TA, Lau J, Trow P, Schmid CH. Closing the gap between methodologists and end-users: R as a computational back-end. J Stat Softw. 2012;49:1–15. [Google Scholar]
- 50.Witvrouw E, Danneels L, Thijs Y, Cambier D, Bellemans J. Does soccer participation lead to genu varum? Knee Surg Sports Traumatol Arthrosc. 2009;17:422–427. [DOI] [PubMed] [Google Scholar]
- 51.Xu T, Lao Y, Wang J, Liu F, Xiao L, Tong P. Mid-term results of Oxford phase-3 medial unicompartmental knee arthroplasty for medial arthritis in Chinese patients. ANZ J Surg. 2017;87:287–290. [DOI] [PubMed] [Google Scholar]
- 52.Xue H, Tu Y, Ma T, Wen T, Yang T, Cai M. Up to twelve year follow-up of the Oxford phase three unicompartmental knee replacement in China: seven hundred and eight knees from an independent centre. Int Orthop. 2017;41:1571–1577. [DOI] [PubMed] [Google Scholar]
- 53.Yoo JH, Choi IH, Cho TJ, Chung CY, Yoo WJ. Development of tibiofemoral angle in Korean children. J Korean Med Sci. 2008;23:714–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yoshida K, Tada M, Yoshida H, Takei S, Fukuoka S, Nakamura H. Oxford phase 3 unicompartmental knee arthroplasty in Japan—clinical results in greater than one thousand cases over ten years. J Arthroplasty. 2013;28:168–171. [DOI] [PubMed] [Google Scholar]
- 55.Yoshida S, Aoyagi K, Felson DT, Aliabadi P, Shindo H, Takemoto T. Comparison of the prevalence of radiographic osteoarthritis of the knee and hand between Japan and the United States. J Rheumatol. 2002;29:1454–1458. [PubMed] [Google Scholar]