Abstract
Background
Sagittal spinopelvic balance and proper sagittal alignment are important when planning corrective or reconstructive spinal surgery. Prior research suggests that people from different races and countries have moderate divergence; to the best of our knowledge, the population of Taiwan has not been studied with respect to this parameter.
Questions/purposes
To investigate normal age- and sex-related differences in whole-spine sagittal alignment and balance of asymptomatic adults without spinal disorders.
Methods
In this prospective study, we used convenience sampling to recruit asymptomatic volunteers who accompanied patients in the outpatient orthopaedic department. One hundred forty males with a mean age of 48 ± 19 years and 252 females with a mean age of 53 ± 17 years underwent standing lateral radiographs of the whole spine. For analysis, participants were divided in three groups by age (20 to 40 years, 41 to 60 years, and 61 to 80 years) and analyzed by sex (male and female). The following eight radiologic parameters were measured: sacral slope, pelvic tilt, pelvic incidence, thoracic kyphosis, lumbar lordosis, cervical lordosis, C2-C7 sagittal vertical axis, and C7-S1 sagittal vertical axis. Three observers performed estimations of the sagittal parameters twice, and the intraclass correlation coefficients for inter- and intraobserver variability were 0.81 and 0.83.
Results
The mean pelvic incidence was 49° ± 12°; lumbar lordosis was smaller in the group that was 61 to 80 years old than in the groups that were 20 to 40 years and 41 to 60 years (95% CI of the difference, 4.50–13.64 and 1.00– 9.60; p < 0.001), while cervical lordosis was greater in the 61 to 80 years age group than the other two groups (95% CI of the difference, -14.64 to -6.57 and -11.57 to -3.45; p < 0.001). The mean C7-S1 sagittal vertical axis was 30 ± 29 mm, and there was no difference among the three groups and between males and females. Pelvic tilt was greater in the group 61 to 80 years old than the 20 to 40 years and 41 to 60 years age groups (95% CI of the difference, -10.81 to -5.42 and -7.15 to -2.08; p < 0.001), while sacral slope was larger in 61 to 80 years age group than in the 41 to 60 years group (95% CI of the difference, 0.79–6.25; p = 0.006). C7 slope was greater in 61 to 80 years age group than in the 20 to 40 years group (95% CI of the difference, -7.49 to -1.26; p = 0.002) and larger in 41 to 60 years age group than in 20 to 40 years group (95% CI of the difference, -6.31 to -0.05; p = 0.045). C2-C7 sagittal vertical axis was greater in males than in females (95% CI of the difference, 2.84–7.74; p < 0.001). C7 slope was negatively correlated with thoracic kyphosis (95% CI of the difference, -0.619 to 0.468; p < 0.001) and lumbar lordosis (95% CI of the difference, -0.356 to -0.223; p < 0.001), and positively correlated with pelvic incidence (95% CI of the difference, 0.058– 0.215; p < 0.001) and cervical lordosis (95% CI of the difference, 0.228 – 0.334; p < 0.001).
Conclusions
Normal values of the spinopelvic sagittal parameters vary by age and sex in Taiwanese individuals.
Clinical Relevance
Pelvic incidence and sacral slope observed in this population seemed smaller than those reported in other studies of white populations; this seems important when considering spine surgery in Taiwanese patients. Future studies should include collection of whole body sagittal parameters of larger and more-diverse populations, and assessments of patients with symptomatic spinal disorders.
