Abstract
To investigate the clinical application ofthe “three lines and one plane” concept as the anatomic landmarks during laparoscopic common bile duct exploration (LCBDE).
From January 2014 to February 2017, 148 cases of LCBDE performed in the General Surgery Department of the 2nd affiliated Hospital of Anhui Medical University were recruited, and analyzed in this study. “Three lines and one plane” was applied as anatomical landmarks during LCBDE, and the perioperative clinical outcomes were analyzed.
No serious operational complications occurred in all the patients in this study. Two cases (1.4%) was converted to open operation. Two other cases (1.4%) suffered post-operative bile leakage and were cured by conservative treatment. All patients recovered uneventfully.
Anatomical landmarks of “three lines and one plane” is benefit in helping surgeons to build a three-dimensional (3D) anatomical construction, and avoiding the operative injury of the bile duct, and vessels.
Keywords: anatomic landmarks, choledochostomy, cholelithiasis, laparoscopic surgery
1. Introduction
Laparoscopic common bile duct exploration (LCBDE) has been widely performed for the treatment of choledocholithiasis. However, for patients accompanied with severe tissue edema, and dense adhesions caused by inflammation, how to avoid the risk of biliary tract injury is always a challenge, especially, for patients with anatomic biliary variations.[1,2]
Concept of “three lines and one plane” was formed, and applied to enhance the safety of the dissection of biliary, and vessel system during operation. “Three lines and one plane” includes 4 anatomical markers: the upper curve of the duodenal bulb (Line A), the arc incisure of the hepatic pedicle of the right posterior lobe (Line B), the middle line between the common hepatic duct, and the common bile duct ([CBD], [Line C]), and the plane of the hilar plate (Plane D) (Fig. 1).
Figure 1.
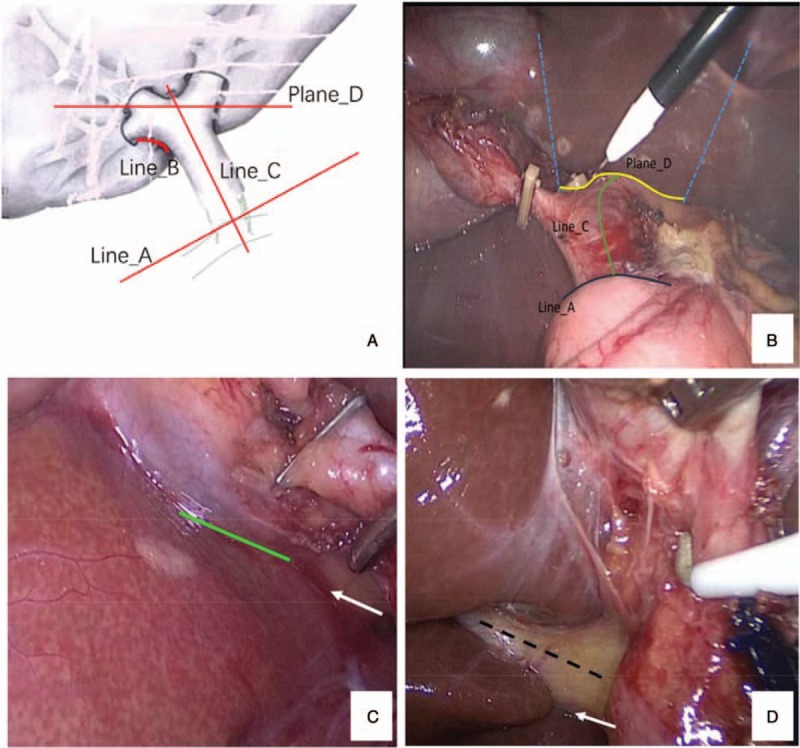
Anatomical landmarks of “three lines and one plane”. (A) schematic drawing of the “three lines and one plane”; (B) the black line shows the locus of Line A, the green line shows the outline of Line C, the yellow line shows the outline of Plane D. the left blue dashed line shows fissure of ligamentum teres, and its extension line. The right blue dashed line shows the left lateral edge of gallbladder, and its extension line. (C) one case without clear Rouviere's sulcus but with clear Plane D (white arrow), the green line is sometimes mistakenly regarded as the Line B in cases with low cystic duct confluence; (D) one case with clear Rouviere's sulcus (the black dotted line), and the white arrow shows the location of Line B. Line A: anatomical markers: the upper curve of the duodenal bulb, Line B: the arc incisure of the hepatic pedicle of the right posterior lobe, Line C: the middle line between the common hepatic duct, Plane D: the common bile duct, and the plane of the hilar plate.