Introduction
Sagittal alignment of the whole spine is reported to be closely related to quality-of-life scores, and malalignment is known to cause back pain and disability [3]. Health-related quality of life correlates with sagittal alignment of the spine as assessed by radiographic parameters, and improvement in sagittal alignment has been reported to be associated with substantial clinical benefits and patient-reported outcomes [2, 21, 25]. In addition to spinal curves, the shape of the pelvis also plays a key role in this linear chain aligning the head and the hips on the sagittal plane [1]. Sagittal plane alignment of the spine and orientation of the pelvis are composed of a set of segments linked together to maintain stable posture with minimum energy expenditure [5]. Sacral slope, pelvic tilt, and pelvic incidence are used to depict the shape and orientation of the pelvis, whereas cervical lordosis, thoracic kyphosis, and lumbar lordosis constitute sagittal alignment of the whole spine [16]. C7-S1 sagittal vertical axis indicates the shape of the standing posture, which could be affected by compensating for sagittal alignment [22]. Pelvic incidence is closely related to the shape of the lumbar spine, as evidenced by several formulas that use mismatched values between pelvic incidence and lumbar lordosis to predict ideal lumbar sagittal alignment [13]. Cervical lordosis is known to be influenced by C7 or T1 slope and C2-C7 sagittal vertical axis, which are key determining factors of cervical sagittal alignment [15].
The results of studies of spinopelvic parameters in asymptomatic adults vary among different countries and different races. Legaye and Duval-Beaupère [16] reported that the mean value of pelvic incidence was 53° in normal adult men and 48° in normal adult women, respectively. Vialle et al. [27] reported a mean value of 54° for pelvic incidence from 300 asymptomatic subjects and Mac-Thiong et al. [17] reported a mean pelvic incidence of 53° for 709 asymptomatic adults. Lee et al. [14] reported a mean pelvic incidence of 48° in a Korean young adult population; by contrast, Zhu et al. [29] reported a mean pelvic incidence of 44° in a Chinese adult population. There were no related radiographic data of Taiwanese asymptomatic adults, which may provide a reference for adequate correction of adult spinal deformity of Taiwanese individuals and comparison to other Asian groups in different countries. In addition, to the best of our knowledge, there are no published studies regarding the relationships among cervical regional alignment, thoracolumbar regional alignment, and whole spine alignment and on the difference between different age groups or sex in asymptomatic adults, and little is known about these parameters in Taiwanese or other ethnic populations.
We therefore examined the relationships between sagittal alignment of the regional spine, the whole spine, and spinopelvic region in asymptomatic Taiwanese adults and the correlation of these parameters with age and sex.
Patients and Methods
This research was approved by the Research Ethics Committee of Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation (IRB103-189-B) under the professional supervision of a senior radiologist (D-WL). The explanation of the radiation dose of whole spine radiographs was part of the informed-consent process for study subjects. We also explained the risk of radiation exposure to the volunteers in detail before they provided informed consent. Asymptomatic volunteers aged 20 to 80 years with no back or neck pain were included in the study. We used a convenience sampling method of individuals who accompanied our patients in the orthopaedic department. Participants were excluded from the study if they fulfilled any of the following criteria: (1) Cobb angle of 10° or greater in the coronal plane; (2) a history of major surgeries of the spine, hip, or knees such as joint replacement, ligament reconstruction, fracture fixation, or spinal fusion; (3) a history of neuromuscular disorders or inflammatory arthritis; (4) recent back pain, neck pain, or lower extremity pain that influenced activities of daily living resulting in dependence on narcotics; (5) inability to stand without assistance; and (6) pregnancy. The imaging was performed at Hualien Tzu-Chi Hospital. The volunteers were divided in three age groups, namely 20 to 40 years, 41 to 60 years, and 61 to 80 years.
Images of the spine were obtained with the participant standing straight with the knees fully extended, with elbow flexion, and putting both hands on the chest. A standing spine lateral radiograph of each participant was taken with standard triple film. The hip and cervical spine were included.
The measured parameters on the radiographs include: (1) sacropelvic parameters: pelvic tilt, sacral slope, and pelvic incidence; (2) regional spine parameters: lumbar lordosis calculated as the Cobb angle between L1 and S1 superior endplates, thoracic kyphosis calculated as the Cobb angle between the T5 and T12 inferior endplates, cervical lordosis calculated as the Cobb angle between the C2 and C7 inferior endplates, C7 slope calculated as the angle between the horizontal plane and C7 superior endplate, and C2-C7 sagittal vertical axis calculated as the distance between a plumb line from the center of the C2 vertebral body and posterior superior corner of the C7; (3) spinopelvic parameter: the mismatch between pelvic incidence and lumbar lordosis; and (4) the whole spine parameter: C7-S1 sagittal vertical axis calculated as the distance between a plumb line from the center of the C7 vertebral body and posterosuperior corner of the sacrum. Three orthopaedic surgeons (K-TY, C-HP, and K-LL) performed the estimations of the sagittal parameters, and each of them assessed the images twice. Intraclass correlation coefficient method (ICC) was calculated for inter- and intraobserver variability. Intra- and interobserver ICCs for estimating the spinopelvic sagittal parameters were 0.81 and 0.83, suggesting high reliability of these measurements using these three observers.
A total of 392 participants, 140 males and 252 females, were included in the study. The numbers of participants in the 20 to 40, 41 to 60, and 61 to 80 years age groups were 114, 135, and 143, respectively. The mean ages of participants in these three groups were 28 ± 7 years, 52 ± 5 years, and 69 ± 6 years, respectively, and there were no differences in the male to female ratios among these groups.
Statistical Analysis
Statistical analyses were performed using SPSS Version 17.0; SPSS Inc, Chicago, IL, USA). All values are expressed as mean ± SD, and all error bars represent the SD of the mean. The comparisons between males and females overall, and between the three age groups, were performed using one-way ANOVA followed by post hoc Bonferroni correction. The mean, SD, and 95% CI were provided. Correlations between C7 slope and thoracic kyphosis, pelvic incidence, lumbar lordosis, and cervical lordosis were assessed using a generalized linear model for calculation of the regression coefficients. A probability less than 0.05 was considered statistically significant.
Results
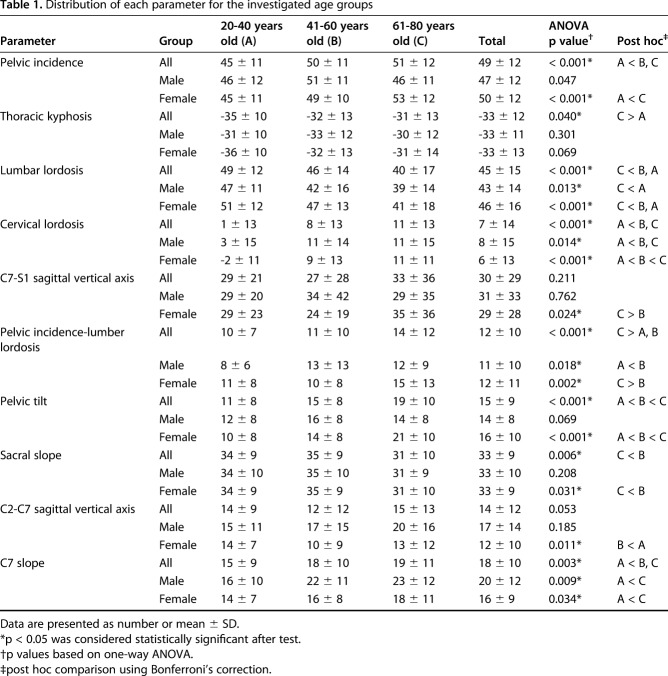
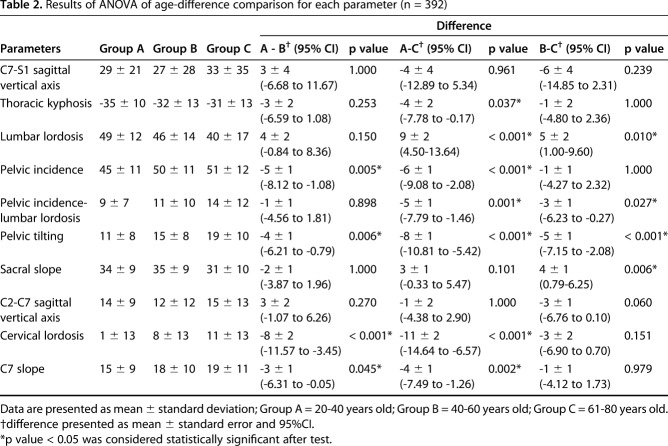
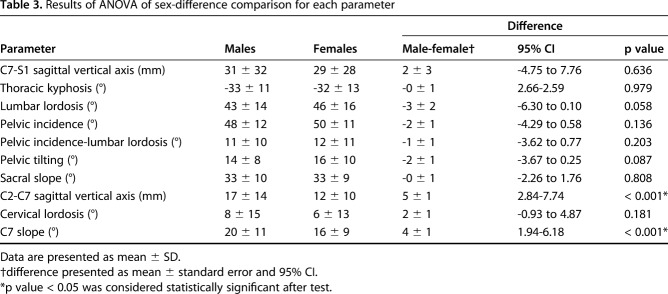