In this study, clinical data of 148 patients underwent LCBDE performed according to the “three lines and one plane” concept were retrospectively, analyzed to evaluate its clinical value.
2. Patients and methods
2.1. Patients
Totally, 148 cases (70 men and 78 women) were subjected to this study. All the patients were treated in the general surgery department of the 2nd affiliated Hospital of Anhui Medical University from January 2014 to February 2017. All the patients were diagnosed with ultrasonography, and magnetic resonance cholangiopancreatography (MRCP) before operation. The complains observed including perioperative abdominal pain, jaundice, chills, and fever. All the recruited patients were suitable for general anesthesia, without severe cardiac, or pulmonary accompanying diseases. Every patient was sent to LCBDE treatment after the consultation of endoscopic physicians, and was not suitable for endoscopic retrograde cholangiopancreatography (ERCP). Intraoperative cholangiography (IOC) was not performed in this study. LCBDE was regard difficulty if the gallbladder or bile duct cannot be identified easily, by laparoscopy due to severe inflammation or anatomic biliary system variation. This study was carried out after the approval from the hospital's ethics board.
Anaesthesia and position: general anaesthesia, and tracheal cannulation were performed, and supine position with head high left was set routinely. Laparoscopic bile duct exploration was routinely, performed with 4-ports. A other 5th port was added, and placed on the left-up quadrant under laparoscope in order to dissect the adhesions if the patients experience the previous abdominal operation.[3] Artificial pneumoperitoneum pressure was set as 12 to 14 mmHg (1 mmHg = 0.133 kPa).
2.2. Operation procedure
Firstly, the duodenal bulb and the CBD are exposed. In most cases, the Line A is clear, and the CBD can be defined easily. If there are severe edema, and adhesions of extrahepatic bile duct caused by inflammation, we dissect adhesions along the Line A. In cases of shortened hepatoduodenal ligament due to severe inflammatory adhesions, we dissect the serosa coat of the hepatoduodenal ligament near the Line A, that is beneficial to drop the duodenum, and reveal the CBD easily. Occasionally, ampulla of gallbladder behind, and adhered to the duodenal bulb is dissociated simultaneously.
Subsequently, the Line B could be exposed through pulling up the ampulla of gallbladder anteriorly and cephalad, or after exposing the right, and posterior of hepatoduodenum ligament. The right posterior edge curve of gallbladder is normally, clear, and separated from Line B. The posterior of Calot's triangle is bluntly, dissociated, and exposed along the gallbladder's right posterior edge curve during operation.
However, in cases with the adhesions between the gallbladder, and duodenum caused by the severe inflammation, we dissected the posterior of Calot's triangle by cutting the posterior serosa of gallbladder, about two centimeters onto the Line B (ventral hilar plate). On the difficulty condition, such as the severe adhesions with the serosa of the posterior gallbladder, and the right hepatic pedicle, attentions are needed to avoid the injury of the anomalous cystic duct (origin from the trunk, or branch of right hepatic duct),[2] or accessory hepatic duct.[4]
In some patients, the junction of cystic duct, and common duct is low, and the location of the Line B is deep, so the dissection should be more carefully. If necessary, the Line A is dissected to expose the posterior of the duodenum to avoid the long residual cystic duct, and bile duct injury, accompanied with reference of Line B.
After dissecting the posterior of Calot's triangle, we reveal “the plane of the hilar plate” (Plan D) along the inferior surface of quadrate lobe (segment IVa). The dissection of the gallbladder is started from the serosa cutting above the “Plane D” and on the right of quadrate lobe, then we dissect softly, and bluntly, onto the “Plane D” till the exposure of the cystic duct, and artery. If there are severe adhesions, or incarcerated stones in cystic duct, we dissect on the ventral side of the plane, as the right anterior hepatic pedicle is behind the hilar plate usually.