The mean pelvic incidence of all volunteers was 49° ± 12° (Table 1), and there was no difference among the three age groups (48° ± 11° versus 50° ± 11° versus; p = 0.136) (Table 2) and no differences between males and females (48° ± 11° versus 50° ± 11°; p = 0.136) (Table 3). Thoracic kyphosis is smaller in 20 to 40 years age group than in 61 to 80 years group (-35° ± 10° versus -31° ± 13°; 95% CI of the difference, -7.78 to -0.17; p = 0.040) (Table 1). Lumbar lordosis was the smaller in the 61 to 80 years age group than the 20 to 40 years and 41 to 60 years age groups (40° ± 17° versus 49° ± 12° and 46° ± 14°; 95% CI of the difference, 4.50–13.64 and 1.00– 9.60; p < 0.001 and = 0.010), while cervical lordosis was greater in the 61 to 80 years age group than in the other two groups (11° ± 13° versus 8° ± 13° and 1° ± 13°; 95% CI of the difference, -14.64 to -6.57 and -11.57 to -3.45; p < 0.001 and < 0.001) (Table 2). The mean C7-S1 sagittal vertical axis was 30 ± 29 mm (Table 1), and there was no difference between the three groups (29 ± 21 mm versus 27 ± 28 mm versus 33 ± 36 mm; p < 0.211) (Table 2) and no difference between males and females (31 ± 32 versus 29 ± 28 mm; p = 0.636) (Table 3). Pelvic incidence-lumber lordosis was 12° ± 10° and the value of the 61 to 80 years group was larger than that of the 41 to 60 years group (14° ± 12° versus 11°±10°; 95% CI of the difference, -6.23 to -0.27; p = 0.027) and the value of the 61 to 80 years group was larger than that of the 20 to 40 years group (14° ± 12° versus 9° ± 7°; 95% CI of the difference, -7.79 to -1.46; p = 0.001) (Table 2). Pelvic tilt was greater in the 61 to 80 years group than in the 20 to 40 years and 41 to 60 years groups (19° ± 10° versus 15° ± 8° and 11° ± 8°; 95% CI of the difference, -10.81 to -5.42 and -7.15 to -2.08; p < 0.001 and < 0.001), while sacral slope was larger in the 61 to 80 years group than in the 41 to 60 years group (11° ± 13° versus 35° ± 9° and 31° ± 10°; 95% CI of the difference, 0.79–6.25; p = 0.006) (Table 2). Mean C7 slope was 18° ± 10° (Table 1) and was larger in the 61 to 80 years group than in the 20 to 40 years group (19° ± 11° versus 15° ± 9°; 95% CI of the difference, -7.49 to -1.26; p = 0.002) and larger in the 41 to 60 years group than in the 20 to 40 years group (18° ± 10° versus 15° ± 9°; 95% CI of the difference, -6.31 to -0.05; p = 0.045) (Table 2). The mean C2-C7 sagittal vertical axis was 14 ± 12 mm and the value was greater in males than in females (17 ± 14 mm versus 12 ± 10 mm; 95% CI of the difference, 2.84 –7.74; p < 0.001).