The fourth step is the LCBDE. The inferior surface of the quadrate lobe, and duodenum bulb usually not be affected by inflammation, and is easily, to be exposed. We choose the midpoint of the inferior surface of the quadrate lobe as a landmark and imagine a line (Line C) from bifurcation point of hepatic ducts to the midpoint of duodenum bulb. Fine needle aspiration is performed routinely, before CBD incision. According to the diameter of CBD, the incisional of CBD close to Line C, or slightly, on the right side is advised. The stone extraction was achieved by intraoperative fiberoptic cholangioscopic lithotomy, or lithotripsy. Interrupted figure 8 sutures of CBD are used for T-tube drainage, and continuous suture for primary closure of the CBD.
3. Results
LCBDE was performed for 148 patients (70 men and 78 women) from January 2014 to February 2017. Among them, 30 cases experienced previous abdominal operations, such as open cholecystectomy (23 cases), open choledocholithotomy (4 cases), and other abdominal surgery history (3 cases). One case was diagnosed as Mirizzi's syndrome type I, two cases were Mirizzi's syndrome type II. Another one case was with gallbladder colon fistula. The 84 cases were confirmed with acute or subacute inflammation after operation.
The mean time of preparation for surgery was 2 days (range 1–4 days). The mean age of patients was 57 years (range 17–85 years). The mean operative time was 142 minutes (range 73–212 min). The mean length of post-operative hospital stay was 6.4 days (range 3–10 days). Two cases (1.4%) were converted to open procedure (1 case due to the severe hilar adhesions with colon caused by previous operation, 1 case with gallbladder colon fistula). Complete stone clearance during operation was successful in all patients (100%) Table 1.
Table 1.
Perioperative clinical outcomes.
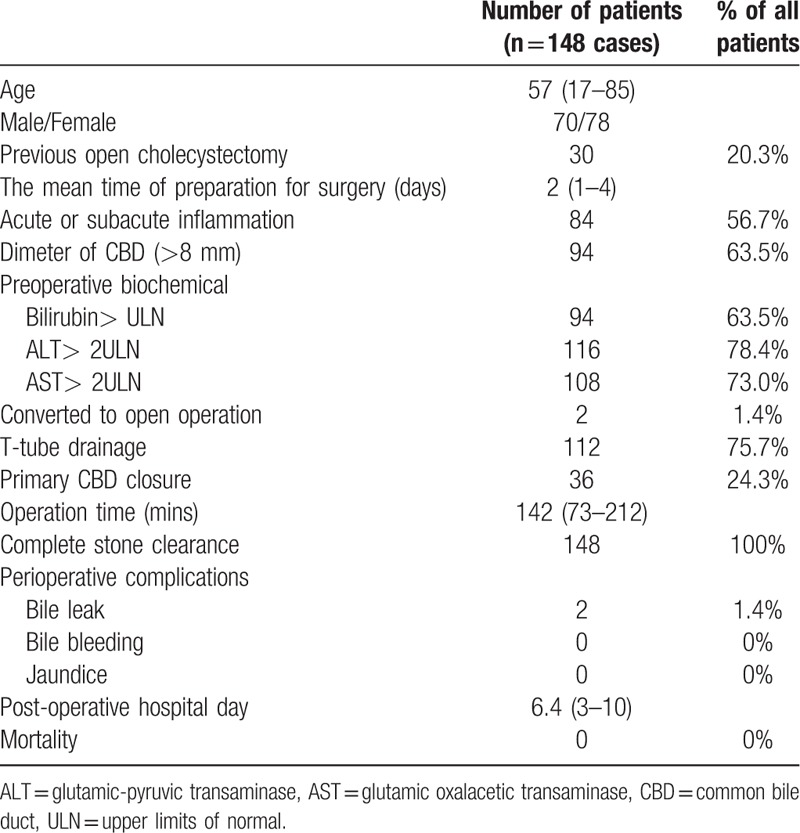
Hundred twelve patients had a T-tube placed, and the other 36 patients underwent primary CBD closure. The peritoneal drainage was set after LCBDE for 3 to 5 days routinely. No serious operative complications occurred, such as massive hemorrhage, bowel, or bile duct injury, right hepatic artery, or portal vein injury. Two patients with T-tube drainage underwent post-operative persistent bile leaks (1.4%), one was caused by the post-operative T-tube slipping off, and then cured by endoscopic nasal biliary drainage (ENBD); the other one was the mild bile leakage, and then cured by peritoneal drainage for 26 days. There was no bile leakage happen after the laparoscopic primary CBD closure. The follow-up time was 5 to 41 months, and there was no mortality, and no calculus recurrence.