Table 1.
Distribution of each parameter for the investigated age groups
Table 2.
Results of ANOVA of age-difference comparison for each parameter (n = 392)
Table 3.
Results of ANOVA of sex-difference comparison for each parameter
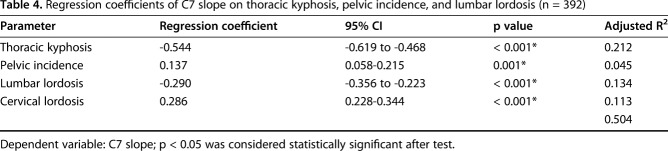
Multiple regression analysis was performed to examine the relationships between C7 slope and the other radiographic parameters, such as thoracic kyphosis (regression coefficient, -0.544; 95% CI of the difference, -0.619 to 0.468; p < 0.001) , pelvic incidence (regression coefficient, 0.137; 95% CI of the difference, 0.058– 0.215; p < 0.001), lumbar lordosis (regression coefficient, -0.290; 95% CI of the difference, -0.356 to -0.223; p < 0.001), and cervical lordosis (regression coefficient, 0.286; 95% CI of the difference, 0.228 0.334; p < 0.001). These parameters were all correlated with C7 slope (adjusted R2 = 0.504; p < 0.001) (Table 4).
Table 4.
Regression coefficients of C7 slope on thoracic kyphosis, pelvic incidence, and lumbar lordosis (n = 392)
Discussion
Pelvic incidence is the primary pelvic anatomic parameter that is specific and constant for each adult [11, 20]. It is important for planning spinal alignment when a patient is evaluated for major spinal correction surgery [23, 24]. C7 slope also is important for overall sagittal alignment, as it acts as a link between the occipitocervical and thoracolumbar spine and may anticipate the future of the spinal sagittal alignment after fusion surgeries [18]. In this cross-sectional study, we evaluated asymptomatic Taiwanese volunteers and compared them by age and sex. The mean pelvic incidence and sacral slope observed in this study seemed to be consistent with values reported in other studies of Asian groups [4, 14] and smaller than values reported in studies of white populations [16, 27]. Lumbar lordosis seems to be smaller and cervical lordosis seems to be larger in the 61 to 80 years group, and the difference between lumbar lordosis and pelvic incidence seems to be larger in the 61 to 80 years group. These changes may be attributable to vertebral disc degeneration and vertebral body compression fracture during aging. Thoracic kyphosis and cervical lordosis seem to have greater influence on C7 slope than lumbar lordosis and pelvic incidence. This finding may indicate that the changes of regional spinal curves influence each other during aging or surgical intervention.
This study had some limitations. First, some of the standard differences were larger than the mean values, although the intra- or interobserver reliability seem to be acceptable. This may be caused by variations of the body shape of the different individuals. This can be improved in future studies by increasing the sample size. Second, this study only includes asymptomatic Taiwanese adults. Although we found the correlations between the spinopelvic sagittal parameters differentiated by age and sex, these findings may not generalize to other patient groups in clinical application owing to the small population and narrow ethnicity. Third, whole-spine radiographs cannot account for several important elements of standing posture, such as lower-extremity compensatory changes, which obviously do not appear on radiographs of the spine itself [8]. Global sagittal alignment parameters from head to foot should be evaluated in future studies using full-body plain radiographs. Although the pelvis has been widely accepted as the regulator of spinal alignment [22], degenerative changes in the thoracolumbar spine also can be affected by the lower extremities and the cervical spine [8].