4. Discussion
The unexpected bile duct, and hepatic artery injuries during LCBDE usually cause serious complications. It is recommended[5] that the operation should be done within the first 72 hours for acute cholelithiasis accompanied with cholangitis. However, for cases that miss the primary surgical treatment within the first 72 hours, the difficulty of dissection, and the risk of bile duct injury during LCBDE is obviously increased, especially, for patients with anatomic variation of biliary system. Fortunately, with the application of “three lines and one plane” concept, no serious complication occurred in all the patients in this study.
Some anatomic landmarks have been reported as the reference during the LCBDE, such as the gallbladder neck, gallbladder triangle, and cystic lymph node, et al.[4,6,7] However, in case of severe tissue adhesions in the hilar region, or tissue edema in Calot's triangle caused by previous surgical operation, or subacute inflammation, these landmarks are difficult to be revealed. Rouviere's ditch is a good anatomic landmark for gallbladder, but not all the patients could show Rouviere's ditch clearly.[8] In contrast, anatomic landmarks of “three lines and the plane” of the hilar plate are relatively, fixed, and not affected by anatomical variation, or inflammatory adhesions. Each anatomic part in this concept will be described separately, as following:
Line A: The serosa of hepatoduodenal ligament close to the duodenumbulb is relatively loose and can be easily dissected. With the protection of the duodenum, the inflammation of the serosa around CBD closed to the duodenal bulb is mild, and can be dissected easily. Therefore, we recommend reveal the duodenal bulb firstly, near the superior border of duodenal bulb, and then the CBD can be identified easily. On the other hand, the middle line of the CBD can be exposed easily, onto the midpoint of duodenum bulb in patients without severe inflammation (Fig. 1B).
Line B: the arc incisura is the lower edge of the right posterior hepatic pedicle that locates the junction where the hepatic pedicle goes into the right liver hilum.[9] The Line B can be identified by pulling the neck of gallbladder anterosuperior, and leftward, or after exposing the right, and posterior of the hepatoduodenum ligament. In cases such as low confluence of cystic ducts, or the occurrence of dense, flaky gastrointestinal adhesions to the gallbladder fossa caused by previous surgeries, Line B may be buried deeply, so we should fully, expose the right, and posterior of hepatoduodenum ligament with the Line A as anatomic reference, to avoid the long stump of cystic duct, or injury of the CBD. Kurata[4] found that a severe, and common anatomical variation that aberrant right posterior hepatic duct goes into the extrahepatic bile duct, cystic duct, or cystic body directly, and there is 6.8% aberrant right posterior hepatic duct approximately. Previous reports[9–11] show that the bile duct injury in cases with anatomic anomaly of the bile duct was 3.2 to 8.4 times higher than that without anatomic anomaly. However, according to the anatomic concept of Glisson sheath,[12] ectopic right posterior hepatic duct is in Glisson sheath, and beneath the “Line B” too. By autopsy, Surjan[6] reported that the average diameter of right posterior hepatic pedicle is about 18 mm (18.4 ± 5.6), so we choose to dissect the serosa of posterior triangle 2 centimeters higher above the incisura plane (ventral) to avoid the injury of the right posterior Glisson sheath. Larger distance from the “Line B” is especially, useful for obesity patients, or patients with bigger liver volume to avoid the injury of the right posterior hepatic duct, or vessel that aberrant, or accessory. In case that the incisura (Line B) is lower, or deeper, the gallbladder neck should be uplifted enough to expose the “Line B” which is helpful to avoid long residual cystic duct (Fig. 1C).