Because sagittal parameters such as thoracic kyphosis and lumbar lordosis varied in our asymptomatic population, it is not feasible to evaluate the abnormalities of sagittal alignment based solely on these measurements. For horizontal gaze, standing, and walking, other regional spine curves would change to compensate for loss of lumbar lordosis. The changes in the regional alignments seem to be compensatory to each other; therefore, the C7-S1 sagittal vertical axis has little difference among the three age groups. We found that the compensating increase in cervical lordosis contributed more than that of thoracic kyphosis. This finding is consistent with findings in another study in which the change was reported to be approximately 10° between people 30 to 70 years old [28]. Previous studies have suggested that worsening of sagittal alignment originates in the pelvis in women and the cervical spine in men among volunteers older than 50 years [19], and global sagittal alignment and C7-S1 sagittal vertical axis increased, whereas lumbar lordosis decreased with age [8]. Glassman et al. [6, 7] showed that increased C7-S1 sagittal vertical axis correlated to a higher level of disability and the mean normal value was approximately 50 mm. These findings indicate that a good compensatory mechanism between the regional spinal alignments exists in asymptomatic aging people. These concepts provide important consideration for spine fusion surgery that may change regional alignment [20].
T1 slope, as the inherent compensatory mechanisms for the relationship between the upper and lower cervical spine, is important for overall balance of cervical sagittal alignment and seems to have no substantial differences among asymptomatic, symptomatic, and surgically treated patients [20]. Oe et al. [19] suggested that T1 slope increased the C2-C7 lordotic angle, and the increased C2-C7 lordosis may keep the C2-C7 sagittal vertical axis decreased by a continuous and compensatory principle. However, the T1 slope is not always visible because of the obstruction of the shoulder and thoracic regions on upright lateral radiographs. CT might provide more clarity regarding the T1 slope, but patients usually are supine for this test. The C7 slope was more visible on the standing lateral plain film and found to be a potential substitute for T1 slope [26]. Nunez-Pereira et al. [18] found that the C7 slope was a useful marker of overall sagittal alignment by acting as a link between the occipitocervical and thoracolumbar spine, so the C7 slope may be an indicator of global sagittal thoracolumbar balance for patients undergoing reconstructive spine surgery. We also found that cervical lordosis and C7 slope were greater in the older age group. The relationship between these parameters may guide the spine surgeon as he or she sets the proper fusion angle for patients [9]. The thoracic spine could be the important junctional region of whole-spine alignment. Previous research suggests that changes in thoracic kyphosis negatively affect sagittal alignment after lumbar pedicle subtraction osteotomy [12]. Thoracic kyphosis can increase by as much as 18° after surgery for degenerative lumbar flat back [10].
We found that sagittal radiographic parameters in asymptomatic Taiwanese adults differ by age and sex. In addition, pelvic incidence and sacral slope observed in this population seemed smaller than in other studies describing white populations [11, 27]; this seems important when considering spine surgery in Taiwanese patients. This concept is important because different surgical correction strategies may be appropriate in patients of different ages and sexes based on the relationships we observed. In addition, cervical regional parameters, such as C7 slope, appeared to correlate with other spinopelvic parameters to varying degrees; this is important because the postoperative C7 slope can anticipate the future of the corrected spinal sagittal alignment [18, 26]. As ours was a pilot study, we suggest that a larger and more-diverse population-based study (including patients of other races and ethnicities) should be performed to confirm and extend our findings. In addition, studies of symptomatic patients may provide more useful information regarding whole-body sagittal balance in the setting of spinal disorders, which may be more informative for planning surgical reconstructions for spinal deformities. Even so, our findings can inform spine surgeons’ decisions about regional alignment for patients of different sexes and ages.
Acknowledgments
We acknowledge Wallace Academic Editing (Taipei, Taiwan, Republic of China) for editing the manuscript; and Dai-Wei Liu MD, PhD (Radiation Oncology, the senior radiologist from the Research Ethics Committee of Hualien Tzu Chi Hospital).