Line C: The junction of the left, and the right hepatic ducts locates around the inferior surface of the quadrate lobe,[9] but no literature has clarified the exact projection of the midline of the common hepatic duct, and the CBD. For patients without severe inflammation in ligamentum hepatoduodenale, the bifurcation of left, and right hepatic duct can be observed at the plane of the hilar plate, and the inferior surface of the quadrate lobe. However, if patients have severe hilar adhesions, such as the history of biliary tract surgery, it is hard to determine the location of the CBD. In these cases, the inferior surface of the quadrate lobe is reported as the anatomical reference, and be used to define an optimal starting point for dissection of the biliary cystic triangle.[13] If the shape of the quadrate lobe is rectangular, we choose the midpoint of its inferior surface of the quadrate lobe as a landmark, and if it is pyramidal, the peak was selected as the landmark. As a result, Line C, from hepatic ducts junction to the midpoint of duodenum bulb, is established as the anatomical reference during operation (Figs. 1A and B)
Application of the Line C has 3 important benefits: First, the tissue on the left side of the Line C of hepatoduodenal ligament should not be dissected sharply, for avoiding damaging the proper hepatic artery. Second, incision along the midpoint of the CBD, or a little right to the Line C is helpful to avoid cutting into the cystic duct, or the confluence when patients with low junction of cystic duct. However, we are not sure whether the define of the Line C is applied in the condition of the hepatic portal translocation which usually, occurs in patient with severe intrahepatic hepatolithiasis, and 1-sided the liver atrophy. So, more studies are needed to figure out this question.
Plane D: The inferior surface of the quadrate lobe, and its horizontal line[9] is clearer than Rouviere's channel plane, and more convenient to be the reference when dissecting the Calot's triangle, or posterior triangle of gallbladder. Anterior right, and left hepatic pedicle are located at dorsal side of this plane, and right anterior segment's Glisson is beneath the Plane D in Calot's triangle area. There are many variations of right hepatic duct, or right hepatic artery in Calot's triangle, and posterior triangle of gallbladder. Cystic artery variation is more unpredictable.[4] Although the right hepatic artery, and the cystic artery atypically run to the common hepatic duct or CBD,[8] they are located below the serosal tunic of the hepatoduodenal ligament, and beneath the “Plane D”. Dissecting tissues hastily, should be avoid if the vessels beneath the Plane D, especially, in Calot's triangle area. However, dissection above the hilar plate along the vessels is safer, and easily, which is benefit in avoiding right, or right anterior hepatic artery injury. Two of included cases in this study have abnormal vessels in the Calot's triangle that beneath the Plane D, which is similar to cystic artery but a little thicker. Then, we track the vessels above the hilar plate, and find that it divided into 1 to 3 branches that go into gallbladder, and the main trunk goes into the edge of the gallbladder bed. Whether the vessel is considered as the right, or right anterior hepatic artery is not confirmed finally. However, it is wise to protect these vessels during operation. Based on these findings, we recommend that if anatomic structure is unclear, dissection of the serosa of gallbladder, and bile duct above the plane of the hilar plate is necessary, and bluntly, dissection is helpful to avoid damaging right anterior hepatic Glisson structure.
For Mirizzi's Syndrome patients, open the cystic duct, and take out the incarcerated stones beside the ventral of the Plane D is benefit to the CBD protection. In this study, 1 Mirizzi's syndrome type I case was treated with the procedure we descripted above. the other 2 type II cases underwent the cystic duct incision above the Plane D, and we found that the coloboma of the bile duct was less than the one third of the diameter, so the excessive injury of the bile duct was avoided. T-tube was placed in all the 3 patients 1 to 6 months, and no bile duct stricture occurred.
The concept of “critical-view-of-safety approach” is recommended to be applied during laparoscopic cholecystectomy.[5] The setting of “three lines and one plane” as the anatomic markers is an important part of the “critical-view-of-safety approach” according to the findings of this study. For patients with severe adhesions, or aberrant cystic ducts, application of “three lines and one plane,” and clearly exposure of these landmarks during operation is benefit in enhancing the safety, and efficiency of the LCBDE.
5. Conclusions
Anatomical landmarks of “three lines and one plane” is benefit in helping surgeons to build a three-dimensional (3D) anatomical construction, and avoid operative injury of the bile duct, and vessels.
Author contributions
Conceptualization: Lei Wang, Chunli Wu, Xiaoping Geng.
Data curation: Lei Wang, Dachen Zhou.
Funding acquisition: Hui Hou.
Investigation: Dachen Zhou.
Project administration: Hui Hou.
Writing – original draft: Lei Wang, Dachen Zhou, Xiaoping Geng.
Writing – review & editing: Lei Wang, Dachen Zhou, Xiaoping Geng.
Footnotes
Abbreviations: CBD = Common bile duct, ERCP = Endoscopic retrograde cholangiopancreatography, IOC = Intraoperative cholangiography, LCBDE = Laparoscopic common bile duct exploration, MRCP = Magnetic resonance cholangiopancreatography.
The authors report no conflicts of interest.
References
- [1].Harrison VL, Dolan JP, Pham TH, et al. Bile duct injury after laparoscopic cholecystectomy in hospitals with and without surgical residency programs: is there a difference? Surg Endosc 2011;25:1969–74. [DOI] [PubMed] [Google Scholar]
- [2].Singh K, Ohri A. Anatomic landmarks: their usefulness in safe laparoscopic cholecystectomy. Surg Endosc 2006;20:1754–8. [DOI] [PubMed] [Google Scholar]
- [3].Zerey M, Haggerty S, Richardson W, et al. Laparoscopic common bile duct exploration. Surg Endosc 2017;Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- [4].Kurata M, Honda G, Okuda Y, et al. Preoperative detection and handling of aberrant right posterior sectoral hepatic duct during laparoscopic cholecystectomy. J Hepatobiliary Pancreat Sci 2015;22:558–62. [DOI] [PubMed] [Google Scholar]
- [5].Buddingh KT, Nieuwenhuijs VB. The critical view of safety and routine intraoperative cholangiography complement each other as safety measures during cholecystectomy. J Gastrointest Surg 2011;15:1069–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Surjan RC, Makdissi FF, Machado MA. Anatomical basis for the intrahepatic glissonian approach during hepatectomies. Arq Bras Cir Dig 2015;28:128–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Sazhin VP, Sazhin IV, Pod”iablonskaia IA, et al. Etiology of “difficult” laparoscopic cholecystectomy. Khirurgiia (Mosk) 2016;1:61–6. [DOI] [PubMed] [Google Scholar]
- [8].Andall RG, Matusz P, du Plessis M, et al. The clinical anatomy of cystic artery variations: a review of over 9800 cases. Surg Radiol Anat 2016;38:529–39. [DOI] [PubMed] [Google Scholar]
- [9].Hugh TB. New strategies to prevent laparoscopic bile duct injury–surgeons can learn from pilots. Surgery 2002;132:826–35. [DOI] [PubMed] [Google Scholar]
- [10].Adamsen S, Hansen OH, Funch-Jensen P, et al. Bile duct injury during laparoscopic cholecystectomy: a prospective nationwide series. J Am Coll Surg 1997;184:571–8. [PubMed] [Google Scholar]
- [11].Suhocki PV, Meyers WC. Injury to aberrant bile ducts during cholecystectomy: a common cause of diagnostic error and treatment delay. AJR Am J Roentgenol 1999;172:955–9. [DOI] [PubMed] [Google Scholar]
- [12].Yamamoto M, Katagiri S, Ariizumi S, et al. Glissonean pedicle transection method for liver surgery (with video). J Hepatobiliary Pancreat Sci 2012;19:3–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Rajkomar K, Bowman M, Rodgers M, et al. Quadrate lobe: a reliable landmark for bile duct anatomy during laparoscopic cholecystectomy. ANZ J Surg 2016;86:560–2. [DOI] [PubMed] [Google Scholar]