Footnotes
Each author certifies that he, or a member of his immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Hualien Tzu Chi Hospital, Buddhist Tzu Chi Medical Foundation, Taiwan, Republic of China.
References
- 1.Berthonnaud E, Dimnet J, Roussouly P, Labelle H. Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech. 2005;18:40–47. [DOI] [PubMed] [Google Scholar]
- 2.Blondel B, Schwab F, Ungar B, Smith J, Bridwell K, Glassman S, Shaffrey C, Farcy JP, Lafage V. Impact of magnitude and percentage of global sagittal plane correction on health-related quality of life at 2-years follow-up. Neurosurgery. 2012;71:341–348; discussion 348. [DOI] [PubMed] [Google Scholar]
- 3.Diebo BG, Varghese JJ, Lafage R, Schwab FJ, Lafage V. Sagittal alignment of the spine: what do you need to know? Clin Neurol Neurosurg. 2015;139:295–301. [DOI] [PubMed] [Google Scholar]
- 4.Endo K, Suzuki H, Nishimura H, Tanaka H, Shishido T, Yamamoto K. Characteristics of sagittal spino-pelvic alignment in Japanese young adults. Asian Spine J. 2014;8:599–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ghandhari H, Hesarikia H, Ameri E, Noori A. Assessment of normal sagittal alignment of the spine and pelvis in children and adolescents. Biomed Res Int. 2013;2013:842624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976). 2005;30:682–688. [DOI] [PubMed] [Google Scholar]
- 7.Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976). 2005;30:2024–2029. [DOI] [PubMed] [Google Scholar]
- 8.Iyer S, Lenke LG, Nemani VM, Albert TJ, Sides BA, Metz LN, Cunningham ME, Kim HJ. Variations in sagittal alignment parameters based on age: a prospective study of asymptomatic volunteers using full-body radiographs. Spine (Phila Pa 1976). 2016;41:1826–1836. [DOI] [PubMed] [Google Scholar]
- 9.Jang JS, Lee SH, Min JH, Kim SK, Han KM, Maeng DH. Surgical treatment of failed back surgery syndrome due to sagittal imbalance. Spine (Phila Pa 1976). 2007;32:3081–3087. [DOI] [PubMed] [Google Scholar]
- 10.Jang JS, Lee SH, Min JH, Maeng DH. Influence of lumbar lordosis restoration on thoracic curve and sagittal position in lumbar degenerative kyphosis patients. Spine (Phila Pa 1976). 2009;34:280–284. [DOI] [PubMed] [Google Scholar]
- 11.Jean L. Influence of age and sagittal balance of the spine on the value of the pelvic incidence. Eur Spine J. 2014;23:1394–1399. [DOI] [PubMed] [Google Scholar]
- 12.Lafage V, Ames C, Schwab F, Klineberg E, Akbarnia B, Smith J, Boachie-Adjei O, Burton D, Hart R, Hostin R, Shaffrey C, Wood K, Bess S; International Spine Study Group. Changes in thoracic kyphosis negatively impact sagittal alignment after lumbar pedicle subtraction osteotomy: a comprehensive radiographic analysis. Spine (Phila Pa 1976). 2012;37:E180–E187. [DOI] [PubMed] [Google Scholar]
- 13.Lafage V, Schwab F, Patel A, Hawkinson N, Farcy JP. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976). 2009;34:E599–E606. [DOI] [PubMed] [Google Scholar]
- 14.Lee CS, Chung SS, Kang KC, Park SJ, Shin SK. Normal patterns of sagittal alignment of the spine in young adults radiological analysis in a Korean population. Spine (Phila Pa 1976). 2011;36:E1648–E1654. [DOI] [PubMed] [Google Scholar]
- 15.Lee SH, Son ES, Seo EM, Suk KS, Kim KT. Factors determining cervical spine sagittal balance in asymptomatic adults: correlation with spinopelvic balance and thoracic inlet alignment. Spine J. 2015;15:705–712. [DOI] [PubMed] [Google Scholar]
- 16.Legaye J, Duval-Beaupère G. Sagittal plane alignment of the spine and gravity: a radiological and clinical evaluation. Acta Orthop Belg. 2005;71:213–220. [PubMed] [Google Scholar]
- 17.Mac-Thiong JM, Roussouly P, Berthonnaud E, Guigui P. Age- and sex-related variations in sagittal sacropelvic morphology and balance in asymptomatic adults. Eur Spine J. 2011;20:572–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nunez-Pereira S, Hitzl W, Bullmann V, Meier O, Koller H. Sagittal balance of the cervical spine: an analysis of occipitocervical and spinopelvic interdependence, with C-7 slope as a marker of cervical and spinopelvic alignment. J Neurosurg Spine. 2015;23:16–23. [DOI] [PubMed] [Google Scholar]
- 19.Oe S, Togawa D, Nakai K, Yamada T, Arima H, Banno T, Yasuda T, Kobayasi S, Yamato Y, Hasegawa T, Yoshida G, Matsuyama Y. The influence of age and sex on cervical spinal alignment among volunteers aged over 50. Spine (Phila Pa 1976). 2015;40:1487–1494. [DOI] [PubMed] [Google Scholar]
- 20.Park JH, Cho CB, Song JH, Kim SW, Ha Y, Oh JK. T1 Slope and cervical sagittal alignment on cervical CT radiographs of asymptomatic persons. J Korean Neurosurg Soc. 2013;53:356–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roussouly P, Nnadi C. Sagittal plane deformity: an overview of interpretation and management. Eur Spine J. 2010;19:1824–1836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schwab F, Lafage V, Patel A, Farcy JP. Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976). 2009;34:1828–1833. [DOI] [PubMed] [Google Scholar]
- 23.Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate? An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976). 2010;35:2224–2231. [DOI] [PubMed] [Google Scholar]
- 24.Schwab FJ, Blondel B, Bess S, Hostin R, Shaffrey CI, Smith JS, Boachie-Adjei O, Burton DC, Akbarnia BA, Mundis GM, Ames CP, Kebaish K, Hart RA, Farcy JP, Lafage V; International Spine Study Group (ISSG). Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976). 2013;38:E803–E812. [DOI] [PubMed] [Google Scholar]
- 25.Smith JS, Klineberg E, Schwab F, Shaffrey CI, Moal B, Ames CP, Hostin R, Fu KM, Burton D, Akbarnia B, Gupta M, Hart R, Bess S, Lafage V; International Spine Study Group. Change in classification grade by the SRS-Schwab Adult Spinal Deformity Classification predicts impact on health-related quality of life measures: prospective analysis of operative and nonoperative treatment. Spine (Phila Pa 1976). 2013;38:1663–1671. [DOI] [PubMed] [Google Scholar]
- 26.Tamai K, Buser Z, Paholpak P, Seesumpun K, Nakamura H, Wang JC.Can C7 slope substitute the T1 slope? An analysis using cervical radiographs and ninematic MRIs. Spine (Phila Pa 1976). 2017 Aug 1. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 27.Vialle R, Levassor N, Rillardon L, Templier A, Skalli W, Guigui P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am. 2005;87:260–267. [DOI] [PubMed] [Google Scholar]
- 28.Yukawa Y, Kato F, Suda K, Yamagata M, Ueta T. Age-related changes in osseous anatomy, alignment, and range of motion of the cervical spine. Part I: Radiographic data from over 1,200 asymptomatic subjects. Eur Spine J. 2012;21:1492–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhu Z, Xu L, Zhu F, Jiang L, Wang Z, Liu Z, Qian BP, Qiu Y. Sagittal alignment of spine and pelvis in asymptomatic adults: norms in Chinese populations. Spine (Phila Pa 1976). 2014;39:E1–E6. [DOI] [PubMed] [Google Scholar]